Abstract
Background
The burden of pre-existing cardiovascular disease and the contribution to adverse pregnancy outcomes are not robustly quantified, particularly in low-income countries. We aimed to determine both the prevalence of maternal heart disease through active case finding and its attributable risk to adverse pregnancy outcomes.
Methods
We conducted a 24-month prospective longitudinal investigation in three Ugandan health centres, using echocardiography for active case finding during antenatal care. Women with and without heart disease were followed to 6 weeks post partum to determine pregnancy outcomes. Prevalence of heart disease was calculated. Per cent attributable risk estimates were generated for maternal, fetal and neonatal mortality.
Results
Screening echocardiography was performed in 3506 women. the prevalence of heart disease was 17 per 1000 women (95% ci 13 to 21); 15 per 1000 was rheumatic heart disease. Only 3.4% of women (2/58) had prior diagnosis. Cardiovascular complications occurred in 51% of women with heart disease, most commonly heart failure. Per cent attributable risk of heart disease on maternal mortality was 88.6% in the exposed population and 10.8% in the overall population. Population attributable risk of heart disease on fetal death was 1.1% and 6.0% for neonatal mortality
Conclusions
Occult maternal heart disease may be responsible for a substantial proportion of adverse pregnancy outcomes in low-resource settings. Rheumatic heart disease is, by far, the most common condition, urging global prioritisation of this neglected cardiovascular disease.
INTRODUCTION
Indirect causes of maternal deaths, which include non-obstetrical pre-existing conditions, account for over one-quarter (28%) of global maternal mortality.1 Recent reports suggest that maternal deaths attributable to indirect causes are on the rise1 2 and that the greatest burden is shouldered by the world’s poorest women, living in Southeast Asia and sub-Saharan Africa.1
Despite this substantial and increasing burden, there has been a lack of global focus on understanding and addressing non-obstetrical drivers of poor pregnancy outcome.3 In part, this inattention is due to the heterogeneity of indirect maternal mortality, which encompasses a diverse set of pre-existing conditions including HIV, anaemia, mental health conditions and cardiovascular disease.4
Obtaining accurate data on the prevalence and impact of maternal cardiovascular disease presents a unique set of challenges, most pronounced in the lowest resource areas. First, more than 70% of the poorest quintile in sub-Saharan Africa delivers at home.5 Among these deliveries, over half are unattended and 40% are attended by a traditional birth attendant,5 making it unlikely that cardiovascular symptoms and deaths will be recognised and reported. Second, patients are most often unaware of cardiovascular disease until the advanced stages. A recent study showed 85% of Ugandan patients with newly diagnosed rheumatic heart disease (RHD), the most common cardiovascular diagnosis in low-resource areas, presented only when advanced valvular damage had occurred and complications had developed.6 Echocardiography is the most sensitive and specific tool for diagnosis of cardiovascular disease, however, it is rarely available outside of large cities in sub-Saharan Africa.7
In contrast, point-of-care ultrasound, deployed to the community and performed by non-physician providers, is increasingly available and has been shown to be effective in improving detection of high-risk obstetrical conditions.8 To enable an innovative assessment of community heart disease burden, the Children’s National Health System and the Uganda Heart Institute partnered with Imaging the World (ITW), a non-governmental organisation, to add a focused echocardiographic screening to an established obstetrical imaging service, for all women presenting for routine antenatal care (ANC) in targeted Ugandan healthcare centres.
Our objectives were twofold: (1) determine the prevalence of pre-existing maternal heart disease, and (2) determine the per cent population attributable risk of cardiovascular disease to adverse maternal, fetal and neonatal outcomes.
METHODS
General design
This was a 24-month prospective longitudinal investigation focusing on pregnant women seeking ANC at three ITW clinics in Uganda.
Study sites and population
Two health centre III’s (HCIII) and one regional referral hospital were chosen as enrolment sites (figure 1). Nawanyago Health Center III, Kamuli District, serves a population of 15 000 persons, with an average of 276 ANC visits per month. Kasambya Health Center III, Mubende District, serves 36 588 persons, with an average of 1200 ANC visits per month (figure 1). Mubende Regional Referral Hospital, a 175-bed public referral hospital in the same district as Kasambya, was selected under consideration that women with cardiovascular symptoms may self-refer to higher level facilities.
Figure 1.
