Patients with CHD or other major atherosclerotic disease
For all patients with coronary heart disease (angina, myocardial infarction) or other major atherosclerotic disease, every effort should be made to achieve the lifestyle, risk factor, and therapeutic targets given in the table. The care of coronary patients should embrace all aspects of cardiac prevention and rehabilitation.
Priorities for CHD prevention in clinical practice
(1) (a) Patients with established coronary heart disease(b) Patients with other major atherosclerotic disease
(2) Patients with hypertension, dyslipidaemia, diabetes mellitus, family history of premature CHD, or a combination of these risk factors, which puts them at high risk of developing CHD or other atherosclerotic disease. Patients with diabetes melitus are at particularly high risk of CHD
Using the coronary risk prediction chart for primary prevention
These charts are for estimating the risk of coronary heart disease (non-fatal myocardial infarction and death from coronary heart disease) for individuals who have not developed symptoms of coronary heart disease or other major atherosclerotic disease. These charts are not appropriate for patients who have existing disease which already puts them at high risk. Such diseases are:
Coronary heart disease or other major atherosclerotic disease
Familial hypercholesterolaemia or other inherited dyslipidaemia
Established hypertension (systolic BP >160 mm Hg or diastolic >100 mm Hg) or associated target organ damage
Diabetes mellitus with associated target organ damage
Renal dysfunction.
Drug treatment is required for all these patients to reduce risk of coronary heart disease.
Estimating risk
To estimate an individual's absolute 10 year risk of developing coronary heart disease, find the table for their sex, diabetes (yes/no), smoking status (smoker/non-smoker), and age. Within this square define the level of risk according to systolic blood pressure and the ratio of total cholesterol to high density lipoprotein (HDL) cholesterol. If there is no HDL cholesterol result, assume this is 1.0 mmol/l; then the lipid scale can be used for total cholesterol alone.
High risk individuals are defined as those whose 10 year risk of coronary heart disease exceeds 15% (equivalent to a cardiovascularrisk of 20% over the same period). As a minimum, those at highest risk (⩾30%; red) should be targeted and treated now, and as resources allow others with a risk of >15% (orange) should be progressively targeted.
Smoking status should reflect lifetime exposure to tobacco and not simply tobacco use at the time of risk assessment. 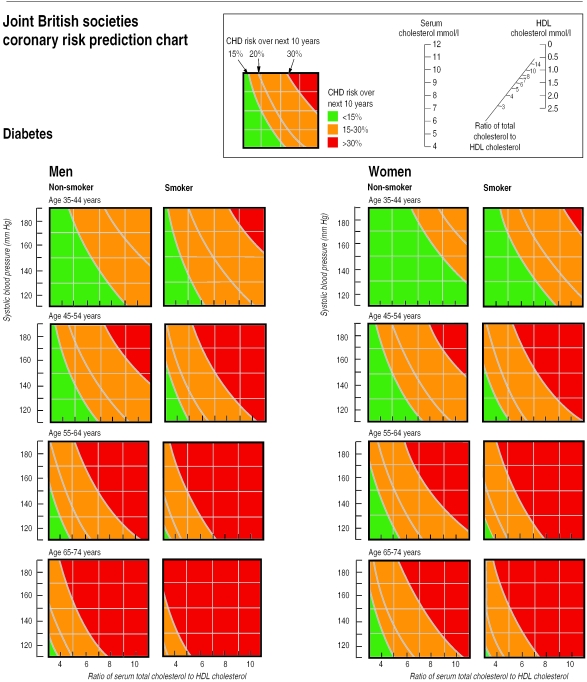
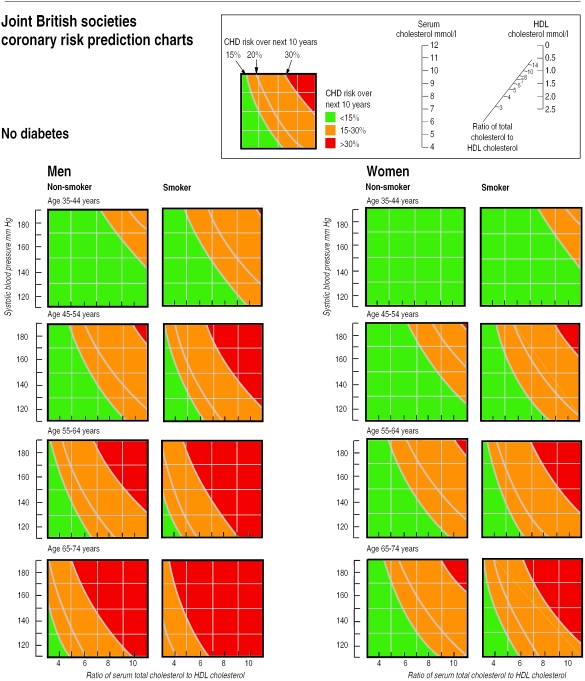
The initial blood pressure and the first random (non-fasting) total cholesterol and HDL cholesterol measurement can be used to estimate an individual's risk. However, the decision on using drug treatment should be based on repeat measurements of risk factors over a period of time. The chart should not be used to estimate risk if treatment of hyperlipidaemia or blood pressure has already been started.
