Abstract
There have been very rare reports on the migration of foreign bodies that are left or implanted in the body, and so far, they have only been reported in the gastrointestinal tract and intestines (a process similar to phagocytosis), later manifesting as an obstruction in the lumen. Meanwhile, no such cases have yet been reported in the cardiovascular system.
The case reported here is a 14-month-old girl who had undergone pulmonary artery banding (PA band made of PTFE) around the pulmonary artery at the age of 8 months due to severe pulmonary hypertension and failure to thrive. She underwent reoperation six months later for a final treatment. It was discovered that the PA band was no longer around the pulmonary artery and had migrated completely into the pulmonary artery while remaining intact and circular and was drawn into the pulmonary artery in a process similar to phagocytosis. The PA band was removed completely. The uneven surface inside the main pulmonary artery was resected and the artery was repaired end-to-end. A total heart repair surgery was again performed on the patient. No problem was observed in the 2.5-year follow-up after the second surgery.
Overall, the authors’ case is the first instance of migration of a biologically-neutral foreign body into the cardiovascular system that had occurred six months after the PA-band implantation, and the first case of erosion of a foreign body into the lumen outside the gastrointestinal tract. Although the authors could not find the cause of the presented case, reports on future cases can help find the underlying reason
Key Words: Erosion, Medical device, Gossypiboma, textiloma, Cardiac surgery
Introduction
Retained surgical bodies (RSB) are of two types. In one type, these foreign bodies are mistakenly left in the patient’s body during surgery, most commonly including leaving the gauze, long gauze, and surgical instruments, which is referred to as textiloma or gossypiboma1. In the other type, medical devices are intentionally left inside the body as part of a treatment, such as prostheses, artificial heart valves, meshes, etc.
Rarely, foreign bodies (gossypiboma) left in the abdomen have eroded the intestinal wall and migrated into the intestine without perforation (a process similar to phagocytosis) and have later manifested as an obstruction in the intestine1. Nevertheless, in cases where the surgeon implants an object inside the body, it is crucial that it be made of a substance that will not erode into adjacent tissues (e.g., in the case of artificial heart valves or prostheses).
All reported cases of a foreign body migrated into an organ have been gastrointestinal1-4 and occurred in the intestines, and no such case has been reported in the cardiovascular system to date.
Retained surgical gauze left inside the patient is sometimes called gossypiboma, a word that comes from the Latin gossypium (cotton) and the Swahili word boma (place of concealment), referred to as textiloma or gauzoma to indicate a foreign object retained in the body2. The biological reaction to a retained gauze is usually of two types. One type is aseptic fibrinous, which is a reaction to the foreign body that leads to the formation of granuloma and manifests as a mass3-8. The other type is an exudative reaction that leads to the formation of an abscess1, 4, 9, 10. Transmural migration might be observed in rare cases where the gauze remains adjacent to the gastrointestinal tract (GI) for a prolonged period1, 9, 10. No specific time has been mentioned for migration cases, but all the reported cases have been related to the GI and occurred after several years. The present case is the first report of erosion and transmural migration into the cardiovascular system throughout the world. It is also the first case of migration of a pulmonary artery band (PA band) into the pulmonary artery.
Case Presentation
The patient was a 14-month-old girl (weight 6900 gr) who was a candidate for PA banding at 8 months old (weight 3700 gr) due to failure to thrive with a diagnosis of Atrial Septal Defect (ASD) + Ventricular Septal Defect (VDS) + systemic pulmonary hypertension (confirmed with echocardiography and catheterization). Surgical staging was performed for the patient. She underwent left thoracotomy and a 2-mm wide PTFE band was inserted in the middle of her pulmonary artery around the artery, and after determining the appropriate size, it was fixed in place with two large metal clips.
After the operation, in the postoperative period, the only noticeable incident was a low-grade fever that lasted for a few days and was relieved with generic antibiotics after the surgery, and the child was discharged on the tenth day post-surgery. There were no problems in the follow-up examinations either.
