Abstract
Sixteen percent of patients referred for cardiology evaluation are found to have no cause for palpitations. Studies show that hypertension intricately influences “heart rate” and “contractility,?” the key components of “palpitation.” While the prevalence of hypertension is 22.4% in 18–39‐year‐olds, the relationship between palpitations and hypertension remains unknown in this age group. In our study, we assessed the incidence and prevalence of hypertension over 5 years in 18–40‐year‐olds referred for palpitations who had no known arrhythmic cause for palpitations between January 1, 206 and December 31, 2017. We found that over a period of 2.2 (0.7–4.1) years, an additional 56% patients were diagnosed with stage 1 (65/130) and stage 2 (28/130) hypertension, increasing the prevalence from 16% at the start of the study period to 72% at the end of the study period (p < .0001). Hypertensive patients were obese (BMI: 29 [24–36] kg/m2 vs. 25 [22–31] kg/m2; p = .03), used nonsteroidal anti‐inflammatory drugs (NSAIDs) (62 vs. 35%; p = .04), had a stronger family history of hypertension (55 vs. 4%; p < .0001) and exhibited higher systolic (124[120–130] mmHg vs. 112[108–115] mmHg; p < .0001) and diastolic (80[76–83] mmHg vs. 72[69–75] mmHg; p < .0001) blood pressures. Hypertension is commonly diagnosed in 18–40‐year‐old predominantly white female patients referred for palpitations without a known arrhythmic cause. The possibility of untreated hypertension causing palpitations in this cohort needs further evaluation.
Keywords: community‐based studies, hypertension—general, left ventricular hypertrophy (LVH) hypertension/arrhythmias, primary care issues
1. BACKGROUND
“Palpitations” is defined as a subjective ability to feel one's own heartbeat, which can be rapid and/or forceful. Palpitation is the second most common reason for cardiology referral after chest pain. Despite extensive clinical evaluation, no cause for the palpitations can be found in up to 16% of patients. 1
Systemic hypertension continues to be a major public health problem. Its definition was revised in 2017 when the ACC/AHA guidelines lowered the blood pressure cutoff for its diagnosis. 2 Consequently, the prevalence of hypertension increased in the age group 18−39 years from 7.5 to 22.4%. 3
We have anecdotally noted young patients with undiagnosed hypertension being referred for palpitations who upon evaluation are found to have no arrhythmic cause for their condition. These patients report feeling better with hypertension treatment, suggesting causality. Despite the above, the relationship between untreated hypertension and palpitations remains unknown in this young referral population.
We sought to determine the incidence and prevalence of undiagnosed hypertension in a younger patient cohort aged 18−40 years, who were referred to an outpatient cardiology clinic for evaluation of palpitations and were noted to have normal cardiac monitor findings as judged by the evaluating cardiac electrophysiologist.
2. METHODS
We conducted a retrospective, chart review of a cohort study to assess the prevalence of hypertension at the time of referral for the symptom of palpitations, and the incidence and prevalence of hypertension over a 5‐year follow‐up period. We also analyzed the salient attributes of patients diagnosed with hypertension and their differences from normotensive patients. Following were the study inclusion criteria:
Patient age was ≥18 years and ≤40 years at the time of consultation.
Patient was evaluated for palpitations in an outpatient cardiology clinic between January 1, 2016, and December 31, 2017.
Patient cardiac monitoring (1–30 days) showed no arrhythmic cause for palpitations.
Patients had at least 1‐year follow‐up with ≥2 BP readings in an outpatient setting.
Patients were referred from outpatient primary care offices to an outpatient cardiology office and evaluated by board‐certified cardiac electrophysiologists for palpitations. Patients were evaluated with pertinent history, physical examination, and laboratory tests with the focus on the symptom of palpitations. Cardiac monitors ranging from 24 h to 30‐day duration based on the clinical features of palpitations were ordered and reviewed. A limited number of patients underwent repeat cardiac monitoring as judged clinically necessary by the evaluating cardiac electrophysiologist. After patient monitors were deemed to exhibit normal findings 4 by the evaluating cardiac electrophysiologist, the patients were generally referred back to the referring primary care physician for continued routine follow‐up care.
For the purpose of our study, “palpitations” was defined as a subjective ability for the patient to feel one's own heartbeat, which could be rapid and/or forceful.
