Abstract
Background
Pregnant women and recent mothers face a higher risk of severe illness from Coronavirus disease 2019 due to physiological and immunological shifts during pregnancy, rendering them more vulnerable to inflammatory lung conditions. This susceptibility poses serious threats to both maternal and newborn health. Therefore, it is imperative for pregnant women to be fully informed about Coronavirus disease 2019 and to implement preventive measures. This study aimed to evaluate the collective knowledge, attitudes, and practices related to Coronavirus disease 2019 among pregnant women across Africa.
Methods
The researchers collected studies from multiple databases, including Pub Med/MEDLINE, EMBASE, CINAHL, Science Direct, Scopus, Web of Science, Cochran library, and Google Scholar. A combination of search terms and Boolean operators were utilized to gather relevant literature. Each study underwent quality assessment by five authors independently, using the modified Newcastle Ottawa Scale tailored for cross-sectional research. Statistical analysis was conducted using STATA™ Version 11 software, and meta-analysis was performed using the random-effects (Der Simonian and Laird) method. Heterogeneity was evaluated using I-squared (I2) statistics, and a one-out sensitivity analysis was carried out.
Results
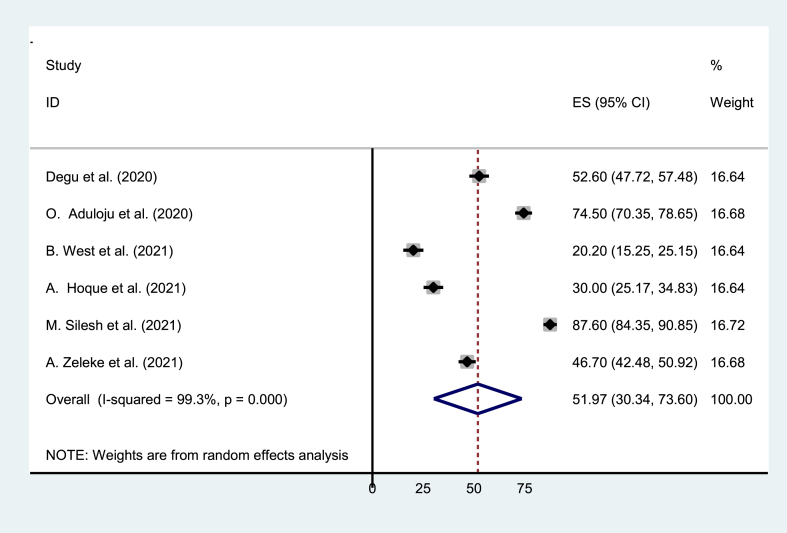
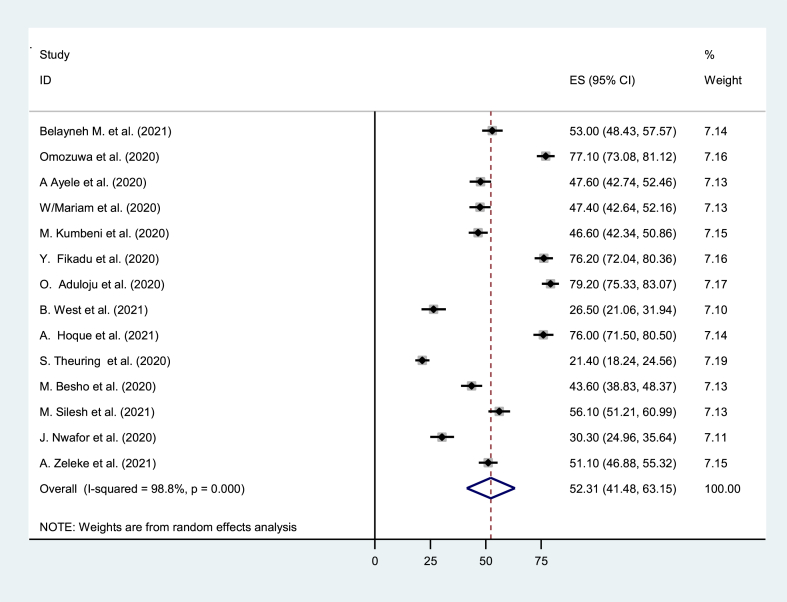
This systematic review and meta-analysis included 19 articles, involving a total of 7852 participants. It revealed that the combined estimated prevalence of good knowledge about Coronavirus disease 2019, positive attitudes, and good practices among pregnant women was found to be 61.8 % (95 % CI: 53.0%–70.65 %; I2 = 98.7 %), 51.7 % (95 % CI: 30.34%–73.6 %; I2 = 99.3 %), and 52.31 % (95 % CI: 41.48%–63.15 %; I2 = 98.8 %) respectively.
Conclusion
This study emphasizes a significant concern: pregnant women exhibit a notable lack of knowledge, positive attitudes, and preventive practices regarding Coronavirus disease 2019. Considering their heightened vulnerability, urgent action is required to improve their understanding, attitudes, and behaviours related to the virus. Healthcare professionals should take proactive measures to educate pregnant women, addressing this crucial gap through various strategies.
Keywords: COVID-19, Knowledge, Attitude, Practice, Pregnant women, Africa
Highlights
-
•
Pregnant women in Africa show 61.8% knowledge but 51.97% attitudes and 52.31% practices for COVID-19 prevention.
-
•
Regional disparities exist: the Western region shows higher knowledge and practice, while the Eastern region has a more positive attitude.
-
•
Healthcare providers should educate pregnant women during prenatal visits to correct misconceptions and promote positive preventive attitudes.
-
•
Tailored interventions for pregnant women are crucial to improve COVID-19 knowledge dissemination and preventive measure adoption.
-
•
Future research should focus on factors contributing to disparities and assessing long-term impacts on maternal and neonatal health outcomes.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), emerged as a global pandemic following its initial outbreak in Wuhan, China. Since then, it has rapidly spread across continents, resulting in an unprecedented public health crisis [1,2].Despite concerted efforts worldwide, the impact of COVID-19 has been profound, with staggering numbers of confirmed cases and fatalities. As of May 27, 2022, the global tally stood at over 525 million confirmed cases and nearly 6.3 million deaths, underscoring the severity of the situation [3]. Within Africa, the pandemic has posed significant challenges, with the continent grappling with over 11 million confirmed cases and 253,000 deaths [4].
Among the vulnerable groups affected by COVID-19, pregnant women stand out due to their heightened susceptibility to severe illness and adverse pregnancy outcomes [[5], [6], [7]] The physiological and immunological changes occurring during pregnancy can exacerbate the severity of COVID-19, potentially leading to complications that pose risks to both maternal and fetal health [[8], [9], [10]]. In this context, vaccination has emerged as a crucial preventive measure, offering protection against the virus for pregnant individuals [[11], [12], [13], [14], [15]]. Despite the safety and effectiveness of COVID-19 vaccines during pregnancy, vaccine acceptance among pregnant women remains a concern globally, including in Africa [16,17]. Various factors, including demographics and educational backgrounds, influence vaccine hesitancy among this population [[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36]].
Understanding the intricate dynamics shaping pregnant women's knowledge, attitudes, and practices regarding COVID-19 prevention is paramount for developing targeted interventions to mitigate risks and improve outcomes. By gaining insights into the factors influencing vaccine acceptance and preventive behaviours among pregnant women in Africa, policymakers can devise tailored approaches to enhance COVID-19 prevention strategies. Therefore, this study aims to assess the knowledge, attitudes, and practices related (KAP) to COVID-19 prevention among pregnant women in the region. The findings of this study will offer valuable insights that can inform the development and implementation of effective policies and interventions aimed at safeguarding the health and well-being of pregnant women and their infants in the face of the on-going pandemic.
