Abstract
BACKGROUND:
High awareness that cardiovascular disease is the leading cause of death (LCOD) among women is critical to prevention. This study evaluated longitudinal trends in this awareness among women.
METHODS AND RESULTS:
Online surveys of US women (≥25 years of age) were conducted in January 2009 and January 2019. Data were weighted to the US population distribution of sociodemographic characteristics. Multivariable logistic regression was used to evaluate knowledge of the LCOD. In 2009, awareness of heart disease as the LCOD was 65%, decreasing to 44% in 2019. In 2019, awareness was greater with older age and increasing education and lower among non-White women and women with hypertension. The 10-year awareness decline was observed in all races/ethnicities and ages except women ≥65 years of age. The greatest declines were among Hispanic women (odds ratio of awareness comparing 2019 to 2009, 0.14 [95% CI, 0.07–0.28]), non-Hispanic Black women (odds ratio, 0.31 [95% CI, 0.19–0.49]), and 25- to 34-year-olds (odds ratio, 0.19 [95% CI, 0.10–0.34]). In 2019, women were more likely than in 2009 to incorrectly identify breast cancer as the LCOD (odds ratio, 2.59 [95% CI, 1.86–3.67]), an association that was greater in younger women. Awareness of heart attack symptoms also declined.
CONCLUSIONS:
Awareness that heart disease is the LCOD among women declined from 2009 to 2019, particularly among Hispanic and non-Hispanic Black women and in younger women (in whom primordial/primary prevention may be most effective). An urgent redoubling of efforts by organizations interested in women’s health is required to reverse these trends.
Keywords: AHA Scientific Statements, cardiovascular diseases, cause of death, ethnic groups, primary prevention, surveys and questionnaires
Heart disease is the leading cause of death (LCOD) among women.1 In 2018, nearly 400 000 deaths among women were caused by heart disease and stroke, which accounted for 28% of all deaths.2 Despite the important impact of these cardiovascular diseases (CVDs) on mortality among women, the level of awareness and knowledge among women is poor.3-8 Awareness programs designed to educate the public about CVD among women in the United States include Go Red for Women by the American Heart Association (AHA); The Heart Truth by the National Heart, Lung, and Blood Institute; and Make the Call, Don’t Miss a Beat by the US Department of Health and Human Services.
Since 1997, the AHA has conducted national surveys among US women to monitor awareness and knowledge of CVD.3-7,9,10 Results indicated that awareness of heart disease as the LCOD among women nearly doubled from 30% to 56% between 1997 and 2012.7 The greatest gains were observed among younger women (25–34 years of age), whereas the smallest improvements were among Hispanic women. Awareness of heart attack symptoms also increased from 1997 to 2012.
In 2019, the AHA repeated this national US survey. The current report provides 10-year differences in women’s awareness of heart disease as the LCOD among women, controlled for respondent differences across time. We quantified awareness of the signs and symptoms of a heart attack and first actions to take in case of a heart attack.
METHODS
The 2019 national AHA Survey of Women’s Cardiovascular Disease Awareness was implemented as a survey that used methods as previously described.7 As in the 2009 survey,6 the methods used in 2019 included an oversampling of non-Hispanic Black and Hispanic women with age/race quotas set to ensure the desired respondent group composition. Race/ethnicity was categorized by self-reporting as non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, and other non-Hispanic group. Compared with prior surveys, the 2019 survey sampled women 18 to 24 years of age and was conducted exclusively online. Surveys were conducted from January 8 to 25, 2019, with Harris Poll Online, a panel of online respondents maintained by Harris Interactive. The panel includes several million people recruited from web, email, mail, and telephone sources, as previously described.7 The database of respondent information was screened and updated according to demographic and sociodemographic variables to allow precision in the online sample. All surveys were administered in English and took ≈18 minutes to complete.
