Newspaper and television stories of catastrophic injuries occurring at the hands of clinicians spotlight the problem of medical error but provide little insight into its nature or magnitude.1 Clinicians, patients, and policymakers may underestimate the magnitude of risk and the extent of harm. We review the epidemiology of medical error, concentrating primarily on the prevalence and consequences of error, which types are most common, which clinicians make errors, and the risk factors that increase the likelihood of injury from error.
Summary points
The Harvard and Australian studies into medical error remain the only studies that provide population level data on the rates of injuries to patients in hospitals and they identified a substantial amount of medical error
In the United States medical error results in 44 000-98 000 unnecessary deaths each year and 1 000 000 excess injuries
Errors often occur when clinicians are inexperienced and new procedures are introduced
Extremes of age, complex care, urgent care, and a prolonged hospital stay are associated with more errors
Prevalence and consequences in hospitals
Benchmark studies
The Harvard study of medical practice is the benchmark for estimating the extent of medical injuries occurring in hospitals. Brennan et al reviewed the medical charts of 30 121 patients admitted to 51 acute care hospitals in New York state in 1984.2 They reported that adverse events—injuries caused by medical management that prolonged admission or produced disability at the time of discharge—occurred in 3.7% of admissions. A subsequent analysis of the same data found that 69% of injuries were caused by errors.3
In a study of the quality of Australian health care, a population based study modelled on the Harvard study, investigators reviewed the medical records of 14 179 admissions to 28 hospitals in New South Wales and South Australia in 1995.4 An adverse event occurred in 16.6% of admissions, resulting in permanent disability in 13.7% of patients and death in 4.9%; 51% of adverse events were considered to have been preventable. The number of preventable adverse events is important because both preventable and potential adverse events (or “near misses”) imply medical error. In contrast, non-preventable adverse events suggest that anticipated and unavoidable “complications” were present. In the Australian study the higher rate of adverse events was attributed in part to methodological differences between the two studies, but a real difference in the rate of injuries to patients in the two populations could not be excluded.
No study rivals the scope of the Harvard study and the Australian study except for a recent replication of the Harvard study in Colorado and Utah.5 Even so, the results probably represent an estimate of the lower boundary of the prevalence of medical injury and error. The Harvard investigators defined adverse events stringently, using disability and injury as prerequisites. This underestimates the error rate as many errors don't produce injury because they are caught in time, the patient is resilient, or because of good luck.
Beyond chart review
Aggressive case finding may identify injuries and errors that are not documented in a patient's chart.6 Using a computerised model to detect adverse drug events among patients at a hospital in Salt Lake City, Utah, Classen et al found that adverse drug events occurred in 1.7% of admissions.7 In comparison, using both chart review and prompted self reports from clinicians, Bates et al found that adverse drug events occurred among 6.5% of patients and potential adverse drug events occurred among 5.5% of patients admitted to two teaching hospitals in Boston.8 Of the adverse drug events 28% were due to errors, making the rate of serious medication errors (that is, preventable adverse drug events plus potential adverse drug events) 7.3%. Both of these studies reported rates that are much higher than the 0.7% rate of adverse drug events identified in the Harvard study's review of medical records.
Observational studies, although costly, have identified even higher rates of error and injury occurring during medical care. For example, observers on the general surgical units of a Chicago teaching hospital who recorded all “situations in which an inappropriate decision was made when, at the time, an appropriate alternative could have been chosen” found that 45.8% of patients experienced an adverse event.9 Eighteen per cent of these patients had a “serious” adverse event—that is, one that produced at least temporary disability.
Similarly, Donchin et al placed an observer at the patient's bedside to observe clinicians in the medical-surgical intensive care unit of a university hospital in Israel. Clinicians made 554 errors over four months, or 1.7 errors per patient per day.10
Patients injured as a result of a medical error spend longer in hospital and have higher hospital costs. At the hospital in Utah adverse drug events caused complications in 2.4% of admissions, cost an average of $2262 (£1414) per patient, and increased the length of stay by 1.9 days in comparison with data from matched controls.11 In the Harvard study of adverse drug events, the incremental cost associated with an event was $2595 and the length of stay was increased by 2.2 days. However, among preventable adverse drug events, the excess cost was $4685 and the length of stay was increased by 4.6 days.12 The cost of adverse drug events for a 700 bed teaching hospital was estimated to be $5.6m (£3.5m) a year.
