Abstract
During our previous bilateral adrenal vein sampling (AVS) procedure, the authors observed that accessing the left adrenal vein through the antecubital vein was more feasible than the conventional femoral vein. Meanwhile, the femoral vein pathway facilitated access to the right adrenal vein than the antecubital vein pathway. Therefore, the authors hypothesized that simultaneous bilateral AVS via the antecubital combined with the femoral vein pathway could improve the success rate. A total of 94 cases of AVS via the antecubital combined with the femoral vein pathway were performed, while the remaining 20 cases employed the antecubital vein pathway at our center between August 2020 and April 2023. Furthermore, a meta‐analysis was conducted in this study using 15 selected articles to determine the success rate of AVS in each center and pathway. The success rate of ACTH‐stimulated simultaneous bilateral AVS via the antecubital vein combined with the femoral vein pathway was 92.85% (P = .503) on the right and 95.00% (P < .001) on the left. In the antecubital vein pathway, the success rates were only 25.00% (P < .001) on the right side and 80.00% (P = .289) on the left side. The results of meta‐analysis demonstrated a success rate of 78.16% on the right and 94.98% on the left for ACTH‐stimulated AVS via the femoral vein pathway. Based on our center's experience, simultaneous bilateral adrenal vein sampling via the combined pathway could improve the success rate of AVS in the short term and shorten the learning curve.
Keywords: adrenal vein sampling (AVS), lateral index (LI), primary hyperaldosteronism (PA), secondary high blood pressure (HBP), selection index (SI)
1. INTRODUCTION
Previously considered infrequent as a cause of secondary hypertension, Primary Aldosteronism (PA) has now been unequivocally established as the predominant etiology in recent times. The prevalence of PA in patients with hypertension ranges from 5% to 10%, but notably increases to 17%−23% among those with refractory hypertension. 1 , 2 , 3 The pathogenesis of PA involves the development of hypertension and hypokalemia, which arise from unilateral or bilateral hyperplasia of the adrenal cortex or adrenal adenomas, resulting in excessive autonomous secretion of aldosterone. In rare cases, PA may also be attributed to adrenal cancer or familial aldosteronism diseases. 1 Unilateral PA can be effectively treated through adrenalectomy, while conservative management with mineralocorticoid antagonists (MRAs) is recommended for bilateral disease. Various diagnostic methods are employed to classify PA subtypes, encompassing evaluation of clinical manifestations, imaging characteristics, posture excitation tests, adrenal scintigraphy, and adrenal vein sampling (AVS). However, in the subtyping of PA, AVS remains the gold standard for determining the lateralization of aldosterone secretion. 4 , 5 , 6 The systematic application of AVS in the categorization of patients with PA has identified unilateral forms in approximately two thirds of cases, including surgically treatable subtypes. The systematic implementation of AVS in the categorization of patients with PA has revealed unilateral forms in approximately two thirds of cases, including subtypes that can be effectively treated through surgery. This rate is twice as high compared to centers that do not utilize AVS, thereby emphasizing both the prevalence of surgically treatable PA and highlighting AVS's capability to identify patients who would benefit from surgical intervention. 7 , 8 The lack of consensus regarding the clinical procedure and interpretation of AVS data has resulted in significant variability in success rates across different centers. Typically, the femoral vein pathway is employed for bilateral blood collection during AVS. 9 The pulsatile secretion of cortisol or aldosterone can result in sequential and asynchronous blood collection from bilateral adrenal veins within the same vein, potentially introducing artificial discrepancies between the left and right adrenal glands. This phenomenon is particularly noteworthy when less experienced practitioners perform AVS. Collecting blood simultaneously from both bilateral adrenal veins can effectively alleviate this concern. 10 Additionally, nearly two thirds of centers employ the sequential technique involving adrenocorticotropic hormone (synthetic adrenocorticotropic hormone 1−24, ACTH) stimulation, while certain research centers opt for the bilateral asynchronous technique without ACTH stimulation. 11 Recently, significant advancements have emerged in AVS cannulation techniques. The majority of clinical centers prefer unilateral or bilateral femoral vein cannulation to facilitate blood collection from both the left and right adrenal veins, allowing for either asynchronous or synchronous sampling. 12 Simultaneously, certain centers utilize the antecubital vein pathway for sequential sampling of the left and right adrenal veins. 9 Our previous observations demonstrated that the antecubital vein pathway offers enhanced accessibility in locating the left adrenal vein compared to the conventional femoral vein pathway, while the femoral vein pathway facilitates easier access to the right adrenal vein than the antecubital vein pathway. This hypothesis suggests that the simultaneous bilateral collection of adrenal vein blood using both the antecubital and femoral vein pathways may improve the short‐term success rate and accuracy of AVS. Additionally, a meta‐analysis was conducted to compare the success rates of AVS performed via the antecubital vein pathway combined with the femoral vein pathway in our center with those reported in previous studies.
