Video
A novel method of bilateral biliary decompression by EUS-guided hepaticogastrostomy with bridging stenting using the partial stent-in-stent method for reintervention of multiple metal stent failure.
We report a case in which anterior and posterior drainage was performed using the partial stent-in-stent method via the transpapillary approach. The patient had a bismuth type IV biliary obstruction, but only the right hepatic lobe was drained due to obstruction of the left portal vein. For the recurrent stent dysfunction, the patient underwent placement of a plastic stent within an uncovered self-expanding metal stent to correct stent dysfunction. A 7F plastic stent inside a metal stent is shown.
The patient later experienced stent failure and jaundice due to tumor progression and was admitted for plastic stent replacement. Neither imaging results nor symptoms suggested duodenal stenosis. The transpapillary approach was attempted first but was unsuccessful. Duodenoscopy was challenging to perform because of duodenal stenosis. Fluoroscopy confirmed the duodenal stenosis. The plastic stent was extracted using an upper endoscope. Multiple uncovered metal stents are shown (1 stent in the anterior bile duct and 2 stents in the posterior bile duct). Jaundice did not resolve despite plastic stent removal.
The patient refused to undergo percutaneous biliary drainage, so a decision was made to perform an EUS-guided hepaticogastrostomy (HGS) instead. The left bile duct was observed in the stomach. The left bile duct was punctured with a 19-gauge FNA needle. A 0.025-inch hydrophilic guidewire was directed into the left bile duct. Enhancement of the bile duct showing malignant hilar biliary obstruction (bismuth IV) is seen. Insertion of the guide wire into the posterior bile duct is shown.
The stent mesh was then dilated using a balloon dilator. However, there was difficulty inserting the catheter. Additional dilation was performed using a spiral dilator. This instrument is a tapered tip dilator that fits into 0.025-inch guidewires and is expandable to 7F. Insertion of a second guidewire with a larger caliber was done to straighten the bile duct and help stabilize stent insertion. A 0.035-inch hydrophilic guidewire into the posterior bile duct using a double-lumen cannula and insertion of a 0.025-inch hydrophilic guidewire into the anterior bile duct are shown.
The stent mesh was then dilated using a spiral dilator. A metal stent was placed through the anterior bile duct at a steep angle. Insertion and deployment of the first uncovered self-expanding metal stent (8 × 60 mm) from the anterior bile duct into the left bile duct is shown. Multiple metal stents were implanted into the hilar area, and the new stent was placed using the partial stent-in-stent method to prevent overexpansion. Guidewire seeking the posterior bile duct from inside the deployed stent through the stent mesh is shown.
The stent mesh was then dilated using a balloon dilator. Insertion and deployment of an uncovered self-expanding metal stent (8 × 60 mm) from the posterior bile duct to the left bile duct using the partial stent-in-stent method is shown. Enhancement of the bile duct shows drainage from the right bile duct. The fistula of the HGS was only dilated with the spiral dilator. The risk of bile leakage was low, so we decided to implant a plastic stent. A 7F × 15-cm plastic stent was placed from the posterior bile duct into the stomach. Anterior and posterior segment drainage by EUS-HGS with bridging stenting using the partial stent-in-stent method is shown, with left segment drainage by EUS-HGS with the plastic stent.
We performed EUS-HGS on a patient with multiple metal stents in place. There were no adverse events, and total bilirubin levels were reduced by more than half within 2 weeks. Six months have passed without stent dysfunction.
EUS-guided hepaticogastrostomy (HGS) has become an effective method for biliary drainage, particularly hilar bile duct obstruction.1, 2, 3, 4, 5 We present the case of an 84-year-old woman with unresectable perihilar cholangiocarcinoma of bismuth type Ⅳ, with occluded stents placed via the transpapillary route, and whose jaundice was ultimately alleviated by pursuing a novel method of bilateral biliary decompression by EUS-HGS with bridging stenting using the partial stent-in-stent method for re-intervention of multiple metal stent failure (Fig. 1). This study was approved by our institutional review board (Approval No. 2018-149).
Figure 1.
Still figure from Video 1.