Thus medical error is ubiquitous and the costs are substantial. In Australia medical error results in as many as 18 000 unnecessary deaths, and more than 50 000 patients become disabled each year. In the United States medical error results in at least 44 000 (and perhaps as many as 98 000) unnecessary deaths each year and 1 000 000 excess injuries.13
Prevalence and consequences among outpatients
Comparatively little is known about the prevalence of medical error outside hospitals. In both the Harvard study and the Australian study 8-9% of adverse events occurred in a doctor's office, 2-3% at home, and 1-2% in nursing homes. In the Australian study about a quarter of the adverse events occurring among outpatients caused permanent disability or death, and investigators judged it likely that more than two thirds could have been prevented. In other studies iatrogenic injury accounted for 5-36% of admissions to medical services14–16 and 11-13% of adult admissions to intensive care units at several university hospitals.17–19 Since these studies included only errors that were serious enough to require admission, these figures underestimate the extent of error associated with outpatient care.
Data on risk management also underestimate medical error occurring among outpatients because there is little association between malpractice claims and medical error.20 Asking clinicians and patients about errors provides information that is more useful. Burnum reported that in a series of 1000 consecutive patients seen in his three person internal medicine practice 42 adverse drug reactions occurred, of which 10 were preventable.21 More recently, Bhasale et al collected anonymous incident reports from Australian general practitioners of “an unintended event . . . that could have harmed or did harm a patient.”22 Of 805 incidents involving drug treatment, diagnosis, and equipment, 27% had the potential to cause severe harm and 76% were judged to have been preventable.
In the most rigorous outpatient study, Gandhi et al evaluated complications associated with medications among patients at 11 primary care sites in Boston.23 Of 2258 patients who had had drugs prescribed, 18% reported having had a drug related complication, such as gastrointestinal symptoms, sleep disturbance, or fatigue, in the previous year.
To calculate the cost of drug related morbidity and mortality among outpatients in the United States Johnson and Bootman asked pharmacists to estimate the probability of adverse outcomes occurring as a result of drug treatment.24 The costs associated with adverse outcomes were taken from statistical and research reports. The authors calculated that drug related problems accounted for 116 million extra visits to the doctor per year, 76 million additional prescriptions, 17 million emergency department visits, 8 million admissions to hospital, 3 million admissions to long term care facilities, and 199 000 additional deaths. The total cost was estimated to be $76.6bn, rivalling the aggregate cost of caring for patients with diabetes.
Types of medical error
In both the Harvard study and the Australian study about half of the adverse events occurring among inpatients resulted from surgery. Complications from drug treatment, therapeutic mishaps, and diagnostic errors were the most common non-operative events. In the Australian study cognitive errors, such as making an incorrect diagnosis or choosing the wrong medication, were more likely to have been preventable and more likely to result in permanent disability than technical errors.25
Adverse drug events have been investigated extensively because they are prevalent and preventable. In Bates et al's study of adverse drug events at two teaching hospitals in Boston, 1% of the events were fatal, 12% were life threatening, 30% were serious, and 57% were significant.8 Forty two per cent of the adverse events classed as life threatening or serious were preventable. Errors resulting in preventable adverse events occurred most often during ordering (56%) and administering (24%). Altogether, 245 of the near misses were the result of ordering errors and 40% were the result of errors in administering drugs. Adverse events were associated with the use of analgesics, antibiotics, sedatives, chemotherapeutic agents, cardiovascular drugs, and anticoagulants.8
Missed and delayed diagnoses may be difficult to detect retrospectively by chart review unless patients continue to use the same sources of care. In the Australian study errors of omission outnumbered errors of commission by 2 to 1. An error of omission is a failure of action such as a missed diagnosis, a delayed evaluation, or a failure to prescribe needed drug treatment. An error of commission is an incorrect action, such as administering the wrong drug to the wrong patient at the wrong time.