2. METHODS
2.1. Subjects
This study included 114 AVS procedures conducted at our center between August 2020 and April 2023, with 94 cases utilizing a combination of antecubital and femoral vein pathway, while 20 cases relied solely on the antecubital vein pathway. All patients fulfilled the diagnostic criteria for PA according to the guidelines established by the American Endocrine Society and were considered suitable candidates for adrenal surgery, with the need for further surgical intervention assessed via AVS. 1 Prior to undergoing AVS, all patients provided informed consent. Simultaneously, the study recorded baseline characteristics, including age, gender, hypertension grade, blood pressure control level, serum potassium levels, aldosterone‐to‐renin ratio (ARR), and other relevant factors. Before AVS procedure initiation, all patients in our center underwent bilateral adrenal glands computed tomography (CT) imaging to confirm the presence of bilateral or unilateral adrenal gland lesions. Prior to AVS, patients with hypokalemia underwent corrective measures for their condition, while ensuring their psychological well‐being was prioritized. The AVS procedures were performed by a proficient cardiovascular physician.
2.2. AVS procedure
Prior to the AVS procedure, the patient was positioned supine and prepared with routine disinfection. Local anesthesia using 2% lidocaine was administered. Intravenous access was established by the nurse in the cardiac catheterization laboratory. The puncture site for forearm access was selected from options including the left cephalic vein, basilic vein, cubital vein, anterior median vein, or subclavian vein; while for lower limb access, it was chosen from the right femoral vein. The AVS procedure was performed by a skilled cardiologist who specializes in PTCA (Percutaneous Transluminal Coronary Angioplasty) and had an experience of performing over 500 procedures annually. In the cardiac catheterization laboratory, a 5F TIG catheter (Terumo Corporation, Tokyo, Japan) was typically used for blood collection from the left adrenal vein via the forearm vein, while an MPA2 catheter (Cordis) equipped with a self‐made side hole at the tip was utilized for blood collection from the right antecubital vein pathway. For gathering blood from the right adrenal vein through femoral vein, a C2 catheter (Cobra2, Cordis) with a self‐made side hole at the head end was employed. During left‐side blood extraction, the .035‐inch guidewire was cautiously advanced through the antecubital veins, superior vena cava, right atrium, and subsequently into the inferior vena cava (IVC). Following this, the TIG contrast catheter was guided into the left common trunk vein (approached from the left side), which is formed by the convergence of the subphrenic vein and left adrenal vein. A small quantity of nonionic contrast agent was gently infused through the catheter's tip, confirmed via digital subtraction angiography (DSA) to reach the common trunk and visualize the left adrenal vein. Subsequently, a 5F MPA2 catheter or a 5F C2 catheter was introduced for accessing the right adrenal vein. Once both catheters were appropriately positioned, blood sample collection commenced by utilizing natural outflow to simultaneously obtain bilateral blood samples whenever feasible. Forty‐two patients were subjected to pre‐ and post‐ACTH stimulation sampling, with an additional bilateral blood sample collected 15 min following the administration of a single intravenous bolus injection of ACTH (250 mg). Upon completion of blood collection, remove the sheath and apply gentle pressure to the puncture site for at least one minute. Secure the wound using sterile gauze and medical tape. Subsequently, refrigerate the specimens for examination aimed at detecting indicators such as cortisol and aldosterone levels. Provide detailed instructions to closely monitor post‐AVS changes in the patient's heart rate, blood pressure, and surgical wound.
2.3. Definition of SI and LI
The Selection Index (SI) typically represents the ratio of plasma cortisol concentration (PCC) in the adrenal vein to PCC in the inferior vena cava, while the Lateral Index (LI) is characterized by comparing the adrenal vein plasma aldosterone concentration (PAC) divided by PCC (A/C ratio) with the contralateral PAC/PCC ratio. The Contralateral Suppression Index (CSI) is defined as the ratio of adrenal vein A/C to peripheral vein (IVC) A/C. 7 Currently, there is no consistent consensus regarding the criteria for successful catheter insertion and lateralization in AVS. Given the potential challenges associated with positioning on the right side, including the occurrence of an adrenal silent period, unsuccessful PA placement on one side may occur. In such cases, evaluating the contralateral suppression index becomes imperative to confirm the diagnosis of the subtype of PA. Moreover, in cases where AVS fails on one side and the successful side exhibits apparent suppression, this outcome can also provide valuable guidance for adrenal surgery. Additionally, it is crucial to incorporate CT assessment of adrenal gland function, blood pressure measurements, potassium levels analysis, etc. in order to determine the suitability for adrenal surgery. In this study, according to the guideline, we established SI ≥ 2 as the benchmark for surgical success in the non‐ACTH stimulation group; LI ≥ 2 and contralateral CSI < 1 indicate lateralization presence. For the ACTH stimulation group, SI ≥ 3 was set as the criterion for successful AVS; LI ≥ 4 and contralateral CSI < 1 signify lateralization presence. 2 , 13
2.4. Statistical methods for clinical research
In statistics, continuous variables were presented as mean ± standard deviation, while categorical variables were depicted as counts and percentages. Significance was set at P < .05. Statistical analysis was conducted employing the SPSS for MAC statistical software package (Version 21; SPSS Inc., Chicago, USA). The statistical comparisons were executed using nonparametric test and chi‐square test.
3. RESULTS
3.1. The success rate of AVS in our center
Our center performed a total of 114 AVS procedures. All patients underwent both adrenal glands CT examination and AVS. The preoperative data included age, gender, hypertension grade, blood pressure control level, serum potassium levels, and aldosterone‐to‐renin ratio (ARR), which were documented and organized in Table 1. In our center, the ARR calculation utilizes the plasma aldosterone concentration(pg/mL) to direct renin concentration (DCC, pg/mL) ratio with a cut‐off value set at 38. Preoperative adrenal CT scans confirmed the presence of unilateral or bilateral lesions in all 72 patients included in this cohort. Among them, 20 patients underwent AVS using the bilateral antecubital vein pathway, while 52 patients underwent AVS through a combined femoral vein and antecubital vein approach. Notably, among these patients, simultaneous ACTH stimulation was performed during AVS in 42 cases.
