Abstract
Introduction
Antenatal care (ANC) interventions improve maternal and neonatal outcomes. However, access to ANC may be inequitable due to sociocultural, monetary and time factors. Examining drivers of ANC disparities may identify those amenable to policy change.
Methods
We conducted an ANC services equity analysis in selected public facilities in Geita, Tanzania, where most services are free to the end-user, and Atlantique, Benin, where every visit incurs user fees. Data on total ANC contacts, quality of care (QoC) indicators and wait times were collected from representative household surveys in the catchment of 40 clinics per country and were analysed by education and wealth. We used indices of inequality, concentration indices and Oaxaca-Blinder decompositions to determine the distribution, direction and magnitude of inequalities and their contributing factors. We assessed out-of-pocket expenses and the benefit incidence of government funding.
Results
ANC clients in both countries received less than the recommended minimum ANC contacts: 3.41 (95% CI 3.36 to 3.41) in Atlantique and 3.33 (95% CI 3.27 to 3.39) in Geita. Wealthier individuals had more ANC contacts than poorer ones at every education level in both countries; the wealthiest and most educated had two visits more than the poorest, least educated. In Atlantique, ANC attendees receive similar QoC regardless of socioeconomic status. In Geita, there are wide disparities in QoC received by education or wealth. In Atlantique, out-of-pocket expenses for the lowest wealth quintile are 2.7% of annual income compared with 0.8% for the highest, with user fees being the primary expense. In Geita, the values are 3.1% and 0.5%, respectively; transportation is the main expense.
Conclusions
Inequalities in total ANC visits favouring wealthier, more educated individuals were apparent in both countries. In Atlantique, reduction of user-fees could improve ANC access. In Geita, training and equipping healthcare staff could improve QoC. Community health services could mitigate access barriers.
INTRODUCTION
Antenatal care (ANC) services allow for timely identification and management of pregnancy risks and complications such as anaemia, HIV and syphilis, and better prenatal, perinatal and postnatal decision-making to improve maternal and neonatal outcomes.1 Despite these benefits, ANC services may be inequitable2 3 due to a combination of demand-side factors such as sociocultural norms,4 lack of education, and cost, and supply-side factors including distance to clinics,5 low funding,6 inadequate availability of ANC services, variation in quality of care (QoC) and inadequate staffing.7 8
Inequalities in ANC services can be identified and quantified by measuring access against an externally set standard, such as the WHO recommended four or eight ANC visits,1 comparing QoC provided and assessing the differences in access and quality across measures of socioeconomic status (SES) such as wealth or education. Each SES measure has advantages and disadvantages for equity analysis. Education can influence health through multiple channels such as improved information acquisition, risk aversion, discounting, mediation of health behaviour and its correlation with occupation.9 Education is relatively easier and less contentious to measure compared with wealth.10–12 Wealth, an imperfect proxy for consumption income, which is difficult to measure, influences health through factors such as affordability, access to health insurance and time.13–15 Assessing both education and wealth provide a more complete picture of equity (fairness/justness of accessibility to healthcare).16 Quantifying inequalities in education, wealth, location, etc, and their impact on healthcare access enables the design and implementation of policies to address inequity. Some policies, such as increasing outreach services or eliminating user fees, may be relatively easy to implement. Other policies, such as building more clinics or addressing sociocultural barriers, may require significant investments and longer-term efforts.
We describe inequalities in ANC and identify their determinants in two countries with different health financing structures. ANC services in Tanzania are predominantly financed by the government with some support from donors for vertical programmes such as HIV and malaria. In Benin, ANC services are also partially financed by user fees, alongside government and donor contributions. We compare total ANC contacts and ANC QoC indicators as outlined by the WHO, for example, blood pressure (BP) and urine tests, using education and wealth as measures of socioeconomic position.1 17
In both countries, pregnant women face additional barriers to care including out-of-pocket (OOP) expenses for transportation and long waiting times. There are also fees for additional recommended services such as ultrasonography as these are not covered by the user fee exemptions or are explicitly charged; in some cases, services such as ultrasonography may not be available in public facilities thus women must use private facilities. These system barriers are often accompanied by other barriers like loss of earnings/productivity during clinic visits or caretaking for children left at home.
Health financing policies in both countries explicitly call for equitable access to ANC. We, therefore, examine the distributional impact (benefit incidence analysis) of government funding for ANC in both countries. By assessing equity of access to quality ANC and intermittent preventive treatment for malaria in pregnancy (IPTp) as a function of wealth and education, this analysis aims to provide insights into the factors that contribute to inequalities in ANC access and QoC, in the hopes of identifying actionable items to improve access and quality of ANC services.
METHODS
This analysis was conducted using data collected during baseline and endline household cross-sectional surveys conducted in the context of cluster randomised trials designed to assess the impact of the group ANC (G-ANC) model on the uptake of ANC and IPTp in Geita Region, northwest Tanzania and Atlantique Department, Benin. In addition, both studies assessed the feasibility and acceptability of using pregnant women as a sentinel surveillance population. Relevant data, including SES, education, age, uptake of ANC and IPTp, and measures of ANC QoC, were used to assess whether services are being delivered equitably across countries. Due to the low uptake of the study intervention, we did not explore the impact of the GANC intervention on equity measures.
In Tanzania, data were collected from all six councils of Geita Region between 2019 and 2021. In 2022, the population of Geita Region was 2977608 with approximately 49% of the population living below the poverty line.18 The region is home to Tanzania’s largest gold mining industries. Other major industries in the region are agriculture and fishing. National ANC guidelines in Tanzania, which are based on the 2016 WHO guidelines,1 recommend pregnant women receive a minimum of eight ANC visits. Geita region in Tanzania was selected as the focus of this research given the low uptake of four ANC visits—in 2022 only 56.4% of women completed four or more ANC visits in Geita Region, as compared with the national average of 64.7%.19 Likewise, the proportion of women delivering in a health facility or by a skilled provider is substantially lower in Geita Region than the national average (72.1% and 77.1%, respectively, in Geita vs 81.0% and 84.8% nationally).19
Atlantique is 1 of 12 departments (administrative divisions) in Benin, located in south-central Benin along the Atlantic coast; the study was conducted from 2021 to 2022 in all three health zones of Atlantique. As of 2013, the total population of the department was 1398229. The major industry in the region is fishing. Atlantique was selected to avoid areas with other concurrent efforts to improve ANC attendance that would have confounded the results of the intervention study. Unlike in Tanzania, the national guidelines recommend a minimum four ANC visits during pregnancy in Benin. A relatively higher proportion of women in Atlantique attended three ANC visits (78%) compared with the country overall (59.6%). Atlantique has relatively higher coverage of skilled attendants at delivery (93.2%) compared with the country overall (89.5% in urban areas and 79.3% in rural areas).20
Study design
The parent study comprised a cluster randomised controlled trial of G-ANC, including a baseline and endline survey to assess the impact of the intervention. In each country, 40 facilities with an average monthly first ANC attendance of 20–120 women were selected to participate, and, following a baseline survey, facilities were randomised 1:1 to control and intervention arms. In the control arm, ANC care was delivered as per standard practice. In the intervention sites, women presenting for first ANC prior to 24 weeks were to be offered the opportunity to join group care starting with the second visit; women presenting after 24 weeks or declining to join a group received standard ANC care. Due to the timing of the study with respect to the COVID-19 pandemic, in Tanzania, the G-ANC intervention was discontinued approximately 2 months after initiation in early 2020 and was not resumed, however, both baseline and endline surveys were still conducted in order to address the question of pregnant women attending ANC could be as a sentinel surveillance population for uptake of malaria interventions.21 Thus, the disruption due to COVID-19 did not affect this study.
