Abstract
BACKGROUND:
Repeat Gamma Knife radiosurgery (GKRS) is an established option for patients whose pain has recurred after the initial procedure, with reported success rates varying from 68% to 95%. Predictive factors for response to the repeat GKRS are ill-defined.
OBJECTIVE:
This cohort study aimed to report the outcomes and factors predictive of success for patients who have undergone repeated GKRS for trigeminal neuralgia at Wake Forest University Baptist Medical Center.
METHODS:
Between 1999 and 2013, 152 patients underwent repeat GKRS at Wake Forest, 125 of whom were available for long-term follow-up. A retrospective chart review and telephone interviews were conducted to determine background medical history, dosimetric data, outcomes, and adverse effects of the procedure.
RESULTS:
Eighty-four percent of patients achieved at least Barrow Neurological Institute (BNI) IIIb pain relief, with 46% achieving BNI I. The 1-, 3-, and 5-year rates of BNI I pain relief were 63%, 50%, and 37%, respectively. The 1-, 3-, and 5-year rates of BNI IIIb or better pain relief were 74%, 59%, and 46%, respectively. One patient experienced bothersome numbness and 2 patients developed anesthesia dolorosa. The dominant predictive factors for pain relief were facial numbness after the first GKRS and a positive pain response to the first GKRS.
CONCLUSION:
Repeat GKRS is an effective method of treating recurrent trigeminal neuralgia. Patients who have facial numbness after the first treatment and a positive pain response to the first GKRS are significantly more likely to respond well to the second treatment.
Keywords: Gamma knife, Predictive factors, Repeat radiosurgery, Trigeminal neuralgia
Gamma Knife radiosurgery (GKRS) is a noninvasive treatment option for trigeminal neuralgia (TN).1–4 Multiple series have reported pain reduction in 81% to 96% of patients3,5–11; however, over time, relapse can occur. Repeat GKRS is an option for further intervention, with reported success rates varying from 68% to 95%.2,12–20 Although complications of repeat GKRS are rare, many patients report facial numbness after the repeat procedure.4 Facial numbness is usually acceptable to patients, with the majority stating that it is either not bothersome or is preferable to the pain of TN. In addition, there appears to be a positive correlation between postprocedure trigeminal nerve dysfunction and pain relief.2,13,15,17,18,20 Despite the overall success of repeat GKRS for TN, the treatment remains controversial, with some advocating only offering a second GKRS if the first was successful,14,17,19,20 and others offering the procedure regardless of the outcome of the initial GKRS.2,12,15,16,18 Furthermore, although postprocedure numbness is a commonly identified predictor of success, preprocedure predictive factors are not well-defined.
The goal of this study was to report the outcomes of TN patients who have undergone repeat GKRS at Wake Forest Baptist Medical Center and to identify potential predictors of successful repeat GKRS.
METHODS
Patient Population
Between 1999 and 2013, 152 patients underwent multiple GKRS procedures for TN at Wake Forest Baptist Medical Center, 37 of whom were reported in a previous study.18 Of those 152, 125 were available for long-term follow-up. Before proceeding with the repeat GKRS, all treatment options, including medical therapy, microvascular decompression, percutaneous trigeminal rhizotomy, and repeat GKRS, were discussed with the patient. Owing to a combination of factors, including pain characteristics, medical comorbidities, and patient preference, some patients elected for repeat GKRS. Patients were encouraged to wait as long as possible before undergoing repeat GKRS, with a median interval time of 15.7 months for those with a successful initial GKRS and 16.5 months for those with an unsuccessful initial GKRS, with a minimum of 3 months. The demographic data, past history, and other relevant data of the 152 patients collected from electronic medical records and telephone interviews are summarized in Table 1. Patients are classified as having typical TN if they reported that more than 50% of their facial pain was episodic after the Burchiel21 criteria. The pain of patients not meeting these criteria are classified as atypical. Patients who had their second procedure less than 6 months before the study or who did not receive both GKRS treatments at Wake Forest Baptist Medical Center were excluded from the study (Figure 1). The number of patients who met the inclusion criteria determined the study size. No outside funding was received for the study.
TABLE 1.
Patient Characteristicsa
| Variable | n | Median (IQR)/% |
|---|---|---|
| Age at initial GKRS, y | 152 | 68 (59–73) |
| Age at subsequent GKRS, y | 152 | 70 (62–78) |
| Sex | ||
| Male | 63 | 41 |
| Female | 89 | 59 |
| Laterality | ||
| Left | 65 | 43 |
| Right | 87 | 57 |
| Type of pain | ||
| Typical | 134 | 88 |
| Atypical | 18 | 12 |
| Distribution of pain (second GKRS) | ||
| V1 | 5 | 3 |
| V2 | 39 | 26 |
| V3 | 26 | 17 |
| V1, V2 | 17 | 11 |
| V1, V3 | 4 | 3 |
| V2, V3 | 34 | 22 |
| V1, V2, V3 | 24 | 16 |
| Multiple sclerosis | 22 | 15 |
| Hypertension | 84 | 55 |
| Diabetes mellitus | 22 | 15 |
| Herpes zoster | 3 | 2 |
| Smoking | ||
| Current smoker | 18 | 12 |
| Former smoker | 59 | 39 |
| Never smoker | 74 | 49 |
| Procedures before initial GKRS | 46 | 30 |
| MVD | 19 | 13 |
| Rhizotomy | 26 | 17 |
| Nerve block | 12 | 8 |
| Procedures between initial and subsequent GKRS | 6 | 4 |
| MVD | 4 | 3 |
| Rhizotomy | 2 | 1 |
| Nerve block | 0 | 0 |
| Initial GKRS outcome (BNI) | ||
| BNI I-IIIb | 127 | 87 |
| BNI IV-V | 21 | 11 |
| Duration of relief after initial GKRS, mo | ||
| BNI I | 127 | 2 (0–20) |
| BNI I-IIIb | 127 | 9 (2.5–24) |
| Time between GKRS, mob | ||
| First GKRS BNI I-IIIb | 127 | 15.7 (7.3–46.8) |
| First GKRS BNI IV-V | 18 | 16.5 (7.59–47.87) |
BNI, Barrow Neurological Institute; GKRS, Gamma Knife radiosurgery; IQR, interquartile range; MVD, microvascular decompression.