A variety of CVD-related questions were included in the survey such as CVD-related medical history, awareness of LCOD among women, knowledge of warning signs of heart attack and stroke, first action to take when someone is having a heart attack or stroke, and heart diseases and stroke risk factors. Survey questions for sociodemographic characteristics included age, sex, race, ethnicity, educational attainment, household income, and marital status. Awareness of the LCOD among women was assessed by asking, “As far as you know, what is the LCOD for all women?” Responses considered here were heart attack/heart disease, cancer (all types), and breast cancer considered separately. Knowledge of the signs and symptoms of a heart attack was elicited with this question: “Based on what you know, what warning signs do you associate with having a heart attack?” Unaided responses were provided in open text boxes, which staff from Harris Poll coded into predetermined categories or as other.
New survey questions in 2019 are shown in Supplemental Table I and included topics related to awareness, knowledge, and behaviors (some results will be reported elsewhere). Women were asked about history of hypertension and if they ever used at least 1 technology-enabled device to improve or monitor health.
To facilitate comparisons between the 2009 and 2019 surveys, women from the 2019 sample who were <25 years of age were excluded, and women who completed the 2009 survey on paper via telephone rather than online were excluded.
Results for stroke and other aspects of awareness will be reported elsewhere.
Statistical Analyses
Survey data were tabulated overall and by age groups and race/ethnicity. Data were weighted by age, race/ethnicity, educational attainment, income, and region to reflect the composition of the US population of women ≥25 years of age who speak English according to distributions reported in the US Census Bureau’s March 2018 Current Population Survey.11 Comparisons of the means and proportions used 2-sample t tests and χ2 tests as appropriate, with values of P<0.05 considered statistically significant.
Multivariable logistic regression models were generated to calculate odds ratios (ORs) to estimate the likelihood of identifying the LCOD in each survey year separately and in 2019 compared with 2009. Data were analyzed with the open-source software R (R Foundation for Statistical Computing, Vienna, Austria).12
RESULTS
In the 2019 survey, of 2700 potential participants, 881 (33%) were not eligible (non-US citizens [n=19], <18 years of age [n=14], male sex [n=22], quality control checks [eg, duplicates, not a confirmed real person, fraud; n=206], survey error [n=1], responses over the desired quota for a category of age or racial/ethnic group [n=600], terminations [n=18], other reason [n=1]). Of 1819 eligible women, 1553 (85%) completed the survey. All comparisons below reflect the commonalities and differences between the 2009 and 2019 survey results.
Respondent characteristics are displayed in Table 1. Mean age was 50 years, and age was similar between surveys overall and across racial/ethnic groups. There were subtle differences between surveys in the distributions of age group and race/ethnicity and age distribution across race/ethnicity categories. Greater proportions of non-Hispanic White and non-Hispanic Asian respondents reported higher educational attainment and income compared with non-Hispanic Black or Hispanic respondents. The largest proportion of women in both surveys were married/cohabitating, with non-Hispanic Black women more frequently single or never married. In the 2009 survey, the largest proportion of women overall reported annual household incomes <$35 000, whereas in 2019, the largest proportion reported incomes >$100 000 and the next largest reported incomes <$35 000. More women in 2009 than in 2019 refused to report household income. Fewer than 5% of respondents in each year reported a history of heart attack or stroke. In 2019, 36.8% of women reported hypertension, and diabetes mellitus and hypertension were more common in non-Hispanic Black women. In 2019, 54.5% reported use of technology-enabled devices (not asked in 2009).
Table 1.
