Abstract
Fragile X syndrome (FXS) is caused by epigenetic silencing of the X-linked fragile X messenger ribonucleoprotein 1 (FMR1) gene located on chromosome Xq27.3, which leads to the loss of its protein product, fragile X messenger ribonucleoprotein (FMRP). It is the most prevalent inherited form of intellectual disability and the highest single genetic cause of autism. Since the discovery of the genetic basis of FXS, extensive studies using animal models and human pluripotent stem cells have unveiled the functions of FMRP and mechanisms underlying FXS. However, clinical trials have not yielded successful treatment. Here we review what we have learned from commonly used models for FXS, potential limitations of these models, and recommendations for future steps.
Supplementary Information
The online version contains supplementary material available at 10.1186/s11689-024-09545-w.
Keywords: Fragile X syndrome, FMR1, Human, iPSCs, Stem cells, Neuron, Organoid, Mouse, Drosophila, FMRP
Background
Fragile X syndrome (FXS) is the most inherited form of intellectual disability and autism [1]. It is caused by epigenetic silencing of the X-linked fragile X messenger ribonucleoprotein 1 (FMR1) gene located on chromosome Xq27.3, which leads to the loss of its protein product, fragile X messenger ribonucleoprotein (FMRP) [2–4]. FXS has a higher penetrance in male than female patients, with a prevalence of 1 in 4000 males and 1 in 7000 females [5, 6]. The 5’ untranslated region (UTR) of the human FMR1 gene has polymorphic CGG trinucleotide repeats, with 30 repeats as the mode in the human population [7, 8]. The expansion of 55 to 200 repeats is associated with pathological conditions, including neurodegenerative disorder fragile X-associated tremor/ataxia syndrome (FXTAS) in males and fragile-X-associated primary ovarian insufficiency (FXPOI) in females [9]. The expansion of CGG repeats to over 200 leads to DNA methylation and silencing of the FMR1 gene, which is the main cause of FXS. However, there are also FXS patients who do not have a CGG repeat expansion but have rare FMR1 coding region mutations that lead to a loss of FMRP function [10].
FMRP is an RNA binding protein that can regulate gene expression through multiple mechanisms, such as protein translation, mRNA stability, RNA transport, and chromatin remodeling [11]. FMRP is widely expressed in many tissue and cell types with the highest expression mainly expressed in the brain and the testes [12]. FMRP is mainly expressed in the cytoplasm but contains a nuclear localization signal (NLS) and a nuclear exportation signal (NES) [13], which allows it to enter the nucleus to carry pre-messenger ribonucleoprotein complexes (pre-mRNP) back to the cytoplasm to interact with polyribosomes and regulate protein translation in neurons. FMRP also has two Tudor domains (TD1 and TD2) [14–16] involved in protein-protein interactions and DNA binding, and three KH domains (KH0, KH1, and KH2) and one RGG box for RNA-binding [7, 11, 17]. Since the discovery of FMR1 as the gene responsible for FXS, much effort has been devoted to identifying FMRP regulated mRNAs and molecular pathways as therapeutic avenues to treat FXS [18–21]. It is known that FMRP and its targets regulate important processes of neurodevelopment, such as synaptogenesis, neurogenesis, and cytoskeleton formation, which share significant overlap with pathways implicated in autism [11, 22].
FXS patients may exhibit a wide range of symptoms, with the most common being moderate to severe intellectual disability, language impairment, anxiety, hyperactivity, aggression, and increased seizure risk [1, 22]. They also have physical attributes such as elongated face, large ears, joint hypermobility, and macroorchidism [9]. Most patients have many behavioral symptoms that overlap with autism such as attention deficit disorder, repetitive behaviors, sleep problems, and sensory overload [9, 23]. To understand the pathophysiology of FXS, researchers have used genetic techniques to create animal models lacking FMRP expression. The most widely used models are the knockout mouse models (Fmr1-KO and Fmr1-floxed mice) and knockout drosophila models (dFmr1-KO drosophila). In the last decade there has also been increasing research performed in neurons or organoids derived from human pluripotent stem cells (hPSCs) including both human induced pluripotent stem cells (hiPSCs) and human embryonic stem cells (hESCs). Several recent review articles have provided detailed descriptions about these models [24–27]. Here, we will compare the strengths and weaknesses among the major models of FXS: the dFmr1-KO drosophila, Fmr1-KO rodent models, and human FXS stem cell models, and discuss how they complement each other to advance our understanding in FXS.
Review
Drosophila model of FXS
Drosophila melanogaster is one of the most useful model organisms in biology because its small genome and its rapid reproduction cycle allow for fast genetic manipulations to study many genetic disorders, including FXS [27]. The functional domains between human FMRP and Drosophila FMRP are highly conserved, with the KH1 and KH2 domains being 35% identical and 65% similar [27–29]. FMRP in Drosophila is highly localized to the brain and the eyes, especially in mushroom bodies which resemble the human hippocampus, important for learning and memory [26, 30, 31]. FMRP in drosophila has been shown to have important roles in synaptic plasticity [30, 31], regulation of calcium signaling [32, 33], apoptosis [34], phagocytosis [35], and regulation of circadian rhythm [36]. Like most models of FXS, the D.melanogaster FXS model was created by deleting the human FMR1 homolog, Fmr1 [31] and many cellular, molecular, and physiological deficits found in Fmr1-KO Drosophila overlap with those found in other animal models and the symptoms of FXS patients [26, 27, 37] (Table S1).
Behaviors of Drosophila FXS models
Many of the behavioral phenotypes found in the D.melanogaster FXS model have matched with that of FXS patients to some extent. For example, 23–46% of FXS patients have sleep disorders, with FXS patients typically sleeping less than the general population [38]. The Fmr1-KO Drosophila exhibit significant deficits in circadian rhythm [39, 40]. In addition, Fmr1-KO Drosophila also have increased sleeping time during both the day and night compared to its control counterparts. Subsequent studies have shown that FMRP may regulate circadian rhythm through a number of mechanisms including microRNA processing [41], expression of FMRP target collapsing response mediator protein (CRMP) [42], insulin signaling [43], and interaction of FMRP with protein Ataxin2 [44].
Other common behavioral problems among FXS patients include hyperactivity, repetitive behaviors, and deficits in learning and memory, which have also been found in autism patients [45]. The Drosophila FXS model has elevated persistent grooming behavior which resembles the hyperactivity and repetitive behaviors found in some FXS patients [46]. Fmr1-KO larva have hyperactive locomotion due to elevated bone morphogenetic protein type 2 receptor (BMPR2) pathway [47]. When assessing learning and memory in drosophila, several studies have used the courtship paradigm and classical conditioning method. During the courtship paradigm, male flies are trained by being put with an unreceptive female in which they should learn they will be rejected in any attempt to court in the future. The Drosophila FXS model demonstrated the ability to learn but they failed to recall what they have learned, indicative of memory deficits [39, 48]. A study looking into the climbing ability of the Drosophila FXS model found that, overall, they were poorer climbers compared to control, and their climbing ability significantly declined with age [49], similar to how their learning capability also declines with age. Likewise, it has been shown that FXS patients have a decrease in IQ scores with aging [50], suggesting that FMRP plays an important role in aging and not only neurodevelopment.
Molecular mechanisms of Drosophila FXS models
Studies using Drosophila have been the trail blazer to unveil mechanisms underlying FMRP function and FXS, and many of these findings are confirmed in mammalian models. For example, the first identified FMRP mRNA target is Futsch, a homolog of mammalian microtubule associated protein 1B (MAP1B), which has been confirmed in subsequent mouse [18, 20, 31] and human [19, 51] studies. In addition, reduced production of cyclic AMP levels were initially discovered in platelets [52] and lymphocytes [53] isolated from FXS individuals and later confirmed in brain tissue of both Fmr1-KO Drosophila and Fmr1-KO mice [54]. This has led to further research on targeting phosphodiesterase (PDE) as a treatment in Fmr1-KO mouse models [55, 56] and finally an ongoing clinical trial using a PDE-4D inhibitor for FXS [57].