2. Materials and methods
2.1. Study design and search strategy
We registered our protocol in International Prospective Register of Systematic Reviews (PROSPERO) (ID: CRD42021291225) and conducted this systematic review and meta-analysis following the guidelines outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [37,38]. We structured our review question using the PICOT format: Population/participants: All pregnant women in Africa; Exposure: COVID-19 preventive measures; Comparator/control: Not applicable; Outcome: The pooled estimated level of knowledge, attitude, and practice about COVID-19 preventive measures; Types of studies: All observational studies reporting data on COVID-19 knowledge, attitude, and practices. In this review, the Comparator (C) was classified as “Not applicable” since all included studies were observational, such as cross-sectional and cohort studies, which do not involve a distinct comparator or control group. Our search strategy comprised three steps. Firstly, we utilized the advanced PubMed search engine to search for studies using all fields and Medical Subject Headings (MeSH) terms with Boolean operators (“OR” and/or “AND”). Subsequently, we examined the title, abstract text, and index terms used to describe the articles. Secondly, we conducted a search across various databases, including Google Scholar, African Journal of Online (AJOL), CINAHL, HINARI, Scopus, Science Direct, Excerpta Medica Database (EMBASE), DOAJ, Web of Science, Google, and other organizations' websites, using the full title (“Knowledge, Attitude, and Practice Towards COVID-19 Among Pregnant Women in Africa”) along with specific search keywords or terms such as knowledge, awareness, attitude, perception, practice, compliance, COVID-19, coronavirus, pandemic, SARS-CoV-2, pregnant women, and Africa. Lastly, we reviewed the reference lists of all included published and unpublished studies to identify any additional relevant studies. We included studies published in English up to February 2022 from all selected databases (See additional File 1).
2.2. Study selection and eligibility criteria
This study included all observational studies reporting data on COVID-19 KAP among pregnant women in Africa, without imposing a time restriction on the study period. Both published and unpublished studies conducted in English were considered. Exclusion criteria encompassed duplicates, articles not meeting the inclusion criteria, reviews of meta-analyses, short reports, case reports, and studies with insufficient data reporting.
2.3. Study extraction and quality appraisal
Five independent authors (TL, MS, BT, MSC, and KD) conducted data extraction using a standardized format in Microsoft Excel 2010, which was pre-tested on a subset of studies. The extracted information included the first author's name, study year, location, study design, sample size, and measures of good knowledge, positive attitude, and good practice, along with their respective odds ratios (See additional File 2). Screening of studies involved assessing duplication, relevance, full-text accessibility, and alignment with outcomes of interest following searches across various international databases and organizational websites. Quality assessment was performed using the Newcastle-Ottawa Scale (NOS) [39] by five authors (TL, MS, TM, YD, and AM), independently evaluating selection, comparability, and outcome components, graded with five stars, two stars, and three stars, respectively. Disagreements among authors were resolved through discussion and re-evaluation by another author (BTT). Only primary studies meeting a medium or higher score on the NOS (fulfilling at least 50 % of the quality criteria) were included for analysis [40] (See additional File 3).
2.4. Outcome measure
The main objective of this review was to assess the current level of COVID-19 KAP among pregnant women in Africa. Knowledge was evaluated based on understanding of various aspects such as signs and symptoms, transmission modes, incubation periods, severity, vaccine availability, preventive measures, and treatment options. Individuals scoring above the mean level were categorized as having good knowledge. Attitude focused on individuals' willingness to engage in efforts to combat the COVID-19 epidemic, as well as their trust in governmental and partner initiatives. Those who scored above the mean level were considered to have a positive attitude towards controlling or managing COVID-19. Practice was assessed based on adherence to recommended safety measures, including physical distancing, hand hygiene, mask-wearing, avoidance of crowded places, and adherence to isolation/quarantine protocols. Individuals scoring at or above the mean level were deemed to have good practice [41].
2.5. Statistical analysis
The analysis utilized STATATM Version 11 software and employed inverse variance (I2) and Cochran Q statistics to evaluate study heterogeneity. I2 test statistics were categorized as low, moderate, and high heterogeneity based on thresholds of 50 %, 50–75 %, and >75 %, respectively [42]. Due to observed heterogeneity, the Dersimonian and Liard random-effects model was applied. Subgroup analysis was conducted to explore potential sources of heterogeneity and mitigate random differences between studies. Funnel plots and Egger's test were employed to assess publication bias, with a significance level of 0.05. Additionally, a leave-one-out sensitivity analysis was performed to assess the impact of individual studies on the overall meta-analysis.
3. Results
3.1. Study selection
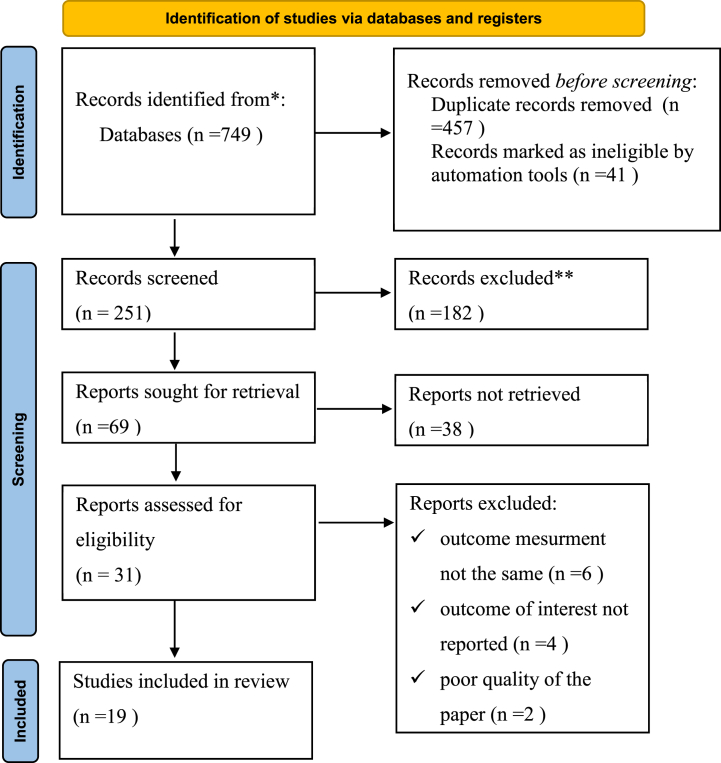
Initially, 749 studies were identified through database searches and manual exploration. Of these, 498 records were excluded due to duplication (n = 457) and ineligibility flagged by automated tools in EndNote software, which screened based on predetermined criteria like language (English) and study type (observational studies) (n = 41). The remaining 251 records underwent title screening, resulting in the removal of 182 articles. Abstract screening further narrowed the selection to 68 studies, with 38 deemed irrelevant and excluded. Thirty-one full-text publications were then assessed for eligibility, with 12 rejected due to various reasons such as differences in outcome measurement, omission of key findings, and poor paper quality. Ultimately, 19 studies met the inclusion criteria and were included in the analysis (See Fig. 1).
Fig. 1.