Baseline and endline cross-sectional household surveys conducted in one randomly selected enumeration area per included health facility consisted of demographics and a questionnaire administered to all women in randomly selected households that had completed a pregnancy (ie, given birth) within the past 12 months. The woman’s questionnaire largely mirrored the questions in the demographic health survey, collecting data on ANC interventions received and pregnancy outcomes.
Indicators
We selected the following ANC quality indicators for the analyses: total ANC visits—to compare attendance against an external threshold of 4–8 recommended visits; care quality—BP, urinalysis, blood tests (eg, haemoglobin, syphilis); system navigation—waiting time and client related—distance to facility, travel time.1 We estimate household wealth relative to national quintiles based on ownership of an abridged set of durable assets that were combined into a ranked index using principal component analysis.22 For analyses on OOP and government financing incidence benefit (who benefits most from government funding), we simulate household income from the created wealth indices using the Harttgen and Vollmer approach.23
Measures of inequality
We use different methods to quantify wealth-related and education-related inequality in ANC services. We first used slope and relative indices of inequality to estimate the differential distribution of each health indicator across education and wealth.24 25 The slope index of inequality (SII) estimates the absolute difference in health status between individuals/groups at both ends of the SES spectrum. However, the SII is sensitive to overall average health levels. The relative index of inequality (RII) instead measures relative inequality between extremes of disadvantage, quantifying disparities through the rate ratio.24 This better accounts for variations between populations of interest. While the strength of the RII lies in its rescaling of inequalities, it can mask the absolute conditions of extreme groups in access to care. Using both indices leverages these strengths while concomitantly offsetting their limitations, giving a more comprehensive picture of inequality.26
We then calculated the concentration index (CI), a generalisation of the Gini index, to quantify the magnitude and directionality of the inequalities.25 27 28 A negative CI indicates that the burden is on the poor while a positive CI indicates that the burden is on wealthier individuals. For example, a negative CI for ANC contacts indicates that poorer people have fewer visits relative to wealthier ones.25 27 28
We then conducted multivariable regressions including Oaxaca-Blinder decomposition analyses to assess (explain) the contribution in inequality in ANC indicators that arise from differences in the characteristics (‘endowments’) of individuals, for example, differences in education and those that arise from the differential effects (‘unexplained’ or ‘coefficients’) of these characteristics.29 30 Some of the unexplained factors include hard-to-measure factors such as discrimination based on wealth, education or tribe. For the decompositions, we dichotomised the wealth variable into non-poor and poor, with those in the two highest quintiles classified as non-poor and the rest classified as poor.
In negative binomial multivariate regressions (ANC attendance as a count variable), we controlled for sociodemographic variables including maternal age and squared maternal age, maternal education, total number of children under-5, marital status and simulated household income. We also controlled for distance, waiting time, spousal support and household composition.
Finally, we assessed if the government financing for ANC services including labour and delivery is equitable, that is, a benefit incidence analysis. We also assessed the share of OOP expenditure for ANC to simulated household income to assess for the proportion of catastrophic ANC-related health expenditure.31
We conducted the analyses in Stata V.14.2 (StataCorp, https://www.stata.com), Python V.3.7 (Python Software Foundation) and R V.4.1.2 (https://www.R-project.org/).
RESULTS
This analysis included 2172 women in Geita, Tanzania (1111 at baseline and 1061 at end line) and 2539 in Atlantique, Benin (1259 at baseline and 1280 at end line). Relative to the national quintiles, among our population, 11.7% were in the lowest, 32.2% in the second lowest, 25.6% in the middle, 23.0% in the second highest and 7.6% in the highest wealth quintile in Geita (vs the 2015 Tanzania Demographic Health Survey19), and 27.7% were in the lowest, 6.5% in the second lowest, 36.9% in the middle, 19.5% in the second highest and 9.4% in the highest wealth quintile in Atlantique (vs 2011–2012 Benin Demographic Health Survey32). In Geita, 33.5% had no formal education/less than primary schooling, 57.4% had completed primary school and 9.1% had completed secondary education or more. In Atlantique, 46.2% had no formal education/less than primary schooling, 31.2% had completed primary school and 22.5% had completed secondary education or more.
ANC clients in Geita are on average younger and have more children than those in Atlantique. The mean number of ANC visits was less than the 4 and 8 recommended visits, respectively, at 3.5 in Atlantique and 3.3 in Geita. The distribution of ANC attendance is more spread out in Atlantique, with the wealthiest women having on average 1.2 visits more than the poorest. In Geita, while the spread is narrower, there is still a prowealthy bias in the number of ANC visits (table 1 and figure 1).
Table 1.
