Abstract
INTRODUCTION:
Out-of-hospital cardiac arrest is a major public health problem with over 90% case fatality. Although it is known that good quality of cardiopulmonary Resuscitation (CPR) leads to improved patient outcomes, health care practitioners commonly perform sub-optimal CPR. The CPR feedback device is a small device designed to measure the number and depth of chest compressions (CC) and if the rate of compressions or the depth of the compressions is low or high, it will try to correct the CPR operation by announcing a warning to the resuscitator. The aim of this study was to evaluate the effectiveness of this device which was designed and made by the authors’ technician study group member in improving CPR operations, to determine the need for it in all hospitals on a routine basis.
METHOD:
This cross-sectional study was performed on patients who have suffered from cardio-pulmonary arrest in Al-Zahra Hospital in 2020. Patients needed primary CPR for any reason, were randomly divided into two groups using random allocation software. The first group contains patients as the CPR Feedback device is on and alarm is on and warns, if resuscitation is ineffective, the second group also uses the device, but with the difference that the alarm is off. The data was analyzed by general linear model method (repeated measure ANOVA).
RESULTS:
80 patients were studied, including 63 men (79%) and 17 women (21%). Patients were divided among two groups. There was no significant difference in demographic characteristics between two groups. The results showed that there was no significant interaction between group and time for the compression depth variable and there was no significant difference in the depth of compressions between the two groups(P>0.05). For the rate of compressions, there was a significant interaction between group and time. These results indicate that turning on the CPR feedback device’s warning increases the number of compressions during CPR and, as a result, makes it more effective. The between-group effect which showed the difference in the number of compressions in the two groups, was statistically significant (P<0.001).
CONCLUSION:
These results indicated that turning on the CPR feedback device’s warning increases the rate of compressions during CPR and, as a result, makes it more effective. Therefore, the use of real-time CPR feedback device during chest compression in real-time CPR improves the quality of CPR.
Key Words: Heart arrest, Cardiopulmonary resuscitation, Chest compression, rate of massages, Depth of the massage
Introduction
Out-of-hospital cardiac arrest (OHCA) is indeed a significant public health issue, with a global incidence estimated at 95.9 per 100,000 person per year and a case fatality rate exceeding 90%. Survival rates to hospital discharge are generally poor and can vary significantly across different emergency systems 1.
The 2010 International Liaison Committee on Resuscitation (ILCOR) consensus guidelines emphasize the importance of optimizing all links in the ‘Chain of Survival’ to maximize neurologically intact survival after cardiac arrest. This includes delivering high-quality cardiopulmonary resuscitation (CPR). Specifically, rescuers should aim for a compression depth of at least 5 cm at a rate of at least 100 compressions per minute, allow full recoil of the chest between compressions, and minimize interruptions in chest compressions. The recommended compression to ventilation ratio is 30:2 2, 3.
Even brief interruptions to chest compressions of around 4 seconds can lead to reduced myocardial perfusion and survival. Furthermore, the success of defibrillation decreases in patients during prolonged periods without chest compressions. The depth and fraction (the proportion of time chest compressions are administered in CPR) of chest compressions are directly related to survival from OHCA. Every 1 mm increase in depth (up to 50 mm) increases the adjusted odds of survival by 5% (OR 1.05, 95% CI 1.01–1.09) 4-6. High chest compression fractions (>60%) are associated with higher rates of return of spontaneous circulation (ROSC) (79% vs. 58%) and survival to discharge (25% vs. 12%) when compared with the lowest fraction group (<20%) 7.
Despite the known benefits of high-quality CPR, health care practitioners often perform sub-optimal CPR. This can include as little as 28% of chest compressions in the target depth range, effective compression rates as low as 64 per minute, and a hands-off fraction of 0.48 8, 9. Real-time feedback may enable rescuers to perform better CPR, potentially leading to improved patient outcomes 10, 11.