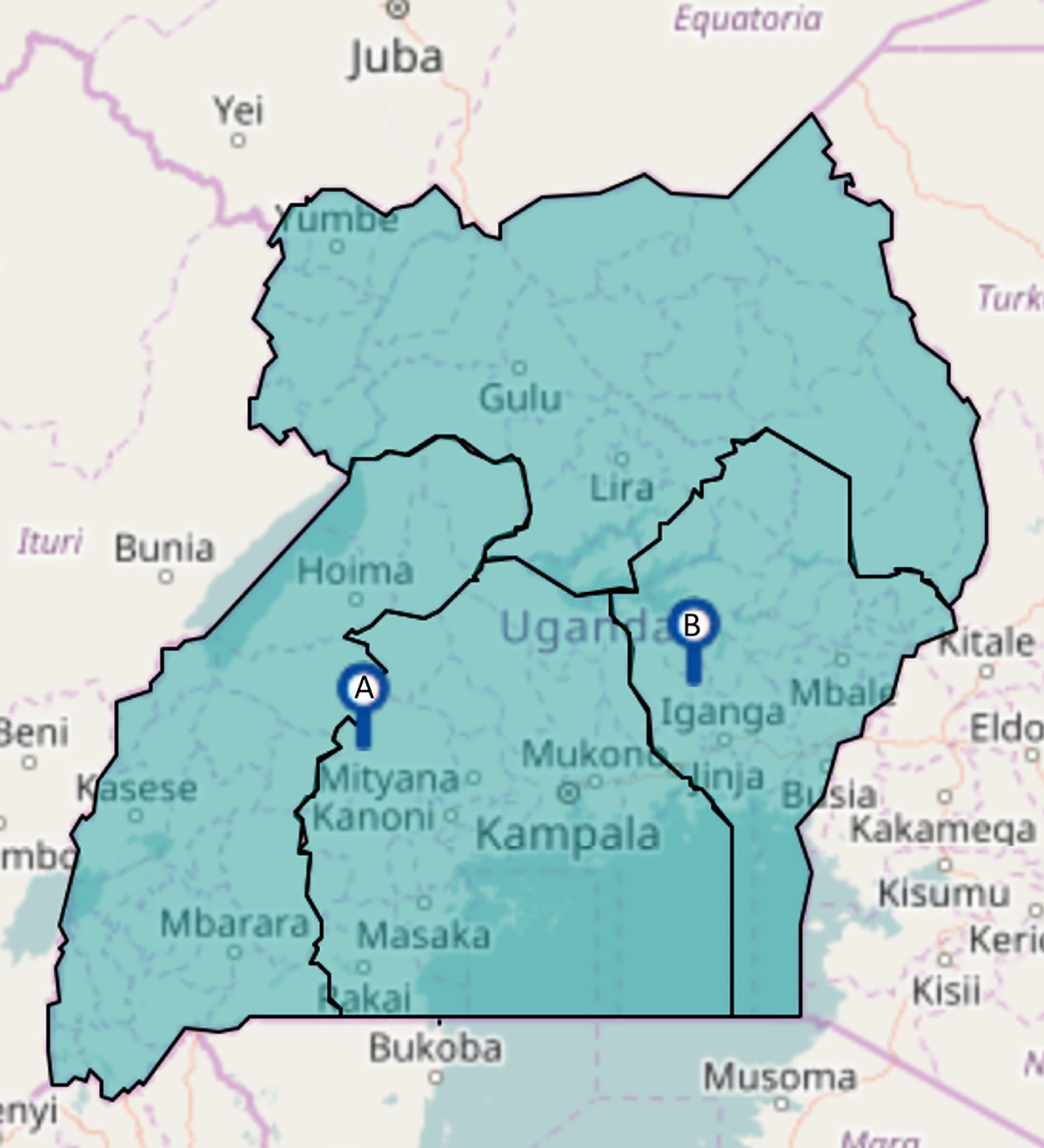
Map of Uganda with enrolment sites. (A) Kasambya (health centre III’s (HCIII) and Mubende Regional Referral Hospital). (B) Nawanyago.
Recruitment and consent
ITW currently encourages women to participate in ANC through community outreach. No additional recruitment strategies were undertaken, but theVillage Health Team (VHTs) were provided education to raise awareness in the community. In communities served by ITW clinics, approximately 80% of women present for at least one ANC visit.8 These numbers are better than Uganda as a whole, presenting an opportunity to capture a representative population. All women attending routine ANC were offered participation and those agreeing signed a written informed consent.
Clinical intake protocol
Directed interview and review of hand-carried medical records was undertaken to capture history.
Image acquisition and interpretation
Two nurses at each site were trained in obtaining a focused echocardiogram using an adult echocardiography probe and a fully functional standard portable-sized ultrasound/echocardiography machine (S4–1 probe, Philips ClearVue 350, Bothell, WA or General Electric VIVID Q, Milwaukee, WI). Echocardiograms were transferred via network cable to a laptop computer where proprietary software was used to compress the images to a hosted server (Datarealm, Phoenix, Arizona) via a USB modem (MTN, Uganda). Images were reviewed by board-certified cardiologists (CS, AB) within 24 hours. Monthly cardiology outreach clinics conducted (EO) to confirm diagnoses and assisted with management.