Means of key demographic and quality of care indicators by wealth quintile in Benin and Tanzania
| Wealth quintile | ||||||
|---|---|---|---|---|---|---|
| Variable | Lowest | Second | Middle | Fourth | Highest | Mean |
| Benin | ||||||
| Maternal age, years | 29.7 (7.7) | 29.4 (7.5) | 29.2 (7.7) | 29.4 (7.6) | 30.2 (7.4) | 29.5 (7.6) |
| Number of children | 3.7 (2.2) | 3.8 (2.0) | 3.4 (2.0) | 3.2 (1.9) | 3.0 (1.6) | 3.4 (2.0) |
| Number of children <5 | 1.6 (0.8) | 1.7 (0.8) | 1.6 (0.8) | 1.6 (0.8) | 1.5 (0.7) | 1.6 (0.8) |
| Total household members | 4.7 (2.2) | 4.7 (1.9) | 4.8 (2.1) | 4.8 (2.1) | 5.2 (2.2) | 4.8 (2.1) |
| Education* | 1.5 (0.7) | 1.5 (0.8) | 1.7 (0.8) | 2.0 (0.9) | 2.4 (0.9) | 1.8 (0.8) |
| Married | 0.9 (0.3) | 0.9 (0.3) | 0.9 (0.3) | 0.9(0.3) | 0.9(0.3) | 0.9(0.3) |
| Total ANC visits | 3.07 (1.54) | 3.18 (1.74) | 3.38 (1.69) | 4.07 (2.01) | 4.22 (2.08) | 3.51 (1.81) |
| Quality of ANC | ||||||
| Urinalysis | 0.96 (0.19) | 0.97 (0.17) | 0.96 (0.20) | 0.95 (0.21) | 0.96 (0.19) | 0.96 (0.20) |
| BP monitoring | 0.96 (0.20) | 0.96 (0.20) | 0.98 (0.15) | 0.98 (0.15) | 0.96 (0.20) | 0.97 (0.17) |
| Blood sample | 0.88 (0.32) | 0.84 (0.37) | 0.90 (0.30) | 0.90 (0.30) | 0.91 (0.29) | 0.89 (0.31) |
| IPTp doses | 2.15 (1.13) | 2.02(.99) | 2.24 (1.26) | 2.34 (1.16) | 2.44 (1.08) | 2.25 (1.18) |
| Waiting time (min) | 88.7 (61.9) | 93.4 (68.2) | 88.7 (59.4) | 89.5 (70.8) | 100.3 (78.4) | 90.4 (65.2) |
| Time away from home (min) | 205.3 (93.0) | 204.1 (91.5) | 207.2 (91.3) | 199.6 (97.1) | 212.5 (99.4) | 205.6 (93.8) |
| Tanzania | ||||||
| Maternal age | 27.0 (7.0) | 27.4 (7.2) | 27.3 (7.1) | 26.8 (6.1) | 27.0 (5.4) | 27.1 (6.8) |
| Number of children | 4.2 (2.7) | 4.2 (2.6) | 4.2 (2.7) | 3.7 (2.4) | 2.9 (1.9) | 4.0 (2.6) |
| Children <5 | 2.0 (1.0) | 2.0 (0.9) | 2.0 (0.9) | 1.9 (0.8) | 1.7 (0.8) | 2.0 (0.9) |
| Total household members | 6.4 (2.9) | 6.9 (2.9) | 7.0 (3.1) | 6.3 (2.8) | 5.8 (3.1) | 6.6 (3.0) |
| Education* | 1.5 (0.5) | 1.6 (0.5) | 1.7 (0.6) | 1.9 (0.7) | 2.3 (0.7) | 1.8 (0.6) |
| Married | 0.8 (0.4) | 0.8 (0.4) | 0.9 (0.3) | 0.9 (0.3) | 0.9 (0.3) | 0.9 (0.3) |
| Total ANC visits | 3.16 (1.53) | 3.19 (1.34) | 3.19 (1.32) | 3.56 (1.37) | 3.88 (1.58) | 3.33 (1.40) |
| Quality of ANC | ||||||
| Urinalysis | 0.52 (0.50) | 0.49 (0.50) | 0.57 (0.50) | 0.59 (0.49) | 0.75 (0.43) | 0.56 (0.50) |
| BP monitoring | 0.64 (0.48) | 0.63 (0.48) | 0.62 (0.49) | 0.68 (0.47) | 0.83 (0.38) | 0.64 (0.48) |
| Blood sample | 0.94 (0.23) | 0.95 (0.21) | 0.96 (0.20) | 0.96 (0.20) | 0.97 (0.17) | 0.96 (0.21) |
| IPTp doses | 2.37 (1.56) | 2.08 (1.37) | 2.21 (1.45) | 2.60 (1.35) | 2.52 (1.54) | 2.30 (1.43) |
| Waiting time (min) | 109.0 (75.6) | 105.0 (73.6) | 96.8 (76.5) | 86.5 (76.7) | 91.0 (84.1) | 98.2 (76.4) |
| Time away from home (min) | 261.9 (123.6) | 257.0 (120.1) | 264.9 (121.8) | 230.1 (111.8) | 207.3 (110.3) | 250.0 (119.7) |
SD in parenthesis.
Education was coded as 0 for no education, 1 for primary, 2 for secondary and 3 for tertiary education; these values represent the mean of the group.
ANC, antenatal care; BP, blood pressure; IPTp, intermittent preventive treatment for malaria in pregnancy.
Figure 1.
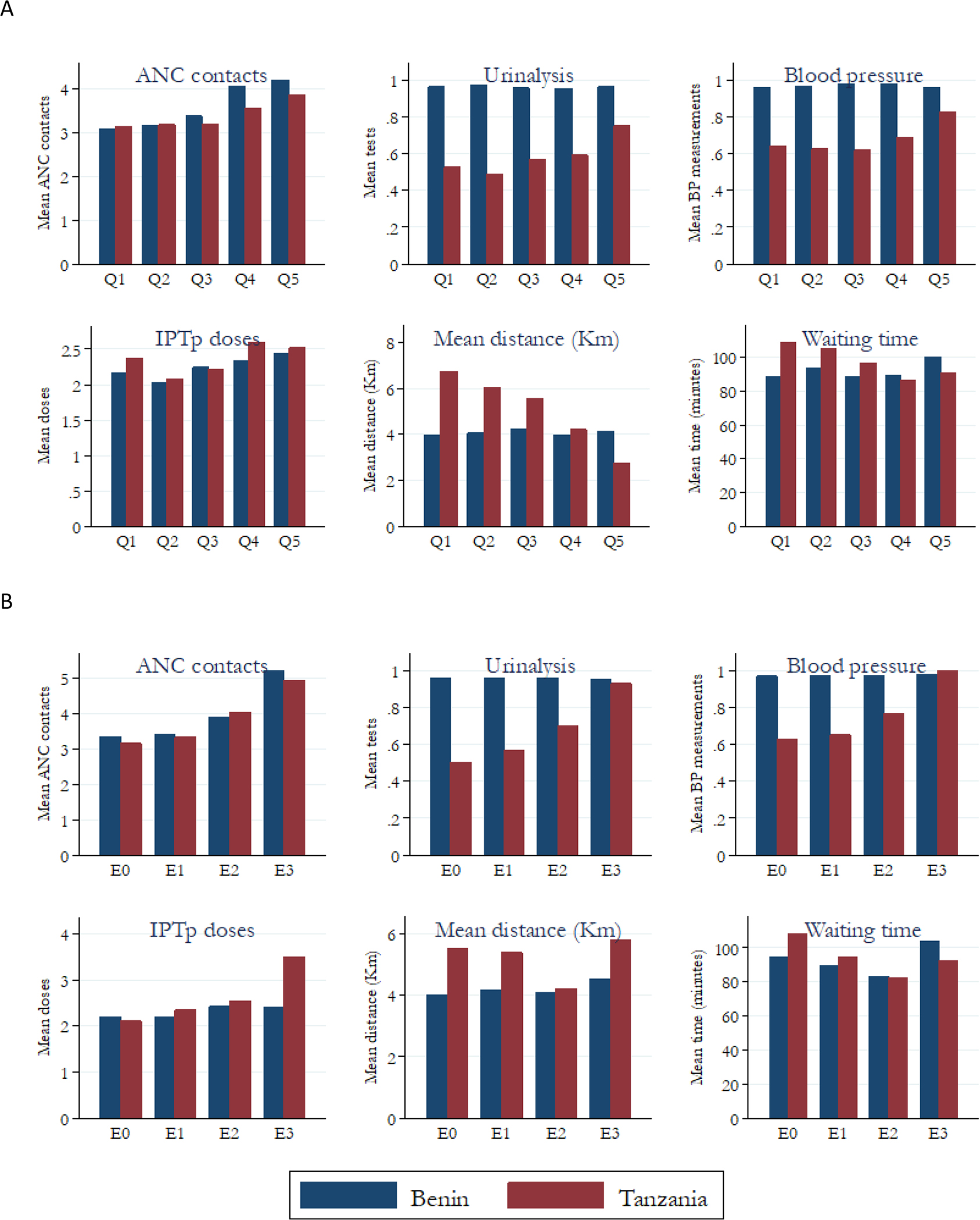
Comparison of selected antenatal care (ANC) indicators by country wealth and education. E0, No education; E1, Primary education; E2, Secondary education; E3, Higher education; Q, Wealth quintile. (A) Mean number of ANC visits completed, proportion of women who had urinalysis, proportion of women who had blood pressure measurement, mean number of IPTp doses, mean distance travelled and mean waiting time by location and wealth quintile. (B) Mean number of ANC visits completed, proportion of women who had urinalysis, proportion of women who had blood pressure measurement, mean number of IPTp doses, mean distance travelled and mean waiting time by location and level of education.
