In the midst of the very public debate on health, the interface between university and medical school remains largely hidden. It is, however, an important influence not only on academic activity and resources but increasingly on commercial interests. The changing roles and responsibilities of medical schools affect many aspects of health, education, and regional development. The ways in which medical schools respond to different challenges should be understood if there is to be agreement on the opportunities and threats facing modern medical education.
Summary points
Medical education comprises a decreasing proportion of the workload of medical schools
Medical schools have close links with the health departments, but links with the funding councils and departments of education may be less robust, and funding streams are complex and poorly understood
Research interests of medical schools and their parent university may take precedence over teaching commitments and clinical duties
Curricular reform has been stimulated by the General Medical Council since graduation is linked to provisional GMC registration, and the public and profession must agree on standards expected at graduation
Medical schools
We all know what they are, but a succinct definition is now elusive. Of course, a medical school educates undergraduate medical students, but that role is decreasing as medical education moves with patients to the community and primary care. Indeed, colleagues in the NHS now undertake at least 70% of the clinical teaching and increasingly participate in planning the curriculum and assessment. Given the considerable diversity of arrangements adopted by different universities, the only other features medical schools have in common are a robust research base, clinical academic staff, and public interest. Many have substantial numbers of undergraduate and postgraduate students in disciplines other than medicine.
A medical school is an integral part of its parent university and is not autonomous. It is, however, often some distance from the main campus and perceived by academic colleagues as remote. Because of the strategically important position it occupies between the NHS and the university, the organisational structure and funding arrangements are complex and are often only imperfectly appreciated. Medical schools enjoy close links with the health departments, whereas the education departments responsible through the funding councils for the universities generally seem less involved.
Universities
These too have changed markedly in recent years as the higher education system expanded. With the abolition of the distinction between universities and polytechnics in 1992, there are now 90 universities in the United Kingdom. As undergraduate numbers have risen, with more than 35% of school leavers (and around 50% in Scotland) entering higher education, the proportion of medical students, whose numbers are controlled, has inevitably fallen (table). Their entry qualifications, however, remain impressively high.
These changes, which are in many ways to be welcomed, have resulted in medical schools having less influence within their parent university and within the higher education system. There is, for example, now no medical member on the Higher Education Funding Council for England and only one medically qualified vice-chancellor. For the moment, it is still possible for an eminent clinician to write of his junior colleagues: “They pick up from their seniors a weariness that comes from continuous bombardment by the local chief executive or vice chancellor, neither of whom (for different reasons) gives a fig for clinicians whether senior or junior.”1
Several other factors contribute to the tensions that may exist between medical school and university. The funding formulas used by the higher education funding councils to allocate resources for teaching are pragmatic and not related to the costs incurred. Although universities are advised to use their judgment in adapting this national approach for local use, many prefer to reflect the funding council formula in their own model for allocating resources. The result is often a vigorous debate within the university as budgets are set. There is, moreover, now a substantial (19%) imbalance in the resources allocated for teaching in England and Scotland—with consequences for academic staffing.
In Britain a primary medical qualification is legally linked to provisional registration with the General Medical Council and patient care. As the public have a right to expect high and consistent standards of care from all registered medical practitioners, differences in funding arrangements agreed by the funding councils and adopted by the universities have an inevitable effect on the ability of medical schools to meet their commitments. The result may be an increase in the teaching duties of local NHS colleagues. In this way decisions taken nationally, sometimes without a clear appreciation of the consequences, can result in friction at a local level between medical school and university.
Medical academic staff
Various national initiatives, stimulated by the House of Lords, have identified problems in recruitment, research training, and retention of high quality medical academic staff. Some of the problems relate to the interface with the NHS, but several occur within the academic sector. The recent longstanding salary dispute, now happily resolved by government action, was unsettling and helped place universities and funding councils in an invidious position. The Bett report2 has recently endorsed the linkage of basic salaries for clinical academic staff with the NHS equivalent. The distinction awards and discretionary points paid by the NHS, paradoxically, help emphasise the different situation in which clinical academic staff find themselves. It is accepted that clinical academic staff must have equal access to these awards if recruitment is to be successful.
Several groups, including the Academy of Medical Sciences and the Royal College of Physicians (London), are now considering how best to support the needs of clinical lecturers. It is an indication of the weakness of the medical schools that the research assessment exercise did not distinguish between clinical lecturers, who are young doctors in training unable to undertake full time research, and the career lecturer posts in academic disciplines other than medicine. The resulting financial penalty on medical schools has reduced the number of university funded posts for some of our most able young clinicians.