Irrespective of maternal age, for the purposes of standardisation, diagnosis of RHD was made in accordance with the 2012 World Heart Federation Criteria for patients >20 years of age.9 Thus, no borderline RHD, a category reserved for those ≤20 years, was diagnosed. Severity of valvular involvement was determined according to the 2017 American Heart Association/American College of Cardiology guidelines.10
Nested cohort
All women with heart disease were invited back for up to three additional study visits based on the gestational age at enrolment, which coincided with routine ANC at 20 weeks’ gestation, 30–35 weeks’ gestation and ≥6 weeks post partum. At each visit, participants underwent a cardiovascular review of systems, an ECG to assess cardiac rhythm, a limited cardiovascular assessment and determination of New York Heart Association (NYHA) classification.11 Participants were counselled on recognition of cardiovascular symptoms including shortness of breath, syncope, haemoptysis, orthopnoea and decreased exercise tolerance, and asked to come back to the healthcare centre for evaluation if these occurred. VHT members (already working closely with pregnant women in the community) as well as research staff visited mothers who did not return for follow-up to increase retention.
Outcome definitions
Maternal death was defined according to current WHO standards12 as: ‘The death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.’ In all cases, an attempt was made to determine the cause of maternal death through structured interview. We also developed a composite definition of adverse maternal cardiac events, defined more broadly to include cardiac death, acute pulmonary oedema, pulmonary haemorrhage, new episode of arrhythmia requiring treatment, new-onset heart failure, need for cardiac medication initiation (not including benzathine penicillin prophylaxis for women with RHD), thromboembolic event, endocarditis, hospitalisation for cardiac reasons or cardiac intervention.13 Fetal adverse outcome was defined as a fetal death after 14 weeks’ gestation to include still-born infants. Neonatal death was defined according to the WHO definition14 as ‘death following live birth during the first 28 days of life.’
Statistics
The goal of the analysis was to evaluate the extent to which heart disease impacts maternal morbidity and maternal, fetal and neonatal mortality in sub-Saharan Africa. Demographics, obstetrical history and cardiovascular symptoms at time of enrolment were summarised as number and percentage, mean and SD or median and IQR as appropriate. Characteristics on physical exam and echocardiography were summarised similarly for women with heart disease. Delivery type and location, gestational age and pregnancy outcomes were summarised and compared between women with and without heart disease with pregnancy outcomes displayed as number affected per 1000 persons. Stata V.14 (StataCorp, 2015, College Station, TX) was used for all further analyses, with two-tailed testing, and a statistical significance cut-off of ≤0.05. Unpaired two-tailed t-tests were used to compare continuous normally distributed data, Wilcoxon rank-sum tests were used to compare non-normally distributed data and presented as medians with IQR, and two-tailed Fisher’s exact tests with estimates of exact p values were used to compare categorical data between pregnancies affected and not affected by cardiovascular abnormalities. These methods were used to generate estimates of heart disease risk with 95% CIs. Next, the procedure punaf15 after Poisson regression in Stata V.1516 was used to estimate the per cent attributable risk (%PAR) in women with and without heart disease for maternal, fetal and neonatal mortality. PAR was calculated with the following formula: PAR=Attributable Fraction among Exposed (AFE)*(RHD exposed deaths/all deaths)*100, with AFE=(Mortality Ratio−1/Mortality Ratio).
RESULTS
Screening echocardiography was performed in 3506 women presenting for routine ANC. Heart disease was diagnosed in 58 women, translating to a community prevalence of maternal heart disease of 1.7% (95% CI 1.3% to 2.1%), or 17 per 1000 women screened (table 1). Of these women, 1501 (42.6%) were evaluated at Nawanyago HCIII, 1351 (38.3%) at Kasambya HCIII and 674 (19.1%) at Mubende Regional Referral Hospital. There was no difference in the prevalence of heart disease across enrolment sites (p=0.84; table 2).
Table 1.
