Abstract
The genome of a candidate dengue type 2 (DEN-2) vaccine virus, strain PDK-53, differs from its DEN-2 16681 parent by nine nucleotides. Using infectious cDNA clones, we constructed 18 recombinant 16681/PDK-53 viruses to analyze four 16681-to-PDK-53 mutations, including 5′ noncoding region (5′NC)-57 C-to-T, premembrane (prM)-29 Asp-to-Val (the only mutation that occurs in the structural proteins), nonstructural protein 1 (NS1)-53 Gly-to-Asp, and NS3-250 Glu-to-Val. The viruses were studied for plaque size, growth rate, and temperature sensitivity in LLC-MK2 cells, growth rate in C6/36 cells, and neurovirulence in newborn mice. All of the viruses replicated to peak titers of 107.3 PFU/ml or greater in LLC-MK2 cells. The crippled replication of PDK-53 virus in C6/36 cells and its attenuation for mice were determined primarily by the 5′NC-57-T and NS1-53-Asp mutations. The temperature sensitivity of PDK-53 virus was attributed to the NS1-53-Asp and NS3-250-Val mutations. The 5′NC-57, NS1-53, and NS3-250 loci all contributed to the small-plaque phenotype of PDK-53 virus. Reversions at two or three of these loci in PDK-53 virus were required to reconstitute the phenotypic characteristics of the parental 16681 virus. The prM-29 locus had little or no effect on viral phenotype. Sequence analyses showed that PDK-53 virus is genetically identical to PDK-45 virus. Restriction of the three major genetic determinants of attenuation markers to nonstructural genomic regions makes the PDK-53 virus genotype attractive for the development of chimeric DEN virus vaccine candidates.
Dengue (DEN) viruses belong to the genus Flavivirus (family Flaviviridae) (66). Flaviviruses contain a single-stranded, positive-sense RNA genome of approximately 11 kb. The RNA genome is capped at the 5′ end and lacks a 3′-terminal poly(A) tail. The gene order is 5′ noncoding region (5′NC)-capsid-premembrane/membrane (prM/M)-envelope (E)-nonstructural protein 1 (NS1)-NS2A-NS2B-NS3-NS4A-NS4B-NS5-3′NC. Three structural and seven nonstructural proteins are co- and posttranslationally processed from the polyprotein precursor by both virus-specified and cellular proteases (14, 66).
DEN viruses are classified antigenically as four serotypes (DEN-1, DEN-2, DEN-3, and DEN-4). Infection with any of these serotypes can produce clinical illness, ranging from a nonspecific febrile syndrome to severe and fatal dengue hemorrhagic fever/dengue shock syndrome (DHF/DSS). An immunopathological response following secondary infection of humans with a heterologous serotype of DEN virus may be one of the risk factors for the more severe forms of the disease (25, 29, 48, 50). Transmission of DEN virus has increased during the past 10 years because of the worldwide distribution of Aedes aegypti mosquitoes in the tropics and subtropics. Currently, an estimated 100 million cases of dengue fever occur each year, and DHF is a leading cause of death and hospitalization of children in many countries of Asia and South America (27).
An effective vaccine against DEN virus is currently not available. Live attenuated vaccine candidates for all four serotypes have been developed by serial passage of wild-type viruses in primary dog kidney (PDK) cells or other cell types at Mahidol University, Bangkok, Thailand (70). The Mahidol candidate DEN-2 vaccine virus, strain PDK-53, was derived by passaging the wild-type DEN-2 16681 virus 53 times in PDK cells. The PDK-53 virus has several biological markers associated with attenuation, including temperature sensitivity, small plaque size, loss of neurovirulence for suckling mice, and decreased incidence of viremia in monkeys (70). In one report, all 7 monkeys challenged with DEN-2 16681 virus, but only 2 of 10 challenged with PDK-53 virus, had detectable viremia (viral titers not reported) (70). In another report, PDK-53 virus was minimally neurotropic for rhesus monkeys, and no viremia was detected (by the direct plaque method in LLC-MK2 cells) in monkeys challenged intramuscularly, intracerebrally, and intraspinally with either 16681 or PDK-53 virus (1). DEN-2 16681 virus itself was only weakly neurovirulent in these monkeys (1). None of the monkeys had detectable prechallenge neutralizing antibodies against any of the four DEN virus serotypes (1). Clinical trials of the candidate PDK-53 virus vaccine have shown that it is safe and immunogenic in humans (4, 6, 65) and induces DEN virus-specific T-cell memory responses in human vaccinees (19). To prevent the possible occurrence of DHF/DSS in vaccinees, a tetravalent vaccine is needed to provide immunity against all four serotypes of the virus.
We previously identified nine nucleotide mutations (three silent) between the genomes of the DEN-2 16681 and PDK-53 viruses (32). One C-to-T (16681-to-PDK-53) nucleotide mutation occurs at genome nucleotide position (nt) 57 in the 5′NC region. Five nucleotide mutations encode amino acid substitutions Asp-to-Val at prM-29, Gly-to-Asp at NS1-53, Leu-to-Phe at NS2A-181, Glu-to-Val at NS3-250, and Gly-to-Ala at NS4A-75. The candidate PDK-53 virus vaccine has a mixed genotype at genome nt 5270: a significant portion (approximately 29%) of the virus population encodes the NS3-250-Glu that is present in the parental DEN-2 16681 virus. In the present study, we investigated several genetic loci as possible determinants of in vitro and in vivo markers of attenuation in the candidate PDK-53 virus vaccine by analyzing a panel of recombinant DEN-2 16681/PDK-53 viruses. These viruses were engineered by recombination of full genome-length cDNA clones derived from both DEN-2 16681 and PDK-53 viruses (32).
MATERIALS AND METHODS
Viruses and cell cultures.
The parental DEN-2 16681 virus, several intermediate PDK passages (PDK-5, -10, -14, -35, and -45) of 16681 virus, recombinant 16681/PDK-53 viruses, and the genetically characterized LLC-MK2-1 passage (32) of the candidate PDK-53 vaccine virus were investigated.
Cell cultures of BHK-21 (clone 15), LLC-MK2, Vero, and C6/36 were grown in Dulbecco's modified minimal essential medium (DMEM) supplemented with 10% heat-inactivated (56°C for 30 min) fetal bovine serum (FBS; HyClone Laboratories, Inc., Logan, Utah), sodium bicarbonate (3.7 g/liter; GIBCO-BRL, Life Technologies, Gaithersburg, Md.), and penicillin G (100 U/ml)-streptomycin sulfate (100 μg/ml) (GIBCO-BRL).
Plaque titrations were performed in confluent monolayers of Vero cells in plastic six-well plates as described previously (47). A 200-μl inoculum of virus was adsorbed for 1.5 h at 37°C, followed by the addition of 4 ml of agarose overlay medium containing 1% SeaKem LE agarose (FMC BioProducts, Rockland, Maine) in nutrient medium (0.165% lactalbumin hydrolysate [Difco Laboratories, Detroit, Mich.], 0.033% yeast extract [Difco], Earle's balanced salt solution, 25 mg of gentamicin sulfate [BioWhittaker, Walkersville, Md.] and 1.0 mg of amphotericin B [Fungizone; E. R. Squibb & Sons, Princeton, N.J.] per liter, 2% FBS). Following incubation at 37°C for 7 days, a second 2-ml agarose overlay containing neutral red vital stain (80 μg/ml; GIBCO-BRL) was added.
Construction of recombinant DEN-2 16681/PDK-53 viruses.
During the genetic validation of clone-derived DEN-2 viruses in the present study, we discovered two cDNA cloning errors, nt 6665 A-to-G (NS4A-97 Tyr-to-Cys) and nt 8840 A-to-G (NS5-424 Glu-to-Gly), in the previously reported PDK-53 virus-specific pD2/IC-130Vc-K (NS3-250-Val variant) clone (32). These defects were corrected in a newly derived PDK-53 virus-specific (NS3-250-Val variant) clone, pD2/IC-VV45R.
