Abstract
Suboptimal teamwork in the operating room (OR) is a contributing factor in a significant proportion of preventable complications for surgical patients. Specifying behaviour is fundamental to closing evidence-practice gaps in healthcare. Current teamwork interventions, however, have yet to be synthesized in this way. This scoping review aimed to identify actionable strategies for use during surgery by mapping the existing literature according to the Action, Actor, Context, Target, Time (AACTT) framework. The databases MEDLINE (Medical Literature Analysis and Retrieval System Online), Embase, Cumulated Index to Nursing and Allied Health Literature (CINAHL), Education Resources Information Center (ERIC), Cochrane, Scopus, and PsycINFO were searched from inception to April 5, 2022. Screening and data extraction were conducted in duplicate by pairs of independent reviewers. The search identified 9,289 references after the removal of duplicates. Across 249 studies deemed eligible for inclusion, eight types of teamwork interventions could be mapped according to the AACTT framework: bundle/checklists, protocols, audit and feedback, clinical practice guidelines, environmental change, cognitive aid, education, and other), yet many were ambiguous regarding the actors and actions involved. The 101 included protocol interventions appeared to be among the most actionable for the OR based on the clear specification of ACCTT elements, and their effectiveness should be evaluated and compared in future work.
Keywords: interdisciplinary teamwork, scoping review, operating room, patient outcomes, human factors, medical education, healthcare simulation, surgical safety checklist
Introduction and background
Suboptimal teamwork in the operating room (OR) is a contributing factor in a significant proportion of preventable complications for surgical patients [1-6]. Despite its critical implications for patient safety, best practices for effective teamwork in the OR have yet to be identified [7,8]. Teamwork is defined as the collaborative effort and the dynamic interactions within a group to achieve a common goal. Whether due to poor communication or unclear roles, suboptimal teamwork causes inefficient collaboration, leading to poor performance and increased errors. When such inefficiencies are overcome, effective teamwork is achieved. This can be brought about using teamwork interventions, which focus on improving interactions to bolster performance, safety, and efficiency. Teamwork interventions in the literature include checklists (e.g., Surgical Safety Checklists (SSC)), time-outs or team huddles, tools to facilitate concise communication (e.g., Situation-Background- Assessment-Recommendation (SBAR)), teamwork tools and frameworks (e.g., Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS™)), and high-fidelity simulation training or courses. Interventions aiming to improve OR teamwork have yielded mixed results [9-11]. While a lack of clarity regarding actionable teamwork practices is one plausible contributing factor, study design and confounding variables likely also play a role [9,12-16]. Unlike other high-risk industries such as aviation, recommendations about teamwork for the OR continue to revolve around general principles such as "mutual trust" or "adaptability" [17]. Without precise specification of who needs to do what differently, when, where, and how, the development of a shared mental model is challenging at best [18].
Teamwork concepts are typically covered to varying degrees in education and training sessions [10], but less attention is given to well-described and actionable behaviours that can facilitate the identification of best teamwork practices in everyday clinical practice. Previous studies have identified one of the most frequent barriers to effective teamwork within healthcare settings as being the clinicians' lack of knowledge of established best practices or strategies [19,20]. It is thus crucial to empirically establish best practices and disseminate them to clinicians to enhance patient safety. This is particularly significant, given the lack of substantial annual reduction in patient safety events in recent years [21,22].
Specifying expected behaviour is fundamental to closing evidence-practice gaps in healthcare [23-25]. In implementation science, the Action, Actor, Context, Target, Time (AACTT) is an established framework that specifies the necessary elements for an intervention to be considered actionable, thus enhancing intervention effectiveness [26]. Existing systematic reviews have broadly included all forms of teamwork interventions without clearly delineating which interventions contain sufficient behavioural detail for application in the OR [10,11,27]. Identifying actionable teamwork strategies for the OR, rather than broad interventions that emphasize abstract concepts in a classroom setting, is an important step towards providing clinicians with a common ground from which to approach interprofessional teamwork.
This scoping review aims to evaluate the extent to which the current teamwork literature describes actionable practices for use in surgery. We aim to achieve this by mapping studies according to the AACTT framework to identify actionable surgical teamwork practices. This may inform future efforts to improve interprofessional teamwork in the OR.
Review
Methods
We carried out the scoping review following the updated Preferred Reported Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines [28]. These guidelines help ensure that scoping reviews possess greater transparency and reliability [28]. Unlike systematic reviews, scoping reviews aim to provide an overview of the available evidence rather than "a summary answer to a discrete research question" [29]. Scoping reviews are useful for answering complex questions in broad areas of literature that have yet to be comprehensively summarized [29,30]. As such, scoping reviews are often preliminary steps to conducting one or several systematic reviews, as the identification of key knowledge gaps informs specific research questions. Since scoping reviews usually contain an expansive purview of information, meta-analytic methods are most often impossible, and risk of bias assessments are not considered essential [29,30].
Information Sources and Search Strategy
Literature searches were conducted using MEDLINE (Medical Literature Analysis and Retrieval System Online), Embase, Cumulated Index to Nursing and Allied Health Literature (CINAHL), Education Resources Information Center (ERIC), Cochrane, Scopus, and PsycINFO databases from inception to April 5, 2022 (See Appendices). The electronic search strategy was developed by an information specialist (AD) in collaboration with the research team and then peer-reviewed in accordance with the Peer Review of Electronic Search Strategies (PRESS) guidelines [31]. A manual screening of the reference lists of included studies was conducted by senior investigators to identify additional potentially relevant articles. All identified articles were imported into DistillerSR (Evidence Partners, Ottawa, Canada), a web-based review software. Duplicate records were removed.
Eligibility Criteria
We defined teamwork interventions as interventions that focus on improving interactions to bolster performance, safety, and efficiency. All empirical study designs were eligible for inclusion provided they explored a teamwork intervention that is actionable, as per the AACTT framework, and could be implemented during the intraoperative period. This meant that an intervention was eligible if it did not require resources/equipment that were not accessible in the OR, did not significantly disrupt OR flow, and did not put at risk patient or staff safety. Studies had to include two or more healthcare professions and could be conducted in any healthcare environment to broaden the possibilities of interventions. Clinical and simulation studies were also eligible for inclusion. Measures of intervention efficacy were not a requirement for inclusion in this scoping review, as our goal was to identify actionable intraoperative teamwork practices or strategies. The elements of the AACTT framework include (I) Action (i.e., behaviour that can be observed and measured), (ii) Actor (i.e., the individual that is doing or could do the behaviour), (iii) Context (i.e., the setting in which the action is performed), (iv) Time (i.e., when the behaviour is performed), and (v) Target (i.e., the person/people with/for whom the action is performed) [26]. Initial eligible study settings included healthcare and other high-risk industries (aviation, military). The protocol was later amended to include only studies conducted in a healthcare setting to provide a more focused review. Only peer-reviewed studies published in English and French were included, while studies in other languages were excluded due to limited resources. Commentaries, editorials, and letters to the editor were not eligible for inclusion.
Screening
Screening was conducted by investigators in two stages using the inclusion and exclusion criteria: (I) title and abstract and (ii) full-length screening. All screeners had a background in research and/or medicine. To ensure standardization, the screening protocol was discussed during an introductory meeting, and a pilot screen was conducted until standardization was achieved.
Two independent investigators screened articles at the title and abstract stage, as well as the full-text stage in duplicate. Excluded studies were flagged with a reason for exclusion and reviewed by two additional healthcare and teamwork experts to confirm the reason for exclusion. Both stages followed the same process, whereby all articles were reviewed in duplicate by two independent reviewers. If consensus could not be achieved, a third reviewer was involved in resolving conflicts.
Data Extraction
A data extraction form was created prior to the literature search and piloted by the research team. There was a training period to trial the form and ensure all reviewers understood the items and documented pilot articles in a unified manner. Data items were extracted using the data extraction form by pairs of independent reviewers. The second reviewer of each pair verified the data extraction of the first reviewer for accuracy, and any disagreements between the two reviewers were flagged for discussion. If consensus could not be reached, a third reviewer was involved. When data items were inadequately reported in the full text, attempts at contacting the original authors were made to clarify and confirm relevant details.
Data Items and Synthesis of Results
The data collected included publication details (e.g., first author, journal, year of publication, country of origin), study design, sample and participants, setting, title, type, description of the teamwork intervention, and which of the AACTT elements the intervention specified. Data collection and synthesis were conducted by one reviewer, with a second reviewer verifying the accuracy and consistency of the extracted data and classifications. Data extracted from the included studies were organized into distinct domains based on established categories of practice-changing interventions. These domains encompassed various types of intraoperative teamwork interventions, including bundle/checklists, protocols, audit and feedback, clinical practice guidelines, environmental changes, cognitive aids, education, and others [32]. Each intervention type was systematically identified and categorized to facilitate comprehensive analysis and synthesis of the literature. Data were organized according to the AACTT framework, which served as a guiding framework for mapping out the specific elements of each intervention, including the actions undertaken, the actors involved, the contextual factors influencing implementation, the intended targets or recipients of the intervention, and the temporal aspects of intervention delivery. This categorization facilitated a nuanced understanding of the teamwork interventions' characteristics and actionability in the intraoperative period.
Quantitative and qualitative data extracted from included studies were subject to comprehensive analysis to elucidate key findings and insights. Quantitative data, such as the frequency of intervention types across studies, were analyzed using appropriate summary statistics, including counts and percentages. This quantitative analysis provided a quantitative overview of the prevalence and distribution of different intervention types within the literature. Qualitative data, including descriptions of intervention components and their associated AACTT elements, were subjected to thematic analysis. The thematic analysis involved the identification of recurrent themes, patterns, and trends within the extracted data. By systematically examining the qualitative data, commonalities, variations, and nuances in intervention characteristics and implementation strategies were identified. These thematic insights provided a qualitative understanding of the diverse approaches to intraoperative teamwork interventions and illuminated the contextual factors shaping their implementation and effectiveness.
Results
Study Selection
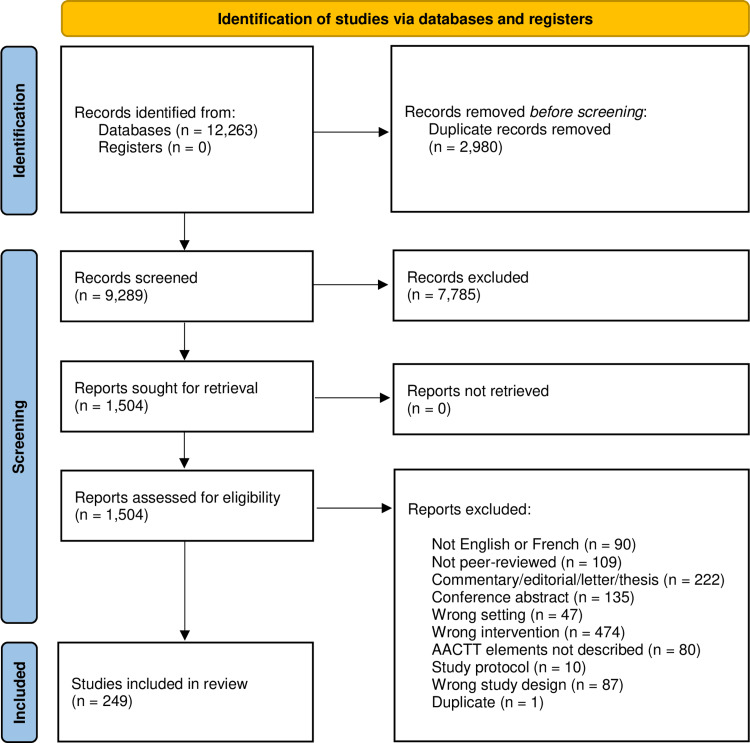
There were 9,289 relevant studies identified from our literature search. Of these, 7,785 were excluded at the title and abstract screening, and 1,255 were excluded at full-text screening. This resulted in a total of 249 articles included in this review (Figure 1).
Figure 1. PRISMA Flowchart.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Summary of Study Characteristics
Of the 249 included studies, 137 (55.0%) were published in the United States. A wide range of study designs were observed, with the most common being before-and-after studies (n=88; 35.3%) and non-randomized experimental studies (n=66; 26.5%). More than two-thirds of studies (n=172; 69.1%) involved the OR and corresponding healthcare professionals such as surgeons, anesthesiologists, and circulating or scrub nurses. Sample populations (i.e., the number of each type of professional involved) were not consistently reported across studies. Outside of the OR, study settings included hospital wards (n=17; 6.8%), obstetrics (n=6; 2.4%), post-anesthesia or intensive care units (n=8; 3.2%), trauma rooms (n=10; 4%), emergency departments (n=5; 2%), multiple health care settings (n=23; 9.2%), and other settings such as long-term care and outpatient clinics (n=8; 3.2%). Education was the most frequently reported type of intervention (n=108; 43.4%), while bundle/checklists were the second most reported (n=76; 30.5%). Other types of interventions described across included studies were protocols (n=38; 15.3%), audit and feedback (n=16; 6.4%), clinical practice guidelines (n=1; <1%), environment improvement (n=1, <1%), cognitive aids (n=5; 2%), and other interventions such as hands-free communication devices (n=4; 1.6%).