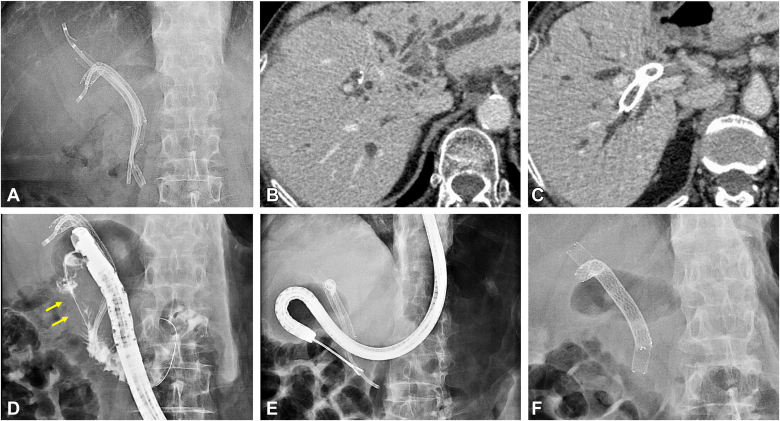
Originally, the patient received multiple uncovered self-expandable metal stents (UCSEMSs) (8 × 80 mm and 8 × 60 mm; YABUSAME; Kaneka Medix, Tokyo, Japan) for bile duct drainage, using a transpapillary approach to the posterior and anterior bile ducts. Due to left portal vein obstruction, the left segment remained undrained. One month later, the patient had stent dysfunction in the posterior segment and a UCSEMS (8 × 80 mm; ZEOSTENT; ZEON Medical, Tokyo, Japan) was placed. To address recurrent biliary obstruction, plastic stents were inserted within the UCSEMS (Fig. 2A). However, 3 months later, stent dysfunction recurred (Fig. 2B and C), complicating further transpapillary re-intervention due to malignant duodenal stenosis (Fig. 2D). We attempted reintervention by EUS-HGS, removing the plastic stent using an upper endoscopy (GIF-H260; Olympus, Tokyo, Japan) (Fig. 2E and F).
Figure 2.
Pre–EUS-guided hepaticogastrostomy images. A, Radiographic image showing the positioning of uncovered metal stents in a partial stent-in-stent configuration using plastic stents. B, CT image depicting anterior segment stent dysfunction. C, CT image depicting posterior segment stent dysfunction. D, ERCP poses challenges owing to duodenal stenosis (arrows). E, Plastic stent removal was performed using an upper endoscope. F, Radiographic view showing the positioning of the uncovered metal stents in a partial “stent-in-stent” configuration.
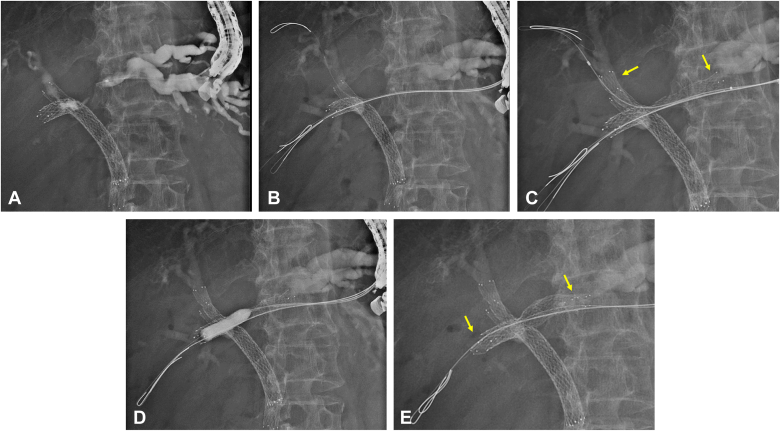
Using a convex echoendoscope (GF-UCT260; Olympus), we performed EUS-HGS (Video 1, available online at www.videogie.org). After enhancement (Fig. 3A), a 0.025-inch, 450-cm hydrophilic guidewire (Fielder 25; ASAHI Intec, Aichi, Japan) was placed in the posterior bile duct. Implantation of a larger guidewire was considered to straighten the bile duct and stabilize the procedure. However, a catheter was difficult to follow, and dilatation was performed. The stent mesh was dilated using a balloon dilator (8 mm wide; REN; Kaneka), but the catheter was difficult to follow. Therefore, additional dilation was performed using a spiral dilator (Tornus ES; Olympus), which is a tapered-tip dilator that fits 0.025-inch guidewires and is rotated clockwise while threading through the guidewire to dilate the lumen to 7F. After dilation, a 0.035-inch, 450-cm hydrophilic guidewire (RevoWave; PIOLAX Medical, Kanagawa, Japan) was placed in the posterior bile duct using a double-lumen cannula (Uneven Double Lumen Cannula; PIOLAX). A 0.025-inch, 450-cm hydrophilic guidewire (VisiGlide 2; Olympus) was then selected for the anterior bile duct (Fig. 3B). We planned to implant the stent first in the anterior bile duct where the angle is more acute, then place a second stent into the posterior. The anterior stent mesh was dilated using the spiral dilator. The first UCSEMS (8 × 60 mm; YABUSAME Neo; Kaneka) was placed in the anterior bile duct (Fig. 3C). The patient had undergone multiple stent placements for hilar bile duct obstruction, which were performed using the partial stent-in-stent method to prevent overexpansion. We threaded the 0.025-inch guidewire through the posterior bile duct within the deployed stent. The meshes were dilated using the balloon dilator (Fig. 3D). A second UCSEMS (8 × 60 mm; YABUSAME Neo) was placed in the posterior bile duct (Fig. 3E).