TABLE 1.
Clinical features of 114 AVS cases.
| Combined pathway (n = 52) | Antecubital vein pathway (n = 20) | After ACTH stimulus (n = 42) | |
|---|---|---|---|
| Age (years) | 53.5 | 56.3 | 53.5 |
| Sex (M/F) (%) | 28/24 | 12/8 | 23/19 |
| Hypertensiongrade (I/II/III) (%) | 5/13/33 | 3/5/12 | 4/7/31 |
| SBP (mmHg a ) | 143.2 | 142.6 | 147 |
| DBP (mmHg) | 85.6 | 85.5 | 87.5 |
| K+ (mmol/L) | 3.70 | 3.71 | 3.60 |
| ARR | 239.41 | 231.6 | 315.5 |
1 mmHg = .133 kPa.
In our combined approach, the success rate for the right side was 86.50% (45/52) and for the left side it was 67.30% (35/52). In contrast, the success rate for the right side in our center's early bilateral antecubital vein pathway was 25.00% (5/20) (P < .001), whereas for the left side, it reached 80.00% (16/20) (P = .289). Notably, in the combined pathway with ACTH stimulation, the success rate on the right side was significantly higher at 92.85% (39/42) (P = .503), compared to our center's bilateral antecubital vein pathway which achieved a success rate of only 25.00%. Similarly, the success rate on the left side for our center's simultaneous combined pathway after ACTH stimulation was 95.00% (40/42) (P < .001), surpassing both the bilateral antecubital vein pathway with an 80.00% success rate and the left side success rate via the combined pathway at 67.30%.
3.2. The success rate of AVS in previous centers by meta‐analysis
3.3. Inclusion and exclusion criteria
3.3.1. Study selection
The included studies consisted of retrospective or randomized clinical trials that evaluated the efficacy of AVS using bilateral antecubital vein versus bilateral femoral vein pathway in patients diagnosed with PA. Language was restricted to Chinese and English, and only human studies were considered. No limitations were imposed on study size or type. Excluded publications encompassed review articles, reviews, and studies lacking a certain degree of relevance. Articles meeting the following inclusion criteria were included in the meta‐analysis:
The study design included either a randomized controlled trial or a retrospective study.
Research subjects: The study enrolled patients diagnosed with PA, all meeting the diagnostic criteria outlined in the American Endocrine Society guidelines [1]. No limitations were imposed based on patient age, gender, or disease duration.
The intervention options for AVS included either the femoral vein or the antecubital vein.
This study incorporates research examining AVS employing either the femoral vein or the antecubital vein. The included studies comprise a systematic review/meta‐analysis rooted in randomized controlled trials (RCTs).
Exclusion Criteria: This study's exclusion criteria encompassed: (1) Conference abstracts; (2) Systematic reviews in the planning stage or unfinished; (3) Duplicate publications; (4) Reviews; (5) Studies lacking primary outcome indicators; (6) Studies with inaccessible full texts.
3.3.2. Screening
A search strategy plan was devised following the PICOS principle, 14 defined as: P(population): Patients diagnosed with PA; I(intervention): Bilateral AVS performed via femoral vein cannulation or antecubital vein cannulation; C(Comparison): Comparison between femoral vein and antecubital vein cannulation for bilateral AVS; O(Outcome): Proportion of cases achieving SI ≥ 2 using distinct veins to cannulate the left and right adrenal glands; S(Study design): no limitations. Initially, a systematic search was performed across English databases including Embase, Cochrane Library, PubMed, Web of Science, and Chinese databases CNKI and Wanfang Data. This search encompassed studies from database inception to May 2023, using keywords and related terms encompassing AVS, PA, forearm vein, catheter, and selectivity index (as detailed in Table 2). Identified studies were compiled into an EndNote file, duplicates were eliminated, and titles/abstracts were screened. Subjects not involving AVS, femoral vein cannulation, or forearm vein cannulation for both left and right sides in individuals with PA were excluded from the analysis of success rate. Subsequently, the remaining studies were scrutinized for pertinent information.
TABLE 2.
Search strategy for database PubMed, Embase and web of science.
| Database | Search strategy |
|---|---|
| PubMed |
#1 “Hyperaldosteronism” [Mesh] OR “Adrenal Vein Sampling” [All Fields] OR “AVS” [All Fields] #2 “Selectivity index” [All Fields] OR“SI” [All Fields] #3 “Catheterization” [All Fields] OR “Catheter” [All Fields] #4 “Forearm Vein” [All Fields] OR “Cubital Vein” [All Fields] #5 #2 OR #3 OR #4 #6 #1 AND #5 |
| Embase |
#1‘adrenal vein sampling’/exp OR ‘hyperaldosteronism’/exp #2‘selectivity index’/exp #3 ‘catheterization’/exp OR ‘catheter’/exp #4 ‘forearm vein’/exp OR ‘cubital vein’/exp #5 #2 OR #3 OR #4 #6 #1 AND #5 |
| Web of Science |
#1 (ALL = (Adrenal vein sampling)) OR ALL = (primary aldosteronism) #2 ALL = (Selectivity index) #3 ALL = (Catheterization) #4 ALL = (Forearm Vein)) OR ALL = (Cubital Vein) #5 #2 OR #3 OR #4 #6 #1 AND #5 |
3.4. The result of meta‐analysis
3.4.1. Screening results
Initially, 571 relevant studies were acquired. After reviewing their titles, abstracts, and full texts, 15 studies met the criteria for inclusion. Of these, nine articles explored AVS through bilateral femoral vein pathways without ACTH stimulation. 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 Additionally, there were six articles examining the femoral vein pathway with ACTH stimulation 18 , 19 , 21 , 22 , 23 , 24 and five articles focused on bilateral antecubital vein. 9 , 25 , 26 , 27 , 28 The process of study screening is depicted in Figure 1.