PRISMA Flow Diagram of Study Selection for Systematic Review and Meta-Analysis of Knowledge, Attitudes, and Practices (KAP) Towards COVID-19 among Pregnant Women in Africa. This diagram outlines the systematic review and meta-analysis process following PRISMA guidelines. Initially, 749 studies were identified. After excluding duplicates (n = 457) and ineligible records (n = 41), 251 records underwent title screening, removing 182 articles. Abstract screening narrowed it to 68 studies, with 38 excluded. Thirty-one full-text publications were assessed, rejecting 12 due to various reasons. Ultimately, 19 studies met inclusion criteria for analysis, providing transparency in study selection.
3.2. Study characteristics
This systematic review and meta-analysis comprised 18 articles assessing knowledge, 14 articles evaluating practice, and 6 articles examining attitude, all meeting the inclusion criteria. The included studies spanned across nine in the eastern region of Africa [18,[29], [30], [31], [32], [33], [34], [35], [36]] and ten in the western region [[19], [20], [21], [22], [23], [24], [25], [26], [27], [28]].
All included studies were cross-sectional in nature, with sample sizes ranging from 253 [24] to 648 [33] participants. Among these, a study conducted in the Western region of Africa reported the highest levels of good knowledge (87.2 %) and practice (79.2 %). Conversely, a study conducted in the Eastern region of Africa found the lowest levels of knowledge (32.8 %) and practice (21.4 %). Notably, the Eastern region reported a high level of positive attitude (87.6 %) (See Table 1).
Table 1.
Characteristics of included studies.
| Authors Name | Year of Study | Study Region | Study design | Data collection technique | Funding source | Sample size | Good level of knowledge % (95%CI) | Good practice% (95%CI) | Positive Attitude % (95%CI) |
|---|---|---|---|---|---|---|---|---|---|
| Omozuwa et al. | 2020 | Western | cross sectional | SAQ | Not reported | 420 | 46.9 | 77.1 | |
| Ayele et al. | 2020 | Eastern | cross sectional | Interview | Not funded | 405 | 46.8 | 47.6 | |
| Degu et al. | 2020 | Eastern | cross sectional | Interview | Not funded | 403 | 52.1 | 52.6 | |
| W/Mariam et al. | 2020 | Eastern | cross sectional | Interview | Not funded | 422 | 55 | 47.4 | |
| Kumbeni et al. | 2020 | Western | cross sectional | Interview | Not reported | 527 | 85.6 | 46.6 | |
| Fikadu et al. | 2020 | Eastern | cross sectional | Interview | Wolkite University | 403 | 54.8 | 76.2 | |
| Adegoke et al. | 2020 | Western | cross sectional | SAQ | Not reported | 382 | 86.65 | ||
| Aduloju et al. | 2020 | Western | cross sectional | SAQ | Not reported | 423 | 87.2 | 79.2 | 74.5 |
| Omoronyia et al. | 2021 | Western | cross sectional | Interview | Authors | 284 | 43.3 | ||
| West et al. | 2021 | Western | cross sectional | SAQ | Not funded | 253 | 81.4 | 26.5 | 20.2 |
| Hoque et al. | 2021 | Southern | cross sectional | Interview | Not funded | 346 | 43.5 | 76 | 30 |
| Theuring et al. | 2020 | Eastern | cross sectional | Interview | H.W. & J. Hector Foundation | 648 | 32.8 | 21.4 | |
| Besho et al. | 2020 | Eastern | cross sectional | Interview | Wollega University | 415 | 75.4 | 43.6 | |
| Silesh et al. | 2021 | Eastern | cross sectional | Interview | Not funded | 396 | 70.5 | 56.1 | 87.6 |
| Nwafor et al. | 2020 | Western | cross sectional | SAQ | Not reported | 284 | 60.9 | 30.3 | |
| Zeleke et al. | 2021 | Eastern | cross sectional | Interview | Not funded | 538 | 67.3 | 51.1 | 46.7 |
| Esike et al. | 2020 | Western | cross sectional | SAQ | Not reported | 385 | 78.4 | ||
| Anikwe et al. | 2020 | Western | cross sectional | Interview | Not reported | 460 | 43.5 | ||
| Belayneh et al. | 2021 | Eastern | cross sectional | Interview | Not funded | 458 | 53 |
Legend: SAQ = Self-administered questioner.
This table outlines key characteristics of studies in the systematic review and meta-analysis on KAP regarding COVID-19 prevention among pregnant women in Africa. It includes Study ID, Region (e.g., Western, Eastern), Year of publication/conduct, Sample Size, Design (usually cross-sectional), and percentages for Good Knowledge, Positive Attitude, and Good Practice regarding COVID-19 preventive measures.
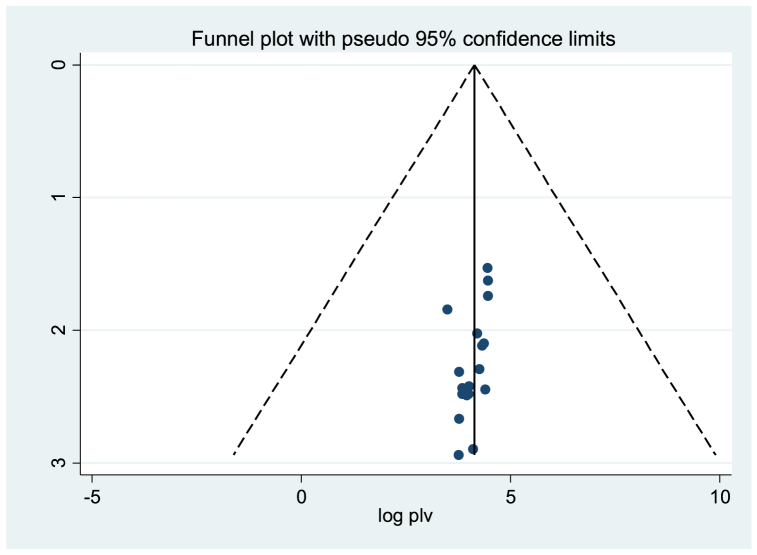
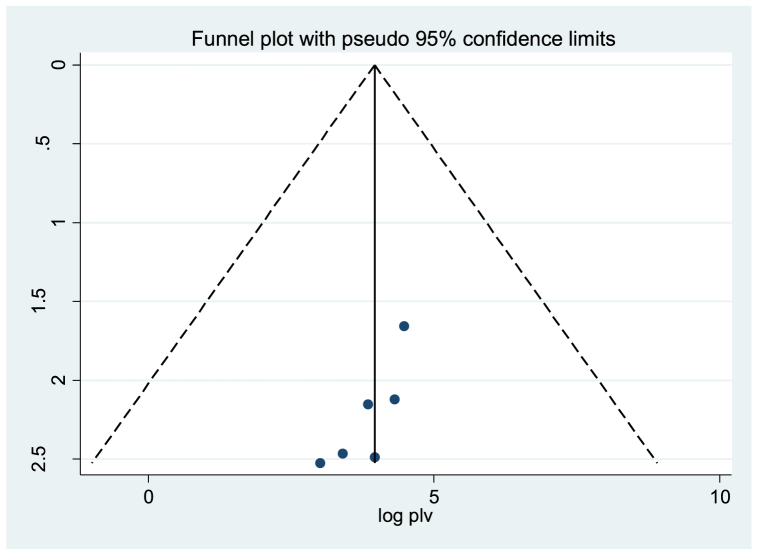
3.3. Publication bias
Publication bias was assessed using a funnel plot and the Egger regression test with a significance threshold of <0.05. For the level of good knowledge, statistical evidence of publication bias was observed. The funnel plot displayed some asymmetry in the distribution, and the Egger test yielded a statistically significant result with a coefficient value of 0.396 and P-value of 0.029 (See Fig. 2). Similarly, publication bias was detected for positive attitude, with the Egger test indicating statistical significance, showing a coefficient value of −1.236 and P-value of 0.04. Additionally, a funnel plot displayed an asymmetrical distribution (See Fig. 3). To address this bias, the Duval and Tweedie nonparametric trim and fill analysis using the random-effects model was conducted [43,44]. The analysis revealed that the pooled estimate values of knowledge and attitude remained unchanged compared to those obtained from the random-effects model, which were 61.8 % (95 % CI: 53.0%–70.65 %) and 51.97 % (95 % CI: 30.34%–73.6 %), respectively. Notably, no statistical evidence of publication bias was found for good practice.