Figure 3.
Additional bridging stenting using the partial stent-in-stent method via hepaticogastrostomy. A, Contrast-enhanced image of the bile duct via the hepaticogastrostomy route, illustrating malignant hilar biliary obstruction (bismuth type IV). B, Concurrent insertion of guidewires into the posterior bile duct and the anterior bile duct segments in parallel. C, Deployment of the first metal stent (arrows) from the anterior bile duct into the left bile duct. D, A guidewire was inserted through the mesh of the first metal stent at the posterior bile duct, followed by the use of a balloon catheter to dilate the stent mesh and alleviate the stricture. E, Using the partial stent-in-stent technique, we placed the second metal stent (arrows) from the posterior bile duct to the left bile duct.
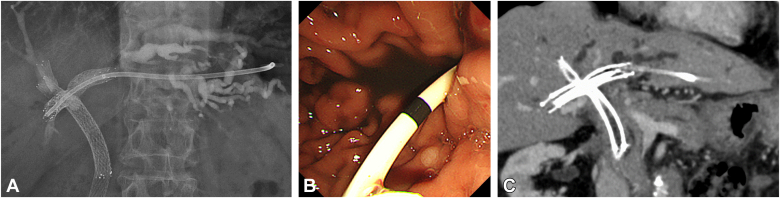
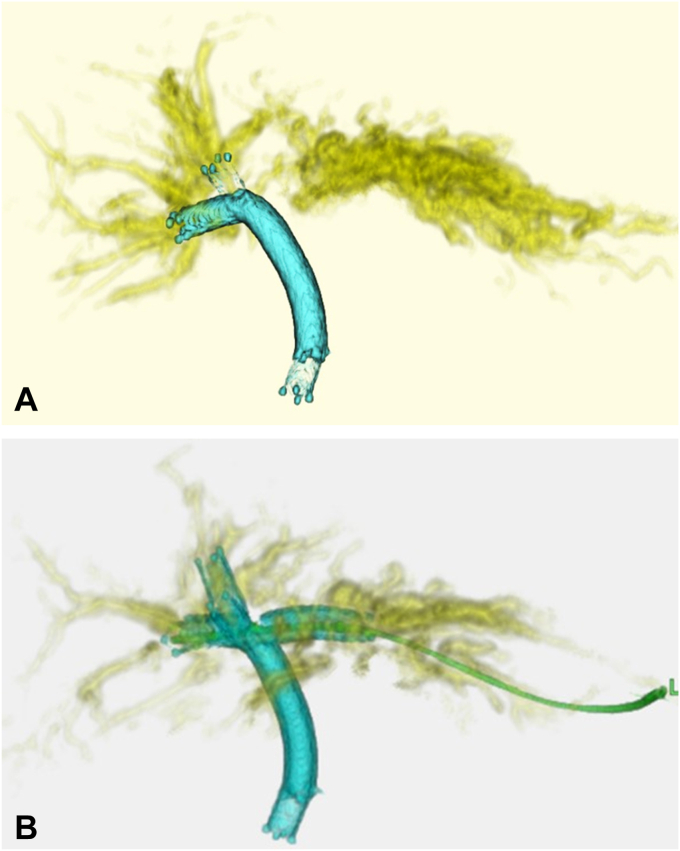
The HGS fistula was dilated using only a spiral dilator, considering the low risk of bile leakage. A plastic stent (7F × 15 cm; Harmo Ray Stent; Hanaco Medical, Saitama, Japan) was deployed from the posterior bile duct into the HGS fistula (Figs. 4 and 5). After the procedure, the patient showed significant improvement in biliary drainage, confirmed by CT scans and blood tests, with bilirubin levels dropping from 11.3 to 0.7 mg/dL over 6 months. Patient was later placed on palliative care, and when malignant gastric outlet obstruction became apparent, a duodenal stent was inserted.