FIGURE 1.
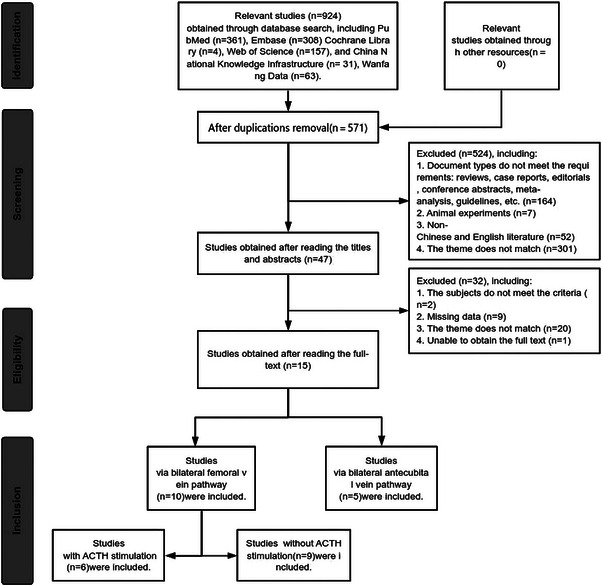
Schematic diagram of the study operation.
3.4.2. Characteristics of included studies
Among the 15 studies 9 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 included in this process, 11 studies were in English 9 , 15 , 16 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 and five studies were in Chinese. 17 , 26 , 27 , 28 These studies were published between 2001 and 2022, and their characteristics are presented in Table 3 for this meta‐analysis.
TABLE 3.
Characteristics of the selected studies for the meta‐analysis.
| Study | Country | Total | Pathway | ACTH | SI |
|---|---|---|---|---|---|
| Vonend O et al., 2011 15 | Germany | 553 | Femoral vein | Without | 2 |
| Graham UM et al., 2012 16 | UK | 100 | Femoral vein | Without | 2 |
| Li HY et al., 2017 17 | China | 50 | Femoral vein | Without | 1.5 |
| Mailhot JP et al., 2015 18 | Canada | 160 | Femoral vein | Both a | 2, 5 b |
| Harvey A et al., 2006 19 | Canada | 60 | Femoral vein | Both | 3, 5 |
| Rossi GP et al., 2001 20 | Italy | 104 | Femoral vein | Without | 1.1 |
| Yatabe M et al., 2020 21 | Japan | 185 | Femoral vein | Both | 2, 5 |
| Chee NYN et al., 2020 22 | Australia | 201 | Femoral vein | Both | 2, 3 |
| Liu W et al., 2021 23 | China | 95 | Femoral vein | Both | 2, 3 |
| Dream S et al., 2022 24 | USA | 101 | Femoral vein | With | 3 |
| X Jiang et al., 2017 9 | China | 194 | Antecubital vein | Without | 3 |
| Xu J et al., 2017 25 | China | 48 | Antecubital vein | Without | 2 |
| Liu J et al., 2017 26 | China | 50 | Antecubital vein | Without | 2 |
| Dong H et al., 2016 27 | China | 50 | Antecubital vein | Without | 3 |
| Fang Z et al., 2020 28 | China | 80 | Antecubital vein | Without | 2 |
The research had both the AVS with ACTH and the AVS without ACTH, so it is included in two groups of Meta‐analysis.
The former value is the SI boundary value without ACTH stimulus, and the latter is the SI boundary value under ACTH stimulus.
3.4.3. Forest plots
This study encompassed a total of 15 studies for the Meta‐analysis of single‐group rates. The criteria for conversion were selected based on the rate distribution across all original studies. If the original data adheres to both np and n(1 − p) ≥ 5 (where n was the sample size, and p was the incidence rate), indicating a close approximation to a normal distribution in the sampling of p, no conversion was required, allowing for risk difference (RD) calculation. Alternatively, if this criterion is not met, the odds ratio (OR) calculation was utilized, followed by logarithmic transformation: P = OR/(1+OR). In this study, only the right‐sided success rate of the femoral pathway met the criteria for the use of RD. As depicted in Figure 2, the success rate of AVS on the right side of the femoral vein pathway was 51.00% [.49–.54], while the success rate on the left side was calculated to be 68.45% [.6540–.7143]. Similarly, Figure 3 illustrated that the success rate on the right side in the included studies was 90.68% [.8744–.9315], whereas the success rate on the left side was reported as 94.44% [.9145–.9643]. Additionally, Figure 4 showcased the success rate of AVS via femoral vein pathway with ACTH stimulation, demonstrating a rate of 78.16% [.7455–.8138] on the right side and 94.98% [.9269–.9658] on the left side.
