Abstract
Introduction
The emergence of cardiovascular risk factors in sub-Saharan Africa suggests an increasing incidence of acute coronary syndromes and STEMI. The aim of the study was to define the prevalence of STEMI and to describe the characteristics of patients diagnosed with STEMI within the tele-electrocardiogram (ECG) network in Côte d’Ivoire.
Method
A retrospective study was conducted from January 2015 to August 2019. All adult patients managed by one of the six hospitals within the telemedicine network who benefited from a remote interpretation of their ECG by the cardiology department of Bouaké University Hospital were included. The main reason for ECG interpretation, patient and ECG characteristics, diagnosis, response time and treatment were described.
Results
A total of 5649 patients were included. The prevalence of STEMI was 0.7% (n = 44 cases) with a mean age of 58.6 ± 11.8 years and a M/F sex ratio of 1.93. Among STEMI patients, chest pain was the main reason for ECG testing (56.8%). Most ECGs were interpreted within 12 hours (72.8%). The anterior inter-ventricular artery location (59.1%, n = 26) was predominant. The Q wave of necrosis was absent in 18% (n = 8) of cases. All patients received double anti-platelet aggregation and 50% (n = 22) additional heparin therapy. No patient underwent primary angioplasty or thrombolysis, 65.9% (n = 29) were referred to the Bouaké Cardiology Department and 34.1% (n = 15) to the Abidjan Heart Institute. Scheduled angioplasty was performed in 20% (n = 3) of patients in Abidjan.
Conclusion
Tele-ECG was an effective means of STEMI screening in Côte d’Ivoire. Systematic telethrombolysis of all patients diagnosed could improve their prognosis.
Keywords: ECG, tele-ECG, telemedicine, STEMI, telecardiology
Introduction
There is a scarcity of epidemiological data concerning acute coronary syndromes (ACS) in Sub-Saharan Africa.1–3 These syndromes, which are the most severe manifestations of heart disease, are increasingly prevalent across the region, where there has been a rapid epidemiological transition in recent years mainly due to lifestyle changes within the population.4,5 This situation is challenging for healthcare systems often lacking resources to provide effective treatment. Additionally, there is a great disparity in healthcare access between people living in major cities and those from rural areas.
The European Society of Cardiology (ESC) guidelines for the treatment of myocardial infarction with persistent ST-segment elevation (STEMI) recommends primary percutaneous transluminal coronary angioplasty (PTCA) as the preferred treatment strategy if it is performed within the recommended time frame.6–9 The maximum benefit is obtained when reperfusion is achieved within three hours of the appearance of symptoms. Performing a pre-hospital 12-lead electrocardiogram (ECG) can significantly reduce the delay in diagnosing, and therefore treating STEMI, which should be done within a 12-hour window after symptoms onset.
In Côte d’Ivoire, however, there is a lack of both the required materials to perform these ECGs and specialised cardiologists able to interpret the results. Côte d’Ivoire has around a hundred cardiologists, with 80% concentrated in the southern part of the country, primarily around the Institute of Cardiology in Abidjan, which is the only centre with a cardiac catheterisation room.
To date, the use of thrombolytic agents in emergency departments for the treatment of patients with STEMI has been limited to the capital city, and the number of primary percutaneous coronary interventions performed in public hospitals has been very low. The cost required to transfer patients to the only reference centre with a catheterisation laboratory for emergency revascularisation in Abidjan is also an issue for most of patients living outside of the capital city.
Since 2015, a national hub-and-spoke telecardiology project was initiated to provide ECG tele-expertise to hospitals located in less urbanised areas of the country based on international experiences from America and Europe.10–14 The project’s aim was to improve the diagnosis and treatment of patients with STEMI. The cardiology department of Bouaké University Hospital was the expert centre providing the remote interpretation of ECG via telemedicine through a secured platform. The objective of this study was to describe the prevalence of STEMI within the tele-ECG project in Côte d’Ivoire and the characteristics of patients diagnosed with STEMI.