Characteristics of Participants in the AHA Women’s Online Awareness Tracking Survey by Year: 2009 and 2019
| Overall | NH White | NH Black | Hispanic | NH Asian | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2009 (n=1158) |
2019 (n=1345) |
2009 (n=634) |
2019 (n=660) |
2009 (n=127) |
2019 (n=209) |
2009 (n=251) |
2019 (n=216) |
2009 (n=125) |
2019 (n=201) |
|
| Mean age (SD), y | 50.0 | 50.6 | 51.4 | 52.9 | 47.6 | 48.8 | 45.7 | 45.6 | 46.1 | 47.4 |
| Age groups, % | ||||||||||
| 25–34 y | 15.7 | 20.2* | 12.7 | 17.3* | 21.4 | 22.1 | 25.0 | 29.5* | 25.4 | 22.4 |
| 35–44 y | 23.2 | 18.2 | 22.9 | 14.1* | 23.7 | 19.8 | 21.6 | 23.6* | 28.2 | 29.4 |
| 45–54 y | 19.4 | 15.9 | 19.5 | 15.7 | 15.3 | 17.4 | 24.1 | 16.6 | 14.1 | 13.7 |
| 55–64 y | 20.3 | 21.4* | 20.3 | 23.6 | 24.0 | 21.5 | 16.9 | 15.8 | 16.3 | 16.7 |
| ≥65 y | 21.4 | 24.3* | 24.7 | 29.2* | 15.6 | 19.2 | 12.3 | 14.5 | 16.0 | 17.9 |
| Race/ethnicity, % | ||||||||||
| NH White | 69.6 | 61.7 | ||||||||
| NH Black | 11.8 | 12.3 | ||||||||
| Hispanic | 12.0 | 15.0* | ||||||||
| NH Asian | 5.1 | 6.5* | ||||||||
| Others | 1.4 | 3.6* | ||||||||
| Educational attainment, % | ||||||||||
| Less than high school | 4.7 | 4.2 | 5.2 | 3.4 | 2.1 | 5.5 | 5.7 | 7.7 | 0.0 | 2.2 |
| High school graduate, job-specific training | 37.9 | 33.9 | 36.1 | 32.6 | 45.7 | 35.5 | 49.5 | 44.9 | 17.2 | 28.9* |
| Some college, associate degree | 26.4 | 25.8 | 27.2 | 24.6 | 27.0 | 31.4 | 22.3 | 25.1* | 23.7 | 14.4 |
| 4-y College degree, some graduate school but less than postgraduate degree | 23.2 | 25.3* | 24.1 | 28.7* | 15.3 | 18.3 | 15.8 | 16.4 | 50.8 | 34.4 |
| Postgraduate degree | 7.8 | 10.8* | 7.6 | 10.7* | 10.2 | 9.8 | 5.7 | 5.7 | 11.2 | 19.6* |
| Household income, % | ||||||||||
| <$35 000 | 25.9 | 25.1 | 22.9 | 21.8 | 38.3 | 38.1 | 34.1 | 30.9 | 15.7 | 16.0 |
| $35 000–$49 999 | 11.8 | 11.5 | 11.2 | 10.9 | 14.7 | 13.6 | 14.8 | 14.6 | 8.4 | 9.3 |
| $50 000–$74 999 | 15.6 | 15.8 | 15.6 | 15.5 | 14.0 | 16.8 | 17.3 | 18.1 | 13.4 | 13.5 |
| $75 000–$99 999 | 11.2 | 13.1* | 11.6 | 12.4 | 9.0 | 10.5 | 10.4 | 15.0* | 12.1 | 13.5 |
| ≥$100 000 | 18.2 | 31.1* | 20.7 | 36.2* | 8.8 | 18.9* | 10.8 | 20.3* | 27.1 | 40.0* |
| Refused | 17.2 | 3.4* | 17.8 | 3.0* | 14.8 | 1.9* | 12.7 | 1.5* | 23.1 | 6.7 |
| Marital status, % | ||||||||||
| Single, never married | 14.8 | 17.9* | 9.5 | 11.5 | 38.9 | 40.7 | 19.4 | 224* | 23.9 | 23.6 |
| Married/cohabitating | 67.1 | 62.3* | 71.6 | 67.8 | 42.3 | 40.6 | 66.9 | 58.6 | 62.6 | 66.0* |
| Separated/divorced | 12.0 | 12.2 | 12.1 | 11.4 | 12.6 | 14.9 | 10.4 | 15.0* | 9.6 | 9.4 |
| Widowed | 6.1 | 7.6* | 6.8 | 9.3* | 6.2 | 3.7 | 3.4 | 4.1 | 3.9 | 1.1 |
| Participant characteristics | ||||||||||
| History of heart attack | 3.7 | 2.9 | 4.8 | 2.8 | 1.9 | 3.3 | 0.2 | 2.8* | 2.9 | 3.3 |
| History of stroke | 2.1 | 4.3* | 2.6 | 3.8 | 0 | 7.0 | 0.8 | 5.3* | 4.3 | 1.2 |
| History of hypertension | NA | 36.8 | NA | 36.4 | NA | 57.6 | NA | 28.4 | NA | 30.4 |
| History of diabetes mellitus | 10.2 | 12.5* | 10.1 | 11.1 | 13.4 | 25.9* | 9.1 | 7.9 | 9.0 | 13.5 |
| Ever use of ≥1 technology-enabled devices to monitor/improve health | NA | 54.5 | NA | 54.1 | NA | 48.8 | NA | 57.3 | NA | 62.0 |
Data were weighted by age, race/ethnicity, educational attainment, household income, and region to reflect the composition of the US population of women ≥25 years of age who speak English according to distributions reported in the US Census Bureau’s March 2018 Current Population Survey.11 AHA indicates American Heart Association; NA, not available; and NH, non-Hispanic.