Research
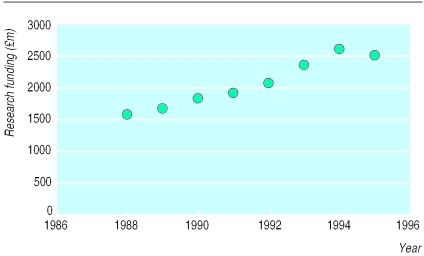
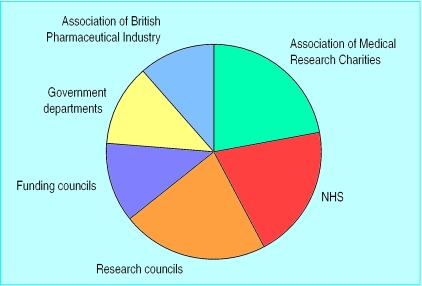
Of major interest to a medical school and its university is its research potential. Local enterprise companies, entrepreneurs, government, and now the funding councils are also aware of the substantial and increasing funding available (fig 1). The total research funding available for biomedical research is now likely to be in excess of £2bn a year—largely but not exclusively from public sources (fig 2). This figure includes an estimated 10% of pharmaceutical research expenditure as being accessible to universities.
Figure 1.
Total annual research expenditures by Medical Research Council, Association of the British Pharmaceutical Industry, and Association of Medical Research Charities in 19953
Figure 2.
Sources of UK funding for biomedical research in the public domain in 19953
Despite funding from the NHS and drug companies, clinical research seems less secure than basic science. Indeed, the research undertaken in clinical departments is commonly basic rather than strategic or applied. This means that clinician scientists are now less likely to link a research interest directly to patient care—more commonly the research will have no overt clinical application in the immediate future. Clinical duties are thus more likely to be seen as a (necessary) distraction from the research laboratory than an integral part of the job. Health services research may help correct this perceived imbalance, but this has yet to acquire the same status as biomedical studies.
The increasing separation of research from clinical practice is often encouraged by the parent university concerned both with the income from research grants and contracts and with the next research assessment exercise, which will determine its future core research funding. This dual support system, with the funding councils providing the infrastructure for research through the research assessment exercise and the research councils supporting specific research projects, is unique to Britain and evokes particular responses from the universities. Strengths and weakness are debated endlessly. The research assessment exercise, however, is largely retrospective, assessing the quality of research undertaken in the previous five years. Moreover, the funding available through the Association of Medical Research Charities, although very substantial (fig 2), does not carry the same amount of “overhead funding” as do grants from the research councils. A university may therefore believe that its medical school's research programme has to be subsidised from other faculties—or at best that the overhead income is less. These debates are likely to be resolved only when information from the current review of university funding (transparency review) becomes available.
The importance of this issue for the UK economy is emphasised by the joint infrastructure fund, in which the government participates and the Wellcome Trust has a leading role. More than £1.2bn has been provided to strengthen the research facilities and equipment required for innovative studies in biomedical science.
Clinical duties
Although few if any clinical services are now totally dependent on a medical school, the clinical commitment of academic staff makes a profound contribution to the NHS. On average, clinical academics spend 50-60% of their time on such duties—at university expense. In return the NHS provides an equivalent contribution to medical undergraduate teaching—supported by substantial NHS funding. In most parts of the country, these arrangements require the combined efforts of the medical school, local trusts (and primary care groups), and regional office (health board) to be successful. The arrangements are complicated by the marked variation in the numbers of staff funded by the local NHS and employed by the university: the proportion ranges from 10% to over half of clinical academic staff in different medical schools. Parent universities are commonly aware of these arrangements only in general terms; no allowance for clinical duties is made in the research assessment exercise nor when local budgets are set for the medical school.
