Ulcerative conditions
Mouth ulcers are common and are usually due to trauma such as from ill fitting dentures, fractured teeth, or fillings. However, patients with an ulcer of over three weeks' duration should be referred for biopsy or other investigations to exclude malignancy (see previous article) or other serious conditions such as chronic infections.
Main systemic and iatrogenic causes of oral ulcers
| Microbial disease | Malignant neoplasms |
| • Herpetic stomatitis | Blood disorders |
| • Chickenpox | • Anaemia |
| • Herpes zoster | • Leukaemia |
| • Hand, foot, and mouth disease | • Neutropenia |
| • Herpangina | • Other white cell dyscrasias |
| • Infectious mononucleosis | Gastrointestinal disease |
| • HIV infection | • Coeliac disease |
| • Acute necrotising gingivitis | • Crohn's disease |
| • Tuberculosis | • Ulcerative colitis |
| • Syphilis | Rheumatoid diseases |
| • Fungal infections | • Lupus erythematosus |
| Cutaneous disease | • Behcet's syndrome |
| • Lichen planus | • Sweet's syndrome |
| • Pemphigus | • Reiter's disease |
| • Pemphigoid | Drugs |
| • Erythema multiforme | • Cytotoxic agents |
| • Dermatitis herpetiformis | • Nicorandil |
| • Linear IgA disease | • Others |
| • Epidermolysis bullosa | Radiotherapy |
| • Chronic ulcerative stomatitis | |
| • Other dermatoses |
Ulcers related to trauma usually resolve in about a week after removal of the cause and use of benzydamine hydrochloride 0.15% mouthwash or spray (Difflam) to provide symptomatic relief and chlorhexidine 0.2% aqueous mouthwash to maintain good oral hygiene.
• Patients with a mouth ulcer lasting over three weeks should be referred for biopsy or other investigations to exclude malignancy or other serious conditions
Recurrent aphthous stomatitis (aphthae, canker sores)
Recurrent aphthous stomatitis typically starts in childhood or adolescence with recurrent small, round, or ovoid ulcers with circumscribed margins, erythematous haloes, and yellow or grey floors. It affects at least 20% of the population, and its natural course is one of eventual remission. There are three main clinical types:
Minor aphthous ulcers (80% of all aphthae) are less than 5 mm in diameter and heal in 7-14 days
Major aphthous ulcers are large ulcers that heal slowly over weeks or months with scarring
Herpetiform ulcers are multiple pinpoint ulcers that heal within about a month.
Some cases have a familial and genetic basis, but most patients seem to be otherwise well. However, a minority have aetiological factors that can be identified, including stress, trauma, stopping smoking, menstruation, and food allergy.
Aphthae are also seen in haematinic deficiency (iron, folate, or vitamin B-12); coeliac disease; Crohn's disease; HIV infection, neutropenia, and other immunodeficiencies; Neumann's bipolar aphthosis, where genital ulcers may also be present; and Behcet's syndrome, where there may be genital, cutaneous, ocular, and other lesions. The mouth ulcers in Behcet's syndrome are often major aphthae with frequent episodes and long duration to healing.
In children aphthae also occur in periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis syndrome. This syndrome resolves spontaneously, and long term sequelae are rare. Corticosteroids are highly effective symptomatically; tonsillectomy and cimetidine treatment have been effective in some patients.
Diagnosis of aphthae is based on the patient's history and clinical features since specific tests are unavailable. A full blood picture (haemoglobin concentration, white cell count and differential, and red cell indices), iron studies, and possibly red cell folate and serum vitamin B-12 measurements and other investigations may help exclude systemic disorders, which should be suspected if there are features suggestive of a systemic background. Biopsy is rarely indicated.
Management—Predisposing factors should be identified and corrected. Chlorhexidine mouthwashes may help. Symptoms can often be controlled with hydrocortisone hemisuccinate pellets or triamcinolone acetonide in carboxymethyl cellulose paste four times daily, but more potent topical corticosteroids may be required. Systemic corticosteroids are best given by a specialist. Thalidomide is also effective but is rarely indicated.
• Patients with aphthae are usually otherwise healthy• Systemic diseases that should be excluded include Behcet's syndrome, gluten sensitive enteropathy, deficiencies of haematinics, and, occasionally, immunodeficiency• Recurrent aphthous stomatitis is a clinical diagnosis• Predisposing factors should be identified and corrected• Topical corticosteroids aid resolution of ulcers• In severe cases systemic immunomodulation may be needed
Malignant ulcers
Oral carcinoma may present as a solitary chronic ulceration (see previous article).