Fig. 2.
Funnel Plots for Publication Bias of Knowledge Levels on COVID-19 among Pregnant Women in Africa. Each point represents a study included in the analysis, with the x-axis indicating the effect size and the y-axis representing a measure of study precision.
Fig. 3.
Funnel plots for publication bias of positive attitudes towards COVID-19 among pregnant women in Africa. Each point represents a study included in the analysis, with the x-axis indicating the effect size and the y-axis representing a measure of study precision.
3.4. Level of KAP towards COVID-19 preventive measures
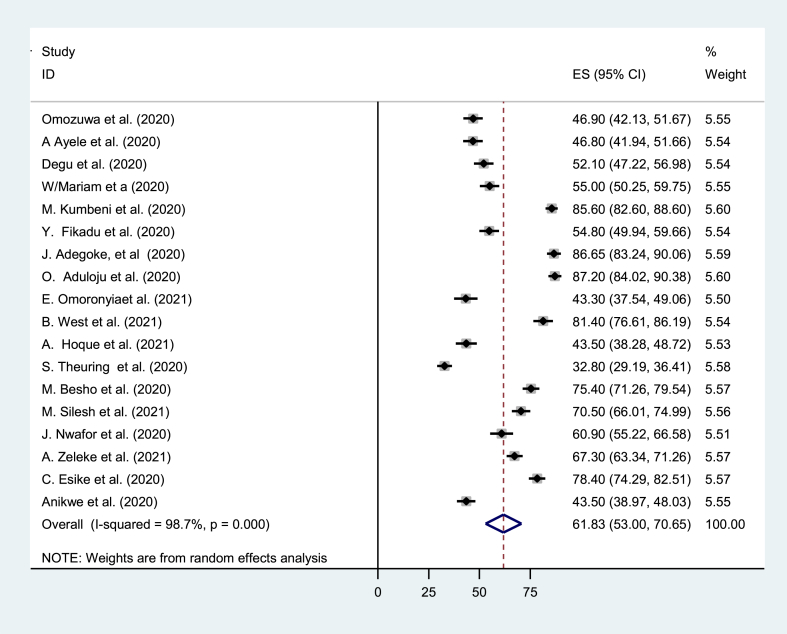
Utilizing the random-effects model, the estimated prevalence of good knowledge regarding COVID-19 was found to be 61.8 % (95 % CI: 53.0%–70.65 %; I2 = 98.7 %) (See Fig. 4). Positive attitudes toward COVID-19 were identified in 51.97 % of pregnant women (95 % CI: 30.34%–73.6 %; I2 = 99.3 %) (See Fig. 5). The pooled estimated level of COVID-19 good practice was 52.31 % (95 % CI: 41.48%–63.15 %; I2 = 98.8 %) (See Fig. 6).
Fig. 4.
Forest Plot for Pooled Good Knowledge Levels on COVID-19 among Pregnant Women in Africa. Square markers denote knowledge levels, their size reflects study weight. The diamond marker indicates pooled prevalence.
Fig. 5.
Forest Plot for Pooled Positive Attitude Levels towards COVID-19 among Pregnant Women in Africa. Square markers represent positive attitudes, their size indicates study weight. The diamond marker indicates pooled prevalence.
Fig. 6.
Forest Plot for Pooled Good Practices towards COVID-19 among Pregnant Women in Africa. Square markers denote the pooled level of good practice, with size indicating study weight. The diamond marker indicates pooled prevalence.
3.5. Subgroup analysis
Initially, the authors planned to employ both meta-regression and subgroup analysis to tackle sources of heterogeneity. However, during data extraction, it became apparent that region was the only differing variable among the studies. Consequently, the authors chose to prioritize subgroup analysis over meta-regression. Subgroup analysis, dividing studies by region, enables separate examination of outcomes in each subgroup, particularly suited for scrutinizing regional differences. Notable differences emerged in the analysis: in the Western region, the highest levels of good knowledge (65.62 %, 95 % CI: 53.25%–77.98 %; I2 = 95.7 %) and high practice (97.695 %, 95 % CI: 35.99%–75.66 %; I2 = 55.8 %) were observed. Conversely, in the Eastern region, the highest level of positive attitude was recorded at 62.21 % (95 % CI: 38.30%–86.12 %; I2 = 96.3 %) (See Table 2).
Table 2.
Subgroup analysis of KAP towards COVID-19 among pregnant women in Africa.
| Knowledge | |||
|---|---|---|---|
| Region | Pooled estimate with 95 %(CI) | I2 (p-value) | % Weight |
| Eastern | 56.71 % (“46.81″ to “66.61″) | 92.2 % (<0.001) | 44.53 |
| Western | 65.62 % (“53.25″ to “77.98″) | 95.7 % (<0.001) | 55.47 |
| Attitude | |||
| Region | Pooled estimate with 95 %(CI) | I2 (p-value) | % Weight |
| Eastern | 62.21 % (“38.30″ to “86.12″) | 96.3 % (<0.001) | 49.85 |
| Western | 41.43 % (“11.77″ to “71.09″) | 98.2 % (<0.001) | 50.15 |
| Practice | |||
| Region | Pooled estimate with 95 %(CI) | I2 (p-value) | % Weight |
| Eastern | 49.42 % (“38.26″ to “60.57″) | 94.4 % (<0.001) | 7.14 |
| Western | 97.6 % (“35.99″ to “75.66″) | 55.82 % (<0.001) | 7.21 |
Legend: CI= Confidence Interval.
This table highlights regional differences in KAP towards COVID-19 among pregnant women in Africa. It categorizes regions into Western and Eastern Africa. For each region, it presents percentages of participants with good knowledge, positive attitudes, and good practices regarding COVID-19 preventive measures, along with 95 % confidence intervals (CI) and I2 statistics indicating heterogeneity.
3.6. Sensitivity analysis
A sensitivity analysis was conducted by systematically removing individual studies to evaluate their impact on the overall effect estimate. The findings indicated that the exclusion of any single study did not substantially alter the pooled levels of good knowledge; positive attitude and good practice (See Table 3).
Table 3.
