Traditionally the extent of patients' involvement in medical decision making has been minimal. This has been true at both the micro level of the patient consultation with a doctor and the macro level of planning and developing healthcare services. Since 1989, however, greater involvement of patients and the community in these processes has been advocated.1–5 In principle, the elicitation of patients' and the community's values represents a big step forward in terms of enhancing the benefits from the provision of health care. For the exercise to be worth while, however, the information obtained must be useful and scientifically defensible.6 During the 1990s, conjoint analysis was developed to elicit patients' and the community's views on health care.
Summary points
Conjoint analysis is a rigorous method of eliciting preferences
It allows estimation of the relative importance of different aspects of care, the trade-offs between these aspects, and the total satisfaction or utility that respondents derive from healthcare services
The technique can help with decision making for some of the issues facing the NHS
Though further applications of conjoint analysis are encouraged, methodological issues need further consideration
Methods
This paper explains conjoint analysis, provides examples of applications in health care which were obtained from a systematic review of databases between 1989 and 1999 (Medline, Embase, HealthSTAR, PsychLIT, EconLIT), and uses a study in orthodontic care to show the uses and pitfalls of the technique.
Conjoint analysis
The survey method of data collection and analysis known as conjoint analysis was developed in mathematical psychologyand has a strong theoretical basis.7–9 It has been successfully used in market research,10transport economics,11 and environmental economics12,13 and was recommended to the UK Treasury for valuing quality in the provision of public services.14 Within these areas it has been well received by policymakers.12,14 The technique is gaining widespread use in health care and has been applied successfully in several areas, including eliciting patients' and the community's preferences in the delivery of health services15–22; establishing consultants' preferences in priority setting23; developing outcome measures24,25; determining optimal treatments for patients26,27; evaluating alternatives within randomised controlled trials28,29; and establishing patients' preferences in the doctor-patient relationship.30,31
The technique is based on the premises that any good or service can be described by its characteristics (or attributes) and that the extent to which an individual values a good or service depends on the levels of these characteristics. The technique can be used to
Show how people are willing to trade between characteristics; this is useful when deciding on the optimal way to provide a service within limited resources16,20–22
Produce overall benefit scores for alternative ways of providing health care; this allows the ranking of health services against one another when setting priorities21,22
Estimate the relative importance of different characteristics of a service; this allows the policymaker to observe the individual impact of each characteristic on overall benefit15–31
Estimate whether an attribute is important; this may be particularly useful when assessing the outcomes of trials. Trials generally include more than one outcome measure. Without further information it is not possible to determine whether these different outcome measures are important to patients.28,29
Undertaking a conjoint analysis study
Stage 1: Identifying the characteristics
The characteristics can be identified by various methods. If a policy question is being addressed, the characteristics will be predefined. For use alongside a randomised controlled trial, the characteristics may be defined by the different components of the arms of the trial.28,29 Where the characteristics are not predefined, literature reviews, group discussions, and individual interviews will be necessary.19
Stage 2: Assigning levels to the characteristics
Levels assigned to the characteristics may be cardinal (for example, waiting time, where two weeks is twice as long as one week), ordinal (for example, though “severe pain” is worse than “moderate pain,” we do not know by how much), or categorical (for example, where there is no natural ordering for specialist nurse, general practitioner, or consultant). Pragmatically, the levels must be plausible and actionable, thus encouraging respondents to take the exercise seriously.
Stage 3: Choice of scenarios
Scenarios are then drawn up that describe all possible service (or outcome) configurations given the characteristics and levels chosen. The number of scenarios increases with the number of characteristics and levels. Rarely can all the scenarios generated be included in the questionnaire, and experimental designs are used to reduce the number to a manageable level.32,33
Stage 4: Establishing preferences
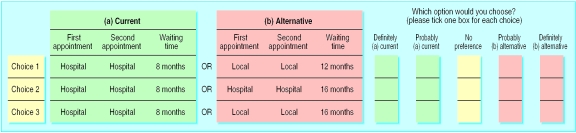
Preferences for scenarios included in the questionnaire are elicited by using one of three methods: ranking, rating, or discrete choices. With ranking, respondents are asked to list the scenarios in order of preference. This method has not as yet been used in health care. The rating method requires the respondents to assign a score, of say 1 to 5, to each of the scenarios.21,25 For the discrete choice method, respondents are presented with a number of choices and, for each, asked to choose their preferred one. Possible responses include stating that either A or B is preferred,15–31 or responding on a five point scale where 1 equals definitely prefer A and 5 equals definitely prefer B (see figure). Given that choices more closely resemble real life decisions, the discrete choice approach has been preferred in health care.