Mouth ulcers in systemic disease
Ulcers may be manifestations of disorders of skin, connective tissue, blood, or gastrointestinal tract.
The main skin disorders are lichen planus, pemphigus, pemphigoid, erythema multiforme, epidermolysis bullosa, and angina bullosa haemorrhagica (blood filled blisters that leave ulcerated areas after rupture). In view of the clinical consequences of pemphigus, accurate diagnosis of oral bullae is important, and referral for direct and indirect immunofluorescence of biopsy tissue is often indicated.
Drug induced mouth ulcers
Among the drugs that may be responsible for mouth ulcers are cytotoxic agents, antithyroid drugs, and nicorandil.
Non-ulcerative causes of oral soreness
Erythema migrans (benign migratory glossitis, geographic tongue)
This common condition of unknown aetiology, which affects about 10% of children and adults, is characterised by map-like red areas of atrophy of filiform tongue papillae in patterns that change even within hours. The tongue is often fissured. Lesions can cause soreness or may be asymptomatic.
Management—There is no reliably effective treatment, although some have reported efficacy for zinc supplements. Similar lesions may be seen in Reiter's syndrome and psoriasis.
Burning mouth syndrome (oral dysaesthesia, glossopyrosis, glossodynia)
This condition is common in people past middle age and is characterised by a persistent burning sensation in the tongue, usually bilaterally. The cause is unclear, but response to topical anaesthesia suggests it is a form of neuropathy. Discomfort is sometimes relieved by eating and drinking, in contrast to the pain from ulcerative lesions, which is typically aggravated by eating.
Causes of a complaint of burning mouth syndrome
| • Local | • Deficiency states |
| Candidiasis | Vitamin B |
| Erythema migrans | Folate |
| Lichen planus | Iron |
| • Psychogenic | • Diabetes mellitus |
| Cancerophobia | • Dry mouth |
| Depression | • Drugs (such as captopril) |
| Anxiety | • Denture problems |
| Hypochondriasis | • Parafunctional habits |
Organic causes of discomfort—such as erythema migrans, lichen planus, a deficiency glossitis (related to deficiency of iron, folate, or vitamin B-12), xerostomia, diabetes, and candidiasis— must be excluded, but these are only occasional causes. More often there is an underlying depression, monosymptomatic hypochondriasis, or anxiety about cancer or a sexually transmitted disease. Burning mouth syndrome is more common in Parkinson's disease.
Management—Reassurance and occasionally psychiatric consultation, vitamins, or antidepressants may be indicated, but they are not reliably effective.
• Erythema migrans commonly affects the tongue, there are usually no serious connotations, and there is no effective treatment• Burning mouth syndrome is common, affects mainly the tongue, and antidepressants may be indicated, though organic disease must first be excluded
Desquamative gingivitis
Widespread erythema, particularly if associated with soreness, is usually caused by desquamative gingivitis. This is fairly common and is seen almost exclusively in women over middle age (see earlier article).
Orofacial pain
Most orofacial pain is caused by
Local disease, especially dental, mainly a consequence of caries (see earlier article)
Psychogenic states
Neurological disorders (such as trigeminal neuralgia). Similar features are seen in the rare SUNCT syndrome (short lasting, unilateral, neuralgiform headache attacks with conjunctival injection and tearing)
Vascular disorders (such as migraine). Recent evidence suggests that chronic pain may occasionally be related to thrombosis or hypofibrinolysis causing small areas of jaw ischaemia and necrosis; this has been termed neuralgia-inducing cavitational necrosis
Referred pain (such as angina).
Psychogenic orofacial pain
This is an ill defined entity that includes burning mouth syndrome, atypical facial pain, atypical odontalgia, and the syndrome of oral complaints.