Baseline maternal characteristics
| No heart disease (n=3448) | Heart disease (n=58) | P values | |
|---|---|---|---|
|
| |||
| Age, years (median, IQR) | 24.0 (21–30) | 29.5 (24–35) | <0.001 |
| Highest level of education | 0.93 | ||
| Did not complete primary school, n (%) | 1451 (42.1) | 28 (48.3) | |
| Completed primary, n (%) | 1270 (36.8) | 27 (46.6) | |
| Completed secondary, n (%) | 90 (2.6) | 2 (3.4) | |
| Completed university, n (%) | 86 (2.4) | 1 (1.7) | |
| Enrolment site | 0.84 | ||
| Nawanyago, n (%) | 1474 (42.7) | 27 (46.6) | |
| Kasambya, n (%) | 1330 (38.6) | 21 (36.2) | |
| Mubende, n (%) | 644 (18.7) | 10 (17.2) | |
| Obstetrical data | |||
| Gestational age at first visit (median, IQR) | 24.0 (20–30) | 24.0 (20–28) | 0.91 |
| Primigravida, n (%) | 353 (10.2) | 6 (10.2) | 0.98 |
| Parity (median, IQR) | 2.0 (1–4) | 4.0 (3–6) | <0.001 |
| History of premature birth, n (%) | 13 (0.4) | 0 | 0.62 |
| History of premature fetal loss, n (%) | 283 (8.2) | 9 (15.3) | 0.03 |
| History of neonatal mortality, n (%) | 103 (3.0) | 1 (1.7) | 0.56 |
| Obstetrical ultrasound, n (%) | 815 (23.6) | 37 (63.8) | <0.001 |
| Medical history | |||
| Maternal HIV*, n (%) | 137 (4.2) | 4 (7.0) | 0.30 |
| History of cardiac disease, n (%) | 0 | 2 (3.4) | <0.001 |
| Cardiac symptoms reported at enrolment | |||
| Shortness of breath, n (%) | 60 (1.7) | 6 (10.3) | <0.001 |
| Excessive swelling, n (%) | 42 (1.2) | 0 | 0.40 |
| Syncope, n(%) | 28 (0.8) | 1 (1.7) | 0.45 |
| Haemoptysis, n(%) | 4 (0.1) | 0 | 0.80 |
| Palpitations, n(%) | 581 (17.0) | 27 (46.5) | <0.001 |
| Limited exercise tolerance, n (%) | 67 (1.9) | 7 (12.0) | <0.001 |
| Chest pain, n (%) | 88 (2.6) | 8 (13.8) | <0.001 |
Data only available for 3256 women without heart disease and 57 women with heart disease.
Table 2.
Characteristics of women with heart disease on echocardiographic screening
| Characteristics of women with heart disease (n=58) | n (%) | Prevalence per 1000 in screened population (95% CI) |
|---|---|---|
|
| ||
| Any heart disease | 58 | 17 (13 to 21) |
| Rheumatic heart disease, n (%) | 51 (87.9) | 15 (11 to 19) |
| Mild, n (%) | 31 (53.4) | 9 (6 to 13) |
| Moderate, n (%) | 14 (24.1) | 4 (2 to 7) |
| Severe, n (%) | 6 (10.3) | 2 (0.8 to 4) |
| Cardiomyopathy, n (%) | 1 (1.7) | 0.3 (0.1 to 2) |
| Structural heart disease, n (%) | 1 (1.7) | 0.3 (0.1 to 2) |
| Other, n (%) | 4 (6.9) | 1 (0.4 to 3) |
| NYHA functional class at entry | ||
| I, n (%) | 7 (13.4) | |
| II, n (%) | 41 (78.8) | |
| III, n (%) | 4 (7.7) | |
| IV, n (%) | 0 | |
| Maternal knowledge of heart disease prior to echo, n (%) | 2 (3.4) | |
| Cardiac medications prior to study, n (%) | 1 (1.7) | |
| Echo finding for women with RHD (n=51) | ||
| LV ejection fraction <55%, n (%) | 0 (0) | |
| Mitral regurgitation, n (%) | 45 (88) | |
| Mild, n (%) | 28 (54.9) | |
| Moderate, n (%) | 15 (29.4) | |
| Severe, n (%) | 2 (3.9) | |
| Mitral stenosis, n (%) | 3 (5.9) | |
| Mild, n (%) | 2 (3.9) | |
| Moderate, n (%) | 1 (2.0) | |
| Severe, n (%) | 0 (0) | |
| Aortic insufficiency, n (%) | 7 (13.7) | |
| Mild, n (%) | 5 (9.8) | |
| Moderate, n (%) | 1 (2.0) | |
| Severe, n (%) | 1 (2.0) | |
| Aortic stenosis, n (%) | 0 (0) | |
LV, left ventricular; NYHA, New York Heart Association; RHD, rheumatic heart disease.
Compared with women without heart disease, affected women were slightly older (mean 29.7 years vs 25.5 years, p<0.001) and more likely to have a history of fetal loss (15.3% vs 8.2%, p=0.03). Some cardiovascular symptoms, including shortness of breath (p<0.001), palpitations (p<0.001), limited exercise tolerance (p<0.001) and chest pain (p<0.001), were more common at presentation among women with heart disease, while other symptoms potentially attributable to heart disease, including excessive swelling (p=0.40), syncope (p=0.45) and haemoptysis (p=0.80), were not different between groups (table 2).