In preliminary studies, we derived recombinant 16681/PDK-53 viruses, each containing PDK-53 virus-specific gene regions within the genetic background of 16681 virus, to investigate the genetic loci involved in the attenuation markers of PDK-53 virus (unpublished data). Analyses of these viruses indicated that the PDK-53 mutation at nt 57 in the 5′NC region (5′NC-57) and the amino acid mutations at NS1-53 (analyzed in a linked manner with the NS2A-181 mutation) and NS3-250 were likely determinants of the PDK-53 virus-specific phenotype (unpublished data). The prM-29 mutation appeared to have little effect. Because the 5′NC mutation occurred in a possible stem structure, and the NS1 and NS3 mutations occurred at loci that are conserved among various flaviviruses (analyses not shown), we decided to investigate these three genetic loci individually and in all possible combinations. We constructed 14 recombinant pD2/IC-16681/PDK-53 plasmids (Table 1) by exchanging cDNA fragments between pD2/IC-30P-A (16681 clone) and pD2/IC-VV45R (PDK-53 clone) at restriction enzyme sites SstI (preceding the T7 promoter), SalI (nt 165), SphI (nt 1380), SpeI (nt 2370 and 3579), KpnI (nt 4493), XhoI (nt 5426), and XbaI (3′ end of the clone). All recombinant plasmids were grown in Escherichia coli XLI-Blue and were linearized at the unique XbaI site engineered at the 3′ terminus of the cDNA. BHK-21 cells were transfected with transcribed viral RNA by the method of Liljeström et al. (37) as described previously (32).
TABLE 1.
Genotypes of recombinant DEN-2 16681/PDK-53 viruses
| Clone-derived virus (cognate)b | DEN-2 16681 virus determinants in PDK-53 virus backgrounda
|
DEN-2 PDK-53 determinants in 16681 backgroundc
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5′NC-57 | prM-29 | NS1-53 | NS2A-181 | NS3-250 | NS4A-75 | 5′NC-57 | prM-29 | NS1-53 | NS2A-181 | NS3-250 | NS4A-75 | |
| DEN-2 PDK-53 | t | V | D | F | V | A | ||||||
| VV45R (V513) | · | · | · | · | · | · | ||||||
| P5 (V13) | c | · | · | · | · | · | ||||||
| P1 (V53) | · | · | G | · | · | · | ||||||
| P3 (V51) | · | · | · | · | E | · | ||||||
| P51 (V3) | c | · | G | · | · | · | ||||||
| P53 (V1) | c | · | · | · | E | · | ||||||
| P13 (V5) | · | · | G | · | E | |||||||
| P513 (30P-A) | c | · | G | · | E | · | ||||||
| DEN-2 16681 | c | D | G | L | E | G | ||||||
| 30P-A (P513) | · | · | · | · | · | · | ||||||
| V5 (P13) | t | · | · | · | · | · | ||||||
| V1 (P53) | · | · | D | · | · | · | ||||||
| V3 (P51) | · | · | · | · | V | · | ||||||
| V51 (P3) | t | · | D | · | · | · | ||||||
| V53 (P1) | t | · | · | · | V | · | ||||||
| V13 (P5) | · | · | D | · | V | · | ||||||
| V513 (VV45R) | t | · | D | · | V | · | ||||||
The genome of the candidate DEN-2 PDK-53 vaccine virus differs from that of its 16681 parent at nine nucleotide loci, including three silent mutations (not shown), a mutation at genome 5′NC-57 (lowercase letters), and five nucleotides encoding amino acid mutations (uppercase, single-letter abbreviations) at viral polypeptide positions prM-29, NS1-53, NS2A-181, NS3-250, and NS4A-75 (32). Genetic loci from the parental 16681 virus were engineered into the cDNA background of the PDK-53 virus-specific infectious clone, pD2/IC-VV45R. Dots indicate sequence identity with PDK-53 virus (NS3-250-Val variant). The candidate PDK-53 vaccine also contains a genetic variant that has Glu at NS3-250 (32).
The genotypes of wild-type DEN-2 16681 virus, its attenuated vaccine derivative, DEN-2 PDK-53 virus, infectious clone-derived VV45R (genetically equivalent to the PDK-53 NS3-250-Val variant) and 30P-A (equivalent to wild-type 16681) viruses, and recombinant 16681/PDK-53 viruses are shown. For designations of recombinant Px and Vx viruses, see Materials and Methods. P5 and V13 are cognate viruses, assuming that the PDK-53 virus-specific phenotype is determined predominantly by the 5′NC-57, NS1-53, and NS3-250 loci. Both P5 and V13 viruses contain the 5′NC-57-c, NS1-53-Asp, and NS3-250-Val loci within the genetic backgrounds of PDK-53 and 16681 viruses, respectively.
Genetic loci from PDK-53 virus were engineered into the cDNA background of the 16681 virus-specific infectious clone, pD2/IC-30P-A. Dots indicate sequence identity with 16681 virus.
The genotypes of the recombinant D2/IC-Px (where x = 5, 1, and/or 3 to indicate the incorporation of the parental [P in the virus designation] 16681 virus-specific 5′NC-57, NS1-53, and/or NS3-250 loci into the pD2/IC-VV45R [PDK-53] backbone) and D2/IC-Vx (where x indicates the reciprocal incorporation of the three candidate PDK-53 vaccine [V in the virus designation] virus-specific loci within the pD2/IC-30P-A [16681] backbone) viruses are shown in Table 1. Given the assumption that the 5′NC, NS1, and NS3 loci are the primary determinants of the PDK-53 virus-specific phenotype, then the D2/IC-P5 and D2/IC-V13 viruses should be equivalent (cognate) because both viruses contain 5′NC-57-C, NS1-53-Asp, and NS3-250-Val. The cognate virus pairs derived from reciprocal mutagenesis of the 16681 and PDK-53 virus-specific infectious clones are indicated in Table 1. To further investigate the prM-29 locus, we moved the prM-29-Asp locus of DEN-2 16681 virus into pD2/IC-VV45R and pD2/IC-P5 to derive recombinant D2/IC-Pp and -P5p viruses, respectively. Reciprocal recombinations yielded D2/IC-Vp and -V5p viruses (not shown in Table 1).
Each clone-derived virus (transfected BHK-21 seed) was propagated once in LLC-MK2 cells. The genotypes of all of the LLC-MK2-1-passaged, recombinant 16681/PDK-53 viruses derived in this study were confirmed by complete nucleotide sequence analyses of their genomes. Because all of the viruses had the expected nucleotide sequences, we inferred that their cDNA clones were also correct. All of the clone-derived viruses contained the 16681 virus-specific nt 8571-C locus, which is the site of a silent mutation in PDK-53 virus. The direct sequencing of cDNA amplicons amplified from DEN-2 viral genomic RNA by reverse transcriptase-mediated PCR (RT-PCR; Titan One-Tube kit; Roche Molecular Biochemicals, Indianapolis, Ind.) has been described previously (32). The sequences of the 5′- and 3′-terminal 30 nt of the genome were determined by direct sequencing of the infectious clone cDNA in plasmid pBRUC-139 (32). The D2/IC- prefix is eliminated in the virus designations in the following text.
Characterization of the replication phenotypes of recombinant 16681/PDK-53 viruses.
Viruses were analyzed for plaque size, temperature sensitivity, and replication in LLC-MK2 and C6/36 cells. Plaque sizes were evaluated after 9 days of incubation under agarose in LLC-MK2 cell monolayers grown in six-well plates (32). Viral growth curves were performed in 75-cm2 flasks of LLC-MK2 or C6/36 cells inoculated at multiplicity of infection (MOI) of approximately 0.001 PFU/cell. After adsorption at 37°C for 2 h, 30 ml of DMEM (LLC-MK2 cells) or overlay nutrient medium (C6/36 cells) containing penicillin-streptomycin and 5% FBS was added, and the cultures were incubated in 5% CO2 at 37 or 29°C, respectively. Aliquots of culture medium were removed at 48-h intervals, adjusted to 12.5% FBS, and stored at −80°C prior to virus titration.
Temperature sensitivity assays were performed in LLC-MK2 cells grown in 75-cm2 flasks. The cells were inoculated at an MOI of about 0.001 PFU/cell. After adsorption for 2 h at 37°C, 30 ml of DMEM containing 5% FBS was added. One set of cultures was incubated for 8 days at 37°C; the other was incubated at 38.7°C. The ratio of virus titer at 38.7°C versus the titer at 37°C was calculated.
Mouse neurovirulence assay.
Litters of newborn, outbred white ICR mice were inoculated intracranially with 104 PFU of virus in a volume of 30 μl. Mice were individually weighed once a week and were observed for paralysis or death for 35 days.
RESULTS
Plaque phenotypes of recombinant 16681/PDK-53 viruses.