In Atlantique, pregnant women in the lowest education category completed 27% (RII=1.27) fewer visits than those in the highest category. Similarly, when ranked by wealth, the poorest quintile completed 51% (RII=1.52) fewer visits compared with those in the wealthiest quintile. In Geita, the equity gaps are slightly narrower with an RII of 1.27 and 1.23 for education and wealth, respectively. The means of ANC quality indicators such as BP monitoring, IPTp, urinalysis and blood tests are higher in Atlantique than Geita. On average, women who attended ANC in Atlantique were likely to get the recommended services irrespective of SES. In Geita, despite lack of cost recovery, there were SES differences in specific care for women who attended ANC (online supplemental table S1 and figure S1); these were not a result of differential facility attendance by wealth; that is, not due to all poorer women attending one facility with poor received service while richer women attended a different, better functioning facility.
In Atlantique and Geita, women with no education account for 12% and 13.5% of all cumulative ANC visits while those with more than secondary school education account for 26% and 29%. The lowest wealth quintiles account for 14% and 16% of all ANC visits in Atlantique and Geita, respectively, while the top quintile consumes 26% and 22% in both countries (online supplemental table S2 and figure S2).27
We found no statistically significant difference in birth weight across wealth quintiles in either country, with a difference of 58.2 (95% CI −112.9 to 229.4) g between the lowest and highest wealth quintiles in Atlantique and 94.3 (95% CI −15.7 to 204.3) g in Geita.
Concentration curves and indices
In the example of Geita, the CI is interpreted as follows: a reallocation of 2.4% of ANC visits from the upper half to the lower half of the income distribution would lead to the achievement of perfect equality. Note that the perfect equality is not the same as attainment of the minimal recommended number of visits (online supplemental table S2 and figure S2).27
Decomposition of CI
Wealth and education lead to inequality in ANC in two ways: through their direct impact (elasticity) on the outcome; and their indirect impact (CI) through their unequal distribution across the main SES disaggregation variable. On decomposition of the CI (online supplemental table S3), most of the direct inequality in total ANC visits in Atlantique is explained by maternal age (positive) and to a lesser extent wealth, spousal support (positive), and total number of children under-5 (negative); while the indirect impacts are mostly driven by maternal education, wealth and total births. There are limited facility effects—that is, service quality is generally equitable. In Geita, the main contributor to direct inequality is maternal age, while the indirect impacts are primarily from maternal education, wealth and facility effects.
In negative binomial regression multivariable analyses, ANC attendance increases by approximately 4.4% (95%CI 1.5% to 7.4%) for every year increase in maternal age to maximum of 30.1 years in Atlantique; while in Geita, the change is a statistically insignificant and modest 1.3% (95% CI −0.1% to 3.5%) to a maximum age of 28.7 years. Using marginal analysis, wealthier individuals attend more ANC services compared with relatively poor ones at every education level (figure 2).
Figure 2.
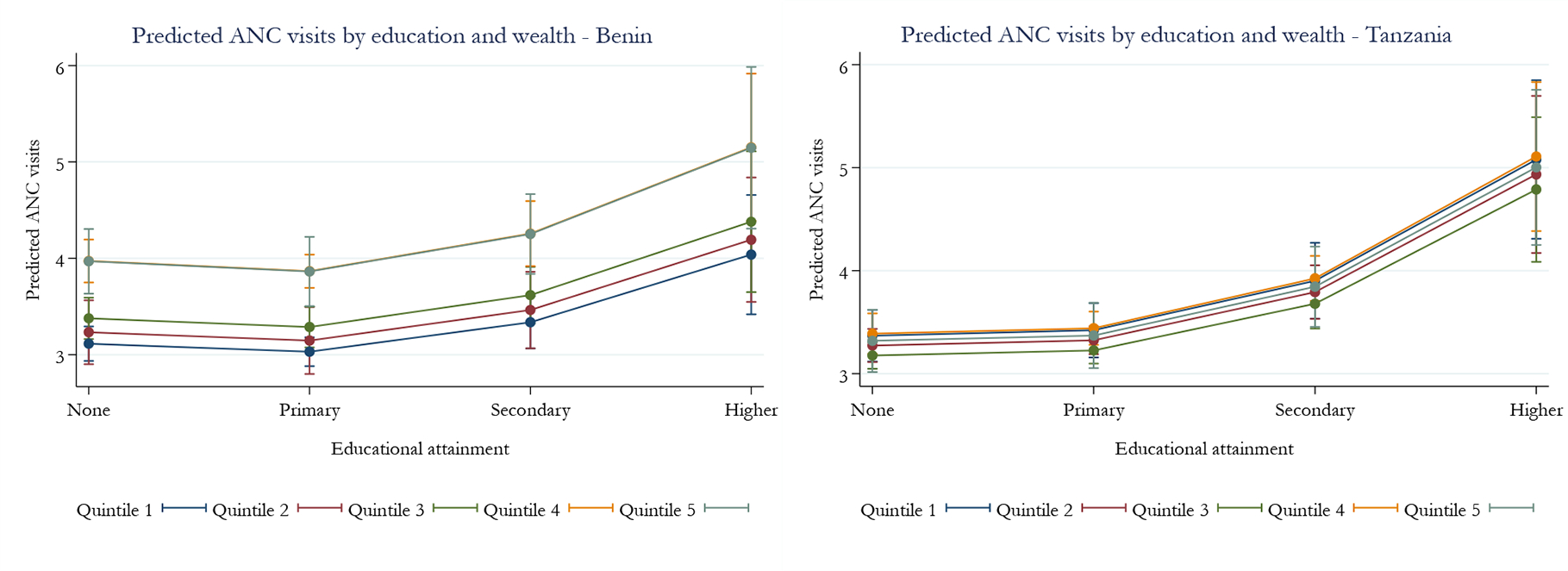
Marginal analysis, ANC attendance by education and wealth. The marginal analysis shows the effect of wealth on ANC contacts while holding education constant. In this case, wealthier people have more ANC contacts across different education levels than poorer ones. ANC, antenatal care.
We, therefore, conduct Oaxaca decomposition analyses to assess the contribution in inequality in ANC attendance that arises from differences in the characteristics (‘endowments’) of individuals, for example, differences in education and those that arise from the differential effects (‘unexplained’ or ‘coefficients’) of these characteristics (online supplemental table S4). That is, poorer people, who on average are less educated than wealthier ones, may not attend ANC services due to barriers to access or because they are less knowledgeable about the benefits of ANC.
