Although diagnostic and therapeutic decisions in patients with vascular disease are guided primarily by the history and physical examination, the use of non-invasive investigations has increased significantly in recent years, mainly as a result of technological advances in ultrasonography. This article describes the main investigative techniques.
Principles of vascular ultrasonography
In the simplest form of ultrasonography, ultrasound is transmitted as a continuous beam from a probe that contains two piezoelectric crystals. The transmitting crystal produces ultrasound at a fixed frequency (set by the operator according to the depth of the vessel being examined), and the receiving crystal vibrates in response to reflected waves and produces an output voltage. Conventional B mode (brightness mode) ultrasonography records the ultrasound waves reflected from tissue interfaces, and a two dimensional picture is built up according to the reflective properties of the tissues.
Doppler ultrasonography
Ultrasound signals reflected off stationary surfaces retain the same frequency with which they were transmitted, but the principle underlying Doppler ultrasonography is that the frequency of signals reflected from moving objects such as red blood cells shifts in proportion to the velocity of the target. The output from a continuous wave Doppler ultrasonograph is usually presented as an audible signal, so that a sound is heard whenever there is movement of blood in the vessel being examined.
Pulsed ultrasonography
Continuous wave ultrasonography provides little scope for restricting the area of tissue that is being examined because any sound waves that are intercepted by the receiving crystal will produce an output signal. The solution is to use pulsed ultrasonography. The investigator can focus on a specific tissue plane by transmitting a pulse of ultrasound and closing the receiver except when signals from a predetermined depth are returning. This allows, for example, the centre of an artery and the areas close to the vessel wall to be examined in turn.
Duplex scanners
An important advance in vascular ultrasonography has been the development of spectral analysis, which delineates the complete spectrum of frequencies (that is, blood flow velocities) found in the arterial waveform during a single cardiac cycle. The normal (“triphasic”) Doppler velocity waveform is made up of three components which correspond to different phases of arterial flow: rapid antegrade flow reaching a peak during systole, transient reversal of flow during early diastole, and slow antegrade flow during late diastole.
Doppler examination of an artery distal to a stenosis will show characteristic changes in the velocity profile: the rate of rise is delayed, the amplitude decreased, and the transient flow reversal in early diastole is lost. In severe disease, the Doppler waveform flattens; in critical limb ischaemia it may be undetectable.
Examination of an arterial stenosis shows an increase in blood velocity through the area of narrowing. The site(s) of any stenotic lesions can be identified by serial placement of the Doppler probe along the extremities. The criteria used to define a stenosis vary between laboratories, but a twofold increase in peak systolic velocity compared with the velocity in an adjacent segment of the artery usually signifies a stenosis of 50% or more.
Relation between increased blood velocity and degree of stenosis
| Diameter of stenosis (%) | Peak sytolic velocity* (m/s) | Peak diastolic velocity* (m/s) | Internal: common carotid artery velocity ratio† |
|---|---|---|---|
| 0-39 | <1.1 | <0.45 | <1.8 |
| 4-59 | 1.1-1.49 | <0.45 | <1.8 |
| 60-79 | 1.5-2.49 | 0.45-1.4 | 1.8-3.7 |
| 80-99 | 2.5-6.1 | >1.4 | >3.7 |
| >99 (critical) | Extremely low | NA | NA |
*Measured in lower part of internal carotid artery
†Ratio of peak systolic velocity in internal carotid artery stenosis relative to proximal measurement in common carotid artery
By combining the pulsed Doppler system with real time B mode ultrasound imaging of vessels, it is possible to examine Doppler flow patterns in a precisely defined area within the vessel lumen. This combination of real time B mode sound imaging with pulsed Doppler ultrasonography is called duplex scanning. The addition of colour frequency mapping (so called colour duplex or triplex scanners) makes the identification of arterial stenoses even easier and reduces the scanning time.
