Acute stroke is now a treatable condition that deserves urgent specialist attention. Drug treatment and specialist care both influence survival and recovery. This article considers the optimal approaches to diagnosis and early management.
Conditions requiring referral to hospital
Admit to hospital
Neurological deficit lasting 1 hour or more
Dependent patients—that is, moderate to severe stroke
Transient ischaemic attack lasting 1 hour or more
More than one transient ischaemic attack within a week
Transient ischaemic attack on anticoagulation
Patient presenting to hospital
At request of general practitioner
Refer to cerebrovascular clinic
Independent patient more than 48 hours after stroke (withhold aspirin)
Transient ischaemic attack lasting less than 1 hour (give aspirin)
Symptoms and signs of stroke
| Anterior circulation strokes | Posterior circulation strokes |
| • Unilateral weakness | • Isolated homonymous hemianopia |
| • Unilateral sensory loss or inattention | • Diplopia and disconjugate eyes |
| • Isolated dysarthria | • Nausea and vomiting |
| • Dysphasia | • Incoordination and unsteadiness |
| • Vision: | • Unilateral or bilateral weakness and/or sensory loss |
| Homonymous hemianopia | Non-specific signs |
| Monocular blindness | • Dysphagia |
| Visual inattention | • Incontinence |
| • Loss of consciousness |
Stroke, a sudden neurological deficit of presumed vascular origin, is a clinical syndrome rather than a single disease. It is a common and devastating condition that causes death in one third of patients at six months and leaves another third permanently dependent on the help of others. Each year in the United Kingdom there are 110 000 first strokes and 30 000 recurrent strokes; 10 000 strokes occur in people younger than 65 and 60 000 people die of stroke. It is the largest cause of disability, and more than five per cent of NHS and social services resources are consumed by stroke patients. Correct management relies on rapid diagnosis and treatment, thorough investigation, and rehabilitation.
Assessing the patient
Patients should be assessed at hospital immediately after a stroke. They may need to go straight to hospital rather than wait to see their general practitioner since hyperacute treatments such as thrombolysis must be administered within as little as three hours after stroke. Ambulance crews can be trained to apply simple screening questions to identify likely stroke patients.
Characteristics of subtypes of stroke
| Lacunar | Partial anterior circulation | Total anterior circulation | Posterior circulation | |
|---|---|---|---|---|
| Signs | Motor or sensory only | 2 of following: motor or sensory; cortical; hemianopia | All of: motor or sensory; cortical; hemianopia | Hemianopia; brain stem; cerebellar |
| % dead at 1 year | 10 | 20 | 60 | 20 |
| % dependent at 1 year | 25 | 30 | 35 | 20 |
Stroke is a clinical diagnosis, but brain imaging is required to distinguish ischaemia from primary intracerebral haemorrhage. The pattern of neurological signs, including evidence of motor, sensory, or cortical dysfunction and hemianopia, can be used to diagnose certain clinical subtypes and thus to predict prognosis. Other signs also relate to outcome and may help identify the cause. If neurological symptoms resolve in less than 24 hours, the traditional diagnostic label is “transient ischaemic attack” rather than stroke. However, not all transient ischaemic attacks are genuinely ischaemic, and many are associated with permanent cerebral damage: a better term therefore is “mini-stroke.”
Pathophysiology
For practical purposes, there are two types of stroke after subarachnoid haemorrhage has been excluded. Ischaemia accounts for 85% of presentations and primary haemorrhage for 15%. Haemorrhage causes direct neuronal injury, and the pressure effect causes adjacent ischaemia. Primary ischaemia results from atherothrombotic occlusion or an embolism. The usual sources of embolism are the left atrium in patients with atrial fibrillation or the left ventricle in patients with myocardial infarction or heart failure.
Signs of stroke at clinical examination
Conscious level
Neurological signs
Blood pressure
Heart rate and rhythm
Heart murmurs
Peripheral pulses
Systemic signs of infection or neoplasm
Vessel occlusion arises from atherosclerosis, typically in the internal carotid artery just above the carotid bifurcation or from small vessel disease deep within the brain. Ischaemia causes direct injury from lack of oxygenation and nutritional support and sets up a cascade of neurochemical events that lead to spreading damage. The ischaemia may be reversible if reperfusion is obtained quickly (now proved in clinical trials), and the chemical injury may be interrupted by various neuroprotective drugs (unproved in humans).