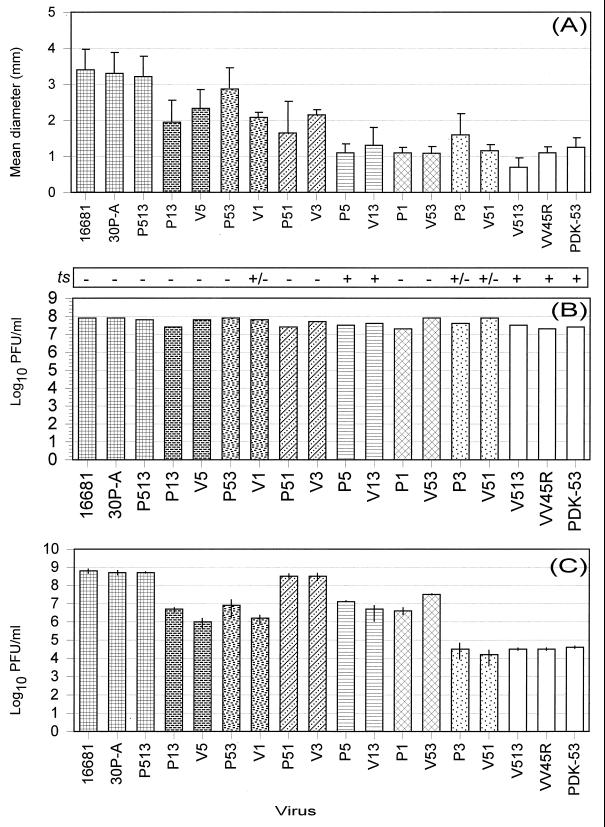
Mean diameters of virus plaques (n = 12) at 9 days after infection under agarose overlay in LLC-MK2 cells are shown in Fig. 1A. The largest plaques (3.2 to 3.4 mm, mean diameter) were produced by the wild-type 16681 virus, its clone-derived 30P-A virus, and the recombinant P513 virus, which contained the 5′NC, NS1, and NS3 16681 virus-specific loci in the VV45R (PDK-53) virus genetic background (Table 1). These three 16681 virus-specific loci within the PDK-53 virus genetic background were sufficient to reconstitute the large-plaque phenotype of the 16681 virus (Fig. 1A).
FIG. 1.
(A) Mean plaque diameters ± standard deviation (n = 12) of DEN-2 16681, PDK-53, and recombinant 16681/PDK-53 viruses at 9 days after infection in LLC-MK2 cells. (B) Peak replication titers at 6 to 8 days after infection of LLC-MK2 cells at an MOI of approximately 0.001 PFU/cell in a single experiment. Temperature sensitivity (ts) scores for viruses grown at 37 or 38.7°C in LLC-MK2 cells are shown above the graph bars for peak replication titers. Scores of −, +/−, and + indicate less than 81, 81 to 89, and 90 to 97% reduction in viral titer, respectively, at 38.7°C. Scores were determined at 8 days after infection. (C) Average peak replication titers at 12 days after infection of C6/36 cells at an MOI of approximately 0.001 PFU/cell in two independent experiments. Individual peak titers from the two experiments are indicated by vertical lines in each graph bar. For designations of recombinant Px and Vx viruses, see Materials and Methods. Cognate viruses are indicated in all three graphs by graph bars of identical solid or cross-hatching pattern. The cognate for P5 virus is V13 virus, assuming that the viral phenotype is determined predominantly by the 5′NC-57, NS1-53, and NS3-250 loci. Both P5 and V13 viruses contain the 5′NC-57-C (16681), NS1-53-Asp (PDK-53), and NS3-250-Val (PDK-53) loci within the genetic backgrounds of PDK-53 and 16681 viruses, respectively.
Individual PDK-53 virus-specific 5′-NC-57-T, NS1-53-Asp, and NS3-250-Val mutations incorporated into the 16681 genotype each resulted in significantly (P < 0.00003) decreased plaque sizes of 2.1 to 2.3 mm in V5, V1, and V3 viruses, respectively, versus those of 16681 virus. The plaque phenotypes of P13 and P51 viruses were similar to those of their cognate V5 and V3 viruses, respectively (Fig. 1). The 2.8-mm plaques of P53 virus differed from 16681 viral plaques to a lesser degree (P < 0.03) than did the 2.1-mm plaques of its cognate V1 virus. The 1.1- to 1.6-mm plaques of cognate virus pairs V13 (P5) (containing PDK-53 virus-specific NS1 and NS3 loci), V53 (P1) (PDK-53 virus-specific 5′NC and NS3 loci), and V51 (P3) virus (PDK-53 virus-specific 5′NC and NS1 loci) were essentially equivalent to the 1.3-mm plaques of PDK-53 virus. These data indicated that all pairwise combinations of these three PDK-53 virus-specific loci in the 16681 backbone generated a small-plaque virus similar to PDK-53 virus. Although V51 virus produced a plaque phenotype similar to that of PDK-53 virus, all three 16681 virus-specific 5′NC-C, NS1-53-Gly, and NS3-250-Glu loci were required within the PDK-53 background of P513 virus to reconstitute the plaque phenotype of 16681 virus. The presence of all three PDK-53 loci in the 16681 backbone generated V513 virus, which had a smaller (P < 0.001, Student's t test) plaque phenotype than that of either PDK-53 or VV45R virus. We are unable to explain the reason for the smaller plaque phenotype of V513 virus. The difference between the plaque size of PDK-53 virus and that of VV45R virus was not significant.
Recombinant Vp virus, which contained the PDK-53 virus-specific prM-29-Val locus in the 16681 virus background, had a significantly (P < 0.002) reduced plaque size of 2.6 mm (not shown). However, the 1.0-mm plaque phenotype of Pp virus (16681 prM-29-Asp locus in the PDK-53 background [not shown]) was essentially identical to the 1.1- and 1.3-mm plaques of VV45R and PDK-53 viruses, respectively (Fig. 1A). The prM-29 locus did not affect the plaque phenotypes of P5p (1.0 ± 0.0 mm) and V5p (2.0 ± 0.4 mm) viruses (not shown), which produced plaques similar to those of P5 (1.1 ± 0.3 mm) and V5 (2.3 ± 0.4 mm) respectively, (Fig. 1A).
Replication of recombinant 16681/PDK-53 viruses in LLC-MK2 and C6/36 cells.
In a single experiment, all of the viruses in this study replicated well in LLC-MK2 cells, reaching peak titers of 107.3 to 107.9 PFU/ml at 6 to 8 days after infection (Fig. 1B; Pp, P5p, Vp, and V5p viruses not shown). PDK-53 virus and its clone-derived VV45R virus replicated more slowly than the other viruses during the first 4 days after infection (data not shown). To determine temperature sensitivities, virus-infected LLC-MK2 cells were incubated at 37 or 38.7°C in two to five experiments. Temperature sensitivity (defined here as a 90% or greater reduction in virus titer at 38.7°C) scores were determined at 8 days after infection. All of the viruses exhibited some degree of temperature sensitivity under these conditions. In individual experiments, wild-type 16681 virus showed 75 to 80% titer reduction at 38.7°C. Virus V1 and cognate virus pair P3 (V51), which showed 84 to 86% average reductions in titer, were slightly more temperature sensitive than 16681 virus. However, only PDK-53, VV45R, V513, P5p, Pp, and the cognate recombinant viruses V13 and P5, all of which contained both the NS1-53-Asp and NS3-250-Val PDK-53 virus-specific loci, reproducibly showed 90 to 97% average reduction in titer at 38.7°C (Fig. 1B and data not shown).
The 16681 virus and its clone-derived 30P-A virus replicated to average peak titers of 108.6 to 108.8 PFU/ml at 12 days after infection in two independent growth curve experiments in C6/36 cells (Fig. 1C). The replication of PDK-53 virus (peak titer of 104.5 PFU/ml) and its clone-derived VV45R (peak titer of 104.6 PFU/ml) virus was approximately 15,000-fold less efficient in C6/36 cells. The 16681 virus-specific 5′NC and NS1 loci within the PDK-53 background of P51 virus fully reconstituted the replication efficacy to that of wild-type 16681 virus (Fig. 1C). Conversely, the PDK-53 virus-specific 5′NC and NS1 loci within the 16681 virus background of V51 virus were sufficient to establish the crippled replication phenotype of PDK-53 virus. Recombinant cognate virus pairs V5 (P13) and V1 (P53), which contained the PDK-53 virus-specific 5′NC region or NS1 locus, respectively, replicated to average peak titers of 105.9 to 106.7 PFU/ml. Although the average peak titer of V53 virus was about 40-fold greater than that of V5 virus in C6/36 cells, the peak titers of P513, P13, P53, V3, V13, V513, and P3 viruses were very similar to those of P51, P1, P5, 30P-A, V1, V51, and VV45R viruses, respectively. These data indicated that the NS3-250 locus had little or no observable effect on replication in C6/36 cells (Fig. 1C). Vp and 16681 viruses had nearly equal average peak titers in C6/36 cells, as did P5 and P5p viruses. Pp and V5p viruses produced average peak titers that were slightly higher (8- and 40-fold, respectively) than those of PDK-53 and V5 viruses, respectively (data not shown). The prM-29 locus appeared to have little or no effect on viral replication in C6/36 cells.