Limitations of the Drosophila FXS Model
While Drosophila has served as an ideal model to identify mRNA targets for FMRP, the biochemical pathways identified in this model may not directly translate to humans, because of genetic differences among species. Drosophila Fmr1 has three homologs in mammals, FMR1, FXR1, and FXR2. Drosophila Fmr1 likely carries out the functions of both FMR1 and its autosomal two mammalian paralogs. In addition, similar to using other animal models, the behavioral phenotypes of Drosophila may not fully reflect cognitive deficits observed in FXS patients. Furthermore, there have been conflicting results in locomotor activities of Fmr1-KO Drosophila, with studies showing no significant change [39], reduced activity [40], or increased activity [58]. Despite these differences, some of the key phenotypes and pathways identified in Drosophila have been replicated in mammalian models of FXS and gone to clinical trials. Therefore, despite its limitations, Drosophila serves as an effective and efficient model to investigate many aspects of FXS.
Rodent models of FXS
The first model of FXS was the Fmr1-KO mouse model created by deletion of exon 5 [59]. The coding sequence of the mouse Fmr1 gene is 97% identical to that of the human FMR1 gene [60]. The mouse models for FXS, including an additional Fmr1-KO mouse line [61], a conditional knockout model (cKO) [61, 62], a point-mutant of FMRP RNA binding domain mouse model [63] and a conditional restoration (cON) line [61, 64], have been useful in studying the roles of FMRP in neurodevelopment and developing therapeutic targets. More recently, Fmr1-KO rat models have been generated [65, 66] which have the advantage of bigger size, better social behavioral measurement and higher genetic similarity to humans, compared to mouse models. Both mice and rat FXS models have striking similarity to FXS phenotypes and have served to confirm results identified in the Drosophila model as well.
Behaviors of rodent FXS models
FXS rodent models have been vital in our understanding of the role of FMRP in regulating behaviors and have led to significant progress in identifying treatment targets for clinical trials. Hyperactivity and repetitive behaviors are among the common clinical features of FXS patients [23]. Several studies have shown that FMRP deficient mice and rats exhibit these features, whereas other studies did not observe these phenotypes [24, 67, 68]. Seizures occur in a subset of young FXS patients with 10–20% of FXS patients reporting they have seizures in their teens and then this prevalence falls by the age of 20 [69]. Spontaneous seizures have not been reported in FXS mouse models; however, when audiogenic stimuli were used, juvenile Fmr1-KO mice had increased audiogenic seizures and defects in the acoustic startle response, similar to FXS patients [70]. In addition, both Fmr1-KO mouse and rat models exhibit increased resting state gamma oscillations and decreased alpha oscillations in their EEG recordings [71–73], similar to what has been shown in FXS patients [74]. Another prominent phenotype in FXS patients is anxiety. While studies have shown elevated anxiety-like behaviors in mouse [75] and rat models [71], other studies found that KO mice seem to be less anxious in an elevated plus maze test and more dominant in an automated tube test than wild-type mice [76]. Similar to the Drosophila FXS model, FXS rodent models also have impairments in spatial memory and spatial learning, reduced social interaction, increased grooming behavior, and aberrant circadian rhythm (Table S1). Limited studies have investigated sex-specific phenotypes in Fmr1-KO rodent models, with one study finding no sex differences in behaviors [77], while others showing some differences in behaviors and EEG recording between male and female Fmr1-KO rodents [71, 78]. Although FXS affects both males and females, female FXS patients are heterozygote for FMR1 gene mutation and exhibit significantly milder symptoms than male FXS patients. Therefore, most animal studies have used male models, which we focus on in this review.
Molecular mechanisms of rodent FXS models
The neurons in Fmr1-KO mice and rats have a higher density of dendritic spines and shorter long thin dendritic branches [79–82], consistent with those found in a limited number of human FXS postmortem brains [83, 84]. Many of the genetic pathways identified in FXS models support the conclusion that increased protein translation at the synapse impairs neuronal plasticity leading to behavioral deficits. These discoveries have led to several clinical trials [23, 85]. Among these discoveries is the mGluR theory, which suggests that FMRP regulates synaptic protein synthesis through metabotropic glutamate receptors (mGluR1 and mGluR5), muscarinic acetylcholine receptors, and Gq-linked receptors, leading to mTOR-dependent signaling pathways to increase protein synthesis [86]. Mouse and rat Fmr1-KO models exhibit increased production of synaptic proteins and high levels of AMPA receptor internalization leading to enhanced mGluR-dependent long-term depression (LTD) in the hippocampus [66, 87], impaired circuit formation, seizures, and behavioral deficits [82, 88]. In addition, several other signaling pathways identified in the Drosophila model have also been reported as dysregulated in Fmr1-KO mice, including mTOR, GSK3β, MMP9, PI3K, MAPK, and insulin pathways, which are all implicated in regulating protein translation at the synapses (reviewed by [1, 11, 23, 89]).
Limitations of rodent FXS models
A major limitation of rodent models is the significant differences between primate and rodent brains, particularly in the prefrontal cortex (PFC) where FMRP is highly expressed [90]. Primate PFC is significantly larger proportionally, much more complex compared to other species [91], and exhibits gene signatures unique to primates [92]. In addition, FXS animal models have Fmr1 gene deletion rather than epigenetic silencing of FMR1 as a result of CGG expansion observed in a majority of human FXS patients, therefore Fmr1-KO rodent models cannot fully model the genetic complexity in human FXS including CGG expansion and retraction, DNA demethylation or loss of CGG repeats leading to FMR1 gene reactivation, and somatic mosaicism [93, 94]. Several studies have attempted to model FXS CGG expansions and epigenetic silencing in mice but found that even with 300 human CGG repeats inserted into the 5’UTR of the mouse Fmr1, the CGG repeat containing mouse Fmr1 gene failed to undergo DNA methylation and gene silencing [93, 95, 96]. Therefore, the transcriptional silencing that occurs in humans has not been replicated in mice.
Fortunately, despite differences among human and animal models, rodent models of FXS have been able to replicate behavioral and cellular changes seen in FXS patients. Some contradicting behavioral results from rodent studies might be due to many factors, including differences in genetic background of mice and methods of analyses. It is important to note that the same strain of mice might have sub strains that are phenotypically different from one another such as the C57BL/6J versus C57BL/6JN mice [97]. Therefore, it is crucial to select and report the appropriate mouse strains when assessing behavioral phenotypes. Another major contributing factor to the variable results of behavioral assessment is the methods used for behavioral testing among different laboratories, which has been a hot topic in the field with the goal to enhance reproducibility [24]. Overall, mice are a great model to understand the function of FMRP and to assess potential treatments for FXS in an in vivo system.
Human stem cell models of FXS
hiPSC and isogenic hPSCs
HPSCs, including hiPSCs and hESCs, have become an important model for studying human brain development and neurodevelopmental disorders [11]. hiPSCs allow us to study molecular pathways in disease-relevant human cells derived from patients, facilitating drug screening for a more rapid transition of treatments to clinical trials. hPSCs and hPSC derived NPCs and 2-dimensional (2D) neurons have been used to develop new drug screens for FXS [98, 99]. Using FXS patient derived iPSCs, we can not only study human-specific pathways dysregulated in FXS patient cells, but also understand how FMR1 gene silencing induced epigenetic changes affect other cellular processes beyond FMRP deficiency.
Neuronal differentiation of FXS hPSCs
Several studies using FXS iPSCs, FXS hESCs, and isogenic FMR1 gene deleted (FMR1-KO) hPSCs have shown that FXS dorsal forebrain neural progenitor cells (NPCs) have increased proliferation but reduced neuronal differentiation [19, 100]. Raj et al. showed that FXS NPCs remain longer in the replication phase of the cell cycle, while control cells mainly stay outside of the cell cycle [100]. An early study shows that neurons differentiated from NPCs directly isolated from one 18-week gestation human postmortem FXS fetal tissue generated more TUJ1 + neurons (immature neurons) and these neurons had reduced neurite length compared to controls [101]. A study using FXS neurons also display reduced expression levels of TUJ1 [102], and FMRP deficient human neurons exhibit reduced complexity and shorter dendrites [51] and impaired axonal growth [103] compared to their controls. The results of these studies are similar to what has been found in Fmr1-KO animal models, supporting that FMRP plays an important role in neuronal maturation during neurodevelopment. Transcriptomic analysis using RNA sequencing and FMRP target identification using crosslinking immunoprecipitation followed by RNA sequencing (CLIP-seq) demonstrate that FXS and FMR1-KO NPCs have upregulation of genes involved in proliferation, but downregulation of genes related to neuronal differentiation, neuronal morphology, and synaptogenesis [19]. In addition, because hPSCs can be differentiated into different cell types, Li et al. were able to identify both unique and common FMRP targets in hPSC differentiated dorsal forebrain excitatory and ventral forebrain inhibitory NPCs and neurons, unveiling cell-type specific roles for FMRP [19]. Overall, a loss of FMRP leads to an aberrant cell cycle and dysfunction in neuronal maturation and differentiation in human neurons.
