Abstract
Background
Transmission of wild poliovirus (WPV) has never been interrupted in Afghanistan, Pakistan, and Nigeria. Since 2003, infections with WPV of Nigerian origin have been detected in 25 polio-free countries. In 2012, the Nigerian government created an emergency operations center and implemented a national emergency action plan to eradicate polio. The 2013 revision of this plan prioritized (1) improving the quality of supplemental immunization activities (SIAs), (2) implementing strategies to reach underserved populations, (3) adopting special approaches in security-compromised areas, (4) improving outbreak response, (5) enhancing routine immunization and activities implemented between SIAs, and (6) strengthening surveillance. This report summarizes implementation of these activities during a period of unprecedented insecurity and violence, including the killing of health workers and the onset of a state of emergency in the northeast zone.
Methods
This report reviews management strategies, innovations, trends in case counts, vaccination and social mobilization activities, and surveillance and monitoring data to assess progress in polio eradication in Nigeria.
Results
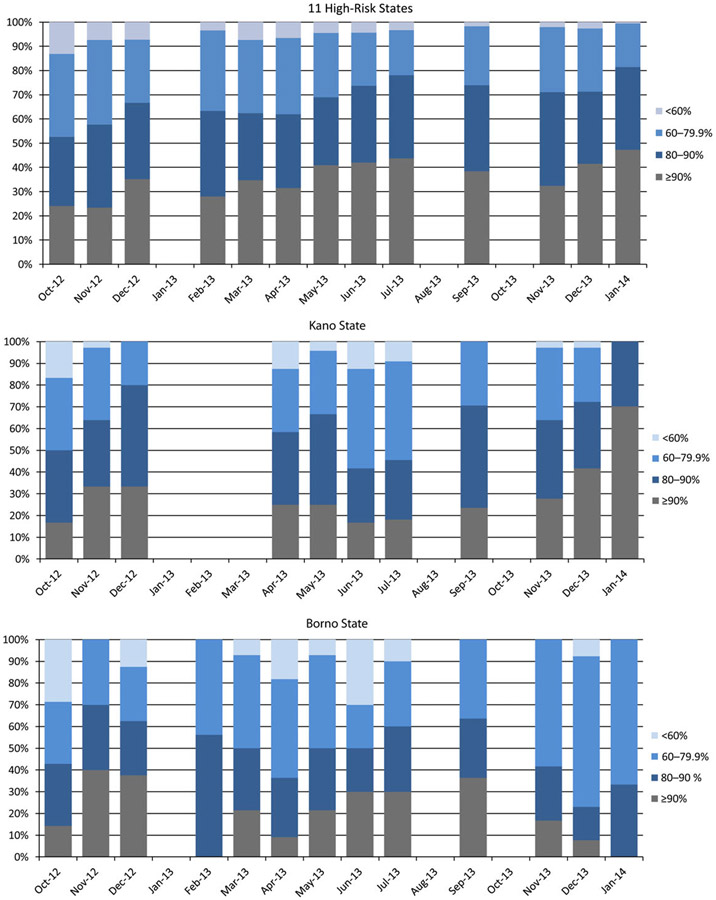
Nigeria has made significant improvements in the management of polio eradication initiative (pei) activities with marked improvement in the quality of SIAs, as measured by lot quality assurance sampling (LQAS). Comparing results from February 2012 with results from December 2013, the proportion of local government areas (LGAs) conducting LQAS in the 11 high-risk states at the ≥90% pass/fail threshold increased from 7% to 42%, and the proportion at the 80%–89% threshold increased from 9% to 30%. During January–December 2013, 53 polio cases were reported from 26 LGAs in 9 states in Nigeria, compared with 122 cases reported from 13 states in 2012 No cases of WPV type 3 infection have been reported since November 2012. In 2013, no polio cases due to any poliovirus type were detected in the northwest sanctuaries of Nigeria. In the second half of 2013, WPV transmission was restricted to Kano, Borno, Bauchi, and Taraba states. Despite considerable progress, 24 LGAs in 2012 and 7 LGAs in 2013 reported ≥2 cases, and WPV continued to circulate in 8 LGAs that had cases in 2012. Campaign activities were negatively impacted by insecurity and violence in Borno and Kano states.
Conclusions
Efforts to interrupt transmission remain impeded by poor SIA implementation in localized areas, anti–polio vaccine sentiment, and limited access to vaccinate children because of insecurity. Sustained improvement in SIA quality, surveillance, and outbreak response and special strategies in security-compromised areas are needed to interrupt WPV transmission in 2014.