Necropsy studies can also uncover missed diagnoses and misdiagnoses. A study of 61 patients who died in a Spanish emergency department identified unexpected major findings, such as malignant tumours or haemorrhagic pancreatitis, in 44% of cases and important discrepancies between the necropsy report and the clinical diagnosis in 26%.26 In a retrospective study of 524 deaths occurring in 1990-1 at a Spanish tertiary care hospital, more than half of the risk of death was accounted for by adverse events that resulted from clinical care.27 The number of misdiagnoses and major unexpected findings at necropsy has remained essentially unchanged for over 40 years, prompting healthcare leaders to cite the falling rate of necropsy as an important impediment to ensuring the safety of patients.28
Clinicians who make errors
Despite rare examples of malevolent providers, there is little evidence that much medical error is due to “bad apples.”29 Although anaesthesiologists pioneered modern research into the safety of patients, no specialty is immune to error.30 Procedural mishaps are common in surgical specialties, perhaps because they are hard to disguise. Mistakes may be more common when the clinician is inexperienced and when new techniques are introduced.31 Misread radiographs and pathology specimens,32 laboratory errors,33 and mistakes made in administering radiation therapy also threaten the safety of patients.34
Trainees often err. Wu et al surveyed medical house officers in three training programmes in internal medicine about their most serious mistake.35 Altogether, 45% reported making at least one error, 31% of which resulted in a patient's death. Lesar et al found that more prescribing errors occurred among first year postgraduate residents than among other clinicians.36 Wilson et al found that more errors occurred in a paediatric intensive care unit when new doctors joined the rotation.37
Risk factors for injury
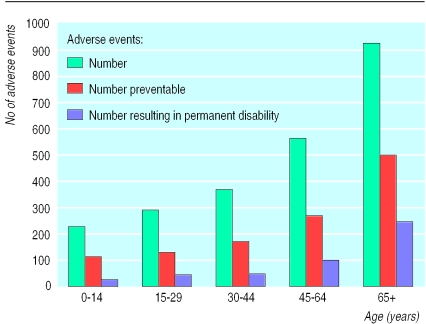
A potentially attractive strategy for preventing injury from medical error is to identify which patients are at an increased risk of harm. Patients aged over 64, for example, have a greater risk of serious injury from adverse events than younger patients.2,4,7,8 This may reflect their greater burden of comorbid illness and frailty (figure).
Certain interventions signal that there is a high risk, such as cardiothoracic surgery, vascular surgery, and neurosurgery. The severity of the patient's underlying illnesses as well as the inherent hazards of certain procedures may increase the likelihood of poor outcomes. Wilson et al found that a greater risk of death and a greater number of preventable adverse events were associated with patients with complex cases, illnesses requiring urgent care, and the use of interventions thought to be potentially life saving.4
Being cared for in the emergency department causes many preventable adverse events.2,4,38 Several factors are implicated: the use of part time doctors not trained in emergency care; fluctuating demand for services, which results in uneven and sometimes abbreviated care; the limited time available to arrive at a definitive diagnosis; and the fact that the emergency department is the point of entry for acutely ill patients.
The characteristics of individual patients may be less important than the duration of care in explaining injury. Andrews et al reported that the likelihood of an adverse event increased by 6% for each day spent in hospital.9 The intensity of care also affects the risk of injury. Among paediatric patients admitted to a British university hospital, drug errors were seven times more likely to occur in the intensive care unit than elsewhere.37 Similarly, the Harvard investigators looking at adverse drug events found that these events occurred more often among adult patients in medical intensive care units than in surgical intensive care units or general medical and surgical wards.39 However, when the number of doses dispensed in the different units was adjusted for, the differences were not significant. In a subsequent analysis of the study, no independent risk factors for preventable adverse events were identified after the length of stay before the event and the use of intensive care were controlled for.
Discussion
Although researchers regularly publish studies of medical error, adequate epidemiological information is limited to a few institutions, procedures, and specialties. Because most studies were conducted in academic referral centres the results may not be generalisable to community based hospitals and outpatient care facilities.
Comparing studies is difficult because research methods are not standardised. The lack of agreement about methods and the variable rigour of their application contribute to the variations found in error rates. There is a serious need for researchers to use consistent definitions and methods and for collaborative work on measuring error.
Systems for monitoring and reporting error could provide the platform from which more detailed studies of subpopulations could develop. However, expecting that individuals will carry out health care flawlessly creates an environment in which clinicians are reluctant to report their errors. Universal underreporting, in turn, undermines the ability to measure error accurately.
For these reasons the precise prevalence and magnitude of medical error is unknown, but it is probably enormous. We are aware of no study showing that medical care can be provided without error. In fact, the more closely we examine patient care, the more error we find. No setting is free from hazards and no specialty is immune, and patients are at risk no matter what their age, sex, or health status.
But the risk is not homogeneous. Patients who are sicker, subjected to multiple interventions, and who remain in hospital longer are more likely to suffer serious injury as a result of medical mistakes. Unless we make substantial changes in the organisation and delivery of health care, all patients—particularly the most vulnerable—will continue to bear the burden of medical error.
Figure.