Electrical activity of human FXS neurons
A prominent phenotype found in hPSC derived FXS neurons is hyperexcitability [51, 104, 105]. Similar to EEG impairments and audiogenic seizures found in FXS animal models, the hyperexcitability of human FXS neurons might be a result of impaired neuronal maturation described above. On the other hand, deficits in calcium and sodium channels have been reported in human NPCs derived from FXS which can contribute to elevated neuronal activities [106]. It has been reported that human FXS neurons do not differ from control neurons in their mEPSC and/or mIPSC properties. However, FXS neurons fire more frequent and shorter action potentials [107]. Sodium channel blockers as well as calcium-activated potassium channel blockers have been used to rescue the elevated activities in human FXS neurons to control levels [106, 108]. Another study has discovered a decrease in GABAergic neurons in FXS organoids suggesting that excitatory/inhibitory imbalance may contribute to elevated activity, similar to what have been shown in mouse models [109–111]. Reactivation of FMR1 expression in human FXS neurons rescues the hyperexcitability deficits [104]. Our group has also shown that human and mouse FXS neurons have mitochondrial deficits and hyperexcitability, and enhancing mitochondrial functions can rescue hyperexcitability [105].
hiPSC derived 3D brain organoids
Cultured human neurons can only be maintained for up to 12 weeks, limiting their application in the study of human embryonic brain development spanning 40 weeks. 3-dimensional cortical organoids derived from iPSCs can be cultured for more than a year and resemble gene expression patterns similar to mid-fetal development [112–114] making them a promising tool for studying human brain development and neurodevelopmental disorders. Organoids enable the measurement of cortical layer formation, synapse maturation, neuron migration, and changes in electrical activities across multiple time-points corresponding to early human development. Therefore, a number of studies have used organoids to study neurodevelopmental disorders, including Timothy syndrome [115, 116], Rett syndrome [117, 118], Down syndrome [119], autism [120], and FXS [111, 121].
The first FXS organoid study found that NPCs in organoids derived from three FXS patient iPSC lines had increased proliferation compared to their healthy controls at 28 days post-differentiation, which confirmed the findings obtained from their own [100] and other 2D studies [19, 100]. A second study used organoids from iPSCs that were CRISPR/Cas9 gene edited to knockout FMRP (FMR1-KO) and found that FMR1 KO leads to overall bigger organoids from 50 to 100 days in culture which resembles the macrocephaly phenotype that has been reported in FXS patients [121]. They also observed more GFAP-expressing glial cells but did not observe significant changes in MAP2-positive neurons between FXS and control organoids [121]. However, the molecular mechanisms regulating these phenotypes were not investigated. The third study performed by Kang et al., 2021 did an in-depth analysis of FXS organoids and found deficits in cortical layer formation, synaptogenesis, electrical activity, and identified human-specific FMRP targets that can be pharmacologically manipulated to rescue these phenotypes [111]. However, they found that day 56 FXS organoids exhibited decreased proliferation along with an expanded cortical plate marked by layer 5 cortical marker CTIP2. It is possible that FXS cells have higher proliferation in early development and then rapidly transition to an accelerated neuronal differentiation near mid-fetal development, which must be confirmed. They also found that FXS organoids had an increase in synapse markers along with an increase in electrical activity. Their single-cell RNA sequencing (scRNA-seq) analysis of three pairs of FXS and control organoids show that FXS organoids were downregulated for genes important in neurogenesis, neuronal differentiation, morphogenesis, but were upregulated for protein translation and oxidative phosphorylation. However, they found that mGLuR5 inhibitors that typically rescue FXS phenotypes in mice did not rescue proliferation or synaptic activity in FXS organoids, but PI3K inhibitors did. This calls to the importance that FMRP might have species specific regulations and why human models should be used to confirm molecular pathways found in animal models for the identification of promising treatments.
Limitations of human stem cell models of FXS
The hPSC derived 2D or 3D models lack many of the cell-types and extracellular signals to guide the formation that reflect the brain anatomy found in vivo. Organoid models have emerged as a promising tool to study human brain development, however, standardized practices to ensure their rigor and reproducibility are still lacking and results from these models may be variable across laboratories [122]. In addition, limited studies using human post-mortem tissue indicate that cortical neurons in the FXS patients have higher density of immature spines [83, 84]. However, modeling spine development and maturation of human neurons are highly challenging due to the protracted developmental period of humans and limited maturation of human neurons in vitro. Furthermore, although functional assays can be performed in hPSC models, behavioral assays are not possible.
Comparison among FXS models
Mechanistic investigations of human diseases require the use of experimental models. As famously stated by the renowned statistician George Box “All models are wrong but some are useful” [123]. Each FXS model has contributed significantly to our understanding of the role of FMRP in development and mechanism underlying FXS. In this review, we mainly discussed the drosophila, rodent, and human models of FXS. However, there are also other powerful models, including the Fmr1-KO zebrafish model [124], the chicken ex ovo Fmr1 knockdown model [125], and the nonhuman primate ex vivo brain slice with FMR1 knockdown model [51, 105]. None of these experimental models are perfect, but they recapitulate certain aspects of FMRP functions and FXS pathogenesis. The similarities and complementary features among these experimental models are driving the field forward to a unified understanding of the mechanisms of FXS.
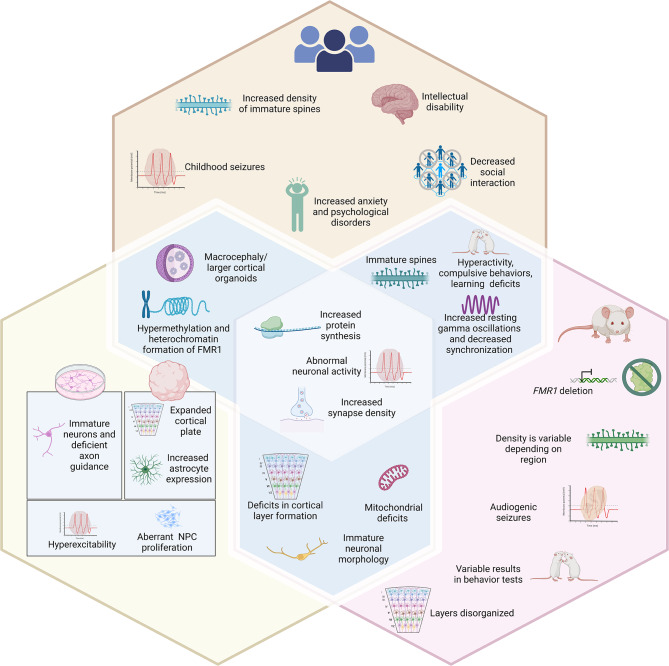
Some of the major similarities among all the models of FXS that are comparable to patient data include increased protein synthesis, impaired neuronal activities, abnormal neuronal morphology, and altered synapse density [23] (Fig. 1). The rodent and drosophila models have been imperative to understand how FMRP deficiency influences behavior. Despite some variabilities among reports published by different laboratories, overall, both models have demonstrated that FMRP-deficiency leads to increased locomotor activity, increased repetitive behaviors, decreased social interaction, aberrant circadian rhythm, and impaired learning ability that match to that of human patient data. Data across the rodent, drosophila models, and human stem cell in vitro models have shown a consistent impairment in dendritic branching and synaptogenesis of neurons, altered neuronal activity, and defective calcium signaling [89]. Further, elevated resting gamma oscillations have been found in rodent models of FXS which matches those observed in human FXS individuals. These convergent phenotypes among FXS models suggest that FMRP may evolutionarily play similar roles in neuronal development across different species.
Fig. 1.