AACTT Specifications Across Included Studies
A summary of the AACTT specifications across the included studies is provided in Table 1. The action (i.e., behaviour) specified by most studies (n=133; 53.4%) was to follow a series of steps or tasks listed in the intervention bundle or checklist; however, only 76 (30.5%) of studies specified the actor (i.e., the person who performs the action). For example, the Surgical Patient Safety System (SURPASS) checklist described by de Vries et al. [33] specifies which individual team member (e.g., anesthesiologist) is responsible for completing each item (e.g., checking patient allergies and equipment) across each phase in the surgical pathway (e.g., at the OR time-out). The SSC was described by 24 studies (9.6%) and specifies many individual actions occurring throughout the procedure but did not always precisely specify the actor or target. For example, the checklist states "with at least nurse and anesthetist" regarding the actions that are to take place before induction of anesthesia but does not explicitly state who does which item. Similarly, actions before skin incision and before the patient leaves the OR are stated to take place "with the nurse, anesthetist, and surgeon," but the specific actor and target of several checklist items are not systematically indicated.
Table 1. Summary of Action, Actor, Context, Target, Time (AACTT) framework across included studies.
%: Represents the number of studies over the total number of studies, N, where N=249.
| Framework Component | Number of studies (%) |
| Action | |
| Follow a series of steps or tasks listed in a checklist or protocol | 133 (53.4%) |
| Take specific individual action (e.g., silence mobile devices) | 101 (40.5%) |
| Use specified electronic tool (e.g., hands free communication device) | 15 (6%) |
| Actor | |
| Any/all team members | 158 (63.4%) |
| Individual (staff) team member as specified | 76 (30.5%) |
| Patient & team members as specified | 3 (1.2%) |
| Trainee | 11 (4.4%) |
| Any team member except trainees and travel nurses | 1 (<1%) |
| Context | |
| Hospital ward | 17 (6.8%) |
| Operating room | 172 (69.1%) |
| Obstetrics | 6 (2.4%) |
| Post-anesthesia care unit | 1 (<1%) |
| Intensive care unit | 7 (2.8%) |
| Trauma centre | 10 (4%) |
| Multiple health care settings | 23 (9.2%) |
| Emergency department | 5 (2.0%) |
| Other (e.g., long-term care, outpatient clinic) | 8 (3.2%) |
| Target | |
| Any/all team members | 161 (64.7%) |
| Individual (staff) team member as specified | 40 (16.1%) |
| Patient | 6 (2.4%) |
| Patient and team members as specified | 35 (14.1%) |
| Trainee | 7 (2.8%) |
| Time | |
| At specified intervals | 18 (7.2%) |
| As needed | 26 (10.4%) |
| Critical situation | 39 (15.6%) |
| Handover | 13 (5.2%) |
| Before procedure | 34 (13.6%) |
| Before procedure and as needed | 1 (<1%) |
| During procedure | 51 (20.4%) |
| Before and after procedure | 11 (4.4%) |
| Before, during and after procedure | 45 (18%) |
| Not reported | 3 (1%) |
Interventions involving specific individual actions rather than a multi-step, multi-actor bundle or checklist were described by 101 studies (40.5%). A representative example of 10 studies is shown in Table 2. One example is closed-loop communication [34], which involves the components of a callout (i.e., verbal order), check back (i.e., confirmation that information was received), and closing the loop (i.e., the acknowledgement that the receiver correctly understood the information). Other examples involved protocols to minimize distractions. The noise reduction intervention described by Wright et al., for example, requires OR team members to eliminate non-essential conversation, turn the volume down or off on electronics, silence mobile devices, and avoid the use of unnecessary instruments or devices that increase noise levels (Table 2) [35]. Similarly, the "sterile cockpit" protocol introduced by West et al. aiming to improve the efficacy and safety of nursing assistants (NAs) specifies the actions for registered nurses to take, such as "engage the NAs only in professional conversations" and "take phone calls and messages for the NAs" (Table 2) [36].
Table 2. Examples of specific teamwork behaviours identified across relevant studies (N=10).
OR: operating room; NA: nursing assistant
| Study | Action | Actor | Context | Target | Time |
| Sucharew and Macaluso, 2019 [29] | Use closed-loop communication: Callout – verbal order Check back – confirm information received Closing the loop – acknowledge correct understanding of information | Team leader | Trauma centre | Any team member | During procedure |
| Sinuff et al., 2013 [32] | Classify situation urgency with the Traffic Lights tool: Red alert – life-threatening emergency Amber assist – help is required within minutes Green query – advice/non-urgent assistance required | Anesthesia trainee | Operating room | Staff anesthesiologist | During procedure |
| Pham et al., 2014 [30] | Reduce noise by eliminating non-essential conversation: Turn the volume down or off on electronics, slience mobile devices, avoid the use of instruments or devices that increase noise levels if they are unnecessary at that time | All team members | OR | All team members | During anesthesia induction, surgical briefing, specimen collection, final surgical counts and debriefing, and anesthesia emergence |
| McGowan et al., 2015 [31] | Minimize distractions and interruptions: Intercept individuals who would otherwise have contact NAs, take phone calls and messages for the NAs, answer call lights and patient requests that normally would have been handled by the NAs, engage the NAs only in professional conversations, restrict overhead paging (use phones or nurse pagers only) | Registered Nurses | Cardiac medicine unit | NAs | Any time during the shift |
| De Vries et al., 2011 [33] | Remind the team when OR traffic is excessive. | Surgeon | OR | All team members | During procedure |
| El-Shafy et al., 2018 [34] | Follow the established communication structure: (Surgeon) Call out the colour for the next tool (Surgeon) Say “disabled” once the tool is disabled on the control panel (Nurse) Say “ready” once the new tool is secured | Surgeon and Nurse | OR | Surgeon and Nurse | During procedure |
| Wright, 2016 [35]; West et al., 2012 [36] | Communicate using the SBAR tool. Situation: describe the current status of the patient and provide a concise statement of the problem; Background: provide pertinent and brief information related to the situation; Assessment: provide an overall analysis of the patient and their status; Recommendation: explain what exactly needs to be done after the original team member leaves | Giver of information | OR/intensive care unit/post-anesthetic care unit | Receiver of information | Handover |
The context (i.e., setting) of the interventions across the included studies was largely in the OR itself (n=172; 69.1%) with the action specified as taking place during the procedure (n=51; 20.5%), without consistently indicating an exact point in or duration of time. By contrast, other studies indicated a specific time for the action to occur, such as during a critical situation (n=39; 15.7%) or handover (n=13; 5.2%). Interventions tended to target team members in general (n=161; 63.8%), or an individual specified team member (n=40; 16.1%). Patients were included as the target (i.e., the person for whom the action is performed) of the interventions in 6 (2.4%) studies.
Discussion
This scoping review provides an overview of actionable teamwork practices that could be implemented intraoperatively. We identified eight different types of teamwork interventions across 249 studies that included practices or strategies that were actionable, and thus mapped according to the AACTT framework. The included interventions typically involved many unspecific actions and actors. Conversely, a smaller number of included studies reported on protocol interventions with single, well-defined actions required of all or specific team members. Within these interventions, the prescribed actions are related primarily to improving communication practices or reducing distractions.
A potential advantage of the communication and distraction protocol interventions identified in this review is that they contain fewer and more specific behavioural specifications (e.g., closed-loop communication, silence mobile devices). By comparison, the included bundle/checklist interventions are more complex, as they contain many possible answers to the key implementation question "who needs to do what differently" [26]. This review ultimately raises important questions about AACTT specification among widely implemented interventions. It is possible that the lack of actionable descriptions of teamwork interventions may explain the mixed results observed regarding the effectiveness of such teamwork interventions [9-11,37,38]. Although these interventions may initially appear straightforward, the ambiguity of the AACTT elements may undermine their effectiveness. Other studies have confirmed that ambiguity remains one of the key implementation and compliance challenges affecting the SSC [39]. These findings, along with the results of this scoping review, speak to the common implementation challenge of balancing fidelity (i.e., the intervention is delivered, received, and enacted as intended) and adaptation (i.e., adjustments to the original intervention made by implementers or users as they go about delivering an intervention) [40,41]. Fidelity may be easier to accomplish with the identified communication and distraction protocols, in comparison to the bundle/checklist interventions, and adaptation may be less variable. Accordingly, the reproducibility and sustained effectiveness of the interventions may be enhanced.
Implementing specific teamwork practices or strategies also has the potential to establish effective teamwork as a routine practice across intraoperative settings. Indeed, in real-world healthcare settings, interventions that explicitly designate specific roles for actors and/or targets are more likely to be actionable for several reasons. Firstly, such interventions provide clarity and accountability by clearly delineating the responsibilities of each team member, ensuring that everyone understands their role in implementing the intervention. This clarity enhances accountability within the healthcare team and minimizes confusion regarding task ownership. Secondly, interventions with clearly defined roles are more effectively implemented, as they reduce ambiguity and enable healthcare professionals to carry out their tasks accurately and consistently [20]. Thirdly, specifying roles allows for customization and adaptation of interventions to fit the unique needs and dynamics of different healthcare settings, fostering flexibility and scalability. Additionally, clear role assignments facilitate communication and collaboration among team members, promoting seamless coordination of actions and effective achievement of common goals. Finally, interventions with specific roles are easier to evaluate and provide feedback on, enabling continuous quality improvement and optimization of outcomes [42]. Overall, interventions that name specific roles for actors and/or targets enhance clarity, accountability, implementation effectiveness, customization, communication, collaboration, and evaluation, making them more actionable and conducive to successful adoption in real-world healthcare contexts [43]. In addition, clinicians’ limited knowledge of specific practices or strategies for engaging in effective teamwork [19,20] is further indicative of the value of interventions that specify the AACTT elements. Studies demonstrate a shared mental model is an essential characteristic of high-performing teams [44-46]. Therefore, at minimum, the teamwork practices or strategies elicited from these types of interventions could promote a common understanding of effective teamwork among interprofessional team members.
Given the proliferation of checklists over the last decade as a strategy for reducing medical errors [47] and the widespread use of the SSC in particular [48,49], it is not surprising that these were among the most identified interventions. While several reviews have demonstrated at least moderate effectiveness of the SSC in improving patient outcomes, there is less evidence that the checklist consistently enhances teamwork [50,51]. In fact, when used sub-optimally, checklists can even negatively impact team functioning [52]. For example, the checklist can reinforce professional divisions by failing to include all individuals or professional groups during the "checking" process. Many studies also suggest the implementation of and compliance with the SSC remains challenging [53-55], and that the checklist "may encourage box-ticking without true fidelity to (its) communications and process assurance aspects" [56]. Future studies utilizing checklists can be improved by ensuring all checklist items can be mapped to all components of the AACTT framework. Analyzing teamwork interventions through the lens of the ACCTT framework is valuable as it specifies how an intervention should be applied and may therefore facilitate implementation. In cases where checklists have previously failed or were deemed to be ineffective, specific communication interventions, such as those identified in this review, may provide a more direct way of improving teamwork rather than expecting it to be a by-product of various task-related checkboxes.
The implementation of any teamwork intervention should take local barriers and enablers into consideration [18]. It could be expected that specific behavioural interventions are more amenable to local tailoring than those which are more ambiguous, and future research may wish to investigate this hypothesis. Differences in compliance rates between specific versus ambiguous interventions may also be an insightful area of research to pursue.
Strengths and Limitations
This scoping review involved a comprehensive search strategy and a rigorous screening process. Nevertheless, it is likely that some relevant studies were missed based on inconsistencies in reporting across studies and the potential subjectivity of reviewers in determining whether interventions satisfied AACTT criteria. To mitigate this risk, screeners were trained prior to conducting the review; all screening was conducted in duplicate, and exclusion decisions were reviewed and verified by two independent research team members.
Although our review focused on practices that can be conducted inside the clinical OR, we recognize that other types of interventions can still be of value. The strategies we identified may be advantageous in that they can be incorporated into daily clinical practice and provide healthcare professionals with a shared foundation for effective teamwork. This, of course, does not preclude the use of additional interventions targeting individual provider skills, professional hierarchies, or organizational culture. Another limitation of this study is the deductive methodology used to identify actionable practices for use during surgery. This specific method was chosen to ensure that our study was based on a recognized framework with pre-defined categories that provide a basis for practical application. We recognize, however, that this approach may prevent us from identifying new categories of interventions that do not fit within the established categories or fit in a non-specific "other" category. In the future, employing an inductive approach may capture a more comprehensive list of practices that go beyond these pre-defined categories. Finally, we did not assess the quality of the included studies or their effectiveness, as this is typically not required for a scoping review. The goal of this scoping review was to identify actionable teamwork practices for the OR, rather than to assess intervention effectiveness. We intend to conduct a subsequent study using the identified strategies to further explore the most promising strategies from the perspective of the AACTT framework for routine application in the OR. Given its advantages, teamwork interventions should be designed and described with the AACTT framework in mind, which may improve the actionability and duplicability of interventions described in future research. Systematic reviews assessing the effectiveness of specific types of interventions based on study-reported outcomes could be among the next steps. Further studies on the varied implementation process may also help to better understand the conflicting success achieved with various teamwork strategies.
Conclusions
This scoping review identifies actionable teamwork practices for intraoperative implementation, encompassing eight intervention types across 249 studies by mapping the existing literature according to the AACTT framework. While most interventions lacked specificity in actions and actors, protocol interventions offered clear roles, primarily focusing on communication improvement and distraction reduction. Specific role designation enhances clarity, accountability, and implementation effectiveness. Clear role assignments facilitate communication, collaboration, and evaluation, promoting effective teamwork and shared mental models among interprofessional team members. The implementation of any teamwork intervention should take local barriers and enablers into consideration, and tailor interventions accordingly. Future research may consider evaluating differences in compliance rates between specific versus ambiguous interventions.