Diagnosis of normotension, elevated BP, and hypertension was made based on the ACC/AHA 2017 High Blood Pressure Clinical Practice Guidelines, by averaging BP readings on at least two separate occasions as noted in their chart review. 2
Patient's electronic medical records were reviewed for data extraction from the time of palpitation evaluation till up to 5 years follow‐up. A REDCap database was used for storing extracted data, which was then used for statistical analysis. Pertinent patient data as listed in supplemental data were extracted for the research study purposes. The study was approved by the ethics committee of OhioHealth IRB.
2.1. Statistical analysis
For continuous variables that were normally distributed, mean and standard deviation were computed. Median and 25th and 75th percentile were calculated if the data were not normally distributed. For categorical variables, proportion and frequency count were calculated. Group comparisons of categorical variables were made using Fisher's exact or Chi‐square test and of continuous variables using Student's t‐test (for normally distributed variables) and nonparametric t‐test or Mann–Whitney U test (for variables not distributed normally). Multiple continuous independent variables were compared using ANOVA or Kruskal–Wallis test for normally and not normally distributed variables, respectively. Paired continuous variables pre‐ and post‐intervention were compared with either paired t‐test or Wilcoxon signed‐rank test for normally or not‐normally distributed data, respectively. Kaplan–Meier analysis with Mantel–Cox (Log‐Rank) test was used to explain the relationship between a dependent binary outcome (incidence of hypertension) and an independent variable (family history of hypertension). Yearly incidence of hypertension was calculated by dividing the number of patients newly diagnosed with hypertension with the total number of patients at risk of developing hypertension at the end of each specified year. Similarly, yearly prevalence of hypertension was calculated by taking a total number of cumulative patients diagnosed with hypertension until the end of the specified year and dividing by 130, the total number of patients in the cohort study.
We used GraphPad statistical software Prism 9 Version 9.1.2 for statistical analysis of the data.
3. RESULTS
A total of 130 patients aged 28 ± 6 years, of whom 72% were females and 88% were White, were included in the study and retrospectively followed over 2.2 (0.7–4.1) years. During the course of the study, patients underwent an average of 1.1 ± 0.4 cardiac monitors. Table 1 depicts the clinical features of the study patient cohort dichotomized based on the diagnosis of hypertension.
TABLE 1.
Patient characteristics and results.
| Patient characteristics | Normotensive (n = 23) | Hypertensive (n = 94) | p‐value |
|---|---|---|---|
| Demographics | |||
| Age (years) | 29 ± 6 | 28 ± 6 | ns |
| Female gender | 19 (83%) | 64 (68%) | ns |
| White race | 22 (96%) | 83 (88%) | ns |
| Medical history pertinent to “palpitations” | |||
| Alcohol consumption | 12 (52%) | 50 (53%) | ns |
| Nicotine use | 4 (17%) | 11 (12%) | ns |
| Beta‐agonist use | 6 (26%) | 16 (17%) | ns |
| Anticholinergic use | 1 (4%) | 15 (16%) | ns |
| Antidepressant/Antipsychotic use | 8 (35%) | 30 (32%) | ns |
| Illicit drug use | 2 (9%) | 9 (10%) | ns |
| NSAIDs use | 7 (35%) | 45 (62%) | .04 |
| Corticosteroid use | 5 (22%) | 19 (20%) | ns |
| Family history of hypertension | 1 (4%) | 51 (55%) | <.0001 |
| Hyper/Hypothyroidism | 3 (13) | 8 (9%) | ns |
| Pregnancy | 1 (5%) | 6 (9%) | ns |
| Anemia | 10 (43%) | 21 (22%) | .04 |
| Caffeine use | 5 (22%) | 18 (19%) | ns |
| Physical Eexamination pertinent to “palpitations” | |||