Methods
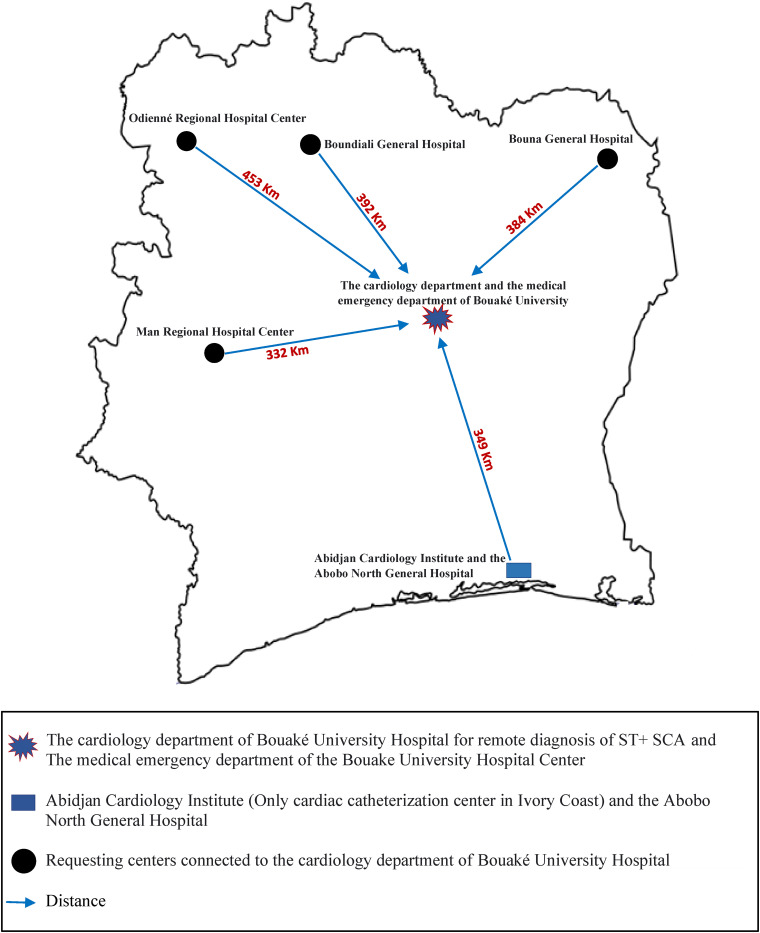
A retrospective study was performed using data collected from January 2015 to August 2019 at six hospital centres in Côte d’Ivoire that did not have any cardiologists (Abobo, Bouaké, Bouna, Boundiali, Man, Odienné) (Figure 1, Table 1).
Figure 1.
Hospital locations within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
Table 1.
Distances in non-medicalised car travel between the satellite hospitals and centres of expertise in Bouaké and Abidjan within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Locations | Distance to centre of expertise (Bouaké) | Distance centre of expertise (Abidjan Institute of Cardiology) | ||
|---|---|---|---|---|
| km | Time | km | Time | |
| Abobo (Municipality of Abidjan) | 349 | 4 h 55 min | 26.9 | 48 min |
| Bouake (Centre) | 0.5 | 5 min | 395 | 5 h 55 min |
| Bouna (North East) | 384 | 5 h 58 min | 577 | 8 h 05 min |
| Boundiali (North) | 392 | 6 h 21 min | 673 | 10 h 13 min |
| Man (West) | 332 | 6 h 24 min | 547 | 8 h 31 min |
| Odienne (North East) | 453 | 6 h 34 min | 721 | 10 h 19 min |
The centres were provided with kits including a digital ECG machine, high-speed reliable internet connection and a secure telemedicine platform locally developed for sharing and interpreting ECGs. Patients presenting at one of the six hospitals underwent a clinical evaluation including a 12-lead ECG. The ECGs were sent to the cardiology department of Bouaké CHU using the telemedicine network, where they were interpreted by an on-call cardiologists within a pool of three cardiologists. The cardiologist then provided tele-expertise to recommend a care pathway for the patient. In case of STEMI, patients were referred either to Abidjan Heart Institute or to Bouaké CHU depending on the medical needs. All adult patients aged 18 years or older with an ECG sent through the platform were included.
Patients were diagnosed with STEMI according to the third universal definition of myocardial infarction (persistent ST segment elevation at ECG localised in a territory associated with symptoms of chest pain) who presented at one of the six study centres. 15 Patient informed consent was obtained to send the ECG to the telemedicine platform. Patient consent was not necessary to collect data for the study as it was a retrospective study based on medical records.