Teaching
With their emphasis on research, universities and medical schools are liable to overlook teaching. Curriculum development has been largely stimulated and implemented by initiatives led by the General Medical Council. The impact of the Quality Assessment Agency and the Institute for Teaching and Learning remains uncertain. The lesser importance attached by universities to teaching and learning than to research may not be in accord with the increasing public interest in standards of health care and lifelong learning. The role model of the doctor as teacher is powerful and enduring. A revival of interest in medical education should now link from undergraduate programmes through training posts to meaningful continuous professional development. It is no longer possible to be outstanding in clinical practice, teaching, and research. Becoming selective and concentrating on either research or clinical practice and education is the model increasingly being adopted.4
It is increasingly apparent that high academic attainment is not, by itself, sufficient for medical practice. The public now expects that all doctors will have the attributes outlined by the GMC in Good Medical Practice.5 Several universities and medical schools are now devising procedures to ensure that medical students will graduate with a primary medical qualification only when the institution is assured that they meet these standards as well as conventional academic criteria. The difficulties of incorporating these requirements into university regulations are not insurmountable, and steady, if slow, progress has been made in implementing the recommendations of the related GMC publication Student Health and Conduct.6 Only now are universities taking seriously their responsibilities for the year medical students spend as preregistration house officers. Indeed, the successful implementation of Tomorrow's Doctors7 was greatly assisted by grants from the Departments of Health rather than the Departments of Education.
The way ahead?
The solutions to these difficulties are straightforward. Links between universities and medical schools must be strengthened. The medical profession and public should come together and take the debate to the government, universities, and funding councils. These bodies often believe that many of the perceived problems relate to special pleading from a privileged profession. The linkage, however, between primary qualification and provisional registration to treat patients requires an appreciation of the overall purpose of medical education—which is more than simply the achievement of high academic standards. Clear aims and defined outcomes are essential and are likely to be helped by the involvement of lay people and NHS clinicians.
The commitment to excellence in teaching and learning throughout a professional career must be manifest, and this can be achieved in various ways. One approach would be for the GMC to make more use of its statutory powers to “promote high standards of medical education and coordinate all stages of medical education.” With increasing public interest in the standards of medical education and with changes being introduced to the quality assessment procedures in universities, such an initiative based on agreed standards might be generally welcomed. Robust links with the Quality Assessment Agency would be essential. Tomorrow's Doctors7 had a considerable influence on undergraduate medical education, and The New Doctor8 has greatly improved the preregistration house officer year. It is possible to envisage a similar approach evolving through the training grades to continuous professional development. Indeed, the GMC publication The Doctor as Teacher9 points in that direction. All of these developments are compatible with the principles of clinical governance, and with the general outline of revalidation as it evolves.
The importance of research and acquisition of new knowledge is self evident. Research has many ancillary advantages in terms of staff motivation and retention. To be of value, however, the research must be of high quality, undertaken by trained staff with coordination of major initiatives. It is reassuring that the research assessment exercise is being radically reassessed (but only after the next exercise) and that the Departments of Health are now involved in the process.
Stronger links between health and education are essential. The overall objectives must be agreed by the whole of the profession and pursued by our myriad of medical dynasties—GMC, BMA, medical royal colleges, and medical schools—acting in concert. Coordination at a national policy level would be helped by government agreement. Could devolution help here? Will the Scottish initiatives seeking closer links between the different participants succeed? Anything less will be a public disappointment.
Table.
Changing proportion of medical students among undergraduates in Britain
| No of students
|
||
|---|---|---|
| Year | Total | Medical students |
| 1962 | 321 000 | 20 000 |
| 1998 | 1 900 000 | 25 000 |
Acknowledgments
This article is based on a paper presented at a symposium on careers in academic medicine sponsored by the Joint Consultants Committee and the Department of Health.
Footnotes
Funding: University of Aberdeen
Competing interests: GRDC is chief scientist at the Scottish Executive Health Department, chairman of the GMC Education Committee, and a member of the Scottish Higher Education Funding Council.
References
- 1.Hampton JR. The rise and fall of modern medicine [book review] J R Soc Med. 1999;92:319–320. [Google Scholar]
- 2.Bett M. Independent review of higher education pay and conditions. London: Stationery Office; 1999. [Google Scholar]
- 3.Wellcome Trust. Mapping the landscape. London: Wellcome Trust; 1998. [Google Scholar]
- 4.Levinson W, Rubenstein A. Mission critical—integrating clinician-educators into academic medical centers. N Engl J Med. 1999;341:840–843. doi: 10.1056/NEJM199909093411111. [DOI] [PubMed] [Google Scholar]
- 5.General Medical Council. Good medical practice. London: GMC; 1998. [Google Scholar]
- 6.General Medical Council. Student health and conduct. London: GMC; 1996. [Google Scholar]
- 7.General Medical Council. Tomorrow's doctors. London: GMC; 1993. [Google Scholar]
- 8.General Medical Council. The new doctor. London: GMC; 1996. [Google Scholar]
- 9.General Medical Council. The doctor as teacher. London: GMC; 1999. [Google Scholar]