Sensitivity analysis for levels of KAP towards COVID-19 among pregnant women in Africa.
| Articles on knowledge | |||
|---|---|---|---|
| Study omitted | Year of study | Pooled estimate (%) | 95%CI |
| Omozuwa et al. | 2020 | 63.76 | “23.03″ to “76.52″ |
| Ayele et al. | 2020 | 63.73 | “23.04″ to “76.31″ |
| Degu et al. | 2020 | 63.43 | “22.93″ to “75.44″ |
| W/Mariam et al. | 2020 | 63.30 | “22.86″ to “75.30″ |
| Kumbeni et al. | 2020 | 60.55 | “21.06″ to “74.06″ |
| Fikadu et al. | 2020 | 63.29 | “22.88″ to “75.09″ |
| Adegoke et al. | 2020 | 61.06 | “21.55″ to “72.98″ |
| Aduloju et al. | 2020 | 60.72 | “21.28″ to “73.27″ |
| Omoronyia et al. | 2021 | 63.64 | “23.15″ to “74.93″ |
| West et al. | 2021 | 62.18 | “22.46″ to “72.13″ |
| Hoque et al. | 2021 | 63.79 | “23.13″ to “75.95″ |
| Theuring et al. | 2020 | 66.37 | “23.55″ to “87.03″ |
| Besho et al. | 2020 | 62.21 | “22.30″ to “73.58″ |
| Silesh et al. | 2021 | 62.54 | “22.52″ to “73.67″ |
|
Articles on attitude | |||
|---|---|---|---|
| Study omitted | Year of study | Pooled estimate (%) | 95%CI |
| Degu et al. | 2020 | 52.37 | “8.25″ to “32.32″ |
| Aduloju et al. | 2020 | 48.68 | “7.28″ to “25.46″ |
| West et al. | 2021 | 59.82 | “9.46″ to “78.13″ |
| Hoque et al. | 2021 | 56.87 | “8.94″ to “61.81″ |
| Silesh et al. | 2021 | 42.76 | “5.55″ to “29.20″ |
| Zeleke et al. | 2021 | 53.63 | “8.07″ to “56.50″ |
|
Articles on practice | |||
|---|---|---|---|
| Study omitted | Year of study | Pooled estimate (%) | 95%CI |
| Belayneh. et al. | 2021 | 47.88 | “14.35″ to"59.81″ |
| Omozuwa et al. | 2020 | 46.16 | “13.66″ to “56.02″ |
| Ayele et al. | 2020 | 48.24 | “14.52″ to “60.21″ |
| W/Mariam et al. | 2020 | 48.25 | “14.50″ to “60.51″ |
| Kumbeni et al. | 2020 | 48.33 | “14.39″ to “62.35″ |
| Fikadu et al. | 2020 | 46.35 | “13.77″to “56.08″ |
| Aduloju et al. | 2020 | 45.87 | “13.51″ to “55.71″ |
| West et al. | 2021 | 49.61 | “15.04″ to “63.58″ |
| Hoque et al. | 2021 | 46.65 | “13.96″ to “55.90″ |
| Theuring et al. | 2020 | 54.78 | “15.63″to “91.97″ |
| Besho et al. | 2020 | 48.51 | “14.58″ to “61.35″ |
| Silesh et al. | 2021 | 47.76 | “14.38″ to “58.58″ |
| Nwafor et al. | 2020 | 49.33 | “14.94″ to “62.83″ |
| Zeleke et al. | 2021 | 47.97 | “14.27″ to “61.26″ |
Legend: CI = Confidence Interval.
This table displays the results of sensitivity analysis conducted to assess the impact of individual studies on the overall levels of KAP towards COVID-19 among pregnant women in Africa.
4. Discussion
The onset of the COVID-19 pandemic in Africa was officially confirmed on February 14, 2020, with Egypt reporting the first confirmed case. According to a WHO report from February 2023, the WHO African Region (WHO AFR) accounted for 82.7 % s (8.9 million) of global cases and 76.2 % of global deaths (174,191 deaths) [45]. Pregnant women face heightened susceptibility to COVID-19 infection, raising concerns about its potential adverse effects on maternal and perinatal outcomes [46]. This systematic review and meta-analysis aimed to estimate the pooled level of knowledge, attitudes, and practices (KAP) regarding COVID-19 preventive measures among pregnant women in Africa. Nineteen studies from various African countries were included in the analysis, with two of them being unpublished, based on predetermined inclusion criteria. According to the findings of this review, the pooled prevalence of good knowledge about COVID-19 preventive measures among pregnant women was 61.8 %, aligning with findings from previous studies [[47], [48], [49], [50], [51], [52]]. Interestingly, this rate was higher than that reported in an Ethiopian study [53]. One potential explanation for this variation could be the difference in study populations; the Ethiopian study included only a limited number of studies from the country, whereas the findings of this review were aggregated from studies across all African countries. Additionally, the dissemination of information regarding COVID-19 may have improved over time, contributing to differences in knowledge levels. Therefore, variations in the year of study among the primary articles could also be a contributing factor to the observed differences.
Nevertheless, this figure was lower than studies conducted on Sub-Saharan Africans and the global population [54,55] The difference could be attributed to the specific focus on pregnant women in this study compared to studies involving the general population. Moreover, the observed lower knowledge level compared to a study conducted in Ethiopia [41,56] and globally [57,58] might be due to differences in the study populations, with those studies focusing on healthcare professionals potentially more knowledgeable about COVID-19.
Regarding attitudes, 51.97 % of pregnant women exhibited favourable attitudes toward COVID-19, comparable to other studies [41,47,49,52] but lower than studies conducted on Sub-Saharan Africans and in Ethiopia [50,51,54]. The discrepancy could be influenced by the prevailing burden of communicable and non-communicable diseases in Sub-Saharan Africa, shaping the public's perception and attitudes toward COVID-19. This finding also diverges notably from the results reported in a systematic review and meta-analysis conducted by different authors [[57], [58]]. One potential explanation for this variance could be attributed to the composition of the study population. Unlike this study, which exclusively focused on pregnant women, the other studies included healthcare professionals who might inherently exhibit more positive attitudes toward COVID-19 preventive measures.
The pooled estimated level of COVID-19 good practice among pregnant women was 52.31 %, consistent with previous studies [41,47,49,52,54] but lower than a global review [55]. This could be attributed to the specific focus on pregnant women in this study compared to global studies involving diverse populations. Moreover, social cohesion and cultural factors may hinder effective implementation of preventive measures, particularly in regions with strong social ties and communal living arrangements. Nevertheless, this discovery contrasts with a study conducted in Ethiopia [51]. This variance could be attributed to differences in the study year and the composition of the primary articles included in the analysis.
Subgroup analysis revealed regional disparities, with the Western region exhibiting the highest levels of good knowledge (65.62 %) and practice (97.695 %). Conversely, the Eastern region had the highest level of positive attitude (62.21 %). These variations could be attributed to differences in access to COVID-19-related information, demographic characteristics, socioeconomic factors, healthcare infrastructure, and cultural and behavioral norms between the two regions.
In this study, pregnant women in Africa demonstrate higher knowledge but lower attitudes and practices toward COVID-19 preventive measures. While increased knowledge may contribute to positive attitudes and better practices, social and cultural factors may hinder effective implementation. Policymakers can leverage these findings to develop targeted interventions aimed at educating pregnant women and improving COVID-19 prevention and vaccination policies in Africa. Additionally, obstetric societies can use these findings to develop guidelines providing essential information and guidance to pregnant women and obstetric care providers.
4.1. Strength and limitation of the study
To the best of our knowledge, this study represents the most comprehensive systematic review and meta-analysis conducted to assess the pooled estimated level of pregnant women's KAP towards COVID-19 preventive measures in Africa. The selection of studies, data extraction, and risk of bias assessment were conducted independently by five reviewers.