Number of adverse events, preventable adverse events, and number resulting in permanent disability by age. Adapted from the quality in Australian healthcare study4
Footnotes
Competing interests: None declared.
References
- 1.Cook RI, Woods DD, Miller C. A tale of two stories: contrasting views of patient safety. Chicago, IL: National Patient Safety Foundation, AMA; 1998. [Google Scholar]
- 2.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, et al. Incidence of adverse events and negligence in hospitalized patients. N Engl J Med. 1991;324:370–376. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 3.Leape LL, Lawthers AG, Brennan TA, Johnson WG. Preventing medical injury. QRB Qual Rev Bull. 1993;19:144–149. doi: 10.1016/s0097-5990(16)30608-x. [DOI] [PubMed] [Google Scholar]
- 4.Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Med J Aust. 1995;163:458–471. doi: 10.5694/j.1326-5377.1995.tb124691.x. [DOI] [PubMed] [Google Scholar]
- 5.Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126:66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 6.O'Neil AC, Petersen LA, Cook F, Bates DW, Lee TH, Brennan TA, et al. Physician reporting compared with medical-record review to identify adverse medical events. Ann Intern Med. 1993;119:370–376. doi: 10.7326/0003-4819-119-5-199309010-00004. [DOI] [PubMed] [Google Scholar]
- 7.Classen DC, Pestotnik SL, Evans RS, Burke JP. Computerized surveillance of adverse drug events in hospitalized patients. JAMA. 1991;266:2847–2851. [PubMed] [Google Scholar]
- 8.Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 9.Andrews LB, Stocking C, Krizek T, Gottlieb L, Krizek C, Vargish T, et al. An alternative strategy for studying adverse events in medical care. Lancet. 1997;349:309–313. doi: 10.1016/S0140-6736(96)08268-2. [DOI] [PubMed] [Google Scholar]
- 10.Donchin Y, Gopher D, Olin M, Badihi Y, Biesky M, Sprung CL, et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23:294–300. doi: 10.1097/00003246-199502000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Classen DC, Pestotnik SL, Evans RS, Lloyd JF, Burke JP. Adverse drug events in hospitalized patients: excess length of stay, extra costs, and attributable mortality. JAMA. 1997;277:301–306. [PubMed] [Google Scholar]
- 12.Bates DW, Spell N, Cullen DJ, Burdick E, Laird N, Petersen LA, et al. The costs of adverse drug events in hospitalized patients. JAMA. 1997;277:307–311. [PubMed] [Google Scholar]
- 13.Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: building a safer health system. Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 14.Shimmel EM. The hazards of hospitalization. Ann Intern Med. 1964;60:100–101. doi: 10.7326/0003-4819-60-1-100. [DOI] [PubMed] [Google Scholar]
- 15.Steel KS, Gertman PM, Crescenzi C, Anderson J. Iatrogenic illness on a general medical service at a university hospital. N Engl J Med. 1981;304:638–642. doi: 10.1056/NEJM198103123041104. [DOI] [PubMed] [Google Scholar]
- 16.Lanshmanan MC, Hershey CO, Breslau D. Hospital admissions caused by iatrogenic disease. Arch Intern Med. 1986;146:1931–1934. [PubMed] [Google Scholar]
- 17.Trunet P, Le Gall JR, Lhoste F, Regnier B, Saillard Y, Carlet J, et al. The role of iatrogenic disease in admission to intensive care. JAMA. 1980;244:2617–2620. [PubMed] [Google Scholar]
- 18.Darchy B, Le Miere E, Figueredo B, Bavoux E, Domart Y. Iatrogenic diseases as a reason for admission to the intensive care unit: incidence, causes, and consequences. Arch Intern Med. 1999;159:71–78. doi: 10.1001/archinte.159.1.71. [DOI] [PubMed] [Google Scholar]
- 19.Stambouly JJ, McLaughlin LL, Mandel FS, Boxer RA. Complications of care in a pediatric intensive care unit: a prospective study. Intensive Care Med. 1996;22:1098–1104. doi: 10.1007/BF01699236. [DOI] [PubMed] [Google Scholar]
- 20.Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. N Engl J Med. 1996;335:1963–1967. doi: 10.1056/NEJM199612263352606. [DOI] [PubMed] [Google Scholar]