The decomposed analyses indicate that education is the most important factor in ANC attendance in both countries. The most educated women attended on average 0.84 (.20) and 0.78 (.13) more visits than their least educated counterparts in Atlantique and Geita, respectively (online supplemental table S1). Wealth was important, but less so than education; poor ANC clients attended on average 1.44 (.18) and 1.516 (.080) fewer visits in Atlantique and Geita, respectively (online supplemental table S1). In Atlantique, the difference in the effects of the coefficients (unexplained) accounts for most of the difference (80.1%–88.8% depending on the type of decomposition done) in ANC attendance. In Geita, the unexplained differences in the mean values of the characteristics of the clients account for 47.1%–65.9% depending on the type of decomposition done. Of the explained differences (endowment effects), education accounts for around 76% of the variation in Benin and 47% in Geita (figure 3).
Figure 3.
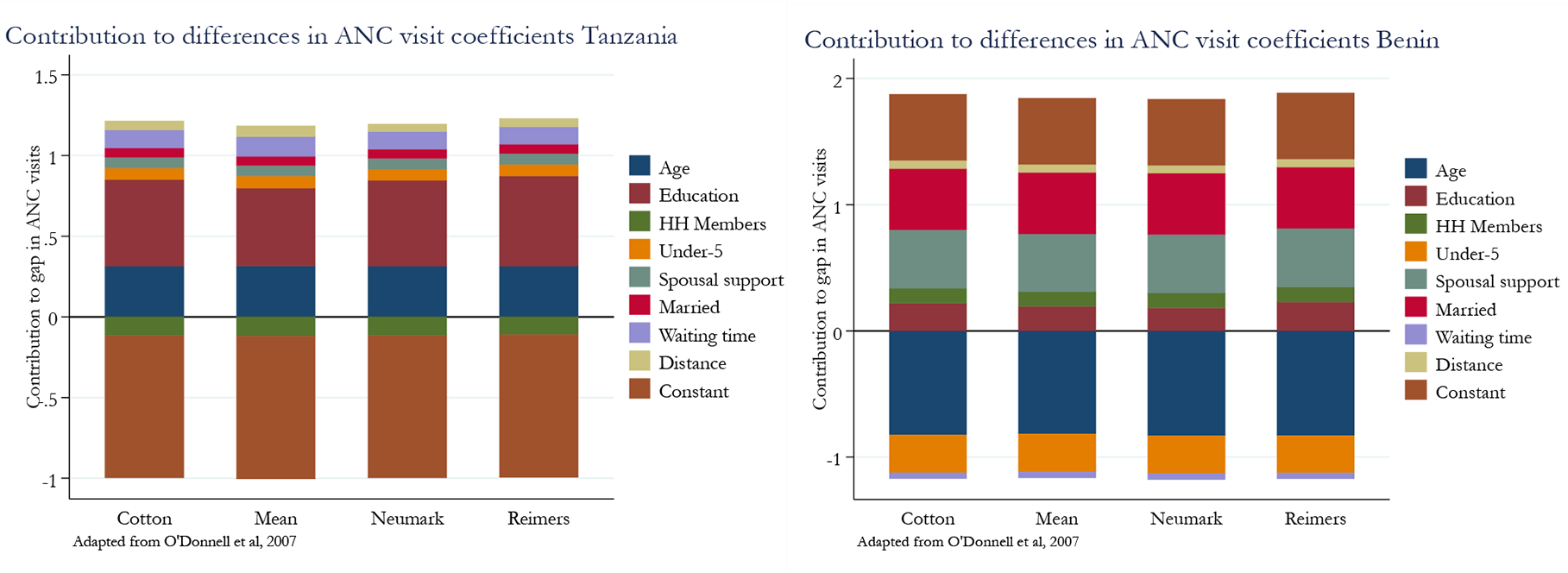
Inequality decomposition analyses for total ANC contacts: Benin and Tanzania. This figure shows the contribution of different variables to inequalities in ANC contacts using various decomposition methods—Cotton, Neumark and Reimers. ANC, antenatal care.
Subsidy analyses
The average concentration (Kakwani) index or pro-rich bias in subsidies is 0.046 (SE 0.006) in Atlantique and 0.018 (SE=0.003) in Geita, showing that government financing for ANC programmes is generally equitable. This suggests a pro-rich slant of 3.4% in Atlantique and 1.3% in Geita (online supplemental figure S3). In absolute financial terms, a targeted reallocation of ANC-specific financing of US$0.56 in Atlantique and US$0.20 in Geita towards the poorest quintiles will be needed to achieve equality.
In Atlantique, the lowest quintiles spend around 2.7% of their annual income as OOP expenditure on ANC and childbirth services, whereas the highest quintile spends only 0.8%. The corresponding figures in Geita are 3.1% and 0.5%, respectively (figure 4).
Figure 4.
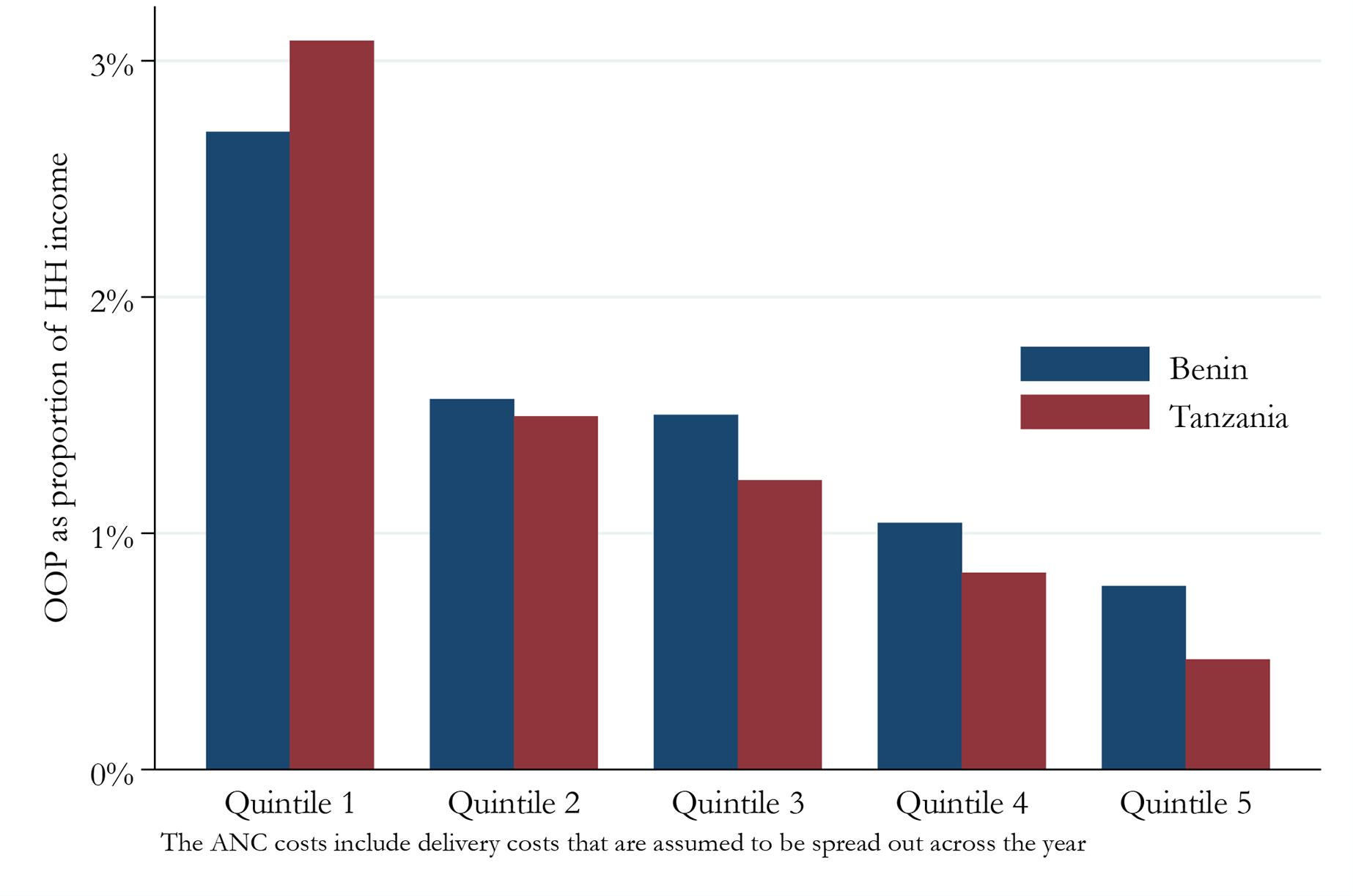
Out-of-pocket (OOP) costs for antenatal care as a proportion of simulated household annual income. While OOP costs as a proportion of total annual household income are relatively lower in the higher wealth categories in both countries, the lowest wealth group spends a disproportionate percentage of their annual household income on healthcare costs, particularly in Tanzania. In Benin, the lowest quintiles spend around 2.7% of their annual income as OOP expenditure on ANC and childbirth services, whereas the highest quintile spends only 0.8%. The corresponding figures in Tanzania are 3.1% and 0.5%, respectively. ANC, antenatal care.