Neurovirulence of recombinant 16681/PDK-53 viruses in newborn mice.
To investigate the neurovirulence of the recombinant viruses, two litters of newborn white ICR mice, eight mice per litter, were infected intracranially with 104 PFU of virus. The DEN-2 16681 virus and its clone-derived 30P-A virus cause 50 to 100% mortality in these mice (32). Average survival times (AST) for mice succumbing to challenge with 16681 or 30P-A virus ranged from 15.2 to 16.8 days in various experiments. Mice were weighed individually every 7 days after infection. A single mouse died by day 1 after infection, presumably as a result of inoculation trauma, in each of the P53 and Vp groups (Table 2). These two mice were excluded from the analyses. There were no fatalities and no weight loss in the control, diluent-inoculated group (not shown in Table 2).
TABLE 2.
Neurovirulence of DEN-2 16681, PDK-53, and recombinant 16681/PDK-53 viruses in newborn white ICR mice
| Virus (cognate)c | Mouse challengea
|
Virus genotypeb
|
||||||
|---|---|---|---|---|---|---|---|---|
| Mortality (%) | AST (SD) (days) | 5′-NC-57 | prM-29 | NS1-53 | NS2A-181 | NS3-250 | NS4A-75 | |
| DEN-2 16681 | 68.75 | 15.2 (1.2) | c | D | G | L | E | G |
| 30P-A (P513) | 81.25 | 14.6 (2.3) | · | · | · | · | · | · |
| P513 (16681) | 100.0 | 13.2 (1.6) | · | V | · | F | · | A |
| P51 (V3) | 50.0d | 15.9 (5.5) | · | V | · | F | V | A |
| P1 (V53) | 37.5d | 19.0 (4.2) | t | V | · | F | V | A |
| P13 (V5) | 37.5d | 13.5 (2.1) | t | V | · | F | · | A |
| P53 (V1) | 20.0d | 17.0 (7.8) | · | V | D | F | · | A |
| P5p (V13) | 6.25 | 15.0 | · | · | D | F | V | A |
| P5 (V13) | 6.25 | 27.0 | · | V | D | F | V | A |
| Pp (PDK-53) | 0 | —e | t | · | D | F | V | A |
| P3 (V51) | 0 | — | t | V | D | F | · | A |
| V3 (P51) | 75.0d | 16.4 (3.2) | · | · | · | · | V | · |
| Vp (16681) | 87.5 | 17.0 (0.9) | · | V | · | · | · | · |
| V53 (P1) | 18.75d | 21.3 (6.1) | t | · | · | · | V | · |
| V5 (P13) | 18.75d | 21.7 (4.2) | t | · | · | · | · | · |
| V5p (P13) | 6.25 | 20.0 | t | V | · | · | · | · |
| V13 (P5) | 6.25 | 17.0 | · | · | D | · | V | · |
| V1 (P53) | 6.25 | 22.0 | · | · | D | · | · | · |
| V51 (P3) | 0 | — | t | · | D | · | · | · |
| V513 (PDK-53) | 0 | — | t | · | D | · | V | · |
| VV45R (V513) | 0 | — | t | V | D | F | V | A |
| DEN-2 PDK-53 | 0 | — | t | V | D | F | V | A |
Percent mortality and AST of newborn, outbred white ICR mice challenged intracranially with 104 PFU of virus. There were 16 mice per group, except for the P53 and Vp groups, in which a single mouse died by day 1 after infection, presumably as a result of inoculation trauma. These two mice were excluded from the study.
See footnote a to Table 1 for explanation of virus genotypes. Dots indicate sequence identity with 16681 virus.
See footnote b to Table 1 for explanation of virus and cognate virus designations.
Mean body weight of surviving mice was significantly lower (P < 0.001, Student's t test) than that of diluent-inoculated control mice (not shown) at 3 weeks after infection.
—, not applicable because there was no mortality in this mouse group.
Three mouse neurovirulence phenotypes were observed (Table 2). The first phenotype consisted of the mouse-virulent viruses DEN-2 16681, 30P-A, P513, P51, V3, and Vp, which caused at least 50% mortality with AST of 13.2 to 17.0 days (Table 2). In two other independent experiments, the Vp virus caused 46.67% mortality with AST of 17.4 ± 1.4 days (n = 16) and 56.25% mortality with AST of 18.3 ± 1.3 days (n = 16) (data not shown). In an independent experiment, P51 virus caused only 25% mortality with AST of 15.9 ± 5.5 days (n = 16) (not shown). A second phenotype consisted of the mouse-attenuated PDK-53, VV45R, V513, Pp, and cognate V51 (P3) viruses, which caused no mortality, and the nearly attenuated V1, cognate V13 (P5), P5p, and V5p viruses, which killed only 1 of 16 mice (Table 2). The presence of the two PDK-53 virus-specific 5′NC-57-T and NS1-53-Asp loci within the 16681 virus genetic background was sufficient to result in or maintain attenuation in cognate viruses V51 (P3). Except for P53 virus, all of the viruses containing the PDK-53 virus-specific NS1-53-Asp locus were attenuated or nearly attenuated.
The third phenotype, that of intermediate virulence, characterized cognate virus pairs V5 (P13) and V53 (P1), and P53 virus which caused 18.75 to 37.5% mouse mortality and significant weight loss (P < 0.001, Student's t test, at 3 weeks after infection, relative to diluent-inoculated control mice) in mice that survived virus challenge. Viruses V5 (P13) and V53 (P1) contained the 5′NC-57-T, but not the NS1-53-Asp, locus of PDK-53 virus. V1 virus (6.25% mortality) was more attenuated than V5 virus, which produced 18.75% mortality and significant weight loss in the survivors. Conversely, the 16681 virus-specific 5′-NC-57-C locus caused little reversion to virulence in P5 virus (6.25% mortality), whereas the NS1-53-Gly moiety in P1 virus resulted in an intermediate level (37.5%) of mortality and significant weight loss in the survivors. Unlike the nearly attenuated cognate V1 virus, P53 virus had an intermediate virulence phenotype. The NS1-53 locus had a more significant effect on the virulence phenotype than did the 5′-NC-57 locus.
The prM-29 locus showed no effect in P5p, Pp, and Vp viruses relative to P5, PDK-53, and 16681 viruses, respectively. The V5p virus, which contained both PDK-53 virus-specific 5′NC-57-T and prM-29-Val loci, was nearly attenuated (Table 2). The NS3-250 locus did not appear to contribute significantly to mouse neurovirulence phenotype in V3, P13, V53, V13, and P3 viruses, which exhibited phenotypes equivalent to those of 16681, P1, V5, V1, and PDK-53 viruses, respectively. The difference in the level of mortality caused by P53 and P5 viruses suggested that the 16681 virus-specific NS3-250-Glu locus might contribute somewhat to the virulence phenotype within certain genetic contexts.
Evolution of mutations in the DEN-2 PDK-53 virus vaccine strain.
We analyzed intermediate passages PDK-5, -10, -14, -35, and -45 of the 16681 virus to determine the accrual of the nine nucleotide mutations in the PDK-53 virus vaccine strain. Amplicons were amplified directly from genomic mRNA extracted from the viral seed by RT-PCR. Automated sequencing of small genomic regions, which contained the nine relevant loci, was performed by using appropriate primers. The nucleotide residues identified at each of the nine loci for these viruses are shown in Table 3. The NS2A-181 Leu-to-Phe mutation and the silent mutations at E-37, NS3-342, and NS5-334 appeared by passage PDK-5 and were the predominant moieties by passage PDK-10 (NS2A-181), PDK-14 (E-373, NS3-342), or PDK-35 (NS5-334). 5′-NC-57 C-to-T, prM-29 Asp-to-Val, NS1-53 Gly-to-Asp, and NS4A-75 Gly-to-Ala mutations occurred by passage PDK-35. The 5′-NC-57-T mutation was predominant at passage PDK-35, while the other listed mutations became predominant by passage PDK-45. The NS3-250 Glu-to-Val mutation appeared by passage PDK-45 and is not fully mutated to the virus-specific Val in the current PDK-53 virus vaccine candidate (Table 3). Approximately 29% of the viral population in the PDK-53 virus vaccine contains NS3-250-Glu (32). The PDK-45 virus was genetically equivalent to the PDK-53 virus vaccine. In the present study, we did not attempt to determine the relative proportions of the two nucleotides at the mixed genetic loci shown in Table 3.
TABLE 3.