Acknowledgments
Authors Nibras Ghanmi and Mostafa Bondok contributed equally to this work. The authors thank Tabitha Tse, MD, Paul Ioudovski, MPH, Jennifer Rowe, MD, Michelle Turcotte, MD, Hira Khan, Amin Zahrai, Agnes Crnic, MD, Sarah Larrigan, MD, Leilani Doyle, MD, and Justin Presseau, PhD for their initial contributions during the early stages of this manuscript. The authors thank Alexandra Davis, MLIS for developing the search strategy.
Appendices
Table 3. Electronic search strategy.
| Line Number | Search Terms |
| Ovid MEDLINE(R) ALL | |
| 1 | *patient care team/ or Patient Care Team/st [Standards] |
| 2 | team*.ti,kw. |
| 3 | teamwork.tw,kw. |
| 4 | team member*.tw,kw. |
| 5 | (team* adj2 (behaviour or behavior or situation or performance)).tw. |
| 6 | or/1-5 |
| 7 | team* communication.tw,kw. |
| 8 | communication.ti,kw. |
| 9 | communication strateg*.tw,kw. |
| 10 | Communication/ |
| 11 | Verbal Behavior/ |
| 12 | Nonverbal Communication/ or ((nonverbal or non verbal) adj3 (communicat* or strateg* or interaction*)).tw. |
| 13 | (hand signal* or visual signal*).tw,kw. |
| 14 | (team* adj3 training).tw. |
| 15 | checklist/ or (checklist* or check list*).tw,kw. |
| 16 | (script* or whiteboard* or toolkit*).tw,kw. |
| 17 | (prompt or prompts or cue or cues).tw,kw. |
| 18 | (sbar or callout* or call out* or checkback* or check back* or DESC).tw,kw. |
| 19 | (situation and background and assessment and recommendation).tw. |
| 20 | (communication adj3 (closed or loop*)).tw. |
| 21 | "clos* the loop".tw,kw. |
| 22 | "pass the baton".tw,kw. |
| 23 | (crew resource or CRM).tw,kw. |
| 24 | "two challenge rule".tw,kw. |
| 25 | ("speak up" or "speaking up").tw,kw. |
| 26 | or/8-25 |
| 27 | 6 and 26 |
| 28 | aviation/ or Military Personnel/ or Nuclear Power Plants/ |
| 29 | (aviation or aerospace or aeronautic* or cockpit or military or aviator* or pilots or fighter pilot or flight personnel or battlefield* or power plant*).tw,kw. |
| 30 | (high risk adj2 (industr*or environment* or setting*)).tw. |
| 31 | exp Surgical Procedures, Operative/ |
| 32 | Operating Rooms/ |
| 33 | (operating adj2 (room* or theatre*)).tw,kw. |
| 34 | surgical team*.tw,kw. |
| 35 | Intraoperative Period/ or ((perioperative or intraoperative) adj2 (period or setting or environment)).tw. |
| 36 | ((during or undergoing) adj3 surgery).tw. |
| 37 | or/28-36 |
| 38 | 7 or 27 |
| 39 | 37 and 38 |
| 40 | limit 39 to dt=20190615-20220404 |
| Embase | |
| 1 | teamwork/ |
| 2 | team*.ti. |
| 3 | teamwork.tw. |
| 4 | (team member or team members).tw. |
| 5 | (team* adj2 (behaviour or behavior or situation or performance)).tw. |
| 6 | or/1-5 |
| 7 | team* communication.tw. |
| 8 | communication.ti. |
| 9 | interpersonal communication/ |
| 10 | verbal behavior/ or verbal communication/ |
| 11 | nonverbal communication/ or ((nonverbal or non verbal) adj3 (communicat* or strateg* or interaction*)).tw. |
| 12 | communication strateg*.tw,kw. |
| 13 | (team* adj3 training).tw. |
| 14 | checklist/ or checklist*.tw. |
| 15 | (script* or whiteboard* or toolkit*).tw. |
| 16 | (prompt or prompts or cue or cues).tw. |
| 17 | (visual signal* or hand signal*).tw. |
| 18 | (sbar or callout* or call out* or checkback* or check back* or DESC).tw. |
| 19 | (situation and background and assessment and recommendation).tw. |
| 20 | (communication adj3 (closed or loop*)).tw. |
| 21 | "clos* the loop".tw. |
| 22 | "pass the baton".tw. |
| 23 | "two challenge rule".tw. |
| 24 | ("speak up" or "speaking up").tw. |
| 25 | crew resource.tw. |
| 26 | CRM.tw. |
| 27 | or/8-26 |
| 28 | 6 and 27 |
| 29 | 7 or 28 |
| 30 | aviation/ |
| 31 | airplane crew/ |
| 32 | nuclear power plant/ |
| 33 | (aviation or aerospace or aeronautic* or cockpit or military or aviator* or flight personnel or pilots or fighter pilot* or battlefield* or power plant*).tw. |
| 34 | aerospace medicine/ |
| 35 | (high risk adj2 (industr*or environment* or setting*)).tw. |
| 36 | exp *surgery/ |
| 37 | operating room/ |
| 38 | (operating adj2 (room* or theatre*)).tw. |
| 39 | operating room personnel/ |
| 40 | intraoperative period/ or ((perioperative or intraoperative) adj2 (period or setting or environment)).tw. |
| 41 | surgical team.tw. |
| 42 | or/30-41 |
| 43 | 29 and 42 |
| 44 | limit 43 to dc=20190615-20220404 |
| APA PsycInfo | |
| 1 | Teams/ or Work Teams/ |
| 2 | team*.ti. |
| 3 | teamwork.tw. |
| 4 | team member*.tw. |
| 5 | (team* adj2 (behaviour or behavior or situation or performance)).tw. |
| 6 | or/1-5 |
| 7 | team* communication*.tw. |
| 8 | communicat*.ti. |
| 9 | Interpersonal Communication/ or Interpersonal Interaction/ |
| 10 | exp nonverbal communication/ |
| 11 | ((nonverbal or non verbal) adj3 (communicat* or interaction*)).tw. |
| 12 | (visual signal* or hand signal*).tw. |
| 13 | oral communication/ |
| 14 | communication strateg*.tw. |
| 15 | (team* adj3 training).tw. |
| 16 | "CHECKLIST (TESTING)"/ |
| 17 | (checklist* or check list*).tw. |
| 18 | (script* or whiteboard* or toolkit*).tw. |
| 19 | CUES/ |
| 20 | (prompt or prompts or cue or cues).tw. |
| 21 | (sbar or callout* or call out* or checkback* or check back* or DESC).tw. |
| 22 | (situation and background and assessment and recommendation).tw. |
| 23 | (communication adj3 (closed or loop*)).tw. |
| 24 | "clos* the loop".tw. |
| 25 | "pass the baton".tw. |
| 26 | crew resource.tw. |
| 27 | "two challenge rule".tw. |
| 28 | ("speak up" or "speaking up").tw. |
| 29 | or/8-28 |
| 30 | 6 and 29 |
| 31 | 7 or 30 |
| 32 | AVIATION SAFETY/ or AVIATION/ |
| 33 | Aircraft Pilots/ or Air Force Personnel/ or Military Personnel/ or Aerospace Personnel/ |
| 34 | (aviation or aerospace or aeronautic* or cockpit or military or aviator* or flight personnel or pilots or fighter pilot* or battlefield* or power plant*).tw. |
| 35 | (high risk adj2 (industr*or environment* or setting*)).tw. |
| 36 | Surgery/ |
| 37 | (operating adj2 (room* or theatre*)).tw. |
| 38 | surgical team*.tw. |
| 39 | ((during or undergoing) adj3 surgery).tw. |
| 40 | (perioperative or intraoperative).tw. |
| 41 | or/32-40 |
| 42 | 31 and 41 |
| 43 | limit 42 to "0200 book" |
| 44 | 42 not 43 |
| 45 | limit 44 to up=20190615-20220404 |
| ERIC | |
| 1 | Teamwork/ |
| 2 | teamwork.tw. |
| 3 | team member*.tw. |
| 4 | team*.ti. |
| 5 | (team* adj2 (behaviour or behavior or situation or performance)).tw. |
| 6 | or/1-5 |
| 7 | team* communication.tw. |
| 8 | "Communication (Thought Transfer)"/ or Communication Strategies/ |
| 9 | communication strateg*.tw. |
| 10 | team training/ or (team* adj3 training).tw. |
| 11 | Check Lists/ |
| 12 | checklist*.tw. |
| 13 | (script* or whiteboard* or toolkit*).tw. |
| 14 | Scripts/ |
| 15 | (prompt or prompts).tw. |
| 16 | Cues/ or (cue or cues).tw. |
| 17 | (sbar or callout* or call out* or checkback* or check back* or DESC).tw. |
| 18 | Active Learning/ |
| 19 | (situation and background and assessment and recommendation).tw. |
| 20 | (communication adj3 (closed or loop*)).tw. |
| 21 | "clos* the loop".tw. |
| 22 | "pass the baton".tw. |
| 23 | crew resource.tw. |
| 24 | "two challenge rule".tw. |
| 25 | ("speak up" or "speaking up").tw. |
| 26 | CRM.tw. |
| 27 | Nonverbal Communication/ or Verbal Communication/ |
| 28 | ((nonverbal or non verbal) adj3 (communicat* or interaction*)).tw. |
| 29 | or/8-28 |
| 30 | 6 and 29 |
| 31 | 7 or 30 |
| 32 | Flight Training/ |
| 33 | (aviation or aerospace or aeronautic* or cockpit or military or aviator* or pilots of fighter pilot* or flight personnel or battlefield* or power plant*).tw. |
| 34 | Military Personnel/ or Armed Forces/ |
| 35 | (high risk adj2 (industr*or environment* or setting*)).tw. |
| 36 | (operating adj2 (room* or theatre*)).tw. |
| 37 | Surgery/ |
| 38 | surgical team*.tw. |
| 39 | (perioperative or intraoperative).tw. |
| 40 | ((during or undergoing) adj3 surgery).tw. |
| 41 | or/32-40 |
| 42 | 31 and 41 |
| 43 | limit 42 to 04012022 |
| CINAHL | |
| S1 | (MH "Teamwork") |
| S2 | TI teamwork or team member* OR AB teamwork or team member* |
| S3 | TI team* |
| S4 | TI ( (team* N2 (behaviour or behavior or situation or performance)) ) OR AB ( (team* N2 (behaviour or behavior or situation or performance)) ) |
| S5 | S1 OR S2 OR S3 OR S4 |
| S6 | (MH "Communication") OR (MH "Nonverbal Communication+") OR (MH "Verbal Behavior+") |
| S7 | TI communication or ((nonverbal or non verbal) N3 (communicat* or interaction*)) OR AB communication strateg* or ((nonverbal or non verbal) N3 (communicat* or interaction*)) |
| S8 | TI checklist* or ( (hand signal* or visual signal*) ) OR AB checklist* or ( (hand signal* or visual signal*) ) OR SU checklist* |
| S9 | TI ( (script* or whiteboard* or toolkit* or prompt or prompts or cue or cues) ) OR AB ( (script* or whiteboard* or toolkit* or prompt or prompts or cue or cues) ) |
| S10 | TI ( (crew resource) ) OR AB ( (crew resource) ) |
| S11 | TI ( (sbar or callout* or call out* or checkback* or check back* or DESC) ) OR AB ( (sbar or callout* or call out* or checkback* or check back* or DESC) ) |
| S12 | TI ( (situation and background and assessment and recommendation) ) OR AB ( (situation and background and assessment and recommendation) ) |
| S13 | TI ( (communication N3 (closed or loop*)) ) OR AB ( (communication N3 (closed or loop*)) ) |
| S14 | TI "pass the baton" OR AB "pass the baton" |
| S15 | TI "two challenge rule" OR AB "two challenge rule" |
| S16 | TI ( ("speak up" or "speaking up") ) OR AB ( ("speak up" or "speaking up") ) |
| S17 | TI "clos* the loop" OR AB "clos* the loop" |
| S18 | S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 |
| S19 | TI ( (aviation or aerospace or aeronautic* or cockpit or military or aviator* or pilots or fighter pilot or flight personnel or battlefield* or power plant*) ) OR AB ( (aviation or aerospace or aeronautic* or cockpit or military or aviator* or pilots or fighter pilot or flight personnel or battlefield* or power plant*) ) |
| S20 | (MH "Aviation+") |
| S21 | SU military |
| S22 | TI ( (operating N2 (room* or theatre*)) ) OR AB ( (operating N2 (room* or theatre*)) ) |
| S23 | SU operating rooms OR (MH "Intraoperative Period") |
| S24 | TI ( ((perioperative or intraoperative) N2 (period or setting or environment)) ) OR AB ( ((perioperative or intraoperative) N2 (period or setting or environment)) ) |
| S25 | TI surgical team* OR AB surgical team* |
| S26 | TI ( ((during or undergoing) N3 surgery) ) OR AB ( ((during or undergoing) N3 surgery) ) |
| S27 | (MH "Surgery, Operative+") |
| S28 | TI ( (high risk N2 (industr*or environment* or setting*)) ) OR AB ( (high risk N2 (industr*or environment* or setting*)) ) |
| S29 | S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 |
| S30 | TI team* communication OR AB team* communication |
| S31 | S5 AND S18 |
| S32 | S30 OR S31 |
| S33 | S29 AND S32 |
| Cochrane Central Register of Controlled Trials | |
| 1 | ..nlpx "query=MeSH descriptor: [Patient Care Team] this term only","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 2 | ..nlpx "query=(team*):ti","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 3 | ..nlpx "query=(teamwork):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 4 | ..nlpx "query=(team* NEAR/2 (behaviour or behavior or situation or performance))","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 5 | ..nlpx "query=("team member" or "team members"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 6 | 1 or 2 or 3 or 4 or 5 |
| 7 | ..nlpx "query=(team* communication):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 8 | ..nlpx "query=MeSH descriptor: [Communication] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 9 | ..nlpx "query=((nonverbal or non verbal) NEAR/3 (communicat* or interaction*)):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 10 | ..nlpx "query=(communication strateg*):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 11 | ..nlpx "query=((team* NEAR/3 training)):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 12 | ..nlpx "query=MeSH descriptor: [Checklist] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 13 | ..nlpx "query=(checklist*):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 14 | ..nlpx "query=((script* or whiteboard* or toolkit*)):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 15 | ..nlpx "query=((prompt or prompts or cue or cues)):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 16 | ..nlpx "query=("hand signal" or "hand signals" or "verbal signal" or "verbal signals"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 17 | ..nlpx "query=((sbar or callout* or call out* or checkback* or check back* or DESC)):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 18 | ..nlpx "query=((communication NEAR/3 (closed or loop*))):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 19 | ..nlpx "query=("closing the loop"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 20 | ..nlpx "query=("pass the baton"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 21 | ..nlpx "query=("crew resource"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 22 | ..nlpx "query=("two challenge rule"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 23 | ..nlpx "query=("speak up" or "speaking up"):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 24 | 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 |
| 25 | 6 and 24 |
| 26 | 7 or 25 |
