Abstract
Background
Injury to the abdomen can be blunt or penetrating. Abdominal injury can damage internal organs such as the liver, spleen, kidneys, intestine, and large blood vessels. There are controversies about the best approach to manage abdominal injuries.
Objectives
To assess the effects of surgical and non‐surgical interventions in the management of abdominal trauma in a haemodynamically stable and non‐peritonitic abdomen.
Search methods
We searched the Cochrane Injuries Group's Specialised Register, The Cochrane Library, Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R), EMBASE Classic+EMBASE (Ovid), ISI WOS (SCI‐EXPANDED, SSCI, CPCI‐S & CPSI‐SSH), CINAHL Plus (EBSCO), and clinical trials registers, and screened reference lists. We ran the most recent search on 17 September 2015.
Selection criteria
Randomised controlled trials of surgical interventions and non‐surgical interventions involving people with abdominal injury who were haemodynamically stable with no signs of peritonitis. The abdominal injury could be blunt or penetrating.
Data collection and analysis
Two review authors independently applied the selection criteria. Data were extracted by two authors using a standard data extraction form, and are reported narratively.
Main results
Two studies are included, which involved a total of 114 people with penetrating abdominal injuries. Both studies are at moderate risk of bias because the randomisation methods are not fully described, and the original study protocols are no longer available. The studies were undertaken in Finland between 1992 and 2002, by the same two researchers.
In one study, 51 people were randomised to surgery or an observation protocol. None of the participants in the study died. Seven people had complications: 5 (18.5%) in the surgical group and 2 (8.3%) in the observation group; the difference was not statistically significant (P = 0.42; Fischer's exact). Among the 27 people who had surgery, 6 (22.2%) surgeries were negative laparotomies, and 15 (55.6%) were non‐therapeutic.
In the other study, 63 people were randomised to diagnostic laparoscopy (surgery) or an observation protocol. There were no deaths and no unnecessary surgeries in either group. Four people did not receive the intervention they were assigned. There was no difference in therapeutic operations between the two groups: 3 of 28 in the diagnostic laparoscopy group versus 1 of 31 in the observation protocol group (P = 0.337).
Authors' conclusions
Based on the findings of 2 studies involving a total of 114 people, there is no evidence to support the use of surgery over an observation protocol for people with penetrating abdominal trauma who have no signs of peritonitis and are stable.
Keywords: Humans; Watchful Waiting; Abdominal Injuries; Abdominal Injuries/surgery; Abdominal Injuries/therapy; Laparoscopy; Randomized Controlled Trials as Topic; Wounds, Nonpenetrating; Wounds, Nonpenetrating/surgery; Wounds, Nonpenetrating/therapy; Wounds, Penetrating; Wounds, Penetrating/surgery; Wounds, Penetrating/therapy
Plain language summary
Surgery versus observation for people with abdominal injury
Injury to the abdomen is common and can be blunt from road traffic crashes or falls, or penetrating from gun shots or stabbing. These injuries are usually associated with injury to the abdominal organs such as the liver, spleen, kidneys, intestine and its covering, and big blood vessels. Massive bleeding or leakage of abdominal content into the abdominal cavity can occur, which may threaten a person's life. Examination of the patient by the doctor (physical examination), though the most accurate method of assessing people, is insufficient to determine the extent of damage. On the other hand, a person should not have a surgical procedure unless it is necessary. There are reports that injuries can be missed even when surgery is carried out.
Observing a patient with the hope that the person's injury heals naturally and intervening surgically if the need arises is known as selective non‐operative management (SNOM) or observation. An observation protocol is used when the person has no sign of internal bleeding or abdominal infection (peritonitis). Surgery is resorted to if, during observation, signs of bleeding or infection are observed.
The authors of this review sought to identify every study where people with an abdominal injury were randomised to surgery or observation. The authors searched a variety of medical databases but only identified 2 studies, involving 51 and 63 people respectively, both of which took place in Finland and were conducted by the same researchers. Both studies included people with penetrating abdominal injuries, from having been stabbed. The review authors considered both studies to be at moderate risk of bias, since only part of the randomisation process was described and the study protocols were not available to enable full assessment of overall quality.
In one study (1992‐1994) people received either an observation protocol or mandatory surgery. None of the people in the study died, and there was no difference in the number of people with medical complications between the study groups. One of the harms mentioned by the study authors was that surgery was performed on some people who did not actually need it. Unnecessary surgery can subject people to potential complications.
In the other study (1997‐2002) people received an observation protocol or diagnostic laparoscopy (minimal surgery). No one died in either group, and there were no differences between the groups in the number of surgeries needed. There were no unnecessary surgeries in either group.
Based on the findings of these two small studies, there is no evidence to support the use of surgical management over an observation protocol for people with abdominal trauma showing no signs of bleeding or infection.
The authors recommend that future randomised controlled studies clearly report the type of injury, number of damaged organs, extent of damage of internal organs, and complications in the people included.
Background
Description of the condition
Injury is a leading cause of morbidity and mortality worldwide. The most common causes of injury are falls from heights, road traffic crashes, and gun shot and stab wounds (Kahn 2006).
Injury to the abdomen can be blunt or penetrating. The most common cause of blunt abdominal trauma (BAT) is road traffic crashes (Kahn 2006). Other causes of BAT include pedestrian crashes and falls from heights (Anjum 2001). Penetrating abdominal trauma (PAT) may be caused by gun shots or stab wounds from piercing instruments. Most injuries to the abdomen are blunt injuries (Kahn 2006) and are associated with higher risk of death because the extent of injury is less obvious compared with penetrating injury (Anjum 2001).
Abdominal injuries are usually associated with injury to internal organs such as the liver, spleen, kidneys, the covering of the intestine and large blood vessels, and subsequent intra‐abdominal haemorrhage. Sometimes the extent of injury may not be readily obvious, particularly for blunt abdominal injuries. Severe bleeding may present with signs of haemodynamic instability: people may have a weak pulse, low blood pressure or be in a state of shock. Quite often these signs of internal injury may delay in manifesting clinically (Poletti 2004). Initial physical examination has been found to be unreliable for detecting people at risk of serious abdominal injury (Mackersie 1989; Hoff 2002). However, serial physical examination by experienced clinicians has been found to be reliable in detecting abdominal injuries in PAT (Como 2010).