Comparison of phenotypes of FXS patients to those observed in in vitro. FXS human stem cell models and mouse FXS models. The symptoms in FXS patients (top hexagon) range from mild to severe. Some characteristics of FXS in patients overlap with autistic features such as intellectual disability, increased anxiety, decreased social interaction, and seizures during a young age. In pursuit of understanding the biological pathways behind FXS symptomology, some of these phenotypes have been successfully replicated in human pluripotent stem cells (hPSC) in vitro (bottom left hexagon) and mouse models of FXS (bottom right hexagon). The shared phenotypes include increased protein synthesis, abnormal neuronal activity, and increased synapse density. There are also some features that are unique to each model. In hPSC in vitro models, a prominent phenotype includes hyperexcitability and disruptions in NPC proliferation in cortical neurons and organoids. While in mouse models audiogenic seizures, immature spines, and disorganization in cortical layer formation have been observed. A main advantage to using hPSC in vitro models is that these neurons can be derived from FXS patient iPSCs that contain the epigenetic silencing of FMR1 not found in mouse models allowing for more comprehensive biochemical analyses. However, in mouse models, behavior that can be correlated to FXS patients can be studied as has been done when assessing hyperactivity, compulsive behaviors, learning and memory deficits, as well as EEG properties. Overall, complementary model systems are needed to fully understand FXS. Please see Table S1 for a complete list and references. Figure created in BioRender.com.
A major advantage of using animal models is that these models allow us to investigate FMRP and FXS in vivo and in intact brains. For example, some of the phenotypes such as impairments in neuronal activities, dendritic morphology, and synaptogenesis have been found to be brain region-specific, suggesting that FMRP may have differential regulatory roles in different brain anatomical regions [23]. Although cell type-specific FMRP targets have been identified in hPSC differentiated dorsal forebrain excitatory neurons and ventral forebrain inhibitory neurons [19], the investigation of brain-region specific role of FMRP is significantly more difficult to perform in human in-vitro stem cell models. Recent advancement of different region-specific organoids may help in this regard. However, organoids are still relatively immature and do not have the complex neural network present in an in vivo model.
Despite their limitations, hPSC models provide a number of advantages for studying FXS, including that we can assess the human-specific role of FMRP at different stages of development and in specific cell types [105, 111]. Human PSC models also allow us to investigate the timing and mechanism of FMR1 gene silencing which cannot be modeled in animal models. Several recent advancements in the stem cell field will further enhance the use of human models in FXS. For example, dorsal forebrain and ventral subpallial assembloids can be used to study the E/I imbalance in FXS and compare in vivo data obtained from animal models and human EEG studies. However, only early fetal development can be effectively studied in human PSC models of FXS. Future development of bioengineering techniques for vascularized organoids and coculture techniques of organoids with glial cells can pave the way to understand the molecular mechanisms of FXS at late developmental time-points. Chimera models such as xeno-transplanted organoids in rodents may also be useful to understand how human FXS cells develop and function in an in-vivo environment.
Conclusion
The FXS field has benefited from having a wide variety of experimental models with both convergent and complementary features. Given the complexity of FXS and human developmental and psychiatric disorders in general, it is essential to validate the observations obtained from one model in at least another model. Therefore, a combination of animal and human models will further help understand the pathogenesis of FXS and improve the development of effective treatments.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table S1. Summary of phenotypes found in Fragile X Syndrome patients and the drosophila, mouse, and human in vitro models of Fragile X Syndrome
Acknowledgements
We thank the Zhao lab members for helpful discussion.
Abbreviations
- ACC
anterior cingulate cortex
- AMPA
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor
- cAMP
Cyclic adenosine monophosphate
- cKO
Conditional knockout
- cON
Conditional restoration
- CLIP-seq
Crosslinking with immunoprecipitation sequencing
- CTIP2
COUP-TF-interacting protein 2
- dFmr1
Drosophila Fmr1
- EEG
Electrocephalogram
- FMR1
Fragile X messenger ribonucleoprotein 1
- FMRP
Fragile X messenger ribonucleoprotein
- FXS
Fragile X syndrome
- FXTAS
Fragile X-associated tremor/ataxia syndrome
- FXPOI
Fragile-X-associated primary ovarian insufficiency
- GFAP
Glial fibrillary acidic protein
- GSK3β
Glycogen synthase kinase-3 beta
- hESCs
Human embryonic stem cells
- hPSCs
human pluripotent stem cells
- iPSCs
Induced pluripotent stem cells
- KH
K homology
- KO
Knockout
- LTP
Long-term potentiation
- MAP1B
Microtubule associated protein 1B
- pre-mRNP
Pre-messenger ribonucleoprotein
- sc-RNAseq
Single cell RNA sequencing
Author contributions
S.O.S. and X.Z. conceived the concept and wrote the manuscript. S.O.S, N.M.M-A, and Z.X created the table and figure.
Funding
This work was supported by grants from the National Institutes of Health (R01MH118827, R01MH116582, and R01MH136152 to X.Z., a diversity supplement to R01MH118827 and R36MH136790 for S.O.S.; P50HD105353 to the Waisman Center), DOD IIRA grant W81XWH-22-1-0621 (to X.Z), UW Kellett Mid-Career Award, Wisconsin Alumni Research Foundation, Jenni and Kyle Professorship, and Eagles Autism Foundation (to X.Z.), SciMed scholarships (to N.M.M-A and S.O.S.), T32 GM141013 Molecular Pharmacology training grant and predoctoral fellowship from the Wisconsin Stem Cell and Regeneration Medicine Center (to N.M.M-A), fellowship from Fragile X Research Foundation (FRAXA to Z.X.)
Data availability
Data and materials are available through contacting the corresponding author: Xinyu Zhao (xinyu.zhao@wisc.edu).
Declarations
Ethical approval and consent to participate
No human subject was used. All authors consented to participate in preparation of this manuscript.
Consent for publication
All authors have consented to publish this manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hagerman PJ, Hagerman R. Fragile X syndrome. Curr Biol. 2021;31(6):R273–5. doi: 10.1016/j.cub.2021.01.043. [DOI] [PubMed] [Google Scholar]
- 2.Pieretti M, Zhang FP, Fu YH, Warren ST, Oostra BA, Caskey CT, Nelson DL. Absence of expression of the FMR-1 gene in fragile X syndrome. Cell. 1991;66(4):817–22. doi: 10.1016/0092-8674(91)90125-I. [DOI] [PubMed] [Google Scholar]
- 3.Verkerk AJ, Pieretti M, Sutcliffe JS, Fu YH, Kuhl DP, Pizzuti A, et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell. 1991;65(5):905–14. doi: 10.1016/0092-8674(91)90397-H. [DOI] [PubMed] [Google Scholar]
- 4.Coffee B, Keith K, Albizua I, Malone T, Mowrey J, Sherman SL, Warren ST. Incidence of fragile X syndrome by newborn screening for methylated FMR1 DNA. Am J Hum Genet. 2009;85(4):503–14. doi: 10.1016/j.ajhg.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schaefer GB, Mendelsohn NJ, Professional P, Guidelines C. Clinical genetics evaluation in identifying the etiology of autism spectrum disorders. Genet Med. 2008;10(4):301–5. doi: 10.1097/GIM.0b013e31816b5cc9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hersh JH, Saul RA. Committee on G. Health supervision for children with fragile X syndrome. Pediatrics. 2011;127(5):994–1006. doi: 10.1542/peds.2010-3500. [DOI] [PubMed] [Google Scholar]