Evolution of the DEN-2 PDK-53 virus vaccine during passage of the parental 16681 virus in PDK cells
| Virus | Genome nt position,a translated polypeptide position,b encoded amino acidsb
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 57 | 524, prM-29, D–V | 2055, E-373, F–F | 2579, NS1-53, G–D | 4018, NS2A-181, L–F | 5270, NS3-250, E–V | 5547, NS3-342, R–R | 6599, NS4A-75, G–A | 8571, NS5-334, V–V | |
| 16681 | C | A | C | G | C | A | T | G | C |
| PDK-5 | C | A | C/Tc | G | T/C | A | T/C | G | C/T |
| PDK-10 | C | A | T/C | G | T | A | C/T | G | T/C |
| PDK-14 | C | A | T | G | T | A | C | G | T/C |
| PDK-35 | T | T/A | T | A/G | T | A | C | C/G | T |
| PDK-45 | T | T | T | A | T | A/T | C | C | T |
| PDK-53 | T | T | T | A | T | A/T | C | C | T |
Of the nine nucleotide sequence differences between 16681 and PDK-53 viruses (32). Nucleotide position 57 lies within the 5′NC of the viral genome. A, C, G, and T (cDNA sense) nucleotides are indicated.
The virus-specific amino acid residues (16681–PDK-53) are shown for each amino acid position.
Two genetic populations were identified for this locus in the virus. The order of the two nucleotides reflects relative peak heights of the nucleotide signals in sequence chromatograms.
DISCUSSION
Amino acid substitutions in the viral E protein, as well as other viral proteins, are associated with attenuation or virulence in flaviviruses (3, 8, 13, 28, 30, 43, 53, 63). It is apparent that the potential repertoire of attenuating mutations in the flavivirus genome is quite extensive. Mutations that occur between other parent/attenuated flaviviruses, such as yellow fever Asibi/17D viruses (28), Japanese encephalitis SA14/SA14-14-2 viruses (53), and DEN-1 Western Pacific 74/45AZ5 PDK-0/45AZ5 PDK-27 viruses (59), do not coincide with each other or with the mutations identified between the DEN-2 16681/PDK-53 viruses (32). The prM-29 Asp-to-Val substitution is the only amino acid mutation that occurs in the structural proteins of the candidate DEN-2 PDK-53 virus vaccine, while the other four amino acid mutations occur in nonstructural genes (32). Depending on the particular recombinant 16681/PDK-53 virus investigated in the current and earlier pilot (unpublished data) studies, the prM-29 locus had minor or no effect on plaque size, replication in LLC-MK2 or C6/36 cells, or mouse neurovirulence. Neither the prM-29-Asp nor the NS2A-181-Leu residue of DEN-2 16681 virus is conserved among flaviviruses. The NS4A-75-Gly is conserved only among the four serotypes of DEN virus. The latter two loci were not specifically investigated in this study. In contrast, the NS1-53-Gly residue is highly conserved among the aligned amino acid sequences of the NS1 proteins of nearly all flaviviruses reported to date, and the NS3-250-Glu is conserved among the mosquito-borne flaviviruses other than yellow fever virus (aligned data not shown). Such sequence conservation probably reflects important functionality of these two loci in the NS1 and NS3 proteins of flaviviruses.
All of the viruses studied here replicated to peak titers of 107.3 PFU/ml or greater in LLC-MK2 cells by 6 to 8 days after infection. However, the three 5′-NC-57 C-to-T, NS1-53 Gly-to-Asp, and NS3-250 Glu-to-Val mutations all contributed individually, as well as synergistically in all combinations, to the small-plaque phenotype of PDK-53 virus. These results indicated that all three mutations affected viral replication in LLC-MK2 cells. Limited spread of viruses among LLC-MK2 cells under agarose might be expected to enhance small differences in replication efficiency. In multiple experiments in our laboratory, PDK-53 and VV45R viruses, which produce small plaques, have clearly and consistently shown lower replication rates during the first 4 to 6 days after infection of LLC-MK2 cells. However, we could not clearly identify a correlation between plaque size under agarose and early replication rate for the other viruses in the single growth curve experiment shown in Fig. 1B. All four of the Mahidol candidate DEN virus vaccines are temperature sensitive to some extent in LLC-MK2 cells (70). In five independent experiments in the present study, the slight temperature sensitivity of PDK-53 virus in LLC-MK2 cells, relative to 16681 virus, appeared to result from synergy between the NS1-53-Asp and NS3-250-Val mutations. We previously reported that 130Vc-K virus, a clone-derived homolog of PDK-53 virus (NS3-250-Val variant), was more temperature sensitive than PDK-53 virus itself (32). In the present study, we identified and corrected two amino acid errors in the pD2/IC-130Vc-K clone to derive pD2/IC-VV45R. The degree of temperature sensitivity of VV45R virus was similar to that of PDK-53 virus. Both 130Vc-K (32) and VV45R viruses replicated very inefficiently in C6/36 cells, as did PDK-53 virus.
Replication of PDK-53 virus is greatly reduced in orally fed A. aegypti mosquitoes (31) and in A. albopictus C6/36 cells (32) relative to its parental 16681 virus. The PDK-53 virus is not transmitted by A. aegypti mosquitoes (31). We demonstrated in this study that the low efficiency of PDK-53 viral replication in C6/36 cells resulted from the 5′NC-57 C-to-T and NS1-53 Gly-to-Asp mutations. Each of these mutations engineered into the 16681 virus-specific background (V5 and V1 viruses) resulted in a 250-fold or greater decrease in peak titer relative to that of 16681 virus. The synergistic effect of both mutations in V51 virus resulted in an approximately 200-fold further decrease in peak titer in C6/36 cells. Low infectivity for mosquitoes reduces the potential for secondary transmission of vaccine viruses and may be a useful biological marker of viral attenuation (2, 31, 46, 61). Low infectivity for mosquitoes has been demonstrated for the 17D and French neurotropic yellow fever vaccine viruses (20, 69), attenuated Japanese encephalitis virus (17), and the candidate DEN-2 PR-159/S-1 virus vaccine (2, 46).
Although determining fine distinctions among viruses of low to moderate virulence in an insensitive mouse model is difficult, attenuation of PDK-53 virus for newborn mice was due primarily to synergy between the 5′NC-57-T and NS1-53-Asp loci. Except for P53 virus, all of the viruses containing the NS1-53-Asp locus of PDK-53 virus were attenuated or nearly attenuated for newborn mice. The NS3-250 locus did not appear to contribute significantly to mouse neurovirulence phenotype, except for P53 virus (relative to the nearly attenuated phenotype of P5 virus).
The in vitro phenotypic markers of small plaque size, temperature sensitivity, and reduced level of replication in C6/36 cells all showed positive correlations with the attenuated phenotype of PDK-53 virus in mice. The NS1-53 locus affected the phenotypic traits of plaque size, temperature sensitivity, replication in C6/36 cells, and mouse neurovirulence. The 5′NC-57 locus affected plaque size, replication in C6/36 cells, and mouse neurovirulence. The NS3-250 locus influenced plaque size and temperature sensitivity, and possibly affected mouse virulence to a minor extent. These three genetic loci defined nearly completely the tested markers of attenuation for PDK-53 virus in order of importance NS1-53-Asp > 5′NC-57-T > NS3-250-Val. These loci probably contribute to the attenuated phenotype of PDK-53 virus in humans and nonhuman primates, but we cannot exclude contributions of the prM-29, NS2A-181, and NS4A-75 loci in these hosts. The relative effects of these mutations might be expected to differ in different cell types and hosts. This seems clear for viruses containing the PDK-53 virus-specific 5′NC-57-T and NS1-53-Val loci. These viruses clearly showed different replication efficiencies in LLC-MK2 and C6/36 cells (Fig. 1B and C). Processing of flavivirus proteins, including NS1 (41), is known to differ in mammalian and mosquito cells.
The N terminus of NS3 possesses serine protease activity (16), while the C terminus exhibits RNA helicase and RNA triphosphatase activities (67). The protease activity of NS3, which resides within the amino-terminal 180 amino acids of the protein, appears to depend on an interaction with NS2B (10, 23, 24). The NS1 protein is a glycoprotein that is present on the cell surface of, and secreted from, flavivirus-infected cells. NS1-specific antibodies are present in the serum of flavivirus-infected individuals, and protection of animals immunized with NS1 protein or passively immunized with anti-NS1 monoclonal antibody has been reported (64). Recent data indicate that the NS1 protein functions in the replication of viral RNA, probably before or during minus-strand synthesis (38). A single Arg-to-Ala mutation at NS1-299 of yellow fever virus resulted in a temperature-sensitive defect in RNA accumulation that delayed virus production (52). Elimination of the first or both glycosylation sites of the yellow fever NS1 decreased RNA accumulation and decreased mouse neurovirulence (51). The mutations in the NS1 and NS3 proteins of DEN-2 PDK-53 virus probably impair the functions of these nonstructural proteins during viral replication. These two mutations resulted in a demonstrable decrease in the replication efficiency of the temperature-sensitive viruses in this study, whose NS1 and NS3 proteins apparently were unable to establish or maintain their fully functional, wild-type conformation at the higher temperature.