The majority of women with heart disease were diagnosed with RHD (51, 87.9%; table 1), for a population prevalence of 15 per 1000 women screened. A wide range of RHD severity was found in the community with 31 (60.8%) women found to have mild, 14 (24.1%) moderate and 6 (11.8%) severe valvular involvement. Other diagnoses included one woman each with dilated cardiomyopathy, congenital heart disease (large secundum atrial septal defect), pericardial effusion, pulmonary hypertension, primary arrhythmia and mild left ventricular dysfunction. There was a wide spectrum of functional class, with most women initially classified as NYHA class II (78.8%); four women (7.7%) were classified as NYHA class III. Maternal knowledge of pre-existing heart disease was very low, with only two women (3.4%) previously aware of their diagnosis (table 2).
Of the 58 women with heart disease, 14 were considered either high risk or moderate risk by the combined cardiology/obstetrical team. Caesarean delivery was recommended at the national referral hospital with the cardiology/obstetrical team for one woman, who was hospitalised 1 month prior to delivery and had both maternal and neonatal survival (after multiple late-term fetal losses in the community). Delivery at the regional referral hospital was recommended for seven women. Of the six who followed the prescribed care plan, there were no maternal deaths and only one neonatal demise secondary to prematurity. The remaining woman, the single maternal mortality, delivered at home. Delivery at the HCIII was recommended for six additional women; three delivered at home, one successfully delivered at the HCIII and two were moved during labour to higher level facilities secondary to cardiovascular symptoms.
Pregnancy outcomes were captured for all women without heart disease and 56 of 58 women (96.6%) with heart disease. Women with heart disease were more likely to deliver at the regional referral hospital and less likely to deliver with a traditional birth attendant (p=0.006). Cardiovascular complications were common among women diagnosed with heart disease, occurring in 51.8% (95% CI 39.0 to 64.3; table 3). Heart failure was the most common complication (33.9%, 95% CI 22.9 to 47.0), followed by pulmonary hypertension (10.7%, 95% CI 5.0% to 21.5%). Over half of women required initiation of cardiovascular medication. There was no difference in median duration of pregnancy between women with and without heart disease, but women with heart disease were more likely to have a caesarean delivery (3.5% vs 10.7%, p=0.004) (table 3).
Table 3.
Outcomes for women with and without heart disease
| Lost to follow-up (n) | 0/3448 |
2/58 |
P values |
|---|---|---|---|
| No heart disease (n=3448) | Heart disease (n=56) | ||
|
| |||
| Place of delivery (n=3438, 56) | Prevalence/100 (95% CI) | Prevalence/100 (95% CI) | 0.006 |
| Home | 13.9 (12.6–14.9) | 23.2 (14.1–35.8) | |
| Health centre (II, III, IV) | 59.9 (57.8–61.1) | 50.0 (37.3–62.7) | |
| District hospital | 6.4 (5.2–6.8) | 3.6 (1.0–12.1) | |
| Regional referral hospital | 12.9 (11.6–13.8) | 2.4 (11.6–34.4) | |
| National referral hospital | 0.4 (0.1–0.5) | 1.8 (0.5–9.6) | |
| Traditional birth attendant | 6.5 (5.6–7.2) | 0 | |
| Delivery data | |||
| Pregnancy duration (median, IQR) | 38.2 (38–39) | 39.0 (36–40) | 0.65 |
| Method of delivery | 0.016 | ||
| Vaginal, n(%) | 96.5 (95.5–96.8) | 89.3 (78.5–95.0) | |
| Caesarean section, n (%) | 3.5 (3.0–4.2) | 10.7 (5.0–21.5) | |
| Cardiovascular complications | |||
| Any | 0 | 51.8 (39.0–64.3) | |
| Heart failure | 0 | 33.9 (22.9–47.0) | |
| Cardiac medication initiation | 0 | 48.2 (35.7–60.1) | |
| Arrhythmia | 0 | 3.6 (1.0–12.1) | |
| Pulmonary hypertension | 0 | 10.7 (5.0–21.5) | |
| Hospital admission (cardiac cause) | 0 | 3.6 (1.0–12.1) | |
| Pregnancy outcome per 1000* | |||
| Maternal mortality | 2.0 (1.0–4.3) | 15.4 (2.4–97.9) | 0.044 |
| Fetal death | 38.6 (32.4–45.5) | 71.4 (19.8–172.9) | 0.124 |
| Neonatal death | 10.2 (7.3–14.2) | 42.1 (13.9–127.1) | 0.016 |
Adjusted for maternal age and enrolment site differences.