Emergency management
Within the first hours after onset of cerebral ischaemia part of the brain is under threat of death. The infarct core may be densely ischaemic and will inevitably die, but there is also tissue with a compromised blood supply balanced on a knife edge between death and recovery. At this stage, oxygenation and haemodynamic and metabolic factors are crucial. The emergency management of stroke requires medical stabilisation and assessment of factors that may lead to complications (such as swallowing and hydration); thrombolysis may be considered (see below). An acute stroke unit concentrates patients, healthcare staff, resources, and expertise into one area, and such units may be associated with a better outcome.
Death rate (percentage) 30 days, one year, and five years after different types of stroke
| 30 days | 1 year | 5 years | |
|---|---|---|---|
| Ischaemic stroke | 10 | 23 | 52 |
| Intracerebral haemorrhage | 52 | 62 | 70 |
| Subarachnoid haemorrhage | 45 | 48 | 52 |
Conditions that mimic stroke
| Diagnosis | Diagnostic features |
| Decompensation of previous stroke | Evidence of infection such as urinary or respiratory tract; metabolic disturbance |
| Cerebral neoplasm (primary or secondary) | Less abrupt onset; primary tumour or secondary to, for example, lung or breast cancer |
| Subdural haematoma | Recent head injury |
| Epileptic seizure | Possible previous episodes |
| Traumatic brain injury | History of trauma |
| Migraine | Less abrupt onset; followed by headache; younger patients |
| Multiple sclerosis | Less abrupt onset; possible previous episodes |
| Cerebral abscess | Infection |
Investigations
Patients with acute stroke should have computed tomography of the brain to distinguish ischaemic and haemorrhagic stroke. This separation is vital since subsequent investigations and treatment differ for the two types. Neuroimaging will also identify conditions mimicking stroke and can help predict outcome. Ideally, imaging will be performed soon after admission. Magnetic resonance imaging of the brain may eventually replace computed tomography since it not only identifies stroke anatomy but can also assess blood flow and perfusion in the brain, detect whether lesions are new or old, and identify carotid artery stenosis.
The extent to which the cause of the stroke should be investigated depends on several factors, including the likely degree of recovery, the presence of obvious risk factors, and the age of the patient; younger patients are more likely to have an identifiable cause such as an inflammatory or clotting disorder which may require specific treatment. Although investigations should be restricted to tests that will inform clinical management, guidelines can be used to determine which investigations are needed after stroke.
Investigation of stroke
All patients
Computed tomography (or magnetic resonance imaging)
Electrocardiography
Chest radiography
Full blood count
Clotting screen
Electrolyte and creatinine concentrations
Subgroups
Carotid duplex scanning
Echocardiography
Thrombophilia screen
Immunology screen
Syphilis serology
Cerebral angiography (rarely)
Swallowing and feeding
Dysphagia affects 35% of stroke patients. It is often unrecognised after mild stroke and is associated with a poor outcome, partly because it predisposes to aspiration and pneumonia and partly because of the nutritional deficit. Presence of a gag reflex is a poor guide to safe swallowing, and a formal assessment by trained staff is essential. Fluids are more difficult to swallow than semisolids. Dysphagic patients should be fed through a nasogastric tube or percutaneous endoscopic feeding tube until it is safe to resume oral food and fluids. Most dysphagic patients will not need enteral feeding beyond a few weeks. However, when and how optimally to feed dysphagic patients remains to be determined.