| 27 | ..nlpx "query=((aviation or aerospace or aeronautic* or cockpit or military or aviator* or flight personnel or pilots or fighter pilot* or battlefield* or power plant*)):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 28 | ..nlpx "query=MeSH descriptor: [Aviation] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 29 | ..nlpx "query=MeSH descriptor: [Military Personnel] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 30 | ..nlpx "query=MeSH descriptor: [Nuclear Power Plants] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 31 | ..nlpx "query=MeSH descriptor: [Operating Rooms] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 32 | ..nlpx "query=((operating NEAR/2 (room* or theatre*))):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 33 | ..nlpx "query=(high risk industr*):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 34 | ..nlpx "query=MeSH descriptor: [Intraoperative Period] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 35 | ..nlpx "query=(((perioperative or intraoperative) NEAR/2 (period or setting or environment))):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 36 | ..nlpx "query=((during or undergoing) NEAR/3 surgery):ti,ab,kw","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 37 | ..nlpx "query=MeSH descriptor: [Surgical Procedures, Operative] explode all trees","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 38 | ..nlpx "query="surgical team*":ti,ab","desiredResults=10000","minHitsDivisor=7","permitHyponyms=NO","lowestVocabularySearchLevel=none","phrasesBroken=NO","speedWanted=NoHypos","comment=Including Related Terms","elimEnable=NO","constraintMinTerms=2" |
| 39 | 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 |
| 40 | 26 and 39 |
| 41 | limit 40 to yr="2019 - 2022" |
| Scopus | |
| 1 | ( ( ( ( TITLE ( team* ) ) OR ( TITLE-ABS ( team* W/2 ( behaviour OR behavior OR situation OR performance ) ) ) OR ( TITLE-ABS-KEY ( "teamwork" OR "team member*" ) ) ) ) AND ( ( TITLE ( communication ) ) OR ( TITLE-ABS-KEY ( communication AND strateg* ) OR ( TITLE-ABS ( ( nonverbal OR nonverbal ) W/3 ( communicat* OR interaction* ) ) ) OR ( KEY ( "Verbal Behavior" ) ) OR ( TITLE-ABS-KEY ( team* W/3 training ) ) OR ( TITLE-ABS-KEY ( checklist* OR "check list*" ) ) OR ( TITLE-ABS-KEY ( script* OR whiteboard* OR toolkit* ) ) OR ( TITLE-ABS-KEY ( prompt OR prompts OR cue OR cues OR "visual signal*" OR "hand signal" ) ) OR ( TITLE-ABS-KEY ( sbar OR callout* OR "call out*" OR checkback* OR "check back*" OR desc ) ) OR ( title ABS ( situation AND background AND assessment AND recommendation ) ) OR ( TITLE-ABS ( communication W/3 ( closed OR loop* ) ) ) OR ( TITLE-ABS ( "clos* the loop" ) ) OR ( TITLE-ABS ( "pass the baton" ) ) OR ( TITLE-ABS ( "two challenge rule" ) ) OR ( TITLE-ABS ( "speak up" OR "speaking up" ) ) OR ( TITLE-ABS-KEY ( "crew resource" ) ) ) ) OR ( TITLE-ABS-KEY ( "team* communication" ) ) ) AND ( ( TITLE-ABS-KEY ( aviation OR aerospace OR aeronautic* OR cockpit OR military OR aviator* OR pilots OR "fighter pilot" OR "flight personnel" OR battlefield* OR "power plant*" ) ) OR ( TITLE-ABS-KEY ( operating W/2 ( room* OR theatre* ) ) . ) OR ( TITLE-ABS ( "surgical team*" ) ) OR ( TITLE-ABS ( ( during OR undergoing ) W/3 surgery ) ) OR ( TITLE-ABS ( ( perioperative OR intraoperative ) W/2 ( period OR setting OR environment ) ) ) OR ( TITLE-ABS ( "high risk" W/2 ( industr* OR environment* OR setting* ) ) ) ) AND ( LIMIT-TO ( PUBYEAR , 2022 ) OR LIMIT-TO ( PUBYEAR , 2021 ) OR LIMIT-TO ( PUBYEAR , 2020 ) OR LIMIT-TO ( PUBYEAR , 2019 ) ) |
Table 4. List and characteristics of included studies (N=249).
| First author, year | Country | Study design | Sample | Setting | Type of intervention | Name of intervention |
| Askarian et al., 2011 | Iran | Before and after interventional study | 144 surgical cases | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Bartz-Kurycki et al., 2017 | United States | Observational cohort study | 603 surgical cases | Operating room | Bundle/Checklists | Debriefing |
| Bereknyei Merrell et al., 2018 | United States | Case report | 6 healthcare professionals (anesthesia attending, surgical resident, surgical attending, surgical technician, circulating nurse, nurse anesthetist) | Operating room | Bundle/Checklists | Emergency manuals |
| Calland et al., 2011 | United States | Randomized controlled trial | 47 surgical cases, 10 surgical attendings | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Chen et al., 2013 | United States | Literature review | N/A | Operating room | Bundle/Checklists | Cerebral aneurysm checklist |
| Cumin et al., 2017 | New Zealand | Observational cohort study | 120 healthcare professionals (20 teams of 6: consultant surgeon, surgical registrar, anaesthetist, anaesthetic technician, circulating nurse, scrub nurse) | Operating room | Bundle/Checklists | Information probes (briefing notes) |
| Dabholkar et al., 2018 | India | Prospective, non-randomised, comparative study | 37 healthcare professionals (15 surgeons, 14 anaesthetists, 8 nurses) | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| De Muinck Keizer et al., 2017 | Netherlands | Experimental study | 1255 surgical procedures, 33 healthcare professionals (17 surgical residents/attendings,16 radiographers) | Operating room | Protocol | Uniform C-arm communication terminology |
| de Vries et al., 2011 | Netherlands | Retrospective claim record review | 294 surgical malpractice claims | Operating room | Bundle/Checklists | SURgical PAtient Safety System (SURPASS) checklist |
| Dixon et al., 2016 | United States | Observational cohort study | Baseline: 39 healthcare professionals (8 anesthesia providers, 9 circulating nurses, 11 scrub technicians, 11 surgeons) Post-intervention: 42 healthcare professionals (10 anesthesia providers, 14 circulating nurses, 7 scrub technicians, 11 surgeons) | Operating room | Bundle/Checklists | Multimedia (video)-based checklist for time-out |
| Dobbie et al., 2019 | United States | Observational cohort study | 680 preoperative audits | Operating room | Audit & Feedback | Remote Audiovisual Observation |
| El-Shafy et al., 2018 | United States | Observational cohort study | 89 trauma activation videos involving surgical attending or fellow, surgical resident, emergency medicine attending, fellow, or resident | Trauma room | Protocol | Closed Loop Communication |
| Erestam et al., 2017 | Sweden | Before and after interventional study | 150 healthcare professionals (surgeons, anesthesiologists, scrub nurses, nurse anaesthetists, nurse assistants) | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Everett et al., 2017 | Canada | Randomized controlled trial | 56 simulation encounters involving OR teams comprised of a surgeon, anaesthetist, and three nurses | Operating room | Bundle/Checklists | Critical event checklists |
| Fang et al., 2018 | United States | Observational cohort study | 100 healthcare professionals (56 interns, 30 residents, 14 attendings) | Internal medicine | Other | Hands Free Communication Devices (HFCD) |
| Fernandes et al., 2015 | Canada | Case series | 4 surgical cases | Operating room | Protocol | Transcatheter aortic valve implantation (TAVI) protocol |
| Freundlich et al., 2015 | United States | Observational cohort study | 166 time-outs involving anesthesia team, surgeons, nurses, scrub technicians | Operating room | Audit & Feedback | Time-out |
| Gillespie et al., 2010 | Australia | Qualitative interview study | 16 healthcare professionals (4 physicians, 3 nurse managers, 9 nurses) | Operating room | Bundle/Checklists | Time-out |
| Goff et al., 2018 | United States | Observational cohort study | 115 healthcare professionals (50 surgical attendings, 65 surgical residents) | Operating room | Protocol | Navigational Grid |
| Henrickson et al., 2009 | United States | Observational cohort study | 56 healthcare professionals (surgical assistants, surgical technicians, circulating nurses, perfusionists, nurse anesthetists) | Operating room | Protocol | Preoperative Briefing Protocol for Cardiovascular Surgery |
| Hicks et al., 2014 | United States | Review | N/A | Operating room | Bundle/Checklists | Operating room briefings |
| Hunter et al., 2017 | United States | Observational cohort study | 23 surgical cases involving circulating nurses, surgical technicians, surgical assistants, anesthesia team members | Operating room | Protocol | SBAR tool |
| Julia et al., 2017 | France | Interventional cohort study | 204 anesthesia handovers involving residents and nurse anesthetists | Operating room | Bundle/Checklists | Intraoperative handover training and checklist |
| Kearns et al., 2011 | United Kingdom | Observational cohort study | 53 healthcare professionals (17 midwives, 8 auxiliaries, 8 obstetric trainees, 8 anaesthetic trainees, 5 anaesthetic nurses, 4 anaesthetic consultants, 3 consultant obstetricians) | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Kozusko et al., 2016 | United States | Observational cohort study | 4,453 surgical cases involving a surgeon, anesthesia care provider, circulating nurse, preoperative nurse, and relief nurse | Operating room | Bundle/Checklists | Surgical time-out patient-focused model |
| Lingard et al., 2008 | Canada | Observational cohort study | 128 health care professionals (11 general surgeons, 24 surgical trainees, 41 operating room nurses, 28 anesthesiologists, 24 anesthesia trainees) | Operating room | Bundle/Checklists | Checklist and Briefing |
| Lingard et al., 2011 | Canada | Retrospective preintervention/postintervention study | 340 surgical cases, 243 healthcare professionals (11 surgeons, 48 surgical residents and fellows, 87 operating room nurses, 3 nursing trainees, 60 staff anesthesiologists, 26 anesthesia residents and fellows, 3 respiratory therapists, 5 technical assistants) | Operating room | Bundle/Checklists | Preoperative team checklist |
| Lingard et al., 2005 | Canada | Observational cohort study | 22 surgical cases, 33 healthcare professionals (8 surgeons, 8 staff anesthesiologists, 4 anesthesia residents, 3 surgical residents, 10 nurses) | Operating room | Bundle/Checklists | Preoperative team briefing |
| Low et al., 2013 | United States | Cross-sectional study | 29 healthcare professionals | Operating room | Bundle/Checklists | Flow checklist |
| MacDougall-Davis et al., 2016 | United Kingdom | Observational cohort study | 32 healthcare professionals (8 teams of 4 anaesthetic trainees and "go-betweens") | Operating room | Protocol | Traffic Lights tool |
| Mainthia et al., 2012 | United States | Observational cohort study | 240 surgical cases involving surgical and anesthesia residents, fellows, and attendings; registered nurse anesthetists, scrub nurses, circulating nurses; OR technicians | Operating room | Bundle/Checklists | Electronic Whiteboard Checklist |
| Makary et al., 2006 | United States | Review | N/A | Operating room | Bundle/Checklists | OR Briefing |
| Marshall et al., 2016 | Australia | Randomized controlled trial | 72 healthcare professionals (24 teams of 3, consisting of a consultant anesthetist, an anesthetic trainee and anesthetic assistant) | Operating room | Clinical Practice Guideline | Guidelines for the management of peri-operative severe allergic reactions |
| Masiglat et al., 2016 | United States | Short Report | N/A | Operating room | Bundle/Checklists | Wilmer Hand-off Communication Tool |
| McFerran et al., 2005 | United States | Short Report | N/A | Perinatal care | Bundle/Checklists | Perinatal Patient Safety Project |
| Norton et al., 2010 | United States | Short Report | N/A | Operating room | Bundle/Checklists | Pediatric Surgical Safety Checklist |
| O'Connor et al., 2013 | Ireland | Cross-sectional study | 107 healthcare professionals (41 surgeons, 33 anaesthetists, 33 nurses) | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Overdyk et al., 2016 | United States | Cluster randomized controlled trial | 2,693 surgical cases involving surgeons, anesthesia providers, nurses, support staff | Operating room | Audit & Feedback | Remote video auditing (RVA) |
| Papaconstantinou et al., 2013 | United States | Cross-sectional study | 437 healthcare professionals (153 nurses, 104 anesthesia providers, 180 surgeons) | Operating room | Protocol | Surgical Safety Checklist |
| Papaspyros et al., 2010 | United Kingdom | Retrospective case review | 118 surgical cases, 15 healthcare professionals (anaesthetists, perfusionists, scrub nurses, technicians) | Operating room | Bundle/Checklists | Briefing and debriefing checklist |
| Pian-Smith et al., 2009 | United States | Observational cohort study | 40 anesthesia trainees | Operating room | Bundle/Checklists | Two-challenge rule |
| Pickering et al., 2013 | United Kingdom | Observational cohort study | 26 surgical cases | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Pulido et al., 2017 | United States | Randomized controlled trial | 17 surgeons | Operating room | Protocol | Surgeon's verbal intervention |
| Ragusa et al., 2016 | United States | Review | N/A | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Randmaa et al., 2014 | Sweden | Randomized controlled trial | 169 healthcare professionals (practical nurses, registered nurses, physicians) | Operating room, intensive care unit, post-anesthesia care unit | Protocol | SBAR tool |
| Rhee et al., 2017 | United States | Observational cohort study | 1,610 surgical time- outs and debriefs | Operating room | Bundle/Checklists | TeamSTEPPS |
| Santana et al., 2016 | Brazil | Cross-sectional study | 472 health professionals (surgeons, anesthesiologists, surgical technologists, nurses, nursing technicians and nursing assistants, resident physicians, medical and nursing students, heads of medical and nursing services) | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Schwendimann et al., 2019 | Switzerland | Observational cohort study | 104 on-site observations, 11 healthcare professionals (6 surgeons and anaesthesiologists, 5 operating room nurses and nurse anaesthetists) | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Webster et al., 2006 | United States | Randomized controlled trial | 36 healthcare professionals | Operating room | Protocol | Scripted/Automatic Speech Communication |