Investigations of arterial disease
Ankle brachial pressure index
Under normal conditions, systolic blood pressure in the legs is equal to or slightly greater than the systolic pressure in the upper limbs. In the presence of an arterial stenosis, a reduction in pressure occurs distal to the lesion. The ankle brachial pressure index, which is calculated from the ratio of ankle to brachial systolic pressure, is a sensitive marker of arterial insufficiency.
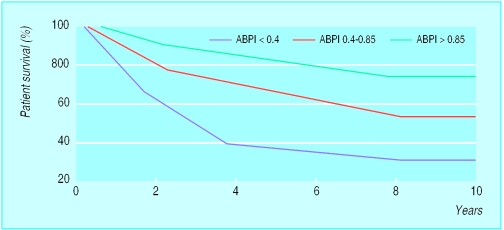
The highest pressure measured in any ankle artery is used as the numerator in the calculation of the index; a value ⩾1.0 is normal and a value <0.9 is abnormal. Patients with claudication tend to have ankle brachial pressure indexes in the range 0.5-0.9, whereas those with critical ischaemia usually have an index of <0.5. The index also has prognostic significance because of the association with arterial disease elsewhere, especially coronary heart disease.
Diabetic limbs
Systolic blood pressure in the lower limbs cannot be measured reliably when the vessels are calcified and incompressible—for example, in patients with diabetes—as this can result in falsely high ankle pressures. An alternative approach is to use either the pole test or measurement of toe pressures. Normal toe systolic pressure ranges from 90-100 mm Hg and is 80-90% of brachial systolic pressure. A toe systolic pressure <30 mm Hg indicates critical ischaemia.
Walk test
Exercise testing will assess the functional limitations of arterial stenoses and differentiate occlusive arterial disease from other causes of exercise induced lower limb symptoms—for example, neurogenic claudication secondary to spinal stenosis. A limited inflow of blood in a limb with occlusive arterial disease results in a fall in ankle systolic blood pressure during exercise induced peripheral vasodilatation.
The walk test is performed by exercising the patient for 5 minutes, ideally on a treadmill, but walking the patient in the surgery or marking time on the spot are adequate. The ankle brachial pressure index is measured before and after exercise. A pressure drop of 20% or more indicates significant arterial disease. If there is no drop in ankle systolic pressure after a 5 minute brisk walk, the patient does not have occlusive arterial disease proximal to the ankle in that limb.
Duplex scanning
Duplex ultrasonography has a sensitivity of 80% and a specificity of 90-100% for detecting femoral and popliteal disease compared with angiography, but it is less reliable for assessing the severity of stenoses in the tibial and peroneal arteries. Duplex scanning is especially useful for assessing the carotid arteries and for surveillance of infrainguinal bypass grafts where sites of stenosis can be identified before complete graft occlusion occurs and before there is a fall in ankle brachial pressure index. The normal velocity within a graft conduit is 50-120 cm/s. As with native arteries, a twofold increase in peak systolic velocity indicates a stenosis of 50% or more. A peak velocity <45 cm/s occurs in grafts at high risk of failure.
Uses of colour duplex scanning
| Arterial | Venous |
| • Identify obstructive atherosclerotic disease: | • Diagnosis of deep vein thrombosis above the knee |
| Carotid | • Assessing competence of valves in deep veins |
| Renal | • Superficial venous reflux: |
| • Surveillance of infrainguinal bypass grafts | Assessing patient with recurrent varicose veins |
| • Surveillance of lower limb arteries after angioplasty | Identify and locate reflux at saphenopopliteal junction |
| • Preoperative mapping of saphenous vein | |
Identification of distal vessels for arterial bypass grafting
In critically ischaemic limbs, where occlusive disease tends to be present at multiple levels, arteriography often fails to show patent calf or pedal vessels as potential outflows for femorodistal bypass grafting. Alternative non-invasive approaches have been developed for preoperative assessment, including pulse generated run off and dependent Doppler assessment.
