Abstract
Background
While the impacts of social and environmental exposure on cardiovascular risks are often reported individually, the combined effect is poorly understood.
Methods and Results
Using the 2022 Environmental Justice Index, socio‐environmental justice index and environmental burden module ranks of census tracts were divided into quartiles (quartile 1, the least vulnerable census tracts; quartile 4, the most vulnerable census tracts). Age‐adjusted rate ratios (RRs) of coronary artery disease, strokes, and various health measures reported in the Prevention Population‐Level Analysis and Community Estimates data were compared between quartiles using multivariable Poisson regression. The quartile 4 Environmental Justice Index was associated with a higher rate of coronary artery disease (RR, 1.684 [95% CI, 1.660–1.708]) and stroke (RR, 2.112 [95% CI, 2.078–2.147]) compared with the quartile 1 Environmental Justice Index. Similarly, coronary artery disease 1.057 [95% CI,1.043‐1.0716] and stroke (RR, 1.118 [95% CI, 1.102–1.135]) were significantly higher in the quartile 4 than in the quartile 1 environmental burden module. Similar results were observed for chronic kidney disease, hypertension, diabetes, obesity, high cholesterol, lack of health insurance, sleep <7 hours per night, no leisure time physical activity, and impaired mental and physical health >14 days.
Conclusions
The prevalence of CVD and its risk factors is highly associated with increased social and environmental adversities, and environmental exposure plays an important role independent of social factors.
Keywords: cardiometabolic outcomes, environmental burden, environmental justice index, social determinants of health, social vulnerability
Subject Categories: Cardiovascular Disease; Obesity; Epidemiology; Diabetes, Type 2; Risk Factors
Nonstandard Abbreviations and Acronyms
- EBM
environmental burden module
- EJI
Environmental Justice Index
- PLACES
Prevention Population‐Level Analysis and Community Estimates
- SE‐EJI
socio‐environmental justice index
- SVM
social vulnerability module
Clinical Perspective.
What Is New?
Chronic environmental burden and social vulnerability work synergistically to widen cardiovascular health inequity; therefore, there is a need to address both simultaneously.
An increase in the environmental burden, independent of social vulnerability, is associated with a graded increase in the prevalence of cardiovascular disease and other adverse health measures.
What Are the Clinical Implications?
An independent increase in environmental burden and a composite of social vulnerability and environmental burden were associated with an increased prevalence of cardiovascular disease and risk factors.
Most of the US population aged 18 to 44 years, Black adults, and Hispanic individuals resided in places with alarmingly high environmental burdens.
The findings from this study could help guide future research examining associations between social disadvantage, environmental exposures, and cardiovascular outcomes while informing policy efforts to reduce inequities and mitigate cardiovascular disease burden among vulnerable populations.
Cardiovascular disease (CVD) continues to be the leading cause of death in the United States and globally, with an alarming deceleration of decline in CVD death in recent years. 1 , 2 , 3 This finding could be partly attributed to the rising burden of cardiovascular risk factors in young adults. 4 , 5 , 6 Recent evidence suggests that neighborhoods with greater social and environmental disadvantages have a higher prevalence of CVD and associated risk factors. 7 , 8 Multiple studies have reported higher CVD morbidity and death in areas with high social vulnerability, measured using the US Centers for Disease Control and Prevention (CDC)/Agency for Toxic Substances and Disease Registry's Social Vulnerability Index. 9 , 10 , 11 , 12 The Environmental Justice Index (EJI) was developed using data from the US Census Bureau, the US Environmental Protection Agency, US Mine Safety and Health Administration, and the CDC. It provides additional information beyond the Social Vulnerability Index by accounting for environmental factors. When examined individually, the association between social and environmental factors with CVD and its risk factors is well established. The impact of combining these factors and, importantly, the incremental value of environmental factors after accounting for social factors is poorly understood. It is essential to address this knowledge gap because the relationship or interaction between social and environmental disadvantages and their relative contribution to health inequities is complex. For example, if environmental exposures mainly mediate the relationship between social disadvantage and health or vice versa, improving any of these factors can potentially improve health disparities. In the present analysis, we examined the association between the EJI ranking of census tracts and the prevalence of CVDs and risk factors. We then explored the incremental effect of environmental factors, over and above social factors, on the prevalence of CVD and its associated risk factors.
METHODS
All data and materials are publicly available on the CDC website and can be accessed at https://onemap.cdc.gov/portal/apps/sites/#/eji‐explorer and https://data.cdc.gov/500‐Cities‐Places/PLACES‐Census‐Tract‐Data‐GIS‐Friendly‐Format‐2022‐/shc3‐fzig/data. Informed consent was not required due to the use of deidentified data.
Data Sources
Prevention Population‐Level Analysis and Community Estimates: The Census Tract Prevalence and Population Data
We used the CDC 2022 Population‐Level Analysis and Community Estimates (PLACES): Local Data for Better Health database to obtain the US census tract prevalence of CVD and risk factors. The population estimates were taken from the 2015 to 2019 American community survey. 13 The CDC's PLACES uses model‐based small‐area, specifically multilevel regression and poststratification, to estimate 29 health measures, categorized into health outcomes, health risk behaviors, prevention, and health status. 14 PLACES also provides data at multiple local area levels, that is, county, place, census tract, and ZIP Code Tabulation Areas. 14 In addition, the CDC used state‐level health data from the Behavioral Risk Factor Surveillance System to cover 3142 counties, 28 484 places (incorporated and census‐designated areas), 72 337 census tracts, and 32 409 ZIP Code Tabulation Areas according to the Census 2010 population of ≥50 people. PLACES data complements the existing surveillance data by providing small‐area estimates to comprehend health issues at the local level. 15
From the PLACES data, we extracted crude prevalence rates of CVDs, including coronary heart disease, stroke, chronic kidney disease, hypertension, diabetes, obesity, and hyperlipidemia. In addition, we extracted the prevalence of additional risk factors, including lack of health insurance among those aged 18 to 64 years, risk behaviors such as sleeping less than 7 hours per night and no leisure time physical activity, and health status indicators such as mental and physical health not good for ≥14 days in the past month.
Environmental Justice Index
We used the 2022 EJI data set from the CDC's Agency for Toxic Substances and Disease Registry, which outlines the census tract's relative environmental burden and social vulnerability. Census tracts are subdivisions of counties in the United States. The US Census Bureau collects census tract–level data and is often used as a substitute for neighborhoods in spatial indices, screening tools, and place‐based research. 16 The EJI uses data from various sources, including the US Census Bureau, the US Environmental Protection Agency, US Mine Safety and Health Administration, and the CDC, to determine the cumulative impact of environmental injustice for over 71 000 census tracts in the United States (Figure 1). 16 The indicators selected for inclusion in the EJI underwent rigorous evaluation on the basis of data criteria, ensuring the index would be high quality, reproducible, and sustainable over time. 16
Figure 1. US choropleth map of environmental justice indices at the census tract level. Source: CDC EJI database. 16 .
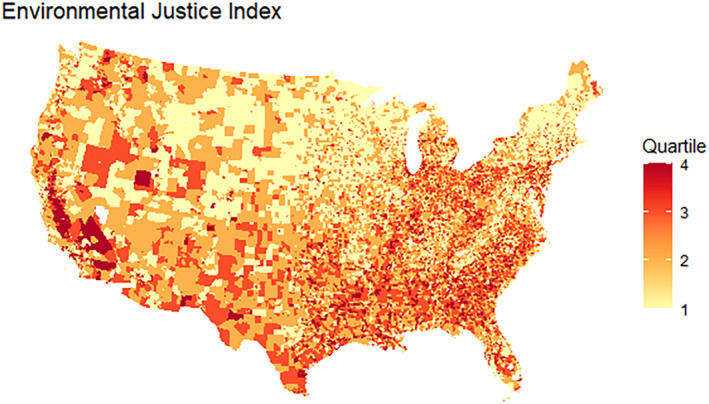
Created using R programming.