Six patients underwent a non-GKRS procedure between their initial and repeat GKRS, and so were excluded from these calculations.
FIGURE 1.
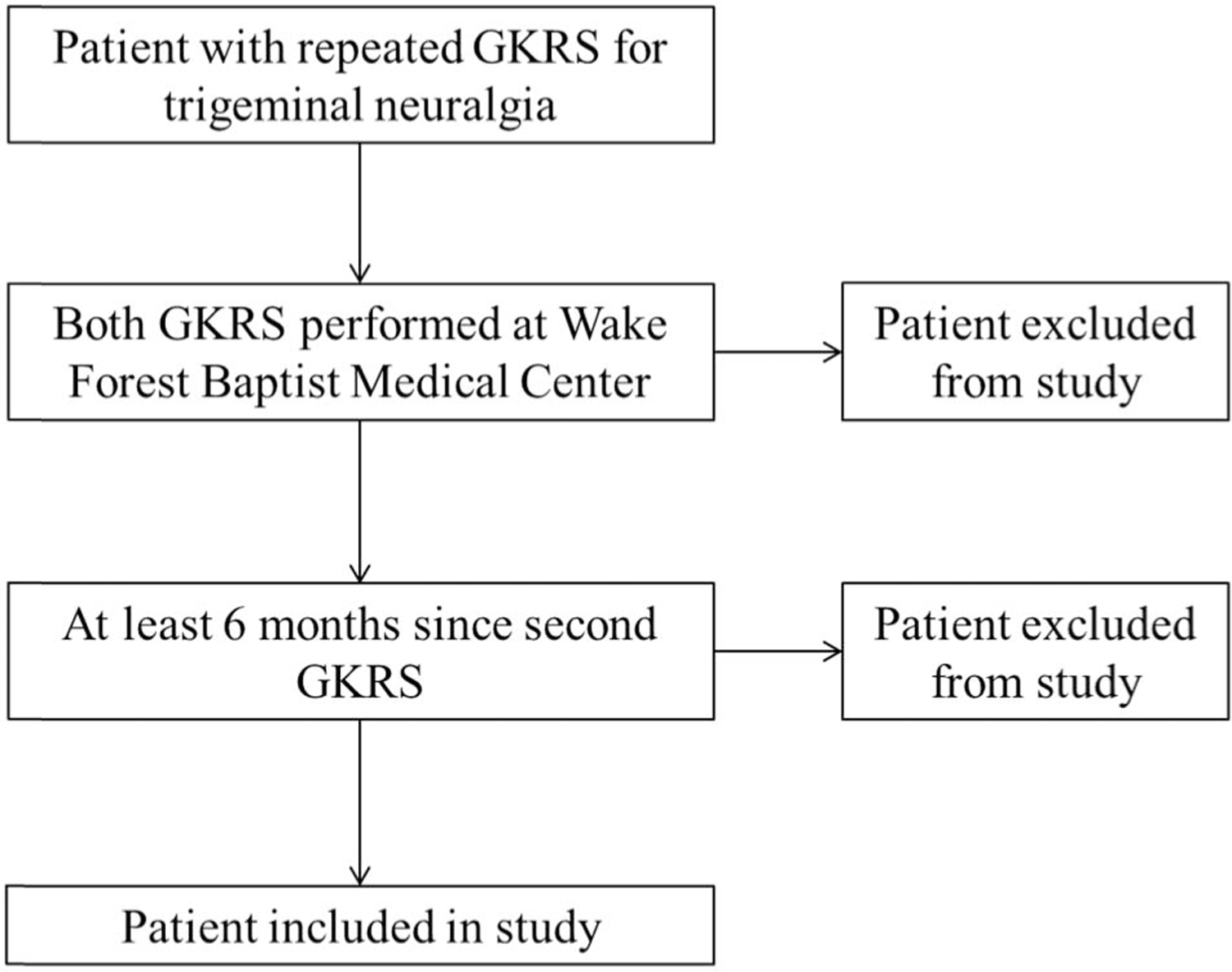
Flow diagram depicting the determination of patient eligibility. GKRS, Gamma Knife radiosurgery.
Radiosurgical Technique
GKRS was performed with the Gamma Knife model B (1999–2004), 4C (2004–2009), or Perfexion (2009–2014; Elekta, Norcross, Georgia). On the day of treatment, a Leksell model G stereotactic head frame (Elekta) was placed, and the patient then underwent a high-resolution magnetic resonance imaging (MRI) study on a GE 3T scanner. If the patient was unable to undergo MRI, a computed tomography (CT) scan was obtained. Six patients had a CT scan performed for both the first and second GKRS, with 2 additional patients having CT scans for the first GKRS only and 6 having CT scans for the second GKRS only. The Leksell GammaPlan treatment planning system (Elekta) was used to generate a treatment plan. A 4-mm collimator was used for all but 2 patients, for whom concentric 4-mm and 8-mm collimators were used. The radiation dose was prescribed at the 100% isodose line for all patients. Early in the study, the initial 4-mm shot coordinate was placed more proximally along the nerve, with the 50% isodose line tangential to the pons. Later in the study, the treatment philosophy changed, and the initial shot coordinate was placed more distally. Shot coordinates for repeat treatments were moved distally if the initial shot was placed proximally and vice versa to minimize overlap. Targeting for patients with CT scans only for planning was as previously described by Attia et al.22 The median dose for the initial treatment was 90 Gy (interquartile range [IQR] 85–90). The median dose for the second treatment was 80 Gy (IQR 80–85). The collimator output factors were 0.87 (models B and 4C) and 0.81 (Perfexion).
Radiosurgery Dosimetry
Dosimetry was obtained from the archived treatment plans by using the Leksell GammaPlan software. For patients whose treatment plans were not retrievable from older archive media, doses were abstracted from the medical record and prior article databases when possible. The dose administered at each treatment and the cumulative dose of the treatments were calculated. The doses to the root entry zone, surface of the pons, and petrous dura at each treatment as well as the cumulative dose to each landmark were also calculated. Anatomic landmarks were defined as previously described by Lucas et al23 and Marshall et al.11
Follow-up
Patients were instructed to return for a follow-up appointment 3 to 6 months after the procedure. If the pain control was acceptable to the patient, they were instructed to taper off of their pain medicines and to follow up as needed. Long-term follow-up data were collected by telephone interview. If the patient was deceased or could not be interviewed by phone, follow-up data were collected from a spouse or caregiver with adequate knowledge of the patient’s condition (n = 10). The median follow-up period from the repeat GKRS was 27.1 months (IQR 11.2–65.3), with 21 patients having less than 6 months of follow-up data. The median follow-up period from the initial GKRS to present was 56.9 months (IQR 23.8–103.8).