%PAR of heart disease on maternal mortality was 86.8% (95% CI 5.0% to 98.2%) in the exposed population, and 10.8% (95% CI –15.0% to 30.9%) in the overall population. Overall population attributable risk of heart disease on fetal death was 1.1% (95% CI −1.6 to 3.7), and for neonatal mortality 6.0% (95% CI −2.9% to 14.1%). Table 4 shows a breakdown of causes of maternal and neonatal death. All seven deaths among women without heart disease were directly attributable to pregnancy-related complications. Among neonatal deaths, the three deaths (100%) among women with heart disease were the result of preterm birth, compared with 8/35 (22.9%) of neonatal deaths attributable to prematurity among women without heart disease.
Table 4.
Details of adverse maternal and neonatal mortality
| No heart disease (n=3448) | Heart disease (n=56) | |
|---|---|---|
|
| ||
| Maternal (up to 6 weeks PP) | 7 maternal deaths | 1 maternal death |
| Haemorrhage | 3 | 0 |
| Hypertensive diseases | 1 | 0 |
| Sepsis/infection | 1 | 0 |
| Obstructed labour | 1 | 0 |
| Embolism | 1 | 0 |
| Heart failure | 0 | 1* |
| Neonatal (up to 6 weeks PP) | 35 neonatal deaths | 3 neonatal deaths |
| Birth asphyxia | 10 | 0 |
| Sepsis/infection | 4 | 0 |
| Preterm delivery <35 weeks’ gestation) | 8 | 3 |
| Congenital malformation | 2 | 0 |
| Other | 4 | 0 |
| Unknown | 7 | 0 |
Thirty-eight years old, 11 prior children, baseline diagnosis dilated cardiomyopathy with moderate mitral regurgitation and severely decreased left ventricular function. Delivery was recommended for a regional referral hospital, but the mother chose to deliver at home against medical advice, and died 4 days post partum with severe, complicated heart failure that worsened with pregnancy and after delivery, which was also complicated by protracted haemorrhage and possible sepsis (indicated by reported fever in the last day prior to death.
PP, postpartum.
DISCUSSION
This prospective, community-based echocardiographic study captures the prevalence and spectrum of maternal heart disease in a low-income sub-Saharan African country with 17 out of 1000 women (95% CI 13 to 21) having echocardiographic evidence of heart disease, 88% of which was RHD. Use of echocardiographic screening during routine ANC was an important advancement in the ascertainment of indirect causes of adverse maternal outcomes; almost all the patients in this study (as was presumed) did not have pre-existing knowledge of their heart disease. Over half of women with heart disease experienced complications related to their heart disease during pregnancy, most commonly heart failure (33%). The per cent population attributable risks of maternal heart disease on maternal, fetal and neonatal mortality were 10.8%, 1.1% and 6.0%, respectively.
While the terms direct and indirect maternal death are falling out of favour,17 there remains an important distinction both in the presence of existing high-risk conditions (indirect) and in our understanding of how to prevent these adverse events. In a WHO systematic analysis of global causes of maternal deaths, data from over 100 countries and 60 000 deaths were analysed. Indirect deaths accounted for 27.5% of maternal mortality, yet almost no granular aetiological data were available. Our data provide the first community-based active surveillance of maternal heart disease, finding 11% of maternal deaths attributable to heart disease. With an average of 28% of global maternal mortality thought to be indirect,1 our data suggest 40% of these deaths result from cardiovascular complications: 35% from RHD and 5% from other heart conditions.
As demonstrated in other low-resource areas, RHD predominated in this population, affecting 88% of women with heart disease. RHD is a largely preventable, acquired heart disease resulting from untreated or undertreated group A streptococcal infections in the community.18 A recent publication on the outcomes of women with rheumatic mitral disease, which largely excluded low-income countries, found that heart failure complicated 23% of women entering pregnancy with moderate or severe mitral regurgitation.13 It is not surprising that our cohort showed a higher rate of heart failure, 33%, as none of the women with RHD in our cohort entered pregnancy with a known diagnosis, and thus with appropriate medical management. Our data provide compelling evidence that strengthening RHD prevention efforts could substantially reduce global maternal mortality.
Population data on mothers with antenatal heart disease are sparse from low-income countries. The majority of existing data come from tertiary centres, which disproportionately reflect women with severe heart disease19–22 and large registry-based data which typically exclude patients from low-income settings.13 23 Use of registries to ascertain outcomes for women with RHD in lower income settings is severely limited as registration inherently requires diagnosis. In our series, 97% of women found to have heart disease on echocardiographic screening were unaware of their diagnosis, highlighting the need for active case finding.