The EJI ranks census tracts on 10 different domains categorized under 3 main modules: (1) the environmental burden module (EBM), (2) the social vulnerability module (SVM), and (3) the health vulnerability module. 16 In addition, a unique cumulative ranked percentile of EBM and SVM without the health vulnerability module is available for statistical analysis, called the socio‐environmental EJI (SE‐EJI). 16 The SE‐EJI ranks can be used to understand the association of certain health outcomes with distributive and procedural environmental justice issues. 16 As evidenced by scientific literature, all indicators that accounted for the environmental burden score were selected on the basis of their ability to cause a quantifiable negative health impact. 16 These indicators also represented distinct aspects of environmental burden with no overlapping effects. 16 All indicators used to calculate the social vulnerability score represented the inability of the vulnerable population to improve the environmental conditions or advocate against unwanted land use in their communities on the basis of historical discrimination. 16
The SE‐EJI metric captures the distributive and procedural environmental justice elements that can subsequently impact human health and well‐being. 16 In this manuscript, we refer to SE‐EJI (a composite measure of social and environmental burden) when we mention EJI to explore the relationships with health phenomena (Figure 1). We did not use the health vulnerability module ranks in the current analysis to assess the impact of the SE‐EJI on CVD and other health measures. The EBM accounted for air pollution, potentially hazardous and toxic sites, the built environment, transport infrastructure, and water pollution. The SVM reported racial and ethnic minority status, socioeconomic status, household characteristics, and housing type as described in the Tables S1 and S2.
The EJI, EBM, and SVM scores are percentile ranks ranging from 0.00 to 1.00, and each census tract is represented with a unique score. Higher scores indicated a significant environmental burden and social vulnerability, as shown in Figure 1. We aggregated the ranks for each census tract into quartiles 1 to 4. The areas with the least socially vulnerable population and the lowest environmental impact constituted the first quartile, with percentile ranks from 0.00 to 0.25. Census tracts with high environmental and social burdens formed the fourth quartile, ranking between 0.75 and 1.00. Additional details regarding the methods used to create percentile ranks are provided in Data S1. We also explored the census tract–level age, race, and ethnic distribution across the EJI categories. Finally, we aggregated the median prevalence for each health measure of interest per 100000 population among the different EJI quartiles. Each census tract with percentile rank was matched with its prevalence rates on the basis of standard geographic identifiers (such as location ID) using the PLACES and EJI databases.
The results were reported according to the Strengthening the Reporting of Observational Studies in Epidemiology statement guidelines for reporting observational studies. This study was exempt from institutional review board approval because it used deidentified data with prior approval from the ethics committee.
Statistical Analysis
Continuous variables (eg, the prevalence of health outcomes or risk factors included in PLACES) were reported as median (interquartile range [IQR]), while categorical variables were presented as absolute numbers and percentages. As mentioned above, the EJI, EBM, and SVM percentile ranks are distributed into quartiles. We compared the rate ratios (RRs) of the prevalence of cardiovascular health measures per 100 000 population at the census tract level with a 95% CI across the EJI, EBM, and SVM quartiles using multivariable Poisson regression combined with an offset function. The RRs for the second, third, and fourth quartiles were calculated and adjusted for age categories relative to the first EJI, SVM, and EBM quartiles. P values <0.05 were considered statistically significant. Two models were created: One with EJI and age categories as covariates. Second, to investigate the incremental effect of environmental burden, we performed multivariable Poisson regression with SVM and EBM as separate covariates in the model and adjusted for SVM and age categories.
RESULTS
Demographics
The demographic characteristics of the US population across the EJI and EBM quartiles are presented in Table 1. EJI and EBM quartile 1 had the highest median percentages of individuals aged 45 to 64 years and age ≥65 years, and White and non‐Hispanic adults. This percentage decreased consistently with increasing EJI and EBM quartiles. EJI quartile 4 and EBM quartile 4 had the highest median percentages of individuals aged 18 to 44 years and Black adults.
Table 1.
Demographic Distribution of the US Population Stratified Across the EJI and EBM Quartiles
| EJI quartile 1 (0–0.25) | EJI quartile 2 (0.26–0.50) | EJI quartile 3 (0.51–0.75) | EJI quartile 4 (0.76–1.0) | EBM quartile 1 (0–0.25) | EBM quartile 2 (0.26–0.50) | EBM quartile 3 (0.51–0.75) | EBM quartile 4 (0.76–1.0) | |
|---|---|---|---|---|---|---|---|---|
| Demographics | ||||||||
| Age 18–44 y | 17 429 804 | 17 770 409 | 18 860 800 | 18 852 898 | 16 825 728 | 17 991 851 | 18 854 433 | 19 251 823 |
| Median % 18–44 (IQR) | 26.05 (25.92–26.18) | 27.93 (27.79–28.05) | 29.88 (29.74–30.01) | 31.87 (31.75–31.99) | 26.82 (26.69–26.95) | 28.24 (28.12–28.38) | 29.68 (29.55–29.75) | 31.54 (31.42–31.67) |
| Age 45–64 y | 17 926 199 | 15 855 665 | 15 158 922 | 13 796 281 | 16 203 006 | 16 049 191 | 15 795 993 | 14 691 457 |
| Median % 45–64 (IQR) | 28.80 (28.71–28.90) | 26.93 (26.85–27.05) | 25.51 (25.49–25.52) | 23.84 (23.74–23.94) | 27.48 (27.36–27.60) | 26.6 (26.55–26.73) | 25.97 (25.86–26.08) | 24.95 (24.83–25.04) |
| Age ≥65 y | 11 439 193 | 10 417 586 | 9 823 571 | 7 983 962 | 10 962 008 | 10 232 373 | 9 829 153 | 8 641 086 |
| Median % ≥65 (IQR) | 17.61 (17.48–17.76) | 17.40 (17.28–17.54) | 16.11 (16.09–16.13) | 13.20 (13.08–13.32) | 18.0 (17.79–18.10) | 16.73 (16.60–16.86) | 15.75 (15.63–15.88) | 14.05 (13.91–14.18) |
| Race, n (%) | ||||||||
| White adults | 51 964 953 (87.1) | 46 598 482 (84.1) | 42 024 671 (77.3) | 29 972 789 (62.4) | 46 481 284 (84.4) | 45 404 166 (81.2) | 42 447 849 (76.4) | 36 240 393 (71.1) |
| Black adults | 3 215 002 (5.3) | 4 996 164 (9) | 8 508 138 (15.6) | 14 577 848 (30.3) | 4 527 777 (8.2) | 6 801 487 (12.1) | 9 130 305 (16.4) | 10 844 960 (21.3) |
| American Indian or Alaskan Native | 282 493 (0.5) | 665 405 (1.2) | 549 790 (1) | 472 874 (1) | 819 675 (1.5) | 458 718 (0.8) | 370 394 (0.6) | 321 927 (0.63) |
| Asian | 4 074 233 (6.8) | 3 077 411 (5.5) | 3 178 799 (5.8) | 2 870 425 (0.06) | 3 119 747 (5.6) | 3 166 011 (5.6) | 3 492 303 (6.2) | 3 424 096 (6.7) |
| Native Hawaiian or Other Pacific Islander | 75 785 (0.1) | 78 768 (0.1) | 89 712 (0.1) | 91 266 (0.2) | 96 041 (0.17) | 81 554 (0.14) | 77 560 (0.1) | 80 376 (0.15) |
| Total | 59 612 466 | 55 416 230 | 54 351 110 | 47 985 202 | 55 044 524 | 55 911 936 | 55 518 411 | 50 911 752 |
| Ethnicity | ||||||||
| Hispanic | 6 043 439 (11.1) | 7 814 179 (15.7) | 11 260 958 (24) | 18 691 796 (48) | 9 371 072 (18.7) | 9 427 037 (19.1) | 10 542 940 (22.3) | 14 472 021 (33.2) |
| Non‐Hispanic | 48 241 555 (88.9) | 41 991 477 (84.3) | 35 623 302 (76) | 20 460 996 (52.2) | 40 691 877 (81.2) | 39 919 008 (80.8) | 36 699 082 (77.6) | 29 018 414 (66.7) |
EBM indicates environmental burden module; EJI, environmental justice index; and IQR, interquartile range.