Treatment Outcomes
Patient outcomes were evaluated by using the Barrow Neurological Institute (BNI) Pain Scale.24 Complete pain relief was defined as BNI of I. Partial pain relief was defined as BNI of II to IIIb. A BNI score of I to IIIb was considered a successful treatment, but a score of IV or V was considered a treatment failure. The time from the procedure to partial and complete pain relief and the total duration of partial and complete pain relief were determined by using the chart review and telephone interviews. If a patient experienced both complete and partial pain relief, the duration of partial pain relief included the time with complete pain relief.
The chart review and telephone interviews were also used to determine whether patients experienced any facial numbness (yes vs no) and, if so, whether the numbness was bothersome (yes vs no), and if it was preferable to the TN pain (yes vs no) before the procedure. Patients were also asked about the presence or absence of any corneal dryness, masseter weakness, and/or anesthesia dolorosa.
Statistical Analysis
Descriptive analyses for continuous data were summarized by using the median and interquartile range or range and tested across groups using either the two-tailed t test or analysis of variance. Categorical and ordinal data were summarized using frequencies and counts and were tested using the χ2 or Fisher exact test. Time-to-event outcomes were described by using the Kaplan-Meier estimator. Comparisons across strata were completed using the log-rank statistic. A univariate logistic regression analysis was used to identify factors predictive of treatment response at 3 to 6 months. Covariates significant at the P < .2 level were selected by using a combination of forward and backward stepwise selection methods. Additional covariates were chosen a priori for inclusion into the multivariate model and include non-GKRS procedures before the second GKRS. After the selection of covariates for the multivariate model, all covariates were tested for interactions with product terms. No interactions were identified and thus no product terms were included in the final model. A multivariate logistic regression model was constructed following assessment for potential interactions. All analyses were completed using SAS v9.3 and data storage was completed with Microsoft Excel 2007. A P value of <.05 was considered statistically significant. When data were not obtainable for a particular field for a patient, the patient was censored from the analysis of the end point of interest. Patients with insufficient data were excluded from the study. No field was systematically absent to suggest a pattern that could introduce analytical bias.
RESULTS
Outcome Data
Treatment outcomes and toxicities of the second GKRS procedure are summarized in Table 2.
TABLE 2.
Outcomes and Toxicity of Repeat GKRSa
| Variable | n | Median (IQR)/% |
|---|---|---|
| Maximal pain response (BNI) | ||
| I | 57 | 38 |
| II | 9 | 6 |
| IIIa | 11 | 7 |
| IIIb | 24 | 16 |
| IV | 3 | 2 |
| V | 20 | 13 |
| Time to BNI IIIb response, wk | 74 | 1.14 (0–4) |
| Time to BNI I response, wk | 54 | 3 (1–6) |
| Duration of BNI IIIb response, y | 106 | 1.56 (0–3.76) |
| Duration of BNI I response, y | 122 | 0 (0–2.23) |
| Recurrence | ||
| Yes | 30 | 20 |
| No | 60 | 39 |
| Partial | 10 | 7 |
| Never remitted | 22 | 14 |
| Numbness | 88 | 59 |
| Bothersome | 1 | 1 |
| Mild/unchanged from first to second GKRS | 44 | 30 |
| Unable to determine severity | 43 | 28 |
| Mild corneal dryness | 10 | 7 |
| Anesthesia dolorosa | 2 | 1 |
| Taste disturbance/loss | 4 | 3 |
| Muscular spasms/weakness | 5 | 3 |
| Hypesthesia/paresthesias | 4 | 3 |
| Trigeminal trophic syndrome | 1 | 1 |
IQR, interquartile range; BNI, Barrow Neurologic Institute; GKRS, Gamma Knife radiosurgery.
Pain Relief
A total of 125 patients had sufficient follow-up data to determine the presence of pain relief. Of those, 124 patients had documented levels of pain response with 105 (84%) achieving at least BNI IIIb relief. A BNI score of I was achieved by 57 patients (46%) at some point, whereas 23 (19%) had no relief (BNI IV or V). The median time to BNI IIIb pain relief was 1 week (range 0–36 weeks) and the median time to BNI I relief was 3 weeks (range 0–24).
Duration of Pain Relief
Kaplan-Meier curves for BNI I and BNI IIIb pain relief after the second GKRS are shown in Figure 2. The 1-, 3-, and 5-year rates of BNI I pain relief were 63%, 50%, and 37%, respectively. The 1-, 3-, and 5-year rates of BNI IIIb or better pain relief were 74%, 59%, and 46%, respectively. The median duration of having at least BNI IIIb pain relief was 3.8 years. Sixty of 122 patients (39%) had maintained their best BNI at last follow-up, with an additional 10 patients (7%) experiencing a partial recurrence, but still maintaining a BNI of IIIb or better. Thirty patients (20%) had experienced a recurrence of their pain.
FIGURE 2.