Stage 5: Data analysis
Regression techniques are used to analyse responses. The appropriate method is determined by the type of data collected.34 For discrete choice data, a benefit function is estimated, which can be specified as
ΔB=β1X1+β2X2+β3X3+. . .+βnX1
where ΔB is the change in benefit in moving from service A to B, Xj (j=1, 2, . . ., n) are the differences in the attribute levels between A and B, and βj (j=1, 2, . . ., n) are the coefficients of the model to be estimated.
An application to orthodontic services
This application considers the trade-offs that individuals were willing to make between location of treatment and waiting time in the provision of orthodontic services.
Subjects and methods
A total of 160 patients attending three orthodontic clinics in the Grampian area of Scotland were asked to take part in the study.
The policy question identified the characteristics to be included in the conjoint analysis study. These and their levels are shown in table 1, together with their coding for the regression analysis. Sixteen scenarios were possible. Fifteen discrete choices were constructed by comparing the current service to all alternatives. Each respondent was presented with the 15 choices and asked, for each, which they preferred (see figure).
Table 1.
Attributes and levels included in conjoint analysis study
| Attributes | Levels | Regression coding |
|---|---|---|
| Waiting time (for first appointment) (WAIT) | 4 months, 8 months, 12 months, 16 months | 4, 8, 12, 16 |
| Location of first appointment (for diagnosis) (LOC1) | Hospital, local | 0=local, 1=hospital |
| Location of second appointment (and subsequent appointments for fixing the appliance) (LOC2) | Hospital, local | 0=local, 1=hospital |
A check for internal consistency was included and dominant preferences (respondents not willing to trade a reduction in one attribute for an improvement in another) were identified. Respondents who were inconsistent or had dominant preferences were dropped from further analysis.
The following benefit equation was estimated for consistent traders:
ΔB=β1LOC1+β2LOC2+β3WAIT
where ΔB is the change in benefit in moving from the current service to an alternative and the explanatory variables are the difference in the attributes of the two clinics, as defined in table 1. Given the nature of the dependent variable, the random effects ordered probit model was used to analyse the data.34,35
Coefficients β1 to β3 show the relative importance of the different attributes, with the associated P statistic indicating whether the attribute has a statistically significant effect on choices. When interpreting these coefficients, it is important to be aware of the unit of measurement: β1and β2 show the change in benefit for a unit change in location from central to local, and β3 for a week's change in waiting time. β1/β3 indicates how much waiting time individuals are willing to give up to have their first appointment at a local clinic, and β2/β3 shows how much waiting time an individual would be willing to give up to have the second (and all subsequent appointments) at the local clinic. Benefit scores were estimated for different ways of providing orthodontic services.
Results
In all, 157 questionnaires were completed. Dropping inconsistent responders, those with dominant preferences, and missing values left 73 individuals and 1081 observations in the sample.
Table 2 presents the regression results for this group. The positive and significant signs on both location coefficients show that respondents prefer a local clinic to a hospital. Moving from a hospital clinic to a local clinic will increase benefit by 0.77 for the first appointment and 0.91 for the second appointment. The negative and significant sign of waiting time indicates that the higher the waiting time, the lower the benefit. The negative coefficient of 0.59 means that a unit increase in waiting time (for instance, from four months to five months) will reduce the benefit score by 0.59. Individuals are willing to wait an extra 1.3 months (0.77/0.59) to have a local clinic for their first appointment and an extra 1.5 months (0.91/0.59) to have a local clinic for their second appointment. From the equation used in the study, the benefit in moving from the current situation to having local first and second appointments and waiting 12 months was estimated to be −2.28. (Benefit scores were estimated for all the choice situations presented to individuals in the questionnaire; more detailed results are available on the BMJ website.) Generally, positive benefit values indicate an improvement over the current service and negative values indicate that patients would be less satisfied with that service configuration. Attempts should be made to reach the best configuration within available resources.
Table 2.
Results from regression analysis (1081 observations in 73 individuals)
| Variable | Coefficient | P value |
|---|---|---|
| Waiting time* | −0.59 | <0.001 |
| Location of first appointment (0=local, 1=central) | −0.77 | <0.001 |
| Location of second appointment (0=local, 1=central) | −0.91 | <0.001 |
| Log likelihood | −1220 | |
| χ2 | 319.49 | |
| McFadden R2 | 0.12 |
Extra months willing to wait for a local first appointment=1.3; extra months willing to wait for a local second appointment=1.54.
Other applications
The orthodontic study shows one way in which conjoint analysis can be applied, but the potential for the technique is much broader. Consider the issues faced by Dumfries and Galloway Health Board, recently highlighted in the BMJ.36This region faces problems common in the NHS. These relate to issues of new build, optimal information systems, relations between central and periphery hospitals, and patients' rising expectations. Conjoint analysis could be used to aid decision making within these areas. For example:
Do patients want more personal and familiar local hospital care, where the level of specialisation may be lower, or more specialised, centrally located services?22
On what basis should priority be given to competing new build projects?23
Although the technique can be applied to a wide range of policy questions within the NHS, several methodological issues remain. Some of these are outlined below within the context of the orthodontics study.