Description of the intervention
The modality of management of people with abdominal injury depends on the severity of injuries incurred and the haemodynamic state of the person. Diagnosis of associated injuries in abdominal trauma presents a great challenge, even to the best of trauma surgeons (Hoff 2002; Radwan 2006). There are reports that physical examinations, though the most important assessment for intervention, are inaccurate (Hoff 2002). Consequently, clinically significant injuries may be missed. This dictates the need for active management of cases by surgical intervention. It has been observed, however, that injured organs may not be identified despite surgery (Jo 2007).
Recently, observation protocols have been adopted to avoid unnecessary surgery for both PAT (Demetriades 2006; Navsaria 2007) and BAT (Holmes 2005; Kahn 2006; Velmahos 2003). One approach involves selecting people based on their haemodynamic state and absence of peritonitis. People with signs of blood loss (haemodynamic instability) undergo surgery, while surgery is delayed for people in a stable condition until signs of blood loss or peritonitis are apparent.
Why it is important to do this review
Some experts oppose an observation protocol, arguing that this leads to delayed management of hollow viscous and mesenteric injuries (Yegiyants 2006). Other experts support this approach. They argue that avoiding unnecessary surgical intervention spares the person the consequences of metabolic response to surgical trauma and possible intra‐ and post‐operative complications (Basile 2006).
To have evidence for practice, there is a need for a synthesis of the evidence on the active surgical management and an observation protocol for the two types of abdominal trauma: blunt abdominal trauma (BAT) and penetrating abdominal trauma (PAT).
Objectives
To assess the effects of surgical interventions and non‐surgical interventions in the management of abdominal trauma in a haemodynamically stable and non‐peritonitic abdomen.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Any person with abdominal trauma who is haemodynamically stable and with no sign of peritonitis. The abdominal injury could be blunt or penetrating.
Types of interventions
Surgical (operative) versus non‐surgical (observation) interventions.
Types of outcome measures
Primary outcomes
Mortality at final follow‐up.
Secondary outcomes
Need for rescue intervention (blood transfusion, surgical intervention, etc);
Morbidity (infection, shock, etc).
Search methods for identification of studies
In order to reduce publication and retrieval bias we did not restrict our search by language, date or publication status.
Electronic searches
The Cochrane Injuries Group's Trial Search Co‐ordinator searched the following:
Cochrane Injuries Group specialised register (17 September 2015);
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library) (Issue 8 of 12, 2015);
Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R) (1946 to 17 September 2015);
EMBASE Classic + EMBASE (OvidSP) (1947 to 17 September 2015);
CINAHL Plus (EBSCO) (1937 to 17 September 2015);
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to 17 September 2015);
ISI Web of Science: Conference Proceedings Citation Index‐Science (CPCI‐S) (1990 to 17 September 2015);
PubMed (17 September 2015).
Search strategies are reported in Appendix 1.
Searching other resources
We checked the reference lists of all relevant studies and reviews to identify further studies. We also searched the Internet and the following trial registers to January 2012:
Current Controlled Trials (www.controlled‐trials.com);
Clinicaltrials.gov (www.clinicaltrials.gov).
Data collection and analysis
The Cochrane Injuries Group's Trials Search Co‐ordinator ran the searches and collated the results before passing them on to the authors for screening.
Selection of studies
Two authors screened the results independently using the inclusion criteria published in this systematic review's protocol (Oyo‐Ita 2008), to identify eligible studies. There was no disagreement on the inclusion of studies. For the first version of the review UU and IAI screened the search results. For the 2015 update, PC and AO screened the search results.
Data extraction and management
Data extraction was carried out using a standard extraction form. Two authors (UU and IAI in 2012; PC in 2015) extracted the data and one author (AO) cross‐checked for errors and completion. As data from the two included studies could not be combined, data were not entered into Review Manager for meta‐analysis as had originally been planned.
Assessment of risk of bias in included studies
Two authors (UU and IAI in 2012; PC and AO in 2015) independently assessed the methodological quality of the included studies. Methodological quality was assessed based on the following criteria: method of generation of the randomisation sequence, concealment of the randomisation sequence, incomplete outcome data, selective reporting, and other sources of bias. The review authors gave a judgement of 'high', 'low' or 'unclear' risk of bias, as outlined in theCochrane Handbook (Higgins 2011). Blinding of participants and treating physicians is not possible for the interventions studied in this review, therefore blinding was not included in the 'Risk of bias' assessment.
Assessment of heterogeneity
Both studies had an observation protocol (which the study authors called 'expectant non‐operative management') as the control arm, but different intervention arms. Due to heterogeneity of the interventions, study results are presented separately and in narrative format.
Assessment of reporting biases
We contacted the study researcher (personal communication, Leppäniemi 2003b), who provided a full response to our request for information. According to Dr. Leppäniemi it was the policy of the hospital ethics committee that the study information and data be destroyed upon publication of the results. As the study protocols have been destroyed it is not possible to assess reporting bias.
Data synthesis
The results of the studies are presented separately, in narrative format.
Sensitivity analysis
There were insufficient data included in the review to enable a sensitivity analysis to be performed.
Results
Description of studies
Results of the search
The electronic search for studies identified 1635 records. Eight potentially‐eligible studies were evaluated in full‐text and two studies (Leppäniemi 1996 and Leppäniemi 2003b) met the inclusion criteria (Figure 1).
1.
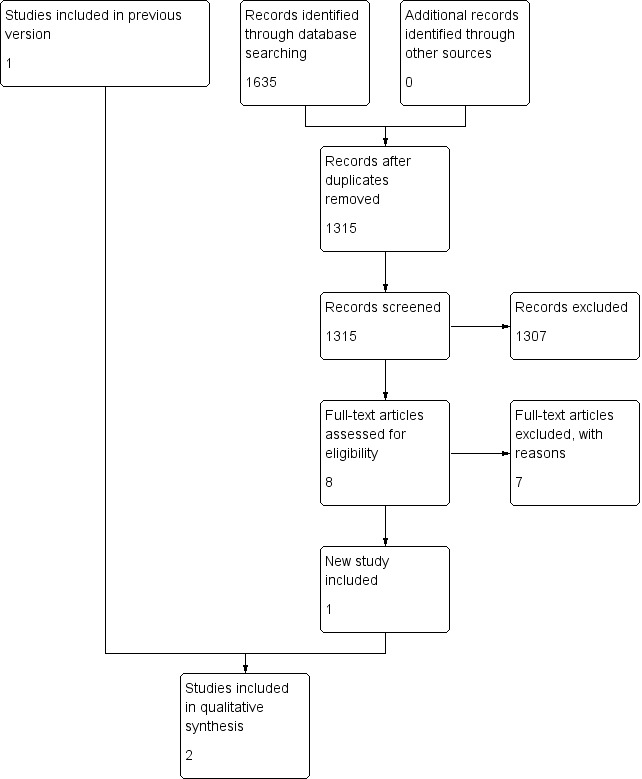
Study flow diagram.