Echocardiographic screening is the most sensitive way to detect heart disease among pregnant mothers. Increasing availability of obstetrical imaging in low-resource settings may provide a platform for diagonal integration of cardiac echocardiography, however further implementation and costing research is needed to support this strategy. While many symptoms of cardiovascular disease overlap with normal findings in pregnancy, our data found women with heart disease significantly more likely than their heart disease-negative peers to have shortness of breath, palpitations, limited exercise tolerance and chest pain during pregnancy. Further research is needed to determine if a clinical risk score for occult heart disease may be useful in identifying high-risk mothers, and to assess the performance of cardiac auscultation and/or ECG as compared with echocardiography.
It is of upmost importance that our data likely reflect the best-case scenario for pregnant women living in low-resource settings with occult heart disease. Over half of women in this cohort required initiation of at least one cardiovascular medication during pregnancy. Women were managed for heart failure, pulmonary hypertension and arrhythmia, among other complications by the local cardiology, and when needed specialty cardio-obstetrical team; specialty care that is rarely available in sub-Saharan Africa. Delivery planning was modified, encouraging delivery at a healthcare facility and caesarean section, significantly higher among women with heart disease (10.7% vs 3.5%, p=0.01), when appropriate. It is unlikely without echocardiographic screening that many of these women would have been diagnosed prior to delivery. Some may have presented prior to delivery with severe symptoms, however data from Senegal show morbid outcomes in this scenario, with 34% maternal death.19 It is likely that more would have been symptomatic in delivery or the postpartum period and experienced complications including higher rates of maternal death, fetal loss and neonatal mortality, without ever knowing they had heart disease.
In addition to the inevitable and ethically appropriate modification of outcome once heart disease was diagnosed, there are other limitations to this cohort. There were slight demographic differences among women with and without heart disease, such as maternal age, that could influence outcomes. Treating physicians, responsible for identifying and diagnosing heart failure, were not blinded to echocardiographic results, which could have introduced bias. Follow-up was limited to 6 weeks post partum when International Classification of Diseases 10th Revision classification recommends recording late maternal death. Future longitudinal studies of these women are planned. The overall number of women with heart disease was small and only a single woman suffered maternal mortality from heart disease. These low numbers lead to wide CIs around relative risk and attributable risk of adverse events and limit the ability and utility of conducting subanalysis to identify those most at risk. However, the high rate of largely occult RHD, 15 per 1000 women (95% CI 13 to 21 per 100), is of high importance and entirely consistent with previous data showing a 1%–2% prevalence of definite RHD among youth in sub-Saharan Africa.24 The global targets for reducing maternal mortality will not be met until heart disease, namely RHD, receives more international attention, research and funding.25
CONCLUSION
There is a high burden of occult heart disease, namely RHD, among pregnant women living in Uganda. Diagnosis prior to pregnancy is uncommon, resulting in missed opportunity for appropriate medical management and delivery planning. This study provides a conservative estimate (considering the required ethical intervention) that pre-existing maternal heart disease accounts for a minimum of 11% of maternal mortality. It is clear that without addressing RHD in low-resource populations, global maternal survival goals cannot be met. While no single strategy can alone prevent all cardiovascular-related pregnancy complications, focusing efforts around RHD prevention holds the highest promise.
Key messages.
What is already known on this subject?
Over one-quarter of global maternal deaths are attributable to non-obstetrical causes, such as pre-existing cardiac disease.
Heart disease, mainly rheumatic heart disease, is common in areas with high maternal mortality, but its contribution to poor maternal outcomes at a community level is not known.
What this study adds?
We determined the prevalence of maternal heart disease in the community, by embedding echocardiographic screening into community antenatal care visits.
1.7% of women screened had pre-existing cardiac disease, and 88% of these women had rheumatic heart disease.
Maternal knowledge of pre-existing cardiac disease was very low prior to screening.
Pre-existing cardiac disease was responsible for substantial risk of adverse maternal outcomes.
How might this impact clinical practice?
These data urge more research and focus on the early detection and prevention of maternal heart disease, namely rheumatic heart disease, in low-resource settings.
Acknowledgements
We gratefully acknowledge the contribution and partnership of imaging the World and imaging the World africa, in particular Collins Owani, Allan Asiimwe, Picho Shaddrack Ali, Hakeem Kasumba, John Kisandi, Moses Amatsiko and Yuvensio Kabaisera. We thank the participating healthcare centres, village health team members, nurses and mothers. AB was primarily supported by the American Heart Association (AHA) Mentored Clinical and Population Award (15MCPRP25090076), the Children’s Research Institute and private donors to Children’s National Medical Center Africa Fund, as well as the Children’s National Global Health Initiative.
Funding
The Work was funded by the American Heart Association Mentored Clinical and Population Award (15MCPRP25090076), the Children’s Research Institute and private donors to Children’s National Medical Center Africa Fund.