Methodological issues
In the orthodontics study, although the attributes were defined by the policy question, defining their levels was more difficult. Variations around the status quo were chosen in this study. In the only study appraising this issue, conjoint analysis has been shown to be relatively insensitive to characteristic levels (M Ryan and S Wordsworth, International Health Economics Association conference, 1999).
Secondly, the attributes and levels gave rise to 16 possible scenarios and, from these, 120 possible choices. Obviously it would not be possible to ask individuals their preferences among 120 choices, so the current situation was compared with the remaining 15 scenarios. An alternative approach is to randomly pair the 16 scenarios into choices.23 Work is needed to assess the sensitivity of results to the method of setting discrete choices.
Thirdly, in data analysis, there is the issue of what to do with inconsistent responders and those exhibiting dominant preferences. For simplicity, inconsistent responders and “non-traders” were dropped in the application to orthodontic services, following the procedure in previous applications of conjoint analysis in health care. Future work, however, should consider the extent to which inconsistent responders are behaving rationally (and therefore should be included in the analysis) and should explore issues related to non-traders. The bias that exclusion may create in the results also needs considering.
Fourthly, there is a question of how to model the benefit function. In the orthodontics study, a linear additive relation was assumed. Research from outside health care has shown that alternatives to the linear additive model seldom result in a significantly better fit.37 Future work applying conjoint analysis in health care should explore this issue.
Conclusions
This paper proposes conjoint analysis as a rigorous survey technique for eliciting the views of patients and people in the community on health care. The application presented here, which was well received by policy- makers, shows the potential uses and pitfalls of the technique. Conjoint analysis has been successfully applied elsewhere in health care and has great potential as an instrument for establishing the preferences of patients and the community (as well as those of clinicians and policymakers). Though further applications of conjoint analysis are encouraged in the NHS, methodological issues arising from its use should continue to be considered.
Supplementary Material
Figure.
Example of conjoint analysis question
Acknowledgments
We are grateful to all respondents who completed questionnaires, to Dr Kate Dawson for help in setting up the study, and to health promotion assistants for their help in collecting the data.
Footnotes
Funding: Financial support from the Medical Research Council and the Chief Scientist Office of the Scottish Office Department of Health are acknowledged. The views expressed in the paper are those of the authors.
Competing interests: None declared.
A table comparing scenarios is available on the BMJ website
References
- 1.Secretaries of State for Health, Wales, Northern Ireland, and Scotland. Working for patients. London: HMSO; 1989. [Google Scholar]
- 2.NHS Management Executive. Local voices: the views of local people in purchasing for health. London: Department of Health; 1992. [Google Scholar]
- 3.Secretaries of State for Health, Wales, Northern Ireland, and Scotland. Promoting better health. London: HMSO; 1989. [Google Scholar]
- 4.Secretary of State for Health. The health of the nation. London: HMSO; 1989. [Google Scholar]
- 5.Scottish Office Department of Health. The patient's charter: what users think. Edinburgh: HMSO; 1992. [Google Scholar]
- 6.Cleary P. The increasing importance of patient surveys. BMJ. 1999;319:720–721. doi: 10.1136/bmj.319.7212.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luce D, Tukey J. Simultaneous conjoint measurement: a new type of fundamental measurement. J Math Psychol. 1964;1:1–27. [Google Scholar]
- 8.Anderson N. Functional measurement and psycho-physical judgement. Psychol Rev. 1977;77:153–170. doi: 10.1037/h0029064. [DOI] [PubMed] [Google Scholar]
- 9.McFadden D. Conditional logit analysis of qualitative choice behaviour. Berkeley, CA: University of California at Berkeley; 1973. . (Working paper No 199/BART 10.) [Google Scholar]
- 10.Cattin P, Wittink D. Commercial use of conjoint analysis: a survey. J Marketing. 1982;46:44–53. [Google Scholar]
- 11.[Conjoint analysis.] J Transport Econ Policy 1988;22(1).