The CPR feedback device is a small device designed to measure the number and depth of CCs. If the number of compressions or the depth of the compressions is low or high, it will attempt to correct the CPR operation by issuing a warning to the resuscitator. A similar model of this device was designed by companies such as Philips and Zoll, but due to their relatively high price in Iran, it is not possible to use them routinely. An in-house sample of this device was produced by a member of the authors’ team and is used in this study. The only systematic review of the impact of real-time feedback during CPR was completed in 2009 and focused on feedback as a training device rather than an adjunct to real-life cardiac arrests. Therefore, the current study was conducted with the aim of evaluating the effectiveness of this device in improving CPR operations to determine the need for it in all hospitals on a routine real-life basis.
Materials and Methods
This study was approved by the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (IR.MUI.MED.REC.1401.180).
This cross-sectional study was conducted on patients who had suffered from cardio-pulmonary arrest in Al-Zahra Hospital from January 2021 to March 2022. Eighty patients requiring primary CPR were selected and evaluated.
Investigational CPR feedback device
An investigational device with CPR-sensing and audiovisual feedback capabilities was used during all cardiac arrests. The feedback component was developed in part from earlier work with CPR audio feedback in simulated resuscitation settings. The device, the size and dimensions of a mobile phone, is placed on the patient’s sternum. The in-house sample is designed exactly with the dimensions and specifications of the standard sample.
In brief, the CPR feedback device detects chest compressions via a pad placed between the hands of the resuscitator and the sternum of the patient. This pad contains both force detector and accelerometer components that allow for the calculation of chest compression rate and depth. If the number of compressions or the depth of the compressions is low or high, it will attempt to correct the CPR operation by issuing a warning to the resuscitator. The use of this device is among the recommendations in European and American CPR guidelines of resuscitation to improve the quality of resuscitation, but it is not used in the authors’ country due to the high cost and non-availability. The purpose of the authors’ study is to use this device in real-life resuscitation situations.
Study protocol
This study was conducted on patients who had suffered from cardio-pulmonary arrest in Al-Zahra Hospital in 2020. Patients requiring primary CPR for any reason were randomly divided into two groups using random allocation software.
The first group, named the “feedback_on” group, consisted of patients for whom the CPR Feedback device was on and the alarm was active, issuing warnings if resuscitation was ineffective. The second group, named the “feedback_off” group, also used the device, but with the alarm turned off. Given that the occurrence of cardiorespiratory arrest is an unpredictable event in hospitalized patients and the use of the mentioned device does not interfere with the course of resuscitation measures or create a change in the process, there was no possibility to fill in an informed consent form. Information collected from patients included age, sex, underlying disease, cause of arrest, and their outcome. In addition, information collected to evaluate the effectiveness of CPR included depth (the amount indicated by the device) and the number of compressions per minute. Also, in the first group, the number of feedback given by the device to the resuscitator was collected. The information was recorded at 5, 10, 15, 20, 25, 30, 35, 40, and 45 minutes after the start of CPR. Before starting the study, resuscitators were trained to use the CPR Feedback device.
Statistical Analysis
Basic descriptives for numerical data were presented as mean (SD). A general linear model (repeated measure ANOVA) was performed to determine the effectiveness of the CPR feedback device by comparing the depth and rate of CPR over time, between the two groups. The data were analyzed using IBM SPSS Statistics (Version 27) with statistical significance set at P < 0.05.
Results
Eighty patients were studied, including 63 men (79%) and 17 women (21%). Patients were divided among two groups. The first group, named the “feedback_on” group, consisted of 40 patients for whom the CPR Feedback device was on and the alarm was active, issuing warnings if resuscitation was ineffective. The second group, named the “feedback_off” group, also used the device, but with the alarm turned off. The mean age was 65.86 ± 7.81 years (Table 1).
Table 1.