| Weingessel et al., 2017 | Austria | Observational cohort study | 18,081 surgical procedures | Operating room | Bundle/Checklists | Time-out |
| West et al., 2012 | United States | Observational cohort study | 47 healthcare professionals (26 registered nurses, 12 licensed vocational nurses, 9 nurse anesthetists) | Cardiac medicine unit | Protocol | Sterile Cockpit Rule |
| Wright et al., 2016 | United States | Observational cohort study | 30 surgical cases | Operating room | Education | Educational noise reduction intervention (No interruption zones) |
| Zeeni et al., 2014 | United States | Observational cohort study | 548 surgical patients | Operating room | Protocol | High Risk Spine Protocol |
| Faiz et al., 2019 | Pakistan | Before and after interventional study | 60 patient transfers | Intensive Care Unit | Bundle/Checklists | Standardized patient handover process |
| Carpini et al., 2020 | Australia | Cross-sectional study | 46 registered nurses from short-stay surgical units | Pre-operative | Protocol | Multidisciplinary team briefings (MDTB) |
| Tankimovich et al., 2020 | United States | Pilot study | 20 participants (trainees) | Outpatient setting | Education | Interprofessional education (IPE) and teamwork (TW) simulation exercise using TeamSTEPPS Pocket Guide |
| Roig et al., 2020 | Argentina | Before and after interventional study | 158 pre-intervention and 124 post-intervention handoff assessments | Pediatric unit | Education | I-PASS |
| Wunder et al., 2020 | United States | Quantitative, descriptive study | 34 student registered nurse anesthetists | Operating room | Education | Operating Room Fire Simulation using Magic Leap OneTM augmented reality headsets |
| Staines et al., 2020 | Switzerland | Pre-and-post observational study | 90 completed questionnaires | Maternity ward | Education | TeamSTEPPS teamwork improvement concept |
| Loesche et al., 2020 | United States | Pre-and-post observational study | 19 participants | Instrument-processing department | Protocol | Daily huddles |
| DeBrún et al., 2020 | Ireland | Cross-sectional study | Four heterogeneous healthcare teams | Heterogeneous healthcare teams, ranging in size from small cross-organisational teams to large unit-based teams in large urban teaching hospitals | Education | The Collective Leadership for Safety Cultures (Co-Lead) programme |
| Valdes et al., 2021 | United States | Before and after interventional study | 10 nursing students | Escape Room | Education | Escape Room Simulation |
| Tervajärvi et al., 2021 | Finland | Prospective, non-randomised, comparative study | 21 participants (trainees) | Emergency Department | Education | Student-LED interprofessional sequential simulation |
| Raîche et al., 2021 | Canada | Prospective observational study | 22 simulation cases | Operating room | Education | In situ simulation sessions |
| Rojo‐rojo et al., 2021 | Spain | Mixed pilot study (qualitative/quantitative) with three phases and a pre-post intragroup quasi-experimental study | 12 simulation participants | Intensive Care Unit; Emergency Department | Education | High Fidelity Simulation |
| Lee et al., 2021 | United States | Prospective pre-post cohort study | 104 surgical staff members | Operating room | Education | Four reinforcement activities |
| Ulmer et al., 2022 | Switzerland | Pre-and-post observational study | 15 nurses | Intensive Care Unit | Education | In situ simulation team training focused on communication |
| Undre et al., 2007 | UK | Cross-sectional study | 50 urology procedures | Operating room | Audit & Feedback | Observational Teamwork Assessment for Surgery (OTAS) |
| Bethune et al., 2011 | UK | Before and after interventional study | 100 questionnaires completed by all OR team members | Operating room | Protocol | Briefings and debriefings |
| Whyte et al., 2008 | Canada | Prospective, non-randomised, comparative study | 302 preoperative team briefings | Operating room | Bundle/Checklists | Preoperative team briefing |
| Marzano et al., 2016 | United States | Pre-and-post observational study | 12 simulation sessions | Operating room | Protocol | Birth Center Pager (BCP) |
| Størkson et al., 2016 | Norway | Cross-sectional study | 268 (54% of total 501 completed forms) | Operating room; Trauma room; Internal medicine; Perinatal care; Intensive Care Unit; Post-anesthesia care unit; Cardiac medicine unit | Audit & Feedback | Care Process Self-Evaluation Tool (CPSET) |
| Kvarnström et al., 2018 | Sweden | Qualitative ethnographic study | 89 health professionals | Surgical ward | Protocol | Introduction of NPs into surgical ward teams |
| Funk et al., 2016 | United States | Pre-and-post observational study | Samples of 52 pre-implementation and 51 post-implementation handover interaction | Post-anesthesia care unit | Protocol | Introductions, Situation,Background, Assessment, Recommendations, and Questions (ISBARQ) checklist |
| Collazos et al., 2013 | Colombia | Cross-sectional study | A total of 246 patients were surveyed during February andMarch 2011, 29% females and 71% males. The mean age was48.5 years; the age range was between 18 and 88 years | Operating room; Post-anesthesia care unit | Bundle/Checklists | WHO's surgical checklist |
| Reed et al., 2016 | UK | Prospective, non-randomised, comparative study | 92 procedures | Operating room | Bundle/Checklists | Audio delivery of the Surgical Safety Checklist (SSC) |
| Vyas et al., 2013 | United States | Before and after interventional study | N/A | Operating room | Protocol | Global Smile Foundation Emergency Response Protocol |
| Yamada et al., 2015 | United States | Prospective, randomised, comparative study | 13 simulation scenarios | Perinatal care | Education | Standardized Communication Techniques |
| Yule et al., 2015 | United States | Randomised controlled trial | 16 surgical residents | Operating room | Education | Non-Technical Skills for Surgeons (NOTSS) behavior observation system coaching |
| Skelton et al., 2016 | Rwanda | Before and after interventional study | 20 participants | Operating room | Education | Anesthetists’ Non-technical Skills (ANTS) training using low-cost high psychological fidelity simulation with debriefing |
| Flin et al., 2004 | UK | Prospective, non-randomised, comparative study | 8 simulated cases (number of participants not specified) | Operating room | Education | Crisis Avoidance Resource Management for Anaesthetists (CARM-A) |
| Sudikoff et al., 2009 | United States | Randomised crossover trial | 16 residents | Operating room | Education | High-fidelity medical simulation |
| Weaver et al., 2010 | United States | Before and after interventional study | N/A | Operating room | Education | TeamSTEPPS Training Program |
| Ostermann et al., 2010 | Germany | Before and after interventional study | 121 participants (77 staff members and 44 patients’ relatives) | Integrative hospital for neurological rehabilitation | Education | Team-building process consisted of didactic instruction and training in problem-solving, teambuilding and constructive conflict resolution. |
| Capella et al., 2010 | United States | Before and after interventional study | A convenience sample (n=33) trauma resuscitations before training, and (n=40) post training | Trauma room | Education | TeamSTEPPS training, augmented by simulation |
| Sculli et al., 2012 | United States | Training design | N/A | Operating room; Internal medicine | Education | Clinical Crew Resource Management (CCRM) |
| Johnson et al., 2012 | United States | Before and after interventional study | 809 participants | Operating room | Education | Perioperative Teamwork Education Program (Safety training program focusing on Crew Resource Management, TeamSTEPPS, and communication techniques) |
| Willaert et al., 2012 | Belgium | Prospective, observational study | 18 cases | Operating room | Education | Patient-specific virtual reality rehearsal |
| Wheeler et al., 2013 | United States | Non-randomised experimental study | 112 simulations | Internal medicine | Education | Simulations |
| Kilday et al., 2013 | United States | Pre-and-post observational study | 29 neonatal rapid response team members participated | NICU | Education | Combined team training program (combining evidence-based education, team concepts and simulation training) |
| Abdelshehid et al., 2013 | United States | Pre-and-post observational study | Nine urology residents, 7 anesthesia residents, and 2 CRNA participated in the 9-study scenario presentation | Operating room | Education | Simulation-based team training (SBTT) |
| Farra et al., 2014 | United States | Prospective, non-randomised, comparative study | 18 nursing students | A midsize public university | Education | Disaster Triage Virtual Reality Simulation |
| Perkins et al., 2015 | United States | Prospective, non-randomized comparative study | 22 surgical technicians and operating room nurses | Operating room | Education | American College of Surgeons’ Advanced Trauma Operative Management (ATOM) course |
| Arora et al., 2015 | UK | Before and after interventional study | 185 residents from 5 hospitals | Surgical wards | Education | Simulation-based training |
| Lisbon et al., 2016 | United States | Pre-and-post observational study | 113 members of an academic emergency department | Emergency Department | Education | TeamSTEPPS educational strategy |
| Hoang et al., 2016 | United States | Before and after interventional study | 55 participants (11 teams) | Operating room | Education | Shipboard Surgical Trauma Training Course (S2T2C) |
| James et al., 2016 | United States | Observational case study and questionnaire of participants in a cross-sectional analysis | 23 learners | Haematology-oncology unit | Education | Simulation-based team training scenarios |
| Xu et al., 2016 | France | Prospective, non-randomised, comparative study | 28 participants | Operating room | Education | Xperience™ Team Trainer (XTT) |
| Chalwin et al., 2016 | Australia | Cross-sectional study | 96 participants | Conference (ANZICS: The Deteriorating Patient Conference) | Education | ANZICS RRT Training Program |
| Savage et al., 2017 | Sweden | Case study | 153 managers and staff | Operating room | Protocol | Crew Resource Management (CRM) safety program |
| Clapper et al., 2018 | United States | Quantitative pre-test and post-test study | 109 participants (16 groups) | Internal medicine unit | Education | Code team course |
| Chamberland et al., 2018 | Canada | Randomised controlled trial | 60 health‐care professionals | Intensive Care Unit | Audit & Feedback | simulation‐based learning - debriefing content |
| Bian et al., 2019 | Netherlands | Concept study | N/A | Operating room | Environment improvement | Automatic Integration of Medical Information (AIMI) |
| Fukushima et al., 2018 | Japan | Randomized, controlled, prospective pilot study | 33 medical students | Simulation Center | Education | Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) program |
| Adams et al., 2004 | United States | Prospective, non-randomised, comparative study | 96 surgical cases | Operating room | Education | Six Sigma |
| McKoin et al., 2010 | United States | Pre-and-post observational study | 530 surgical staff members | Operating room | Education | Crew Resource Management (CRM) Team Training |
| Catchpole et al., 2010 | UK | Prospective, non-randomised, comparative study | 112 operations (51 before and 61 after intervention) | Operating room | Education | Aviation-style team training (+Theatre Aide Memoir) |
| Spence et al., 2011 | Canada | Cross-sectional study | 130 students visiting 65 Operating rooms | Operating room | Audit & Feedback | Student-observed surgical safety practices + WHO surgical checklist |
| Mayer et al., 2011 | United States | Pre-and-post observational study | 12 attendings, 157 nursing staff, and 90 respiratory therapists participated. | Intensive Care Unit; Post-anesthesia care unit | Education | TeamSTEPPS |
| Sculli et al., 2011 | United States | Short Report | 54025 employees (147 locations) | Veterans Health Administration | Audit & Feedback | National Center for Patient Safety (NCPS) patient safety culture survey |
| Paull et al., 2013 | United States | Pre-and-post observational study | 334 perioperative surgical staff | Operating room; Intensive Care Unit | Education | point-of-care simulation-based team training curriculum |
| Harvey et al., 2013 | United States | Prospective, non-randomised, comparative study | N/A | Trauma room | Education | TeamSTEPPS simulation-based training |
| Fernandez et al., 2013 | United States | Randomized comparison trial | 231 participants (medical students and residents) | Emergency Room | Education | Computer-based teamwork process training intervention |
| Howe et al., 2014 | United States | Before and after interventional study | 15 staff members | Long-term care facility | Bundle/Checklists | TeamSTEPPS Long-Term Care (LTC) Team Talk |
| Braham et al., 2014 | UK | Before and after interventional study | 54 cases total. 20 cases (pre, old checklist) vs 34 cases (post, modified checklist) | Operating room | Bundle/Checklists | A modified World Health Organization (WHO) Safety Checklist |
| Tibbs et al., 2014 | United States | Pre-and-post observational study | 18 surgical team members | Operating room | Bundle/Checklists | Team Strategies & Tools to Enhance Performance and Patient Safety (TeamSTEPPS) |
| Korkiakangas et al., 2015 | UK | Non-randomised experimental study | Two scenarios | Operating room | Education | Video-Supported Simulation for Interactions in the Operating Theatre (ViSIOT) |