Causes of orofacial pain
| Local diseases | Neurological disorders |
| • Teeth and supporting tissues | • Trigeminal neuralgia |
| • Jaws | • Malignant neoplasms |
| • Maxillary antrum | • Multiple sclerosis |
| • Salivary glands | • Herpes zoster |
| • Eyes | • SUNCT syndrome |
| Psychogenic pain | Vascular disorders |
| • Atypical facial pain and other | • Migraine |
| oral symptoms associated with | • Migrainous neuralgia |
| anxiety or depression (such as | • Temporal arteritis (giant cell arteritis) |
| mandibular pain-dysfunction) | • Paroxysmal hemicrania |
| • Burning mouth syndrome | • Neuralgia-inducing cavitational osteonecrosis |
| Referred pain | |
| • Angina | |
| • Lesions in neck or chest | |
| (including lung cancer) |
The pain is often of a dull, boring, or burning type of ill defined location. Most patients are women who are middle aged or older. They typically have constant chronic discomfort or pain, rarely use analgesics, sleep undisturbed by pain, have consulted several clinicians, have no objective signs and have negative investigations, and have recent adverse life events such as bereavement or family illness and also multiple psychogenic related complaints.
Management—Attempts at relieving pain by restorative treatment, endodontia, or exodontia are usually unsuccessful. Many patients lack insight and will persist in blaming organic diseases for their pain. Some patients are depressed or hypochondriacal and may respond to fluoxetine or dosulepin hydrochloride. However, many refuse drugs or psychiatric help. Those who will respond invariably do so early in treatment.
Atypical odontalgia presents with pain and hypersensitive teeth typically indistinguishable from pulpitis or periodontitis but without detectable pathology. It is probably a variant of atypical facial pain and should be treated similarly.
Temporomandibular joint pain-dysfunction syndrome (myofascial pain-dysfunction syndrome, facial arthromyalgia)
This common disorder afflicts young women mainly. Symptoms are highly variable but characterised by
Recurrent clicking in the temporomandibular joint at any point of jaw movement, and there may be crepitus especially with lateral movements
Periods of limitation of jaw movement, with variable jaw deviation or locking but rarely severe trismus
Pain in the joint and surrounding muscles, which may be tender to palpation.
• Atypical facial pain and mandibular pain-dysfunction are common forms of orofacial pain• There is typically a poorly localised dull ache• Organic disease must be excluded• Antidepressants may be indicated
Patients with a night time habit of clenching or grinding the teeth (bruxism) may awake with joint pain which abates during the day. In people who clench or grind during working hours the symptoms tend to worsen towards evening and sometimes have a psychogenic basis.
Different aetiological factors that have been implicated include muscle overactivity (such as bruxism and clenching), disruption of the temporomandibular joint, and psychological stress (such as anxiety and stressful life events). Precipitating factors may include wide mouth opening, local trauma, nail biting, and emotional upset. However, there is rarely one specific aetiology, and a combination of factors is often contributory. Occlusal factors do not in general seem to be important.
Diagnosis—This is clinical. Radiographic changes are uncommon, and arthrography or magnetic resonance imaging is seldom indicated.
Further reading
Krause I, Rosen Y, Kaplan I, Milo G, Guedj D, Molad Y, et al. Recurrent aphthous stomatitis in Behcet's disease: clinical features and correlation with systemic disease expression and severity. J Oral Pathol Med 1999;28:193-6
Marbach JJ. Medically unexplained chronic orofacial pain. Temporomandibular pain and dysfunction syndrome, orofacial phantom pain, burning mouth syndrome, and trigeminal neuralgia. Med Clin North Am 1999;83:691-710, vi-vii
Porter SR, Scully C, Pedersen A. Recurrent aphthous stomatitis.
Crit Rev Oral Biol Med 1998;9:306-21
Sakane T, Takeno M, Suzuki N, Inaba G. Behcet's disease. N Engl J Med 1999;341;1284-91
Scully C. A review of common mucocutaneous disorders affecting the mouth and lips. Ann Acad Med Singapore 1999;28:704-7
Scully C, Flint S, Porter SR. Oral diseases. London: Martin Dunitz, 1996
Tammiala-Salonen T, Forssell H. Trazodone in burning mouth pain: a placebo-controlled, double-blind study. J Orofac Pain 1999;13:83-8
Van der Waal I. The burning mouth syndrome. Copenhagen: Munksgaard, 1990
Management—Most patients recover spontaneously, and therefore reassurance and conservative measures are the main management. These include rest, jaw exercises (opening and closing), a soft diet, and analgesics. If these are insufficient, it can be helpful to use plastic splints on the occlusal surfaces (occlusal splints) to reduce joint loading, heat, ultrasound treatment, anxiolytic agents, or antidepressants. A very small minority of patients fail to respond to the above measures and require local corticosteroid or sclerosant therapy, local nerve destruction, or, often as a last resort, joint surgery.