Figure 4.
Hepatic drainage with additional partial stent-in-stent placement using EUS-guided hepaticogastrostomy. A, Insertion of a plastic stent extending from the posterior bile duct into the stomach. B, Endoscopic image of the stomach. C, Postprocedure CT image.
Figure 5.
Pre– and post–EUS-guided hepaticogastrostomy 3-dimensional (3D) CT images. A, Preprocedural 3D image. B, Postprocedural 3D image.
We believe that our approach is innovative and leads to successful re-intervention after transpapillary multistenting.
Funding
This work was supported by the National Cancer Center Research and Development Fund (2022-A-16).
Disclosure
The authors disclosed no financial relationships relevant to this publication.
Acknowledgments
The authors thank the members of the Endoscopy Team of the Department of Hepatobiliary and Pancreatic Oncology, National Cancer Center Hospital, for their support of this research.
Supplementary data
A novel method of bilateral biliary decompression by EUS-guided hepaticogastrostomy with bridging stenting using the partial stent-in-stent method for reintervention of multiple metal stent failure.
We report a case in which anterior and posterior drainage was performed using the partial stent-in-stent method via the transpapillary approach. The patient had a bismuth type IV biliary obstruction, but only the right hepatic lobe was drained due to obstruction of the left portal vein. For the recurrent stent dysfunction, the patient underwent placement of a plastic stent within an uncovered self-expanding metal stent to correct stent dysfunction. A 7F plastic stent inside a metal stent is shown.
The patient later experienced stent failure and jaundice due to tumor progression and was admitted for plastic stent replacement. Neither imaging results nor symptoms suggested duodenal stenosis. The transpapillary approach was attempted first but was unsuccessful. Duodenoscopy was challenging to perform because of duodenal stenosis. Fluoroscopy confirmed the duodenal stenosis. The plastic stent was extracted using an upper endoscope. Multiple uncovered metal stents are shown (1 stent in the anterior bile duct and 2 stents in the posterior bile duct). Jaundice did not resolve despite plastic stent removal.
The patient refused to undergo percutaneous biliary drainage, so a decision was made to perform an EUS-guided hepaticogastrostomy (HGS) instead. The left bile duct was observed in the stomach. The left bile duct was punctured with a 19-gauge FNA needle. A 0.025-inch hydrophilic guidewire was directed into the left bile duct. Enhancement of the bile duct showing malignant hilar biliary obstruction (bismuth IV) is seen. Insertion of the guide wire into the posterior bile duct is shown.
The stent mesh was then dilated using a balloon dilator. However, there was difficulty inserting the catheter. Additional dilation was performed using a spiral dilator. This instrument is a tapered tip dilator that fits into 0.025-inch guidewires and is expandable to 7F. Insertion of a second guidewire with a larger caliber was done to straighten the bile duct and help stabilize stent insertion. A 0.035-inch hydrophilic guidewire into the posterior bile duct using a double-lumen cannula and insertion of a 0.025-inch hydrophilic guidewire into the anterior bile duct are shown.
The stent mesh was then dilated using a spiral dilator. A metal stent was placed through the anterior bile duct at a steep angle. Insertion and deployment of the first uncovered self-expanding metal stent (8 × 60 mm) from the anterior bile duct into the left bile duct is shown. Multiple metal stents were implanted into the hilar area, and the new stent was placed using the partial stent-in-stent method to prevent overexpansion. Guidewire seeking the posterior bile duct from inside the deployed stent through the stent mesh is shown.
The stent mesh was then dilated using a balloon dilator. Insertion and deployment of an uncovered self-expanding metal stent (8 × 60 mm) from the posterior bile duct to the left bile duct using the partial stent-in-stent method is shown. Enhancement of the bile duct shows drainage from the right bile duct. The fistula of the HGS was only dilated with the spiral dilator. The risk of bile leakage was low, so we decided to implant a plastic stent. A 7F × 15-cm plastic stent was placed from the posterior bile duct into the stomach. Anterior and posterior segment drainage by EUS-HGS with bridging stenting using the partial stent-in-stent method is shown, with left segment drainage by EUS-HGS with the plastic stent.