Acute drug treatments for ischaemic stroke
Aspirin
Most patients
Heparin (unfractionated or low molecular weight):
Prophylactic
Previous venous thromboembolism
Morbid obesity
Therapeutic
Carotid artery dissection
Embolic, recurrent transient ischaemic attacks
Acute intervention
Firm evidence from two large trials has shown that aspirin (160-300 mg daily by mouth, nasogastric tube, or rectum) started within 48 hours of onset of acute ischaemic stroke reduces the risk of subsequent death and disability. However, the effect of aspirin is small (number needed to treat (NNT)=77) and is principally mediated through reducing the risk of early reinfarction. Neuroimaging is strongly recommended before starting aspirin. A large trial of unfractionated heparin in stroke patients found that heparin did not improve outcome, even in patients with presumed embolic stroke. Heparin may still be useful in certain groups of patients.
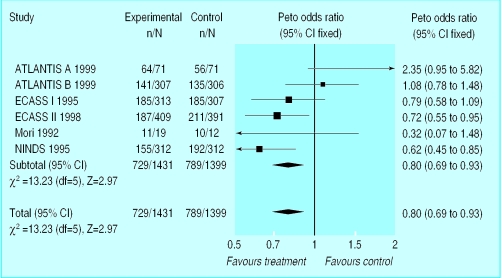
Thrombolysis with alteplase within three hours of onset of stroke significantly increases the chance of a near complete recovery (NNT=7) when administered by specialists. Treatment up to six hours after stroke has been found less effective in meta-analysis of randomised controlled trials (estimated NNT=12). Thrombolysis is currently licensed for stroke only in North America and New Zealand, and concerns remain about its safety.
Neuroprotectant drugs (which may protect neurones from ischaemia) have, to date, shown no benefit in ischaemic or haemorrhagic stroke, although several trials are still in progress.
Patients with a large cerebellar infarct or bleed should be referred for immediate neurosurgical evaluation to facilitate evacuation of the clot or infarct, or shunting for acute hydrocephalus, if required. Anticoagulants should be reversed in patients with primary intracerebral haemorrhage.
Complications of stroke
Stroke may be complicated by several conditions that can alter outcome adversely. Hyperglycaemia, fever, and hypertension are each associated with a poor prognosis. In the absence of trial evidence, raised glucose concentrations should be normalised and paracetamol given for fever. In contrast, hypertension should not be treated for the first week since some antihypertensive drugs (notably calcium channel blockers) seem to worsen outcome, possibly by reducing regional cerebral blood flow. Large ischaemic strokes are often complicated by oedema, swelling, and herniation leading to death; no proved treatment is available for these complications.
Complications of stroke
Hyperglycaemia
Hypertension
Fever
Infarct extension or rebleeding
Cerebral oedema, herniation, coning
Aspiration
Pneumonia
Urinary tract infection
Cardiac dysrhythmia
Recurrence
Deep vein thrombosis, pulmonary embolism
Venous thromboembolic disease (deep vein thrombosis, pulmonary embolism) develops in half of immobile patients unless preventive measures are taken. Although compression stockings reduce the risk of deep vein thrombosis in other groups of high risk patients, this has not been confirmed in stroke. A combination of stockings, early mobilisation, adequate hydration, and aspirin is considered good practice in patients with ischaemic stroke. Early mobilisation may also reduce the risk of pressure sores, respiratory tract infections, and urinary tract infections. When possible, urinary catheters should be avoided to minimise the risk of infection.
Rehabilitation
The principal aims of rehabilitation are to restore function and reduce the effect of the stroke on patients and their carers. Rehabilitation should start early during recovery with assessment and mobilisation while the patient is in the acute stroke unit. Once patients are medically stable, they should be transferred to a stroke rehabilitation unit if further rehabilitation is required. Formal rehabilitation in a stroke unit is associated with reduced death and disability (NNT=12) and a shorter stay in hospital. Optimal care is multidisciplinary: doctors, nurses, physiotherapists, occupational therapists, speech and language therapists, dieticians, psychologists, and social workers all have a role.
Healthcare professionals, patients, and carers can obtain further information about strokes from the Stroke Association (020 7566 0300), Chest, Heart and Stroke Association Scotland (0131 225 6963), Chest, Heart, and Stroke Association Northern Ireland (01232 320184), or Different Strokes (01908 236033)
Secondary prevention
Secondary prevention (apart from blood pressure control) should start shortly after admission. All patients should be offered lifestyle guidance, including advice to stop smoking, reduce saturated fat and salt consumption and alcohol intake, lose weight, and increase exercise. Aspirin started for the treatment of acute ischaemic stroke should be continued indefinitely for secondary prevention. The use of alternative or additional antithrombotic drugs (dipyridamole, clopidogrel, and warfarin), carotid endarterectomy, and management of hypertension and hyperlipidaemia after stroke are discussed in the next article in the series.