Keywords: OPV, oral polio vaccine, poliovirus, Nigeria
Remarkable progress has been made toward polio eradication since 1988, when the World Health Assembly (WHA) launched the Global Polio Eradication Initiative (GPEI) [1-3]. Despite this progress, the WHA became concerned when member states did not achieve eradication and declared the completion of polio eradication a programmatic emergency for global public health in May 2012 [4]. Nigeria is one of 3 countries that have never interrupted wild poliovirus (WPV) transmission and has repeatedly served as a source for the reintroduction of WPV into polio-free countries [5]. States in the northern part of the country account for most WPV transmission and are the source of infection in the rest of Nigeria and neighboring countries. In response to ongoing WPV transmission, the Nigerian government changed the management of the polio program in 2012 by creating emergency operations centers (EOCs) at the national and state levels, redefining and instituting the government-led program, streamlining financial and programmatic reporting processes, adopting a data-driven risk algorithm to identify areas at highest risk of sustaining transmission, and implementing a national polio eradication emergency plan (NPEEP), as described previously [6]. In 2013, the NPEEP was revised and included several strategic priorities, including improving SIA quality, promoting accountability, implementing special strategies to reach underserved populations, adopting special approaches for security challenged areas, improving outbreak response, enhancing routine immunization and between-round activities, and enhancing surveillance.
Coupled with the revision in the NPEEP, the Government of Nigeria and GPEI partners have scaled up human, financial, and operational support for program activities and introduced numerous interventions to address long-standing problems. These problems include poor community education; a long legacy of conjecture about the safety of polio vaccine, leading to high levels of noncompliance; and anti–polio vaccine sentiment in many northern states [7-10]. Unfounded rumors and misinformation resulted in a political decision to suspend polio vaccination campaigns in Kano and Zamfara in 2003, resulting in large outbreaks across the north and globally. After these concerns were addressed, the state resumed vaccination activities, in 2004. However, the program in Kano, Zamfara, and several other northern states still experienced problems, including poor microplanning, residual mistrust of vaccination at the community level, surveillance gaps, lack of accountability and government support at all levels, and poor social mobilization, that were not addressed for several years. The national program began responding to these challenges more aggressively in 2009, with stronger political and programmatic oversight, increased accountability, mobilization of the country’s traditional leaders, and increased domestic funding for the national program. These changes set the stage for improved program management through the scaling up of staff, the use of innovative approaches to address constraints, and the application of an accountability framework at all levels in the program. This report reviews overall management of the pei activities in Nigeria and documents considerable progress in achieving polio eradication in the past 2 years.
METHODS
Review of Program Management and Vaccination Activities
This report summarizes changes in program management and reviews the scale and schedule of SIAs, including the type of vaccines used for each activity. The report also describes the use of innovations and the strengthening of communication activities to engage households and communities from 2012 through 2013.
Case Finding and Review of Surveillance Data
Polio case finding is conducted by active case searching for all patients meeting the WHO case definition of acute flaccid paralysis (AFP), using a standardized case investigation form, and the collection of stool samples for virus isolation and intratypic differentiation (ITD), using recommended laboratory procedures [11]. Isolates identified as WPV or vaccine-derived poliovirus (VDPV) are sent to the Centers for Disease Control and Prevention (CDC; Atlanta, GA) for virus characterization, genetic sequencing, and classification into genetic clusters. AFP case reports are entered into a database in Abuja and summarized weekly in reports to the EOCs and key stakeholders. Patients are classified as having confirmed WPV infection based on isolation of virus and ITD results. In this report, we reviewed AFP surveillance data at all levels and trends in WPV case counts, including age, sex, and geographic distribution of patients with confirmed paralytic polio.
Environmental Surveillance
Environmental surveillance is conducted in selected cities in Kano, Borno, Sokoto, the Federal Capital Territory (FCT), and Lagos. Sewage samples are collected in Kano, Kaduna, the FCT, Lagos, and Borno every 4–5 weeks and, in Sokoto, every 2 weeks. Samples are sent to the polio reference laboratory in Ibadan for processing as described previously [12]. Positive samples are sent to CDC for virus characterization. We reviewed environmental surveillance data, including trends in isolation of WPV and circulating VDPVs (cVDPVs) for 2012–2013.
Monitoring and Evaluation
SIA quality at the LGA level is assessed through independent monitoring and lot quality assurance sampling (LQAS) surveys. LQAS uses a 4-category pass/fail scheme based on the proportion of children with a finger mark indicating they received oral polio vaccine (OPV) during the SIA [13]. In each LGA, 6 settlements are randomly selected using probability proportional sampling methods from a master list of all settlements. In each settlement, 10 households are randomly selected, and 1 randomly selected child in each household is assessed. Results are classified as “passing” at the greater than 90% threshold if < 4 children are missed, in the 80 to 90% range if 4 to 8 children are missed, in the 60 to 79.9% range if 9 to 19 children are missed and < 60% if more than 19 children are missed. We reviewed all available LQAS data from October 2012 through January 2014.