However, there are certain limitations to this research. Firstly, the scarcity of studies from some African regions poses challenges in generalizing the findings to the continent as a whole. Secondly, the results should be interpreted cautiously due to significant heterogeneity among the included studies. Thirdly, there may be limitations in outcome comparability due to variations in operational definitions and measurement methods used across the primary studies to assess knowledge, attitudes, and practices. Lastly, the comparison of our results with existing literature was hindered by the limited number of systematic reviews and meta-analyses conducted at regional and international levels.
4.2. Implication of the study
The findings underscore the importance of tailored public health interventions targeting pregnant women in Africa. Policymakers can utilize these results to develop targeted educational campaigns aimed at improving knowledge about COVID-19 preventive measures among pregnant women. These campaigns can focus on disseminating accurate information about transmission, prevention strategies, and vaccination benefits during pregnancy.
Healthcare providers play a crucial role in educating pregnant women about COVID-19 prevention and vaccination. The results of this study emphasize the need for healthcare professionals to prioritize discussions on COVID-19 prevention measures during prenatal care visits. By addressing misconceptions and promoting positive attitudes towards preventive measures, clinicians can empower pregnant women to adopt safer behaviors and protect themselves and their unborn babies from COVID-19.
The study highlights gaps in KAP towards COVID-19 among pregnant women in Africa. Future research should focus on understanding the underlying factors contributing to these disparities, such as socioeconomic status, access to healthcare, and cultural beliefs. Additionally, longitudinal studies are needed to assess the long-term impact of COVID-19 on maternal and neonatal health outcomes in the African context.
5. Conclusions
Improving the KAP of pregnant women regarding COVID-19 preventive measures is paramount, given their heightened vulnerability to the virus. This study underscores the pressing need for targeted interventions, as it reveals that only around half of pregnant women in Africa possess adequate knowledge, attitudes, and practices towards COVID-19 prevention—indicating a lower level compared to other continents. Healthcare professionals must take the lead in educating pregnant women about COVID-19 preventive measures, while healthcare systems should sustain community-wide awareness campaigns. While this study provides valuable insights into the KAP of pregnant women in Africa, it is crucial to conduct additional reviews on a global scale to offer a broader perspective. Such research endeavors will facilitate the development of future strategies and policies aimed at enhancing COVID-19 preparedness among pregnant women worldwide.
Data availability
All data used in the generation of the results presented in this manuscript will be made available upon reasonable request from the corresponding author.
Funding
The author(s) received no specific funding for this work.
CRediT authorship contribution statement
Tesfanesh Lemma: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Mulualem Silesh: Writing – review & editing, Visualization, Validation, Software, Funding acquisition, Formal analysis, Data curation, Conceptualization. Birhan Tsegaw Taye: Writing – review & editing, Supervision, Software, Methodology, Formal analysis. Kelem Desta: Writing – review & editing, Supervision, Software. Tebabere Moltot: Writing – review & editing, Visualization, Supervision, Methodology, Formal analysis. Abebayehu Melisew: Writing – review & editing, Validation, Software, Methodology, Funding acquisition, Formal analysis. Mages Sisay: Writing – review & editing, Software, Methodology, Formal analysis. Wegayehu Zeneb: Writing – review & editing, Validation, Methodology, Formal analysis. Yalemtsehay Dagnaw: Writing – review & editing, Validation, Supervision, Software, Formal analysis.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to express our gratitude to all of the authors of the studies included in this systematic review and meta-analysis.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e31926.
Contributor Information
Tesfanesh Lemma, Email: tesfitimnt@gmail.com.
Mulualem Silesh, Email: sileshmulualem22@gmail.com.
Birhan Tsegaw Taye, Email: tsegawbirhan2@gmail.com.
Kelem Desta, Email: kelemdesta2015@gmail.com.
Tebabere Moltot, Email: mtebabere@gmail.com.
Abebayehu Melisew, Email: abebayehumelesew@gmail.com.
Mages Sisay, Email: sisaymoges07@gmail.com.
Wegayehu Zeneb, Email: wegayehuzeneb@gmail.com.
Yalemtsehay Dagnaw, Email: tsehayworld@gmail.com.
Abbreviations
- COVID-19
Coronavirus Disease 2019
- KAP
Knowledge, Attitude, and Practice
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MeSH
Medical Subject Headings
- AJOL:
African Journal of Online
- NOS
Newcastle-Ottawa Scale
- PICOT
Population, Intervention, Comparator, Outcome, Type of Study
- PROSPERO
International Prospective Register of Systematic Reviews
- WHO
World Health Organization
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Elflein J. Coronavirus (COVID-19) disease pandemic- Statistics & Facts _ Statista. 2023 https://www.statista.com/topics/5994/the-coronavirus-disease-covid-19-outbreak/ Available from: [Google Scholar]
- 2.Cennimo D.J., Bergman S.J., Olsen K.M. Coronavirus disease 2019 (COVID-19): practice essentials, background, Route of transmission. Medscape. 2020 https://emedicine.medscape.com/article/2500114-overview [Internet] [Google Scholar]
- 3.World Health Organization . World Health Organization; 2022. WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data | WHO Coronavirus (COVID-19) Dashboard with Vaccination Data; pp. 1–5.https://covid19.who.int/ [Internet] [Google Scholar]
- 4.WHO Africa . WHO Press; 2022. COVID-19 Deaths in African Region to Fall by Nearly 94% in 2022: WHO Analysis [Internet]https://www.afro.who.int/news/covid-19-deaths-african-region-fall-nearly-94-2022-who-analysis [Google Scholar]
- 5.Centers of Diseases and Control Prevention Pregnant and recently pregnant people increased risk of severe illness COVID-19. Centers Dis Control Prev. 2022 https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html#:∼:text=IncreasedRiskofSevereIllness&text=Pregnancycauseschangesinthe,Hospitalization [Google Scholar]
- 6.WHO Coronavirus disease (COVID-19): Pregnancy, childbirth and the postnatal period. 2022 https://who.int/News-Room/Questions-and-Answers/Item/Coronavirus-Disease-Covid-19-Pregnancy-and-Childbirth https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-pregnancy-and-childbirth [Internet] [Google Scholar]
- 7.Samadi P., Alipour Z., Ghaedrahmati M., Ahangari R. The severity of COVID-19 among pregnant women and the risk of adverse maternal outcomes. Int. J. Gynecol. Obstet. 2021;154(1):92–99. doi: 10.1002/ijgo.13700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chamseddine R.S., Wahbeh F., Chervenak F., Salomon L.J., Ahmed B., Rafii A. Pregnancy and neonatal outcomes in SARS-CoV-2 infection: a systematic review. Journal of Pregnancy. 2020;2020 doi: 10.1155/2020/4592450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei S.Q., Bilodeau-Bertrand M., Liu S., Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ (Can. Med. Assoc. J.) 2021;193:E540–E548. doi: 10.1503/cmaj.202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Advisory M. National Institute of Child Health and Human Development; 2021. Severe COVID-19 in Pregnancy Associated with Preterm Birth, Other Complications _ NICHD - Eunice Kennedy Shriver. [Google Scholar]