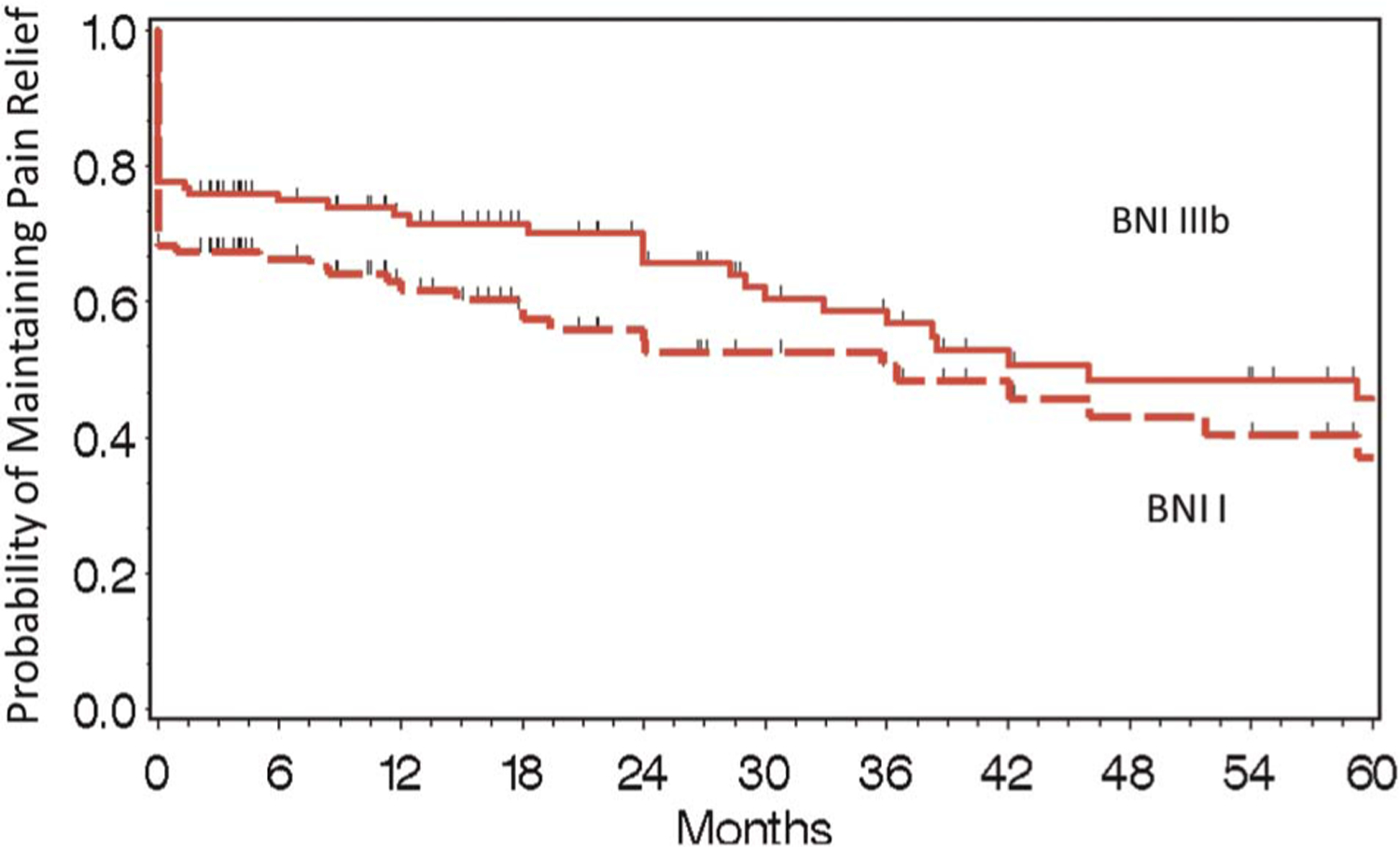
Time to BNI II to V failure and BNI IV to V following second GKRS. Kaplan-Meier curve for maintenance BNI I and BNI IIIb pain relief after the second GKRS. BNI, Barrow Neurological Institute; GKRS, Gamma Knife radiosurgery.
Figure 3 illustrates the duration of BNI I to IIIb pain relief after the second GKRS for patients with a BNI I to IIIb response after the initial GKRS compared with patients with a BNI IV to V response after the initial GKRS. The 1-, 3-, and 5-year rates of at least BNI IIIb relief after the second GKRS were 78%, 63%, and 49% for patients with a BNI I to IIIb response to the first GKRS, compared with 39%, 32%, and 24% for patients with a BNI IV to V response to the first GKRS.
FIGURE 3.
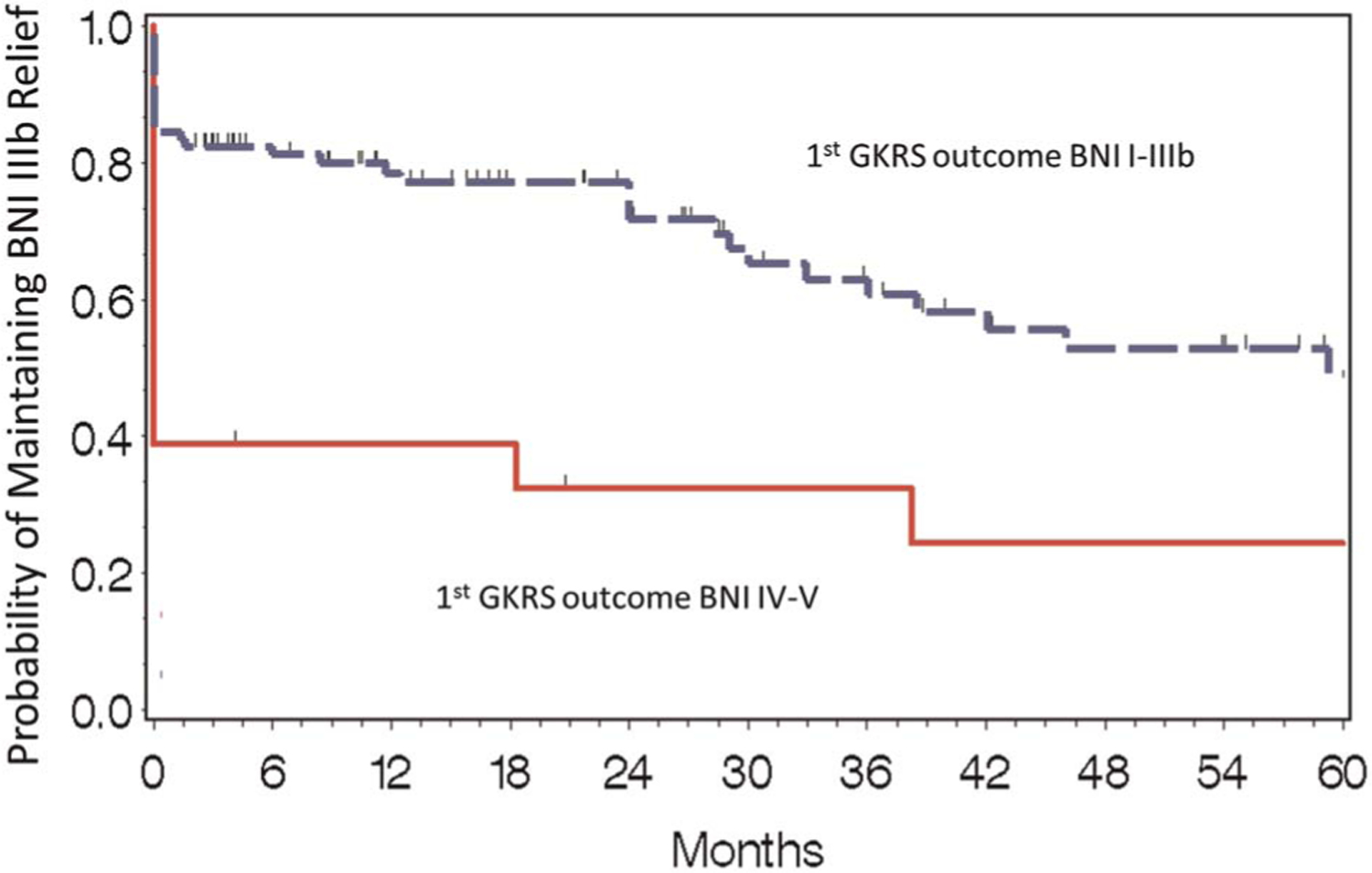
Time to BNI IV/V failure following second GKRS by IIIb or greater response to initial GKRS. Kaplan-Meier curves for maintenance of at least BNI IIIb pain relief after the second GKRS by pain relief after initial GKRS (BNI I-IIIb vs BNI IV-V). Patients with a good outcome (BNI I-IIIb) after the first GKRS were significantly more likely to have durable pain relief than those who did not respond to the first GKRS (BNI IV-V). BNI, Barrow Neurological Institute; GKRS, Gamma Knife radiosurgery.
