Isolated functional tricuspid regurgitation (Is‐FTR), characterized by the absence of organic, left‐sided, or pulmonary hypertension causes, is relatively common, reported in 8% of tricuspid regurgitation case burden. 1 While in pilot studies, incrementally worse outcome was associated with increasing Is‐FTR severity, 1 doubts remain as this form of functional tricuspid regurgitation (FTR) appears to show that it is not the most severe form of FTR, 1 and recent consensus documents affirmed considerable gaps in knowledge on natural history. 2 In view of advanced age of affected patients, intrinsic outcome implications warrant defining its associated risk of excess mortality under medical management compared with the general population.
Thus, this study conducted in 7 French centers (Amiens, Lille, Nancy, Nantes, Rennes, Saint Denis, and Toulouse) identified retrospectively patients with moderate‐to‐severe or greater Is‐FTR diagnosed between 2013 and 2021 with their clinical/echocardiographic information prospectively collected at diagnosis. Is‐FTR was defined by moderate‐to‐severe or greater FTR with structurally normal tricuspid valves without pacemaker lead, mild or less left‐sided valvular disease, no pulmonary hypertension, preserved left ventricular ejection fraction (>50%), and no previous cardiac surgery. 1 , 3 , 4 Is‐FTR severity was assessed by Doppler echocardiography based on current guidelines using an integrative multiparametric approach. 5 Informed consent was waived because of the retrospective nature of the study. The data that support the findings of this study are available from the corresponding author on reasonable request.
The main end point was survival under conservative management, and patients who underwent tricuspid transcatheter/surgical treatment during follow‐up (60 surgeries and 26 edge‐to‐edge repairs) were censored at procedure date. The cohort included 715 consecutive patients with median follow‐up of 22 (interquartile range, 8–36) months. Each patient with Is‐FTR was matched to all individuals with the same birth year and sex in France to estimate expected survival, using French life tables established by population census. 4 Relative survival (RS) was computed as the ratio between estimated/expected survival. The study was approved by an independent ethics committee.
The main baseline characteristics of the study population (mean±SD age, 75±12 years; 61.5% women) are presented in Figure [A] and are in line with previous reports. 1 , 2 , 3 , 4 During follow‐up, 175 deaths (24.4%) occurred, of which 92 (52.5%) were cardiovascular. Survival rates of patients with moderate‐to‐severe or greater Is‐FTR were lower than expected survival rates (Figure [B]): 85%±1% versus 93% at 1 year and 57%±3% versus 71% at 5 years (RS, 80%). Moreover, this reduction in 5‐year survival compared with expected was observed in all strata of the population, for both men (52%±5% versus 69%; RS, 75%) and women (60%±4% versus 72%; RS, 83%), in patients with Charlson Comorbidity Index ≤2 (66%±5% versus 75%; RS, 88%) or >2 (50%± 4% versus 68%; RS, 73%), in atrial fibrillation (54%±4% versus 69%; RS, 78%), or in sinus rhythm (64%±6% versus 92%; RS, 78%), with right ventricular dysfunction (43%±4% versus 71%; RS, 60%) or without right ventricular dysfunction (66%±4% versus 71%; RS, 93%), and with severe tricuspid regurgitation (TR) (52%±4% versus 71%; RS, 73%) or moderate‐to‐severe TR (62%±5% versus 72%; RS, 86%). Using a robust estimation of SEs in the Cox model, after adjustment for age, sex, Charlson Comorbidity Index, atrial fibrillation, and right ventricular dysfunction, severe TR was associated with increased mortality compared with moderate‐to‐severe TR (hazard ratio [95% CI], 1.46 [1.05–1.78]; P=0.021).
Figure 1. Characteristics and survival of patients with isolated functional tricuspid regurgitation (Is‐FTR).