CVD Prevalence
From 2015 to 2019, the prevalence of coronary artery disease was highest in EJI quartile 4 (6700 [IQR, 5400–8100] per 100 000 people) and lowest in EJI quartile 1 (5400 [IQR, 4400–6500] per 100 000 people; RR, 1.684 [95% CI, 1.660–1.708]; Tables 2 and 3; Figure 2A). The prevalence of stroke was highest in EJI quartile 4 (3700 [IQR, 3000–4800] per 100 000 people) and lowest in EJI quartile 1 (2400 [IQR, 2000–2900] per 100 000 people; RR, 2.112 (95% CI, 2.078–2.147); Tables 2 and 3; Figure 2B). A similar pattern was noted for chronic kidney disease (Figure 2C).
Table 2.
Prevalence of Cardiovascular Health Measures per 100 000 Overall and Across the EJI Quartiles
| Health outcomes and risk factors | Overall prevalence per 100 000, median (IQR) | Prevalence per 100 000 in EJI quartile 1 (0.00–0.25), median (IQR) | Prevalence per 100 000 in EJI quartile 2 (0.26–0.50), median (IQR) | Prevalence per 100 000 in EJI quartile 3 (0.51–0.75), median (IQR) | Prevalence per 100 000 in EJI quartile 4 (0.76–1.00), median (IQR) |
|---|---|---|---|---|---|
| Coronary artery disease | 6100 (4900–7500) | 5400 (4400–6500) | 6100 (4900–7400) | 6400 (5100–7700) | 6700 (5400–8100) |
| Stroke | 3000 (2400–3700) | 2400 (2000–2900) | 2800 (2300–3500) | 3200 (2600–3800) | 3700 (3000–4800) |
| Chronic kidney disease | 2900 (2400–3400) | 2500 (2200–2800) | 2800 (2400–3200) | 3000 (2600–3400) | 3400 (2900–4100) |
| Hypertension | 32 100 (27 800–36 900) | 29 400 (26 100–33 100) | 31 800 (27 700–36 000) | 33 100 (28 500–37 300) | 35 200 (29 800–41 300) |
| Diabetes | 10 300 (8500–12 600) | 8500 (7400–9900) | 9700 (8200–11 500) | 10 800 (9000–12 800) | 13 000 (11 000–15 900) |
| Obesity | 33 100 (28 100–37 700) | 28 900 (25 000–32 800) | 32 200 (27 700–36 100) | 34 100 (29 350–38 200) | 38 000 (33 300–42 800) |
| High cholesterol | 32 200 (29 300–31 953) | 32 400 (29 600–34 900) | 32 800 (29 600–35 500) | 32 300 (29 200–35 200) | 31 400 (28 700–34 300) |
| Lack of health insurance | 13 300 (9800–19 200) | 9600 (7600–12 200) | 11 700 (9200–16 000) | 14 100 (11 000–19 500) | 20 200 (15 600–26 400) |
| Sleep <7 h/night | 33 500 (30 700–36 600) | 30 500 (28 200–32 800) | 32 500 (30 200–35 000) | 34 300 (31 900–36 900) | 37 300 (34 600–41 100) |
| No leisure time physical activity | 23 700 (18 800–29 600) | 18 000 (15 200–21 300) | 22 100 (18 100–26 100) | 25 200 (21 100–29 600) | 31 700 (27 000–36 900) |
| Mental health not good for ≥14 d | 15 000 (13 100–16 900) | 13 100 (11 800–14 400) | 14 500 (12 900–16 000) | 15 500 (13 900–17 100) | 17 200 (15 600–18 900) |
| Physical health not good for ≥14 d | 10 300 (8400–12 700) | 8400 (7300–9800) | 9800 (8200–11 700) | 10 800 (9100–12 800) | 13 100 (11 100–15 400) |
EJI indicates environmental justice index; and IQR, interquartile range.
Table 3.
Rate Ratios of Cardiovascular Health Measures per 100 000 Stratified Across the EJI Quartiles
| Regression model 1 | Regression model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcomes | EJI quartile 2 | EJI quartile 3 | EJI quartile 4 | SVM quartile 2 | SVM quartile 3 | SVM quartile 4 | EBM quartile 2 | EBM quartile 3 | EBM quartile 4 |
| Coronary artery disease |
1.222 (1.205–1.239) P<0.001 |
1.348 (1.329–1.368) P<0.001 |
1.684 (1.660–1.708) P<0.001 |
1.256 (1.239–1.273) P<0.001 |
1.516 (1.495–1.537) P<0.001 |
1.907 (1.881–1.934) P<0.001 |
1.006 (0.993–1.020) P=0.3 |
1.0197 (1.006–1.0332) P=0.0035 |
1.057 (1.043–1.0716) P<0.001 |
| Stroke |
1.270 (1.249–1.291) P<0.001 |
1.483 (1.459–1.508) P<0.001 |
2.112 (2.078–2.147) P<0.001 |
1.318 (1.297–1.340) P<0.001 | 1.693 (1.667–1.720) P<0.001 | 2.452 (2.415–2.491) P<0.001 |
1.0142 (0.999–1.0292) P=0.057 |
1.052 (1.037–1.067) P<0.001 |
1.118 (1.102–1.135) P<0.001 |
| Chronic kidney disease |
1.195 (1.17–1.212) P<0.001 |
1.346 (1.327–1.366) P<0.001 |
1.805 (1.779–1.831) P<0.001 |
1.224 (1.207–1.241) P<0.001 |
1.493 (1.473–1.514) P<0.001 |
2.038 (2.010–2.066) P<0.001 |
1.000 (0.987–1.013) P=0.93 |
1.028 (1.0147–1.041) P<0.001 |
1.086 (1.071–1.100) P<0.001 |
| Hypertension |
1.159 (1.143–1.174) P<0.001 |
1.260 (1.243–1.277) P<0.001 |
1.561 (1.540–1.583) P<0.001 |
1.169 (1.153–1.184) P<0.001 | 1.359 (1.341–1.377) P<0.001 | 1.674 (1.651–1.696) P<0.001 |
1.017 (1.004–1.030) P=0.007 |
1.039 (1.0264–1.053) P<0.001 |
1.084 (1.070–1.098) P<0.001 |
| Diabetes |
1.232 (1.213–1.252) P<0.001 |
1.436 (1.414–1.459) P<0.001 |
2.024 (1.993–2.056) P<0.001 |
1.263 (1.244–1.282) P<0.001 | 1.601 (1.578–1.625) P<0.001 | 2.304 (2.271–2.338) P<0.001 |
1.009 (0.995–1.0236) P=0.18 |
1.046 (1.031–1.060) P<0.001 |
1.119 (1.103–1.1351) P<0.001 |
| Obesity |
1.154 (1.138–1.170) P<0.001 |
1.249 (1.232–1.266) P<0.001 |
1.540 (1.519–1.561) P<0.001 |
1.185 (1.169–1.201) P<0.001 | 1.361 (1.343–1.379) P<0.001 | 1.665 (1.642–1.687) P<0.001 |
1.014 (1.001–1.0276) P=0.029 |
1.035 (1.021–1.048) P<0.001 |
1.074 (1.060–1.089) P<0.001 |
| High cholesterol |
1.082 (1.069–1.094) P<0.001 |
1.117 (1.104–1.130) P<0.001 |
1.255 (1.240–1.270) P<0.001 |
1.075 (1.063–1.088) P<0.001 | 1.172 (1.158–1.185) P<0.001 | 1.307 (1.291–1.323) P<0.001 |
1.002 (0.991–1.013) P=0.69 |
1.008 (0.997–1.020) P=0.12 |
1.034 (1.022–1.046) P<0.001 |
| Lack of health insurance |
1.297 (1.274–1.321) P<0.001 |
1.576 (1.549–1.604) P<0.001 |
2.234 (2.196–2.272) P<0.001 |
1.423 (1.399–1.447) P<0.001 | 1.951 (1.919–1.983) P<0.001 | 2.952 (2.905–2.999) P<0.001 |
0.946 (0.933–0.960) P<0.001 |
0.946 (0.932–0.960) P<0.001 |
0.993 (0.979–1.007) P=0.36 |
| Sleep <7 h/night |
1.114 (1.100–1.128) P<0.001 |
1.197 (1.182–1.212) P<0.001 |
1.433 (1.416–1.451) P<0.001 |
1.129 (1.115–1.143) P<0.001 | 1.258 (1.242–1.273) P<0.001 | 1.470 (1.452–1.488) P<0.001 |
1.009 (0.997–1.022) P=0.11 |
1.045 (1.033–1.058) P<0.001 |
1.101 (1.088–1.114) P<0.001 |
| No leisure time physical activity |
1.274 (1.254–1.294) P<0.001 |
1.493 (1.471–1.516) P<0.001 |
2.050 (2.020–2.081) P<0.001 |
1.342 (1.323–1.363) P<0.001 | 1.698 (1.674–1.723) P<0.001 | 2.301 (2.268–2.334) P<0.001 |
1.020 (1.006–1.034) P=0.0044 |
1.062 (1.048–1.077) P<0.001 |
1.143 (1.127–1.159) P<0.001 |
| Mental health not good for ≥14 d |
1.136 (1.122–1.151) P<0.001 |
1.219 (1.203–1.235) P<0.001 |
1.444 (1.425–1.463) P<0.001 |
1.177 (1.161–1.192) P<0.001 | 1.326 (1.309–1.343) P<0.001 | 1.543 (1.523–1.563) P<0.001 |
0.996 (0.984–1.008) P=0.564 |
1.016 (1.004–1.029) P=0.0093 |
1.061 (1.048–1.075) P<0.001 |
| Physical health not good for ≥14 d |
1.238 (1.220–1.257) P<0.001 |
1.410 (1.388–1.431) P<0.001 |
1.891 (1.863–1.920) P<0.001 |
1.309 (1.290–1.328) P<0.001 | 1.645 (1.622–1.669) P<0.001 | 2.242 (2.210–2.274) P<0.001 |
0.949 (0.936–0.962) P<0.001 |
0.936 (0.923–0.948) P<0.001 |
0.949 (0.936–0.961) P<0.001 |
Model 1 shows rate ratios (95% CIs) from multivariate Poisson regression with EJI and age categories as covariates. Model 2 shows rate ratios (95% CIs) from multivariate Poisson regression with SVM and EBM as separate covariates along with age categories. EBM indicates environmental burden module; EJI, Environmental Justice Index; and SVM, social vulnerability module.