Risk of coronary heart disease is higher than indicated in the charts for:
Patients with a family history of premature coronary heart disease (<55 years in men and <65 years in women), which increases the risk by a factor of approximately 1.5
Those with raised triglyceride concentrations
Those who are not diabetic but have impaired glucose tolerance
Women with premature menopause
Ages approaching the next age category: as risk increases exponentially with age, the risk will be closer to the higher decennium for the last four years of each decade.
In ethnic minorities the risk chart should be used with caution as it has not been validated in these populations.
The estimates of risk from the chart are based on groups of people, and in managing an individual patientthe doctor also has to use clinical judgment in deciding how intensively to intervene on lifestyle and whether or not to use drug treatment.
A patient can be shown on the chart the direction in which the risk of coronary heart disease can be reduced by changing smoking status, blood pressure, or cholesterol.
People at high risk without clinically overt CHD or other major atherosclerotic disease
Patients with hypertension, dyslipidaemia, diabetes mellitus, family history of premature coronary heart disease, or a combination of these risk factors, are at high risk of developing coronary heart disease or other atherosclerotic disease. Patients with diabetes mellitus are at particularly high risk. Individuals at high multifactorial risk of developing coronary heart disease, or other atherosclerotic disease, can be identified from the coronary risk prediction chart (figure).
As absolute risk of coronary heart disease (non-fatal myocardial infarction or death from coronary heart disease) increases, so lifestyle intervention should be intensified. Introducing drug treatment for raised blood pressure or lipid concentrations should be strongly determined by the absolute level of risk of developing disease(see table). An absolute risk of coronary heart disease ⩾15% (equivalent to a cardiovascular risk of 20%) over 10 years is sufficiently high to justify drug treatment.
Exceptions to treatment based on absolute risk are:
Hypertension (systolic blood pressure >160 mm Hg or diastolic blood pressure >100 mm Hg) or hypertension with associated target organ damage
Familial hypercholesterolaemia or other inherited dyslipidaemia
Diabetes mellitus with associated target organ damage.
Drug treatment is required for all these patients to reduce the risk of coronary heart disease (and cardiovascular risk).
A staged approach to managing patients at high risk is advised. As a minimum, those with an absolute coronary heart disease risk ⩾30% should be targeted and treated now and, as resources allow, individuals with a risk ⩾15% should be progressively targeted. For all high risk patients, every effort should be made to achieve the lifestyle, risk factor, and therapeutic targets given in the table.
Key references
Wood DA, Durrington P, McInnes G, Poulter N, Rees A, Wray R. Joint British recommendations on prevention of coronary heart disease in clinical practice. Heart 1998;80(suppl):S1-29.
British Hypertension Society. Guidelines for hypertension management 1999:summary. BMJ 1999;319:630-5.
Other resources available from the British Heart Foundation
BHF Factfiles 8/99 and 9/99
Colour wall poster of the coronary risk prediction chart
Cardiac risk assessor program to estimate absolute risk of coronary heart disease (or cardiovascular risk) on a personal computer
Contact the British Heart Foundation (tel: 020 7935 0185; fax: 020 7486 1273)
Table.