Data collected included the patient age, sex, diagnosis, reason of consultation, delay in hours of ECG interpretation since received ECG at expert centre, localisation of the involved arteries, presence of Q wave, the treatment given, as well as the referral decision. ECGs were subdivided into two groups: acute electrocardiographic abnormalities including level 1 ECGs (urgent abnormalities) and level 2 ECGs (important abnormalities), and non-acute anomalies included those of level 3 (non-serious anomalies).
Statistical analysis
The software EPIDATA 3.1 and SPSS v22 were used to conduct the statistical analysis. The categorical variables are presented as raw numbers and as percentages. The quantitative variables are presented as a mean ± standard deviation in the case of a normal distribution.
Results
There were 5649 patients included in the study. Most of ECGs had acute anomalies (52.93%) and STEMI represented 13.75% of acute anomalies, second after atrial fibrillation accounting for 43.33% of acute cases (Table 2 and Table 3).
Table 2.
Classification of ECG according to their severity profile within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Classification | Numbers | Percentage (%) |
|---|---|---|
| Level 3 ECG (normal and non-significant abnormalities) | 2659 | 47.07 |
| Level 2 ECG (significant abnormalities) | 2670 | 47.26 |
| Level 1 ECG (urgent abnormalities) | 320 | 5.67 |
| Total | 5649 | 100 |
Table 3.
Classification of urgent abnormalities ECG diagnosis within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Diagnosis a | Numbers | Percentage (%) |
|---|---|---|
| Atrial fibrillation | 139 | 43.33 |
| STEMI | 44 | 13.75 |
| Others | 30 | 9.38 |
| Atrial Flutter | 21 | 6.67 |
| Complete BAV | 21 | 6.67 |
| Atrial tachycardia | 21 | 6.67 |
| Alternating sinus and junctional tachycardia | 11 | 3.33 |
| Supraventricular tachycardia | 11 | 3.33 |
| Junctional tachycardia | 11 | 3.33 |
| Prefibrillar state | 11 | 3.33 |
| Total | 320 | 100 |
Prognosis of these patients was not collected within this study.
The prevalence of STEMI was 0.78% (n = 44). The prevalence was 0.23% in 2015, 1.01% in 2016, 0.81% in 2017, 0.58% in 2018 and 1.09% in 2019. The highest number of STEMI cases were recorded in 2016 (31.8%). All ECGs of patients with STEMI were performed between 7 AM and 10 PM, 40.9% were interpreted within 6 hours, 72.7% within 12 hours, and 100% within 24 hours after receiving the ECG, as planned in the protocol.
The hospital of Abobo had the highest number of patients with STEMI (34.1%), followed by the hospital of Man (25%) (Table 4). For the patients with STEMI, the first clinical motive for conducting the ECG was chest pain (59.1%) followed by hypertension (22.7%) (Table 5). The mean age of patients with STEMI was 58.6 ± 11.8 years (minimum:35, maximum: 82 years). The STEMI population was 66% male, with a sex ratio of 1.93.
Table 4.
Distribution of STEMI cases among participating hospitals within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Locations | Number of patients with STEMI | Percentage a |
|---|---|---|
| Abobo | 15 | 34.1 |
| Bouake | 8 | 18.2 |
| Bouna | 5 | 11.4 |
| Boundiali | 2 | 4.5 |
| Man | 11 | 25.0 |
| Odienne | 3 | 6.8 |
| Total | 44 | 100.0 |
Percentage of patient within hospitals was not collected within this study.
Table 5.
Reasons for performing the ECG among the patients with diagnosed STEMI within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Number (n) | Percentage (%) | |
|---|---|---|
| Chest pain | 26 | 59.1 |
| High blood pressure | 10 | 22.7 |
| Palpitations | 3 | 6.8 |
| Cardiomegaly | 2 | 4.5 |
| Preoperative workup | 2 | 4.5 |
| Dyspnea | 1 | 2.3 |
| Total | 44 | 100.0 |
Among the patients with STEMI, the left anterior descending artery was the coronary arteries most affected (59.1%) (Table 6). Pathological Q waves (necrosis) were present in 82% of STEMI cases.
Table 6.