We performed EUS-HGS on a patient with multiple metal stents in place. There were no adverse events, and total bilirubin levels were reduced by more than half within 2 weeks. Six months have passed without stent dysfunction.
References
- 1.Nakai Y., Kogure H., Isayama H., et al. Endoscopic ultrasound-guided biliary drainage for unresectable hilar malignant biliary obstruction. Clin Endosc. 2019;52:220–225. doi: 10.5946/ce.2018.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caillol F., Bosshardt C., Reimao S., et al. Drainage of the right liver under EUS guidance: a bridge technique allowing drainage of the right liver through the left liver into the stomach or jejunum. Endosc Ultrasound. 2019;8:199–203. doi: 10.4103/eus.eus_64_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogura T., Sano T., Onda S., et al. Endoscopic ultrasound-guided biliary drainage for right hepatic bile duct obstruction: novel technical tips. Endoscopy. 2015;47:72–75. doi: 10.1055/s-0034-1378111. [DOI] [PubMed] [Google Scholar]
- 4.Maehara K., Hijioka S., Nagashio Y., et al. Simultaneous endoscopic ultrasound-guided hepaticogastrostomy and bridging stenting with partial stent-in-stent method. Endoscopy. 2020;52:E381–E382. doi: 10.1055/a-1134-4482. [DOI] [PubMed] [Google Scholar]
- 5.Kanai S., Saito T., Hakuta R., et al. Transverse stent placement for hilar malignant biliary obstruction through an endoscopic ultrasound-guided hepaticogastrostomy route. Endoscopy. 2019;51:E245–E246. doi: 10.1055/a-0889-7329. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A novel method of bilateral biliary decompression by EUS-guided hepaticogastrostomy with bridging stenting using the partial stent-in-stent method for reintervention of multiple metal stent failure.
We report a case in which anterior and posterior drainage was performed using the partial stent-in-stent method via the transpapillary approach. The patient had a bismuth type IV biliary obstruction, but only the right hepatic lobe was drained due to obstruction of the left portal vein. For the recurrent stent dysfunction, the patient underwent placement of a plastic stent within an uncovered self-expanding metal stent to correct stent dysfunction. A 7F plastic stent inside a metal stent is shown.
The patient later experienced stent failure and jaundice due to tumor progression and was admitted for plastic stent replacement. Neither imaging results nor symptoms suggested duodenal stenosis. The transpapillary approach was attempted first but was unsuccessful. Duodenoscopy was challenging to perform because of duodenal stenosis. Fluoroscopy confirmed the duodenal stenosis. The plastic stent was extracted using an upper endoscope. Multiple uncovered metal stents are shown (1 stent in the anterior bile duct and 2 stents in the posterior bile duct). Jaundice did not resolve despite plastic stent removal.
The patient refused to undergo percutaneous biliary drainage, so a decision was made to perform an EUS-guided hepaticogastrostomy (HGS) instead. The left bile duct was observed in the stomach. The left bile duct was punctured with a 19-gauge FNA needle. A 0.025-inch hydrophilic guidewire was directed into the left bile duct. Enhancement of the bile duct showing malignant hilar biliary obstruction (bismuth IV) is seen. Insertion of the guide wire into the posterior bile duct is shown.
The stent mesh was then dilated using a balloon dilator. However, there was difficulty inserting the catheter. Additional dilation was performed using a spiral dilator. This instrument is a tapered tip dilator that fits into 0.025-inch guidewires and is expandable to 7F. Insertion of a second guidewire with a larger caliber was done to straighten the bile duct and help stabilize stent insertion. A 0.035-inch hydrophilic guidewire into the posterior bile duct using a double-lumen cannula and insertion of a 0.025-inch hydrophilic guidewire into the anterior bile duct are shown.
The stent mesh was then dilated using a spiral dilator. A metal stent was placed through the anterior bile duct at a steep angle. Insertion and deployment of the first uncovered self-expanding metal stent (8 × 60 mm) from the anterior bile duct into the left bile duct is shown. Multiple metal stents were implanted into the hilar area, and the new stent was placed using the partial stent-in-stent method to prevent overexpansion. Guidewire seeking the posterior bile duct from inside the deployed stent through the stent mesh is shown.