P<0.05 vs 2009.
Table 2 shows the percentages of respondents who correctly identified warning signs of a heart attack. For nearly every heart attack symptom, fewer women in 2019 identified the possible warning sign compared with 2009, both overall and within each racial/ethnic group. This difference was statistically significant overall and among non-Hispanic White women for 7 of 13 symptoms and among non-Hispanic Black and Hispanic women for 3 symptoms. For example, awareness of the symptom tightness of the chest declined from 17.1% in 2009 to 5.7% in 2019, a decline that was similar across racial/ethnic groups. Notably, awareness of chest pain and shortness of breath as symptoms increased significantly over time among women ≥65 years of age, whereas awareness of these symptoms declined non-significantly in women 25 to 34 years of age.
Table 2.
US Women’s Awareness of the Warning Signs and Symptoms of a Heart Attack: 2009 and 2019
| Race/Ethnicity | Age, y | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | NH White | NH Black | Hispanic | NH Asian | 25–34 | 35–44 | 45–64 | ≥65 | ||||||||||
| 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | 2009 | 2019 | |
| n | 1158 | 1345 | 634 | 660 | 127 | 209 | 251 | 216 | 125 | 201 | 205 | 278 | 305 | 284 | 455 | 525 | 193 | 258 |
| Warning signs, %* | ||||||||||||||||||
| Chest pain | 52.4 | 51.5† | 53.5 | 57.3 | 52.2 | 39.2 | 46.3 | 40.7 | 50.6 | 37.2 | 60.7 | 42.0 | 50.3 | 43.9 | 51.7 | 54.8 | 49.8 | 59.8† |
| Pain that spreads to the shoulders, neck, or arms | 44.8 | 38.3 | 48.6 | 46.0 | 33.4 | 33.3 | 39.0 | 24.1 | 29.2 | 15.9 | 38.3 | 25.6 | 40.3 | 29.4† | 45.7 | 40.7 | 52.8 | 51.9† |
| Shortness of breath | 34.4 | 27.9 | 34.0 | 30.1 | 35.0 | 24.6 | 34.2 | 24.8 | 38.7 | 26.8 | 42.5 | 27.4 | 25.1 | 24.5 | 37.2 | 24.1† | 33.3 | 36.8† |
| Numbness | 20.9 | 13.1† | 19.9 | 12.8† | 27.3 | 8.6† | 20.4 | 18.0 | 18.8 | 8.9 | 28.8 | 13.8 | 27.9 | 13.0† | 19.4 | 16.2 | 10.4 | 7.7 |
| Nausea | 9.7 | 9.3 | 11.7 | 10.2 | 0.5 | 8.3† | 7.6 | 7.1 | 4.8 | 5.8 | 5.4 | 1.7 | 5.9 | 6.1 | 11.5 | 13.0 | 13.9 | 12.5 |
| Pain in jaw | 13.2 | 8.2† | 15.3 | 11.0† | 5.9 | 3.1 | 12.2 | 2.5† | 5.3 | 3.5 | 6.3 | 3.5 | 9.3 | 2.7† | 15.3 | 11.0 | 18.6 | 11.8 |
| Heaviness/pressure on the chest | NA | 7.9 | NA | 9.7 | NA | 5.5 | NA | 4.3 | NA | 5.5 | NA | 1.8 | NA | 5.2 | NA | 8.2 | NA | 14.5 |