- 7.Mailick MR, Hong J, DaWalt LS, Greenberg JS, Movaghar A, Baker MW, et al. FMR1 low zone CGG repeats: phenotypic associations in the context of parenting stress. Front Pediatr. 2020;8:223. doi: 10.3389/fped.2020.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peprah E, Fragile X syndrome: the FMR1 CGG repeat distribution among world populations. Ann Hum Genet. 2012;76(2):178–91. doi: 10.1111/j.1469-1809.2011.00694.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajaratnam A, Shergill J, Salcedo-Arellano M, Saldarriaga W, Duan X, Hagerman R. Fragile X syndrome and fragile X-associated disorders. F1000Res. 2017;6:2112. doi: 10.12688/f1000research.11885.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sitzmann AF, Hagelstrom RT, Tassone F, Hagerman RJ, Butler MG. Rare FMR1 gene mutations causing fragile X syndrome: a review. Am J Med Genet A. 2018;176(1):11–8. doi: 10.1002/ajmg.a.38504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Richter JD, Zhao X. The molecular biology of FMRP: new insights into fragile X syndrome. Nat Rev Neurosci. 2021;22(4):209–22. doi: 10.1038/s41583-021-00432-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu B, Zhang Y, Zhan S, Wang X, Zhang H, Meng X, Ge W. Proteomic profiling of Brain and Testis reveals the diverse changes in ribosomal proteins in fmr1 knockout mice. Neuroscience. 2018;371:469–83. doi: 10.1016/j.neuroscience.2017.12.023. [DOI] [PubMed] [Google Scholar]
- 13.Eberhart DE, Malter HE, Feng Y, Warren ST. The fragile X mental retardation protein is a ribonucleoprotein containing both nuclear localization and nuclear export signals. Hum Mol Genet. 1996;5(8):1083–91. doi: 10.1093/hmg/5.8.1083. [DOI] [PubMed] [Google Scholar]
- 14.Myrick LK, Hashimoto H, Cheng X, Warren ST. Human FMRP contains an integral tandem Agenet (Tudor) and KH motif in the amino terminal domain. Hum Mol Genet. 2015;24(6):1733–40. doi: 10.1093/hmg/ddu586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adinolfi S, Ramos A, Martin SR, Dal Piaz F, Pucci P, Bardoni B, et al. The N-terminus of the fragile X mental retardation protein contains a novel domain involved in dimerization and RNA binding. Biochemistry. 2003;42(35):10437–44. doi: 10.1021/bi034909g. [DOI] [PubMed] [Google Scholar]
- 16.Ramos A, Hollingworth D, Adinolfi S, Castets M, Kelly G, Frenkiel TA, et al. The structure of the N-terminal domain of the fragile X mental retardation protein: a platform for protein-protein interaction. Structure. 2006;14(1):21–31. doi: 10.1016/j.str.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 17.Nelson DL, Orr HT, Warren ST. The unstable repeats–three evolving faces of neurological disease. Neuron. 2013;77(5):825–43. doi: 10.1016/j.neuron.2013.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Darnell JC, Van Driesche SJ, Zhang C, Hung KY, Mele A, Fraser CE, et al. FMRP stalls ribosomal translocation on mRNAs linked to synaptic function and autism. Cell. 2011;146(2):247–61. doi: 10.1016/j.cell.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li M, Shin J, Risgaard RD, Parries MJ, Wang J, Chasman D, et al. Identification of FMR1-regulated molecular networks in human neurodevelopment. Genome Res. 2020;30(3):361–74. doi: 10.1101/gr.251405.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maurin T, Lebrigand K, Castagnola S, Paquet A, Jarjat M, Popa A, et al. HITS-CLIP in various brain areas reveals new targets and new modalities of RNA binding by fragile X mental retardation protein. Nucleic Acids Res. 2018;46(12):6344–55. doi: 10.1093/nar/gky267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sawicka K, Hale CR, Park CY, Fak JJ, Gresack JE, Van Driesche SJ, et al. FMRP has a cell-type-specific role in CA1 pyramidal neurons to regulate autism-related transcripts and circadian memory. eLife. 2019;8:e46919. doi: 10.7554/eLife.46919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Niu M, Han Y, Dy ABC, Du J, Jin H, Qin J, et al. Autism symptoms in Fragile X Syndrome. J Child Neurol. 2017;32(10):903–9. doi: 10.1177/0883073817712875. [DOI] [PubMed] [Google Scholar]
- 23.Berry-Kravis E. Disease-targeted treatment translation in Fragile X Syndrome as a Model for Neurodevelopmental disorders. J Child Neurol. 2022:8830738221089740. [DOI] [PubMed]
- 24.Willemsen R, Kooy RF. Mouse models of fragile X-related disorders. Dis Model Mech. 2023;16(2). [DOI] [PMC free article] [PubMed]
- 25.Lee A, Xu J, Wen Z, Jin P. Across dimensions: developing 2D and 3D human iPSC-Based models of Fragile X Syndrome. Cells. 2022;11(11). [DOI] [PMC free article] [PubMed]
- 26.Drozd M, Bardoni B, Capovilla M. Modeling fragile X syndrome in Drosophila. Front Mol Neurosci. 2018;11:124. doi: 10.3389/fnmol.2018.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trajkovic J, Makevic V, Pesic M, Pavkovic-Lucic S, Milojevic S, Cvjetkovic S et al. Drosophila melanogaster as a model to study Fragile X-Associated disorders. Genes (Basel). 2022;14(1). [DOI] [PMC free article] [PubMed]
- 28.Coffee RL, Jr, Tessier CR, Woodruff EA, Broadie K. Fragile X mental retardation protein has a unique, evolutionarily conserved neuronal function not shared with FXR1P or FXR2P. Dis Model Mech. 2010;3(7–8):471–85. doi: 10.1242/dmm.004598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhogal B, Jongens TA. Fragile X syndrome and model organisms: identifying potential routes of therapeutic intervention. Dis Model Mech. 2010;3(11–12):693–700. doi: 10.1242/dmm.002006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pan L, Zhang YQ, Woodruff E, Broadie K. The Drosophila fragile X gene negatively regulates neuronal elaboration and synaptic differentiation. Curr Biol. 2004;14(20):1863–70. doi: 10.1016/j.cub.2004.09.085. [DOI] [PubMed] [Google Scholar]
- 31.Zhang YQ, Bailey AM, Matthies HJ, Renden RB, Smith MA, Speese SD, et al. Drosophila fragile X-related gene regulates the MAP1B homolog Futsch to control synaptic structure and function. Cell. 2001;107(5):591–603. doi: 10.1016/S0092-8674(01)00589-X. [DOI] [PubMed] [Google Scholar]
- 32.Doll CA, Broadie K. Neuron class-specific requirements for Fragile X Mental retardation protein in critical period development of calcium signaling in learning and memory circuitry. Neurobiol Dis. 2016;89:76–87. doi: 10.1016/j.nbd.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tessier CR, Broadie K. The fragile X mental retardation protein developmentally regulates the strength and fidelity of calcium signaling in Drosophila mushroom body neurons. Neurobiol Dis. 2011;41(1):147–59. doi: 10.1016/j.nbd.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu W, Jiang F, Bi X, Zhang YQ. Drosophila FMRP participates in the DNA damage response by regulating G2/M cell cycle checkpoint and apoptosis. Hum Mol Genet. 2012;21(21):4655–68. doi: 10.1093/hmg/dds307. [DOI] [PubMed] [Google Scholar]
- 35.O’Connor RM, Stone EF, Wayne CR, Marcinkevicius EV, Ulgherait M, Delventhal R, et al. A Drosophila model of Fragile X syndrome exhibits defects in phagocytosis by innate immune cells. J Cell Biol. 2017;216(3):595–605. doi: 10.1083/jcb.201607093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Specchia V, Puricella A, D’Attis S, Massari S, Giangrande A, Bozzetti MP. Drosophila melanogaster as a model to study the multiple phenotypes, related to Genome Stability of the Fragile-X syndrome. Front Genet. 2019;10:10. doi: 10.3389/fgene.2019.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Curnow E, Wang Y. New Animal models for understanding FMRP functions and FXS Pathology. Cells. 2022;11(10). [DOI] [PMC free article] [PubMed]