Further reading
Bath PMW. The medical management of stroke. Int J Clin Pract 1997;51:504-10.
Lees KR. If I had a stroke. . . . Lancet 1998;352 (suppl III):28-30.
Royal College of Physicians. Stroke audit package. London: RCP, 1994.
Stroke Units Trialists' Collaboration. Collaborative systematic review of the randomised trials of organised inpatient (stroke unit) care after stroke. BMJ 1997;314:1151-9.
The future
Stroke management is now supported by good quality evidence, but many questions remain unanswered. Whenever possible, patients should be given the opportunity to enrol in randomised trials of acute interventions, rehabilitation, or secondary prevention.
Figure.
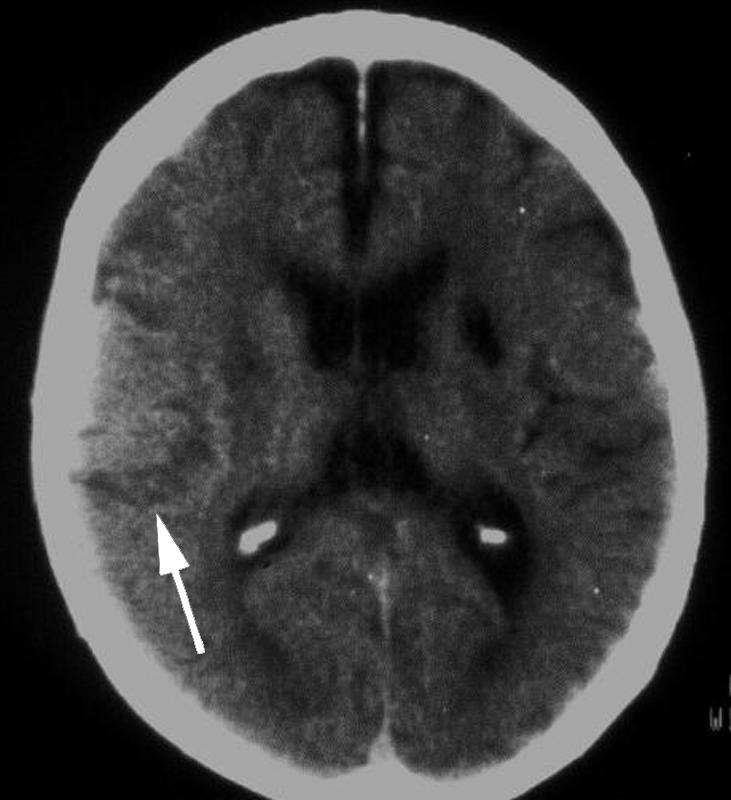
Computed tomogram showing ischaemic stroke
Figure.

Computed tomogram showing haemorrhagic stroke
Figure.

Magnetic resonance angiogram showing middle cerebral artery occlusion
Figure.
Meta-analysis shows that thrombolysis reduces combined death and disability from stroke
Figure.
Stroke patient receiving rehabilitation therapy
Acknowledgments
The magnetic resonance image was provided by Professor Alan Moody, University of Nottingham. The data on thrombolysis were provided by Dr Joanna Wardlaw, University of Edinburgh.
Footnotes
Philip M W Bath is professor of stroke medicine, University of Nottingham, and Kennedy R Lees is professor of cerebrovascular medicine, university department of medicine and therapeutics, Western Infirmary, Glasgow.
The ABC of arterial and venous disease is edited by Richard Donnelly, professor of vascular medicine, University of Nottingham and Southern Derbyshire Acute Hospitals NHS Trust (richard.donnelly@nottingham.ac.uk) and Nick J M London, professor of surgery, University of Leicester, Leicester (sms16@leicester.ac.uk). It will be published as a book later this year.