| Sweating | 9.9 | 6.8 | 10.6 | 6.8† | 8.8 | 10.2 | 8.1 | 5.2 | 5.9 | 6.2 | 8.1 | 1.7† | 3.8 | 4.5 | 13.5 | 9.2 | 11.0 | 9.2 |
| Fatigue | 10.1 | 6.6 | 10.8 | 7.8 | 9.9 | 4.7 | 8.4 | 3.7 | 3.8 | 7.8 | 4.3 | 5.3 | 5.7 | 4.9 | 14.1 | 5.5† | 11.6 | 10.7 |
| Back pain | 10.6 | 6.1† | 13.3 | 7.3† | 3.2 | 4.0 | 5.0 | 3.8 | 7.1 | 3.0 | 4.5 | 3.0 | 5.3 | 3.8 | 12.5 | 10.3 | 17.6 | 4.2† |
| Tightness of the chest | 17.1 | 5.7† | 17.8 | 6.1† | 18.2 | 6.3† | 15.3 | 4.0† | 11.2 | 3.3 | 16.1 | 6.0 | 16.8 | 6.4† | 18.7 | 6.0† | 15.1 | 4.3† |
| Dizziness | 11.0 | 5.6† | 10.7 | 5.4† | 7.9 | 6.8 | 16.5 | 3.8† | 13.0 | 9.3 | 13.2 | 3.5† | 12.1 | 5.2† | 12.6 | 4.9† | 5.3 | 8.7† |
| Indigestion | 7.0 | 2.7† | 8.0 | 3.5† | 3.5 | 1.3 | 5.4 | 1.2 | 1.0 | 1.3 | 0.9 | 1.0 | 3.7 | 1.1† | 11.0 | 3.1† | 7.8 | 4.8 |
Data were weighted by age, race/ethnicity, educational attainment, household income, and region to reflect the composition of the US population of women ≥25 years of age who speak English according to distributions reported in the US Census Bureau’s March 2018 Current Population Survey.11 NA indicates not available; and NH, non-Hispanic.
Other responses at <5% overall in both years: pain/unease discomfort (unspecified), tingling sensation, headache, increased heart rate/palpitation, pain on left side of body, heartburn, fainting, feeling unwell, stomach pain, vomiting, anxiety, heartache, high blood pressure, slurred speech, cold sweat, blurred vision, irregular heart rate, tightness of the body, mental disorientation, high cholesterol, clamminess, toothache, overweight/obesity, pasty complexion, slow heart rate, none, do not know, and refused.
Significantly different from values of 2009, P<0.05.
Supplemental Table II shows responses for the first action to take when having a heart attack. Although the proportion of women reporting that they would call 9-1-1 was higher in 2019 compared with 2009 (54.4% versus 47.5%, respectively; P<0.05), the proportion who would take aspirin was lower in 2019 compared with 2009 (14.3% versus 23.4%, respectively; P<0.05), with similar patterns across age groups and race/ethnicity except non-Hispanic Asians. A higher proportion of women would alert someone/call/ask for help in 2019 compared with 2009 (7.6% versus 4.4%, respectively; P<0.05); however, this was an infrequent response in both years.