| Body mass Index (kg/m2) | 25 (22–31) | 29 (24–36) | .03 |
| Average systolic BP (mmHg) | 112 (108–115) | 124(120–130) | <.0001 |
| Average diastolic BP (mmHg) | 72 (69–75) | 80 (76–83) | <.0001 |
| Echocardiographic data | |||
| LV posterior wall diastolic thickness (cm) | 0.86 ± 0.18 | 0.90 ± 0.18 | ns |
| Left Ventricular ejection fraction (%) | 59 ± 4 | 60 ± 4 | ns |
| Left atrial dimension (cm) | 3 ± 0.4 | 3.2 ± 0.6 | ns |
| Mitral regurgitation | 4 (17%) | 39 (41%) | .03 |
| Tricuspid regurgitation | 3 (13%) | 39 (41%) | .01 |
| Pulmonic regurgitation | 2 (9%) | 27 (29%) | ns |
| Baseline laboratory data | |||
| Serum sodium (meq/L) | 140 ± 2.2 | 140 ± 2.3 | ns |
| Serum potassium (mmol/L) | 3.8 ± 0.5 | 4 ± 0.4 | ns |
3.1. Incidence and prevalence of hypertension in the study cohort
At the time of initial evaluation of palpitations, 21/130 (16%) referred patients already had the diagnosis of hypertension. Over the study period of 2.2 (0.7–4.1) years, an additional 73 patients met the ACC/AHA criteria per 2017 guidelines for hypertension and 13 patients were deemed to exhibit elevated BP without confirmation of hypertension. 2 Importantly, a 4.5‐fold increase in hypertension prevalence from pre‐ to post‐evaluation for palpitations (p < .0001) was noted in the study cohort (Figure 1A). More women met the criteria for (previously undiagnosed) hypertension or elevated BP than men during the course of the study (74 vs. 26%; p = .04).
FIGURE 1.
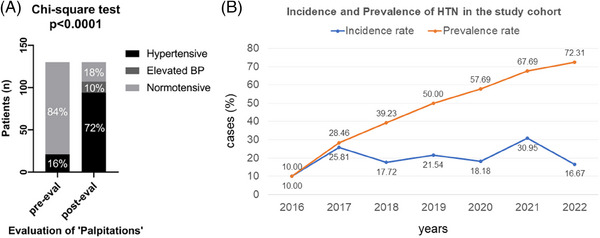
Incidence and prevalence of hypertension over the study period: (A) bar graph depicting the prevalence of hypertension pre‐ and post‐palpitations evaluation. Note a 4.5‐fold increase in hypertension prevalence over the study period of 2.2 (0.7–4.1) years. (B) Graph showing the incidence and prevalence of hypertension in the study cohort between 2016 and 2022.
All 21 patients with hypertension at the start of the evaluation were being treated with a mean of 1.5 ± 0.8 antihypertensive medications. Despite treatment, the mean arterial BP was still higher in known hypertensives than in patients with the new diagnosis of hypertension (99 ± 9.4 mm Hg vs. 94 ± 5 mm Hg; p = .004). Only two additional antihypertensives were started during the course of the study (one previously known hypertensive patient and one newly diagnosed with hypertension) when referred back to the primary care physician.
Figure 1B depicts the incidence and prevalence rate of hypertension in the study cohort from year 2016 to 2022. When evaluated against historical control data in a comparable age group of 18−39 years 3 in the US general population, our study cohort had significantly higher prevalence of hypertension at the end of the study period (22.4 vs. 72%; p < .0001).
3.2. Hypertension characteristics in the study cohort
The average systolic BP (124[120–130] mmHg vs. 112[108–115] mmHg; p < .0001) and diastolic BP (80[76–83] mmHg vs. 72[69–75] mmHg; p < .0001) in the hypertensive group was significantly higher than the normotensive group.
The commonest type of hypertension noted in the study cohort was combined systolic and diastolic hypertension (45%) followed by isolated diastolic hypertension (25%). Figure 2A shows a pie chart depicting hypertension types in the study cohort. Figure 2B shows the hypertension categories noted across the patient cohort with stage 1 hypertension (130–139/80–89 mmHg) being the most prevalent at 50%.
FIGURE 2.
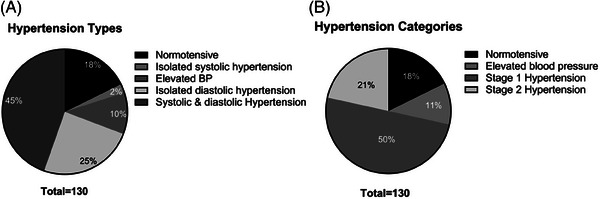
Hypertension characteristics: pie charts depicting hypertension types (A) and categories (B) noted in the study population during the study period. Note that majority of study patients had both systolic and diastolic stage 1 hypertension.