| Copeland et al., 2016 | United States | Before and after interventional study | Forty-six (27 females, 19 males) of the 155 staff members (30%) responded to the pre-implementation survey: 32 RNs, 10 MDs/DOs, two psychiatric assessors, one PA, and one critical care technician (CCT). Thirty-seven (24 females, 13 males) of the 192 staff members (19%) responded to the mid-implementation survey: 26 RNs, seven MDs/DOs, two CCTs, and two unit secretaries. Thirty-three (21 females, 12 males) of the 173 staff members (19%) responded to the post-implementation survey: 25 RNs, four MD/DOs, three unit secretaries, and one CCT. | Trauma room (Emergency department) | Protocol | Post-Code Pause |
| Yang et al., 2016 | China | Before and after interventional study | 168 Handovers [Nurses (n=77), resident physicians (n=20), intensive care specialists (n=10) and respiratory therapists (n=2) of the ICU as well as all neurosurgeons(n=34) and anaesthetists (n=13)] | Intensive Care Unit | Protocol | Handover protocol |
| Parush et al., 2017 | Canada | Pre-and-post observational study | 13 | Trauma room | Technological Cognitive Aid | Situation Display |
| Finch et al., 2019 | United States | Before and after interventional study | 32 OR rooms (exact number not collected) | Operating room | Education | Coaches for improving SSC debriefing |
| Small et al., 1999 | United States | Non-randomised experimental study | 15 patient scenario concepts, 15 participants | Emergency Room | Education | High-fidelity Simulation Team Training Course for Emergency Medicine |
| Morey et al., 2002 | United States | Pre-and-post observational study | 1058 physicians, nurses, and technicians (374 control group, 684 experimental group) | Emergency Department | Education | EmergencyTeam Coordination Course (ETCC) |
| Blum et al., 2005 | United States | Cross-sectional study | 22 pilot teams | Operating room | Audit & Feedback | Anesthesia Crisis Resource Management (ACRM) |
| Leming-Lee et al., 2005 | United States | Prospective, non-randomised, comparative study | 737 providers were trained and provided feedback | Operating room | Education | Crew Resource Management (CRM) |
| Awad et al., 2005 | United States | Pre-and-post observational study | N/A | Operating room | Education | Medical Team Training (MTT) |
| Undre et al., 2007 | UK | Prospective, non-randomised, comparative study | 80 participants (20 teams) | Operating room | Education | Multidisciplinary Crisis Simulations |
| Catchpole et al., 2007 | UK | Pre-and-post observational study | 48 surgical cases | Operating room | Audit & Feedback | Direct observation |
| Flin et al., 2007 | UK | Cross-sectional study | 18 surgeons returned the evaluation form | Operating room | Education | Non-Technical Skills for Surgeons (NOTSS) training course |
| Sax et al., 2009 | United States | Prospective, non-randomised, comparative study | 857 participants | Operating room | Education | Crew resource management training intervention |
| Willaert et al., 2010 | UK | Before and after interventional study | One surgical case (one patient) | Simulation centre | Education | Patient-specific virtual reality simulation |
| Neily et al., 2010 | United States | Descriptive analysis | 32 facilities | Operating room | Education | Learning session |
| Gore et al., 2010 | United States | Before and after interventional study | 600 surveys | Operating room | Education | Crew Resource Management (CRM) training |
| Wolf et al., 2010 | United States | Prospective, non-randomised, comparative study | 4,863 cases | Operating room | Education | Medical Team Training (MTT) |
| Polack et al., 2010 | United States | Prospective, non-randomised, comparative study | 149 trauma personnel | Trauma room | Education | Communication curriculum |
| Joy et al., 2011 | United States | Prospective, interventional study | 79 patient handovers | Operating room; Intensive Care Unit | Protocol | Standardized handover protocol |
| Steinemann et al., 2011 | United States | Before and after interventional study | 137 multidisciplinary trauma team members | Trauma room | Education | In situ, multidisciplinary, simulation-based teamwork training |
| Deering et al., 2011 | United States | Before and after interventional study | 153 patient safety reports submitted (94 before implementation, 59 after implementation) | Operating room; Trauma room | Education | TeamSTEPPS |
| Suva et al., 2012 | Switzerland | Prospective, non-randomised, comparative study | 99 participants | Operating room | Education | Crew Resource Management (CRM) program |
| Hoang et al., 2013 | United States | Prospective, non-randomised, comparative study | N/A | Trauma room | Education | Deployment Fleet Surgical Team Training |
| Böhmer et al., 2013 | Germany | Pre-and-post observational study | A survey of 99 co-workers | Operating room; Trauma room | Bundle/Checklists | "Safety checklist", an adaptation of 'safe surgery checklist’ of the WHO |
| Passauer-Baierl et al., 2014 | Germany | Prospective, non-randomised, comparative study | 11 surgical cases | Operating room | Audit & Feedback | Observational Teamwork Assessment for Surgery Tool (OTAS-D) |
| Kellicut et al., 2014 | US study (but took place in Iraq) | Before and after interventional study | 220 personnel completed the training, of which 61 completed the survey. | Operating room; Trauma room | Education | Surgical Team Assessment Training (STAT) |
| Fouilloux et al., 2014 | France | Prospective, non-randomised, comparative study | 4 participants (1 team) | Operating room | Education | Team training in management of adverse acute events occurring during cardiopulmonary bypass procedure |
| Hughes et al., 2014 | United States | Before and after interventional study | 160 personnel (132 surveys and 38 observations post) | Trauma room | Protocol | Crew Ressource Management (CRM) |
| Morgan et al., 2015 | UK | Controlled interrupted time series study | 2,221 patients and 94 surgical cases (1,121 patients before intervention and 1,100 after intervention; 44 operations observed before and 50 after) | Operating room | Education | Teamwork training (SOP and CRM-style team training) |
| Phitayakorn et al., 2015 | United States | Prospective, non-randomised, comparative study | 5 intraoperative teams | Operating room | Simulation | Anesthesiologists’ Non-Technical Skills (ANTS), Scrub Practitioners List of Intra-operative Non-Technical Skills (SPLINTS), Non-Technical Skills for Surgeons (NOTSS), Objective Teamwork Assessment System (OTAS), and an evidence-based MH checklist. |
| Nakarada-Kordic et al., 2016 | New Zealand | Prospective, non-randomised, comparative study | 20 complete OR teams (comprising 120 healthcare professionals in total) | Operating room | Cognitive aid | Computer-based card sorting tool (Momento) |
| Norton et al., 2016 | United States | Before and after interventional study | 196 multidisciplinary operating room clinicians responded to the survey | Operating room | Bundle/Checklists | Pediatric Surgical Safety Checklist |
| Stephens et al., 2016 | UK | Prospective, non-randomised, comparative study | 130 staff | Operating room | Education | Interprofessional training course in crises and human factors |
| Weller et al., 2016 | New Zealand | Before and after interventional study | 437 general surgical cases (224 cases before and 213 cases after MORSim) | Operating room | Education | Multidisciplinary Operating Room Simulation (MORSim) |
| Rao et al., 2016 | United States | Prospective cohort study with pretesting or posttesting | 15 postgraduate year 1 general surgery residents | Operating room | Education | Team-based tasks designed to teach communication and teamwork |
| Henderson et al., 2016 | United States | Pre-and-post observational study | 68 nurses | Operating room; Intensive Care Unit; Post-anesthesia care unit | Protocol | Pop-form (postoperative communication system) |
| Earle et al., 2017 | United States | Pre-and-post observational study | N/A | Operating room | Protocol | Circulate, Scrub and Technical AssistanceTeam (C-STAT) |
| Stewart-Parker et al., 2017 | UK | Before and after interventional study | 68 healthcare professionals | Operating room | Education | S-TEAMS Course |
| Khademian et al., 2018 | Iran | Quasi-Experimental | 60 students (45 anesthesia and 15 operating room nursing students) | Operating room | Education | Teamwork Training Workshop |
| Caskey et al., 2017 | United States | Pre-and-post observational study | 9 surgical cases (9 PGY-1 residents) | Operating room | Education | Laparoscopic team-based task training for nontechnical skills |
| Rao et al., 2017 | United States | Prospective, non-randomised, comparative study | 53 participants | Operating room | Education | Phase 3 team-based skills curriculum for general surgery residents |
| Malenka et al., 2018 | United States | Before and after interventional study | 52 handoffs (29 preintervention, 23 postintervention) | Operating room; Intensive Care Unit; Pediatric Intensive Care Unit (PICU) | Protocol | Standardized handoff protocol (including a checklist) |
| Kinoshita et al., 2009 | Japan | Prospective, non-randomised, comparative study | 80 participants (47 surgeons and 33 nurses) | Operating room | Education | LADG Basic Lab Course |
| Zattoni et al., 2017 | Italy | Prospective, non-randomised, comparative study | 20 simulated emergencies | Operating room | Education and checklist | Surgical team safety training program and institutional checklist |
| Defontes et al., 2004 | United States | Prospective, non-randomised, comparative study | N/A | Operating room | Bundle/Checklists | Preoperative Safety Briefing |
| Guerlain et al., 2005 | United States | Prospective, non-randomised, comparative study | 10 surgical cases | Operating room | Audit & Feedback | RATE tool (multitrack, synchronized, digital audio-visual recording system) |
| Dunn et al., 2007 | United States | Before and after interventional study | N/A | Operating room; Intensive Care Unit; Post-anesthesia care unit | Education | Medical Team Training (MTT) program |
| Marshall et al., 2007 | United States | Prospective, non-randomised, comparative study | No specific number provided | Surgical facilities | Education | Human factors program based on Crew Resource Management training |
| Gururaja et al., 2008 | United States | Prospective, non-randomised, comparative study | 10 training session videos | Operating room | Education | Debriefing at the Point of Care in Simulation-Based Operating Room Team Training |
| Edel et al., 2010 | United States | Pre-and-post observational study | N/A | Operating room | Bundle/Checklists | Pre-operative Time out/count board |
| Sewell et al., 2011 | UK | Prospective, non-randomised, comparative study | 965 surgical cases (480 patients before and 485 patients after the intervention) | Operating room | Education | Educational program (no real name) |
| Haynes et al., 2011 | United States | Pre- and post-intervention survey | 257 clinicians actively working in the designated study operating rooms at the eight hospitals participating in a trial of a WHO surgical safety checklist | Operating room | Bundle/Checklists | WHO Surgical Safety Checklist |
| Forse et al., 2011 | United States | Prospective, non-randomised, comparative study | N/A | Operating room | Education | TeamSTEPPS program |
| Young-Xu et al., 2011 | United States | Retrospective health services study | 119 383 sampled procedures from 74 Veterans Health Administration facilities that provide care to veterans | Operating room | Education | Veterans Health Administration Medical Team Training (MTT) program |
| Lee et al., 2012 | New Zealand | Before and after interventional study | 35,416 procedures; (Phase 1, 10330 procedures) vs (Phase 2, 25086 procedures) | Operating room | Bundle/Checklists | Time Out Procedure (TOP) |
| Fargen et al., 2013 | United States | Before and after interventional study | 71 procedures before checklist implementation and 60 procedures after checklist implementation | Operating room | Bundle/Checklists | Neurointerventional-specific WHO surgical checklist |
| Kawano et al., 2014 | Japan | Before and after interventional study | 339 responders (177 pre- and 162 post-intervention) | Operating room | Bundle/Checklists | Surgical Safety Checklist (SSCL) |
| Porter et al., 2014 | United States | Before and after interventional study | 31 cases | Operating room | Bundle/Checklists | Preprocedural pause (PPP) |
| Cullati et al., 2014 | Switzerland | Cross-sectional study | 152 respondents | Operating room | Bundle/Checklists | Surgical Safety Checklist (SSC) |
| Hsu et al., 2014 | Taiwan | Prospective, non-randomised, comparative study | 34 staff members | Operating room | Education | Team Resource Management (TRM) Program |
| Russ et al., 2015 | UK | Longitudinal interview study | 119 interviews with operating room personnel | Operating room | Bundle/Checklists | World Health Organization (WHO) Surgical Safety Checklist |
| Hawranek et al., 2015 | Poland | Pre-and-post observational study | 2,064 cases (1,011 cases pre, 1,053 cases post) | Catheterisation laboratory | Bundle/Checklists | Periprocedural checklist |
| Hill et al., 2015 | UK | Before and after interventional study | 113 surgical cases (60 cases at baseline and 53 cases one year later) | Operating room | Bundle/Checklists | The 5 Steps to Safer Surgery (5SSS) |
| Hsu et al., 2016 | United States | Before and after interventional study | 103 ICUs | Intensive Care Unit | Education | Comprehensive Unit-based Safety Program (CUSP) |