Included studies
Two studies (Leppäniemi 1996; Leppäniemi 2003b) are included in this review.
The first (Leppäniemi 1996) was carried out between 1 March 1992 and 3 July 1994 in Finland and included any person with an abdominal or lower thoracic stab injury received in the preceding 48 hours. Abdominal or lower thoracic was defined as the area bounded anteriorly and laterally by the fifth intercostal space, posteriorly by the inferior tip of the scapular, caudally and anteriorly by the inguinal creases and laterally and posteriorly by the iliac bone crests. A person with suspected peritoneal penetration who did not require immediate laparotomy was randomised using a sealed opaque envelope to either mandatory laparotomy or the observation protocol. A person randomised to receive mandatory surgery was operated on immediately. A person in the observation protocol was physically examined every 2 hours for the first 6 hours, then every 12 hours for at least 48 hours. Twenty seven people were randomised to the surgery group and 24 to the observation group; 74% and 83% were males in the surgery and observation groups respectively.
On admission, the following tests were carried out on people in the observation group: haemoglobin level, urine amylase, urine blood, chest and plain abdominal radiographs. Investigations six hours after admission included haemoglobin level and contrast‐enhanced computed tomography. No antibiotics were given to either group except when wound contamination was suspected. A person was observed for 48 hours if there was no need for intervention. A person was required to return for follow up 4 to 6 weeks after the injury and later if necessary. The main outcomes studied included early morbidity (for complications within the initial hospital stay or within 90 days of the injury) and length of hospital stay (including readmission for complications within 90 days of the injury).
The second study (Leppäniemi 2003b) was carried out in Finland from May 1997 to January 2002. Fifty‐nine people with equivocal peritoneal violation on local wound exploration were randomised to diagnostic laparoscopy or an observation protocol. While the laparoscopy was restricted to diagnostic purposes, we considered it to be a surgical intervention as the technique of laparoscopy involves the making of an incision. (This study also included another arm not relevant to this review (Leppäniemi 2003a) in which people who were stable and without peritonitis but who had demonstrated peritoneal violation were randomised to one or other of two surgical interventions ‐ exploratory laparotomy or diagnostic laparoscopy). The number of people randomised to diagnostic laparotomy and observation were 28 and 31 respectively. Males accounted for 89% of people in the diagnostic laparoscopy group and 87% of people in the observation group.
The observation protocol (expectant non‐operative management) was performed according to the hospital's previously published guidelines. Diagnostic laparoscopy was performed in the operating room under general anaesthesia after insertion of a nasogastric tube and a Foley catheter. Pneumoperitoneum was created through an infra‐umbilical incision using a Veress needle or open technique, and air leakage from the stab wound was controlled with sutures, if needed. Special attention was paid to the possibility of a tension pneumothorax developing during the procedure. A 10‐mm port was inserted and a 30‐degree laparoscope used for abdominal exploration starting with the identification of peritoneal violation at the stab wound site followed by systematic exploration of the abdominal contents using the person's position.
Excluded studies
Ten studies (Bitseff 1984; Croce 1995; Demetriades 2006; Heyns 1992; Karateke 2013; Leppäniemi 2003a; Liebenberg 1988; Sherman 1994; Velmahos 2003; Yucel 2014) were excluded from the review; nine of them were prospective observational studies. One (Leppäniemi 2003a) was a randomised trial that compared two surgical interventions (diagnostic laparoscopy and exploratory laparotomy).
Risk of bias in included studies
Figure 2 shows the 'Risk of bias' assessments of the two included studies.
2.
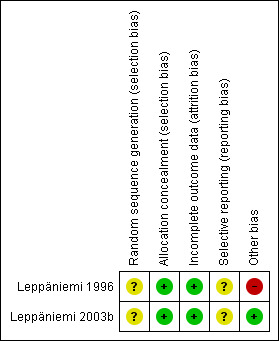
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Sequence generation (selection bias)
There was no mention of how the randomisation sequence was generated in either of the two included studies.
Allocation
Allocation was concealed by use of sealed opaque envelopes in the two included studies.
Incomplete outcome data
In Leppäniemi 1996 all 51 people who were randomised completed the study, and there were complete data on the outcomes sought for this review. Data were collected on people for 90 days following their injury.
In Leppäniemi 2003b of the 63 people randomised there were 4 dropouts; 3 were associated with protocol violation and 1 person refused consent. The published report states "two underwent a nontherapeutic laparotomy and one was treated nonoperatively; all three people recovered without complications." (p.637) As the report does not specify to which study group these people were randomised, it is not possible to analyse the data on an intention‐to‐treat basis. Data are presented for the remaining 59 people only, on a per‐protocol basis. The duration of the post‐injury follow‐up period is not reported in this study.
Selective reporting
We were unable to assess selective reporting as the protocols of both included studies were destroyed following publication of the results, which was stated as being in accordance with the requirements of the researchers' institutional review board.
Other potential sources of bias
In Leppäniemi 1996 people in the observation group were monitored more closely than people in the surgical group.
In Leppäniemi 2003b there were statistically significant differences between groups at baseline in terms of injury severity scores and abdominal trauma index, which were higher in the diagnostic laparoscopy group.
Effects of interventions
Primary outcome
Mortality
No one died in either of the included studies.
Secondary outcomes
Need for rescue intervention
Leppäniemi 1996: Four (16.7%) of the 24 people in the observation group required surgical intervention. (Therefore, 20 (83.3%) of the 24 people in the observation group were successfully managed conservatively). Two people developed peritonitis from a perforated colon 6 and 18 hours, respectively, after admission. One person had an intra‐abdominal haemorrhage from a lacerated liver 44 hours after admission. The fourth patient was initially discharged 3 days after admission but was readmitted 52 days after discharge with pleural empyema. At surgery, a perforated stomach that had herniated through a laceration in the diaphragm was seen.