DISCUSSION
This study assessed health equity in ANC and delivery outcomes in two relatively rural areas, Atlantique Department, Benin and Geita Region, Tanzania. In both sites, women of all SES levels were receiving fewer than the minimum recommended number of ANC visits, though wealthier, more educated individuals were more likely to achieve the recommended number, as has been previously described.33–35 In addition, we found gaps in the quality of ANC services received across all wealth and educational quintiles in both study areas, as has been described in Ghana.36 Inequalities appear worse in Atlantique, Benin when disaggregated by wealth and appear worse in Geita, Tanzania when education is used.33–35 In addition, we found gaps in the quality of ANC services received across all wealth and educational quintiles in both study areas, as has been described in Ghana.36 Inequalities appear worse in Atlantique, Benin when disaggregated by wealth and appear worse in Geita, Tanzania when education is used. The inequalities in ANC visits in Benin seem to be driven by non-health system factors such as maternal age, education and wealth.
ANC quality indicators were generally equitable in Atlantique, Benin, except for gestational age at first ANC visit. In Atlantique, once women enrol in ANC, they are likely to receive all recommended services, while this is not the case in Geita, where government policy is that ANC services are free. There were inequalities in most quality parameters in Geita except for blood tests; both facility and non-health system factors play a role in inequalities (online supplemental table S3). In Atlantique, facility-specific factors such as human resource constraints and commodity shortages had a negligible contribution on inequality as seen in the decomposition of the CI (online supplemental table S3—fixed effects). These facility effects were a major contributor to inequalities in Geita. We were not able to fully test for the reasons behind this. These facility effects were stable in facility-level analyses which suggests that these factors were unlikely to be solely driven by personnel training gaps. For example, BP monitoring was offered to all women in Atlantique while only partially offered in Geita. Similar patterns are seen for urinalysis, which is also a free service in Tanzania. Our decomposition analyses results mirror those we obtain in the descriptive analyses in both directionality and magnitude, increasing confidence in the estimates. While others have described rural–urban equity gaps in ANC coverage,37–39 we were unable to find any studies which explored whether these stemmed from underlying facility level differences or other confounding factors.
Our results are similar to those of other studies in the region that have found generally low quality of ANC services as measured against the WHO QoC indicators. A secondary data analysis by Raru et al using demographic and health survey (DHS) data from six East African countries found that only 11% of pregnant mothers had received the minimum package of care, with the main determinants of better care being maternal age, education, wealth and urban residence.40 Another study from Ethiopia, also using DHS data, found 23% of mothers had received the minimum package of ANC care but with similar determinants.41 In each country, it is important to identify and address the root causes underlying why some recommended services are not offered. For example, commodity shortages could be resolved by strengthening logistic management systems. Additionally, it may be helpful for policy-makers to emphasise the importance of providing the complete package of ANC services as outlined by national policies/WHO.
Initiation of ANC later in pregnancy is associated with adverse maternal and fetal outcomes including eclampsia, preterm birth and low birth weight.42 43 These outcomes, such as low birth weight, can have longer-term impacts on health and education attainment, perpetuating inequality. Our analysis found a downward SES trend in gestational age at first visit in both countries, with wealthier and more educated women more likely to initiate ANC earlier in pregnancy. This finding is similar to those found in other studies in Tanzania,44 Ethiopia45 and Nepal.46 Prior research has identified cultural factors, uncertainty about pregnancy and lack of knowledge about ANC as additional contributing factors to late ANC initiation,35 47 although we did not examine these in our analysis. Potential interventions to address barriers to early ANC initiation could include use of community health worker programmes and women’s groups to disseminate information about the importance of early ANC.
We found negligible differences in birth weights across wealth in both countries. Several factors may have contributed to this. Birth weights used in the analysis were those obtained routinely at the time of delivery by ministry of health staff. These are often rounded to the nearest 100 g, which can obscure small differences.48 49 In addition, birth weight is multifactorial and has a large SE, thus, large sample sizes are generally needed to detect an effect. Our study may not have been sufficiently powered to detect these differences.
There are operational inequalities in ANC care—waiting time—where on average wealthier/more educated clients spend less time at health facilities compared with those in the lowest rank in both categories (online supplemental tables S1 and S2). It is unclear if this is due to the ability of more educated/wealthier individuals to navigate the health system, or if this is due to some SES-based preferential treatment. While the relationship between SES and waiting time has been well studied in the context of elective procedures such as surgeries,50 51 we are not aware of any studies that have looked at this in ANC services. In the former, waiting times are seen as a non-monetary tool to harmonise the supply and demand for healthcare. There is some evidence of income, employment status and education gradients for waiting time in general primary care, which ANC can be seen as part of.52
We find that poor individuals in both countries pay a higher proportion of OOP payments as a proportion of their total annual income compared with the wealthiest. Transport costs are the main drivers of OOP in Geita, given the longer travel distances in the study area and the fact that most services are provided free of charge. In Atlantique, transport costs are negligible, and OOP payments are driven by cost of services. Strategies to mitigate the financial barriers to healthcare access need to be tailored to the specific contexts and cost drivers in each country.