- 11.Ma Y., Deng J., Liu Q., Du M., Liu M., Liu J. Effectiveness and safety of COVID-19 vaccine among pregnant women in real-world studies: a systematic review and meta-analysis. Vaccines [Internet] 2022 Feb 6;10(2):246. doi: 10.3390/vaccines10020246. https://www.mdpi.com/2076-393X/10/2/246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ellington S., Jatlaoui T.C. COVID-19 vaccination is effective at preventing severe illness and complications during pregnancy. Lancet. 2023;401:412–413. doi: 10.1016/S0140-6736(22)02613-7. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Villar J., Soto Conti C.P., Gunier R.B., Ariff S., Craik R., Cavoretto P.I., et al. Pregnancy outcomes and vaccine effectiveness during the period of omicron as the variant of concern, INTERCOVID-2022: a multinational, observational study. Lancet. 2023;401(10375):447–457. doi: 10.1016/S0140-6736(22)02467-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu S., Wang L., Dong J., Bao Y., Liu X., Li Y., et al. The dose- and time-dependent effectiveness and safety associated with COVID-19 vaccination during pregnancy: a systematic review and meta-analysis. Int J Infect Dis [Internet] 2023;128:335–346. doi: 10.1016/j.ijid.2023.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schrag S.J., Verani J.R., Dixon B.E., Page J.M., Butterfield K.A., Gaglani M., et al. Estimation of COVID-19 mRNA vaccine effectiveness against medically attended COVID-19 in pregnancy during periods of delta and omicron variant predominance in the United States. JAMA Netw. Open. 2022;5(9) doi: 10.1001/jamanetworkopen.2022.33273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunawardhana N., Baecher K., Boutwell A., Pekwarake S., Kifem M., Ngong M.G., et al. COVID-19 vaccine acceptance and perceived risk among pregnant and non-pregnant adults in Cameroon, Africa. PLoS One [Internet] 2022;17(9 September):1–13. doi: 10.1371/journal.pone.0274541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azami M., Nasirkandy M.P., Ghaleh H.E.G., Ranjbar R. COVID-19 vaccine acceptance among pregnant women worldwide: a systematic review and meta-analysis. PLoS One. 2022;17 doi: 10.1371/journal.pone.0272273. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Belayneh M., Agumas Y., Engidaw D. Factors influencing knowledge , attitude and practice of COVID-19 preventive measures among pregnant women attending antenatal care in Adiarkay District , Northwest Ethiopia. GJMEDPH. 2021 Feb 6;10(January):2277–9604. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=+Belayneh+M.+Factors+influencing+knowledge+%2C+attitude+and+practice+of+COVID-19+preventive+measures+among+pregnant+women+attending+antenatal+care+in+Adiarkay+District+%2C+Northwest+Ethiopia.+2022%3B10%28January%29.&btnG= [Internet] [Google Scholar]
- 19.Adegoke J.I., Ajibade B.L., Knowledge Rhoda D. Attitude and practice of preventive measures towards covid-19 among pregnant women attending selected primary health centre's in Osogbo, Osun state. Int. J. Nurs. 2020;6(2):29–45. https://eajournals.org/ijnmh/vol-6-issue-2-december-2020/knowledge-attitude-and-practice-of-preventive-measures-towards-covid-19-among-pregnant-women-attending-selected-primary-health-centres-in-osogbo-osun-state/ Midwife Heal Relat Cases [Internet] [Google Scholar]
- 20.Omozuwa E., Uwaibi N., Erhabor J. Level of practice of safety precautions against COVID 19 among pregnant women attending antenatal clinics in central hospital Benin, Benin City in Nigeria. J. Appl. Sci. Environ. Manag. 2021;24(11):1925–1931. [Google Scholar]
- 21.Kumbeni M.T., Apanga P.A., Yeboah E.O., Lettor I.B.K. Knowledge and preventive practices towards COVID-19 among pregnant women seeking antenatal services in Northern Ghana. PLoS One. 2021;16(6 June):1–11. doi: 10.1371/journal.pone.0253446. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aduloju O.P., Okunola T.O., Adefisan A.S., Aduloju T. Knowledge, attitude and practice of preventive measures against coronavirus disease 2019 among pregnant women in a tertiary health facility in southwest Nigeria. Int J Clin Obstet Gynaecol. 2021;5(3):101–107. [Google Scholar]
- 23.Omoronyia E., Eyong E., Omoronyia O., Akpan U., Arogundade K., Ekanem E. Knowledge, attitude, and practice of preventive measures against COVID-19 among pregnant women receiving antenatal care in Calabar, Nigeria. Niger. J. Med. 2021;30(5):548. [Google Scholar]
- 24.West B.A., Aitafo J.E., Bietonka Kalio D.G. Knowledge, attitudes and practices of pregnant women attending the antenatal clinic of rivers state university teaching hospital, Nigeria towards the coronavirus (COVID-19) pandemic. Int. J. Health Sci. Res. 2021;11(4):21–33. [Google Scholar]
- 25.Nwafor J.I., Aniukwu J.K., Anozie B.O., Ikeotuonye A.C., Okedo-Alex I.N. Pregnant women's knowledge and practice of preventive measures against COVID-19 in a low-resource African setting. Int. J. Gynecol. Obstet. 2020;150(1):121–123. doi: 10.1002/ijgo.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Esike C., Eze J., Anozie O., Onwe E., Ewah R., Emeka-Irem E., et al. Shock wave of a new pandemic: response of antenatal women in ebonyi state, Nigeria to corona virus 19 infection—knowledge, attitude and practice. Adv. Infect. Dis. 2021;11(1):29–41. [Google Scholar]
- 27.Anikwe C.C., Ogah C.O., Anikwe I.H., Ewah L., Onwe O.E., Ikeoha C.C. Coronavirus 2019 pandemic : assessment of the level of knowledge , attitude , and anxiety among pregnant women in ebonyi state , Nigeria. Ann Med Health Sci Res [Internet] 2021;4(2):1267–1273. [Google Scholar]
- 28.Hoque A.M., Alam A.M., Hoque M., Hoque M.E., Van Hal G. Knowledge, attitudes, and practices towards COVID-19 of pregnant women at a primary health care facility in South Africa. Eur J Med Heal Sci. 2021;3(1):50–55. [Google Scholar]
- 29.Ayele A.D., Mihretie G.N., Belay H.G., Teffera A.G., Kassa B.G., Amsalu B.T. Knowledge and practice to prevent COVID-19 and its associated factors among pregnant women in Debre Tabor Town Northwest Ethiopia, a community-based cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–12. doi: 10.1186/s12884-021-03877-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Degu A., Nibret G., Gebrehana H., Getie A., Getnet B. Knowledge and attitude towards the current pandemic corona virus disease and associated factors among pregnant women attending antenatal care in debre tabor general hospital northwest Ethiopia: an institutional-based cross-sectional study. Int J Womens Health. 2021;13:61–71. doi: 10.2147/IJWH.S285552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tesfamichael T.G.M., Kassie B.A., Asratie M.H., Abate A.T. The effects of fear and knowledge of COVID-19 on preventive practice among pregnant women who attend antenatal care in northwest Ethiopia, 2020: Institution-based cross-sectional study. Int J Womens Health. 2021;13:95–100. doi: 10.2147/IJWH.S286088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fikadu Y., Yeshaneh A., Melis T., Mesele M., Anmut W., Argaw M. Covid-19 preventive measure practices and knowledge of pregnant women in guraghe zone hospitals. Int J Womens Health. 