Leppäniemi 2003b: There was no significant difference in therapeutic operations between the two groups: 3 of 28 in the diagnostic laparoscopy group versus 1 of 31 in the observation group (P = 0.337).
Morbidity
Leppäniemi 1996: Five of 27 (18.5%) people in the surgical group and 2 of 24 (8.3%) people in the observation group had early morbidity. The difference was not statistically significant, P = 0.42 (Fischer's exact). The complications in the surgical group were pulmonary atelectasis, intestinal obstruction, delirium, biliary fistula and pneumonia, delayed splenic rupture, pancreatic fistula and pleural effusion. Two people in the observation group had superficial thrombophlebitis, pleural empyema, candida pleuritis and wound infection.
Leppäniemi 2003b: There was no difference in morbidity between the two groups: 3 of 28 in the diagnostic laparoscopy group versus 0 of 31 in the observation group (P = 0.101).
Unnecessary surgeries
Leppäniemi 1996: In the surgical group, 15 of 27 (56%) laparotomies were non‐therapeutic. Non‐therapeutic laparotomy was defined as an operation involving the opening of the peritoneal cavity that indicated minimal injuries with no need for active surgical management. Also considered non‐therapeutic was evacuation of non‐contaminated blood from the peritoneal cavity. The management of stab injuries in the abdominal wall without the need for opening the peritoneal cavity does not meet the definition of laparotomy. Six of the 12 (50%) therapeutic surgeries were also said to be unnecessary as they involved arrest of minimal bleeding which could have been managed conservatively.
Leppäniemi 2003b: The surgical group in this study was the group in which diagnostic laparoscopy was performed. There were no unnecessary surgeries in either this or the observation group.
Discussion
Summary of main results
Two small studies involving 51 and 63 people respectively were identified through the systematic search for studies. Both studies were at moderate risk of bias as only part of the randomisation process was described and we could not obtain the study protocols.
In the first study (Leppäniemi 1996), people with penetrating abdominal stab wounds were randomised to surgery or an observation protocol, and follow‐up was for 90 days following injury. No one taking part in the study died, and there was no difference in the number of people with complications between treatment groups.
In the second study (Leppäniemi 2003b), people with equivocal peritoneal violation on local wound exploration were randomised to diagnostic laparoscopic surgery or an observation protocol. The follow‐up period was not stated. No one taking part in the study died, no unnecessary surgeries were performed, and there was no statistically significant difference between the groups in morbidity or therapeutic surgery.
Based on the findings of two small studies, there is no evidence to support the use of surgery (including diagnostic laparoscopy) over an observation protocol for people with asymptomatic abdominal stab wounds.
Overall completeness and applicability of evidence
With the help of the Cochrane Injuries Group, we searched a variety of biomedical science databases, conference abstracts, trial registers and the Internet, and identified only 2 studies involving a total of 114 people. Clinical evidence on this topic is therefore incomplete.
Despite the lack of evidence from randomised controlled trials, an observation protocol for people with blunt abdominal injuries has been accepted as routine practice in some centres (Como 2010; Gibson 2006; Lenzini 2006; Miller 2002; Ozturk 2004; Schroeppel 2007).
Quality of the evidence
We assessed the studies as being at moderate risk of bias. The method of generating the randomisation sequence was not reported, but allocation concealment was through use of opaque envelopes. Blinding was not possible due to the nature of surgical studies. There was no loss to follow up in 1 trial and a loss of 4 (out of 63) people in the second trial. We were unable to assess selective reporting as we could not obtain the study protocols.
Agreements and disagreements with other studies or reviews
There are only two RCTs on this topic, and we did not come across any other systematic reviews of RCTs on this topic when screening the search results.
Experts generally support observation as the management of choice for both blunt and penetrating abdominal injuries, provided patients are asymptomatic. This is particularly so with the emerging new technologies used in damage‐control resuscitation and transvascular interventions in the management of blunt abdominal injury with associated spleen or liver injury (Stengel 2015). Diagnostic accuracy is required to select patients who should be managed with an observation protocol. The Eastern Association for the Surgery of Trauma (EAST) has developed a guideline for the screening of people with blunt abdominal trauma into observation and surgical groups (Hoff 2002).
In another publication, the EAST Practice Mangement Committee searched in PubMed for data published in English from 1960 to 2007 on non‐operative management of penetrating abdominal trauma, for the development of a guideline on selective management of penetrating abdominal trauma. Evidence for the guideline was from observational studies and one RCT. The guideline supports an observation protocol for the management of abdominal stab wounds that are haemodynamically stable and without peritonitis, but is inconclusive on the management of non‐tangential gun shot wounds that are asymptomatic (Como 2010). In abdominal stab wounds with eviscerated omentum in the haemodynamically stable patient, arguments exist for and against laparotomy versus an observation protocol (Como 2010). Some experts have recommended observation for omental evisceration without peritoneal signs (Huizinga 1987). Management of thoracoabdominal trauma also remains controversial (Parreira 2008). Though the diagnosis of diaphragmatic injury may be made with the use of new generation computerised tomography, there are questions on managing patients with an observation protocol using these technologies in view of the low risk of herniation and high risk of strangulation among those with herniation (Parreira 2008).
Authors' conclusions
Implications for practice.
With the availability of newer imaging technologies, the consensus on the management of patients with haemodynamically stable blunt abdominal injuries is in favour of observation. In 2 small RCTs involving 114 people included in this review, following an observation protocol for management of abdominal stab wounds was as good as immediate surgery (including diagnostic laparoscopic surgery).
Evidence is lacking for the management of asymptomatic peritoneal penetration with omental evisceration and thoracoabdominal trauma with diaphragmatic laceration. Trials are required to address these gaps.
Implications for research.
Future RCTs should provide data on whether the participants had:
single or multiple organ injury;
hollow viscous/mesenteric injury;
gun shot, stab, or other penetrating wounds;
a pre‐specified minimum period of follow up, particularly in the observation group.
What's new
| Date | Event | Description |
|---|---|---|
| 26 October 2015 | New search has been performed | The search was updated to September 2015. One new study is included in the review. This study was overlooked in the original version of the review (Oyo‐Ita 2012), but was identified following correspondence with the study author. |
| 26 October 2015 | New citation required and conclusions have changed | The review has been updated. Paul Chinnock has been added as an author. |
Acknowledgements
Dr. Udey Ugare contributed to the protocol and first version of this review as a co‐author.