The findings suggest that in Geita, it may be more fruitful to focus on improved access to mothers in distant villages through interventions such as conditional-cash transfers, outreach services in the short term and facility construction in the long term. In Benin, policy-makers could consider subsidising the cost of specific services, for example, ANC consultation fees, malaria in pregnancy prevention and facility childbirth costs. The government of Benin waived most Caesarean section costs since 2005. In our crude estimates, had this not been done, and given prevailing Caesarean section rates in the country, 5.3% of mothers would have faced catastrophic financial expenditure defined as spending more than 10% of annual income on healthcare.53 54 Targeted subsidies, such as employing distinct income thresholds (means-testing) to establish eligibility for government support, could be advantageous. However, means-testing often comes with significant administrative costs, encompassing tasks like eligibility assessment and compliance, which might outweigh the benefits they offer.55
Our results also show the importance of reporting both absolute and relative measures when testing for inequalities. The RIIs indicated statistically significant prowealthy or pro-educated bias across all parameters except for birth weights, while the SII results are more nuanced (online supplemental table S1).
Our financial results need to be viewed with caution. The analyses suggest that a targeted pro-poor investment of US$0.56 in Atlantique and US$0.20 in Geita is needed to close the government finance benefit inequality gap. In reality, women from all SES levels are failing to achieve the recommended level of ANC services in both countries. This suggests the need for extra investments in ANC in both countries.
Our study has several limitations. We assume that families save for giving birth in a health facility and as such costs are amortised across the year. This might be unrealistic, especially for low earners who face overall resource constraints and is unlikely for emergency caesarean sections which are difficult to plan for.56 Costs for childbirth among the poorest may cause temporary fiscal shocks that could lead to disposal of liquid assets or dissavings. These studies were conducted in specific regions of both countries and may not be nationally representative. The equity analyses were also conducted among a study population and could suffer from both sample selection issues as well as study-mediated improvements in ANC services. It is unclear if this population is representative of the entire pregnant population including those who access services in private facilities.
While we find minimal effect of distance from ANC in the analyses, this result should be viewed with caution as it could be a study design artefact. That is, ANC clients and their villages were linked to study facilities, in essence washing out the effects of distance. There were no differences in the main outcome variable, birth weight, across wealth or educational attainment in both countries. Birth weights were used as a primary outcome, but we were unable to test for other neonatal/postnatal outcomes. There were also no data on place of delivery or quality of delivery care. The OOP and subsidy results should also be viewed cautiously since we use simulated consumption income created from the wealth index which may not reflect actual incomes.23 Despite this limitation, the results are in the expected direction.
CONCLUSION
In both Atlantique, Benin and Geita, Tanzania, ANC clients are not receiving the recommended number of ANC visits. Inequalities in ANC attendance were identified in the study sites in both Tanzania and Benin, with a bias towards wealthier, more educated individuals. Specific barriers and proposed solutions are different in the two countries. This analysis highlights the need to continue to improve access to, and quality of, care for pregnant women by addressing specific financial and access barriers and solutions in each context.
Supplementary Material
WHAT IS ALREADY KNOWN ON THIS TOPIC
Despite well-documented existing inequalities in antenatal care (ANC) by socioeconomic status, few studies have assessed how different government health financing structures (user-fee exempt and non-exempt) impact ANC service inequalities.
WHAT THIS STUDY ADDS
We use different methods to describe and delineate drivers of inequalities in ANC services. We find that while inequalities are present across both financing mechanisms, the underlying drivers are different, with health system quality factors being the main determinants in the user-fee exempt system, while costs being the primary driver in the non-exempt one.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study highlights the underlying drivers of inequality in ANC programmes, to allow for tailored policy interventions.
Acknowledgements
We thank the field collectors and participants.
Funding
This study is made possible by the generous support of the American people, through the United States Agency for International Development (USAID) under the terms of Cooperative Agreements AID-621-A-16-00003 (Tanzania) and contract 7200AA18C00014 (Benin).
Footnotes
Competing interests None declared.
Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention or that of the United States Agency for International Development.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not applicable.
Ethics approval This study involves human participants and the ethics committees of the US Centers for Disease Control and Prevention (both country protocols, IRB numbers 7226 and 7254), National Institute for Medical Research in Tanzania (NIMR/HQ/R.8c/Vol.I/1621) and the Comité National pour l’Ethique pour la Recherche en Santé (National Ethics Committee for Research in Health, or CNERS; No 88/MS/DC/SGM/CNERS/ST) in Benin reviewed and approved these studies. Participants gave informed consent to participate in the study before taking part.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
► Additional supplemental material is published online only. To view, please visit the journal online (https://doi.org/10.1136/bmjph-2023-000547).
Data availability statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information. Data are available on reasonable request from the corresponding author.
REFERENCES
- 1.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience; 2016. [PubMed]
- 2.Arsenault C, Jordan K, Lee D, et al. Equity in antenatal care quality: an analysis of 91 national household surveys. Lancet Glob Health 2018;6:e1186–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orach CG. Health equity: challenges in low income countries. Afr Health Sci 2009;9 Suppl 2:S49–51. [PMC free article] [PubMed] [Google Scholar]
- 4.Idriss-Wheeler D, Yaya S. Exploring antenatal care utilization and intimate partner violence in benin - are lives at stake? BMC Public Health 2021;21:830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanou M, Kishida T, Kamiya Y. The effects of geographical accessibility to health facilities on antenatal care and delivery services utilization in Benin: a cross-sectional study. Reprod Health 2021;18:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atim C, Arthur E, Achala DM, et al. An assessment of domestic financing for reproductive, maternal, neonatal and child health in sub-Saharan Africa: potential gains and fiscal space. Appl Health Econ Health Policy 2020;18:789–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahinkorah BO, Ameyaw EK, Seidu AA, et al. Examining barriers to healthcare access and utilization of antenatal care services: evidence from demographic health surveys in sub-Saharan Africa. BMC Health Serv Res 2021;21:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dahab R, Sakellariou D. Barriers to accessing maternal care in low income countries in Africa: a systematic review. Int J Environ Res Public Health 2020;17:4292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health 2018;39:273–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chandola T, Clarke P, Morris JN, et al. Pathways between education and health: a causal modelling approach. Journal of the Royal Statistical Society Series A 2006;169:337–59. [Google Scholar]
- 11.d’Uva TB, Lindeboom M, O’Donnell O, et al. Education-related inequity in healthcare with heterogeneous reporting of health. J R Stat Soc Ser A Stat Soc 2011;174:639–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ 2010;29:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deaton A. The analysis of household surveys: a microeconometric approach to development policy. Washington, DC: World Bank, 2019. [Google Scholar]