FIGURE 2.
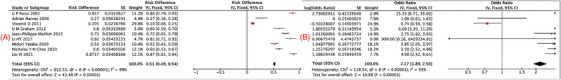
Forest plot: nine articles implement AVS via femoral vein pathway without ACTH A: Right success rate; B: Left success rate.
FIGURE 3.

Forest plot: five articles implement AVS via antecubital vein pathway without ACTH A: Right success rate; B: Left success rate.
FIGURE 4.

Forest plot: six articles implement AVS via femoral vein pathway with ACTH A: Right success rate; B: Left success rate.
4. SUMMARIZE
Figure 5 illustrates the different success rates of AVS obtained from our center and previous researches. To summarize, our center's simultaneous use of the antecubital vein combined with the femoral vein pathway, along with ACTH stimulation, achieved the highest success rate on the right side (92.85%). This rate significantly out performed both our center's bilateral antecubital vein pathway (P < .001) and the bilateral femoral vein pathway reported in previous studies (51.00%) (P < .001). The simultaneous combined pathway of our center on the left side achieved an impressively high success rate of 95.00% with ACTH stimulation, closely resembling the success rates reported in studies for bilateral femoral vein pathway with ACTH stimulation (94.98%). These findings demonstrate a superior success rate compared to the bilateral antecubital vein pathway observed in our center (25%) and the bilateral femoral vein pathway reported in previous studies (68.45%). Therefore, these results suggest that the femoral vein pathway is more favorable for locating the right adrenal vein than the antecubital vein pathway, resulting in a significantly higher success rate (the early antecubital vein pathway in our center had only achieved a 25% success rate), with statistical significance. The left adrenal vein can be more readily accessed through the antecubital vein pathway compared to the femoral vein pathway, albeit with a slightly lower SI. Our center's antecubital vein pathway on the left side demonstrates a success rate of 70.83% (51/72), marginally surpassing the reported success rate of bilateral femoral vein pathways in previous studies (68.45%). This suggests that although the antecubital vein pathway provides easier anatomical access to the left adrenal vein, it results in higher dilution compared to the femoral vein pathway, thereby necessitating ACTH stimulation to achieve a higher success rate.
FIGURE 5.
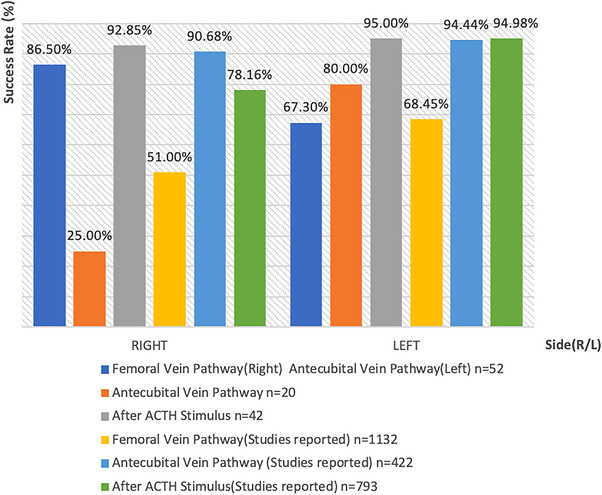
The success rate of AVS via different pathways (revised).
5. DISCUSSION
In this study, we conducted a comparative analysis of the success rates of right and left AVS across various approaches. For the right side, the combined pathway following ACTH stimulation exhibited a significantly higher efficacy compared to both the early bilateral antecubital pathway in our center and the bilateral femoral pathway documented in the literature, thus establishing it as the most successful approach within our research study. Regarding the left side, our combined pathway also exhibited the highest success rate following ACTH stimulation, aligning well with previous literature on both bilateral antecubital and bilateral femoral pathways.
Presently, the utilization of AVS is constrained owing to its comparatively modest success rates (ranging from 10.5% to 87.3%, as indicated by relevant studies). 15 , 18 , 29 Achieving accurate cannulation for effective AVS presents a substantial technical hurdle, substantiated by multiple centers reporting success rates below 50%. 15 , 19 The intricate anatomical structure of the adrenal vein complicates catheter insertion, particularly on the right side. Most research centers implement AVS based on experience using unlateral femoral pathway, but the right adrenal vein is typically smaller and shorter than the left side, frequently joining the inferior vena cava directly at an acute angle. Approximately 10%–20% of cases involve the right adrenal vein merging with the accessory hepatic vein before joining the inferior vena cava at an acute angle. 10 Consequently, considering the predominant anatomical configuration where the right adrenal vein converges into the inferior vena cava at an acute angle, it has been proposed by a particular institution that obtaining blood samples from the right adrenal vein for AVS through the antecubital vein pathway may be more appropriate. 30 According to the findings of our study, the success rate of right adrenal vein cannulation through the antecubital pathway was only 25.00% in the early stage. In contrast, using the femoral pathway resulted in a success rate of 86.50% without ACTH stimulation and 92.85% with ACTH stimulation, suggesting that performing right adrenal vein cannulation via the femoral pathway is considerably facile. Currently, there are approximately five studies available in China on the cannulation of AVS through the bilateral antecubital vein 9 , 25 , 26 , 27 , 28 while no relevant research has been conducted in other countries. The success rates for the bilateral antecubital vein pathway in the meta‐analysis surpass 90% for both left and right sides of AVS. However, in our initial attempt, the success rate of AVS via the antecubital vein pathway on the right side was merely 25.00%. These 20 cases can be attributed to early operations, which demonstrate a significant correlation with the operator's level of expertise. However, subsequent modifications to the femoral vein pathway significantly enhanced the success rate to 92.85%. This suggests that novices face challenges when utilizing the antecubital vein pathway, and there is no apparent advantage in cannulating the right adrenal vein.