Facial Numbness and Toxicity
Of 125 patients with relevant follow-up data, 88 patients (70%) experienced numbness from one of their treatments. Of those 88, only 1 reported that the numbness was significantly bothersome. The most commonly reported toxicity of the second GKRS was mild corneal dryness, with 10 patients (6.58%) reporting this side effect. Only 2 patients (1.3%) reported symptoms consistent with anesthesia dolorosa.
Dosimetry
GKRS plans were accessible for 95 initial GKRS and 105 repeat GKRS patients. The median doses at the first and second GKRS were 90 and 80 Gy, respectively. The median cumulative dose was 170 Gy. Dosimetric data, including the doses at the pons surface, root entry zone, and intersection of the nerve and the petrous dura, are contained in Table 3. A sample size less than 152 indicates unavailable dosimetric data.
TABLE 3.
Dosimetric Dataa
| Variable | n | Median (IQR) |
|---|---|---|
| First GKRS dose, Gy | 152 | 90 (85–90) |
| To REZ | 113 | 19.6 (11.1–54.8) |
| To petrous dura | 96 | 22 (11.3–59.5) |
| To pons surface | 113 | 40 (25.1–64.1) |
| Second GKRS dose, Gy | 152 | 80 (80–85) |
| To REZ | 124 | 18.6 (8.9–35.1) |
| To petrous dura | 104 | 28.6 (12.7–56.7) |
| To pons surface | 124 | 35 (21.2–50.9) |
| Distance from isocenter to landmarks at first GKRS, mm | ||
| REZ | 95 | 4.6 (2.5–6.8) |
| Petrous dura | 96 | 4.3 (2.4–5.8) |
| Pons surface | 113 | 3.2 (2.2–4.2) |
| Distance from isocenter to landmarks at second GKRS, mm | ||
| REZ | 103 | 4.7 (3.5–6.7) |
| Petrous dura | 104 | 3.7 (2.4–5.4) |
| Pons surface | 124 | 3.5 (2.7–4.4) |
IQR, interquartile range; REZ, root entry zone; GKRS, Gamma Knife radiosurgery.
Predictors of Pain Relief Following Repeat GKRS
A logistic regression model was constructed to define predictors of pain relief from the second GKRS. The predictive factors are shown in Table 4. The 2 dominant factors in the model were the presence of facial numbness after the first GKRS (yes vs no, odds ratio 12.26; 95% confidence interval 3.194–47.052) and a positive pain response to the first GKRS (BNI IIIb or better vs BNI IV-V, odds ratio 11.98; 95% confidence interval 2.77–51.82). Seven of 18 patients (39%) without pain relief (BNI IV-V) after the first GKRS achieved at least BNI IIIb or better pain relief at some point after the second GKRS, including 4 with BNI I (22%). There was no statistically significant relationship between outcomes and any of the dosimetric data in this study.
TABLE 4.
Predictive Factors for Pain Relief Following Second GKRSa
| Variable | Odds Ratio | 95% CI | P Value |
|---|---|---|---|
| Response to first GKRS (BNI I-IIIb vs BNI IV-V) | 11.98 | 2.77–51.82 | <.001 |
| Facial numbness after first GKRS | 12.26 | 3.19–47.05 | <.001 |
| Hypertension | 4.56 | 1.22–17.07 | .02 |
| Time between first and second GKRS | 1.33 | 0.95–1.85 | .10 |
| Non-GKRS procedure between first and second GKRS | 1.24 | 0.07–23.68 | .89 |
CI, confidence interval; BNI, Barrow Neurologic Institute; GKRS, Gamma Knife radiosurgery.
Multiple Sclerosis Population
The present analysis included 22 patients with multiple sclerosis (MS). The Kaplan-Meier curves for patients with a history of MS in comparison with those without are shown in Figure 4. Although a history of MS was predictive of both the response to treatment and the durability of treatment in univariate analysis, it was not significant in either multivariate model.
FIGURE 4.