RESULTS
Program Management
Improving program management and operational execution of SIAs has been a major focus of the program for the past 2 years. Critically linked to these efforts was extensive use of data for evidence-based decision making and a coordinated response by the government and partners to the evolving situation of polio in Nigeria. Much of the response (outlined below) includes the design and implementation of novel strategies/innovations to address evolving challenges (Table 1). The National Primary Health Care Development Agency (NPHCDA) is the primary government agency responsible for implementing program activities. Oversight of the program is provided by the Presidential Task Force on Polio Eradication (PTF). The PTF, chaired by the Minister of State for Health, includes representatives from the Governors Forum, the heads of technical partner agencies, the commissioners for health from high-priority states, representatives from religious groups, and traditional leaders. The engagement of the Governors Forum provides an opportunity for the executive governors and other officials to review progress in implementing agreed upon commitments and discuss implementation of strategies proposed by the national program. The traditional leaders are actively involved in the PTF and polio state task forces. In addition to their roles as task force members, the traditional authorities have an organization called the Northern Traditional Leaders Committee on Primary Health Care, established by the Sultan of Sokoto, that supports the establishment of polio committees at emirate and district levels. These committees coordinate the support of traditional leaders in the LGAs, wards, and settlements and are actively involved in microplanning, vaccination team selection, and SIA monitoring. They are particularly helpful in resolving noncompliance and engaging community support for polio and routine infant immunization services.
Table 1.
List of Key Activities and Innovations Used to Address Key Constraints Facing the Polio Program in Nigeria, 2012–2013
| Activity/Innovation | Issue Addressed | Application | Key Results |
|---|---|---|---|
| Dashboard | Lack of ownership and accountability at all levels in the program | Used to monitor preparedness and execution of SIAs | Real time monitoring of program activities with feedback to key officials at the state and LGA levels |
| EOC management structure | Lack of strategic direction and coordination among partners | Creation of EOCs at the national and state level (n = 5) | Better use of data for strategic decisions; improved communication among partners; coordinated response |
| Engagement of traditional and religious leaders | Lack of community support for polio vaccination activities; concerns about vaccine safety | Creation of committees at community level to support program activities; engagement of leaders in planning and monitoring of activities | Improved community acceptance and compliance |
| Use of LQAS to monitor campaign performance | Poor quality campaign performance | Monitor quality of campaign at the LGA level | Useful tool to monitor trends in quality of campaign; identification of high-risk LGAs |
| Outreach to underserved | Communities that are chronically missed during SIAs | Use of SOP for outreach to underserved communities | Identification and naming of missed settlements; improved surveillance in remote communities; vaccination of 0-dose communities |
| Volunteer community mobilizers | Noncompliance and lack of community support for polio vaccination | Recruitment of local female volunteers to support program activities in high-risk wards | Better community acceptance of routine infant immunization and polio vaccination during SIA |
| National Stop Transmission of Polio officers | Low coverage for routine infant immunization | Assignment of officers in 100 high-risk LGAs to support routine infant immunization | Applied training in routine infant immunization with focus on outreach to underserved communities |
| Doctors Against Polio | Noncompliance | Locally recruited medical providers to address community concerns during SIAs | Improved community acceptance; engagement of broader medical community to address concerns about vaccine safety |
| Polio survivor’s group | Noncompliance | Engagement of polio survivors to address noncompliance during SIAs | Improved community awareness of polio risk; reduction in noncompliance |
| Vaccinator tracking | Poor vaccinator team performance | GIS tracking of vaccinator teams with real-time feedback during SIAs | Better monitoring of team performance; improved accountability |
| Management support teams | Poor campaign planning and execution | Management team deployed by all partners to high-risk LGAs to support SIA planning and implementation. | Improved quality of SIAs |
| Health Camps | Unmet health needs in community | Establishment of health camps in high risk communities to provide additional primary health care services. | Greater acceptance of polio vaccine in high risk communities. |
Abbreviations: EOC, emergency operations center; GIS, geographic information system; LGA, local government authority; LQAS, lot quality assurance sampling; SIA, supplemental immunization activity; SOP, standard operating procedure.
The EOC serves as the operational arm of the NPHCDA and is responsible for providing strategic direction and managing all operational aspects of the program. It serves as a forum for ensuring effective and efficient coordination, information sharing, in-depth data analysis, planning, developing communication strategies, managing outbreak response, and monitoring operational activities. The EOC makes extensive use of data, including the distribution of dashboard data to monitor key indicators. The dashboard provides feedback to officials at the national, state, and LGA levels and is used to hold staff accountable for program performance. Data are also shared with external partners (the World Health Organization [WHO], CDC, and Global Good) to conduct in-depth risk analysis to identify high risk LGAs for prioritization of activities. To facilitate better coordination at the state level, the program established state-based EOCs in Kano, Borno, Kaduna, Sokoto, and Katsina, with additional EOCs to opening during 2014 in Yobe and Bauchi. The state EOCs provide a forum for all partners to coordinate work at the state level, to help states coordinate with the national program on strategic priorities and operational oversight of program activities.
Vaccination Activities
Increasing routine immunization (RI) coverage is a key polio eradication strategy. Monitoring RI coverage is challenging since population-based coverage surveys have consistently shown that administrative coverage data generally indicate higher coverage than that measured in surveys [14, 15]. Given these constraints in the interpretation of data, reported administrative vaccination data indicate that national coverage with 3 doses of trivalent OPV (OPV3) increased from 73% in 2012 to 84% in 2013. Data from children aged 6–35 months with non–polio-associated AFP also showed an increase in the proportion of patients with a history of ≥4 OPV doses nationwide, from 75% in 2012 to 87% in 2013. Efforts to increase RI coverage include intensified outreach in 17 LGAs with cVDPVs; a combined WHO–United Nations Children’s Fund program of RI intensification in an additional 39 LGAs; a state-wide effort between the Kano state government, the Dangote and Bill and Melinda Gates Foundations, and the CDC; and the assignment of National Stop Transmission of Polio officers to 100 high-risk LGAs to assist in building capacity for delivery of RI services [16]. In addition, partners such as the World Bank, the US Agency for International Development, European Union—Prime, and the Department for International Development have supported state-level efforts to improve routine immunization and primary healthcare service delivery in several northern states.