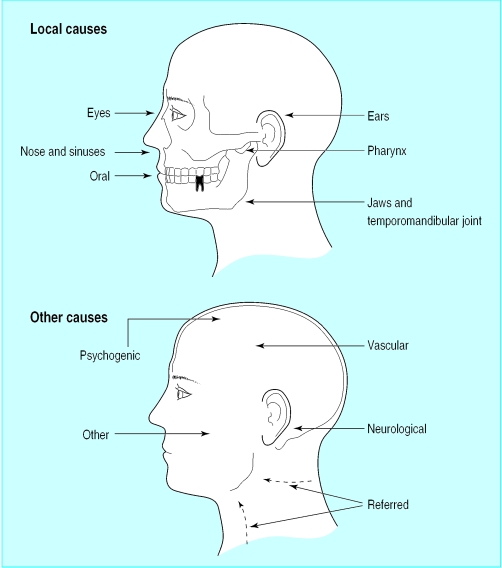
Figure.


Minor aphthous ulceration (top) and major aphthous ulceration (bottom)
Figure.
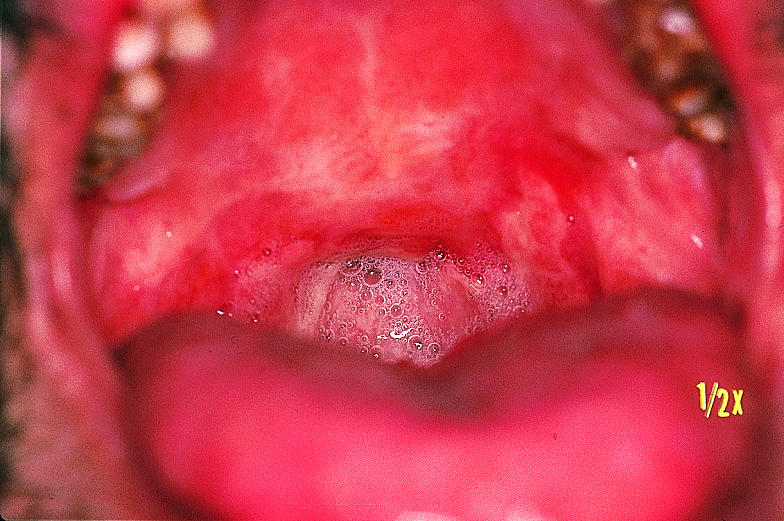
Major aphthous ulceration with severe scarring in patient with Behcet's syndrome
Figure.
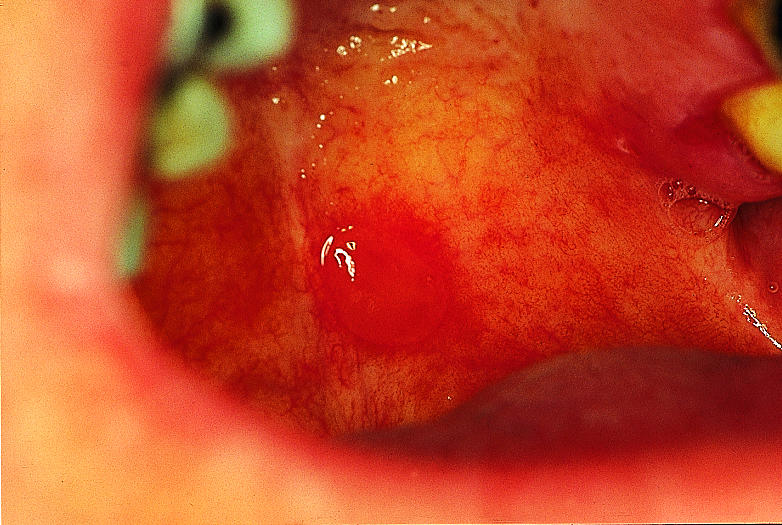
Bulla in oral pemphigoid
Figure.

Erythema migrans
Figure.
Causes of orofacial pain
Acknowledgments
Crispian Scully is grateful for the advice of Rosemary Toy, general practitioner, Rickmansworth, Hertfordshire.
Footnotes
Crispian Scully is dean and Rosemary Shotts is honorary lecturer at the Eastman Dental Institute for Oral Health Care Sciences, University College London, University of London (www.eastman.ucl.ac.uk).
The ABC of oral health is edited by Crispian Scully and will be published as a book in autumn 2000.