Transcranial Doppler ultrasonography
Lower frequency Doppler probes (1-2 MHz) can be used to obtain information about blood flow in arteries comprising the circle of Willis and its principal branches. Mean flow velocities >80 cm/s in the middle cerebral artery, or >70 cm/s in the posterior and basilar arteries, indicate a serious stenosis. Transcranial Doppler scanning has several applications but is especially useful for intraoperative and postoperative monitoring of patients having carotid endarterectomy.
Clinical use of transcranial Doppler scanning in adults
Intraoperative monitoring during carotid endarterctomy: Shunt function Cerebral perfusion
Postoperative montoring after carotid endarterectomy: Detection of emboliFormation of carotid thrombus
Detection of intracranial vasospasm after subarachnoid haemorrhage
Detection of middle cerebral artery disease
Evaluation of collateral circulation in patients with carotid disease
Evaluation of arteriovenous malformations of the brain
Helical or spiral computed tomography
Spiral computed tomography is a new, minimally invasive technique for vascular imaging that is made possible by combining two recent advances: slip ring computed tomography (which allows the x ray tube detector apparatus to rotate continuously) and computerised three dimensional reconstruction. A helical scan can cover the entire region of interest (for example, the abdominal aorta from the diaphragm to the iliac bifurcation) in one 30-40 second exposure, usually in a single breath hold. This minimises motion artefact and allows all the scan data to be collected during the first pass of an intravenous bolus of contrast through the arterial tree—that is during the time of maximal arterial opacification. A large number of finely spaced slices from one scan can then be reconstructed to produce high quality two or three dimensional images of the contrast enhanced vessels.
Magnetic resonance angiography
Magnetic resonance angiography has developed rapidly over the past five years. It has the advantage of imaging a moving column of blood and does not require ionising radiation or iodinated contrast, but the technique has obvious drawbacks in terms of cost efficiency and accessibility to scanners. A variety of imaging sequences are used depending on the vessels being studied and the field strength of the machine. The most commonly used techniques include time of flight, two and three dimensional angiography and phase contrast.
Use of a magnetic resonance imaging scanner with a high field strength (which allows rapid acquisition of data) and a carefully timed bolus of gadolinium contrast enables high quality angiographic images to be obtained in a single breath hold. Magnetic resonance angiography is well established for examining the cerebral vessels and the carotid arteries, and its role in other territories is being extended.
Investigations of venous disease
Venous thrombosis
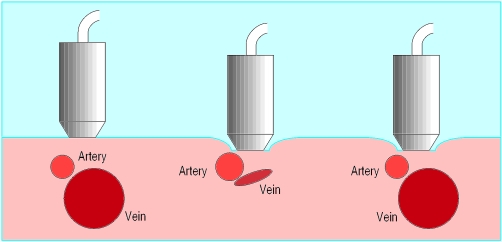
Colour Duplex scanning is both sensitive and specific (90-100% in most series) for detecting proximal deep vein thrombosis. Deep veins and arteries lie together in the leg, and the normal vein appears as an echo-free channel and is usually larger than the accompanying artery.
Venous ultrasonography is a very accurate method of identifying deep vein thrombi from the level of the common femoral vein at the groin crease to the popliteal vein but is less reliable for diagnosing calf vein thrombosis.
Criteria for diagnosis of deep vein thrombosis
Failure of vein to collapse on direct compression
Visualisation of thrombus within lumen
Absent or abnormal venous pulsation on Doppler scanning
Venous reflux
Colour duplex scanning has revolutionised the investigation of the lower limb venous system because it allows instant visualisation of blood flow and its direction. Thus, reflux at the saphenofemoral junction, saphenopopliteal junction, and within the deep venous system, including the popliteal vein beneath the knee and the gastrocnemius veins, can be detected without invasive techniques. Although venous reflux can be assessed with a pencil Doppler, this technique misses 12% of saphenofemoral and 20% of saphenopopliteal junction reflux compared with colour duplex scanning.