Demographic parameters of patients Note: SD: Standard deviation,n: number, %: percent
| Group 1 Feedback_on | Group2 Feedback_off |
Total
n (%) |
p-value | |
|---|---|---|---|---|
| Sex | ||||
| Men n.(%) | 32(80%) | 31(77%) | 63(79%) | 0.30 |
| Women n.(%) | 8(20%) | 9(23%) | 17(21%) | 0.29 |
| Total n. | 40 | 40 | 80 | - |
| Age | ||||
| Mean | 62.71 | 63.01 | 65.86 | 0.23 |
| SD | 6.80 | 7.92 | 7.51 | - |
The difference in demographic parameters between two groups was compared. There was no significant difference in demographic characteristics between two groups. Also means and Standard deviations of depth and rate of CPR in two groups computed (Table2).
Table 2.
Comparison of rate of CPR and depth in 9 times point in two groups with and Without Feedback
| Time points | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | 5min | 10min | 15min | 20 min | 25min | 30 min | 35min | 40min | 45 min | P Group |
P Time |
P Group*time |
|
| Rate | |||||||||||||
| Feedback on | 100.62±5.15 | 108.72 ±5.92 |
108.75 ±6.27 |
105.8 ±8.34 |
107.1 ±8.14 |
106.7 ±6.98 |
105.17 ±4.30 |
100.42 ±5.88 |
100.48 ±4.63 |
<0.001 | 0.001 | 0.001 | |
| Feedback off | 100.85±5.03 | 100.27 ±4.01 |
98.78 ±5.04 |
96.9 ±3.67 |
93.77 ±5.11 |
94.45 ±5.19 |
89.93 ±6.03 |
89.6 ±5.05 |
88.3 ±3.58 |
||||
| Depth | |||||||||||||
| Feedback on | 56.4 ±3.38 |
56.75 ±3.55 |
56.88 ±3.196 |
59.33 ±4.75 |
58.75 ±4.68 |
58.75 ±4.82 |
59.10 ±4.75 |
58.83 ±4.53 |
57.7 ±3.43 |
0.434 | 0.049 | 0.149 | |
| Feedback off | 58.63±3.91 | 58.4± 5.32 |
57.65 ±3.94 |
58.13 ±4.40 |
59.43 ±4.67 |
58.55 ±4.56 |
57.98 ±4.74 |
58.25 ±4.54 |
57.37 ±3.01 |
||||
Based on Table 2, in the first group (feedback_on), the massage depth variable initially increased and then decreased over time. There is no specific pattern regarding the variable number of massages. In the second group (feedback_off), there is no particular pattern of increase or decrease for the massage depth variable at consecutive times, but for the number of massages, the average number of CPR has decreased over time. In order to answer the main research question of comparing the effect of the CPR feedback device on the effectiveness of CPR in the two states of the device’s alarm being on and off, a variance analysis test with repeated measurements was used (repeated measure ANOVA). Initially, the assumptions of this test were checked.
The Box test was used to check the homogeneity of variance-covariance matrices. Since the significance of the Box test is higher than 0.05 in all scales, it can be said that the variance-covariance matrices are homogeneous. Levine’s test was also used to check the homogeneity of the variances of the two groups, and the results showed the non-significance of the components (P>0.05), so the assumption of the homogeneity of the variances was also confirmed. In line with the assumption of the same variance, the results of the sphericity test showed that it is not significant at the 0.05 level in all variables. Therefore, the conditions for using the statistical model of repeated measurement were provided. After verifying the assumptions of the test, an analysis of variance between and within the subjects was performed with repeated measurements for the variables of massage depth and number of massages. The results are presented in Table 2
Table 2 shows that there was no significant interaction between group and time for the massage depth variable (Wilks’ Lambda=0.844, P=0.149, F=1.513, η2=0.019). Also, the within-group effects that indicate the main effect of time were significant (Wilks’ Lambda=0.810, P=0.049, F=2.081, η2=0.159). Significant pairwise comparisons between different times are identified with post hoc tests (Bonferroni) and show the direction of change. For depth variables, no significant difference was observed across times. The effect size obtained for time was 0.156, which according to Cohen (1988) indicates a large effect (small effect = 0.01, medium effect = 0.06, and large effect = 0.14). The between-group effect, which shows the main effects of comparing two groups in the massage depth variable, was not significant (P>0.05). Therefore, it is concluded that there is no difference in the depth of massage in the two groups.