We acknowledge the support of the Cochrane Injuries Group staff. Karen Blackhall designed the search for studies and Emma Sydenham provided technical and moral support to the review team.
This project was supported by the United Kingdom (UK) National Institute for Health Research (NIHR), through Cochrane Infrastructure funding to the Cochrane Injuries Group. The views and opinions expressed are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health.
Appendices
Appendix 1. Search strategies
Cochrane Injuries Group's Specialised Register (abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*) AND (trauma* or injur* or penetrat* or stab* or blunt* or wound*or perforat* or stab* or gunshot or shot) or (Hernia* and Trauma*) or ((Splenic or spleen or stomach or gastric) and (ruptur* or burst*)) Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library) #1MeSH descriptor: [Wounds, Gunshot] explode all trees #2MeSH descriptor: [Wounds, Stab] explode all trees #3MeSH descriptor: [Wounds, Penetrating] explode all trees #4MeSH descriptor: [Wounds, Nonpenetrating] explode all trees #5MeSH descriptor: [Multiple Trauma] explode all trees #6(multiple trauma or polytrauma):ab,ti #7#1 or #2 or #3 or #4 or #5 or #6 #8MeSH descriptor: [Abdomen] explode all trees #9MeSH descriptor: [Abdomen, Acute] explode all trees #10(abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*):ab,ti #11MeSH descriptor: [Abdominal Cavity] explode all trees #12#8 or #9 or #10 or #11 #13#7 and #12 #14MeSH descriptor: [Abdominal Injuries] explode all trees #15MeSH descriptor: [Liver] explode all trees and with qualifiers: [Injuries ‐ IN] #16#13 or #14 or #15 #17Hernia* near/5 Trauma*:ab,ti #18((abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*) near/3 (trauma* or injur* or penetrat* or stab* or blunt* or wound*or perforat* or stab* or gunshot or shot)):ab,ti #19(abdominal and compartment* and syndrome):ab,ti #20((Splenic or spleen or stomach or gastric) and (ruptur* or burst*)):ab,ti #21#16 or #17 or #18 or #19 or #20 #22(surgery or surgical*):ab,ti #23MeSH descriptor: [General Surgery] explode all trees #24MeSH descriptor: [Surgical Procedures, Minor] explode all trees #25MeSH descriptor: [Surgical Procedures, Minimally Invasive] explode all trees #26MeSH descriptor: [Surgical Procedures, Operative] explode all trees #27#22 or #23 or #24 or #25 or #26 #28#21 and #27 Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R) 1. wounds, gunshot/ 2. wounds, stab/ 3. wounds, penetrating/ 4. wounds, nonpenetrating/ 5. exp Multiple Trauma/ 6. (multiple trauma or polytrauma).ab,ti. 7. 1 or 2 or 3 or 5 or 6 8. exp Abdomen/ 9. exp Abdomen, Acute/ 10. exp Abdominal cavity/ 11. (abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta*).ab,ti. 12. 8 or 9 or 10 or 11 13. 7 and 12 14. exp Abdominal Injuries/ 15. exp Liver injuries/ 16. 13 or 14 or 15 17. ((Splenic or spleen or stomach or gastric) adj3 (ruptur* or burst*)).ab,ti. 18. (abdominal adj3 compartment* adj3 syndrome).ab,ti. 19. ((abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*) adj3 (trauma* or injur* or penetrat* or stab* or blunt* or wound*or perforat* or stab* or gunshot or shot)).ab,ti. 20. (Hernia* adj3 Trauma*).ab,ti. 21. 16 or 17 or 18 or 19 or 20 22. exp surgery/ 23. exp surgical procedures, operative/ 24. exp Surgical Procedures, Minor/ 25. exp Surgical Procedures, Minimally Invasive/ 26. (surgery or surgical*).ab,ti. 27. 22 or 23 or 24 or 25 or 26 28. 21 and 27 29. randomi?ed.ab,ti. 30. randomized controlled trial.pt. 31. controlled clinical trial.pt. 32. placebo.ab. 33. clinical trials as topic.sh. 34. randomly.ab. 35. trial.ti. 36. 29 or 30 or 31 or 32 or 33 or 34 or 35 37. (animals not (humans and animals)).sh. 38. 36 not 37 39. 28 and 38 EMBASE Classic + EMBASE (OvidSP) 1 exp Abdominal Injury/su, dt, th [Surgery, Drug Therapy, Therapy] 2 exp Abdominal Penetrating Trauma/ 3 exp Abdominal Blunt Trauma/ 4 exp Multiple Trauma/ 5 (multiple trauma or polytrauma).ab,ti. 6 exp Gunshot Injury/ 7 exp Stab Wound/ 8 4 or 5 or 6 or 7 9 *Abdomen/ 10 *Acute Abdomen/ 11 (abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*).ab,ti. (2294208) 12 9 or 10 or 11 13 8 and 12 14 1 or 2 or 3 or 13 15 ((Splenic or spleen or stomach or gastric) adj3 (ruptur* or burst*)).ab,ti. 16 (abdominal adj3 compartment* adj3 syndrome).ab,ti. 17 ((abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*) adj3 (trauma* or injur* or penetrat* or stab* or blunt* or wound*or perforat* or stab* or gunshot or shot)).ab,ti. 18 (Hernia* adj3 Trauma*).ab,ti. 19 14 or 15 or 16 or 17 or 18 20 (surgery or surgical*).ab,ti. 21 exp Abdominal Surgery/ 22 20 or 21 23 22 and 19 24 exp Randomized Controlled Trial/ 25 exp controlled clinical trial/ 26 randomi?ed.ab,ti. 27 placebo.ab. 28 *Clinical Trial/ 29 randomly.ab. 30 trial.ti. 31 24 or 25 or 26 or 27 or 28 or 29 or 30 32 exp animal/ not (exp human/ and exp animal/) 33 31 not 32 34 23 and 33 ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) & Conference Proceedings Citation Index‐Science (CPCI‐S)