- 21.Burnum JF. Preventability of adverse drug reactions [letter] Ann Intern Med. 1976;85:80–81. doi: 10.7326/0003-4819-85-1-80. [DOI] [PubMed] [Google Scholar]
- 22.Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust. 1998;169:73–76. doi: 10.5694/j.1326-5377.1998.tb140186.x. [DOI] [PubMed] [Google Scholar]
- 23.Gandhi TK, Bates DW, Burstin HR, Puopolo AL, Cook EF, Haas JS, et al. Drug complications in outpatients. J Gen Intern Med (in press). [DOI] [PMC free article] [PubMed]
- 24.Johnson JA, Bootman JL. Drug-related morbidity and mortality and the economic impact of pharmaceutical care. Am J Health Syst Pharm. 1997;54:554–558. doi: 10.1093/ajhp/54.5.554. [DOI] [PubMed] [Google Scholar]
- 25.Wilson RM, Harrison BT, Gibberd RW, Hamilton JD. An analysis of the causes of adverse events from the quality in Australian health care study. Med J Aust. 1999;170:411–415. doi: 10.5694/j.1326-5377.1999.tb127814.x. [DOI] [PubMed] [Google Scholar]
- 26.Balaguer Martinez JV, Gabriel Botella F, Braso Aznar JV, Nunez Sanchez C, Catala Barcelo T, Labios Gomez M. El papel de la autopsia clinica en el control de calidad de los diagnosticos clinicos en una unidad de urgencias [The role of clinical autopsy in monitoring the quality of the clinical diagnosis in an emergency department] An Med Interna. 1998;15:179–182. [PubMed] [Google Scholar]
- 27.Garcia-Martin M, Lardelli-Claret P, Bueno-Cavanillas A, Luna-del-Castillo JD, Espigares-Garcia M, Galvez-Vargas R. Proportion of hospital deaths associated with adverse events. J Clin Epidemiol. 1997;50:1319–1326. doi: 10.1016/s0895-4356(97)00219-9. [DOI] [PubMed] [Google Scholar]
- 28.Lundberg GD. Low-tech autopsies in an era of high-tech medicine: continued value for quality assurance and patient safety. JAMA. 1998;280:1273–1274. doi: 10.1001/jama.280.14.1273. [DOI] [PubMed] [Google Scholar]
- 29.Leape LL. Error in medicine. JAMA. 1994;272:1851–1857. [PubMed] [Google Scholar]
- 30.Cooper JB, Newbower RS, Kitz RJ. An analysis of major errors and equipment failures in anesthesia management: considerations for prevention and detection. Anesthesiology. 1984;60:34–42. doi: 10.1097/00000542-198401000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Windsor JA, Pong J. Laparoscopic biliary injury: more than a learning curve problem. Aust N Z J Surg. 1998;68:186–189. doi: 10.1111/j.1445-2197.1998.tb04742.x. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell H, Medley G, Giles G. Cervical cancers diagnosed after negative results on cervical cytology: perspective in the 1980s. BMJ. 1990;300:1622–1626. doi: 10.1136/bmj.300.6740.1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Plebani M, Carraro P. Mistakes in a stat laboratory: types and frequency. Clin Chem. 1997;43:1348–1351. [PubMed] [Google Scholar]
- 34.Macklis RM, Meier T, Weinhous MS. Error rates in clinical radiotherapy. J Clin Oncol. 1998;16:551–556. doi: 10.1200/JCO.1998.16.2.551. [DOI] [PubMed] [Google Scholar]
- 35.Wu AW, Folkman S, McPhee SJ, Lo B. Do house officers learn from their mistakes? JAMA. 1991;265:2089–2094. [PubMed] [Google Scholar]
- 36.Lesar TS, Briceland LL, Delcoure K, Parmalee CJ, Masta-Gornic V, Pohl H. Medication prescribing errors in a teaching hospital. JAMA. 1990;263:2329–2334. [PubMed] [Google Scholar]
- 37.Wilson DG, McArtney RG, Newcombe RG, McArtney RJ, Gracie J, Kirk CR, et al. Medication errors in paediatric practice: insights from a continuous quality improvement approach. Eur J Pediatr. 1998;157:769–774. doi: 10.1007/s004310050932. [DOI] [PubMed] [Google Scholar]
- 38.Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. N Engl J Med. 1991;324:377–384. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- 39.Bates DW, Miller EB, Cullen DJ, Burdick L, Williams L, Laird N, et al. Patient risk factors for adverse drug events in hospitalised patients. Arch Intern Med. 1999;159:2553–2560. doi: 10.1001/archinte.159.21.2553. [DOI] [PubMed] [Google Scholar]