Coronary arteries affected for patients diagnosed with STEMI within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Territory | Number | Percentage (%) |
|---|---|---|
| Left anterior descending artery | 26 | 59.1 |
| Right coronary artery | 11 | 25 |
| Left circumflex artery | 5 | 11.3 |
| Septal branches | 1 | 2.3 |
| Several coronary arteries | 1 | 2.3 |
| Total | 44 | 100.0 |
No patients were treated by thrombolysis. All patients received dual anti-platelet therapy. More than half of patients received heparin treatment (Table 7). Among STEMI patients, 65.9% (n = 29) were referred to the Bouaké Cardiology Department and 34.1% (n = 15) to the Abidjan Heart Institute. Scheduled angioplasty was performed in 20% (n = 3) of patients in Abidjan.
Table 7.
Treatment of patients diagnosed with STEMI within the telecardiology network of Côte d’Ivoire between 2015 and 2019.
| Treatment | Number | Percentage (%) |
|---|---|---|
| Aspirin (loading dose)/clopidogrel 75 mg/beta blocker/statin | 44 | 100 |
| Anticoagulant (LMWH) | 42 | 95.45 |
| ACE inhibitor/angiotensin II receptor antagonist | 40 | 90.91 |
| Analgesic | 30 | 68.19 |
| Thrombolysis | 0 | 0 |
LMWH: low molecular weight heparin; ACE: angiotensin converting enzyme.
Discussion
The prevalence of STEMI in our population of patients receiving an ECG was 0.78% (n = 44). To our knowledge, our study is the first to have described a prevalence of STEMI at the national level in Côte d’Ivoire based on international guidelines. While this result should not be considered as a population level STEMI prevalence, it reveals that STEMI exists, is probably under-diagnosed and its impact under-estimated. The national telecardiology network led by CHU Bouaké is therefore a critical tool to improve the diagnosis and treatment of ACS and STEMI in the country. Without this project, the hospitals participating in the network would have no diagnostic or therapeutic capacity at all. This study was also the largest study in Côte d’Ivoire regarding cardiology patients with more than 5000 patients included. 16
A previous study related to ACS in Côte d’Ivoire identified a prevalence of 9.6% (n = 304) of STEMI among a population consulting at the Cardiology Institute of Abidjan in a period between 2010 and 2013. 17 The higher prevalence in this study could be related with a selection bias as patients were included from the main cardiology centre of the capital city while our study included patients from local non-specialised rural hospitals. Other reasons which may explain the lower prevalence in our study may be the lowest awareness of the population towards heart diseases in rural areas, the perception of lack of treatment options refraining patients to consult to the hospital, or a less probable lower prevalence in rural regions. The prevalence of STEMI may also be higher due to the non-inclusion of certain private practices in our network and possible sudden deaths at home.
Characteristics of patients diagnosed with STEMI in our study, however, matched well with the previous studies conducted on STEMI in Côte d’Ivoire. The mean age found in our study was 58.6 ± 11.8 years, while other studies reported mean ages of 54.5, 53.2, 57, 55.6 and 55.4 years old. Regarding the sex ratio, our study was also matching a male predominance found in all other studies in Côte d’Ivoire.16–19 The percentage of male of 66% in our study was within the range of 55.4 to 91.6 identified in previous research. The territory of the lesion being anterior and around 50% of patients was also similar to previous studies.
Within the network, most ECGs were performed during the day and read within a 12-hour delay. No ECGs were performed during the night which could be an issue for patients coming during the night to not have proper diagnosis on time.20,21 It could therefore be very beneficial for health professionals to be prepared to perform ECGs 24/7 to reduce the time between onset of symptoms and realisation of the ECG. The delay of interpretation, while being within the 24 hours planned for this project, was still too long and should be optimised by updating the processes for ECG interpretation. In a similar study from Brazil, the median interval time between the ECG and the remote interpretation was 31 minutes (interquartile range, 21–44 minutes). 22 Another tele-ECG study from Cameroon, however, reported an average time of ECG interpretation of 10.3 ± 11.6 days. 23
In our study, the eight patients admitted within the therapeutic window (less than 12 hours after symptom onset) did not receive reperfusion therapy due to the unavailability of thrombolytic medications, making it therefore impossible to respect international guidelines. This represents a real challenge to organise telethrombolysis in the country for hospitals far from the capital which currently has the cardiac catheterisation rooms in the country.