2021;13:39–50. doi: 10.2147/IJWH.S291507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Theuring S., Kengonzi A., Hafermann L., Herrmann C., Kabwama S.N., Rubaihayo J. Repercussions of the COVID-19 response in pregnant women in western Uganda: knowledge, behavior, and emotional state after the first lockdown in 2020. Int. J. Environ. Res. Publ. Health. 2021;18(15) doi: 10.3390/ijerph18157817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Besho M., Tsegaye R., Yilma M.T., Kasaye H.K., Tolossa T., Hiko N., et al. Knowledge, attitude and practice toward corona virus infection among pregnant women attending antenatal care at public hospitals in three wollega zones, Ethiopia. Int. J. Gen. Med. 2021;14:3563–3573. doi: 10.2147/IJGM.S295490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Silesh M., Demisse T.L., Taye B.T., Desta K., Kitaw T.M., Mekuria A.D., et al. Compliance with covid-19 preventive measures and associated factors among women attending antenatal care at public health facilities of debre berhan town, Ethiopia. Risk Manag. Healthc. Pol. 2021;14:4561–4569. doi: 10.2147/RMHP.S330932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mengistie Zeleke Agerie, Bayeh Gashaw Melkie. Knowledge, attitude and practice towards COVID-19 and associated factors among pregnant women at Debark Town Northwest Ethiopia: an institutional-based cross-sectional study. World J Adv Sci Technol. 2022;1(1):1–14. [Google Scholar]
- 37.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(7716):332–336. doi: 10.1136/bmj.b2535. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62:1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 39.Modesti P.A., Reboldi G., Cappuccio F.P., Agyemang C., Remuzzi G., Rapi S., et al. In: Panethnic Differences in Blood Pressure in Europe: A Systematic Review and Meta-Analysis. Fuchs F.D., editor. PLoS One; 2016 Jan 25. https://dx.plos.org/10.1371/journal.pone.0147601 11(1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kassa B.G., Ayele A.D., Belay H.G., Tefera A.G., Tiruneh G.A., Ayenew N.T., et al. Postpartum intrauterine contraceptive device use and its associated factors in Ethiopia: systematic review and meta-analysis. Reprod. Health. 2021;18(1):1–12. doi: 10.1186/s12978-021-01273-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lake E.A., Demissie B.W., Gebeyehu N.A., Wassie A.Y., Gelaw K.A., Azeze G.A. Knowledge, attitude and practice towards COVID-19 among health professionals in Ethiopia: a systematic review and meta-analysis. PLoS One [Internet] 2021;16(2 February 2021):1–16. doi: 10.1371/journal.pone.0247204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pal B.K., Sahedur Rahman M. Sensitive spectrofluorimetric determination of ruthenium at nanotrace levels using 2-(α-pyridyl) thioquinaldinamide [PTQA] Talanta. 1999;48(5):1075–1084. doi: 10.1016/s0039-9140(98)00318-x. [DOI] [PubMed] [Google Scholar]
- 44.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.WHO AFRO Situation and Response in the WHO AFRO Region. 2023 https://www.afro.who.int/sites/default/files/2023-04/Final_Dec_Feb23_COVID-19Bulletin_AFRO.pdf [Internet] [Google Scholar]
- 46.Allotey J., Stallings E., Bonet M., Yap M., Chatterjee S., Kew T., et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370 doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lake E.A., Demissie B.W., Gebeyehu N.A., Wassie A.Y., Gelaw K.A., Azeze G.A. Knowledge, attitude and practice towards COVID-19 among health professionals in Ethiopia: a systematic review and meta-analysis. PLoS One. 2021;16(2 February 2021):337–348. doi: 10.1371/journal.pone.0247204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bekele F., Sheleme T., Fekadu G., Bekele K. Patterns and associated factors of COVID-19 knowledge, attitude, and practice among general population and health care workers: a systematic review. SAGE Open Medicine. 2020;8 doi: 10.1177/2050312120970721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Azene A.G., Workie M.S., Aragaw A.M. Knowledge, attitude, and prevention practices toward coronavirus disease 2019 in Ethiopia: a systematic review and meta-analysis. Curr Ther Res - Clin Exp [Internet] 2021;94 doi: 10.1016/j.curtheres.2021.100633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mose A., Zewdie A., Sahle T. Pregnant women's knowledge, attitude, and practice towards COVID-19 infection prevention in Ethiopia: a systematic review and meta-analysis. PLoS One. 2022;17:1–17. doi: 10.1371/journal.pone.0276692. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gamtesa D.F., Tola H.H., Gutema G., Dagne B., Bedassa B.B. Knowledge, attitude and practice towards Coronavirus disease 2019 prevention in Ethiopia: systematic review and meta-analysis. J Biostat Epidemiol. 2021;7(4):344–359. [Google Scholar]
- 52.Jahromi A.S., Jokar M., Sharifi N., Omidmokhtarloo B., Rahmanian V. Global knowledge, attitude, and practice towards COVID-19 among pregnant women: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2023 Apr 22;23(1):278. doi: 10.1186/s12884-023-05560-2. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-05560-2 [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Argaw Eniyew M., Mesfin Y., GezeTenaw S., Tefera B. Knowledge and its factors associated towards the prevention of COVID-19 among pregnant women in Ethiopia. Afr Health Sci [Internet] 2022 Dec 25;22(4):587–596. doi: 10.4314/ahs.v22i4.64. https://www.ajol.info/index.php/ahs/article/view/238942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Obi C.G., Fozeu L.F., Ezaka E.I., Ochonma C., Kamwela R. Knowledge, attitudes, practices, and misconceptions towards COVID-19 among sub-Sahara Africans. Eur J Environ Public Heal [Internet] 2022 Jan 14;6(1) https://www.ejeph.com/article/knowledge-attitudes-practices-and-misconceptions-towards-covid-19-among-sub-sahara-africans-11559 [Google Scholar]
- 55.Siddiquea B.N., Shetty A., Bhattacharya O., Afroz A., Billah B. Global epidemiology of COVID-19 knowledge, attitude and practice: a systematic review and meta-analysis. BMJ Open. 2021 Sep 14;11(9) doi: 10.1136/bmjopen-2021-051447. https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-051447 [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meseret M., Regasa Z., Hailye G., Tilahun B., Dagnew A. Knowledge and attitude towards COVID-19 and its associated factors among health care providers in Ethiopia: a systematic and meta-analysis. Am. J. Clin. Exp. Med. 2021;9(4):109. https://www.sciencepublishinggroup.com/journal/paperinfo?journalid=254&doi=10.11648/j.ajcem.20210904.14 [Internet] [Google Scholar]
- 57.Hesaraki M., Akbarizadeh M., Ahmadidarrehsima S., Moghadam M.P., Izadpanah F. Knowledge, attitude, practice and clinical recommendations of health care workers towards COVID-19: a systematic review. Rev. Environ. Health. 2021;36:345–357. doi: 10.1515/reveh-2020-0099. https://www.degruyter.com/document/doi/10.1515/reveh-2020-0099/html [Internet] [DOI] [PubMed] [Google Scholar]
- 58.Tegegne G.T., Kefale B., Engidaw M.T., Degu A., Tesfa D., Ewunetei A., et al. Knowledge, attitude, and practice of healthcare providers toward novel coronavirus 19 during the first months of the pandemic: a systematic review. Front. Public Health. 2021 Jun 25;9(June):1–9. doi: 10.3389/fpubh.2021.606666. https://www.frontiersin.org/articles/10.3389/fpubh.2021.606666/full [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data used in the generation of the results presented in this manuscript will be made available upon reasonable request from the corresponding author.