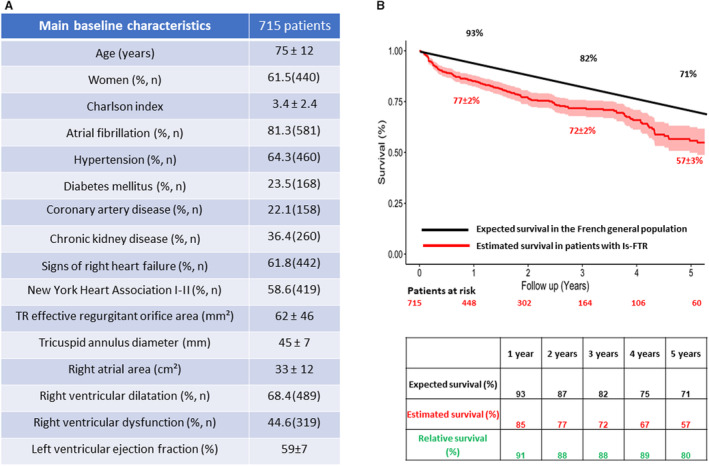
A, Main baseline characteristics of the study population. B, Five‐year estimated survival of patients with Is‐FTR compared with that of the age‐ and sex‐matched general population.
This first study on the comparison of survival in patients with clinically significant (moderate‐to‐severe or greater) Is‐FTR to that in the general population shows, for the first time to our knowledge, that this disease under conservative management is associated with excess mortality relative to expected survival in the general population. This negative outcome is found in all subgroup strata by comorbidity, cardiac rhythm, right ventricular function, or TR severity. A previous study has reported that patients with severe Is‐FTR experience higher mortality than those with less severe degrees of TR. 3 A low 5‐year survival rate of 52% has been observed in a study of 89 patients with severe Is‐FTR, 1 close to that found in our study.
This study involved retrospective identification of subjects with inherent limitations, but all descriptors were collected prospectively at baseline. Thus, although Is‐FTR is not the most severe type of FTR, it is associated in all subsets possible with excess mortality, underscoring the serious nature of the condition. The inclusion of patients from tertiary centers only may have led to selection bias. As expected, atrial fibrillation in our population with Is‐FTR, a classic cause or consequence of the disease, was frequent, but excess mortality was present irrespective of the cardiac rhythm. Comorbidity index related to advanced age was comparable to that previously reported. 1 , 3 , 4
Our results contribute to underscoring the seriousness of clinical outcomes incurred by patients with Is‐FTR, show the limits of conservative treatment of these patients, and suggest consideration of earlier surgical or percutaneous management based on criteria that will be better defined by ongoing and future clinical trials. Further studies are also warranted to define the optimal timing for tricuspid valve intervention in Is‐FTR.
Sources of Funding
None.
Disclosures
None.
This manuscript was sent to Amgad Mentias, MD, Associate Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 3.
References
- 1. Topilsky Y, Maltais S, Medina Inojosa J, Oguz D, Michelena H, Maalouf J, Mahoney DW, Enriquez‐Sarano M. Burden of tricuspid regurgitation in patients diagnosed in the community setting. JACC Cardiovasc Imaging. 2019;12:433–442. doi: 10.1016/j.jcmg.2018.06.014 [DOI] [PubMed] [Google Scholar]
- 2. Grapsa J, Praz F, Sorajja P, Cavalcante JL, Sitges M, Taramasso M, Piazza N, Messika‐Zeitoun D, Michelena HI, Hamid N, et al. Tricuspid regurgitation: from imaging to clinical trials to resolving the unmet need for treatment. JACC Cardiovasc Imaging. 2024;17:79–95. doi: 10.1016/j.jcmg.2023.08.013 [DOI] [PubMed] [Google Scholar]
- 3. Topilsky Y, Nkomo VT, Vatury O, Michelena HI, Letourneau T, Suri RM, Pislaru S, Park S, Mahoney DW, Biner S, et al. Clinical outcome of isolated tricuspid regurgitation. JACC Cardiovasc Imaging. 2014;7:1185–1194. doi: 10.1016/j.jcmg.2014.07.018 [DOI] [PubMed] [Google Scholar]
- 4. Bohbot Y, Chadha G, Delabre J, Landemaine T, Beyls C, Tribouilloy C. Characteristics and prognosis of patients with significant tricuspid regurgitation. Arch Cardiovasc Dis. 2019;112:604–614. doi: 10.1016/j.acvd.2019.06.011 [DOI] [PubMed] [Google Scholar]
- 5. Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA, Badano L, Zamorano JL. Scientific document Committee of the European Association of cardiovascular imaging. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2013;14:611–644. doi: 10.1093/ehjci/jet105 [DOI] [PubMed] [Google Scholar]