The stent mesh was then dilated using a balloon dilator. Insertion and deployment of an uncovered self-expanding metal stent (8 × 60 mm) from the posterior bile duct to the left bile duct using the partial stent-in-stent method is shown. Enhancement of the bile duct shows drainage from the right bile duct. The fistula of the HGS was only dilated with the spiral dilator. The risk of bile leakage was low, so we decided to implant a plastic stent. A 7F × 15-cm plastic stent was placed from the posterior bile duct into the stomach. Anterior and posterior segment drainage by EUS-HGS with bridging stenting using the partial stent-in-stent method is shown, with left segment drainage by EUS-HGS with the plastic stent.
We performed EUS-HGS on a patient with multiple metal stents in place. There were no adverse events, and total bilirubin levels were reduced by more than half within 2 weeks. Six months have passed without stent dysfunction.
A novel method of bilateral biliary decompression by EUS-guided hepaticogastrostomy with bridging stenting using the partial stent-in-stent method for reintervention of multiple metal stent failure.
We report a case in which anterior and posterior drainage was performed using the partial stent-in-stent method via the transpapillary approach. The patient had a bismuth type IV biliary obstruction, but only the right hepatic lobe was drained due to obstruction of the left portal vein. For the recurrent stent dysfunction, the patient underwent placement of a plastic stent within an uncovered self-expanding metal stent to correct stent dysfunction. A 7F plastic stent inside a metal stent is shown.
The patient later experienced stent failure and jaundice due to tumor progression and was admitted for plastic stent replacement. Neither imaging results nor symptoms suggested duodenal stenosis. The transpapillary approach was attempted first but was unsuccessful. Duodenoscopy was challenging to perform because of duodenal stenosis. Fluoroscopy confirmed the duodenal stenosis. The plastic stent was extracted using an upper endoscope. Multiple uncovered metal stents are shown (1 stent in the anterior bile duct and 2 stents in the posterior bile duct). Jaundice did not resolve despite plastic stent removal.
The patient refused to undergo percutaneous biliary drainage, so a decision was made to perform an EUS-guided hepaticogastrostomy (HGS) instead. The left bile duct was observed in the stomach. The left bile duct was punctured with a 19-gauge FNA needle. A 0.025-inch hydrophilic guidewire was directed into the left bile duct. Enhancement of the bile duct showing malignant hilar biliary obstruction (bismuth IV) is seen. Insertion of the guide wire into the posterior bile duct is shown.
The stent mesh was then dilated using a balloon dilator. However, there was difficulty inserting the catheter. Additional dilation was performed using a spiral dilator. This instrument is a tapered tip dilator that fits into 0.025-inch guidewires and is expandable to 7F. Insertion of a second guidewire with a larger caliber was done to straighten the bile duct and help stabilize stent insertion. A 0.035-inch hydrophilic guidewire into the posterior bile duct using a double-lumen cannula and insertion of a 0.025-inch hydrophilic guidewire into the anterior bile duct are shown.
The stent mesh was then dilated using a spiral dilator. A metal stent was placed through the anterior bile duct at a steep angle. Insertion and deployment of the first uncovered self-expanding metal stent (8 × 60 mm) from the anterior bile duct into the left bile duct is shown. Multiple metal stents were implanted into the hilar area, and the new stent was placed using the partial stent-in-stent method to prevent overexpansion. Guidewire seeking the posterior bile duct from inside the deployed stent through the stent mesh is shown.
The stent mesh was then dilated using a balloon dilator. Insertion and deployment of an uncovered self-expanding metal stent (8 × 60 mm) from the posterior bile duct to the left bile duct using the partial stent-in-stent method is shown. Enhancement of the bile duct shows drainage from the right bile duct. The fistula of the HGS was only dilated with the spiral dilator. The risk of bile leakage was low, so we decided to implant a plastic stent. A 7F × 15-cm plastic stent was placed from the posterior bile duct into the stomach. Anterior and posterior segment drainage by EUS-HGS with bridging stenting using the partial stent-in-stent method is shown, with left segment drainage by EUS-HGS with the plastic stent.
We performed EUS-HGS on a patient with multiple metal stents in place. There were no adverse events, and total bilirubin levels were reduced by more than half within 2 weeks. Six months have passed without stent dysfunction.