3.3. Salient attributes of hypertensive patients in the study cohort
Patients diagnosed with hypertension over the study period had significantly higher BMI (29 [24–36] kg/m2 vs. 25 [22–31] kg/m2; p = .03) (Figure 3A), which was primarily due to higher body weight (82 [68‐–104] kg vs. 70 [60–82] kg; p = .01). Height was not significantly different between the hypertensive and normotensive patient groups.
FIGURE 3.
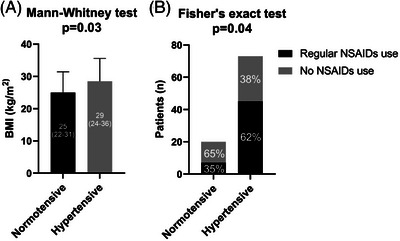
Salient attributes of hypertensive patients: during the study period, patients diagnosed with hypertension had significantly higher BMI (A) and had higher regular use of NSAIDs (B). Both these attributes are strongly associated with hypertension.
Hypertensive patients were more likely to use nonsteroidal anti‐inflammatory drug (NSAIDs) on a regular basis than patients who were normotensive over the study period (62 vs. 35%; p = .04) (Figure 3B). Furthermore, a significantly higher percentage of patients in the hypertensive group had a family history of hypertension than in the normotensive group (55 vs. 4%; p < .0001) (Figure 4A). Accordingly, patients with a family history of hypertension were more likely to be diagnosed with hypertension (Figure 4B) over the study period.
FIGURE 4.
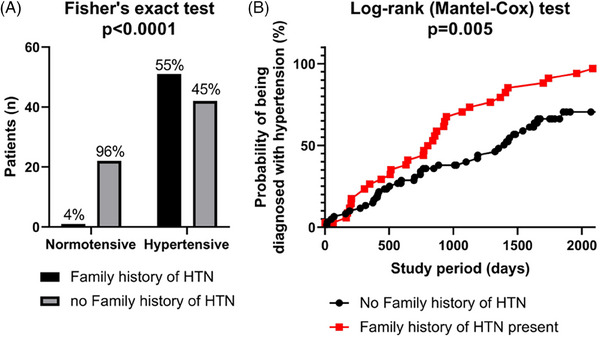
Salient attributes of hypertensive patients (cont.): (A) significantly more patients diagnosed with hypertension had family history of hypertension. (B) Furthermore, patients with family history of hypertension were more likely to be diagnosed with hypertension during the study period.
Although, the number of pregnant females in the normotensive (5%) and the hypertensive (9%) groups were similar, a significant number of patients in the “elevated BP without hypertension diagnosis” group were pregnant at the time of “palpitation” evaluation (4/11 [36%]; p = .03).
Hypertensive patients were also less likely to be anemic (22 vs. 43%; p = .04) than normotensive patients (Table 1). Additionally, significantly more patients in the hypertensive group were noted to have (mitral and tricuspid) regurgitant valvular pathology than in the normotensive group on their surface echocardiogram (Table 1) despite having no difference in LV thickness or LA size (data not shown).
4. DISCUSSION
The salient finding from our study is that the prevalence of undiagnosed and therefore untreated hypertension is significantly higher in a patient cohort aged 18−40 years without a known arrhythmic cause for “palpitations” than in a comparable age‐matched historical control US population. White women with newly diagnosed hypertension/elevated BP outnumbered men in this study cohort.