# 11 #10 AND #9
# 10 #2 OR #1
# 9 #8 AND #7
# 8 TOPIC: (((surgery or surgical) NEAR/5 (abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver*))) NOT TOPIC: ((cancer* or carcinoma* or disease*))
# 7 #6 OR #5 OR #4 OR #3
# 6 TOPIC: ((abdominal NEAR/3 compartment*) OR (Hernia* NEAR/3 Trauma*))
# 5 TOPIC: (((Splenic or spleen or stomach or gastric or liver) NEAR/3 (ruptur* or burst*)))
# 4 TOPIC: (((abdominal or abdomen or liver) NEAR/3 (trauma* or injur* or penetrat* or stab* or blunt* or wound* or perforat* or stab* or gunshot or shot)))
# 3 TOPIC: ((("Multiple Trauma" or polytrauma or gunshot or stab* or blunt or penetrating or nonpenetrating) NEAR/3 (abdominal or abdomen or liver)))
# 2 TOPIC: (((clinical OR control* OR placebo OR random*) NEAR/3 (trial* or group* or study or studies or placebo or controlled)))
# 1 TOPIC: (((singl* OR doubl* OR trebl* OR tripl*) NEAR/3 (blind* OR mask*)))
CINAHL Plus (EBSCO)
1. (MH "Abdominal Injuries+") 2. (MM "Abdomen, Acute") 3. (MM "Wounds, Gunshot") 4. (MH "Wounds, Stab+") 5. (MH "Wounds, Penetrating+") 6. (MM "Multiple Trauma") 7. TX Multiple Trauma or polytrauma 8. 3 OR 4 OR 5 OR 6 OR 7 9. (MH "Abdomen+") 10. TX abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta or liver* 11. 9 OR 10 12. 8 AND 11 13. TI ( abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver ) and TI ( trauma* or injur* or penetrat* or stab* or blunt* or wound*or perforat* or stab* or gunshot or shot ) or AB ( abdominal or abdomen or stomach or gastric or diaphram* or spleen or splenic or colon or intestin* or pancreas or aortic or aorta* or liver ) and AB ( trauma* or injur* or penetrat* or stab* or blunt* or wound* or perforat* or stab* or gunshot or shot ) 14.TI ( Splenic or spleen or stomach or gastric ) and TI ( ruptur* or burst* ) or AB ( Splenic or spleen or stomach or gastric ) and AB ( ruptur* or burst* ) 15.TX abdominal N3 compartment* N3 syndrome 16.1 or 2 or 12 or 13 or 14 or 15 17.(MH "Surgery, Operative+") or (MH "Surgery Outside the OR") 18.TX surgery or surgical 19.17 or 18 20.16 and 19 21.MH clinical trials 22.PT clinical trial* 23.TX clinical N3 trial* 24.TI ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) or (tripl* N3 blind*) ) or TI ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) or AB ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) ) or AB ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) 25.TX randomi?ed N3 control* N3 trial* 26.MH placebos 27.TX placebo* 28.MH random assignment 29.TX random* N3 allocat* 30.MH quantitative studies 31.21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 32. 20 and 31 PubMed ((pubmednotmedline [sb] OR (pubstatusnihms OR pubstatuspmcsd AND publisher [sb]))) AND ((((((((("Comparative Study"[Publication Type]) OR "Randomized Controlled Trial"[Publication Type]) OR "Controlled Clinical Trial"[Publication Type])) OR (((((((randomized[Title/Abstract]) OR randomised[Title/Abstract]) OR placebo[Title/Abstract]) OR randomly[Title/Abstract]) OR trial[Title/Abstract]) OR groups[Title/Abstract]) OR group[Title/Abstract]))) NOT (("Animals"[Mesh]) NOT ("Animals"[Mesh] AND "Humans"[Mesh])))) AND (((((("surgery"[Title/Abstract]) OR "surgical"[Title/Abstract])) OR ((("Surgical Procedures, Operative"[Mesh]) OR "Surgical Procedures, Minor"[Mesh]) OR "Surgical Procedures, Minimally Invasive"[Mesh]))) AND (((((("Abdominal Injuries"[Mesh:NoExp]) OR ((((((abdominal[Title/Abstract] or abdomen[Title/Abstract] or stomach[Title/Abstract] or gastric[Title/Abstract] or diaphram*[Title/Abstract] or spleen[Title/Abstract] or splenic[Title/Abstract] or colon[Title/Abstract] or intestin*[Title/Abstract] or pancreas[Title/Abstract] or aortic[Title/Abstract]or aorta*[Title/Abstract]))) OR ((("Abdomen"[Mesh:NoExp]) OR "Abdomen, Acute"[Mesh]) OR "Abdominal Cavity"[Mesh:NoExp]))) AND (((((("Wounds, Gunshot"[Mesh]) OR "Wounds, Stab"[Mesh:NoExp]) OR "Wounds, Penetrating"[Mesh:NoExp]) OR "Multiple Trauma"[Mesh])) OR (("multiple trauma"[Title/Abstract]) OR "polytrauma"[Title/Abstract]))))) OR ((rupture[Title/Abstract]) AND (Splenic[Title/Abstract] or spleen[Title/Abstract] or stomach[Title/Abstract] or gastric[Title/Abstract]))) OR "abdominal compartment syndrome"[Title/Abstract]) OR (((trauma*[Title/Abstract] or injur*[Title/Abstract] or penetrat*[Title/Abstract] or stab*[Title/Abstract] or blunt*[Title/Abstract] or wound*[Title/Abstract] or perforat*[Title/Abstract] or stab*[Title/Abstract] or gunshot[Title/Abstract] or shot[Title/Abstract])) AND (abdominal[Title/Abstract] or abdomen[Title/Abstract] or stomach[Title/Abstract] or gastric[Title/Abstract] or diaphram*[Title/Abstract] or spleen[Title/Abstract] or splenic[Title/Abstract] or colon[Title/Abstract] or intestin*[Title/Abstract] or pancreas[Title/Abstract] or aortic[Title/Abstract] or aorta*[Title/Abstract] or liver*[Title/Abstract]))))) The following source was not searched after 2012
ZETOC abdom* inj* surg* random* abdom* trauma* surg* random*
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Leppäniemi 1996.