Footnotes
Competing interests None declared.
Disclaimer The funders had no role in study design; data collection, analysis, interpretation; or writing the report. the corresponding author had full access to all the data in the study and final responsibility for the decision to submit for publication.
Patient consent Not required.
Ethics approval Mengo Institutional Review Board and Children’s National Medical Center Institutional Review Board as well as the Uganda National Council of Science and Technology.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health 2014;2:e323–33. [DOI] [PubMed] [Google Scholar]
- 2.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Strategy to accelerate progress towards the attainment of international development goals and targets related to reproductive health. Reprod Health Matters 2005;13:11–18. [DOI] [PubMed] [Google Scholar]
- 4.Organization TWh. The WHO application of ICD-10 to deaths during pregnancy, childbirth and puerperium. 66: ICD-MM, 2012. [Google Scholar]
- 5.Montagu D, Yamey G, Visconti A, et al. Where do poor women in developing countries give birth? A multi-country analysis of demographic and health survey data. PLoS One 2011;6:e17155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang W, Mondo C, Okello E, et al. Presenting features of newly diagnosed rheumatic heart disease patients in Mulago Hospital: a pilot study. Cardiovasc J Afr 2013;24:28–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.carlson S, Duber HC, Achan J, et al. Capacity for diagnosis and treatment of heart failure in sub-Saharan Africa. Heart 2017;103:1874–9. [DOI] [PubMed] [Google Scholar]
- 8.Ross AB, DeStigter KK, Rielly M, et al. A low-cost ultrasound program leads to increased antenatal clinic visits and attended deliveries at a health care clinic in rural Uganda. PLoS One 2013;8:e78450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reményi B, Wilson N, Steer A, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease–an evidence-based guideline. Nat Rev Cardiol 2012;9:297–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused update of the 2014 AHA/ACC Guideline for the management of patients with valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;70:252–89. [DOI] [PubMed] [Google Scholar]
- 11.Dolgin MAN, Fox AC, Gorlin R, et al. ; Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th edn. Boston, MA: Lippincott Williams and Wilkins, 1994. [Google Scholar]
- 12.Organization TWH. Revised 1990 Estimates of Maternal Mortality. 1996.
- 13.van Hagen IM, Thorne SA, Taha N, et al. Pregnancy outcomes in women with rheumatic mitral valve disease: results from the registry of pregnancy and cardiac disease. Circulation 2018;137:806–16. [DOI] [PubMed] [Google Scholar]
- 14.Pathirana J, Muñoz FM, Abbing-Karahagopian V, et al. Neonatal death: case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine 2016;34:6027–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newson RB. Attributable and unattributable risks and fractions and other scenario comparisons. The Stata Journal 2013;13:672–98. [Google Scholar]
- 16.StataCorp LLC. Stata Statistical Software: release 15 computer program. College Station, TX: StataCorp LLC, 2017. [Google Scholar]
- 17.van den akker T, Nair M, Goedhart M, et al. Maternal mortality: direct or indirect has become irrelevant. Lancet Glob Health 2017;5:e1181–2. [DOI] [PubMed] [Google Scholar]
- 18.Zühlke LJ, Beaton A, Engel Me, et al. Group A Streptococcus, Acute Rheumatic Fever and Rheumatic Heart Disease: epidemiology and clinical considerations. Curr Treat Options Cardiovasc Med 2017;19:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diao M, Kane A, Ndiaye MB, et al. Pregnancy in women with heart disease in Sub-Saharan Africa. Arch Cardiovasc Dis 2011;104:370–4. [DOI] [PubMed] [Google Scholar]
- 20.Naidoo DP, Desai DK, Moodley J. Maternal deaths due to pre-existing cardiac disease. Cardiovasc J S Afr 2002;13:17–20. [PubMed] [Google Scholar]
- 21.Soma-Pillay P, Seabe J, Sliwa K. The importance of cardiovascular pathology contributing to maternal death: Confidential Enquiry into Maternal Deaths in South Africa, 2011–2013. Cardiovasc J Afr 2016;27:60–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watkins DA, Sebitloane M, Engel ME, et al. The burden of antenatal heart disease in South Africa: a systematic review. BMC Cardiovasc Disord 2012;12:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siu SC, Sermer M, Colman JM, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001;104:515–21. [DOI] [PubMed] [Google Scholar]
- 24.Rothenbühler M, O’Sullivan CJ, Stortecky S, et al. Active surveillance for rheumatic heart disease in endemic regions: a systematic review and meta-analysis of prevalence among children and adolescents. Lancet Glob Health 2014;2:e717–e726. [DOI] [PubMed] [Google Scholar]
- 25.Nations U Millennium development goals report. 2015.