Figure 2. Choropleth maps CVD risk factor prevalence.
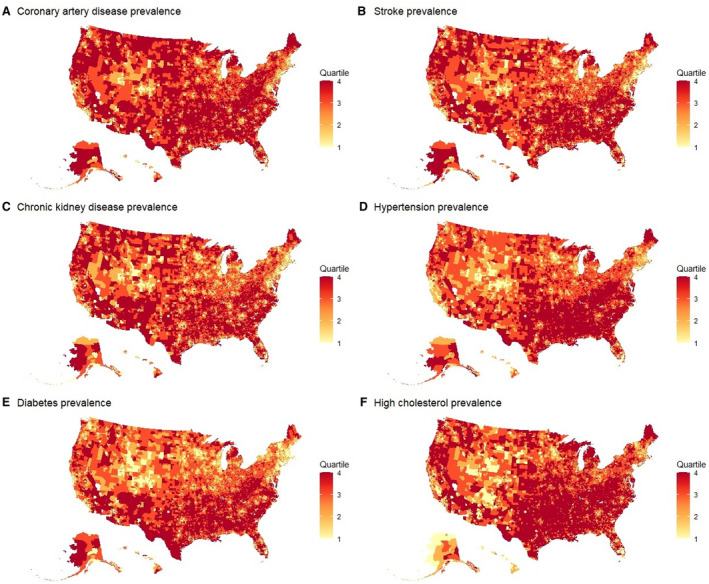
US choropleth maps of coronary artery disease prevalence (A), stroke prevalence (B), chronic kidney disease prevalence (C), hypertension prevalence (D), diabetes prevalence (E), and high cholesterol prevalence (F) at the census tract level. Source: CDC PLACES database. 15 Created using R programming. CVD indicates cardiovascular disease.
Cardiovascular Risk Factor Prevalence
Similarly, the prevalence of hypertension was highest in EJI quartile 4 (35 200 [IQR, 29 800–41 300] per 100 000 people) and lowest in EJI quartile 1 29 400 [IQR 26 100‐33 100] per 100 000 people; RR, 1.561 [95% CI, 1.540–1.583]; Figure 2D). The prevalence of diabetes was highest in EJI quartile 4 (13 000 [IQR, 11 000–15 900] per 100 000 people) and lowest in EJI Q1 (8500 [IQR, (7400‐9900)] per 100 000 people; RR, 2.024 [95% CI, 1.993–2.056]; Figure 2E). Similar patterns of lower prevalence in the EJI quartile 1 and higher prevalence in the EJI quartile 4 were observed for high cholesterol (Figure 2F), obesity (Figure 3A), lack of health insurance (Figure 3B), sleep <7 hours (Figure 3C), no leisure time physical activity (Figure 3D), physical health not good for >14 days (Figure 3E), and mental health not good for >14 days (Figure 3F; Tables 2 and 3).
Figure 3. Choropleth maps CVD risk factor and health status indicator prevalence.
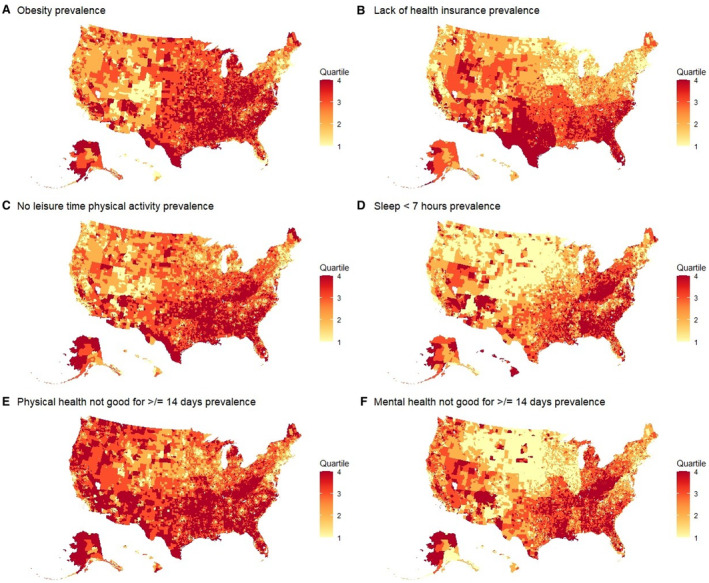
US choropleth maps of obesity prevalence (A), lack of health insurance prevalence (B), sleep <7 hours/night prevalence (C), prevalence rate of no leisure time physical activity (D), physical health unwell for ≥14 days (E), and prevalence rates of mental health unwell for ≥14 days (F) at the census tract level. Created using R programming. Source: CDC PLACES database. 15 CVD indicates cardiovascular disease.
Incremental Value of Environmental Factors Over Social Vulnerability
Multivariate Poisson regression was performed with SVM and EBM as covariates, as depicted in Table 3. The RRs across the EBM quartiles consistently increased from quartile 2 to quartile 4 of the EBM, relative to quartile 1 of the EBM. Interestingly, there was no notable difference between quartile 1 and quartile 2 of the EBM for many CVDs and risk factors. However, the RRs across the EBM quartiles consistently increased from quartile 2 to quartile 4 of the EBM, relative to quartile 1 of the EBM. The risk of having coronary artery disease 1.057 [95% CI,1.043‐1.0716] and stroke (RR, 1.118 [95% CI, 1.102–1.135]) was significantly higher in quartile 4 of the EBM than in quartile 1 of the EBM. The highest increase in the risk was noted for no leisure time physical activity, diabetes, and stroke (Table 3).
DISCUSSION
In the present analysis, using the census tract–level EJI and health measures, we show the combined impact of social and environmental factors on the prevalence of CVDs and risk factors. Increasing EJI quartiles (reflecting increased social and environmental adversities) were associated with an increased prevalence of cardiovascular disease and related risk factors. Additionally, we demonstrate that adverse environmental factors, independent of social determinants (Figure 4), affect health measures. These results indicate that increasing environmental burden and social vulnerability have an independent and deleterious effect on CVDs and risk factors in the United States (Figure 4).
Figure 4. Components of socio‐environmental EJI.