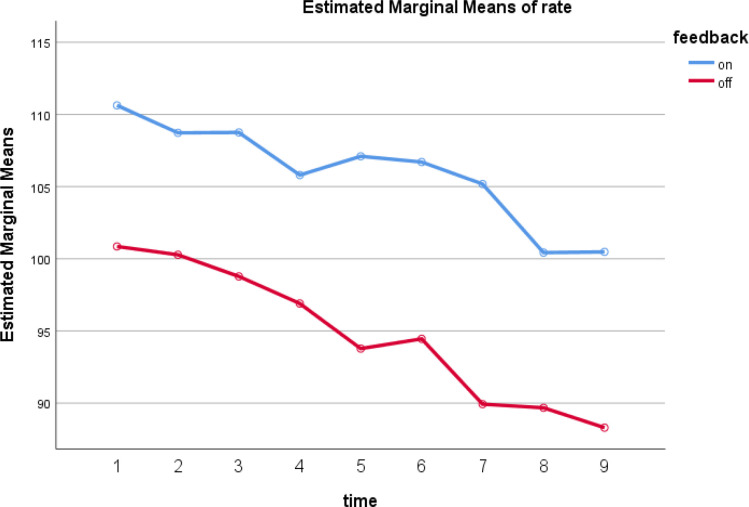
Also, the study results show that for the variable number of massages, there is a significant interaction between group and time (Wilks’ Lambda=0.657, P<0.001, F=4.624, η2=0.343). This means that there is a uniform change in the values of the number of massages over time. Also, the within-group effects indicating the main effect of time were significant (Wilks’ Lambda=0.141, P=0.001, F=53.854, η2= 0.859). Significant pairwise comparisons between different times are identified with post hoc tests and show the direction of change. The post hoc result for the rate variable showed that almost all times are significant except times 5 min with 10 min, 15 min. Time 20 min with 15 min, 25 min, and 30 min. Time 25 min with 30 min and 35 min. The effect size obtained for time is 0.343, which indicates a large effect size. The between-group effect, which shows the main effects of comparing two groups in the massage depth variable, was also significant (P<0.001) which shows the difference in the number of massages in the two groups. The group effect size was also very large (η2=0.871). The interaction effects of group and time for the variable number of massages are shown in Figure 1.
Figure 1.
Estimated Marginal Means of rate
In Figure 1, the average number of compressions in the first group (feedback_off) at time 1 (first 5 minutes) was less than the second group (feedback_on) and this trend continued until time 9 (45 minutes). Also, over time, the average number of compressions in both groups has decreased. These results indicate that activating the warning on the CPR feedback device increases the number of compressions during CPR and, as a result, makes it more effective.
Discussion
The authors have demonstrated improvements in the quality of CPR delivered during actual in-hospital cardiac arrests with the use of a CPR feedback device. The rate and depth of chest compressions improved during resuscitation efforts in the cohort of patients receiving real-time feedback.
The 2015 AHA Guidelines recommend, and the AHA mandated in 2017, the use of audiovisual feedback in all CPR training12,13. Some other studies have found similar improvements in CPR quality using the same technology in the out-of-hospital setting. These findings are consistent with prior work in simulated settings as well, in which CPR performance improved using a voice-activated manikin system or a free-standing CPR feedback device 14-16. Another recent investigation has demonstrated general improvement with ACLS protocol compliance when voice prompts were incorporated into an automatic external defibrillator (AED) 17, 18. To the best of the authors’ knowledge, their work represents the first clinical demonstration of real-time feedback to improve the performance of manual CPR.