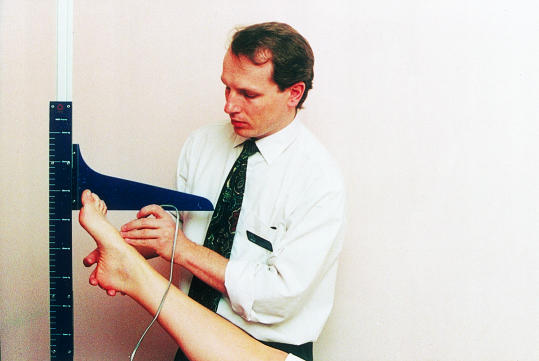
Figure.
Handheld pencil Doppler being used to measure ankle brachial pressure index
Figure.
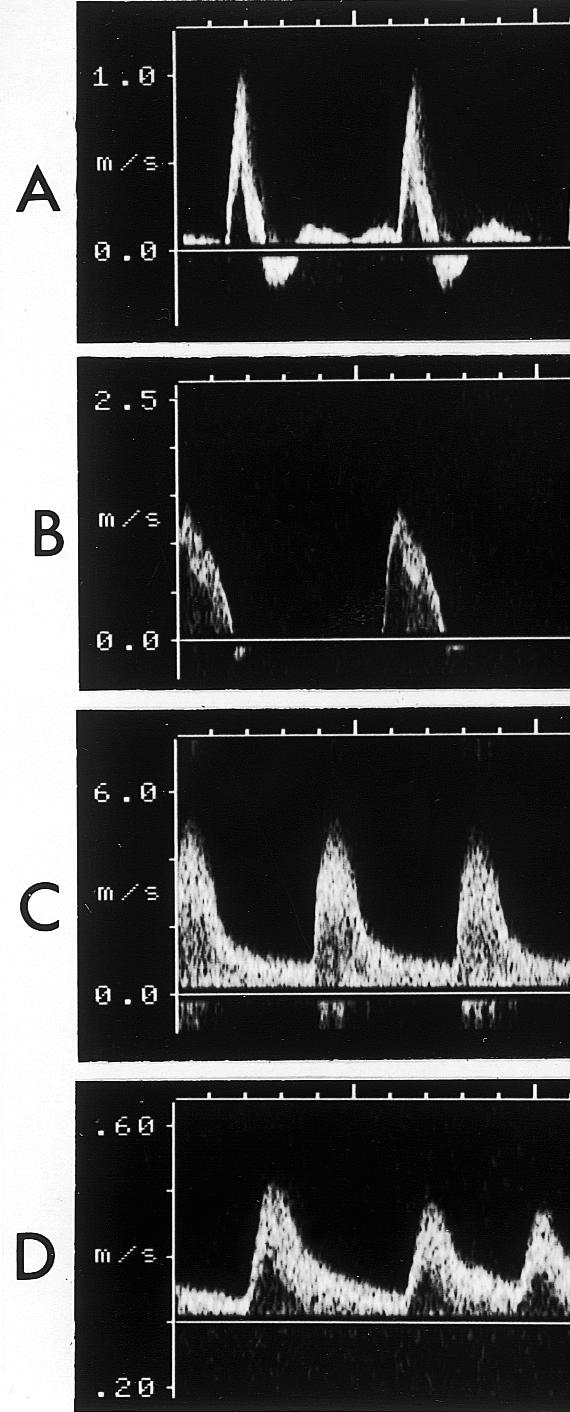
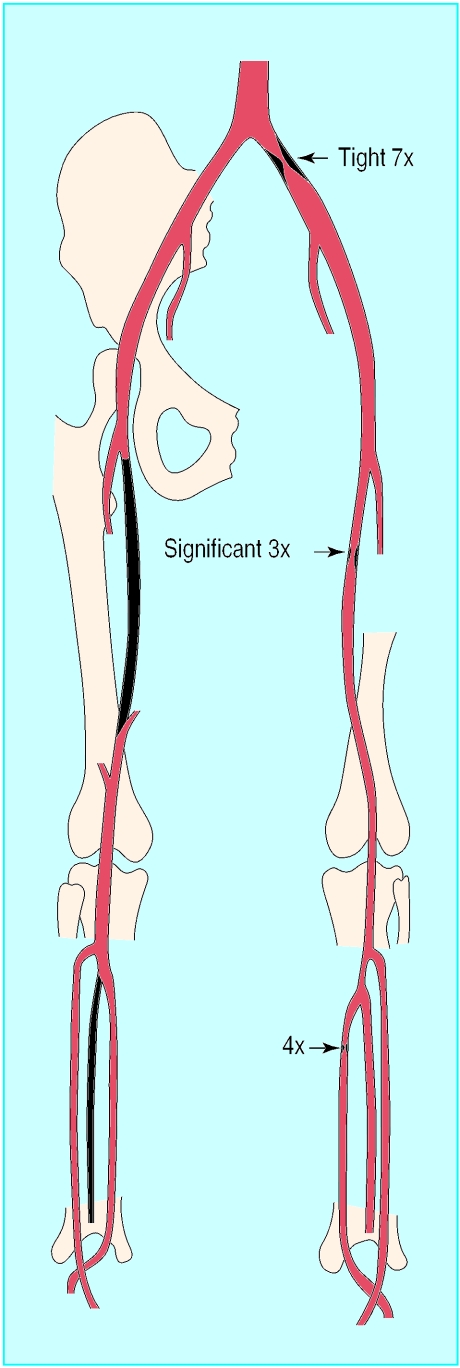
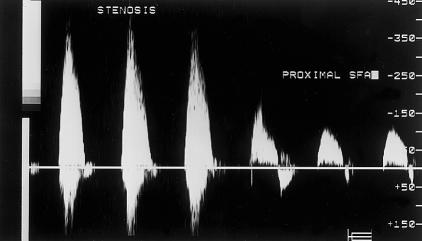
Left: Doppler velocity waveforms: (a) triphasic waveform in normal artery; (b) biphasic waveform, with increased velocity, through a mild stenosis; (c) monophasic waveform, with greatly increased velocity, through tight stenosis; and (d) dampened monophasic waveform, with reduced velocity, recorded distal to tight stenosis. Right: Anatomical chart used to record position of stenoses, showing three stenoses with velocity increases of 7×, 4×, and 3× compared with adjacent unaffected arteries