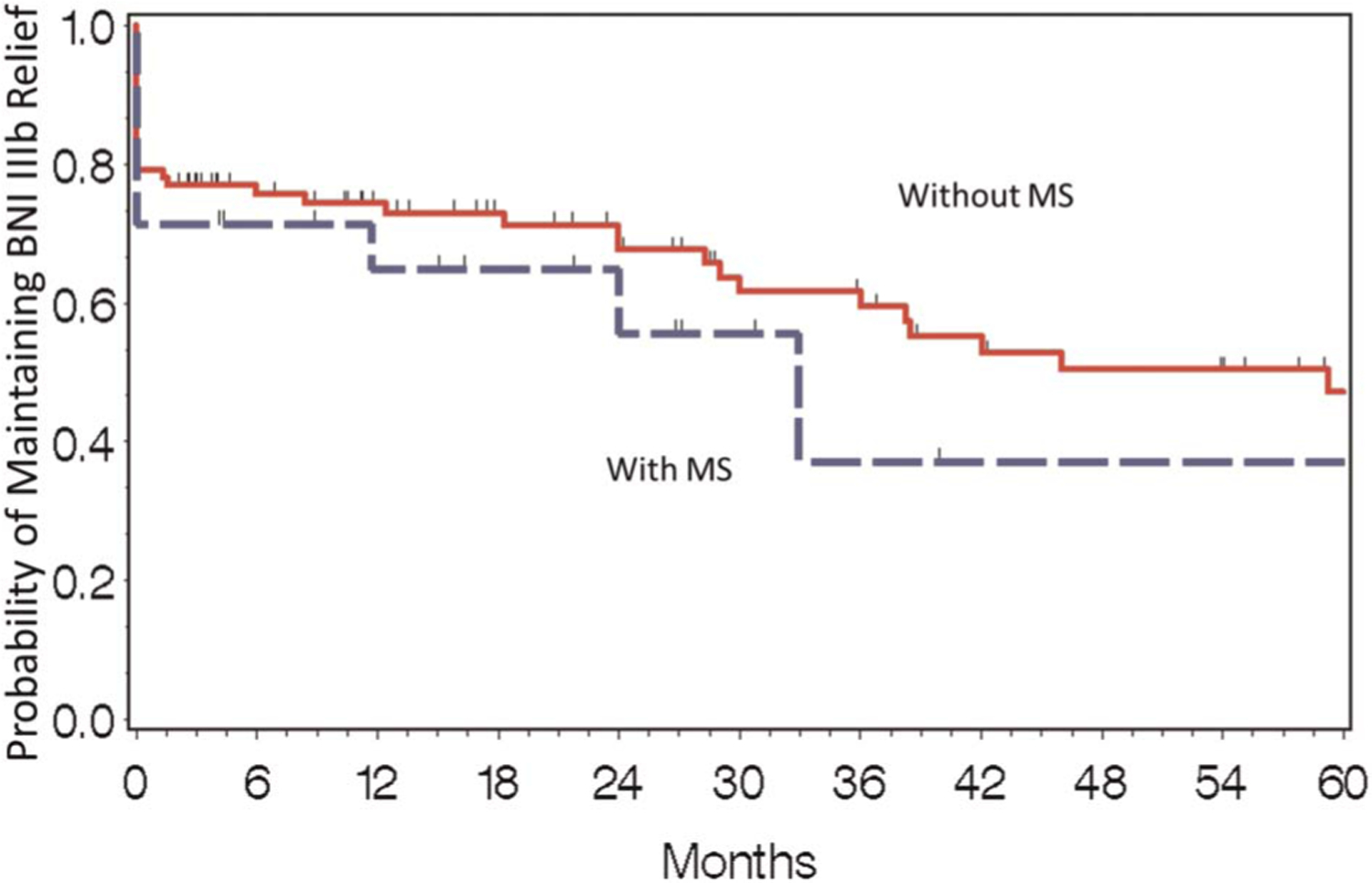
Time to BNI IV/V failure following second GKRS by concurrent diagnosis of multiple sclerosis. Kaplan-Meier curves for maintenance of at least BNI IIIb pain relief after the second GKRS depending on a past history of multiple sclerosis. Although those without MS appeared to be more likely to maintain pain relief after the second GKRS on univariate analysis, there was not a significant relationship on multivariate analysis. BNI, Barrow Neurological Institute; GKRS, Gamma Knife radiosurgery; MS, multiple sclerosis.
DISCUSSION
Key Results
GKRS is a valuable tool in the treatment of TN. Several institutions have reported performing a second GKRS when the TN pain recurs, with summarized results shown in Table 5. The present series is one of the largest reported to date. With 84% of patients achieving a BNI of IIIb or better, the results of our analysis are consistent with previous studies. Major predictive factors for positive response to repeat GKRS include BNI IIIb or better outcome following the initial GKRS and the presence of facial numbness following the initial GKRS.
TABLE 5.
Repeat GKRS for TN Seriesa
| Author | n | First GK Dose, Gy | Second GK Dose, Gy | Favorable Outcome, % | Toxicity/Facial Numbness, % | Recurrence, % |
|---|---|---|---|---|---|---|
| Hasegawa et al12 | 27 | 75.6 (mean) | 64.4 (mean) | 85 | 13 | 17 |
| Herman et at14 | 18 | 75 (median) | 70 (median) | 78 | 11 | 22 (at 1 y) |
| Pollock et al15 | 19 | 81.6 (median) | 76.1 (median) | 95 | 58 | 11 |
| Huang et al16 | 18 | 79.3 (mean) | 52 (mean) | 68 | 36 | NA |
| Gellner et al2 | 22 | 75.2 (mean) | 74.3 (mean) | 73 | 74 | 23 |
| Dvorak et al17 | 28 | 80 (median) | 45 (median) | 61 | 29 | 25 |
| Aubuchon et al18 | 37 | 87 (mean) | 84 (mean) | 84 | 57 | 19 |
| Kimball et al19 | 45 | 80 | 70 | 91 | 48 | 44 |
| Park et al20 | 119 | 79.2 (mean) | 66.2 (mean) | 87 | 21 | 34 |
| Current study | 125 | 90 (median) | 80 (median) | 84 | 70 (cumulative) | 20 |
GK, Gamma Knife; TN, trigeminal neuralgia; NA, not available; Favorable Outcome, as defined by cited study.
Limitations
Although this is one of the largest series to date on the subject, there are some limitations to the study. The greatest limitation of the study is its retrospective nature. Other limitations of the study include recall bias on the part of the patient, particularly those with very long intervals between treatments, patient selection bias on the part of the provider, and interviewer bias in the telephone interviews. Interviewer bias was limited by having 1 person conduct all telephone interviews. A randomized prospective trial would minimize the majority of these limitations, but such a study would most likely require the participation of multiple institutions to ensure a sufficient patient population.