However, the left adrenal vein presents a superior option for implementing AVS through the antecubital vein pathway, with a success rate of 70.83% without ACTH stimulation and up to 95.00% after satisfactory ACTH stimulation, which is consistent with previous reports on left adrenal vein cannulation via the femoral pathway in literature. Furthermore, our combined approach enables the simultaneous cannulation of both adrenal veins. Due to the pulsatile nature of cortisol secretion during successive samplings, there is a possibility of temporal fluctuations in cortisol concentrations, which may potentially introduce artificial disparities between bilateral AVS. 3 To enhance the precision and dependability of AVS results, this study employed simultaneous catheterization and sampling of bilateral adrenal veins to counterbalance the impact of fluctuations in cortisol concentration over time. The schematic diagram of the left and right AVS angiography in our center is shown in Figure 6. To ensure catheter stability throughout, it is crucial to verify its position using a small amount of contrast agent before and after sampling. Figure 7 depicts the simultaneous blood collection process during AVS conducted at our center.
FIGURE 6.
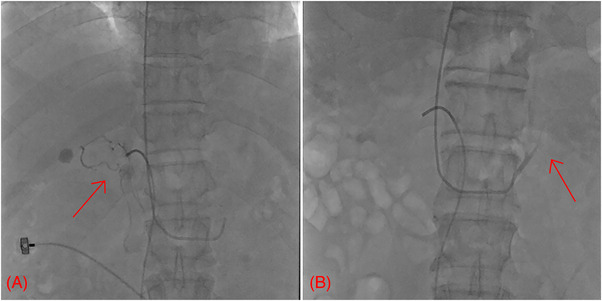
The representative angiography of bilateral adrenal vein. A: Right adrenal vein; B: Left adrenal vein.
FIGURE 7.
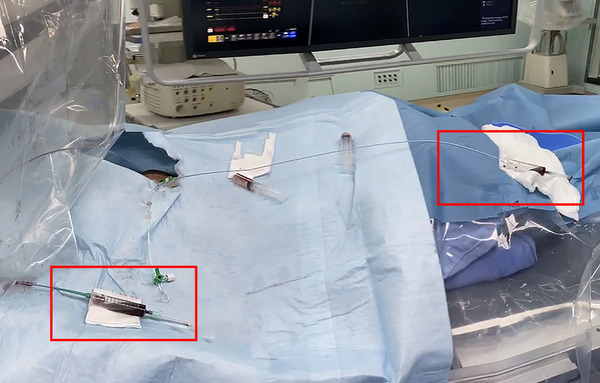
The schematic diagram of AVS procedure implemented in our center.
The left adrenal vein is frequently connected to the inferior phrenic vein prior to its entry into the left renal vein; therefore, it is imperative to guide the catheter towards the opening of the left adrenal vein, away from the opening of the inferior phrenic vein, in order to prevent dilution of cortisol concentration. The data from this study specifically focus on the advancement of the left catheter to reach the opening of the subphrenic vein, while data concerning further catheter advancement to a more distal location (microcatheter superselection) are addressed in another study. The present study demonstrated that the antecubital vein pathway provided relatively easy access to the left adrenal vein; however, its SI was slightly lower compared to the femoral vein pathway. This suggests that although anatomically more accessible for reaching the left adrenal vein, the antecubital vein pathway exhibited higher dilution than the femoral vein pathway, necessitating ACTH stimulation to achieve a higher success rate.
Among the AVS performed in our center, vascular dissection was occurred in 2 subjects during catheterization. One of subject had transient pain and transient retention of contrast medium, and both were disappeared after operation; the other subject only had transient retention of contrast medium, and it also disappeared after operation. In addition, bruising and swelling were observed at the site of inguinal puncture, accompanied by pain in another two subjects, no pseudoaneurysm was revealed by ultrasonography, and the mass was significantly reduced after one month of follow‐up. The rest of all the subjects had no related complications during the operation, and the basic vital signs such as blood pressure and oxygen saturation were within the normal range after the operation.
Controversy persists regarding the intubation of bilateral adrenal glands, as certain data suggest that performing bilateral AVS may potentially increase the risk of adrenal venous spasm, thrombosis, and hematoma. This elevated risk could arise from potential catheter obstruction within the blood vessels or cavities during contralateral vein cannulation attempts. Consequently, surgeons often prioritize initial placement of the challenging right adrenal vein followed by addressing the more accessible left adrenal vein. The technique of simultaneous intubation effectively minimizes the temporal discrepancy between both sides and significantly reduces the duration. Moreover, surgeons strive to optimize the utilization of natural blood outflow instead of employing negative pressure suction, thereby minimizing potential damage to veins. Reports suggest a potential risk of venous dissection during AVS. This risk is contingent upon the proficiency and expertise of the interventionalist performing the procedure, and exhibits notable correlation with both the frequency of procedures conducted by each interventionalist and their respective complication rates. There exists an inverse correlation. 11 Our center's surgeons have collectively performed nearly 10 000 coronary interventions. There are no relevant complications were observed during the procedures. Postsurgery, patients exhibited consistent and stable basic vital signs, including blood pressure and blood oxygen saturation. Additionally, no associated complications were observed during the follow‐up period.