Seventeen SIAs were implemented during January 2012–December 2013, including 4 national rounds with trivalent (types 1–3) OPV, and 13 subnational rounds using bivalent (types 1 and 3) OPV in high-risk northern states. The program took advantage of all opportunities to provide OPV, including adding bivalent OPV (bOPV) to SIAs originally targeting measles and meningitis. Vaccination rounds in January and June 2013 were limited in scope, focusing on underserved areas, persistently poor-performing areas, and states with recent polio cases. Geographic information system (GIS)–based tracking of vaccination teams during SIAs is conducted in 9 of the highest-risk states to determine geographic coverage of vaccination teams and to identify settlements that were not visited. The tracking takes place each campaign in at least 40 high-risk LGAs and includes daily feedback and a missed settlement list on day 4, which is being used to guide mop-up activities. The tracking data are also available on the Web (available at: http://vts.eocng.org/) for examination by stakeholders, program managers, and other interested parties. The GIS-based maps developed for these states are also being used to support microplanning and to ensure all settlements are included in the SIA microplan.
Additional efforts to reach underserved communities included walk-through microplans, which identified >1000 settlements not included in the preexisting microplans, and special efforts to map all settlements in the northern states. These maps are used to update microplans on an ongoing basis. Special outreach efforts were also conducted to vaccinate nomadic, scattered, and border settlements during SIAs [17]. Many of these hard-to-reach settlements were consistently missed during previous campaigns. During these outreach activities, teams identified and geocoded approximately 6000 settlements that had never been reached by vaccination teams, including approximately 76 238 children who had never received polio vaccine. After enumeration, special efforts are made to ensure that these settlements are included in the ward-level microplans and that resources are provided to support outreach to these areas.
Several strategies are being used to improve program performance and address constraints in high-risk LGAs, as defined by SIA evaluation data, statistical modeling, and insecurity, including interagency management support teams deployed at the ward level, to assist in the supervision of SIAs; management and accountability officers, who monitor implementation of planned activities and funding expenditures and increase local accountability and transparency; and the use of health camps, to provide other health interventions along with attractive incentives for children and caregivers, such as candies, whistles, and bar soaps. Household-based walk-through microplanning including vaccination-team workload rationalization and validation has been completed in 15 states, 321 LGAs, and 36 621 team catchment areas. The program has also had 2 rounds of border vaccinations with Benin, Niger, and Cameroon to build a so-called firewall against importations.
The program lost momentum in February 2013, when 13 health workers were killed in separate attacks in Borno and Kano, resulting in suspension of an SIA and cancellation of the follow-up SIA in Borno and Kano during the March round in 2013. Security incidents also had a negative impact on planned SIAs in selected LGAs in Yobe and Borno throughout 2012 and 2013. Borno participated widely in only 3 of 8 scheduled SIAs in 2013; even when Borno was included, not all LGAs took part, and the SIAs were of poor quality, as indicated by findings of a postcampaign LQAS. To address anti–polio vaccination sentiment and the threat of violence, social and community mobilization activities provide opportunities for community leaders to engage and become advocates for the protection of children. These leaders also guide security risk assessments, which categorize risk into high, medium, and low. The outcome is to ensure there are minimal threats to polio workers before each SIA.
Social Mobilization and Advocacy
The program made a significant shift to a community-based approach for social mobilization and implemented diverse strategies to address problems with noncompliance and concerns about vaccine safety in selected communities in the past 2 years. Before the killing of health workers in Borno and Kano, a locally produced video was widely circulated that expressed concern about polio vaccine safety and efficacy, leading to considerable anti–polio vaccine sentiment in selected communities. To address these concerns, the program intensified community and household engagement, with particular emphasis on traditional and religious leaders, to provide advocacy and pro–polio vaccine messages. The program also produced a CD advocating for the benefits of polio vaccination that was distributed to households, media outlets, viewing centers and shared through Bluetooth. Religious focal persons were deployed in high-risk LGAs to map and coordinate the systematic engagement of religious leaders at the local level, to assist with gaining community support in community meetings and facilitate the vaccination of children attending Islamic schools.
In selected areas, the program has also enlisted the support of local physicians (Doctors Against Polio) during SIAs, given that they are respected in their communities. Given the low risk perception of polio within communities, the Polio Survivors Group was engaged to enlist community support for the program and assist with resolving noncompliance during and in between SIAs. As part of efforts to enhance community demand and address unmet health needs, the program is conducting health camps during SIAs in communities with high levels of noncompliance. These camps are staffed by local physicians, who provide treatment for common ailments in the community and provide polio and routine immunizations for children <5 years of age. The program has also ensured integration of bOPV with other health interventions, including outreach therapeutic feeding to treat malnutrition.