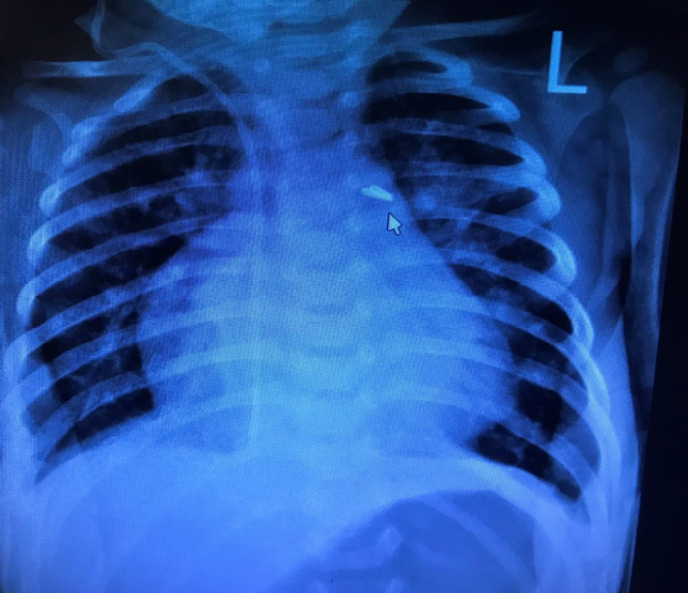
After six months, she was selected for total correction surgery. Figure 1 shows the location of the PA band metal clip in the patient’s CXR.
Figure 1.
The CXR of the patient before the second surgery; the location of the PAb and metal clips is marked with an arrow
After the necessary preparations, the child underwent surgery. Her sternum was opened from the middle. The thymic remnants were removed to access the heart and were then sent for pathological analysis. Adhesion had formed in the pericardium, which was released and removed. The aorta, IVC, and SVC were cannulated. Cardiopulmonary Bypass (CPB) was established to look for the PA band, which was not found. The entire pulmonary artery up to its junction and the right and left pulmonary arteries were completely dissected, its adhesions were broken and removed, and the artery was carefully examined.
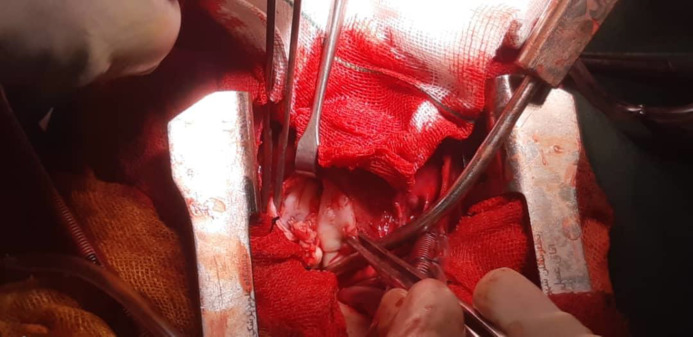
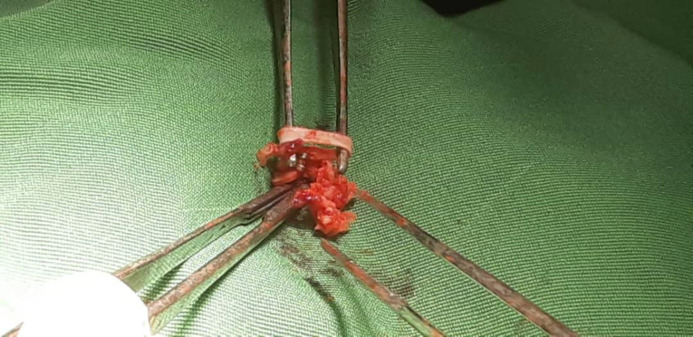
There were no blood or clots present. The PTFE bands and metal clips that were visible in the CXR (Figure 1) were not found on site. The patient was brought down to a temperature of 32°C, the aorta was clamped, and blood cardioplegia was injected, which was repeated every 20 minutes. The right atrium was opened. The ASD had a size of 1x1 cm and the VSD was also large, with a size of 3x3 cm. The tricuspid and mitral valves were checked and found to be healthy. VSD was repaired with a Gore-Tex patch, and ASD with a pericardial patch. Since the PA band could not be found, although the pulmonary size was larger than normal, the pulmonary artery was opened longitudinally. The PA band and its two metal clips had migrated into the lumen of the pulmonary artery (Figure 2). The PA band was intact and fully circular (Figure 3). The inner surface of the pulmonary artery had become uneven due to the PA band erosion and its migration into the pulmonary artery, but its false wall and the uneven surface inside the pulmonary artery were resected, and the pulmonary artery was then repaired end to end. Ventilation was performed, the patient was warmed up, the aortic clamp was opened, the CPB was separated without any problems, and the heart surgery was completed.