- 14.Onwujekwe O, Hanson K, Fox-Rushby J. Some indicators of socio-economic status may not be reliable and use of indices with these data could worsen equity. Health Econ 2006;15:639–44. [DOI] [PubMed] [Google Scholar]
- 15.Sahn DE, Stifel D. Exploring alternative measures of welfare in the absence of expenditure data. Rev Income Wealth 2003;49:463–89. [Google Scholar]
- 16.Lindelow M. Sometimes more equal than others: how health inequalities depend on the choice of welfare indicator. Health Econ 2006;15:263–79. [DOI] [PubMed] [Google Scholar]
- 17.Howe LD, Galobardes B, Matijasevich A, et al. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol 2012;41:871–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Population and housing census. 2022. Available: https://www.nbs.go.tz/index.php/en/census-surveys/population-and-housing-census/802-matokeo-ya-mwanzo-ya-sensa-ya-watu-na-makazi-ya-mwaka-2022
- 19.Ministry of Health CD, Gender, Elderly and Children (MoHCDGEC) [Tanzania, Mainland] MoHMZ, National Bureau of Statistics (NBS), Office of the Chief, Government Statistician (OCGS) aI . Tanzania demographic and health survey and malaria indicator survey (TDHS-MIS) 2015–16. Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF; 2016. [Google Scholar]
- 20.Institut national de la Statistique et de L’Analyse Économique (INSAE) et ICF: Enquête Démographique et de Santé au Bénin, 2017–2018. Cotonou, Bénin et Rockville, Maryland, USA: INSAE et ICF; 2019. [Google Scholar]
- 21.Munsey A, Kinyina A, Assenga M, et al. Assessing the utility of pregnant women as a sentinel surveillance population for malaria in Geita, Tanzania, 2019 – 2021. Int J Infect Dis 2023;136:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Theequitytool. n.d. Available: https://www.equitytool.org/
- 23.Harttgen K, Vollmer S. Using an asset index to simulate household income. Econ Lett 2013;121:257–62. [Google Scholar]
- 24.Moreno-Betancur M, Latouche A, Menvielle G, et al. Relative index of inequality and slope index of inequality: a structured regression framework for estimation. Epidemiology 2015;26:518–27. [DOI] [PubMed] [Google Scholar]
- 25.Kakwani N, Wagstaff A, van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econom 1997;77:87–103. [Google Scholar]
- 26.Houweling TA, Kunst AE, Huisman M, et al. Using relative and absolute measures for monitoring health inequalities: experiences from cross-national analyses on maternal and child health. Int J Equity Health 2007;6:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Doorslaer E, Koolman X. Explaining the differences in income-related health inequalities across European countries. Health Econ 2004;13:609–28. [DOI] [PubMed] [Google Scholar]
- 28.Koolman X, van Doorslaer E. On the interpretation of a concentration index of inequality. Health Econ 2004;13:649–56. [DOI] [PubMed] [Google Scholar]
- 29.Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev 1973;14:693. [Google Scholar]
- 30.Owen OD, Eddy van D, Adam W. Decomposition of inequalities in health and health care. Edward Elgar Publishing: Chapters, 2006. [Google Scholar]
- 31.Eze P, Lawani LO, Agu UJ, et al. Factors associated with catastrophic health expenditure in sub-Saharan Africa: a systematic review. PLoS One 2022;17:e0276266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Institut national de la Statistique et de L’Analyse Économique (INSAE) et ICF International: Enquête Démographique et de Santé Du Bénin 2011–2012. Calverton, Maryland, USA: INSAE et ICF International; 2013. [Google Scholar]
- 33.Bobo FT, Asante A, Woldie M, et al. Evaluating equity across the continuum of care for maternal health services: analysis of national health surveys from 25 sub-Saharan African countries. Int J Equity Health 2023;22:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Selebano KM, Ataguba JE. Decomposing socio-economic inequalities in Antenatal care utilisation in 12 Southern African development Community countries. SSM Popul Health 2022;17:101004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. Uneke CJ: determinants of Antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ Open 2019;9:e031890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Afulani PA. Rural/urban and socioeconomic differentials in quality of Antenatal care in Ghana. PLoS One 2015;10:e0117996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zeng D, You W, Mills B, et al. A closer look at the rural-urban health disparities: insights from four major diseases in the commonwealth of Virginia. Soc Sci Med 2015;140:62–8. [DOI] [PubMed] [Google Scholar]
- 38.Van de Poel E, O’Donnell O, Van Doorslaer E. Are urban children really healthier? Evidence from 47 developing countries. Soc Sci Med 2007;65:1986–2003. [DOI] [PubMed] [Google Scholar]
- 39.Ellen van de P, Owen OD, Eddy Van D. What explains the rural-urban gap in infant mortality — household or community characteristics? Tinbergen Institute; 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raru TB, Mamo Ayana G, Bahiru N, et al. Quality of antenatal care and associated factors among pregnant women in East Africa using demographic and health surveys: a multilevel analysis. Womens Health (Lond) 2022;18:17455065221076731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Negash WD, Fetene SM, Shewarega ES, et al. Multilevel analysis of quality of antenatal care and associated factors among pregnant women in Ethiopia: a community based cross-sectional study. BMJ Open 2022;12:e063426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Izulla P, Muriuki A, Kiragu M, et al. Proximate and distant determinants of maternal and neonatal mortality in the postnatal period: a scoping review of data from low- and middle-income countries. PLoS One 2023;18:e0293479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nagatani S, Horiuchi S, Takahashi K, et al. Risk of low birthweight associated with the timing and frequency of antenatal care visits in Lao PDR: a retrospective cohort study. BMC Pregnancy Childbirth 2023;23:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gross K, Alba S, Glass TR, et al. Timing of antenatal care for adolescent and adult pregnant women in South-E astern Tanzania. BMC Pregnancy Childbirth 2012;12:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.kitaw TA, Haile RN. Time to first antenatal care booking and its determinants among pregnant women in Ethiopia: survival analysis of recent evidence from EDHS 2019. BMC Pregnancy Childbirth 2022;22:921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paudel YR, Jha T, Mehata S. Timing of first Antenatal care (ANC) and inequalities in early initiation of ANC in Nepal. Front Public Health 2017;5:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ochieng CA, Odhiambo AS. Barriers to formal health care seeking during pregnancy, childbirth and postnatal period: a qualitative study in Siaya county in rural Kenya. BMC Pregnancy Childbirth 2019;19:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Edouard L, Senthilselvan A. Observer error and birthweight: digit preference in recording. Public Health 1997;111:77–9. [DOI] [PubMed] [Google Scholar]
- 49.K’Oloo A, Godfrey E, Koivu AM, et al. Improving birth weight measurement and recording practices in Kenya and Tanzania: a prospective intervention study with historical controls. Popul Health Metr 2023;21:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baron JC, Kaura D. Perspectives on waiting times in an antenatal clinic: a case study in the Western Cape. Health SA 2021;26:1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Monstad K, Engesaeter LB, Espehaug B. Waiting time and socioeconomic status--an individual-level analysis. Health Econ 2014;23:446–61. [DOI] [PubMed] [Google Scholar]
- 52.García-Corchero JD, Jiménez-Rubio D. Waiting times in healthcare: equal treatment for equal need? Int J Equity Health 2022;21:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schantz C, Ravit M, Traoré AB, et al. Why are caesarean section rates so high in facilities in Mali and Benin. Sex Reprod Healthc 2018;16:10–4. [DOI] [PubMed] [Google Scholar]
- 54.Ravit M, Audibert M, Ridde V, et al. Do free caesarean section policies increase inequalities in Benin and Mali? Int J Equity Health 2018;17:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Umeh CA. Identifying the poor for premium exemption: a critical step towards universal health coverage in sub-Saharan Africa. Glob Health Res Policy 2017;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dossou J-P, Cresswell JA, Makoutodé P, et al. ‘Rowing against the current’: the policy process and effects of removing user fees for Caesarean sections in Benin. BMJ Glob Health 2018;3:e000537. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information. Data are available on reasonable request from the corresponding author.