The CPR feedback device can improve the quality of CPR where chest compression depth and rate are concerned, and these devices can be used as part of training and during actual CPR during a real cardiac arrest scenario. Furthermore, if the quality of CPR is deteriorating, it may be a sign of fatigue, and the person performing CPR should be swapped. Rescuer fatigue has been shown to adversely affect the quality of CPR 19. Perberdy et al. showed improvements with the use of a similar accelerometer-based audiovisual feedback device and concluded that these devices can be used to improve the quality of CPR 20.
A large body of studies has supported the importance of CPR, but only recently has the quality of CPR been formally assessed and found to be deficient in a number of clinical studies 21-24. These performance deficiencies are especially important and worrisome in the context of literature showing that CPR may be a more important immediate intervention than defibrillation, especially with long (>5 min) arrest times 24. In addition, recent work has shown that chest compressions may have an important influence on subsequent defibrillation success and the probability of achieving Return of Spontaneous Circulation (ROSC) 25. Taken together, these findings led to a renewed emphasis on CPR quality in the recent Emergency Cardiovascular Care guidelines revision as formulated by the International Liaison Committee on Resuscitation 26. The guidelines recommended that medical systems develop programs to monitor CPR quality and improve training in Basic Life Support skills. It is important to note, however, that scant literature exists to support the clinical relevance of specific improvements in CPR variables, such as the relative importance of a change in chest compression rate or depth. So, the authors designed their study to improve the literature. CPR quality can be improved through a variety of different strategies such as training programs or using a CPR feedback device.
A limitation of the study would be the lack of randomization of the order of CPR with and without feedback. There may be an element of “learning” whereby after the first attempt at CPR the performers get better because of practice and the study could have been improved with randomization of the order of the intervention and control. More studies with larger samples and in different settings like out-of-hospital CPR are recommended.
Conclusion
In conclusion, the use of a real-time CPR feedback device during chest compression in real-time CPR improves the quality of CPR. The authors recommend the use of CPR feedback during training and during actual CPR to improve the quality of CPR. More studies are required to show that feedback devices can improve survival in patients with cardiac arrest receiving CPR.
Conflict of Interests
Authors have no conflict of interests.
Acknowledgments
The authors would like to express their gratitude to all those who assisted in this study, especially Isfahan University of Medical Sciences and Mr. Madhkhan for the design of the in-house sample of this device that was used in this study. They would also like to thank all the patients and staff of Al-Zahra Hospital, Isfahan.
References
- 1.Berdowski J, Berg RA, Tijssen JGP, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Fischer H, Gruber J, Neuhold S, Frantal S, Hochbrugger E, Steinlechner B, et al. Effects and limitations of an automated external defibrillator with audiovisual feedback for cardiopulmonary resuscitation: a randomized manikin study. 2011;15(1):1–190. doi: 10.1016/j.resuscitation.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 3.Havel C, Schreiber W, Trimmel H, Malzer R, Haugk M, Richling N, et al. Quality of closed chest compression on a manikin in ambulance vehicles and flying helicopters with a real time automated feedback. Resuscitation. 2010;81(1):59–64. doi: 10.1016/j.resuscitation.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. 2011:342. doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirkbright S, Finn J, Jacobs I, Sprivulis P, Thompson PJ. The relationship between quality of cardiopulmonary resuscitation performed by healthcare professionals and patient survival following cardiac arrest: a systematic review of randomised and non-randomised trials. 2013 [Google Scholar]