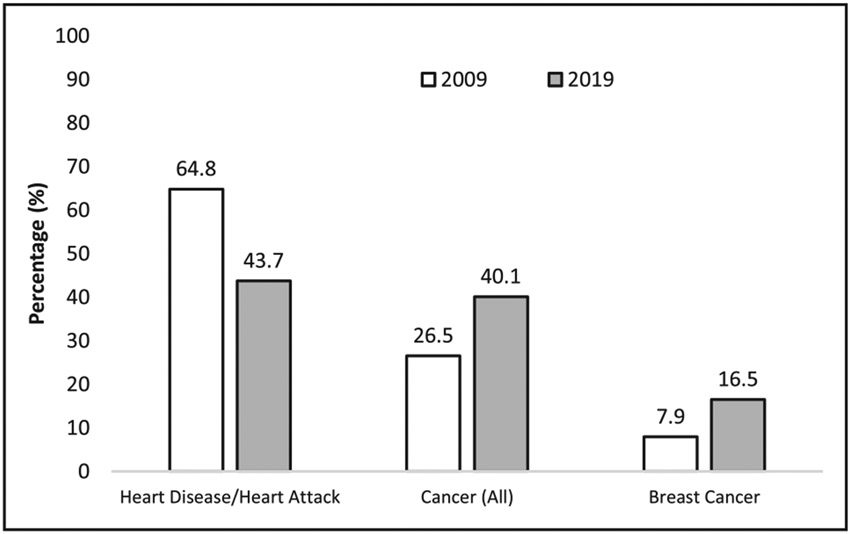
The Figure shows the percentages of women who identified heart disease/heart attack, cancer (all), or breast cancer as the LCOD among women. Overall, although heart disease/heart attack remained the most frequently identified LCOD among women, recognition was far lower in 2019 compared with 2009 (43.7% versus 64.8%; P<0.05). In 2019, significantly greater proportions of women than in 2009 identified cancer (all) (40.1% versus 26.5%; P<0.05) and breast cancer (16.5% versus 7.9%; P<0.05) as the LCOD (both P<0.05).
Figure. Proportion of US women identifying heart disease/heart attack, cancer (all), or breast cancer as the leading cause of death among women: 2009 vs 2019.
All values between 2009 and 2019, P<0.05.
We conducted multivariable analyses for awareness of heart disease as the LCOD in each survey year (Table 3). In 2019, non-Hispanic Black, Hispanic, and non-Hispanic Asian women were substantially less likely to identify heart disease as the LCOD among women (58%, 59%, and 67% less likely, respectively) compared with non-Hispanic White women, even after accounting for age, educational attainment, household income, and history of heart attack, stroke, and diabetes mellitus. Similar associations were observed in 2009, although the differences for non-Hispanic Black and Hispanic women were smaller compared with those in 2019. Among women surveyed in 2019, there was a positive linear relationship between awareness and educational attainment, with women completing postgraduate education being >10 times as likely to identify heart disease as the LCOD compared with women with less than a high school education. In 2009, education was also significantly associated with awareness, but the gradient was less steep. No consistent trends were observed between household income and awareness in either year.
Table 3.
Multivariable Analysis of Associations Between Participant Sociodemographic Characteristics and Likelihood of Identifying Heart Disease/Heart Attack as the LCOD Among US Women ≥25 Years of Age in 2009 and 2019
| 2009* | 2019* | 2019† | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (per 10 y) | 1.03 | 0.94–1.12 | 1.39‡ | 1.28–1.51‡ | 1.42‡ | 1.31–1.55‡ |
| Race/ethnicity | ||||||
| NH White | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |||
| NH Black | 0.70 | 0.47–1.04 | 0.42‡ | 0.29–0.63‡ | 0.46‡ | 0.31–0.68‡ |
| Hispanic | 0.61‡ | 0.42–0.90‡ | 0.41‡ | 0.29–0.59‡ | 0.40‡ | 0.28–0.58‡ |
| NH Asian | 0.30‡ | 0.17–0.53‡ | 0.33‡ | 0.20–0.55‡ | 0.33‡ | 0.20–0.54‡ |
| Other | 0.73 | 0.26–2.13 | 0.63 | 0.34–1.18 | 0.62 | 0.33–1.15 |
| Educational attainment | ||||||
| Less than high school | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |||
| High school graduate | 1.83‡ | 1.01–3.33‡ | 2.59‡ | 1.20–6.32‡ | 2.44‡ | 1.13 −5.96‡ |
| Some college | 2.40‡ | 1.31–4.46‡ | 5.42‡ | 2.48–13.34‡ | 5.12‡ | 2.34–12.61‡ |
| College graduate | 3.44‡ | 1.81–6.63‡ | 8.53‡ | 3.88–21.17‡ | 7.87‡ | 3.57–19.54‡ |
| Postgraduate | 4.09‡ | 1.89–9.14‡ | 10.80‡ | 4.66–27.92‡ | 10.13‡ | 4.38–26.19‡ |
| Household income, $ | ||||||
| <35,000 | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | |||