- 38.Budimirovic DB, Protic DD, Delahunty CM, Andrews HF, Choo TH, Xu Q, et al. Sleep problems in fragile X syndrome: cross-sectional analysis of a large clinic-based cohort. Am J Med Genet A. 2022;188(4):1029–39. doi: 10.1002/ajmg.a.62601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dockendorff TC, Su HS, McBride SM, Yang Z, Choi CH, Siwicki KK, et al. Drosophila lacking dfmr1 activity show defects in circadian output and fail to maintain courtship interest. Neuron. 2002;34(6):973–84. doi: 10.1016/S0896-6273(02)00724-9. [DOI] [PubMed] [Google Scholar]
- 40.Morales J, Hiesinger PR, Schroeder AJ, Kume K, Verstreken P, Jackson FR, et al. Drosophila fragile X protein, DFXR, regulates neuronal morphology and function in the brain. Neuron. 2002;34(6):961–72. doi: 10.1016/S0896-6273(02)00731-6. [DOI] [PubMed] [Google Scholar]
- 41.Xu S, Poidevin M, Han E, Bi J, Jin P. Circadian rhythm-dependent alterations of gene expression in Drosophila brain lacking fragile X mental retardation protein. PLoS ONE. 2012;7(5):e37937. doi: 10.1371/journal.pone.0037937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao J, Xue J, Zhu T, He H, Kang H, Jiang X, et al. Dysregulated CRMP mediates circadian deficits in a Drosophila Model of Fragile X Syndrome. Neurosci Bull. 2021;37(7):973–84. doi: 10.1007/s12264-021-00682-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monyak RE, Emerson D, Schoenfeld BP, Zheng X, Chambers DB, Rosenfelt C, et al. Insulin signaling misregulation underlies circadian and cognitive deficits in a Drosophila fragile X model. Mol Psychiatry. 2017;22(8):1140–8. doi: 10.1038/mp.2016.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu F, Kula-Eversole E, Iwanaszko M, Lim C, Allada R. Ataxin2 functions via CrebA to mediate huntingtin toxicity in circadian clock neurons. PLoS Genet. 2019;15(10):e1008356. doi: 10.1371/journal.pgen.1008356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaufmann WE, Kidd SA, Andrews HF, Budimirovic DB, Esler A, Haas-Givler B, et al. Autism spectrum disorder in Fragile X syndrome: cooccurring conditions and current treatment. Pediatrics. 2017;139(Suppl 3):S194–206. doi: 10.1542/peds.2016-1159F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tauber JM, Vanlandingham PA, Zhang B. Elevated levels of the vesicular monoamine transporter and a novel repetitive behavior in the Drosophila model of fragile X syndrome. PLoS ONE. 2011;6(11):e27100. doi: 10.1371/journal.pone.0027100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kashima R, Redmond PL, Ghatpande P, Roy S, Kornberg TB, Hanke T et al. Hyperactive locomotion in a Drosophila model is a functional readout for the synaptic abnormalities underlying fragile X syndrome. Sci Signal. 2017;10(477). [DOI] [PMC free article] [PubMed]
- 48.Choi CH, McBride SM, Schoenfeld BP, Liebelt DA, Ferreiro D, Ferrick NJ, et al. Age-dependent cognitive impairment in a Drosophila fragile X model and its pharmacological rescue. Biogerontology. 2010;11(3):347–62. doi: 10.1007/s10522-009-9259-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martinez VG, Javadi CS, Ngo E, Ngo L, Lagow RD, Zhang B. Age-related changes in climbing behavior and neural circuit physiology in Drosophila. Dev Neurobiol. 2007;67(6):778–91. doi: 10.1002/dneu.20388. [DOI] [PubMed] [Google Scholar]
- 50.Utari A, Adams E, Berry-Kravis E, Chavez A, Scaggs F, Ngotran L, et al. Aging in fragile X syndrome. J Neurodev Disord. 2010;2(2):70–6. doi: 10.1007/s11689-010-9047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guo Y, Shen M, Dong Q, Mendez-Albelo NM, Huang SX, Sirois CL, et al. Elevated levels of FMRP-target MAP1B impair human and mouse neuronal development and mouse social behaviors via autophagy pathway. Nat Commun. 2023;14(1):3801. doi: 10.1038/s41467-023-39337-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berry-Kravis E, Huttenlocher PR. Cyclic AMP metabolism in fragile X syndrome. Ann Neurol. 1992;31(1):22–6. doi: 10.1002/ana.410310105. [DOI] [PubMed] [Google Scholar]
- 53.Berry-Kravis E, Hicar M, Ciurlionis R. Reduced cyclic AMP production in fragile X syndrome: cytogenetic and molecular correlations. Pediatr Res. 1995;38(5):638–43. doi: 10.1203/00006450-199511000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Kelley DJ, Davidson RJ, Elliott JL, Lahvis GP, Yin JC, Bhattacharyya A. The cyclic AMP cascade is altered in the fragile X nervous system. PLoS ONE. 2007;2(9):e931. doi: 10.1371/journal.pone.0000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gurney ME, Cogram P, Deacon RM, Rex C, Tranfaglia M. Multiple behavior phenotypes of the Fragile-X Syndrome Mouse Model respond to Chronic Inhibition of Phosphodiesterase-4D (PDE4D) Sci Rep. 2017;7(1):14653. doi: 10.1038/s41598-017-15028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rosenheck M, Sheeler C, Sare RM, Gurney ME, Smith CB. Effects of chronic inhibition of phosphodiesterase-4D on behavior and regional rates of cerebral protein synthesis in a mouse model of fragile X syndrome. Neurobiol Dis. 2021;159:105485. doi: 10.1016/j.nbd.2021.105485. [DOI] [PubMed] [Google Scholar]
- 57.Berry-Kravis EM, Harnett MD, Reines SA, Reese MA, Ethridge LE, Outterson AH, et al. Inhibition of phosphodiesterase-4D in adults with fragile X syndrome: a randomized, placebo-controlled, phase 2 clinical trial. Nat Med. 2021;27(5):862–70. doi: 10.1038/s41591-021-01321-w. [DOI] [PubMed] [Google Scholar]
- 58.Bolduc FV, Valente D, Nguyen AT, Mitra PP, Tully T. An assay for social interaction in Drosophila fragile X mutants. Fly (Austin) 2010;4(3):216–25. doi: 10.4161/fly.4.3.12280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fmr1 knockout Mice: a model to study fragile X mental retardation. The dutch-belgian Fragile X Consortium. Cell. 1994;78(1):23–33. [PubMed] [Google Scholar]
- 60.Ashley CT, Sutcliffe JS, Kunst CB, Leiner HA, Eichler EE, Nelson DL, Warren ST. Human and murine FMR-1: alternative splicing and translational initiation downstream of the CGG-repeat. Nat Genet. 1993;4(3):244–51. doi: 10.1038/ng0793-244. [DOI] [PubMed] [Google Scholar]
- 61.Mientjes EJ, Nieuwenhuizen I, Kirkpatrick L, Zu T, Hoogeveen-Westerveld M, Severijnen L, et al. The generation of a conditional Fmr1 knock out mouse model to study Fmrp function in vivo. Neurobiol Dis. 2006;21(3):549–55. doi: 10.1016/j.nbd.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 62.Koekkoek SK, Yamaguchi K, Milojkovic BA, Dortland BR, Ruigrok TJ, Maex R, et al. Deletion of FMR1 in Purkinje cells enhances parallel fiber LTD, enlarges spines, and attenuates cerebellar eyelid conditioning in Fragile X syndrome. Neuron. 2005;47(3):339–52. doi: 10.1016/j.neuron.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 63.Zang JB, Nosyreva ED, Spencer CM, Volk LJ, Musunuru K, Zhong R, et al. A mouse model of the human fragile X syndrome I304N mutation. PLoS Genet. 2009;5(12):e1000758. doi: 10.1371/journal.pgen.1000758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Guo W, Allan AM, Zong R, Zhang L, Johnson EB, Schaller EG, et al. Ablation of Fmrp in adult neural stem cells disrupts hippocampus-dependent learning. Nat Med. 2011;17(5):559–65. doi: 10.1038/nm.2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hamilton SM, Green JR, Veeraragavan S, Yuva L, McCoy A, Wu Y, et al. Fmr1 and Nlgn3 knockout rats: novel tools for investigating autism spectrum disorders. Behav Neurosci. 2014;128(2):103–9. doi: 10.1037/a0035988. [DOI] [PubMed] [Google Scholar]