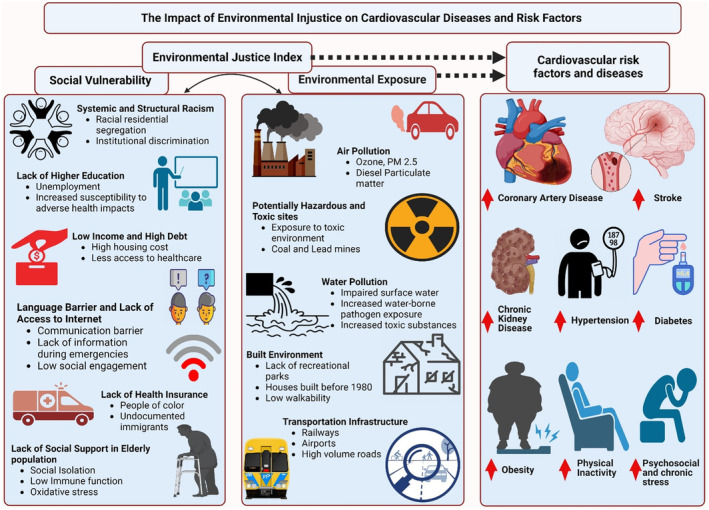
An increase in a composite burden of social vulnerability and environmental exposure predicts an increase in the prevalence of cardiovascular risk factors and diseases. An increase in environmental burden, independent of social vulnerability, predicts an increase in the prevalence of cardiovascular disease. Created using Biorender.com with publication license. EJI indicates environmental justice index.
This study builds on prior work by leveraging a novel composite index of environmental injustice, the CDC's EJI, to capture cumulative exposure across multiple domains. The EJI provides a more comprehensive measurement of environmental adversity than focusing only on air pollution, as in most previous studies. Our approach is also innovative in evaluating the effects of a unified index composed of environmental and social vulnerabilities. Rather than adjusting for social factors, we examine their interaction with environmental components. The 2‐model approach quantifies the incremental contribution of environmental burden above social factors. Prior neighborhood‐level studies have not consistently separated these intertwined exposures or formally tested incremental effects. Additionally, we leverage large national data sets, PLACES and EJI, to obtain stable precinct‐level estimates across the country. The sample size and geographic breadth provide generalizability and scope exceeding single‐city studies.
To the best of our knowledge, this is the first study to (1) examine the combined impact of social and environmental factors on health measures, (2) assess the impact of myriad environmental factors in an aggregate manner beyond just air pollution, and (3) demonstrate the incremental impact of environmental factors after adjusting for social determinants of health.
The current analysis showed a disparity in the demographic distribution across the EJI quartiles, with a higher percentage of White adults living in less vulnerable areas (EJI quartile 1) and a higher percentage of Black adults living in highly vulnerable areas (EJI quartile 4). This disparity is likely a result of many aspects of structural racism and segregation that have shaped neighborhoods in the United States for generations. For example, the redlining of predominantly Black population neighborhoods dating back to the 1930s, followed by public disinvestment, has led to poor air quality and other environmental risk factors in these locations. 17 , 18 , 19 Therefore, it is unsurprising that EJI quartile 4 also had the highest proportion of Hispanic individuals. Studies have shown that societies with disparities are more likely to suffer from pollution and environmental degradation. 17 , 20 , 21 While prior studies have examined individual social or environmental factors separately, our study is novel in using a composite index to capture joint exposure at the neighborhood level. Additionally, we go beyond air pollution to incorporate a broader set of environmental domains contributing to climate change. Therefore, the fight against climate change should also address social and economic disparities because these are closely linked to environmental quality.
Our study reported an increasing prevalence of adverse health‐related outcomes with increasing EJI. Several studies have reported the determinate effect of environmental pollution on health and CVD. 22 , 23 , 24 Although the role of particulate matter air pollution in the pathogenies of coronary artery disease, stroke, chronic kidney disease, and obesity has been well established, 25 , 26 , 27 it is notable that the EJI includes several other critical environmental factors beyond particulate matter air pollution, including exposure to other toxic materials, accessibility to recreational parks and overall walkability, proximity to polluting transportation infrastructure, and water pollution. The current study highlights additional factors that may be important for understanding composite environmental exposure on health outcomes beyond air pollution. This is particularly important for better understanding the complex interplay between the living environment and air pollution, social vulnerabilities, and health outcomes.
Our analysis also found that census tracts with higher environmental burden scores had higher cardiovascular risk factors and disease rates, independent of social vulnerability scores. While multiple studies have reported the detrimental effects of social and environmental factors on health measures individually, 28 limited data have reported an independent association of these factors with adverse health outcomes after accounting for one another. Prior studies have shown that at the county level, social deprivation and air pollution that consists of particles smaller than 2.5 microns have positive associations concerning cardiovascular and chronic kidney disease death. 29 , 30 Regions with high environmental pollution usually have a higher social vulnerability burden; hence, the effect can be masked. In a review of social inequalities in exposure to air pollution, a higher deprivation index and lower economic status were associated with higher particulate matter exposure. 31 , 32 , 33 Furthermore, economically disadvantaged minorities have less political power to fight environmental injustice in their proximity, and economic constraints further aggravate the burden of considering alternate residential options. 34 , 35 , 36 , 37
Our study additionally demonstrated that individuals with higher exposure to environmental adversities (EBM quartile 4) were at a higher risk of not engaging in leisure time physical activity and developing diabetes, in addition to other cardiovascular risk factors. This information provides additional preliminary insight into the increased risk of CVD with environmental adversities. It may help to develop short‐term targeted policies and point‐of‐care interventions for high‐risk individuals.
The recent establishment of the White House Office of Environmental Justice aimed to address the health impact of environmental pollution and its disproportionate effect on minority communities. The Inflation Reduction Act, which includes $369 billion in funding for climate and clean energy provisions, is estimated to provide substantial public health benefits across various disease domains. Additionally, racial and ethnic minorities are expected to have the largest relative reduction in deaths by 2050 with the implementation of the Inflation Reduction Act. 38 Other measures addressing this environmental injustice include the creation of the White House Environmental Justice Interagency Council, the White House Environmental Justice Advisory Council, and the Justice40 Initiative to provide at least 40% of the overall benefits of certain federal investments to communities that are marginalized, underserved, and overburdened by pollution. The Climate and Economic Justice Screening Tool and Environmental Justice Scorecard have been implemented at the administrative level to monitor and adapt the implementation of policies put forward by these agencies. The results presented in this study provide further motivation and support for the agenda of these agencies and strengthen the argument for more vigorous measures aimed at reducing social and environmental disparities.
Finally, as we embark on developing social determinants of health screening tools to collect information in health care settings to address individual patients' health‐related social needs, our study emphasizes the importance of understanding the collective impact of social and environmental factors, as they are both inseparable and independently associated with adverse outcomes. The current tools widely lack the consideration of environmental factors. Our study suggests the role of environmental factors in combination with social factors and the incremental role of environmental factors after adjusting for social factors. This makes a case for incorporating accurate information regarding individual patients' environmental risk factors.
Limitations
Despite its novelty, EJI is not a holistic indicator of all the environmental, social, and health vulnerabilities that communities face and, hence, cannot account for all the factors influencing cardiovascular health locally. 16 EJI does not represent a detailed risk or exposure assessment. 16 Additionally, because of the percentile method used for EJI, the relative weighting of the individual components of the social and environmental modules may not reflect their adverse health effects. Yet it could be a starting place to investigate variations in distributive and procedural justice contributing to health inequity. 16 As this analysis uses aggregate data at the census tract level, it is subject to ecological fallacy, and the associations found between neighborhood‐level factors and health outcomes may not apply at the individual level. Further confirmation using individual‐level data is needed, as relationships observed in aggregate ecological data do not necessarily translate to individuals. 39 Due to the lack of patient‐level data, we could not adjust for risk factors other than age, which could lead to potential confounding. 40 During the creation of EJI, data regarding drinking water quality, low infant birth weight, and pesticide usage was available at a coarser geographic resolution, for example, at the county level and not at the census tract level, so it could not be considered. 16 In the current scenario, EJI rank computations are based on recent historical data and do not factor in the measurements of uncertainty for EJI indicators; hence, it is essential to supplement the EJI data with local environmental and health mapping data for a holistic understanding of environmental injustice. 16
CONCLUSIONS
The current study, using the EJI developed by the CDC, demonstrates a graded increase in the prevalence of CVD and risk factors at a population level across the United States, with an increase in aggregate social and environmental adversities. Furthermore, a higher environmental burden continued to be associated with adverse health outcomes independent of social determinants. Policies to protect against climate change, reduce environmental pollution, and decrease social disparity are needed to improve cardiovascular health outcomes, particularly in vulnerable populations.