- 6.Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. 2014;85(4):460–71. doi: 10.1016/j.resuscitation.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Kong MH, Fonarow GC, Peterson ED, Curtis AB, Hernandez AF, Sanders GD, et al. Systematic Review of the Incidence of Sudden Cardiac Death in the United States. J Am Coll Cardiol. 2011;57(7):794–801. doi: 10.1016/j.jacc.2010.09.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kramer-Johansen J, Myklebust H, Wik L, Fellows B, Svensson L, Sørebø H, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: A prospective interventional study. Resuscitation. 2006;71(3):283–92. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Semeraro F, Frisoli A, Loconsole C, Bannò F, Tammaro G, Imbriaco G, et al. Motion detection technology as a tool for cardiopulmonary resuscitation (CPR) quality training: A randomised crossover mannequin pilot study. Resuscitation. 2013;84(4):501–7. doi: 10.1016/j.resuscitation.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Skorning M, Beckers SK, Brokmann JC, Rörtgen D, Bergrath S, Veiser T, et al. New visual feedback device improves performance of chest compressions by professionals in simulated cardiac arrest. Resuscitation. 2010;81(1):53–8. doi: 10.1016/j.resuscitation.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka S, Tsukigase K, Hara T, Sagisaka R, Myklebust H, Birkenes TS, et al. Effect of real-time visual feedback device ‘Quality Cardiopulmonary Resuscitation (QCPR) Classroom’ with a metronome sound on layperson CPR training in Japan: a cluster randomized control trial. 2019;9(6):e026140 . doi: 10.1136/bmjopen-2018-026140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhanji F, Donoghue AJ, Wolff MS, Flores GE, Halamek LP, Berman JM, et al. Part 14: education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. 2015;132(18_suppl_2):S561–S73. doi: 10.1161/CIR.0000000000000268. [DOI] [PubMed] [Google Scholar]
- 13.Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. 2015;95:81–99. doi: 10.1016/j.resuscitation.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 14.Handley AJ, Handley SA. Improving CPR performance using an audible feedback system suitable for incorporation into an automated external defibrillator. Resuscitation. 2003;57(1):57–62. doi: 10.1016/s0300-9572(02)00400-8. [DOI] [PubMed] [Google Scholar]
- 15.Wik L, Thowsen J, Steen PA. An automated voice advisory manikin system for training in basic life support without an instructor A novel approach to CPR training. 2001;50(2):167–72. doi: 10.1016/s0300-9572(01)00331-8. [DOI] [PubMed] [Google Scholar]
- 16.Boyle AJ, Wilson AM, Connelly K, McGuigan L, Wilson J, Whitbourn R. Improvement in timing and effectiveness of external cardiac compressions with a new non-invasive device: the CPR-Ezy. 2002;54(1):63–7. doi: 10.1016/s0300-9572(02)00049-7. [DOI] [PubMed] [Google Scholar]
- 17.Chiang W-C, Chen W-J, Chen S-Y, Ko PC-I, Lin C-H, Tsai M-S, et al. Better adherence to the guidelines during cardiopulmonary resuscitation through the provision of audio-prompts. 2005;64(3):297–301. doi: 10.1016/j.resuscitation.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 18.Abella BS, Edelson DP, Kim S, Retzer E, Myklebust H, Barry AM, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. 2007;73(1):54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 19.Wee J, Nandakumar M, Chan YH, Yeo RS, Kaur K, Anantharaman V, et al. Effect of using an audiovisual CPR feedback device on chest compression rate and depth. 2014;43(1):33–8. [PubMed] [Google Scholar]
- 20.Peberdy MA, Silver A, Ornato JP. Effect of caregiver gender, age, and feedback prompts on chest compression rate and depth. 2009;80(10):1169–74. doi: 10.1016/j.resuscitation.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 21.Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O’Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. 2005;293(3):305–10. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 22.Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O’Hearn N, Wigder HN, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. 2005;111(4):428–34. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 23.Valenzuela TD, Kern KB, Clark LL, Berg RA, Berg MD, Berg DD, et al. Interruptions of chest compressions during emergency medical systems resuscitation. 2005;112(9):1259–65. doi: 10.1161/CIRCULATIONAHA.105.537282. [DOI] [PubMed] [Google Scholar]
- 24.Wik L, Kramer-Johansen J, Myklebust H, Sørebø H, Svensson L, Fellows B, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. 2005;293(3):299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 25.Edelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. 2006;71(2):137–45. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 26.Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. 2006;8(9):746–837. doi: 10.1093/europace/eul108. [DOI] [PubMed] [Google Scholar]