Other innovations include the realignment of the volunteer community mobilizer networks (VCMs) to include tracking and vaccinating newborns and 0-dose (ie, unvaccinated) children and referral to health facilities for routine immunization. VCMs are assigned to monitor approximately 200 households each and to ensure that all children in these households receive routine infant immunizations, as well as polio vaccine during SIAs. More than 10 000 0-dose children are routinely immunized by the VCMs on a monthly basis and referred to health facilities for routine immunization. VCMs also support community-based surveillance activities, including AFP surveillance, and house-to-house mobilization activities between polio SIAs. During these visits, they monitor households to ensure that newborns are vaccinated. During 2012–2013, 8500 VCMs were recruited to work in 152 LGAs in 10 states. There are plans to increase the number of VCMs in Borno and Yobe in the coming months. Intensified household and community engagement approaches in the high-risk LGAs have led to a >60% reduction in the percentage of children missed because of noncompliance.
Monitoring and Evaluation
SIA quality at the LGA level is assessed through LQAS, using a 4-category pass/fail scheme based on the proportion of children with a finger mark (indicating they received OPV during the SIA). During February 2012–December 2013, the number of LGAs conducting LQAS among the 11 high-risk states increased from 87 to 195. During February 2012–December 2013, in the 11 high-risk states, the proportion of LGAs achieving LQAS results at the ≥90% threshold increased from 7% to 42%, and the proportion at the 80%–89% threshold increased from 9% to 30%. The proportion of LGAs at the 60%–79% threshold decreased from 43% to 26%, and the proportion at the <60% threshold declined from 40% to 3% (Figure 1). Of note, some LGAs in Borno did not conduct any SIAs during this period because of insecurity. In addition, during October 2012–February 2013, when SIAs were held, less overall improvement was noted in these states, suggesting that insecurity negatively impacted quality. This also was noted in Kano, where LQAS results decreased for several SIAs after February 2013, when polio workers were attacked (Figure 1). However, with increased commitment of the governor, deputy governor, health commissioner, LGA chairmen, and Kano EOC, there was progressive improvement in SIA quality in LGAs with persistently poor performance, with 72% passing the 80% threshold in the December 2013 SIA.
Figure 1.
Trends in results of lot quality assurance sampling in high-risk states, Kano, and Borno, October 2012–January 2014.
Following every SIA campaign, the national EOC reviews the quality of the campaign by using precampaign and intracampaign dashboards, LQAS, and independent monitoring data. During this process, poorly performing LGAs are identified and invited to participate in planning workshops before the next immunization plus day. During these workshops, teams review lessons learned and revise their high-risk operational plans. Participants receive training about innovative strategies, prioritizing activities, and the best practices to improve quality, as learned from other areas. At the end of these sessions, monitoring and accountability officers follow up on the agreed plans of action and report to the national program, where there are challenges or issues associated with accountability. Other innovations include changes in vaccination team composition (ie, from a 6-person team to a 3-person team), better team workload rationalization, concurrent monitoring, improved microplanning, and enhanced team selection process.
Poliovirus Surveillance
The government of Nigeria conducts active surveillance for patients with AFP in a network of sentinel hospitals and clinics in all 36 states and the Federal Capitol Territory. A non–polio-associated AFP rate of ≥2 cases per 100 000 among children aged <15 years and collection of adequate stool specimens in ≥80% of AFP cases are key performance indicators for AFP surveillance. In 2013, the non–polio-associated AFP rate was 8.8 cases per 100 000, and 86.5% of AFP cases had adequate stool specimens collected, although values of these indicators decreased slightly from 2012. The proportion of high-risk states that met both indicators increased from 82% in 2012 to 91% in 2013. Within these states, the proportion of LGAs meeting both requirements increased from 67% in 2012 to 75% in 2013.