Sources of Funding
None.
Disclosures
Dr Nohria receives research support from Bristol Myers Squibb and consulting fees from Altathera Pharmaceuticals, AstraZeneca, Bantam Pharmaceuticals, Regeneron Pharmaceuticals, and Takeda Oncology. The remaining authors have no disclosures to report.
Supporting information
Data S1
Tables S1–S2
References 41–94
Acknowledgments
All authors participated in the research and preparation of the manuscript as per the International Committee of Medical Journal Editors.
S. Khadke and A. Kumar are co‐first authors.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.033428
For Sources of Funding and Disclosures, see page 11.
References
- 1. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, et al. Heart disease and stroke statistics—2021 update. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 2. Motairek I, Janus SE, Hajjari J, Nasir K, Khan SU, Rajagopalan S, Al‐Kindi S. Social vulnerability and excess mortality in the COVID‐19 era. Am J Cardiol. 2022;172:172–174. doi: 10.1016/j.amjcard.2022.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Janus SE, Makhlouf M, Chahine N, Motairek I, Al‐Kindi SG. Examining disparities and excess cardiovascular mortality before and during the COVID‐19 pandemic. Mayo Clin Proc. 2022;97:2206–2214. doi: 10.1016/j.mayocp.2022.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mohebi R, Chen C, Ibrahim NE, McCarthy CP, Gaggin HK, Singer DE, Hyle EP, Wasfy JH, Januzzi JL Jr. Cardiovascular disease projections in the United States based on the 2020 census estimates. J Am Coll Cardiol. 2022;80:565–578. doi: 10.1016/j.jacc.2022.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aggarwal R, Yeh RW, Joynt Maddox KE, Wadhera RK. Cardiovascular risk factor prevalence, treatment, and control in US adults aged 20 to 44 years, 2009 to March 2020. JAMA. 2023;329:899–909. doi: 10.1001/jama.2023.2307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jacobs DR Jr, Woo JG, Sinaiko AR, Daniels SR, Ikonen J, Juonala M, Kartiosuo N, Lehtimäki T, Magnussen CG, Viikari JSA, et al. Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med. 2022;386:1877–1888. doi: 10.1056/NEJMoa2109191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ganatra S, Dani SS, Kumar A, Khan SU, Wadhera R, Neilan TG, Thavendiranathan P, Barac A, Hermann J, Leja M, et al. Impact of social vulnerability on comorbid cancer and cardiovascular disease mortality in the United States. JACC CardioOncol. 2022;4:326–337. doi: 10.1016/j.jaccao.2022.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bhatnagar A. Environmental determinants of cardiovascular disease. Circ Res. 2017;121:162–180. doi: 10.1161/circresaha.117.306458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bevan G, Pandey A, Griggs S, Dalton JE, Zidar D, Patel S, Khan SU, Nasir K, Rajagopalan S, Al‐Kindi S. Neighborhood‐level social vulnerability and prevalence of cardiovascular risk factors and coronary heart disease. Curr Probl Cardiol. 2023;48:101182. doi: 10.1016/j.cpcardiol.2022.101182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bevan GH, Josephson R, Al‐Kindi SG. Socioeconomic deprivation and heart failure mortality in the United States. J Card Fail. 2020;26:1106–1107. doi: 10.1016/j.cardfail.2020.07.014 [DOI] [PubMed] [Google Scholar]
- 11. Bevan GH, Nasir K, Rajagopalan S, Al‐Kindi S. Socioeconomic deprivation and premature cardiovascular mortality in the United States. Mayo Clin Proc. 2022;97:1108–1113. doi: 10.1016/j.mayocp.2022.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Khan SU, Javed Z, Lone AN, Dani SS, Amin Z, Al‐Kindi SG, Virani SS, Sharma G, Blankstein R, Blaha MJ, et al. Social vulnerability and premature cardiovascular mortality among US counties, 2014 to 2018. Circulation. 2021;144:1272–1279. doi: 10.1161/CIRCULATIONAHA.121.054516 [DOI] [PubMed] [Google Scholar]
- 13. United States Census Bureau . The American Community Survey. Accessed August 28, 2023. https://www.census.gov/programssurveys/acs
- 14. Greenlund KJ, Lu H, Wang Y, Matthews KA, LeClercq JM, Lee B, Carlson SA. PLACES: local data for better health. Prev Chronic Dis. 2022;19:E31. doi: 10.5888/pcd19.210459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention . PLACES: Local Data for Better Health [2022]. Accessed August 28, 2023. https://www.data.cdc.gov/500‐Cities‐Places/PLACES‐Census‐Tract‐Data‐GIS‐Friendly‐Format‐2022‐/shc3‐fzig/data
- 16. Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry . EJI Technical Documentation [2022]. Accessed August 28, 2023. https://www.atsdr.cdc.gov/placeandhealth/eji/technical_documentation.html
- 17. Motairek I, Chen Z, Makhlouf MHE, Rajagopalan S, Al‐Kindi S. Historical neighbourhood redlining and contemporary environmental racism. Local Environ. 2023;28:518–528. doi: 10.1080/13549839.2022.2155942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Morello‐Frosch R, Obasogie OK. The climate gap and the color line—racial health inequities and climate change. N Engl J Med. 2023;388:943–949. doi: 10.1056/NEJMsb2213250 [DOI] [PubMed] [Google Scholar]
- 19. Motairek I, Lee EK, Janus S, Farkouh M, Freedman D, Wright J, Nasir K, Rajagopalan S, Al‐Kindi S. Historical neighborhood redlining and contemporary cardiometabolic risk. J Am Coll Cardiol. 2022;80:171–175. doi: 10.1016/j.jacc.2022.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cushing L, Morello‐Frosch R, Wander M, Pastor M. The haves, the have‐nots, and the health of everyone: the relationship between social inequality and environmental quality. Annu Rev Public Health. 2015;36:193–209. doi: 10.1146/annurev-publhealth-031914-122646 [DOI] [PubMed] [Google Scholar]
- 21. Motairek I, Rajagopalan S, Al‐Kindi S. The “heart” of environmental justice. Am J Cardiol. 2023;189:148–149. doi: 10.1016/j.amjcard.2022.11.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fuller R, Landrigan PJ, Balakrishnan K, Bathan G, Bose‐O'Reilly S, Brauer M, Caravanos J, Chiles T, Cohen A, Corra L, et al. Pollution and health: a progress update. Lancet Planet Health. 2022;6:e535–e547. doi: 10.1016/S2542-5196(22)00090-0 [DOI] [PubMed] [Google Scholar]
- 23. Juginović A, Vuković M, Aranza I, Biloš V. Health impacts of air pollution exposure from 1990 to 2019 in 43 European countries. Sci Rep. 2021;11:22516. doi: 10.1038/s41598-021-01802-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kelishadi R. Environmental pollution: health effects and operational implications for pollutants removal. J Environ Public Health. 2012;2012:341637. doi: 10.1155/2012/341637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rajagopalan S, Landrigan PJ. Pollution and the heart. N Engl J Med. 2021;385:1881–1892. doi: 10.1056/NEJMra2030281 [DOI] [PubMed] [Google Scholar]
- 26. Verhoeven JI, Allach Y, Vaartjes ICH, Klijn CJM, de Leeuw FE. Ambient air pollution and the risk of ischaemic and haemorrhagic stroke. Lancet Planet Health. 2021;5:e542–e552. doi: 10.1016/s2542-5196(21)00145-5 [DOI] [PubMed] [Google Scholar]
- 27. Xu X, Nie S, Ding H, Hou FF. Environmental pollution and kidney diseases. Nat Rev Nephrol. 2018;14:313–324. doi: 10.1038/nrneph.2018.11 [DOI] [PubMed] [Google Scholar]
- 28. Motairek I, Makhlouf MHE, Rajagopalan S, Al‐Kindi S. The exposome and cardiovascular health. Can J Cardiol. 2023;39:1191–1203. doi: 10.1016/j.cjca.2023.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Motairek I, Sharara J, Makhlouf MHE, Dobre M, Rahman M, Rajagopalan S, Al‐Kindi S. Association between particulate matter pollution and CKD mortality by social deprivation. Am J Kidney Dis. 2023;81:497–499. doi: 10.1053/j.ajkd.2022.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bevan GH, Freedman DA, Lee EK, Rajagopalan S, Al‐Kindi SG. Association between ambient air pollution and county‐level cardiovascular mortality in the United States by social deprivation index. Am Heart J. 2021;235:125–131. doi: 10.1016/j.ahj.2021.02.005 [DOI] [PubMed] [Google Scholar]