The 5′NC region of flaviviruses and other positive-stranded viruses has the potential to form secondary structures that are functionally important for viral replication (11, 12, 40, 62). Mutations in the 5′NC region might affect the function of the positive-sense RNA strand as well as the function of its complement in the negative-sense strand during replication. Determinants of attenuation have been demonstrated to lie within the 5′NC region of the Sabin polio vaccine viruses (22, 40) and Venezuelan equine encephalitis virus (33). The 5′NC-57-T mutation in DEN-2 PDK-53 virus occurs within the context of a possible 6-mer stem structure (36) of 16681 viral RNA consisting of genome nt 11 to 16 (5′-CUACGU-3′) and 56 to 61 (5′-ACGUAG-3′; underlined nucleotide is U in PDK-53 virus). The replicative importance of short stem structures in RNA molecules may be inferred by identification of pairs of compensatory nucleotide mutations that maintain the stem (44, 54, 56). Two pairs of such stem-preserving, compensatory substitutions occur at nt 11 to 16 (5′-CUGUGU-3′) and 55 to 60 (5′-ACACAG-3′) in the 5′NC region of DEN-4 814669 virus (71).
Infectious cDNA clones have been used to study the genetic basis of attenuation in a number of viruses, including poliovirus (5, 39, 40, 42, 55, 60, 68), Venezuelan equine encephalitis virus (21, 33), and Japanese encephalitis virus (63). Construction of an infectious clone of DEN-4 virus (35) has led to an understanding of genetic markers of neurovirulence in mice (9) as well as important functions of the 5′NC and 3′NC regions on growth of this virus in cell culture (12, 45). An understanding of the genetic basis of attenuation for the promising DEN-2 PDK-53 vaccine candidate should improve the prospect of constructing safe and reliable attenuated vaccines for DEN virus. The PDK-53 virus replicates well in mammalian cell culture, and its genotype was stable after at least eight passages in PDK cells (Table 3) and another passage in LLC-MK2 cells (32). The phenotypic markers of PDK-53 virus appear to remain stable after sequential passage in human vaccinees and A. aegypti mosquitoes (31). The present study demonstrated that complete reversion of PDK-53 virus to the phenotypic characteristics of the parental 16681 virus required at least two reverse mutations at the 5′NC-57 and NS1-53 loci. Reversion at the NS3-250 locus was also required to reconstitute the large-plaque phenotype, and possibly the mouse virulence phenotype, of 16681 virus.
Chimeric viruses expressing structural genes of DEN-1, DEN-2, DEN-3, or tick-borne encephalitis virus have been engineered successfully in the genetic background of DEN-4 virus (7, 8, 18, 34, 57, 58). Chimeric viruses expressing the prM and E genes of Japanese encephalitis virus within the genetic background of yellow fever 17D virus have also been reported (15, 26, 49). The restriction of the major genetic loci affecting the markers of attenuation to nonstructural regions of PDK-53 virus makes the infectious clone of this virus an attractive candidate for the development of chimeric viruses that express the structural proteins of DEN-1, DEN-3, DEN-4, or other flaviviruses. The attenuated genetic background of PDK-53 virus, which has been characterized in detail in this study, may permit the engineering of chimeric vaccine candidates which express the structural genes of wild-type, heterologous flaviviruses, assuming that the attenuated phenotypic markers of DEN-2 PDK-53 virus are retained in the chimeric viruses. We have recently engineered chimeric DEN-2/DEN-1 viruses that express the structural genes of DEN-1 16007 virus or its candidate DEN-1 PDK-13 virus vaccine derivative within the genetic background of DEN-2 PDK-53 virus to investigate the feasibility of such chimeras (unpublished data).
ACKNOWLEDGMENTS
We are grateful to the Biotechnology Core Facility Branch, Centers for Disease Control and Prevention (Atlanta, Ga.), for supplying the synthetic oligonucleotide primers used in this study. We thank Barry Miller and Mary Crabtree for providing protocols for plaque titration of viruses. We thank Richard Tsuchiya for running sequence reactions on the Prism 377 DNA sequencer.
REFERENCES
- 1.Angsubhakorn S, Moe J B, Marchette N J, Palumbo N F, Yoksan S, Bhamarapravati N. Neurovirulence effects of dengue-2 viruses on the rhesus (Macaca mulatta) brain and spinal cord. Southeast Asian J Trop Med Public Health. 1987;18:52–55. [PubMed] [Google Scholar]
- 2.Bancroft W H, Scott R McN, Brandt W E, McCown J M, Eckels K H, Hayes D E, Gould D J, Russell P K. Dengue-2 vaccine: infection of Aedes aegypti mosquitoes by feeding on viremic recipients. Am J Trop Med Hyg. 1982;31:1229–1231. doi: 10.4269/ajtmh.1982.31.1229. [DOI] [PubMed] [Google Scholar]
- 3.Barrett A D T, Dunster L M, Ledger T N, Gibson C A, Sil B K, Sanders P G, Gould E A, Minor P D. Evidence that the envelope protein of flaviviruses encodes determinants of attenuation and virulence. In: Brown F, Chanock R M, Ginsberg H S, Lerner R A, editors. Vaccines 90. New York, N.Y: Cold Spring Harbor Laboratory Press; 1990. pp. 101–104. [Google Scholar]
- 4.Bhamarapravati N, Yoksan S, Chayaniyayothin T, Angsubphakorn S, Bunyaratvej A. Immunization with a live attenuated dengue-2-virus candidate vaccine (16681-PDK 53): clinical, immunological and biological responses in adult volunteers. Bull WHO. 1987;65:189–195. [PMC free article] [PubMed] [Google Scholar]
- 5.Bouchard M J, Lam D-H, Racaniello V R. Determinants of attenuation and temperature sensitivity in type 1 poliovirus Sabin vaccine. J Virol. 1995;69:4972–4978. doi: 10.1128/jvi.69.8.4972-4978.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brandt W E. Development of dengue and Japanese encephalitis vaccines. J Infect Dis. 1990;162:577–583. doi: 10.1093/infdis/162.3.577. [DOI] [PubMed] [Google Scholar]
- 7.Bray M, Lai C-J. Construction of intertypic chimeric dengue viruses by substitution of structural protein genes. Proc Natl Acad Sci USA. 1991;88:10342–10346. doi: 10.1073/pnas.88.22.10342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bray M, Men R, Lai C-J. Monkeys immunized with intertypic chimeric dengue viruses are protected against wild-type virus challenge. J Virol. 1996;70:4162–4166. doi: 10.1128/jvi.70.6.4162-4166.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bray M, Men R, Tokimatsu I, Lai C J. Genetic determinants responsible for acquisition of dengue type 2 virus mouse neurovirulence. J Virol. 1998;72:1647–1651. doi: 10.1128/jvi.72.2.1647-1651.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brinkworth R I, Fairlie D P, Leung D, Young P R. Homology model of the dengue 2 virus NS3 protease: putative interactions with both substrate and NS2B cofactor. J Gen Virol. 1999;80:1167–1177. doi: 10.1099/0022-1317-80-5-1167. [DOI] [PubMed] [Google Scholar]
- 11.Brinton M A, Dispoto J H. Sequence and secondary structure analysis of the 5′-terminal region of flavivirus genome RNA. Virology. 1987;162:290–299. doi: 10.1016/0042-6822(88)90468-0. [DOI] [PubMed] [Google Scholar]
- 12.Cahour A, Pletnov A, Vazeille-Falcoz M, Rosen L, Lai C J. Growth-restricted dengue virus mutants containing deletions in the 5′ noncoding region of the RNA genome. Virology. 1995;207:68–76. doi: 10.1006/viro.1995.1052. [DOI] [PubMed] [Google Scholar]
- 13.Cao J X, Ni H, Wills M R, Campbell G A, Sil B K, Ryman K D, Kitchen I, Barrett A D T. Passage of Japanese encephalitis virus in Hela cells results in attenuation of virulence in mice. J Gen Virol. 1995;76:2757–2764. doi: 10.1099/0022-1317-76-11-2757. [DOI] [PubMed] [Google Scholar]