| Methods | Randomised controlled trial | |
| Participants | People with abdominal or lower thoracic stab wounds, who were injured in the preceding 48 hours | |
| Interventions | Mandatory laparotomy versus selective non‐operative management | |
| Outcomes | 90‐day mortality, morbidity, length of hospital stay and cost of care | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation is not stated |
| Allocation concealment (selection bias) | Low risk | Allocation concealed in sealed opaque envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no incomplete outcome data |
| Selective reporting (reporting bias) | Unclear risk | We contacted the study authors but were unable to obtain the study protocol in order to assess selective reporting. The authors say: "Indeed, there was a study protocol (in Finnish) but ...I... have destroyed the paper trail after the study was published (as required by our ethics committee instructions)." Personal communication from Ari Leppaniemi 6 October 2012 |
| Other bias | High risk | The non‐surgical intervention group was monitored more closely than the surgical group |
Leppäniemi 2003b.
| Methods | Randomised controlled trial | |
| Participants | People with equivocal peritoneal violation on local wound exploration. | |
| Interventions | Diagnostic laparoscopy versus expectant non‐operative management | |
| Outcomes | Hospital morbidity, therapeutic operations, days of hospital stay, hospital costs, sick leave requirements | |
| Notes | Study also included another arm not relevant to this review (Leppäniemi 2003a), in which stable patients without peritonitis but with demonstrated peritoneal violation were randomised to one or other of two surgical interventions ‐ exploratory laparotomy or diagnostic laparoscopy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation is not stated |
| Allocation concealment (selection bias) | Low risk | Allocation concealed in sealed opaque envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no incomplete outcome data |
| Selective reporting (reporting bias) | Unclear risk | We contacted the study authors but were unable to obtain the study protocol in order to assess selective reporting. The authors said, regarding the protocol, that the same applied as for their previous study, i.e.: "Indeed, there was a study protocol (in Finnish) but ...I... have destroyed the paper trail after the study was published (as required by our ethics committee instructions)." Personal communication from Ari Leppaniemi 6 October 2012 |
| Other bias | Low risk | Some differences in patient characteristics were significant ‐ injury severity scores |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bitseff 1984 | Prospective observational study |
| Croce 1995 | Prospective observational study |
| Demetriades 2006 | Prospective observational study |
| Heyns 1992 | Prospective observational study |
| Karateke 2013 | Prospective non‐randomised study comparing two surgical techniques ‐ diagnostic laparoscopy and exploratory laparotomy |
| Leppäniemi 2003a | Compares two surgical techniques ‐ diagnostic laparoscopy and exploratory laparotomy |
| Liebenberg 1988 | Prospective observational study |
| Sherman 1994 | Prospective observational study |
| Velmahos 2003 | Prospective observational study |
| Yucel 2014 | Prospective observational study |
Differences between protocol and review
In the protocol (Oyo‐Ita 2008) the methodological quality of included studies was planned to be measured in terms of: assessment of method of random allocation of people to care, quality of care rendered to the treatment and control groups, the extent of loss to follow‐up and outcome assessment. In the completed review the current 'Risk of bias' criteria (Higgins 2011) were used to assess the methodological quality of the included studies. We did not perform handsearching as part of the search for studies.
Contributions of authors
2012 version (Oyo‐Ita 2012): IAI and UU screened the titles and abstracts of potentially relevant studies. They also applied the inclusion criteria independently and selected the papers to be included in the review. Data extraction and assessment of the risk of bias were done by AO and UU. AO wrote the manuscript and IAI and UU commented on the draft of the review.
2015 version: AO and PC screened the abstracts and applied the inclusion criteria independently to select potentially relevant studies. PC extracted data from the one new study and assessed the risk of bias. PC wrote the draft update which was reviewed by AO and IAI.
Declarations of interest
None known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Leppäniemi 1996 {published data only}
- Leppäniemi AK. Protocol request [personal communication]. Email to: Emma Sydenham 6 October 2012.
- Leppäniemi AK, Haapiainen RK. Selective nonoperative management of abdominal stab wounds: prospective randomized study. World Journal of Surgery 1996;20(8):1101‐6. [DOI] [PubMed] [Google Scholar]
Leppäniemi 2003b {published data only}
- Leppäniemi A, Haapiainen R. Diagnostic laparoscopy in abdominal stab wounds: a prospective, randomized study. Journal of Trauma, Injury, Infection, and Critical Care 2003;55:636–45. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bitseff 1984 {published data only}
- Bitseff EL, Adkins RB Jr. Splenic trauma: a trial at selective management. South African Medical Journal 1984;77(10):1286‐90. [PubMed] [Google Scholar]
Croce 1995 {published data only}
- Croce MA, Fabian TC, Menke PG, Waddle‐Smith L, Minard G, Kudsk KA, et al. Nonoperative management of blunt hepatic trauma is the treatment of choice for hemodynamically stable patients: Results of a prospective trial. Annals of Surgery 1995;221(6):744‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Demetriades 2006 {published data only}
- Demetriades D, Hadjizacharia P, Constantinou C, Brown C, Inaba K, Rhee P, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Annals of Surgery 2006;244(4):620‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heyns 1992 {published data only}
- Heyns CF, Vanvollenhoven P. Selective surgical‐management of renal stab wounds. British Journal of Urology 1992;69(4):351‐7. [DOI] [PubMed] [Google Scholar]
Karateke 2013 {published data only}
- Karateke F, Ozdogan M, Ozyazici S, Das K, Menekse E, Gulnerman YC, et al. The management of penetrating abdominal trauma by diagnostic laparoscopy: a prospective non‐randomized study [Penetran karin travmalarinin tanisal lapararoskopi ile yonetimi: Prospektif randomize olmayan calisma]. Ulusal Travma ve Acil Cerrahi Dergisi 2013;9(1):53‐7. [DOI] [PubMed] [Google Scholar]
Leppäniemi 2003a {published data only}
- Leppäniemi A, Haapiainen R. Diagnostic laparoscopy in abdominal stab wounds: a prospective, randomized study. Journal of Trauma: Injury, Infection, and Critical Care 1993;55:636‐45. [DOI] [PubMed] [Google Scholar]
Liebenberg 1988 {published data only}
- Liebenberg ND, Maasch AJ. Penetrating abdominal wounds‐‐a prospective trial of conservative treatment based on physical signs. South African Medical Journal 1988;74(5):231‐3. [PubMed] [Google Scholar]
Sherman 1994 {published data only}
- Sherman HF, Savage BA, Jones LM, Barrette RR, Latenser BA, Varcelotti JR, et al. Nonoperative management of blunt hepatic injuries ‐ safe at any grade. Journal of Trauma‐Injury Infection and Critical Care 1994;37(4):616‐21. [DOI] [PubMed] [Google Scholar]
Velmahos 2003 {published data only}
- Velmahos GC, Toutouzas KG, Radin R, Chan L, Demetriades D. Nonoperative treatment of blunt injury to solid abdominal organs: a prospective study. Archives of Surgery 2003;138(8):844‐51. [DOI] [PubMed] [Google Scholar]
Yucel 2014 {published data only}
- Yucel M, Ozpek A, Yuksekdag S, Kabak I, Basak F, Kilic A, et al. The management of penetrating abdominal stab wounds with organ or omentum evisceration: the results of a clinical trial. Ulusal cerrahi dergisi 2014;30:207‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Anjum 2001
- Anjum Fazili MS, Shabana Nazir MB. Clinical profile and operative management of blunt abdominal trauma (BAT): A retrospective one‐year experience at SMHS hospital, Kashmir, India. JK ‐ Practitioner (International Journal of Current Medical Science and Practice) 2001;8(4):219‐21. [Google Scholar]
Basile 2006
- Basile G, Chiarenza S, DiMari P, Primus A, Boscarelli G, Buffone A, et al. The treatment of blunt abdominal trauma. Personal experience. Annali Italiani Chirurgia 2006;77(2):149‐54. [PubMed] [Google Scholar]
Como 2010
- Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. Journal of Trauma 2010;68:721‐33. [DOI] [PubMed] [Google Scholar]
Gibson 2006
- Gibson DE, Canfield CM, Levy PD. Selective non‐operative management of blunt abdominal injury. Journal of Emergency Medicine 2006;31(2):215‐21. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated March 2011]. The Cochrane Collaboration. Available from www.cochrane‐handbook.org.