- 31. Fairburn J, Schüle SA, Dreger S, Karla Hilz L, Bolte G. Social inequalities in exposure to ambient air pollution: a systematic review in the WHO European region. Int J Environ Res Public Health. 2019;16:3127. doi: 10.3390/ijerph16173127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Josey KP, Delaney SW, Wu X, Nethery RC, DeSouza P, Braun D, Dominici F. Air pollution and mortality at the intersection of race and social class. N Engl J Med. 2023;388:1396–1404. doi: 10.1056/NEJMsa2300523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jbaily A, Zhou X, Liu J, Lee T‐H, Kamareddine L, Verguet S, Dominici F. Air pollution exposure disparities across US population and income groups. Nature. 2022;601:228–233. doi: 10.1038/s41586-021-04190-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shrestha R, Flacke J, Martinez J, van Maarseveen M. Environmental health related socio‐spatial inequalities: identifying “hotspots” of environmental burdens and social vulnerability. Int J Environ Res Public Health. 2016;13:691. doi: 10.3390/ijerph13070691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mennis JL, Jordan L. The distribution of environmental equity: exploring spatial nonstationarity in multivariate models of air toxic releases. Ann Assoc Am Geogr. 2005;95:249–268. doi: 10.1111/j.1467-8306.2005.00459.x [DOI] [Google Scholar]
- 36. Raddatz L, Mennis J. Environmental justice in Hamburg, Germany. Prof Geogr. 2013;65:495–511. doi: 10.1080/00330124.2012.700500 [DOI] [Google Scholar]
- 37. Hamilton JT. Testing for environmental racism: prejudice, profits, political power? J Policy Anal Manage. 1995;14:107–132. doi: 10.2307/3325435 [DOI] [Google Scholar]
- 38. Levy JI. 2022 Inflation Reduction Act: climate investments are public health investments. Am J Public Health. 2022;112:1525. doi: 10.2105/AJPH.2022.307089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shih Y‐CT, Bradley C, Yabroff KR. Ecological and individualistic fallacies in health disparities research. JNCI J Natl Cancer Inst. 2023;115:488–491. doi: 10.1093/jnci/djad047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Centers for Disease Control and Prevention, Agency for Toxic Substances Disease Registry . Environmental Justice Index [2022]. Database. Accessed February 20, 2023. https://www.atsdr.cdc.gov/placeandhealth/eji/index.html
- 41. Cutter SL, Boruff BJ, Shirley WL. Social vulnerability to environmental hazards*. Soc Sci Q. 2003;84:242–261. doi: 10.1111/1540-6237.8402002 [DOI] [Google Scholar]
- 42. Cutter SL, Emrich CT. Moral hazard, social catastrophe: the changing face of vulnerability along the hurricane coasts. Ann Am Acad Pol Soc Sci. 2006;604:102–112. doi: 10.1177/0002716205285515 [DOI] [Google Scholar]
- 43. Flanagan BE, Gregory EW, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J Homeland Secur Emerg Manag. 2011;8:0000102202154773551792. doi: 10.2202/1547-7355.1792 [DOI] [Google Scholar]
- 44. Huang G, London J. Mapping cumulative environmental effects, social vulnerability, and health in the San Joaquin Valley, California. Am J Public Health. 2012;102:830–832. doi: 10.2105/ajph.2011.300466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sadd JL, Pastor M, Morello‐Frosch R, Scoggins J, Jesdale B. Playing it safe: assessing cumulative impact and social vulnerability through an environmental justice screening method in the South Coast Air Basin, California. Int J Environ Res Public Health. 2011;8:1441–1459. doi: 10.3390/ijerph8051441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Morello‐Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff (Millwood). 2011;30:879–887. doi: 10.1377/hlthaff.2011.0153 [DOI] [PubMed] [Google Scholar]
- 47. Clougherty JE, Kubzansky LD. A framework for examining social stress and susceptibility to air pollution in respiratory health. Environ Health Perspect. 2009;117:1351–1358. doi: 10.1289/ehp.0900612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bullard RD, Mohai P, Saha R, Wright B. Toxic wastes and race at twenty: why race still matters after all of these years. Environ Law. 2008;38:371–411. [Google Scholar]
- 49. Mohai P, Bryant B. Race, poverty & the distribution of environmental hazards: reviewing the evidence. Race Poverty Environ. 1991;2:3–27. [Google Scholar]
- 50. Mohai P, Saha R. Which came first, people or pollution? Assessing the disparate siting and post‐siting demographic change hypotheses of environmental injustice. Environ Res Lett. 2015;10:115008. doi: 10.1088/1748-9326/10/11/115008 [DOI] [Google Scholar]
- 51. Evans GW, Kim P. Childhood poverty, chronic stress, self‐regulation, and coping. Child Dev Perspect. 2013;7:43–48. doi: 10.1111/cdep.12013 [DOI] [Google Scholar]
- 52. Haushofer J, Fehr E. On the psychology of poverty. Science. 2014;344:862–867. doi: 10.1126/science.1232491 [DOI] [PubMed] [Google Scholar]
- 53. Padula AM, Mortimer KM, Tager IB, Hammond SK, Lurmann FW, Yang W, Stevenson DK, Shaw GM. Traffic‐related air pollution and risk of preterm birth in the San Joaquin Valley of California. Ann Epidemiol. 2014;24:888–895.e4. doi: 10.1016/j.annepidem.2014.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Helfand GE, Peyton LJ. A conceptual model of environmental justice. Soc Sci Q. 1999;80:68–83. [Google Scholar]
- 55. Gray SC, Edwards SE, Schultz BD, Miranda ML. Assessing the impact of race, social factors and air pollution on birth outcomes: a population‐based study. Environ Health. 2014;13:4. doi: 10.1186/1476-069X-13-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bullard RD. The threat of environmental racism. Nat Resour Environ. 1993;7:23–56. [Google Scholar]
- 57. Dettenborn L, Tietze A, Bruckner F, Kirschbaum C. Higher cortisol content in hair among long‐term unemployed individuals compared to controls. Psychoneuroendocrinology. 2010;35:1404–1409. doi: 10.1016/j.psyneuen.2010.04.006 [DOI] [PubMed] [Google Scholar]
- 58. Malcoe LH, Lynch RA, Keger MC, Skaggs VJ. Lead sources, behaviors, and socioeconomic factors in relation to blood lead of Native American and White children: a community‐based assessment of a former mining area. Environ Health Perspect. 2002;110(Suppl 2):221–231. doi: 10.1289/ehp.02110s2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Meltzer R, Schwartz A. Housing affordability and health: evidence from New York City. Hous Policy Debate. 2016;26:80–104. doi: 10.1080/10511482.2015.1020321 [DOI] [Google Scholar]
- 60. Mulchandani R, Smith M, Armstrong B, Beck CR, Oliver I. Effect of insurance‐related factors on the association between flooding and mental health outcomes. Int J Environ Res Public Health. 2019;16:1174. doi: 10.3390/ijerph16071174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Early J, Hernandez A. Digital disenfranchisement and COVID‐19: broadband internet access as a social determinant of health. Health Promot Pract. 2021;22:605–610. doi: 10.1177/15248399211014490 [DOI] [PubMed] [Google Scholar]
- 62. Andrew MK, Keefe JM. Social vulnerability from a social ecology perspective: a cohort study of older adults from the National Population Health Survey of Canada. BMC Geriatr. 2014;14:90. doi: 10.1186/1471-2318-14-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Chakraborty TC, Newman AJ, Qian Y, Hsu A, Sheriff G. Residential segregation and outdoor urban moist heat stress disparities in the United States. One Earth. 2023;6:738–750. doi: 10.1016/j.oneear.2023.05.016 [DOI] [Google Scholar]