| Ong et al., 2015 | New Zealand | Pre-and-post observational study | 111 operations | Operating room | Bundle/Checklists | "checklist"; adaptation of "WHO Surgical Safety Checklist" |
| True et al., 2016 | United States | Before and after interventional study | 108 providers (nursing and medical) in 36 births (18 births per facility) | Perinatal care | Bundle/Checklists | Vaginal Delivery Safety (VaDS) checklist |
| Chan et al., 2016 | China | Cross-sectional study | 55 individuals in the departments of Obstetrics and Gynaecology, Anaesthesiology and Operating Theatre Services, Intensive Care Unit and Accident and Emergency | Operating room; Trauma room; Intensive Care Unit | Education | Simulation training using crew resource management |
| Molina et al., 2016 | United States | Before and after interventional study | 929 at baseline and 815 at follow-up across 13 hospitals | Operating room | Bundle/Checklists | Surgical Safety Checklist (SSC) |
| Sucupira et al., 2016 | Brazil | Prospective, non-randomized, comparative study | The tool was applied to 486 patients | Operating room | Bundle/Checklists | safety checklist in aesthetic plastic surgery |
| Riley et al., 2016 | United States | Prospective, non-randomised, comparative study | 342,754 deliveries | Perinatal care | Audit & Feedback | Premier Perinatal Safety Initiative (PPSI) |
| New et al., 2016 | United States | Before and after interventional study | 1120 surgical cases | Operating room | Education | Lean Participative Process Improvement |
| Riley et al., 2017 | United States | Before and after interventional study | 26 bed pediatric cardiac ICU | Intensive Care Unit; Cardiac medicine unit | Bundle/Checklists | OR to CICU Handoff |
| Egenberg et al., 2017 | Tanzania | Before and after interventional study | 3308 patients | Perinatal care | Education | Scenario-based PPH training |
| Gillespie et al., 2017 | Australia | Pre-and-post observational study | 179 surgeries (99 before, 80 after) | Operating room | Education | TEAMANATOMY (brief team training program) |
| Kuy et al., 2017 | United States | Prospective, non-randomised, comparative study | All surgical service staff (88 employees in the surgical service) | Operating room; Perioperative care areas | Education | Crew Resource Management (CRM) training |
| Leong et al., 2017 | Netherlands | Prospective, non-randomised, comparative study | 5 surgical teams | Operating room | Bundle/Checklists | Perioperative briefing and debriefing |
| Gillespie et al., 2017 | Australia | Before and after interventional study | 520 individual cases (292 pretest, 228 posttest) | Operating room | Education | TEAMANATOMY, a team training program |
| Lee et al., 2017 | United States | Prospective pre-post cohort study | 24 surgical cases | Operating room | Education | TeamSTEPPS principles training |
| Sharma et al., 2018 | United States | Non-randomised experimental study | 50 cases | Operating room | Protocol | The Whiteboard Technique |
| Mukhopadhyay et al., 2018 | United States | Prospective, non-randomised, comparative study | 124 caregivers representing surgery (n=49), anesthesia (n=31) and ICU nursing (n=44) | Operating room; Intensive Care Unit | Bundle/Checklists | The Perioperative Hand Off Protocol |
| Krimminger et al., 2018 | United States | Prospective, non-randomised, comparative study | 38 cardiothoracic patients | Intensive Care Unit | Protocol | Standardized handover process and communication template between the OR and the ICU. |
| Friend et al., 2018 | United States | Before and after interventional study | 500 video-assisted thoracoscopic surgeries (VATS) | Operating room | Protocol | VATS Kit |
| Fleetwood et al., 2018 | United States | Pre-and-post observational study | 4 participants | Simulated Operating Room (SOR) | Simulation | Communication skills training through simulation |
| Kherad et al., 2018 | Canada | Before and after interventional study | 2,458 colonoscopies (1,317 colonoscopies at baseline and 1,141 colonoscopies during the intervention period) | Endoscopy unit | Bundle/Checklists | Endoscopy checklist before colonoscopy |
| Gardezi et al., 2009 | Canada | Retrospective claim review | Over 700 surgical procedures | Operating room | Bundle/Checklists | Structured checklist |
| Seamons et al., 2017 | United States | Prospective, non-randomised, comparative study | 56 employees | Ophthalmological surgical department | Audit & Feedback | Technology change |
| Valerio et al., 2017 | United States | Pre-and-post observational study | 219 participants | Operating room | Bundle/Checklists | Standardized Surgical Checklist (SSC) |
| Dommaraju et al., 2019 | United States | Retrospective study | 100 CT-guided procedures | Operating room | Bundle/Checklists | Pre-procedure timeouts |
| Ravindran et al., 2020 | UK | Prospective, non-randomised, comparative study | N/A | Endoscopy units | Cognitive Aid | Endoscopy Team Toolkit |
| Goldhaber-Fiebert et al., 2020 | United States | Prospective, non-randomised, comparative study | 69 unique cases | Operating room; Intensive Care Unit; Post-anesthesia care unit | Protocol | The Stanford Emergency Manual - Cognitive Aids for Perioperative Critical Events |
| Yule et al., 2021 | United States | Cross-sectional study | 10 surgical experts | Operating room | Education | Gathering Validity Evidence to Adapt the Non-technical Skills for Surgeons (NOTSS) Assessment Tool |
| Swanson et al., 2021 | United States | Quasi-experimental study | 50 radiation oncology staff | Radiation oncology department | Education | Crew Resource Management (CRM) Training and Incident Learning System (ILS) |
| Rose et al., 2018 | United States | Prospective, non-randomised, comparative study | 54,003 surgical cases | Operating room | Bundle/Checklists | Surgical debriefing checklist |
| Weldon et al., 2019 | UK | Prospective, non-randomised, comparative study | 8 surgical simulation courses | Operating room | Education | Video-Supported Simulation of Interactions in the Operating Theatre (ViSIOT) |
| Zevin et al., 2019 | Canada | Prospective cohort study | 25 general surgical residents | Operating room | Education | Comprehensive proficiency-based curriculum |
| Wong et al., 2019 | Canada | Pre-and-post observational study | 205 interventional radiology procedures | Interventional radiology suite | Bundle/Checklists | Preprocedural checklist |
| Hemingway et al., 2019 | United States | Non-randomised experimental study | 56 perioperative nurses | Perioperative environment | Communication device | Hands-free PCD |
| Randell et al., 2018 | UK | Prospective, non-randomised, comparative study | 44 theatre staff with experience of robot-assisted colorectal surgery from 9 hospitals | Operating room | Audit & Feedback | Interviews |
| Geoffrion et al., 2020 | United States | Pre-and-post observational study | Video recordings of 64 pre-intervention and 62 post-intervention handoffs | Intensive Care Unit; Cardiac Surgery Intensive Care Unit | Bundle/checklists | Handoff bundle |
| Lau et al., 2020 | United States | Prospective interrupted time series study | 22,420 cases (11,447 neurosurgical patients in the preintervention period and 10,973 in the postintervention period) | Operating room | Bundle/Checklists | UC Care Check OR checklist |
| Soma et al., 2020 | Australia | Before and after interventional study | 14 patients | Operating room | Bundle/Checklists | Operative team checklist for aerosol generating procedures to minimise exposure of healthcare workers to SARS-CoV-2 |
| Ridley et al., 2021 | United States | Prospective, non-randomised, comparative study | 141 clinicians (73 surveyed before and 68 after) | Operating room | Education | TeamSTEPPS training |
| Vortman, 2020 | United States | Prospective, non-randomised, comparative study | Not specified (more than 150 employees) | Operating room | Education | Simulation-Based Education for Massive Transfusion Protocol (MTP) |
| McLaughlin, 2014 | United States | Before and after interventional study | 93 surgical team members | Operating room | Protocol | Time-out process |
| Aydin et al., 2021 | Turkey | Prospective, non-randomised, comparative study | Interruptions in the operating theatre across 52 surgical procedures (12 neurosurgery and 40 general surgery operations) were recorded. Operations were performed by seven surgical teams at two tertiary care centres. routine operative procedures (ROP, n=26, observed without any intervention) and intervened operative procedures (IOP, n=26, observed after implementation of preventive measures) | Operating room | Bundle/Checklists | Intervened operative procedures |
| Towning et al., 2021 | UK | Prospective, non-randomized comparative study | 94 staff participants | Operating room | Education | Simulation Training for Surgical Tracheostomy |
| Chilakapati et al., 2021 | United States | Pre-and-post observational study | The pre- and post-implementation surveys were completed by 19 and 26 operating room staff members, respectively | Operating room | Cognitive aid | Strabismus-specific whiteboard |
| Ber et al., 2021 | United States | Before and after interventional study | 637 and 893 cases during the preintervention and intervention periods, respectively. | Operating room | Protocol | Aviation-like structured team communication practices |
| Urban et al., 2021 | Canada | Cross-sectional study | 2,032 healthcare professionals | Operating room | Bundle/Checklists | Surgical Safety Checklist |
| Sujan et al., 2022 | UK | Before and after interventional study | 14 participants | Surgical Emergency Unit | Education | Functional Resonance Analysis Method (FRAM) |
| Sillero et al., 2021 | Spain | Prospective, non-randomised, comparative study | 16 surgical staff | Operating room | Audit & Feedback | In-depth interviews |
| Truong et al., 2021 | United States | Two-wave survey study | 208 participants | Operating room | Education | Multidisciplinary simulated operating room (OR) team training |
| Grogan et al., 2022 | United States | Cross-sectional study | 72 participants | Operating room | Protocol | Identifier Bouffants |
| Van Dalen et al., 2022 | Netherlands | Prospective, non-randomised, comparative study | 98 study participants | Operating room | Protocol | Theatre cap challenge |
| Kalantari et al., 2021 | Iran | Randomised controlled trial | 300 nurses | Operating room | Education | Intraoperative education session |
| Vigo et al., 2022 | Switzerland | Prospective, non-randomised, comparative study | 175 robotic laparoscopic procedures | Operating room | Education | Interdisciplinary surgical team-training protocol for robotic gynecologic surgery |
| Hartman et al., 2022 | United States | Pre-and-post observational study | 3 liver transplant teams | Operating room | Education | Veno-veno bypass simulation |
| Thomas et al., 2019 | United States | Prospective, non-randomised, comparative study | 960 surgical phrases (480 spoken via the Da Vinci Si speakers, and 480 expressed through a wireless, hands-free system) | Operating room | Other | Wireless, hands-free audio system |
| Guris et al., 2019 | United States | Prospective observational cohort study with a double-blind and randomised controlled component | 22 1st-year anaesthesiology residents | Operating room | Education | Simulation education +/- a didactic session on speaking up behaviour |
| Acar et al., 2019 | Turkey | Prospective, randomized simulation study | A total of 19 scenarios were run with 28 participants | Operating room | Bundle/Checklists | Standardized evacuation checklist |
| Urman et al., 2021 | United States | Randomized controlled trial | 304 anesthesiologists (95 simulations) | Post-anesthesia care unit; Emergency Department | Education | Emergency manual (EM) |
| Sharma et al., 2021 | Canada | Prospective Cohort Study | 144 laparoscopic operations | Operating room | Protocol | Device-related interruptions characterized using the OR Black Box |
| Turrentine et al., 2020 | United States | Prospective, non-randomised, comparative study | 208 medical students (67 postintervention and 141 preintervention) | Operating room | Education | Simulated Room of Errors |
| Soares et al., 2021 | Brazil | Methodological Study | 24 participants | Simulation Laboratory of Clinical Practice in Nursing and Health | Education | Professional Nursing Communication Competence (IMC- CPE) |
| Tsafrir et al., 2020 | United States | Non-randomized, prospective controlled trial | 137 procedures | Operating room | Other | Quail Digital Healthcare headset system |
| Hussain et al., 2020 | Pakistan | Qualitative case study research | 16 health professionals | Operating room; Perinatal care | Education | Multidisciplinary team training |
| Suresh et al., 2021 | India | Cross-sectional study | 200 cases | Operating room | Bundle/Checklists | Modified WHO SSC for Neurosurgery |
| Shi et al., 2021 | United States | Before and after interventional study | 22 surgical staff | Operating room | Education | In-situ simulations |
| Wai et al., 2021 | Hong Kong | Pre-and-post observational study | 46 students | Classroom | Education | Crew Resource Management Training |
| Catchpole et al., 2022 | United States | Pre-and-post observational study | 367 trauma cases | Trauma room | Cognitive aid | “in the wild” smartphone communication app |
| Douglas et al., 2021 | Australia | Before and after interventional study | 107 operating room staff members | Operating room | Protocol | Surgical caps displaying team members’ names and roles |
| Nasiri et al., 2021 | Iran | Prospective, non-randomised, comparative study | 120 handovers | Operating room | Bundle/Checklists | SWITCH Checklist |
The authors have declared that no competing interests exist.