Figure 2.
The PA band eroded into the pulmonary artery is marked with an arrow. The opened edges of the pulmonary artery are also shown clamped with two Pinzette forceps
Figure 3.
The PA band removed from inside the pulmonary arteryremains fully intact and circular
In the ICU, the patient was extubated without any problems and the post-treatment process ended without any incidents. The PA band was sent to the laboratory for fungi and bacteria culture. The child was transferred to the pediatric ward on the fifth day after the surgery to continue her treatment and was discharged after completing the treatment.
She recovered after the surgery and did not show any problems in the 2.5-year follow-up.
Discussion
The surgical instruments that the surgeon implants in the body are sometimes permanent and are used as a long-term treatment, similar to orthopedic prostheses and artificial heart valves; sometimes, however, they are implanted temporarily as a stage of treatment to prepare the body to endure the next stage of the treatment.
One of the practices in staged heart surgery is the implanting of an unabsorbable band around the pulmonary artery that leads to the narrowing of the pulmonary artery to a certain extent, and after a few months when the heart has been trained, the pulmonary artery pressure has dropped and the heart has become capable of tolerating full recovery, the patient undergoes total correction and the PA band is opened and removed from around the pulmonary artery (in such cases, these surgeries are called staged surgeries performed for large VSDs). In such cases, a band of non-absorbable material (often a strip made of PTFE) is strapped around the pulmonary artery and tightened according to guidelines so that the right ventricle of the heart is put under certain pressure. After about six months, when the heart is adequately trained and the pulmonary artery pressure is reduced, the PA band is opened and the patient undergoes total correction surgery. PA band repair site surgery should also be performed based on the lesion that may remain in the pulmonary artery. The foreign object implanted in the body is of a non-absorbable and biologically-neutral material.
In many cases where the surgeon intentionally implants a foreign object in the body for treatment purposes, it usually does not cause a reaction in the surrounding tissues (e.g., orthopedic prostheses and artificial heart valves), but in cases where foreign objects are mistakenly left in the body, they can lead to abscess or reactions such as granulomas or gradually erode into the GI lumen1, 9. There is a difference between Retained Foreign Body (RFB) and gossypiboma. RFB refers to the presence of a tool in the patient’s body (usually gauze and long-gauze, towel, and surgical instruments), while gossypiboma is the product of the body’s reaction to a foreign object that has been gradually ingested by the body without the occurrence of perforation. For example, a piece of gauze left in the abdomen is gradually phagocytosed into the intestine by the intestine, later manifesting as intestinal obstruction without the occurrence of perforations1.
So far, all reports of the migration of RFBs have been related to non-cardiovascular systems and have usually been long-term, and most of the reported cases have been related to the gastrointestinal tract1, 4, 11, 12.
In rare cases where a Retained Foreign Body (RFB) has been reported following heart or thoracic surgery13, all have been caused by a piece of gauze left in the pericardial cavity, manifested as a mass in the pericardium between six and 11 years after surgery3, 6. Heart surgery stages in which a gauze was mistakenly retained in the body have been reported in both heart valve surgeries and Coronary Artery Bypass Graft (CABG) surgeries3, 5, 6, but no erosion or migration into the arteries or heart have ever been reported in these instances.