- 12.Opaluch J, Swallow S, Weaver T, Wessells C, Wichelns D. Evaluating impacts from noxious facilities: including public preferences in current siting mechanisms. J Environ Econ Manage. 1993;24:41–59. [Google Scholar]
- 13.Adamowicz W, Louviere J, Williams M. Combining revealed preference and stated preference methods for valuing environmental amenities. J Environ Econ Manage. 1994;6:271–292. [Google Scholar]
- 14.Cave M, Burningham D, Buxton M, Hanney S, Pollitt C, Scanlan M, et al. The valuation of changes in quality in the public services. London: HMSO; 1993. [Google Scholar]
- 15.Bryan S, Buxton M, Sheldon R, Grant A. Magnetic resonance imaging for the investigation of knee injuries: an investigation of preference. Health Econ. 1998;7:595–604. doi: 10.1002/(sici)1099-1050(1998110)7:7<595::aid-hec381>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 16.Propper C. Contingent valuation of time spent on NHS waiting list. Econ J. 1991;100:193–199. [Google Scholar]
- 17.Propper C. The disutility of time spent on the United Kingdom's National Health Service waiting lists. J Hum Resources. 1995;30:677–700. [Google Scholar]
- 18.Ratcliffe J, Buxton M. Patients' preferences regarding the process and outcomes of life saving technology: an application of conjoint analysis to liver transplantation. Int J Technol Assess Health Care. 1999;15:340–351. [PubMed] [Google Scholar]
- 19.Ryan M. Using conjoint analysis to go beyond health outcomes: an application to in vitro fertilisation. Soc Sci Med. 1999;8:535–546. doi: 10.1016/s0277-9536(98)00374-8. [DOI] [PubMed] [Google Scholar]
- 20.Van der Pol M, Cairns J. Establishing preferences for blood transfusion support: an application of conjoint analysis. J Health Services Res Manage. 1998;3:70–76. doi: 10.1177/135581969800300203. [DOI] [PubMed] [Google Scholar]
- 21.Ryan M, McIntosh E, Shackley P. Using conjoint analysis to assess consumer preferences in primary care: an application to the patient health card. Health Expectations. 1998;1:117–129. doi: 10.1046/j.1369-6513.1998.00024.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ryan M, McIntosh E, Dean T, Old P. Trade-offs between location and waiting times in the provision of health care: the case of elective surgery on the Isle of Wight. J Public Health Med (in press). [DOI] [PubMed]
- 23.Farrar S, Ryan M, Ross D, Ludbrook A. Using discrete choice modelling in priority setting: an application to clinical service developments. Soc Sci Med. 2000;50:63–75. doi: 10.1016/s0277-9536(99)00268-3. [DOI] [PubMed] [Google Scholar]
- 24.Hakim Z, Pathak D. Modelling the EuroQol data: a comparison of discrete choice conjoint and conditional preference modelling. Health Econ. 1999;8:103–116. doi: 10.1002/(sici)1099-1050(199903)8:2<103::aid-hec393>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 25.Harwood R, Rogers A, Dickinson E, Ebrahim S. Measuring handicap: the London handicap scale, a new outcome measure for chronic disease. Qual Health Care. 1994;3:11–16. doi: 10.1136/qshc.3.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maas A, Stalpers L. Assessing utilities by means of conjoint measurement: an application in medical decision analysis. Med Decision Making. 1992;12:288–297. doi: 10.1177/0272989X9201200408. [DOI] [PubMed] [Google Scholar]
- 27.Verhoef C, Maas A, Stalpers L, Verbeek A, Wobbes T, Daal W. The feasibility of additive conjoint measurement in measuring utilities in breast cancer patients. Health Policy. 1991;17:39–50. [Google Scholar]
- 28.Ryan M, Hughes J. Using conjoint analysis to value surgical versus medical management of miscarriage. Health Econ. 1997;6:261–273. doi: 10.1002/(sici)1099-1050(199705)6:3<261::aid-hec262>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 29.San Miguel F, Ryan M, Mcintosh E. Applying conjoint analysis in economic evaluations: an application to menorrhagia. Appl Econ (in press).
- 30.Scott A, Vick S. Patients, doctors and contracts: an application of principal-agent theory to the doctor-patient relationship. Scot J Political Econ. 1999;46:111–134. [Google Scholar]
- 31.Vick S, Scott A. What makes a perfect agent? A pilot study of patients' preferences in the doctor patient relationship. J Health Econ. 1998;17:587–606. doi: 10.1016/s0167-6296(97)00035-0. [DOI] [PubMed] [Google Scholar]
- 32.Kocur G, Alder T, Hyman W, Aunet B. Guide to forecasting travel demand with direct utility assessment. Washington, DC: US Department of Transportation; 1982. [Google Scholar]
- 33.Bradley M. User's manual for the SPEED version 2.1. Stated preference experiment editor and designer. Hague: Hague Consulting Group; 1991. [Google Scholar]
- 34.Greene W. Econometric analysis. Englewood Cliffs, NJ: Prentice Hall; 1993. [Google Scholar]
- 35.Greene W. LIMDEP version 7.0. New York: Econometric Software; 1995. [Google Scholar]
- 36.Smith R. The NHS in Dumfries and Galloway: straining but optimistic. BMJ. 1999;319:1123–1127. doi: 10.1136/bmj.319.7217.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Emery D, Barron F. Axiomatic and numerical conjoint measurement: an evaluation of diagnostic efficacy. Psychometrika. 179;44:195–210. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.