- 66.Tian Y, Yang C, Shang S, Cai Y, Deng X, Zhang J, et al. Loss of FMRP impaired hippocampal long-term plasticity and spatial learning in rats. Front Mol Neurosci. 2017;10:269. doi: 10.3389/fnmol.2017.00269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dahlhaus R. Of men and mice: modeling the Fragile X Syndrome. Front Mol Neurosci. 2018;11:41. doi: 10.3389/fnmol.2018.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.D’Elia A, Schiavi S, Manduca A, Rava A, Buzzelli V, Ascone F, et al. FMR1 deletion in rats induces hyperactivity with no changes in striatal dopamine transporter availability. Sci Rep. 2022;12(1):22535. doi: 10.1038/s41598-022-26986-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Berry-Kravis E, Filipink RA, Frye RE, Golla S, Morris SM, Andrews H, et al. Seizures in Fragile X Syndrome: associations and Longitudinal Analysis of a large clinic-based cohort. Front Pediatr. 2021;9:736255. doi: 10.3389/fped.2021.736255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Musumeci SA, Calabrese G, Bonaccorso CM, D’Antoni S, Brouwer JR, Bakker CE, et al. Audiogenic seizure susceptibility is reduced in fragile X knockout mice after introduction of FMR1 transgenes. Exp Neurol. 2007;203(1):233–40. doi: 10.1016/j.expneurol.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 71.Wong H, Hooper AWM, Niibori Y, Lee SJ, Hategan LA, Zhang L, et al. Sexually dimorphic patterns in electroencephalography power spectrum and autism-related behaviors in a rat model of fragile X syndrome. Neurobiol Dis. 2020;146:105118. doi: 10.1016/j.nbd.2020.105118. [DOI] [PubMed] [Google Scholar]
- 72.Kozono N, Okamura A, Honda S, Matsumoto M, Mihara T. Gamma power abnormalities in a Fmr1-targeted transgenic rat model of fragile X syndrome. Sci Rep. 2020;10(1):18799. doi: 10.1038/s41598-020-75893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lovelace JW, Ethell IM, Binder DK, Razak KA. Translation-relevant EEG phenotypes in a mouse model of Fragile X Syndrome. Neurobiol Dis. 2018;115:39–48. doi: 10.1016/j.nbd.2018.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang J, Ethridge LE, Mosconi MW, White SP, Binder DK, Pedapati EV, et al. A resting EEG study of neocortical hyperexcitability and altered functional connectivity in fragile X syndrome. J Neurodev Disord. 2017;9:11. doi: 10.1186/s11689-017-9191-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Spencer CM, Alekseyenko O, Serysheva E, Yuva-Paylor LA, Paylor R. Altered anxiety-related and social behaviors in the Fmr1 knockout mouse model of fragile X syndrome. Genes Brain Behav. 2005;4(7):420–30. doi: 10.1111/j.1601-183X.2005.00123.x. [DOI] [PubMed] [Google Scholar]
- 76.de Esch CE, van den Berg WE, Buijsen RA, Jaafar IA, Nieuwenhuizen-Bakker IM, Gasparini F, et al. Fragile X mice have robust mGluR5-dependent alterations of social behaviour in the automated tube test. Neurobiol Dis. 2015;75:31–9. doi: 10.1016/j.nbd.2014.12.021. [DOI] [PubMed] [Google Scholar]
- 77.Ding Q, Sethna F, Wang H. Behavioral analysis of male and female Fmr1 knockout mice on C57BL/6 background. Behav Brain Res. 2014;271:72–8. doi: 10.1016/j.bbr.2014.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ruggiero-Ruff RE, Villa PA, Hijleh SA, Avalos B, DiPatrizio NV, Haga-Yamanaka S, Coss D. Increased body weight in mice with fragile X messenger ribonucleoprotein 1 (Fmr1) gene mutation is associated with hypothalamic dysfunction. Sci Rep. 2023;13(1):12666. doi: 10.1038/s41598-023-39643-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Irwin SA, Idupulapati M, Gilbert ME, Harris JB, Chakravarti AB, Rogers EJ, et al. Dendritic spine and dendritic field characteristics of layer V pyramidal neurons in the visual cortex of fragile-X knockout mice. Am J Med Genet. 2002;111(2):140–6. doi: 10.1002/ajmg.10500. [DOI] [PubMed] [Google Scholar]
- 80.Speranza L, Filiz KD, Goebel S, Perrone-Capano C, Pulcrano S, Volpicelli F, Francesconi A. Combined DiI and antibody labeling reveals Complex Dysgenesis of hippocampal dendritic spines in a mouse model of Fragile X Syndrome. Biomedicines. 2022;10(11). [DOI] [PMC free article] [PubMed]
- 81.Wijetunge LS, Angibaud J, Frick A, Kind PC, Nagerl UV. Stimulated emission depletion (STED) microscopy reveals nanoscale defects in the developmental trajectory of dendritic spine morphogenesis in a mouse model of fragile X syndrome. J Neurosci. 2014;34(18):6405–12. doi: 10.1523/JNEUROSCI.5302-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Till SM, Asiminas A, Jackson AD, Katsanevaki D, Barnes SA, Osterweil EK, et al. Conserved hippocampal cellular pathophysiology but distinct behavioural deficits in a new rat model of FXS. Hum Mol Genet. 2015;24(21):5977–84. doi: 10.1093/hmg/ddv299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Irwin SA, Patel B, Idupulapati M, Harris JB, Crisostomo RA, Larsen BP, et al. Abnormal dendritic spine characteristics in the temporal and visual cortices of patients with fragile-X syndrome: a quantitative examination. Am J Med Genet. 2001;98(2):161–7. doi: 10.1002/1096-8628(20010115)98:2<161::AID-AJMG1025>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 84.Hinton VJ, Brown WT, Wisniewski K, Rudelli RD. Analysis of neocortex in three males with the fragile X syndrome. Am J Med Genet. 1991;41(3):289–94. doi: 10.1002/ajmg.1320410306. [DOI] [PubMed] [Google Scholar]
- 85.Gross C, Hoffmann A, Bassell GJ, Berry-Kravis EM. Therapeutic strategies in Fragile X Syndrome: from bench to Bedside and back. Neurotherapeutics. 2015;12(3):584–608. doi: 10.1007/s13311-015-0355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Huber KM, Gallagher SM, Warren ST, Bear MF. Altered synaptic plasticity in a mouse model of fragile X mental retardation. Proc Natl Acad Sci U S A. 2002;99(11):7746–50. doi: 10.1073/pnas.122205699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang J, Hou L, Klann E, Nelson DL. Altered hippocampal synaptic plasticity in the FMR1 gene family knockout mouse models. J Neurophysiol. 2009;101(5):2572–80. doi: 10.1152/jn.90558.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ntoulas G, Brakatselos C, Nakas G, Asprogerakas MZ, Delis F, Leontiadis LJ, et al. Multi-level profiling of the Fmr1 KO rat unveils altered behavioral traits along with aberrant glutamatergic function. Transl Psychiatry. 2024;14(1):104. doi: 10.1038/s41398-024-02815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Contractor A, Klyachko VA, Portera-Cailliau C. Altered neuronal and Circuit Excitability in Fragile X Syndrome. Neuron. 2015;87(4):699–715. doi: 10.1016/j.neuron.2015.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu Y, Sousa AMM, Gao T, Skarica M, Li M, Santpere G et al. Spatiotemporal transcriptomic divergence across human and macaque brain development. Science. 2018;362(6420). [DOI] [PMC free article] [PubMed]
- 91.Petrides M, Tomaiuolo F, Yeterian EH, Pandya DN. The prefrontal cortex: comparative architectonic organization in the human and the macaque monkey brains. Cortex. 2012;48(1):46–57. doi: 10.1016/j.cortex.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 92.Ma S, Skarica M, Li Q, Xu C, Risgaard RD, Tebbenkamp ATN, et al. Molecular and cellular evolution of the primate dorsolateral prefrontal cortex. Science. 2022;377(6614):eabo7257. doi: 10.1126/science.abo7257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brouwer JR, Mientjes EJ, Bakker CE, Nieuwenhuizen IM, Severijnen LA, Van der Linde HC, et al. Elevated Fmr1 mRNA levels and reduced protein expression in a mouse model with an unmethylated fragile X full mutation. Exp Cell Res. 2007;313(2):244–53. doi: 10.1016/j.yexcr.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhao X, Bhattacharyya A. Human models are needed for studying Human Neurodevelopmental disorders. Am J Hum Genet. 2018;103(6):829–57. doi: 10.1016/j.ajhg.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Colvin S, Lea N, Zhang Q, Wienisch M, Kaiser T, Aida T, Feng G. 341 repeats is not enough for methylation in a New Fragile X Mouse Model. eNeuro. 2022;9(5). [DOI] [PMC free article] [PubMed]
- 96.Bontekoe CJ, Bakker CE, Nieuwenhuizen IM, van der Linde H, Lans H, de Lange D, et al. Instability of a (CGG)98 repeat in the Fmr1 promoter. Hum Mol Genet. 2001;10(16):1693–9. doi: 10.1093/hmg/10.16.1693. [DOI] [PubMed] [Google Scholar]