The main strengths of our study were its national geographical scope, the volume of patients included and the centralised homogenous interpretation of ECG. The main limits were the retrospective study design, the lack of clinical data collected for the whole population, as well as the lack of prognostic data for patients diagnosed with STEMI. The lack of troponin test in the hospitals from the network additionally did not allow to better identify and categorise non-STEMI patients in our sample.
In our study of the telemedicine network set up by the cardiology department of Bouaké CHU in Côte d’Ivoire, ECG tele-expertise contributed significantly to the diagnosis of STEMI in health centres with no cardiologists. These results suggest that this model could be helpful in developing countries. However, we nevertheless observed delays in the time to diagnosis, which could reflect a lack of healthcare education in both urban and rural populations in Côte d’Ivoire as well as a lack of optimised telecardiology processes. 24
The major uptake increase of telemedicine since the COVID-19 pandemic and the experience of other countries related to tele-expertise such as France could also encourage the national health authorities in Côte d’Ivoire to develop dedicated policies to promote these innovative medical activities to improve public health.25,26 While some countries, such as Indonesia, demonstrated the feasibility of tele-ECG in primary care settings with general practitioners, it should be easier to develop a stronger network within hospitals in Côte d’Ivoire at first. 27 Pre-hospital triage with tele-ECG, while being of potential higher public health impact, may additionally prove difficult to implement in Côte d’Ivoire. 28
Conclusions
The national telecardiology network led by CHU Bouaké is a critical tool to improve the diagnosis and treatment of ACS and STEMI in Côte d’Ivoire. Without this project, the hospitals participating in the network would have no diagnostic or therapeutic capacity. The network should be further expanded.
Acknowledgments
The authors thank the CHU Bouaké as well as Expertise France.
Footnotes
Contributorship: FD, RO and TM supervised the study. AG, PO, GA, AG, GR, SD, FS, AA, EN, participated in the data collection. All authors equally contributed to the protocol definition. The data analysis was conducted by FD and AG. The preparation and writing of the manuscript was conducted by FD, RO and TM. All authors reviewed the final manuscript.
Data availability: Data will be made available upon request by email to the corresponding author.
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethics approval: Ethics approval was not required according to the national legislation of Côte d’Ivoire since observational studies are exempt.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by a grant from Expertise France (French Development Agency).
Guarantor: FD.
Patient and public involvement: It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
ORCID iD: R. Ohannessian https://orcid.org/0000-0003-1999-7683
References
- 1.Schamroth C. and ACCESS South Africa investigators. Management of acute coronary syndrome in South Africa: insights from the ACCESS (acute coronary events – a multinational survey of current management strategies) registry. Cardiovasc J Afr 2012; 23: 365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shavadia J, Yonga G, Otieno H. A prospective review of acute coronarys yndromes in an urban hospital in sub-Saharan Africa. Cardiovasc J Afr 2012; 23: 318–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mboup MC, Diao M, Dia Ket al. et al. Les syndromes coronaires aigus à Dakar : aspects cliniques thérapeutiques et évolutifs. Pan Afr Med J 2014; 19: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yayehd K, Damorou F, N’Da NW, et al. Evolution of cardiovascular diseases admissions in cardiology departments of Lome hospitals: a cross-sectional study on 7959 patients from June 2004 to May 2009. Rev Epidemiol Sante Publique 2012; 60: 205–211. [DOI] [PubMed] [Google Scholar]
- 5.Touze JE. Les maladies cardiovasculaires et la transition épidémiologique du monde tropical. Med Trop 2007; 67: 541–542. [PubMed] [Google Scholar]
- 6.Steg PG, James SK, Atar D, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33: 2569–2619. [DOI] [PubMed] [Google Scholar]
- 7.Terkelsen CJ, Sørensen JT, Maeng M, et al. Stent for life initiative: leading example in building STEMI systems of care in emerging countries. Euro Intervention 2014; 10: T87–T95. [DOI] [PubMed] [Google Scholar]