Interpretation
Currently, there is no consensus as to whether a second GKRS procedure should be offered to all patients or only to those who had a good response to the first treatment. Herman et al14 reported that 14 of 15 (93%) patients with a successful first procedure had a successful repeat procedure, whereas none of the 3 patients without relief after the first GKRS achieved adequate relief after the repeat procedure. However, Pollock et al15 reported that having an excellent outcome after the first procedure did not correlate with an excellent outcome after the repeat procedure. Multivariate analysis of the current series showed that patients who had a BNI of IIIb or better after their first procedure were significantly more likely to have BNI IIIb or better pain relief following the second procedure. However, 39% of patients with no response to the first procedure had a BNI IIIb or better pain response to the second GKRS. This information is useful to review with patients when discussing the option of repeat radiosurgery for refractory TN.
The other major predictive factor for beneficial pain response to the second GKRS in our multivariate analysis was facial numbness after the first GKRS. A relationship between facial numbness after a repeat GKRS and pain relief has been well reported in the literature.15,16,18 However, this is the first report of a significant relationship between numbness after the first procedure and a good outcome after the second. Review of both the presence of pain relief and facial numbness may improve patient selection for a second procedure.
Initial response has been shown to be predictive of response durability.23 The only significant predictive factor for durability in this series was response to the first GKRS, with a successful first treatment predictive for a durable response to the second. The initial response of atypical TN to GKRS has been shown to be similar to that of typical TN, but with a shorter durability of relief.23,25 Laterality of pain has also been described as a predictor of pain relief in patients undergoing initial GKRS.23 In the present series, atypical facial pain and laterality both appeared to be potential predictors of durability of pain relief, but we were not able to demonstrate any significant relationships.
Patients in this series tolerated the second GKRS very well. Although 70% of patients had numbness after the second treatment, only 1 patient reported the numbness as bothersome. Ten patients experienced mild corneal dryness, reported to be associated with the amount of brainstem irradiated,26 which was the most common nonnumbness toxicity. The most common significant toxicity was anesthesia dolorosa, which occurred in 2 patients (1.3%).
Although the rate of numbness is higher than in most series, it is still within the reported range. Furthermore, this series reports cumulative numbness from all treatments, whereas most others report only new numbness after the second GKRS. Our series also reported a similar or better rate of corneal dryness (6.58%) to previous series.15,19 This study is the first to assess the efficacy and toxicity of a repeat GKRS in the symptomatic TN population. The interest in this population stems from their distinct etiology of trigeminal pain, and the limited durable treatment alternatives. Several series have demonstrated that GKRS has similar outcomes with symptomatic TN variant.27 It had previously been unclear whether a second GKRS may increase the toxicity rates, given the preexisting demyelination from MS and recent histopathologic evidence of increased trigeminal nerve inflammation after GKRS.27,28 In the current series, underlying MS did not appear to affect the durability of pain relief or the likelihood of side effects.
Generalizability
Although this series does have its limitations, it is the largest reported series to date. The results are generally in line with previous series, and predictive factors are similar to those identified before. This information can be used to improve patient selection and outcomes.
CONCLUSION
This series demonstrates that repeated GKRS is an effective option for TN patients who have pain after an initial GKRS. Patients with a BNI IIIb or better response to the first GKRS are significantly more likely to have a BNI IIIb or better response, and to maintain that response for a longer period of time compared with those who did not respond to the first GKRS. Patients with postprocedure facial numbness after the initial GKRS were also more likely to respond to a second procedure. These findings are useful for counseling patients on their treatment options and deciding whether to offer a second GKRS, thereby improving patient selection and treatment outcomes.
COMMENT.
Gamma knife radiosurgery is effective for trigeminal neuralgia, and repeat treatment is sometimes useful when symptoms recur or fail to respond. In this study, the authors followed 152 patients who underwent a second gamma knife treatment for trigeminal neuralgia after recurrence of symptoms or failure to improve after the first treatment. They found that most patients responded well to the second procedure, with almost half experiencing some degree pain relief at 5 years. Logistic regression analysis suggested that better outcome was observed after the second procedure if pain relief and/or facial numbness were seen after the first. The authors conclude that repeat radiosurgery for trigeminal neuralgia relapse is viable.
As the authors acknowledge, the idea of repeat radiosurgery for refractory trigeminal neuralgia is not new, and multiple previous studies have identified similar results. There are nevertheless a few unexpected findings in this study. First, the reported response after radiosurgery is very short in this series, with median pain relief at 3 weeks and some patients responding as early as 1 week posttreatment. Second, although less effective if it did not work the first time, a surprising number of patients (39%) did respond to the second treatment despite no response to the first, suggesting that cumulative dose of repeated treatment may rescue non-responders. Finally, outcome in patients with multiple sclerosis was not found to be worse than for idiopathic trigeminal neuralgia, although the number of patients may have been too small to identify an effect. Otherwise, the findings of this study confirm information from previous reports.