- 97.Mekada K, Yoshiki A. Substrains matter in phenotyping of C57BL/6 mice. Exp Anim. 2021;70(2):145–60. doi: 10.1538/expanim.20-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hunt J, Li M, Zhao X, Bhattacharyya A. Using human neural progenitor cell models to Conduct large-Scale Drug Screens for Neurological and Psychiatric diseases. Methods Mol Biol. 2019;1942:79–88. doi: 10.1007/978-1-4939-9080-1_7. [DOI] [PubMed] [Google Scholar]
- 99.Hunt JFV, Li M, Risgaard R, Ananiev GE, Wildman S, Zhang F et al. High throughput small molecule screen for reactivation of FMR1 in Fragile X Syndrome Human neural cells. Cells. 2021;11(1). [DOI] [PMC free article] [PubMed]
- 100.Raj N, McEachin ZT, Harousseau W, Zhou Y, Zhang F, Merritt-Garza ME, et al. Cell-type-specific profiling of human cellular models of fragile X syndrome reveal PI3K-dependent defects in translation and neurogenesis. Cell Rep. 2021;35(2):108991. doi: 10.1016/j.celrep.2021.108991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Castren M, Tervonen T, Karkkainen V, Heinonen S, Castren E, Larsson K, et al. Altered differentiation of neural stem cells in fragile X syndrome. Proc Natl Acad Sci U S A. 2005;102(49):17834–9. doi: 10.1073/pnas.0508995102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sheridan SD, Theriault KM, Reis SA, Zhou F, Madison JM, Daheron L, et al. Epigenetic characterization of the FMR1 gene and aberrant neurodevelopment in human induced pluripotent stem cell models of fragile X syndrome. PLoS ONE. 2011;6(10):e26203. doi: 10.1371/journal.pone.0026203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Doers ME, Musser MT, Nichol R, Berndt ER, Baker M, Gomez TM, et al. iPSC-derived forebrain neurons from FXS individuals show defects in initial neurite outgrowth. Stem Cells Dev. 2014;23(15):1777–87. doi: 10.1089/scd.2014.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu XS, Wu H, Krzisch M, Wu X, Graef J, Muffat J, et al. Rescue of fragile X syndrome neurons by DNA methylation editing of the FMR1 gene. Cell. 2018;172(5):979–92. doi: 10.1016/j.cell.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shen M, Sirois CL, Guo Y, Li M, Dong Q, Mendez-Albelo NM et al. Species-specific FMRP regulation of RACK1 is critical for prenatal cortical development. Neuron. 2023. [DOI] [PMC free article] [PubMed]
- 106.Danesi C, Achuta VS, Corcoran P, Peteri UK, Turconi G, Matsui N, et al. Increased calcium influx through L-type calcium channels in human and mouse neural progenitors lacking Fragile X Mental retardation protein. Stem Cell Rep. 2018;11(6):1449–61. doi: 10.1016/j.stemcr.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang Z, Marro SG, Zhang Y, Arendt KL, Patzke C, Zhou B et al. The fragile X mutation impairs homeostatic plasticity in human neurons by blocking synaptic retinoic acid signaling. Sci Transl Med. 2018;10(452). [DOI] [PMC free article] [PubMed]
- 108.Das Sharma S, Pal R, Reddy BK, Selvaraj BT, Raj N, Samaga KK, et al. Cortical neurons derived from human pluripotent stem cells lacking FMRP display altered spontaneous firing patterns. Mol Autism. 2020;11(1):52. doi: 10.1186/s13229-020-00351-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Svalina MN, Guthman EM, Cea-Del Rio CA, Kushner JK, Baca SM, Restrepo D, Huntsman MM. Hyperexcitability and loss of Feedforward Inhibition Contribute to aberrant plasticity in the Fmr1KO amygdala. eNeuro. 2021;8(3). [DOI] [PMC free article] [PubMed]
- 110.Song YJ, Xing B, Barbour AJ, Zhou C, Jensen FE. Dysregulation of GABAA receptor-mediated neurotransmission during the auditory cortex critical period in the Fragile X Syndrome Mouse Model. Cereb Cortex. 2021;32(1):197–215. doi: 10.1093/cercor/bhab203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kang Y, Zhou Y, Li Y, Han Y, Xu J, Niu W, et al. A human forebrain organoid model of fragile X syndrome exhibits altered neurogenesis and highlights new treatment strategies. Nat Neurosci. 2021;24(10):1377–91. doi: 10.1038/s41593-021-00913-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Amiri A, Coppola G, Scuderi S, Wu F, Roychowdhury T, Liu F et al. Transcriptome and epigenome landscape of human cortical development modeled in organoids. Science. 2018;362(6420). [DOI] [PMC free article] [PubMed]
- 113.Gordon A, Yoon SJ, Tran SS, Makinson CD, Park JY, Andersen J, et al. Long-term maturation of human cortical organoids matches key early postnatal transitions. Nat Neurosci. 2021;24(3):331–42. doi: 10.1038/s41593-021-00802-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.He C, Kalafut NC, Sandoval SO, Risgaard R, Sirois CL, Yang C, et al. BOMA, a machine-learning framework for comparative gene expression analysis across brains and organoids. Cell Rep Methods. 2023;3(2):100409. doi: 10.1016/j.crmeth.2023.100409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Birey F, Andersen J, Makinson CD, Islam S, Wei W, Huber N, et al. Assembly of functionally integrated human forebrain spheroids. Nature. 2017;545(7652):54–9. doi: 10.1038/nature22330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Birey F, Li MY, Gordon A, Thete MV, Valencia AM, Revah O, et al. Dissecting the molecular basis of human interneuron migration in forebrain assembloids from Timothy syndrome. Cell Stem Cell. 2022;29(2):248–64. doi: 10.1016/j.stem.2021.11.011. [DOI] [PubMed] [Google Scholar]
- 117.Samarasinghe RA, Miranda OA, Buth JE, Mitchell S, Ferando I, Watanabe M, et al. Identification of neural oscillations and epileptiform changes in human brain organoids. Nat Neurosci. 2021;24(10):1488–500. doi: 10.1038/s41593-021-00906-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gomes AR, Fernandes TG, Vaz SH, Silva TP, Bekman EP, Xapelli S, et al. Modeling Rett Syndrome with Human patient-specific Forebrain Organoids. Front Cell Dev Biol. 2020;8:610427. doi: 10.3389/fcell.2020.610427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tang XY, Xu L, Wang J, Hong Y, Wang Y, Zhu Q et al. DSCAM/PAK1 pathway suppression reverses neurogenesis deficits in iPSC-derived cerebral organoids from patients with Down syndrome. J Clin Invest. 2021;131(12). [DOI] [PMC free article] [PubMed]
- 120.Chan WK, Griffiths R, Price DJ, Mason JO. Cerebral organoids as tools to identify the developmental roots of autism. Mol Autism. 2020;11(1):58. doi: 10.1186/s13229-020-00360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Brighi C, Salaris F, Soloperto A, Cordella F, Ghirga S, de Turris V, et al. Novel fragile X syndrome 2D and 3D brain models based on human isogenic FMRP-KO iPSCs. Cell Death Dis. 2021;12(5):498. doi: 10.1038/s41419-021-03776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang Z, Wang X, Park S, Song H, Ming GL. Development and application of Brain Region-Specific Organoids for investigating Psychiatric disorders. Biol Psychiatry. 2023;93(7):594–605. doi: 10.1016/j.biopsych.2022.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Box GEP. Science and statistics. J Am Stat Assoc. 1976;71(356):791–9. doi: 10.1080/01621459.1976.10480949. [DOI] [Google Scholar]
- 124.den Broeder MJ, van der Linde H, Brouwer JR, Oostra BA, Willemsen R, Ketting RF. Generation and characterization of FMR1 knockout zebrafish. PLoS ONE. 2009;4(11):e7910. doi: 10.1371/journal.pone.0007910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wang X, Zorio DAR, Schecterson L, Lu Y, Wang Y. Postsynaptic FMRP regulates synaptogenesis in Vivo in the developing cochlear nucleus. J Neurosci. 2018;38(29):6445–60. doi: 10.1523/JNEUROSCI.0665-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Summary of phenotypes found in Fragile X Syndrome patients and the drosophila, mouse, and human in vitro models of Fragile X Syndrome
Data Availability Statement
Data and materials are available through contacting the corresponding author: Xinyu Zhao (xinyu.zhao@wisc.edu).