Major emphasis is put on the technique of obtaining BP as per the ACC/AHA hypertension guidelines. 2 Erroneous technique can overestimate BP readings falsely diagnosing a patient with hypertension. Given our study is retrospective, there is no way to confirm that all the BP measurements were made with the recommended technique. However, there are several facts noted in our study that suggest that the BP measurements were largely accurate and not an over‐estimation: (1) there were subsets of patients who remained normotensive throughout the study during repeated measurements and another that displayed elevated BP on some occasions but normotensive on others (elevated BP without hypertension), (2) the patient cohort diagnosed with hypertension over the study period exhibited clinical features typically associated with hypertension like higher BMI, family history of hypertension and higher daily use of NSAIDs. 2 The hypertensive group also exhibited cardiac structural changes like a higher prevalence of mitral regurgitation than the normotensive group as previously reported in patients with elevated BP. 5
There is abundant literature associating hypertension with cardiac arrhythmias. 6 , 7 In fact, this relationship is so strong and well known that a consensus statement was published for the physicians to use in their clinical practice in 2017. 8 Both brady‐arrhythmias like sinus node disease and atrioventricular block and tachy‐arrhythmias like atrial fibrillation/flutter, paroxysmal supraventricular tachycardia (atrial tachycardia) and ventricular arrhythmias can occur as a manifestation of hypertensive heart disease and in some instances instigated by medications used in treatment of hypertension like diuretics. 8
Ironically, there is a paucity of literature suggesting undiagnosed hypertension causing nonarrhythmic palpitations. Our study does not prove this association, but provides preliminary data for a future prospective trial to test this hypothesis. There are several pathophysiological reasons to believe that this causal relationship exists. Hypertension has a well‐established relationship with heart rate and cardiac contractility, which form the key components of “palpitation.” Increase in the resting heart rate has been associated with an increased risk of hypertension. 9 , 10 , 11 A linear relationship exists between the two especially in individuals with heart rates >80/min. 12 Furthermore, an increase in left ventricular contractility is noted in patients with early hypertension. 13 , 14
Our study also highlights that younger patients in the age group 18−40 years are being underdiagnosed and hence undertreated for hypertension. This could be from a number of reasons. Blood pressure readings for hypertension diagnosis have been revised recently in 2017 ACC/AHA hypertension guidelines 2 and the lower cutoffs may not have caught on in primary care. Palpitation is not considered a classic symptom of hypertension and therefore can be easily overlooked. Easy referral access and patient demand for super‐specialty care like cardiac electrophysiology may further dampen the enthusiasm for basic evaluation for palpitation at the primary care level.
Daily NSAID use is associated with BP increase in both normotensive and hypertensive individuals 2 especially in younger women 15 and also increases the risk of atrial fibrillation. 16 Despite the above, we did not observe atrial fibrillation, a well‐known cause for palpitations in any of our study patients on repeated cardiac monitors and follow up during the entire study period. This suggests that sustained elevated BP may be enough to instigate palpitations.
Anemia is a well‐known cause for “palpitations” especially with exertion when both cardiac contractility and heart rate increase to compensate for low hemoglobin. We found hypertensive patients less likely to be anemic than normotensive patients consistent with a prior observation of a positive relationship between hemoglobin levels and BP. 17 This indirectly suggests that anemia was an unlikely cause of palpitations in the hypertensive group but may contribute to this symptom in the normotensive group.
5. PERSPECTIVES
Findings from our study are preliminary data and should fuel a prospective, randomized, placebo‐controlled trial to confirm them. We propose a study in which 18−40‐year‐old patients who have palpitations without a known arrhythmic cause as confirmed by enhanced cardiac monitoring using conventional cardiac monitors, implanted loop recorder and over‐the‐counter wearables like KardiaMobile EKG monitor should be asked to maintain a BP log. If indeed hypertension is diagnosed, then hypertensive patients should be randomized to either antihypertensive medications or placebo. The patients should then be followed to evaluate whether their symptoms of palpitations abate with the treatment of hypertension.
6. LIMITATIONS
Ours being a retrospective research study, there are several limitations including patient selection and symptom recall bias and possibly inadequate power to evaluate small differences in study parameters. Additionally, this study utilized data originally collected during the course of clinical care, which may be recorded differently across providers or be incomplete. This was a single center study in a midwestern tertiary care medical center, and therefore cannot be generalizable over other areas with different demographics. Our study was not designed to establish causality between undiagnosed hypertension and palpitations, which cannot be categorically concluded from our study. Lastly, our study lacks a control cohort, in lieu of which we have used historical control data from age‐matched US population, 3 which has its own limitations.
7. CONCLUSIONS
When referred for evaluation, the prevalence of undiagnosed hypertension is significantly higher in 18−40‐year‐old predominantly White females who do not harbor a known arrhythmic cause for palpitations. The possibility of untreated hypertension causing palpitations in this patient cohort needs further evaluation.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Wasco C, Khan Z, Willett A, et al. Incidence and prevalence of hypertension in 18–40‐year‐old patients referred for palpitations with normal cardiac monitor findings. J Clin Hypertens. 2024;26:696–702. 10.1111/jch.14813
DATA AVAILABILITY STATEMENT
Upon request.