Funding Statement
This study was funded by The Ottawa Hospital Academic Medical Organization (TOHAMO) Innovation Fund. Dr. Boet was supported by The Ottawa Hospital Anesthesia Alternate Funds Association and the Faculty of Medicine, University of Ottawa with a Tier 2 Clinical Research Chair
Author Contributions
Concept and design: Mostafa Bondok, Nibras Ghanmi, Cole Etherington, Youssef Saddiki, Pierre-Marc Dion, Sylvain Boet
Acquisition, analysis, or interpretation of data: Mostafa Bondok, Nibras Ghanmi, Cole Etherington, Youssef Saddiki, Isabelle Lefebvre , Pauline Berthelot, Pierre-Marc Dion, Benjamin Raymond, Jeanne Seguin, Pooyan Sekhavati, Sindeed Islam, Sylvain Boet
Drafting of the manuscript: Mostafa Bondok, Nibras Ghanmi, Cole Etherington, Youssef Saddiki, Sylvain Boet
Critical review of the manuscript for important intellectual content: Mostafa Bondok, Nibras Ghanmi, Cole Etherington, Youssef Saddiki, Isabelle Lefebvre , Pauline Berthelot, Pierre-Marc Dion, Benjamin Raymond, Jeanne Seguin, Pooyan Sekhavati, Sindeed Islam, Sylvain Boet
Supervision: Sylvain Boet
References
- 1.Surgical adverse events: a systematic review. Anderson O, Davis R, Hanna GB, Vincent CA. Am J Surg. 2013;206:253–262. doi: 10.1016/j.amjsurg.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 2.The incidence, root-causes, and outcomes of adverse events in surgical units: implication for potential prevention strategies. Zegers M, de Bruijne MC, de Keizer B, Merten H, Groenewegen PP, van der Wal G, Wagner C. Patient Saf Surg. 2011;5:13. doi: 10.1186/1754-9493-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Surgical team behaviors and patient outcomes. Mazzocco K, Petitti DB, Fong KT, et al. Am J Surg. 2009;197:678–685. doi: 10.1016/j.amjsurg.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Oakbrook Terrace, IL: The Joint Commission; [ Dec; 2023 ]. 2016. Sentinel Event Data: Root Causes by Event Type, 2004 - 3Q 2015. [Google Scholar]
- 5.Improving patient safety by identifying latent failures in successful operations. Catchpole KR, Giddings AE, Wilkinson M, Hirst G, Dale T, de Leval MR. Surgery. 2007;142:102–110. doi: 10.1016/j.surg.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 6.Making a difference through improving teamwork in the operating room: a systematic review of the evidence on what works. Weller J, Boyd M. Curr Anesthesiol Rep. 2014;4:77–83. [Google Scholar]
- 7.Effective surgical teams: an integrative literature review. Teunissen C, Burrell B, Maskill V. West J Nurs Res. 2020;42:61–75. doi: 10.1177/0193945919834896. [DOI] [PubMed] [Google Scholar]
- 8.Processes and tools to improve teamwork and communication in surgical settings: a narrative review. Espin S, Indar A, Gross M, Labricciosa A, D'Arpino M. BMJ Open Qual. 2020;9:1–9. doi: 10.1136/bmjoq-2020-000937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Factors influencing team behaviors in surgery: a qualitative study to inform teamwork interventions. Aveling EL, Stone J, Sundt T, Wright C, Gino F, Singer S. Ann Thorac Surg. 2018;106:115–120. doi: 10.1016/j.athoracsur.2017.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The impact of improving teamwork on patient outcomes in surgery: a systematic review. Sun R, Marshall DC, Sykes MC, Maruthappu M, Shalhoub J. Int J Surg. 2018;53:171–177. doi: 10.1016/j.ijsu.2018.03.044. [DOI] [PubMed] [Google Scholar]
- 11.Interventions to improve teamwork and communications among healthcare staff. McCulloch P, Rathbone J, Catchpole K. Br J Surg. 2011;98:469–479. doi: 10.1002/bjs.7434. [DOI] [PubMed] [Google Scholar]
- 12.Investigating teamwork in the operating room: engaging stakeholders and setting the agenda. Frasier LL, Pavuluri Quamme SR, Becker A, Booth S, Gutt A, Wiegmann D, Greenberg CC. JAMA Surg. 2017;152:109–111. doi: 10.1001/jamasurg.2016.3110. [DOI] [PubMed] [Google Scholar]
- 13.Patient-centered operating room briefings to improve surgical quality. Koo K. JAMA Surg. 2015;150:183. doi: 10.1001/jamasurg.2014.2917. [DOI] [PubMed] [Google Scholar]
- 14.A meta-ethnographic review of interprofessional teamwork in hospitals: what it is and why it doesn't happen more often. Petit Dit Dariel O, Cristofalo P. J Health Serv Res Policy. 2018;23:272–279. doi: 10.1177/1355819618788384. [DOI] [PubMed] [Google Scholar]
- 15.Approaching the evidence basis for aviation-derived teamwork training in medicine. Zeltser MV, Nash DB. Am J Med Qual. 2019;34:455–464. doi: 10.1177/1062860619873215. [DOI] [PubMed] [Google Scholar]
- 16.Aviation safety: a whole new world? Barnett A. Transportation Science. 2020;54:84–96. [Google Scholar]
- 17.Is there a ‘big five’ in teamwork? Salas E, Sims DE, Burke CS. Small Group Res. 2005;36:555–599. [Google Scholar]
- 18.Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. French SD, Green SE, O'Connor DA, et al. Implement Sci. 2012;7:38. doi: 10.1186/1748-5908-7-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enhancing interprofessional collaboration in perioperative setting from the qualitative perspectives of physicians and nurses. Sillero Sillero A, Buil N. Int J Environ Res Public Health. 2021;18:10775. doi: 10.3390/ijerph182010775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barriers and enablers to effective interprofessional teamwork in the operating room: a qualitative study using the Theoretical Domains Framework. Etherington C, Burns JK, Kitto S, Brehaut JC, Britton M, Singh S, Boet S. PLoS One. 2021;16:0. doi: 10.1371/journal.pone.0249576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aviation and healthcare: a comparative review with implications for patient safety. Kapur N, Parand A, Soukup T, Reader T, Sevdalis N. JRSM Open. 2016;7:2054270415616548. doi: 10.1177/2054270415616548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan B, Cochrane D. Ottawa, ON: Canadian Institute for Health Information, Canadian Patient Safety Institute; 2016. Measuring patient harm in Canadian hospitals. [Google Scholar]
- 23.Systematic techniques to enhance retention in randomised controlled trials: the STEER study protocol. Gillies K, Bower P, Elliott J, et al. Trials. 2018;19:197. doi: 10.1186/s13063-018-2572-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferguson C, Robinson K, Cohen L. Bunbury WA: Edith Cowan University; 2022. Improving research results with the theory of planned behaviour. [Google Scholar]
- 25. Cambridge Handbook of Psychology, Health and Medicine. Cambridge: Cambridge University Press; 2019. [Google Scholar]
- 26.Action, actor, context, target, time (AACTT): a framework for specifying behaviour. Presseau J, McCleary N, Lorencatto F, Patey AM, Grimshaw JM, Francis JJ. Implement Sci. 2019;14:102. doi: 10.1186/s13012-019-0951-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teamwork, communication and safety climate: a systematic review of interventions to improve surgical culture. Sacks GD, Shannon EM, Dawes AJ, et al. BMJ Qual Saf. 2015;24:458–467. doi: 10.1136/bmjqs-2014-003764. [DOI] [PubMed] [Google Scholar]
- 28.PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Tricco AC, Lillie E, Zarin W, et al. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 29.Methods for research evidence synthesis: the scoping review approach. Sucharew H, Macaluso M. J Hosp Med. 2019;14:416–418. doi: 10.12788/jhm.3248. [DOI] [PubMed] [Google Scholar]
- 30.A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. Res Synth Methods. 2014;5:371–385. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.PRESS peer review of electronic search strategies: 2015 guideline statement. McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. J Clin Epidemiol. 2016;75:40–46. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 32.Knowledge translation interventions for critically ill patients: a systematic review*. Sinuff T, Muscedere J, Adhikari NK, et al. Crit Care Med. 2013;41:2627–2640. doi: 10.1097/CCM.0b013e3182982b03. [DOI] [PubMed] [Google Scholar]
- 33.Prevention of surgical malpractice claims by use of a surgical safety checklist. de Vries EN, Eikens-Jansen MP, Hamersma AM, Smorenburg SM, Gouma DJ, Boermeester MA. Ann Surg. 2011;253:624–628. doi: 10.1097/SLA.0b013e3182068880. [DOI] [PubMed] [Google Scholar]
- 34.Closed-loop communication improves task completion in pediatric trauma resuscitation. El-Shafy IA, Delgado J, Akerman M, Bullaro F, Christopherson NA, Prince JM. J Surg Educ. 2018;75:58–64. doi: 10.1016/j.jsurg.2017.06.025. [DOI] [PubMed] [Google Scholar]
- 35.Implementing no interruption zones in the perioperative environment. Wright MI. AORN J. 2016;104:536–540. doi: 10.1016/j.aorn.2016.09.018. [DOI] [PubMed] [Google Scholar]
- 36.Improving patient safety and optimizing nursing teamwork using crew resource management techniques. West P, Sculli G, Fore A, Okam N, Dunlap C, Neily J, Mills P. J Nurs Adm. 2012;42:15–20. doi: 10.1097/NNA.0b013e31823c17c7. [DOI] [PubMed] [Google Scholar]
- 37.Positive deviance: a different approach to achieving patient safety. Lawton R, Taylor N, Clay-Williams R, Braithwaite J. BMJ Qual Saf. 2014;23:880–883. doi: 10.1136/bmjqs-2014-003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Temporal trends in rates of patient harm resulting from medical care. Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. N Engl J Med. 2010;363:2124–2134. doi: 10.1056/NEJMsa1004404. [DOI] [PubMed] [Google Scholar]
- 39.Barriers to staff adoption of a surgical safety checklist. Fourcade A, Blache JL, Grenier C, Bourgain JL, Minvielle E. BMJ Qual Saf. 2012;21:191–197. doi: 10.1136/bmjqs-2011-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.A modified theoretical framework to assess implementation fidelity of adaptive public health interventions. Pérez D, Van der Stuyft P, Zabala MC, Castro M, Lefèvre P. Implement Sci. 2016;11:91. doi: 10.1186/s13012-016-0457-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.The tug-of-war: fidelity versus adaptation throughout the health promotion program life cycle. Bopp M, Saunders RP, Lattimore D. J Prim Prev. 2013;34:193–207. doi: 10.1007/s10935-013-0299-y. [DOI] [PubMed] [Google Scholar]
- 42.The definition of critical and non-critical moments in the operating room: a modified Delphi consensus study [Article in French] Boet S, Etherington C, Crnic A, et al. Can J Anaesth. 2020;67:949–958. doi: 10.1007/s12630-020-01688-3. [DOI] [PubMed] [Google Scholar]
- 43.Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder. Makary MA, Sexton JB, Freischlag JA, Holzmueller CG, Millman EA, Rowen L, Pronovost PJ. J Am Coll Surg. 2006;202:746–752. doi: 10.1016/j.jamcollsurg.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 44.Assessing the similarity of mental models of operating room team members and implications for patient safety: a prospective, replicated study. Nakarada-Kordic I, Weller JM, Webster CS, Cumin D, Frampton C, Boyd M, Merry AF. BMC Med Educ. 2016;16:229. doi: 10.1186/s12909-016-0752-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Do great teams think alike? An examination of team mental models and their impact on team performance. Gardner AK, Scott DJ, AbdelFattah KR. Surgery. 2017;161:1203–1208. doi: 10.1016/j.surg.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 46.Communication and relationship dynamics in surgical teams in the operating room: an ethnographic study. Tørring B, Gittell JH, Laursen M, Rasmussen BS, Sørensen EE. BMC Health Serv Res. 2019;19:528. doi: 10.1186/s12913-019-4362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Systematic review of safety checklists for use by medical care teams in acute hospital settings--limited evidence of effectiveness. Ko HC, Turner TJ, Finnigan MA. BMC Health Serv Res. 2011;11:211. doi: 10.1186/1472-6963-11-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.The surgical safety checklist and patient outcomes after surgery: a prospective observational cohort study, systematic review and meta-analysis. Abbott TE, Ahmad T, Phull MK, et al. Br J Anaesth. 2018;120:146–155. doi: 10.1016/j.bja.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 49.Systematic review and meta-analysis of the effect of the World Health Organization surgical safety checklist on postoperative complications. Bergs J, Hellings J, Cleemput I, et al. Br J Surg. 2014;101:150–158. doi: 10.1002/bjs.9381. [DOI] [PubMed] [Google Scholar]
- 50.World Health Organization surgical safety checklist modification: do changes emphasize communication and teamwork? Solsky I, Berry W, Edmondson L, et al. J Surg Res. 2020;246:614–622. doi: 10.1016/j.jss.2018.09.035. [DOI] [PubMed] [Google Scholar]
- 51.Changes in safety climate and teamwork in the operating room after implementation of a revised WHO checklist: a prospective interventional study. Erestam S, Haglind E, Bock D, Andersson AE, Angenete E. Patient Saf Surg. 2017;11:4. doi: 10.1186/s13037-017-0120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Do safety checklists improve teamwork and communication in the operating room? A systematic review. Russ S, Rout S, Sevdalis N, Moorthy K, Darzi A, Vincent C. Ann Surg. 2013;258:856–871. doi: 10.1097/SLA.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 53.Looking beyond the checklist: an ethnography of interprofessional operating room safety cultures. Ziman R, Espin S, Grant RE, Kitto S. J Interprof Care. 2018;32:575–583. doi: 10.1080/13561820.2018.1459514. [DOI] [PubMed] [Google Scholar]
- 54.A mixed methods study of challenges in the implementation and use of the surgical safety checklist. Mahmood T, Mylopoulos M, Bagli D, Damignani R, Aminmohamed Haji F. Surgery. 2019;165:832–837. doi: 10.1016/j.surg.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 55.Effect of the surgical safety checklist on provider and patient outcomes: a systematic review. Armstrong BA, Dutescu IA, Nemoy L, et al. BMJ Qual Saf. 2022;31:463–478. doi: 10.1136/bmjqs-2021-014361. [DOI] [PubMed] [Google Scholar]
- 56.Ten years of the surgical safety checklist. Weiser TG, Haynes AB. Br J Surg. 2018;105:927–929. doi: 10.1002/bjs.10907. [DOI] [PMC free article] [PubMed] [Google Scholar]