This study had two limitations: Firstly, the paucity of studies investigating AVS via intravenous access in the bilateral antecubital vein pathway and the relatively limited number of clinically performed surgeries constrained a comprehensive exploration of the benefits and incidence of adverse events associated with the bilateral antecubital vein pathway. Secondly, the absence of a control group utilizing the femoral vein pathway to the left adrenal vein in our center limited comparisons to traditional studies using the femoral vein pathway.
The findings of this study demonstrate that the antecubital vein pathway provides convenient access to the left adrenal vein, while resulting in a relatively lower success rate without ACTH stimulation. Similarly, the femoral vein pathway also exhibits an increased success rate, enabling synchronous sampling from both adrenal veins. Currently, no center has made attempts to utilize the combined antecubital vein and femoral vein pathway for AVS procedures. Previous studies have demonstrated that the success rate of simultaneous AVS using this combined pathway is significantly higher compared to utilizing either the antecubital or femoral veins alone in other centers. Consequently, performing bilateral AVS simultaneously through the antecubital vein and femoral vein pathway could enhance short‐term AVS success rates and expedite the learning curve (see Supporting Information).
AUTHOR CONTRIBUTIONS
Jiaqi Liu: Formal analysis; resources and writing original draft. Shuai Shao: Data curation and writing original draft. Qiuli Wang: Resources and supervision. Zhiping Zhang: Resources. Xiaoying Ding: Funding acquisition and resources. Li Zhao: Funding acquisition and resources. Jinliang Wang: Validation. Xiaohong Ji: Data curation. Qiuyan Dai: Writing review & editing. Mingli Du: Conceptualization and writing review & editing. Zhi Zhang: Conceptualization; methodology and writing review & editing.
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest.
Supporting information
How to perform bilateral AVS simultaneously through the antecubital vein and femoral vein pathway.
ACKNOWLEDGMENTS
The authors thank Li Li, Department of Nursing, Shanghai General Hospital, for providing technical support. This study was funded by the National Key Research and Development Program of China (2021YFC2501600, 2021YFC2501601), and the National Natural Science Foundation of China (no. 82270536).
Liu J, Shao S, Wang Q, et al. Antecubital vein combined with femoral vein pathway could shorten the learning curve of simultaneous bilateral adrenal vein sampling. J Clin Hypertens. 2024;26:635–644. 10.1111/jch.14828
Jiaqi Liu, Shuai Shao, and Qiuli Wang are co‐first authors.
Contributor Information
Mingli Du, Email: shikareely@163.com.
Zhi Zhang, Email: zhi.zhang@shgh.cn.
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1. Funder JW, Carey RM, Mantero F, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(5):1889‐1916. [DOI] [PubMed] [Google Scholar]
- 2. Wu J, Lu AD, Zhang LP, et al. Study of clinical outcome and prognosis in pediatric core binding factor‐acute myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi. 2019;40(1):52‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rossi GP, Auchus RJ, Brown M, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63(1):151‐160. [DOI] [PubMed] [Google Scholar]
- 4. Mulatero P, Bertello C, Rossato D, et al. Roles of clinical criteria, computed tomography scan, and adrenal vein sampling in differential diagnosis of primary aldosteronism subtypes. J Clin Endocrinol Metab. 2008;93(4):1366‐1371. [DOI] [PubMed] [Google Scholar]
- 5. Lau JH, Sze WC, Reznek RH, et al. A prospective evaluation of postural stimulation testing, computed tomography and adrenal vein sampling in the differential diagnosis of primary aldosteronism. Clin Endocrinol (Oxf). 2012;76(2):182‐188. [DOI] [PubMed] [Google Scholar]
- 6. Nomura K, Kusakabe K, Maki M, et al. Iodomethylnorcholesterol uptake in an aldosteronoma shown by dexamethasone‐suppression scintigraphy—relationship to adenoma size and functional‐activity. J Clin Endocr Metab. 1990;71(4):825‐830. [DOI] [PubMed] [Google Scholar]
- 7. Rossi GP. Primary aldosteronism: JACC state‐of‐the‐art review. J Am Coll Cardiol. 2019;74(22):2799‐2811. [DOI] [PubMed] [Google Scholar]
- 8. Rossi GP, Bernini G, Caliumi C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48(11):2293‐2300. [DOI] [PubMed] [Google Scholar]
- 9. Jiang X, Dong H, Peng M, et al. A novel method of adrenal venous sampling via an antecubital approach. Cardiovasc Intervent Radiol. 2017;40(3):388‐393. [DOI] [PubMed] [Google Scholar]
- 10. Rossi GP, Pitter G, Bernante P, et al. Adrenal vein sampling for primary aldosteronism: the assessment of selectivity and lateralization of aldosterone excess baseline and after adrenocorticotropic hormone (ACTH) stimulation. J Hypertens. 2008;26(5):989‐997. [DOI] [PubMed] [Google Scholar]