Figure.
Spectral analysis of blood velocity in a stenosis, and unaffected area of proximal superficial femoral artery. The velocity increases from 150 to 300 m/s across the stenosis
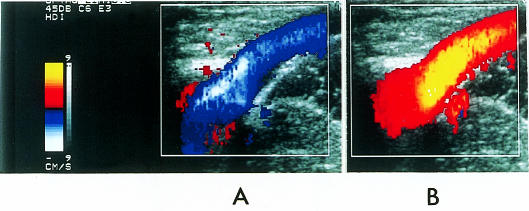
Figure.
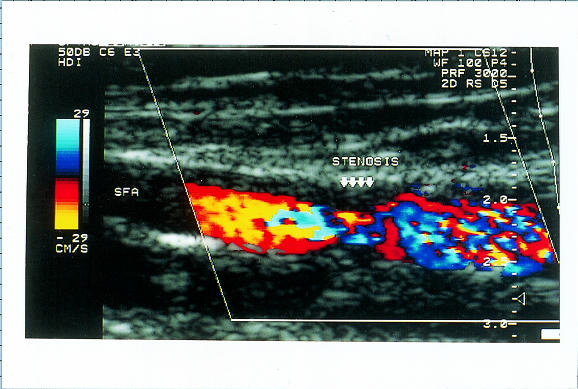
Colour duplex scanning of blood flow through stenosis of superficial femoral artery. Colour assignment (red or blue) depends on direction of blood flow and colour saturation reflects velocity of blood flow. Less saturation indicates regions of higher blood flow and deeper colours indicate slower flow; the absence of flow is coded as black
Figure.