- 8.O’Gara PT, Kushner FG, Ascheim DD, et al. ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013; 127: 529–555. [DOI] [PubMed] [Google Scholar]
- 9.Gershlick AH, Westerhout CM, Armstrong PW, et al. Impact of a pharmaco invasive strategy when delays to primary PCI are prolonged. Heart 2015; 101: 692–698. [DOI] [PubMed] [Google Scholar]
- 10.Diby F, Adoubi A, Gnaba A, et al. Téléexpertise dans l’interprétation de l’électrocardiogramme d’une population noire africaine en Côte d’Ivoire (Afrique Subsaharienne). Eur Res Telemed 2015; 4: 109–117. [Google Scholar]
- 11.Diby FK, Adoubi AK, Esse-Diby M-CA, et al. A medico-socio-economic analysis of TeleEKG in Ivory Coast. Telemed e-Health 2020; 27: 286–295. [DOI] [PubMed] [Google Scholar]
- 12.Henry TD, Unger BT, Sharkey SW, et al. Design of a standardized system for transfer of patients with ST-elevation myocardial infarction for percutaneous coronary intervention. Am Heart J 2005; 150: 373–384. [DOI] [PubMed] [Google Scholar]
- 13.Jollis JG, Roettig ML, Aluko AO, et al. Reperfusion of acute myocardial infarction in North Carolina emergency departments (RACE) investigators. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA 2007; 298: 2371–2380. [DOI] [PubMed] [Google Scholar]
- 14.Aguirre FV, Varghese JJ, Kelley MP, et al. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: the Stat Heart Program. Circulation 2008; 117: 1145–1152. [DOI] [PubMed] [Google Scholar]
- 15.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation 2012; 126: 2020–2035. [DOI] [PubMed] [Google Scholar]
- 16.Yao H, Ekou A, Niamkey T, et al. Acute coronary syndromes in sub-Saharan Africa: a 10-year systematic review. J Am Heart Assoc 2022; 11: e021107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.N’Guetta R, et al. Prévalence et caractéristiques des syndromes coronariens aigus dans une population d’Afrique subsaharienne. Ann Cardiol Angeiol 2016; 65: 59–63. [DOI] [PubMed] [Google Scholar]
- 18.Hanssen M, Cottin Y, Khalife K, et al. French registry on acute ST-elevation and non-ST-elevation myocardial infarction. FAST-MI 2010. Heart 2012; 98: 699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organisation. Côte d’Ivoire. Ministère de la Santé et de l’Hygiène publique. Enquête sur les facteurs de risque des maladies non transmissibles. Régions sanitaires des Lagunes; 2005 [(en ligne). Available at : http://www.who.int/chp/steps/Cotedivoire 2005.pdf. Last accessed on 03 Septembre 2023.
- 20.Ibanez B, James S, et al. The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119–177. [DOI] [PubMed] [Google Scholar]
- 21.NHLBI. National Heart Attack Alert Program Coordinating Committee, 60 Minutes to Treatment Working Group. Emergency department: rapid identification and treatment of patients with acute myocardial infarction. Ann Emerg Med 1994; 23: 311–329. [PubMed] [Google Scholar]
- 22.Solla, et al. Integrated regional networks for ST-segment–elevation myocardial infarction care in developing countries. The experience of Salvador, Bahia, Brazil. Circ Cardiovasc Qual Outcomes 2013; 6: 9–17. [DOI] [PubMed] [Google Scholar]
- 23.Bediang G, Nganou-Gnindjio CN, Kamga Y, et al. Evaluation of the effectiveness of telemedicine in the management of cardiovascular diseases in primary health care in Cameroon: an interventional study. Stud Health Technol Inform 2021; 281: 615–619. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira CdP, Jr, Marcolino MS, Manoel Fernandes Canesin MF. Executive summary – guideline on telecardiology in the care of patients with acute coronary syndrome and other cardiac diseases. Arq Bras Cardiol 2015; 105: 105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020; 6: e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohannessian R, Yaghobian S, Duong TA, et al. Letter to the Editor: France is the first country to reimburse tele-expertise at a national level to all medical doctors. Telemed J E Health 2021; 27: 378–381. [DOI] [PubMed] [Google Scholar]
- 27.Mappangara I, Qanitha A, Uiterwaal CSPM, et al. Tele-ECG consulting and outcomes on primary care patients in a low-to-middle income population: the first experience from Makassar telemedicine program, Indonesia. BMC Fam Pract 2020; 21: 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lazarus G, Kirchner HL, Siswanto BB. Prehospital tele-electrocardiographic triage improves the management of acute coronary syndrome in rural populations: a systematic review and meta-analysis. J Telemed Telecare 2022; 28: 632–641. [DOI] [PubMed] [Google Scholar]