- 11. Rossi GP, Barisa M, Allolio B, et al. The adrenal vein sampling international study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012;97(5):1606‐1614. [DOI] [PubMed] [Google Scholar]
- 12. Lupi A, Battistel M, Barbiero G, et al. Simultaneous bilateral adrenal vein sampling for primary aldosteronism: useful tips to make it simple and safe. Eur Radiol. 2019;29(11):6330‐6335. [DOI] [PubMed] [Google Scholar]
- 13. Wolley M, Thuzar M, Stowasser M. Controversies and advances in adrenal venous sampling in the diagnostic workup of primary aldosteronism. Best Pract Res Clin Endocrinol Metab. 2020;34(3):101400. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JP, Thompson SG, Deeks JJ, et al. Measuring incon‐sistency in meta‐analyses. BMJ. 2003;327(7414):557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vonend O, Ockenfels N, Gao X, et al. Adrenal venous sampling: evaluation of the German Conn's registry. Hypertension. 2011;57(5):990‐995. [DOI] [PubMed] [Google Scholar]
- 16. Graham UM, Ellis PK, Hunter SJ, et al. 100 cases of primary aldosteronism: careful choice of patients for surgery using adrenal venous sampling and CT imaging results in excellent blood pressure and potassium outcomes. Clin Endocrinol (Oxf). 2012;76(1):26‐32. [DOI] [PubMed] [Google Scholar]
- 17. Li HY, Li P, Shen SM, et al. Role of adrenal vein sampling in differential diagnosis of primary aldosteronism subtypes. Zhonghua Yi Xue Za Zhi. 2017;97(42):3291‐3296. [DOI] [PubMed] [Google Scholar]
- 18. Mailhot JP, Traistaru M, Soulez G, et al. Adrenal vein sampling in primary aldosteronism: sensitivity and specificity of basal adrenal vein to peripheral vein cortisol and aldosterone ratios to confirm catheterization of the adrenal vein. Radiology. 2015;277(3):887‐894. [DOI] [PubMed] [Google Scholar]
- 19. Harvey A, Kline G, Pasieka JL. Adrenal venous sampling in primary hyperaldosteronism: comparison of radiographic with biochemical success and the clinical decision‐making with “less than ideal” testing. Surgery. 2006;140(6):847‐855. [DOI] [PubMed] [Google Scholar]
- 20. Rossi GP, Sacchetto A, Chiesura‐Corona M, et al. Identification of the etiology of primary aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab. 2001;86(3):1083‐1090. [DOI] [PubMed] [Google Scholar]
- 21. Yatabe M, Bokuda K, Yamashita K, et al. Cosyntropin stimulation in adrenal vein sampling improves the judgment of successful adrenal vein catheterization and outcome prediction for primary aldosteronism. Hypertens Res. 2020;43(10):1105‐1112. [DOI] [PubMed] [Google Scholar]
- 22. Chee NYN, Abdul‐Wahab A, Libianto R, et al. Utility of adrenocorticotropic hormone in adrenal vein sampling despite the occurrence of discordant lateralization. Clin Endocrinol (Oxf). 2020;93(4):394‐403. [DOI] [PubMed] [Google Scholar]
- 23. Liu W, Zhang J, Yang Y, et al. Effect of adrenocorticotropic hormone stimulation during simultaneous bilateral adrenal vein sampling in primary aldosteronism. Horm Metab Res. 2021;53(6):364‐370. [DOI] [PubMed] [Google Scholar]
- 24. Dream S, Park S, Yen TW, et al. Utility of epinephrine levels in determining adrenal vein cannulation during adrenal venous sampling for primary aldosteronism. Endocr Pract. 2022;28(3):276‐281. [DOI] [PubMed] [Google Scholar]
- 25. Xu J, Sheng C, Li M, et al. A feasibility study on percutaneous forearm vein access for adrenal venous sampling. J Hum Hypertens. 2017;31(1):76‐78. [DOI] [PubMed] [Google Scholar]
- 26. Liu J, Gu A, Xu J, et al. Comparison of adrenal venous sampling via elbow vein and femoral vein. Shanghai Yi Xue. 2017;40(04):210‐213. [Google Scholar]
- 27. Dong H, Jiang X, Peng M, et al. The safety and feasibility study of adrenal vein sampling via median cubital vein: the first report of 50 cases. Zhonghua Gao Xue Ya Za Zhi. 2016;24(02):158‐162. [Google Scholar]
- 28. Fang Z, Cai H, Lin J, et al. 80 patients with Primary Aldosteronism are analyzed and operated by the results of bilateral adrenal vein via the forearm vein. Zhonghua Gao Xue Ya Za Zhi. 2020;28(10):965‐970. [Google Scholar]
- 29. Lethielleux G, Amar L, Raynaud A, et al. Influence of diagnostic criteria on the interpretation of adrenal vein sampling. Hypertension. 2015;65(4):849‐854. [DOI] [PubMed] [Google Scholar]
- 30. Daunt N. Adrenal vein sampling: how to make it quick, easy, and successful. Radiographics. 2005;25(1):S143‐S158. [DOI] [PubMed] [Google Scholar]
- 31. Steichen O, Amar L. Diagnostic criteria for adrenal venous sampling. Curr Opin Endocrinol Diabetes Obes. 2016;23(3):218‐224. [DOI] [PubMed] [Google Scholar]
- 32. Webb R, Mathur A, Chang R, et al. What is the best criterion for the interpretation of adrenal vein sample results in patients with primary hyperaldosteronism? Ann Surg Oncol. 2012;19(6):1881‐1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
How to perform bilateral AVS simultaneously through the antecubital vein and femoral vein pathway.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