- 64. Dales RE, Cakmak S. Does mental health status influence susceptibility to the physiologic effects of air pollution? A population based study of Canadian children. PLoS One. 2016;11:e0168931. doi: 10.1371/journal.pone.0168931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Gee GC, Ponce N. Associations between racial discrimination, limited English proficiency, and health‐related quality of life among 6 Asian ethnic groups in California. Am J Public Health. 2010;100:888–895. doi: 10.2105/AJPH.2009.178012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Pellow DN. Struggles for environmental justice in US prisons and jails. Antipode. 2021;53:56–73. doi: 10.1111/anti.12569 [DOI] [Google Scholar]
- 67. Broomandi P, Guney M, Kim JR, Karaca F. Soil contamination in areas impacted by military activities: a critical review. Sustainability. 2020;12:9002. doi: 10.3390/su12219002 [DOI] [Google Scholar]
- 68. Maantay J. Zoning law, health, and environmental justice: what's the connection? J Law Med Ethics. 2002;30:572–593. doi: 10.1111/j.1748-720X.2002.tb00427.x [DOI] [PubMed] [Google Scholar]
- 69. Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, Villeneuve PJ, Jerrett M, Goldberg MS, Pope CA III, et al. Ambient PM2.5, O₃, and NO₂ exposures and associations with mortality over 16 years of follow‐up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect. 2015;123:1180–1186. doi: 10.1289/ehp.1409276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Dockery DW, Pope CA. Acute respiratory effects of particulate air pollution. Annu Rev Public Health. 1994;15:107–132. doi: 10.1146/annurev.pu.15.050194.000543 [DOI] [PubMed] [Google Scholar]
- 71. Ristovski ZD, Miljevic B, Surawski NC, Morawska L, Fong KM, Goh F, Yang IA. Respiratory health effects of diesel particulate matter. Respirology. 2012;17:201–212. doi: 10.1111/j.1440-1843.2011.02109.x [DOI] [PubMed] [Google Scholar]
- 72. Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103:2810–2815. doi: 10.1161/01.cir.103.23.2810 [DOI] [PubMed] [Google Scholar]
- 73. Wu J, Wilhelm M, Chung J, Ritz B. Comparing exposure assessment methods for traffic‐related air pollution in an adverse pregnancy outcome study. Environ Res. 2011;111:685–692. doi: 10.1016/j.envres.2011.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Pearsall H, Anguelovski I. Contesting and resisting environmental gentrification: responses to new paradoxes and challenges for urban environmental justice. Sociol Res Online. 2016;21:6–127. doi: 10.5153/sro.3979 [DOI] [Google Scholar]
- 75. Brown‐Amilian S, Akolade Y. Disparities in COPD hospitalizations: a spatial analysis of proximity to toxics release inventory facilities in Illinois. Int J Environ Res Public Health. 2021;18:13128. doi: 10.3390/ijerph182413128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Wilson‐Salandy S, Nies MA. The effect of physical activity on the stress management, interpersonal relationships, and alcohol consumption of college freshmen. SAGE Open. 2012;2:2158244012464975. doi: 10.1177/2158244012464975 [DOI] [Google Scholar]
- 77. DeFelice Nicholas B, Johnston Jill E, Gibson Jacqueline M. Reducing emergency department visits for acute gastrointestinal illnesses in North Carolina (USA) by extending community water service. Environ Health Perspect. 2016;124:1583–1591. doi: 10.1289/EHP160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Maria K, Xiaoyu H, Ma J, Lessner L, Carpenter DO. Increased rate of hospitalization for diabetes and residential proximity of hazardous waste sites. Environ Health Perspect. 2007;115:75–79. doi: 10.1289/ehp.9223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Hendryx M, Ahern MM. Relations between health indicators and residential proximity to coal mining in West Virginia. Am J Public Health. 2008;98:669–671. doi: 10.2105/ajph.2007.113472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Hendryx M, Luo J. An examination of the effects of mountaintop removal coal mining on respiratory symptoms and COPD using propensity scores. Int J Environ Health Res. 2015;25:265–276. doi: 10.1080/09603123.2014.938027 [DOI] [PubMed] [Google Scholar]
- 81. Ahern AL, Olson AD, Aston LM, Jebb SA. Weight Watchers on prescription: an observational study of weight change among adults referred to Weight Watchers by the NHS. BMC Public Health. 2011;11:434. doi: 10.1186/1471-2458-11-434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ducatman A, LaPier J, Fuoco R, DeWitt JC. Official health communications are failing PFAS‐contaminated communities. Environ Health. 2022;21:51. doi: 10.1186/s12940-022-00857-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Bedimo‐Rung AL, Mowen AJ, Cohen DA. The significance of parks to physical activity and public health: a conceptual model. Am J Prev Med. 2005;28:159–168. doi: 10.1016/j.amepre.2004.10.024 [DOI] [PubMed] [Google Scholar]
- 84. Bojorquez I, Ojeda‐Revah L. Urban public parks and mental health in adult women: mediating and moderating factors. Int J Soc Psychiatry. 2018;64:637–646. doi: 10.1177/0020764018795198 [DOI] [PubMed] [Google Scholar]
- 85. Cohen DA, Marsh T, Williamson S, Derose KP, Martinez H, Setodji C, McKenzie TL. Parks and physical activity: why are some parks used more than others? Prev Med. 2010;50(Suppl 1):S9–S12. doi: 10.1016/j.ypmed.2009.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Boone CG, Buckley GL, Grove JM, Sister C. Parks and people: an environmental justice inquiry in Baltimore, Maryland. Ann Assoc Am Geogr. 2009;99:767–787. doi: 10.1080/00045600903102949 [DOI] [Google Scholar]
- 87. Lanphear BP, Hornung R, Khoury J, Yolton K, Baghurst P, Bellinger DC, Canfield RL, Dietrich KN, Bornschein R, Greene T, et al. Low‐level environmental lead exposure and children's intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113:894–899. doi: 10.1289/ehp.7688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Awuor L, Melles S. The influence of environmental and health indicators on premature mortality: an empirical analysis of the City of Toronto's 140 neighborhoods. Health Place. 2019;58:102155. doi: 10.1016/j.healthplace.2019.102155 [DOI] [PubMed] [Google Scholar]
- 89. Stowe EW, Hughey SM, Hallum SH, Kaczynski AT. Associations between walkability and youth obesity: differences by urbanicity. Child Obes. 2019;15:555–559. doi: 10.1089/chi.2019.0063 [DOI] [PubMed] [Google Scholar]
- 90. Boothe VL, Shendell DG. Potential health effects associated with residential proximity to freeways and primary roads: review of scientific literature, 1999–2006. J Environ Health. 2008;70:33–41. [PubMed] [Google Scholar]
- 91. Öhrström E, Hadzibajramovic E, Holmes M, Svensson H. Effects of road traffic noise on sleep: studies on children and adults. J Environ Psychol. 2006;26:116–126. doi: 10.1016/j.jenvp.2006.06.004 [DOI] [Google Scholar]
- 92. Nunes LM, Zhu YG, Stigter TY, Monteiro JP, Teixeira MR. Environmental impacts on soil and groundwater at airports: origin, contaminants of concern and environmental risks. J Environ Monit. 2011;13:3026–3039. doi: 10.1039/C1EM10458F [DOI] [PubMed] [Google Scholar]
- 93. McKee AM, Cruz MA. Microbial and viral indicators of pathogens and human health risks from recreational exposure to waters impaired by fecal contamination. J Sustain Water Built Environ. 2021;7:03121001. doi: 10.1061/JSWBAY.0000936 [DOI] [Google Scholar]
- 94. Dórea JG. Persistent, bioaccumulative and toxic substances in fish: human health considerations. Sci Total Environ. 2008;400:93–114. doi: 10.1016/j.scitotenv.2008.06.017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Tables S1–S2
References 41–94