Environmental Surveillance
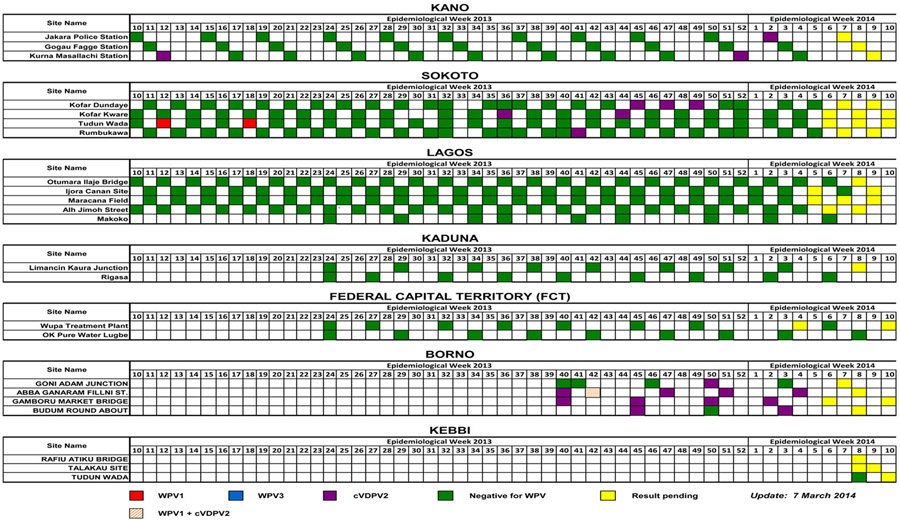
AFP surveillance is supplemented by environmental surveillance, for which sewage samples taken every 4–5 weeks are tested for polioviruses. The program expanded environmental surveillance from 3 sites in Kano during 2011 to 19 sites during 2013, including 3 in Borno, 2 in Kaduna, 3 in Kano, 5 in Lagos, 4 in Sokoto, and 2 in the FCT (Figure 2). In 2012, WPV1 was detected in 16 samples in Sokoto (during weeks 13 to 39) and 2 samples from Kano (during weeks 39 and 43). In 2013, WPV was detected in 1 sample from Kano (during week 6), 2 samples from Sokoto (during weeks 12 and 16), and 1 sample from Borno (during week 42). Positive samples in Sokoto were detected at a time when no WPV cases were detected in the AFP surveillance program. In addition, samples tested in Kano were negative at times when there was WPV circulation in the community. In 2012, cVDPVs were detected throughout the year in Sokoto (22 cases), Kano (4), and, in the later part of the year, Borno (9).
Figure 2.
Trends in environmental surveillance data, by state, 2013–2014. Abbreviations: cVDPV, circulating vaccine-derived poliovirus; VDPV, vaccine-derived poliovirus; WPV, wild poliovirus.
Trends in Polio Case Counts
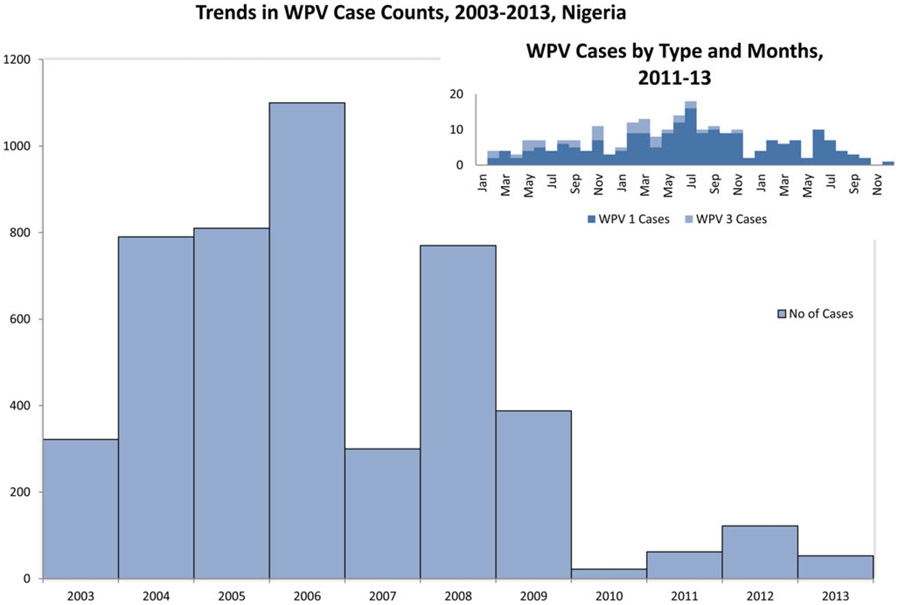
Between 2003 and 2009, Nigeria experienced large outbreaks of polio on a yearly basis, with a peak case count of 1122 in 2006 (Figure 3). Most of these outbreaks occurred in the north within well-established so-called sanctuaries in the north-central states (Kano, Kaduna, and Katsina), the northwest states (Sokoto and Zamfara), and the northeast states (Borno and Yobe). Within these sanctuaries, there were well-defined high-risk LGAs where most transmission occurred. After considerable efforts to strengthen program management in 2009, there was a decrease in case counts to 22 in 2010, followed by a resurgence to 62 cases in 2011. In 2012, 122 patients with AFP tested positive for WPV, decreasing to 53 confirmed cases in 2013 (as of 12 March 2014). No WPV3 cases have been reported in Nigeria since November 2012 (Figure 3).
Figure 3.
Trends in case counts of wild poliovirus (WPV) infection, 2003–2013, Nigeria.