REFERENCES
- 1. Weber BE, Kapoor WN. Evaluation and outcomes of patients with palpitations. Am J Med. 1996;100(2):138‐148. [DOI] [PubMed] [Google Scholar]
- 2. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive Summary: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269‐1324. [DOI] [PubMed] [Google Scholar]
- 3. Ostchega Y, Fryar CD, Nwankwo T, Nguyen DT. Hypertension prevalence among adults aged 18 and over: United States, 2017–2018. NCHS Data Brief. 2020(364):1‐8. [PubMed] [Google Scholar]
- 4. Williams CB, Andrade JG, Hawkins NM, et al. Establishing reference ranges for ambulatory electrocardiography parameters: meta‐analysis. Heart. 2020;106(22):1732‐1739. [DOI] [PubMed] [Google Scholar]
- 5. Rahimi K, Mohseni H, Otto CM. Elevated blood pressure and risk of mitral regurgitation: a longitudinal cohort study of 5.5 million United Kingdom adults. PLoS Med. 2017;14(10):e1002404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Varvarousis D, Kallistratos M, Poulimenos L, et al. Cardiac arrhythmias in arterial hypertension. J Clin Hypertens (Greenwich). 2020;22(8):1371‐1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marazzato J, Blasi F, Golino M, Verdecchia P, Angeli F, De Ponti R. Hypertension and arrhythmias: a clinical overview of the pathophysiology‐driven management of cardiac arrhythmias in hypertensive patients. J Cardiovasc Dev Dis. 2022;9(4):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lip GYH, Coca A, Kahan T, et al. Hypertension and cardiac arrhythmias: a consensus document from the European Heart Rhythm Association (EHRA) and ESC Council on Hypertension, endorsed by the Heart Rhythm Society (HRS), Asia‐Pacific Heart Rhythm Society (APHRS) and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). Europace. 2017;19(6):891‐911. [DOI] [PubMed] [Google Scholar]
- 9. Rao D, Balagopalan JP, Sharma A, Chauhan VC, Jhala D. BEAT survey: a cross‐sectional study of resting heart rate in young (18‐55 year) hypertensive patients. J Assoc Physicians India. 2015;63(5):14‐17. [PubMed] [Google Scholar]
- 10. Wang A, Liu X, Guo X, et al. Resting heart rate and risk of hypertension. J Hypertens. 2014;32(8):1600‐1605. [DOI] [PubMed] [Google Scholar]
- 11. Kim DI, Yang HI, Park JH, et al. The association between resting heart rate and type 2 diabetes and hypertension in Korean adults. Heart. 2016;102(21):1757‐1762. [DOI] [PubMed] [Google Scholar]
- 12. Dalal J, Dasbiswas A, Sathyamurthy I, et al. Heart rate in hypertension: review and expert opinion. Int J Hypertens. 2019;2019:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Borlaug BA, Lam CSP, Roger VL, Rodeheffer RJ, Redfield MM. Contractility and ventricular systolic stiffening in hypertensive heart disease. J Am Coll Cardiol. 2009;54(5):410‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hinderliter AL, Light KC, Willis PW. Patients with borderline elevated blood pressure have enhanced left ventricular contractility*. Am J Hypertens. 1995;8(10):1040‐1045. [DOI] [PubMed] [Google Scholar]
- 15. Curhan GC, Willett WC, Rosner B, Stampfer MJ. Frequency of analgesic use and risk of hypertension in younger women. Arch Intern Med. 2002;162(19):2204. [DOI] [PubMed] [Google Scholar]
- 16. Schmidt M, Christiansen CF, Mehnert F, Rothman KJ, Sorensen HT. Non‐steroidal anti‐inflammatory drug use and risk of atrial fibrillation or flutter: population based case‐control study. BMJ. 2011;343(1):d3450. jul04. [DOI] [PubMed] [Google Scholar]
- 17. Atsma F, Veldhuizen I, de Kort W, van Kraaij M, Pasker‐de Jong P, Deinum J. Hemoglobin level is positively associated with blood pressure in a large cohort of healthy individuals. Hypertension. 2012;60(4):936‐941. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon request.