Patient survival according to measurements of ankle brachial pressure index (adapted from McKenna et al, Atherosclerosis 1991;87:119-28)
Figure.
Pole test for measurement of ankle pressures in patients with calcified vessels: the Doppler probe is placed over a patent pedal artery and the foot raised against a pole that is calibrated in mm Hg. The point at which the pedal signal disappears is taken as the ankle pressure
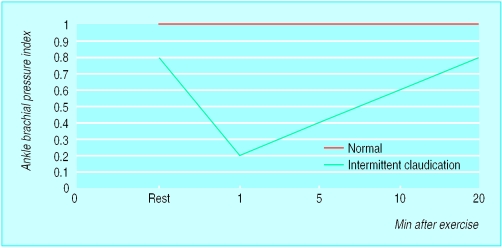
Figure.
Fall in ankle brachial pressure index with exercise in patient with intermittent claudication and normal subject (adapted from Creager, Vasc Med 1997;2:231-7)
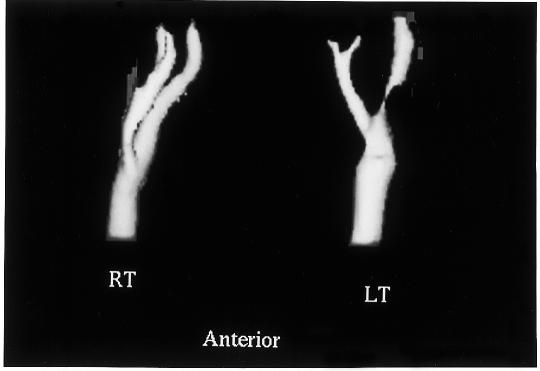
Figure.
Spiral computed tomogram of both carotid systems showing a tight stenosis in the proximal segment of left internal carotid artery
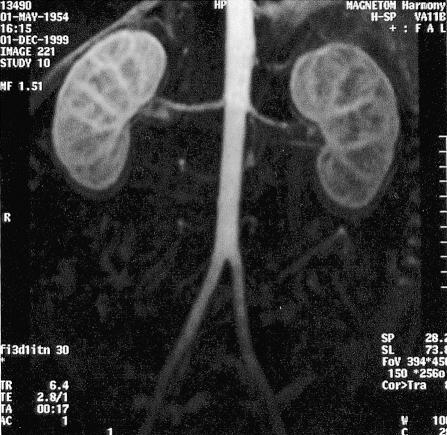
Figure.
Magnetic resonance angiogram using an intravenous bolus of gadolinium contrast showing normal renal arteries
Figure.
Ultrasound detection of deep vein thrombosis. The probe is held lightly on the skin and advanced along the course of the vein (left). Pressure is applied every few centimetres by compressing the transducer head against the skin. The vein collapses during compression if no thrombus is present (middle) but not if a deep vein thrombus is present (right)
Figure.
Colour duplex scanning of saphenopopliteal junction. The calf muscles are manually compressed producing upward flow in the vein (top), which appears as a blue colour for flow towards the heart (panel A). Sudden release of the distal compression causes reflux, seen as a red colour indicating flow away from the heart (panel B)
Acknowledgments
We thank Jean Clarke for expert secretarial assistance; Frances Ryan and Tim Hartshorne (vascular technicians) and colleagues in the vascular laboratories at Derbyshire Royal Infirmary and Leicester Royal Infirmary; Ken Callum and Roddy Nash (vascular surgeons) for helpful input to the manuscript and illustrations; and Jane Wain and staff of the audiovisual department at Derbyshire Royal Infirmary.
Footnotes
David Hinwood is consultant vascular radiologist, Derbyshire Royal Infirmary, Derby.
The ABC of arterial and venous disease is edited by Richard Donnelly, professor of vascular medicine, University of Nottingham and Southern Derbyshire Acute Hospitals NHS Trust (richard.donnelly@nottingham.ac.uk) and Nick J M London, professor of surgery, University of Leicester, Leicester (sms16@leicester.ac.uk). It will be published as a book later this year.