- 14.Chambers T J, Hahn C S, Galler R, Rice C M. Flavivirus genome organization, expression, and replication. Annu Rev Microbiol. 1990;44:649–688. doi: 10.1146/annurev.mi.44.100190.003245. [DOI] [PubMed] [Google Scholar]
- 15.Chambers T J, Nestorowicz A, Mason P W, Rice C M. Yellow fever/Japanese encephalitis chimeric viruses: construction and biological properties. J Virol. 1999;73:3095–3101. doi: 10.1128/jvi.73.4.3095-3101.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chambers T J, Nestorowicz A, Rice C M. Mutagenesis of the yellow fever virus NS2B/3 cleavage site: determinants of cleavage site specificity and effects on polyprotein processing and viral replication. J Virol. 1995;69:1600–1605. doi: 10.1128/jvi.69.3.1600-1605.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen B Q, Beaty B J. Comparative infection and transmission rates of Japanese encephalitis vaccine (2-8 strain) and parent (SA 14 strain) viruses in Culex tritaeniorhynchus mosquitoes. Am J Trop Med Hyg. 1982;31:403–407. doi: 10.4269/ajtmh.1982.31.403. [DOI] [PubMed] [Google Scholar]
- 18.Chen W, Kawano H, Men R, Clark D, Lai C-J. Construction of intertypic chimeric dengue viruses exhibiting type 3 antigenicity and neurovirulence for mice. J Virol. 1995;69:5186–5190. doi: 10.1128/jvi.69.8.5186-5190.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dharakul T, Kurane I, Bhamarapravati N, Yoksan S, Vaughn D W, Hoke C H, Ennis F A. Dengue virus-specific memory T-cell responses in human volunteers receiving a live attenuated dengue virus type 2 candidate vaccine. J Infect Dis. 1994;170:27–33. doi: 10.1093/infdis/170.1.27. [DOI] [PubMed] [Google Scholar]
- 20.Davis N D, Lloyd W, Frobisher M., Jr Transmission of neurotropic yellow fever virus by Stegomyia mosquitoes. J Exp Med. 1932;56:853–865. doi: 10.1084/jem.56.6.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis N L, Powell N, Greenwald G F, Willis L V, Johnson B J B, Smith J F, Johnston R E. Attenuating mutations in the E2 glycoprotein gene of Venezuelan equine encephalitis virus: construction of single and multiple mutants in a full-length cDNA clone. Virology. 1991;183:20–31. doi: 10.1016/0042-6822(91)90114-q. [DOI] [PubMed] [Google Scholar]
- 22.Evans D M A, Dunn G, Minor P D, Schild G C, Cann A J, Stanway G, Almond J W, Currey K, Maizel J V., Jr Increased neurovirulence associated with a single nucleotide change in a noncoding region of the Sabin type 3 poliovaccine genome. Nature. 1985;314:548–550. doi: 10.1038/314548a0. [DOI] [PubMed] [Google Scholar]
- 23.Falgout B, Miller R H, Lai C-J. Deletion analysis of dengue virus type 4 nonstructural protein NS2B: identification of a domain required for NS2B-NS3 protease activity. J Virol. 1993;67:2034–2042. doi: 10.1128/jvi.67.4.2034-2042.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Falgout B, Pethel M, Zhang Y-M, Lai C-J. Both nonstructural proteins NS2B and NS3 are required for the proteolytic processing of dengue virus nonstructural proteins. J Virol. 1991;65:2467–2475. doi: 10.1128/jvi.65.5.2467-2475.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gagnon S J, Ennis F A, Rothman A L. Bystander target cell lysis and cytokine production by dengue virus-specific human CD4+ cytotoxic T-lymphocyte clones. J Virol. 1999;73:3623–3629. doi: 10.1128/jvi.73.5.3623-3629.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guirakhoo F, Zhang Z-X, Chambers T J, Delagrave S, Arroyo J, Barrett A D T, Monath T P. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated, vaccine candidate against Japanese encephalitis. Virology. 1999;257:363–372. doi: 10.1006/viro.1999.9695. [DOI] [PubMed] [Google Scholar]
- 27.Gubler D J. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998;11:480–496. doi: 10.1128/cmr.11.3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hahn C S, Dalrymple J M, Strauss J H, Rice C M. Comparison of the virulent Asibi strain of yellow fever virus with the 17D vaccine strain derived from it. Proc Natl Acad Sci USA. 1987;84:2019–2023. doi: 10.1073/pnas.84.7.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Halstead S B. Cellular receptors for animal viruses. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1994. pp. 493–516. [Google Scholar]
- 30.Kawanao H, Rostapshov V, Rosen L, Lai C J. Genetic determinants of dengue type 4 virus neurovirulence for mice. J Virol. 1993;67:6567–6575. doi: 10.1128/jvi.67.11.6567-6575.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khin M M, Jirakanjanakit N, Yoksan S, Bhamarapravati N. Infection, dissemination, transmission, and biological attributes of dengue-2 PDK53 candidate vaccine virus after oral infection in Aedes aegypti. Am J Trop Med Hyg. 1994;51:864–869. doi: 10.4269/ajtmh.1994.51.864. [DOI] [PubMed] [Google Scholar]
- 32.Kinney R M, Butrapet S, Chang G-J J, Tsuchiya K R, Roehrig J T, Bhamarapravati N, Gubler D J. Construction of infectious cDNA clones for dengue 2 virus: strain 16681 and its attenuated vaccine derivative, strain PDK-53. Virology. 1997;230:300–308. doi: 10.1006/viro.1997.8500. [DOI] [PubMed] [Google Scholar]
- 33.Kinney R M, Chang G-J, Tsuchiya K R, Sneider J M, Roehrig J T, Woodward T M, Trent D W. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5′-noncoding region and the E2 envelope glycoprotein. J Virol. 1993;67:1269–1277. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lai C-J, Bray M, Men R, Cahour A, Chen W, Kawano H, Tadano M, Hiramatsu K, Tokimatsu I, Pletnev A, Arakai S, Shameem G, Rinaudo R. Evaluation of molecular strategies to develop a live dengue vaccine. Clin Diagn Virol. 1998;10:173–179. doi: 10.1016/s0928-0197(98)00035-x. [DOI] [PubMed] [Google Scholar]
- 35.Lai C-J, Zhao B T, Hori H, Bray M. Infectious RNA transcribed from stably cloned full-length cDNA of dengue type 4 virus. Proc Natl Acad Sci USA. 1991;88:5139–5143. doi: 10.1073/pnas.88.12.5139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leitmeyer K C, Vaughn D W, Watts D M, Salas R, de Chacon I V, Ramos C, Hesse R-H. Dengue virus structural differences that correlate with pathogenesis. J Virol. 1999;73:4738–4747. doi: 10.1128/jvi.73.6.4738-4747.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liljeström P, Lusa S, Huylebroeck D, Garoff H. In vitro mutagenesis of a full-length cDNA clone of Semliki Forest virus: the small 6,000-molecular-weight membrane protein modulates virus release. J Virol. 1991;65:4107–4113. doi: 10.1128/jvi.65.8.4107-4113.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lindenbach B D, Rice C M. trans-complementation of yellow fever virus NS1 reveals a role in early RNA replication. J Virol. 1997;71:9608–9617. doi: 10.1128/jvi.71.12.9608-9617.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Macadam A J, Pollard S R, Ferguson G, Skuce R, Wood D, Almond J W, Minor P D. Genetic basis of attenuation of the Sabin type 2 vaccine strain of poliovirus in primates. Virology. 1993;192:18–26. doi: 10.1006/viro.1993.1003. [DOI] [PubMed] [Google Scholar]
- 40.Macadam A J, Stone D M, Almond J W, Minor P D. The 5′ noncoding region and virulence of poliovirus vaccine strains. Trends Microbiol. 1994;2:449–454. doi: 10.1016/0966-842x(94)90803-6. [DOI] [PubMed] [Google Scholar]
- 41.Mason P W. Maturation of Japanese encephalitis virus glycoproteins produced by infected mammalian and mosquito cells. Virology. 1989;169:354–364. doi: 10.1016/0042-6822(89)90161-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McGoldrick A, Macadam A J, Dunn G, Rowe A, Burlison J, Minor P D, Meredith J, Evans D J, Almond J W. Role of mutations G-480 and C-6203 in the attenuation phenotype of Sabin type 1 poliovirus. J Virol. 1995;69:7601–7605. doi: 10.1128/jvi.69.12.7601-7605.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McMinn P C, Marshall I D, Dalgarno L. Neurovirulence and neuroinvasiveness of Murray Valley encephalitis virus mutants selected by passage in a monkey kidney cell line. J Gen Virol. 1995;76:865–872. doi: 10.1099/0022-1317-76-4-865. [DOI] [PubMed] [Google Scholar]