Jonathan P. Miller
Cleveland, Ohio
ABBREVIATIONS:
- BNI
Barrow Neurological Institute
- GKRS
Gamma Knife radiosurgery
- IQR
interquartile range
- MS
multiple sclerosis
- TN
trigeminal neuralgia
Footnotes
Disclosure
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
REFERENCES
- 1.Elaimy AL, Lamm AF, Demakas JJ, et al. Gamma knife radiosurgery for typical trigeminal neuralgia: an institutional review of 108 patients. Surg Neurol Int 2013; 4:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gellner V, Kurschel S, Kreil W, Holl EM, Ofner-Kopeinig P, Unger F. Recurrent trigeminal neuralgia: long term outcome of repeat gamma knife radiosurgery. J Neurol Neurosurg Psychiatry 2008;79(12):1405–1407. [DOI] [PubMed] [Google Scholar]
- 3.Rogers CL, Shetter AG, Fielder JA, Smith KA, Han PP, Speiser BL. Gamma knife radiosurgery for trigeminal neuralgia: the initial experience of the barrow neurological institute. Int J Radiat Oncol Biol Phys 2000;47(4):1013–1019. [DOI] [PubMed] [Google Scholar]
- 4.Pollock BE. Surgical management of medically refractory trigeminal neuralgia. Curr Neurol Neurosci Rep 2011;12(2):125–131. [DOI] [PubMed] [Google Scholar]
- 5.Dhople AA, Adams JR, Maggio WW, Naqvi SA, Regine WF, Kwok Y. Long-term outcomes of gamma knife radiosurgery for classic trigeminal neuralgia: implications of treatment and critical review of the literature. J Neurosurg 2009;111(2): 351–358. [DOI] [PubMed] [Google Scholar]
- 6.Kondziolka D, Lunsford LD, Flickinger JC, et al. Stereotactic radiosurgery for trigeminal neuralgia: a multiinstitutional study using the gamma unit. J Neurosurg 1996;84(6):940–945. [DOI] [PubMed] [Google Scholar]
- 7.Sheehan J, Pan HC, Stroila M, Steiner L. Gamma knife surgery for trigeminal neuralgia: outcomes and prognostic factors. J Neurosurg 2005;102(3):434–441. [DOI] [PubMed] [Google Scholar]
- 8.Régis J, Metellus P, Hayashi M, Roussel P, Donnet A, Bille-Turc F. Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg 2006;104(6):913–924. [DOI] [PubMed] [Google Scholar]
- 9.Kondziolka D, Zorro O, Lobato-Polo J, et al. Gamma knife stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg 2010;112(4): 758–765. [DOI] [PubMed] [Google Scholar]
- 10.Maesawa S, Salame C, Flickinger JC, Pirris S, Kondziolka D, Lunsford LD. Clinical outcomes after stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg 2001;94(1):14–20. [DOI] [PubMed] [Google Scholar]
- 11.Marshall K, Chan MD, McCoy TP, et al. Predictive variables for the successful treatment of trigeminal neuralgia with gamma knife radiosurgery. Neurosurgery 2012;70(3):566–572. [DOI] [PubMed] [Google Scholar]
- 12.Hasegawa T, Kondziolka D, Spiro R, Flickinger JC, Lunsford LD. Repeat radiosurgery for refractory trigeminal neuralgia. Neurosurgery 2002;50(3): 494–500. [DOI] [PubMed] [Google Scholar]
- 13.Shetter AG, Rogers CL, Ponce F, Fielder JA, Smith K, Speiser BL. Gamma knife radiosurgery for recurrent trigeminal neuralgia. J Neurosurg 2002;97(5 suppl): 536–538. [DOI] [PubMed] [Google Scholar]
- 14.Herman JM, Petit JH, Amin P, Kwok Y, Dutta PR, Chin LS. Repeat gamma knife radiosurgery for refractory or recurrent trigeminal neuralgia: treatment outcomes and quality-of-life assessment. Int J Radiat Oncol Biol Phys 2004;59(1):112–116. [DOI] [PubMed] [Google Scholar]
- 15.Pollock BE, Foote RL, Link MJ, Stafford SL, Brown PD, Schomberg PJ. Repeat radiosurgery for idiopathic trigeminal neuralgia. Int J Radiat Oncol Biol Phys 2005; 61(1):192–195. [DOI] [PubMed] [Google Scholar]
- 16.Huang CF, Chuang JC, Tu HT, Lin LY. Repeated gamma knife surgery for refractory trigeminal neuralgia. J Neurosurg 2006;105(suppl):99–102. [DOI] [PubMed] [Google Scholar]
- 17.Dvorak T, Finn A, Price LL, et al. Retreatment of trigeminal neuralgia with gamma knife radiosurgery: is there an appropriate cumulative dose? Clinical article. J Neurosurg 2009;111(2):359–364. [DOI] [PubMed] [Google Scholar]
- 18.Aubuchon AC, Chan MD, Lovato JF, et al. Repeat gamma knife radiosurgery for trigeminal neuralgia. Int J Radiat Oncol Biol Phys 2011;81(4):1059–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kimball BY, Sorenson JM, Cunningham D. Repeat gamma knife surgery for trigeminal neuralgia: long-term results. J Neurosurg 2010;113(suppl):178–183. [DOI] [PubMed] [Google Scholar]
- 20.Park KJ, Kondziolka D, Berkowitz O, et al. Repeat gamma knife radiosurgery for trigeminal neuralgia. Neurosurgery 2012;70(2):295–305. [DOI] [PubMed] [Google Scholar]
- 21.Burchiel KJ. A new classification for facial pain. Neurosurgery 2003;53(5):1164–1166. [DOI] [PubMed] [Google Scholar]
- 22.Attia A, Tatter SB, Weller M, et al. CT-only planning for gamma knife radiosurgery in the treatment of trigeminal neuralgia: methodology and outcomes from a single institution. J Med Imaging Radiat Oncol 2012;56(4):490–494. [DOI] [PubMed] [Google Scholar]
- 23.Lucas JT Jr, Nida AM, Isom S, et al. Predictive Nomogram for the durability of pain relief from gamma knife radiation surgery in the treatment of trigeminal neuralgia. Int J Radiat Oncol Biol Phys 2014;89(1):120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rogers CL, Shetter AG, Ponce FA, Fielder JA, Smith KA, Speiser BL. Gamma knife radiosurgery for trigeminal neuralgia associated with multiple sclerosis. J Neurosurg 2002;97(5 suppl):529–532. [DOI] [PubMed] [Google Scholar]
- 25.Dhople A, Kwok Y, Chin L, et al. Efficacy and quality of life outcomes in patients with atypical trigeminal neuralgia treated with gamma-knife radiosurgery. Int J Radiat Oncol Biol Phys 2007;69(2):397–403. [DOI] [PubMed] [Google Scholar]
- 26.Matsuda S, Serizawa T, Sato M, Ono J. Gamma knife radiosurgery for trigeminal neuralgia: the dry-eye complication. J Neurosurg 2002;97(5 suppl):525–528. [DOI] [PubMed] [Google Scholar]
- 27.Weller M, Marshall K, Lovato JF, et al. Single-institution retrospective series of gamma knife radiosurgery in the treatment of multiple sclerosis-related trigeminal neuralgia: factors that predict efficacy. Stereotact Funct Neurosurg 2014;92(1):53–58. [DOI] [PubMed] [Google Scholar]
- 28.Phillips DB, Del Bigio MR, Kaufmann AM. Gamma Knife rhizotomy-induced histopathology in multiple sclerosis-related trigeminal neuralgia. J Neurosurg 2014;121(6):1508–1513. [DOI] [PubMed] [Google Scholar]