Lifestyle, risk factor, and therapeutic targets for prevention of coronary heart disease (CHD) in patients with established CHD or other atherosclerotic disease and in healthy people at high risk of developing this disease
| Patients with CHD or other atherosclerotic disease | People without overt CHD or atherosclerotic disease at high risk (absolute CHD risk⩾15% over 10 years) | |
|---|---|---|
| Lifestyle targets for all patients | ||
| Stop smoking, make healthier food choices, increase aerobic exercise, and moderate alcohol consumption Body mass index <25 kg/m2 is desirable, with no central obesity | ||
| Targets for other risk factors | ||
| Blood pressure <140 mm Hg systolic and <85 mm Hg diastolic | ||
| • All patients to have blood pressure reduced to consistently <140/85 mm Hg | • Systolic blood pressure ⩾160 mm Hg or diastolic blood pressure ⩾100 mm Hg: lifestyle advice and drug treatment if blood pressure is sustained at these levels on repeat measurements regardless of absolute CHD risk | |
| • Systolic blood pressure 140-159 mm Hg or diastolic blood pressure 90-99 mm Hg: | ||
| CHD risk ⩾15% or target organ damage: Lifestyle advice and drug treatment if blood pressure is sustained at these levels on repeat measurements | If CHD risk <15% and no target organ damage: Lifestyle advice and reassess annually | |
| • Systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg: | ||
| Lifestyle advice and reassess in 5 years | ||
| Total cholesterol <5.0 mmol/l (LDL cholesterol <3.0 mmol/l) | ||
| • All patients to have total cholesterol reduced to consistently below 5.0 mmol/l (LDL cholesterol <3.0 mmol/l) | • Familial hypercholesterolaemia or other inherited dyslipidaemia: Lifestyle advice and drug treatment | |
| • Total cholesterol >5.0 mmol/l: | ||
| CHD risk ⩾15%: Lifestyle advice and drug treatment* if cholesterol sustained on repeat measurements | If CHD risk <15%: Lifestyle advice; reassess annually if risk is close to 15% | |
| Patients with diabetes mellitus | ||
| Total cholesterol <5.0 mmol/l (LDL cholesterol <3.0 mmol/l) | ||
| Blood pressure <130 mm Hg systolic and <80 mm Hg diastolic (<125 mm Hg systolic and <75 mm Hg diastolic when there is proteinuria) | ||
| Optimal glycaemic control: HbA1c <7% | ||
| Cardioprotective drug treatment | ||
| • Aspirin for all patients | • Aspirin (75 mg daily) in individuals aged >50 years whose hypertension, if present, is controlled | |
| • β blockers at doses prescribed in clinical trials after myocardial infarction, particularly in high risk coronary patients and for at least 3 years | ||
| • Cholesterol lowering agents (statins) at doses prescribed in clinical trials | ||
| • ACE inhibitors at doses prescribed in clinical trials for patients with symptoms or signs of heart failure at time of myocardial infarction, or in those with persistent left ventricular systolic dysfunction (ejection fraction <40%) | ||
| • Anticoagulants for patients at risk of systemic embolisation with large anterior infarctions, severe heart failure, left ventricular aneurysm, or paroxysmal tachyarrhythmias | ||
| Screening of first degree blood relatives | ||
| • Screening of first degree blood relatives (principally siblings and offspring aged 18 years or older) of patients with premature CHD (men <55 years and women <65 years) or other atherosclerotic disease is encouraged and in the context of familial dyslipidaemias is essential | • Screen close relatives if familial hypercholesterolaemia or other inherited dyslipidaemia is suspected | |
LDL=low density lipoprotein; HbA1c=glycated haemoglobin; ACE=angiotensin converting enzyme.
If resources do not permit drug treatment at 15% then 30% is the minimum acceptable standard of care.
Acknowledgments
The coronary risk prediction chart is reproduced (and modified) with permission from Heart 1998;80:S1-29. © The University of Manchester.
Footnotes
Editorial by Jackson
Competing interests: None declared.