- 44.Meissner J D, Huang C Y-H, Pfeffer M, Kinney R M. Sequencing of the prototype viruses in the Venezuelan equine encephalitis antigenic complex. Virus Res. 1999;64:43–59. doi: 10.1016/S0168-1702(99)00078-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Men R, Bray M, Clark D, Chanock R M, Lai C J. Dengue type 4 virus mutants containing deletions in the 3′ noncoding region of the RNA genome: analysis of growth restriction in cell culture and altered viremia pattern and immunogenicity in rhesus monkeys. J Virol. 1996;70:3930–3937. doi: 10.1128/jvi.70.6.3930-3937.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miller B R, Beaty B J, Aitken T H G, Eckels K H, Russell P K. Dengue-2 vaccine: oral infection, transmission, and lack of evidence for reversion in the mosquito, Aedes aegypti. Am J Trop Med Hyg. 1982;31:1232–1237. doi: 10.4269/ajtmh.1982.31.1232. [DOI] [PubMed] [Google Scholar]
- 47.Miller B R, Mitchell C J. Passage of yellow fever virus: its effect on infection and transmission rates in Aedes aegypti. Am J Trop Med Hyg. 1986;35:1302–1309. doi: 10.4269/ajtmh.1986.35.1302. [DOI] [PubMed] [Google Scholar]
- 48.Monath T P. Dengue: the risk to developed and developing countries. Proc Natl Acad Sci USA. 1994;91:2395–2400. doi: 10.1073/pnas.91.7.2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Monath T P, Soike K, Levenbook I, Zhang Z-X, Arroyo J, Delagrave S, Myers G, Barrett A D T, Shope R E, Chambers T J, Guirakhoo F. Recombinant, chimeric live, attenuated vaccine (ChimeriVax) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) and the capsid and nonstructural genes of yellow fever (17D) is safe, immunogenic and protective in non-human primates. Vaccine. 1999;17:1869–1882. doi: 10.1016/s0264-410x(98)00487-3. [DOI] [PubMed] [Google Scholar]
- 50.Morens D M. Antibody-dependent enhancement of infection and the pathogenesis of viral disease. Clin Infect Dis. 1994;19:500–512. doi: 10.1093/clinids/19.3.500. [DOI] [PubMed] [Google Scholar]
- 51.Muylaert I R, Chambers T J, Galler R, Rice C M. Mutagenesis of the N-linked glycosylation site of the yellow fever virus NS1 protein: effects on virus replication and mouse neurovirulence. Virology. 1996;222:159–168. doi: 10.1006/viro.1996.0406. [DOI] [PubMed] [Google Scholar]
- 52.Muylaert I R, Galler R, Rice C M. Genetic analysis of the yellow fever virus NS1 protein: identification of a temperature-sensitive mutation which blocks RNA accumulation. J Virol. 1997;71:291–298. doi: 10.1128/jvi.71.1.291-298.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ni H, Chang G-J, Xie H, Trent D W, Barrett A D T. Molecular basis of attenuation of neurovirulence of wild-type Japanese encephalitis virus strain SA14. J Gen Virol. 1995;76:409–413. doi: 10.1099/0022-1317-76-2-409. [DOI] [PubMed] [Google Scholar]
- 54.Noller H F, Woese C R. Secondary structure of 16S ribosomal RNA. Science. 1981;212:403–411. doi: 10.1126/science.6163215. [DOI] [PubMed] [Google Scholar]
- 55.Omato T, Kohara M, Kuge S, Komatsu T, Abe S, Semler B L, Kameda A, Itoh H, Arita M, Wimmer E, Nomoto A. Genetic analysis of the attenuation phenotype of poliovirus type 1. J Virol. 1986;58:348–358. doi: 10.1128/jvi.58.2.348-358.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pace N R, Smith D K, Olsen G J, James B D. Phylogenetic comparative analysis and the secondary structure of ribonuclease P RNA. Gene. 1989;82:65–75. doi: 10.1016/0378-1119(89)90031-0. [DOI] [PubMed] [Google Scholar]
- 57.Pletnev A G, Bray M, Huggins J, Lai C-J. Construction and characterization of chimeric tick-borne encephalitis/dengue type 4 viruses. Proc Natl Acad Sci USA. 1992;89:10532–10536. doi: 10.1073/pnas.89.21.10532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pletnev A G, Bray M, Lai C-J. Chimeric tick-borne encephalitis and dengue type 4 viruses: effects of mutations on neurovirulence in mice. J Virol. 1993;67:4956–4963. doi: 10.1128/jvi.67.8.4956-4963.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Puri B, Nelson W M, Henchal E A, Hoke C H, Eckels K H, Dubois D R, Porter K R, Hayes C G. Molecular analysis of dengue virus attenuation after serial passage in primary dog kidney cells. J Gen Virol. 1997;78:2287–2291. doi: 10.1099/0022-1317-78-9-2287. [DOI] [PubMed] [Google Scholar]
- 60.Ren R, Moss E G, Racaniello V R. Identification of two determinants that attenuate vaccine-related type 2 poliovirus. J Virol. 1991;65:1377–1382. doi: 10.1128/jvi.65.3.1377-1382.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schoepp R J, Beaty B J, Eckels K H. Infection of Aedes albopictus and Aedes aegypti mosquitoes with dengue parent and progeny candidate vaccine viruses: a possible marker of human attenuation. Am J Trop Med Hyg. 1991;45:202–210. doi: 10.4269/ajtmh.1991.45.202. [DOI] [PubMed] [Google Scholar]
- 62.Strauss J H, Strauss E G. The alphaviruses: gene expression, replication, and evolution. Microbiol Rev. 1994;58:491–562. doi: 10.1128/mr.58.3.491-562.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sumiyoshi H, Tignor G H, Shope R E. Characterization of a highly attenuated Japanese encephalitis virus generated from molecularly cloned cDNA. J Infect Dis. 1994;171:1144–1151. doi: 10.1093/infdis/171.5.1144. [DOI] [PubMed] [Google Scholar]
- 64.Trent D W, Kinney R M, Huang C Y-H. Recombinant dengue virus vaccines. In: Gubler D J, Kuno G, editors. Dengue and dengue hemorrhagic fever. New York, N.Y: CAB International; 1997. pp. 379–403. [Google Scholar]
- 65.Vaughn D W, Hoke C H, Jr, Yoksan S, LaChances R, Innis B L, Rice R M, Bhamarapravati N. Testing of a dengue 2 live-attenuated vaccine (strain 16681 PDK 53) in ten American volunteers. Vaccine. 1996;14:329–336. doi: 10.1016/0264-410x(95)00167-y. [DOI] [PubMed] [Google Scholar]
- 66.Wengler G, Bradley D W, Collett M S, Heinz F X, Schlesinger R W, Strauss J H. Flaviviridae. In: Murphy F A, Fauguet C M, Bishop D H L, Ghabrial S A, Jarvis A W, Martelli G P, Mayo M A, Summers M D, editors. Virus taxonomy. Sixth Report of the International Committee on Taxonomy of Viruses. New York, N.Y: Springer-Verlag; 1995. pp. 415–427. [Google Scholar]
- 67.Wengler G, Wengler G. The NS3 nonstructural protein of flaviviruses contains an RNA triphosphatase activity. Virology. 1993;197:265–273. doi: 10.1006/viro.1993.1587. [DOI] [PubMed] [Google Scholar]
- 68.Westrop G D, Evans D M A, Dunn G, Minor P D, Magrath D I, Taffs F, Marsden S, Wareham K A, Skinner M, Schild G C, Almond J W. Genetic basis of attenuation of the Sabin type 3 oral polio vaccine. J Virol. 1989;63:1338–1344. doi: 10.1128/jvi.63.3.1338-1344.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Whitman L. Failure of Aedes aegypti to transmit yellow fever cultured virus (17D) Am J Trop Med. 1939;19:19–26. [Google Scholar]
- 70.Yoksan S, Bhamarapravati N, Halstead S B. Dengue virus vaccine development: study on biological markers of uncloned dengue 1-4 viruses serially passaged in primary kidney cells. In: St. George T D, Kay B H, Blok J, editors. Arbovirus research in Australia. Proceedings of the Fourth Symposium. Brisbane, Australia: CSIRO/QIMR; 1986. pp. 35–38. [Google Scholar]
- 71.Zhao B, Mackow E, Buckler-White A, Markoff L, Chanock R M, Lai C-J, Makino Y. Cloning full-length dengue type 4 viral DNA sequences: analyses of genes coding for structural proteins. Virology. 1986;155:77–88. doi: 10.1016/0042-6822(86)90169-8. [DOI] [PubMed] [Google Scholar]