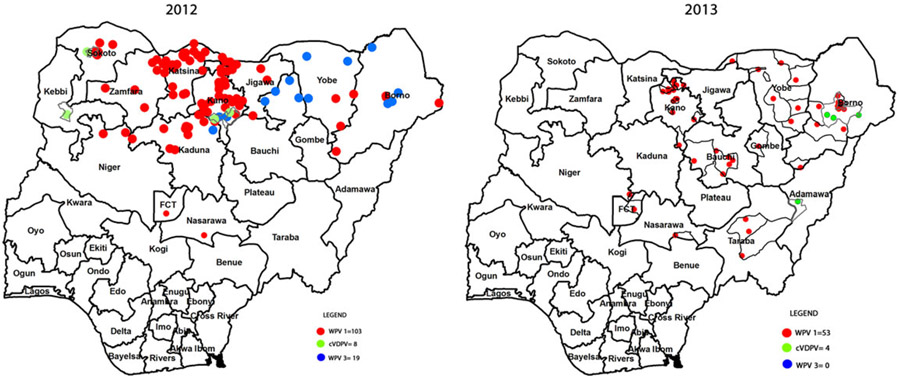
In 2013, individuals with polio ranged in age from 4 months to 14 years, with a mean age of 34 months; 7 patients (13%) were ≥5 years of age. Early in 2013, cases were reported in previously unaffected LGAs in the north-central states of Nasarawa, Niger, and FCT. Later in the year, WPV transmission was detected in Kano and the northeast (Figure 4). Forty-six of 53 cases in 2013 (86%) were reported from Borno (17 cases), Kano (15), Yobe (8), and Bauchi (6). Compared with 2012, the number of affected states declined from 13 to 9, and the number of affected LGAs dropped from 70 to 26. Eight cases of cVDPV type 2 (cVDPV2) infection were reported in 2012, compared with 5 cases reported in 2013. Four of the 5 cases reported in 2013 were detected in Borno.
Figure 4.
Geographic distribution of wild poliovirus and circulating vaccine-derived polio viruses, by type, 2012–2013.
As poliovirus circulation declined in reservoir communities, the genetic diversity of poliovirus isolates also declined. In 2011, 11 WPV1 clusters were circulating, including 8 that continued to circulate in 2012. At the time of writing, only 2 genetic clusters present in 2012 have been found in 2013, although either or both of these might be divided into additional clusters later in 2014, when all data from 2013 are analyzed. Partial genomic sequence analysis is used to assess surveillance sensitivity: a nucleotide difference of ≥1.5% in the coding region of the major capsid protein, VP1, from the closest matching sequences of previously identified isolates indicates gaps in surveillance involving >1 year of undetected virus circulation. Of 122 cases of WPV infection detected during January–December 2012, 13 (11%) had more genetic divergence than expected with sensitive AFP surveillance, compared with 10 of 53 cases (19%) detected in 2013. Genomic sequence analysis indicated that the cases of cVDPV2 infection identified in Borno in 2013 were closely related to a cVDPV2 lineage that had circulated in Chad during 2012 and spread to neighboring countries, including Cameroon and Niger. Similarly, sequence analysis indicated that WPV1 isolated from an environmental sample in Sokoto was not of the same cluster circulating in the area in 2012.
DISCUSSION
Considerable progress has been made in Nigeria toward stopping WPV transmission, owing to the management policies and program innovations put in place by the government and partners since 2012. As of late June 2014, no cases of WPV3 infection had been reported for >18 months. This could represent a landmark achievement for the global program. The geographic extent of WPV1 transmission appears to no longer include the northwestern states, and the number of WPV cases reported in 2013 (53) was <50% of that reported during 2012. This report suggests that the traditional sanctuaries of WPV transmission in northern Nigeria have been substantially reduced, with a reduction in the number of circulating clusters and no transmission in the traditional reservoirs of the northwest for the past 18 months. For the last 6 months of 2013 and first 6 months of 2014 transmission was restricted to Borno, Yobe, Kano, Bauchi, and Taraba.
The program experienced considerable setbacks in early 2013, including continued low SIA quality in specific areas and states, the killing of polio workers, and high levels of insecurity in the northeast. With increased political commitment and accountability in Kano, there has been progressive improvement in SIA quality, starting in late 2013, in previously poor-performing LGAs, with all achieving >80% coverage in the first 6 campaigns of 2014. These results during the season of low polio incidence, coupled with very low levels of WPV transmission, are encouraging. With such progress in a key endemic state like Kano, the 2014 national plan emphasizes sustaining improvements in the quality of SIAs and addressing key constraints in security-compromised areas of Borno and Yobe.
Activities planned to address the substantial immunity gap among children living in the security-compromised areas of Borno and Yobe include (1) mobile vaccination teams, (2) intensified routine infant immunization and other health services, (3) shortened intervals between OPV doses, (4) health camps coupled with intensified community engagement, (5) vaccination posts placed at state and LGA borders to vaccinate children in transit, and (6) simultaneous administration of OPV and inactivated polio vaccines in areas where access is limited. In addition, operational funds and prepositioned vaccine stocks are being provided so that SIAs can be organized quickly and implemented when windows of opportunity open for safe deployment of vaccination teams.