Hoff 2002
Holmes 2005
- Holmes JH 4th, Wiebe DJ, Tataria M, Mattix KD, Mooney DP, Scaife ER. The failure of nonoperative management in pediatric solid organ injury: a multi‐institutional experience. Journal of Trauma 2005;59(6):1309‐13. [DOI] [PubMed] [Google Scholar]
Huizinga 1987
- Huizinga WKJ, Baker LW, Mtshall ZW. Selective management of abdominal and thoracic stab wounds with established peritoneal penetration: the eviscerated omentum. The American Journal of Surgery 1987;153(6):564‐8. [DOI] [PubMed] [Google Scholar]
Jo 2007
- Jo K, Bjerke H. Abdominal trauma, penetrating. www.emedicine.com (accessed 12 June 2007).
Kahn 2006
- Khan JS, Iqbal N, Gardezi JR. Pattern of visceral injuries following blunt abdominal trauma in motor vehicular accidents. Journal of College of Physicians and Surgeons 2006;16(10):645‐7. [DOI] [PubMed] [Google Scholar]
Lenzini 2006
- Lenzini MM. Nonoperative management of penetrating abdominal trauma. Journal of the American Academy of Physician Assistants 2006;19(7):52‐6. [DOI] [PubMed] [Google Scholar]
Mackersie 1989
- Mackersie RC, Tiwary AD, Shackford SR, Hoft DB. Intraabdominal injury following blunt trauma. Identifying the high‐risk patient using objective risk factors. Archives of Surgery 1989;124(7):809‐13. [DOI] [PubMed] [Google Scholar]
Miller 2002
- Miller PR, Croce MA, Bee TK, Malhotra AK, Fabian TC. Associated injuries in blunt solid organ trauma: implications for missed injury in non‐operative management. Journal of Trauma 2002;53(2):238‐48. [DOI] [PubMed] [Google Scholar]
Navsaria 2007
- Navsaria PH, Berli JU, Edu S, Nicol AJ. Non‐operative management of abdominal stab wounds‐an analysis of 186 patients. South African Journal of Surgery 2007;45(4):128‐30. [PubMed] [Google Scholar]
Ozturk 2004
- Ozturk K, Dokucu AI, Onen A, Otcu S, Gedik S, Azal OF. Non‐operative management of isolated solid organ injuries due to blunt abdominal trauma in children: a fifteen year experience. European Journal of Pediatric Surgery 2004;14(1):29‐34. [DOI] [PubMed] [Google Scholar]
Parreira 2008
- Parreira JG, Rasslan S, Utiyama EM. Controversies in the management of asymptomatic patients sustaining penetrating thoracoabdominal wounds. Clinics 2008;63(5):695‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
Poletti 2004
- Poletti P, Platon A, Becker CD, Mentha G, Vermeulen B, Buhler LH, et al. Blunt abdominal trauma: does the use of a second‐generation sonographic contrast agent help to detect solid organ injuries. American Journal of Roentgenology 2004;183:1293‐301. [DOI] [PubMed] [Google Scholar]
Radwan 2006
- Radwan MM, Abu‐Zidan FM. Focussed Assessment Sonograph Trauma (FAST) and CT scan in blunt abdominal trauma: surgeon's perspective. African Health Science 2006;6(3):187‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager [Computer program]
- The Nordic Cochrane Center, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014.
Schroeppel 2007
- Schroeppel TJ, Croce MA. Diagnosis and management of blunt abdominal solid organ injury. Current Opinion on Critical Care 2007;13(4):399‐404. [DOI] [PubMed] [Google Scholar]
Stengel 2015
- Stengel D, Rademacher G, Ekkernkamp A, Güthoff C, Mutze S. Emergency ultrasound‐based algorithms for diagnosing blunt abdominal trauma. Cochrane Database of Systematic Reviews 2015, Issue 9. [DOI: 10.1002/14651858.CD004446.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yegiyants 2006
- Yegiyants S, Abou‐Lahoud G, Taylor E. The management of blunt abdominal trauma patients with computed tomography scan findings of free peritoneal fluid and no evidence of solid organ injury. The American Surgeon 2006;72(10):943‐6. [PubMed] [Google Scholar]
References to other published versions of this review
Oyo‐Ita 2008
- Oyo‐Ita A, Ugare UG, Ikpeme IA. Surgical versus non surgical management of abdominal injury. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007383] [DOI] [PubMed] [Google Scholar]
Oyo‐Ita 2012
- Oyo‐Ita A, Ugare UG, Ikpeme IA. Surgical versus non‐surgical management of abdominal injury. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD007383.pub2] [DOI] [PubMed] [Google Scholar]