Overall, the authors’ patient was the first case with the migration of a biologically-neutral foreign body into the vascular system. Six months after its implantation, they found in the second surgery that the PA band had been removed. Its site was repaired, and the patient did not encounter any specific problems during the 2.5-year follow-up. Although no cause was found for this case, reports on future cases can help better identify the cause of this particular case as well.
Authors’ contributions
M.H was the head of the surgical team in charge of managing the complications in this patient. H.G was a member of the surgical team and helped with the data collection. S.A.M had a major contribution in the literature search and drafting of the discussion. H.G drafted the manuscript and provided administrative, technical, and material support. Z.A.A and M.H edited the final draft. All the writers contributed to editing the final draft and the approval of the manuscript.
Ethical considerations
The authors have observed ethical issues, including no plagiarism, no data fabrication, and no double publication. The patient gave informed consent for the publication of her data.
Competing interests
The authors declare that they have no competing interests.
Funding/support
The authors declare that they did not receive any funding for this study.
Informed Consent
Informed consent was taken from the patient.
Acknowledgments
The authors would like to express their gratitude to the staff of Shahid Modarres Hospital.
References
- 1.Aminian A. Gossypiboma: a case report. Cases J. 2008;1(1):1–3. doi: 10.1186/1757-1626-1-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alemu BN, Tiruneh AG. Gossypiboma: a case series and literature review. Ethiop J Health Sci. 2020;30(1):147–149. doi: 10.4314/ejhs.v30i1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Retnamma RK, Nair SG, Umadethan B, Manoj P. An unusual case of thoracic gossypiboma. Ann Card Anaesth. 2010;13(3):261 –3. doi: 10.4103/0971-9784.69059. [DOI] [PubMed] [Google Scholar]
- 4.Srivastava K, Agarwal A. Gossypiboma posing as a diagnostic dilemma: a case report and review of the literature. Case Rep Surg. 2014;2014:713428. doi: 10.1155/2014/713428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim DK, Hwang SK, Lee SC, Lee YJ, Jung JP, Park CR, et al. A 31-year-old pericardial textiloma. Cardiovasc J Afr. 2020;31(2):e5–e8. doi: 10.5830/CVJA-2019-068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sologashvili T, Kalangos A, Tissot-Daguette C, Myers PO. Incidental gossypiboma discovered during tricuspid valve re-repair 11 years after Ebstein anomaly repair. Heart Surg Forum. 2013;16(4):E216–8. doi: 10.1532/HSF98.20131015. [DOI] [PubMed] [Google Scholar]
- 7.Suliman H, Blickman J, Amrane A. Chest gossypiboma after coronary surgery. JBR-BTR. 2007;90(3):216–7. [PubMed] [Google Scholar]
- 8.Shahreza FD. From oxidative stress to endothelial cell dysfunction. J Prev Epidemiol. 2016;1(1):e04–e. [Google Scholar]
- 9.Pujahari A. Gossypiboma: Three cases. Trop Gastroenterol. 2010;31(3):217–8. [PubMed] [Google Scholar]
- 10.Dhillon JS, Park A. Transmural migration of a retained laparotomy sponge. Am Surg. 2002;68(7):603–5. [PubMed] [Google Scholar]
- 11.Yildirim S, Tarim A, Nursal TZ, Yildirim T, Caliskan K, Torer N, et al. Retained surgical sponge (gossypiboma) after intraabdominal or retroperitoneal surgery: 14 cases treated at a single center. Langenbecks Arch Surg. 2006;391(4):390–5. doi: 10.1007/s00423-005-0581-4. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad G, Attiq-ur-Rehman S, Anjum MZ. Retained sponge after abdominal surgery. J Coll Physicians Surg Pak. 2003;13(11):640–3. [PubMed] [Google Scholar]
- 13.Andronic D, Lupaşcu C, Târcoveanu E, Georgescu S. Gossypiboma-retained textile foreign body. Chirurgia (Bucur) 2010;105(6):767–77. [PubMed] [Google Scholar]