Improving AFP surveillance is a high priority in the 2014 strategic plan. The high proportion of orphan viruses detected in 2013 raises concern that wild virus could be circulating undetected. The majority of polio cases identified in the past 2 years were among children living in scattered and border settlements, and it is likely that these communities have served as a hidden reservoir where virus can circulate undetected. Of particular concern are underserved areas of Borno and Yobe, which have been difficult to access because of insecurity. The finding that cVDPVs in Borno and Chad share the same genetic lineage suggests that viruses are circulating across the border between Borno and Chad and emphasizes the importance of crossborder collaboration on surveillance and SIAs. Special efforts are planned to improve access to the underserved areas of Borno and Yobe, including the use of inactivated polio vaccine for children who have limited access to the healthcare system. Trivalent OPV was used in the December immunization plus days in selected areas of Borno to address the circulation of cVDPVs.
To sustain the progress in reducing WPV transmission, the program has adopted an aggressive SIA schedule in 2014 with innovations and is making considerable investments to improve routine infant vaccination coverage in northern Nigeria. While the reported OPV3 coverage data in 2013 is high, the 2013 Demographic Health Survey found that approximately 53% of children 12 to 23 months of age received 3 doses of polio vaccine [18]. To improve coverage, particular efforts are being made to take advantage of the substantial polio vaccination infrastructure to increase access to routine immunization services and raise vaccination coverage for other childhood vaccines. These efforts are receiving considerable support for addressing unmet health needs in many communities where morbidity and mortality from vaccine-preventable diseases is high. It is expected that these efforts will be a lasting legacy of the long walk to eradicate polio from Nigeria.
Acknowledgments.
The polio program in Nigeria is supported by thousands of dedicated healthcare workers and community volunteers. Key leadership is provided by health commissioners and the management teams at the state and LGA levels. This article is dedicated to the polio workers who lost their lives supporting program activities. It is incumbent on us, their colleagues, to remain dedicated to the unfinished work for which they died and to resolve that future generations will honor their ultimate sacrifice in the global eradication of polio.
Footnotes
Supplement sponsorship. This article is part of a supplement entitled “The Final Phase of Polio Eradication and Endgame Strategies for the Post-Eradication Era,” which was sponsored by the Centers for Disease Control and Prevention.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Burki T. The final push for polio. Lancet Infect Dis 2012; 12:591–2. [DOI] [PubMed] [Google Scholar]
- 2.Kew O. Reaching the last one per cent: progress and challenges in global polio eradication. Curr Opin Virol 2012; 2:188–98. [DOI] [PubMed] [Google Scholar]
- 3.Eighth Report of the Independent Monitoring Board of the Global Polio Eradication Initiative, 2013. http://www.polioeradication.org/Portals/0/Document/Aboutus/Governance/IMB/9IMBMeeting/9IMB_Report_EN.pdf. Accessed October 2013.
- 4.World Health Organization. Media centre Poliomyelitis, 2014; 2–4. [Google Scholar]
- 5.Aylward B, Tangermann R. The global polio eradication initiative: Lessons learned and prospects for success. Vaccine 2011; 29(Suppl 4):D80–5. [DOI] [PubMed] [Google Scholar]
- 6.CDC. MMWR_2012_nigeria_polio.
- 7.Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med 2007; 4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Obadare E. A crisis of trust: history, politics, religion and the polio controversy in Northern Nigeria. Patterns Prejudice 2005; 39:265–84. [Google Scholar]
- 9.Olufowote JO. Local resistance to the global eradication of polio: newspaper coverage of the 2003–2004 vaccination stoppage in Northern Nigeria. Health Commun 2011; 26:743–53. [DOI] [PubMed] [Google Scholar]
- 10.Renne E. Perspectives on polio and immunization in Northern Nigeria. Soc Sci Med 2006; 63:1857–69. [DOI] [PubMed] [Google Scholar]
- 11.WHO. Polio laboratory manual. Geneva: WHO, 2004. http://whqlibdoc.who.int/hq/2004/WHO_IVB_04.10.pdf. Accessed 31 August 2004. [Google Scholar]
- 12.Burns CC, Shaw J, Kew O. Multiple independent emergences of type 2 vaccine-derived polioviruses during a large outbreak in northern Nigeria. J Virol 2014; 2:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. Assessing vaccination coverage levels using clustered lot quality assurance sampling, 2012. http://www.polioeradication.org/portals/0/document/research/opvdelivery/lqas.pdf. Accessed 27 April 2012.
- 14.National Population Commission Nigeria. Nigeria, 2008. http://www.measuredhs.com/pubs/pdf/FR222/FR222.pdf. Accessed November 2013.
- 15.Murray CJL, Shengelia B, Gupta N, Moussavi S, Tandon A, Thieren M. Validity of reported vaccination coverage in 45 countries. Lancet 2003; 362:1022–7. [DOI] [PubMed] [Google Scholar]
- 16.Waziri NE, Ohuabunwo C, Nguku PM, et al. Polio eradication in Nigeria and the role of the National Stop Transmission of Polio (N-STOP) program, 2012–2013. J Infect Dis 2014; 210(suppl 1):S111–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CDC. Polio field census and vaccination of underserved populations in northern Nigeria. MMWR Morb Mortal Wkly Rep 2013; 62:663–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Nigeria Polulation Commission, Measure DHS II. Nigeria Demographic and Health Survey, 2013. http://dhsprogram.com/pubs/pdf/PR41/PR41.pdf. Accessed October 2013.