| 35 000–49 999 | 1.00 | 0.66–1.53 | 1.23 | 0.80–1.87 | 1.22 | 0.80–1.87 |
| 50 000–74 999 | 1.08 | 0.73–1.60 | 1.21 | 0.82–1.79 | 1.26 | 0.85–1.86 |
| 75 000–99 999 | 2.23‡ | 1.36–3.72‡ | 0.82 | 0.54–1.25 | 0.82 | 0.54–1.25 |
| ≥100 000 | 1.94‡ | 1.27–2.98‡ | 0.93 | 0.66–1.32 | 0.95 | 0.67–1.34 |
| Participant characteristics | ||||||
| History of heart attack | 2.31‡ | 1.07–5.58‡ | 0.82 | 0.38–1.77 | 0.88 | 0.40–1.91 |
| History of stroke | 2.53 | 0.94–8.38 | 0.94 | 0.49–1.76 | 0.95 | 0.50–1.79 |
| History of diabetes mellitus | 1.17 | 0.76–1.84 | 0.87 | 0.58–1.28 | 0.97 | 0.64–1.44 |
| History of hypertension | NA | NA | 0.70‡ | 0.54–0.92‡ | ||
Data were weighted by age, race/ethnicity, educational attainment, household income, and region to reflect the composition of the US population of women ≥25 years of age who speak English according to distributions reported in the US Census Bureau’s March 2018 Current Population Survey.11 LCOD indicates leading cause of death; NA, not available; NH, non-Hispanic; OR, odds ratio; and Ref, reference group.
All variables shown are included in the model.
Additionally adjusted for history of hypertension (available only in 2019).
P<0.05.
In multivariable analyses for each survey year (Table 3), in 2009, there were strong positive associations between history of heart attack and stroke, but not diabetes mellitus, and awareness of heart disease as the LCOD; these associations were not present in 2019. Only in 2019 were women asked about hypertension history, and women with hypertension had lower knowledge that heart disease was the LCOD (OR, 0.70 [95% CI, 0.54–0.92]) after accounting for all other factors shown in Table 3. Use of at least 1 technology-enabled device to improve or monitor health was not associated with awareness in 2019 (OR, 0.93 [95% CI, 0.72–1.20]) in the multivariable model (data not shown). Neither a history of hypertension nor use of technology affected the ORs for the other variables in Table 3.
In analyses comparing responses between years, women surveyed in 2019 compared with 2009 were 74% less likely to identify heart disease as the LCOD among women after accounting for differences over time in age, race/ethnicity, educational attainment, and household income (OR, 0.36 [95% CI, 0.29–0.45]; Table 4). After adjustment for other factors, Hispanic women had the largest decrease in this knowledge over time (OR, 0.14 [95% CI, 0.07–0.28]), followed by non-Hispanic Black (OR, 0.33 [95% CI, 0.16–0.67]), non-Hispanic Asian (OR, 0.39 [95% CI, 0.16–0.91]), and non-Hispanic White women (OR, 0.41 [95% CI, 0.32–0.53]). Among age groups, younger women (25–34 years) had the largest decrease in this knowledge (OR, 0.19 [95% CI, 0.10–0.34]), whereas there was no decrease among women ≥65 years of age.
Table 4.
Ten-Year Change in Awareness and Likelihood (OR) of Identifying Heart Disease/Heart Attack, Cancer (All), or Breast Cancer as the LCOD Among US Women by Age and Race/Ethnicity, 2019 vs 2009*
| Heart Disease/Heart Attack | Cancer (All) | Breast Cancer | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Absolute % Difference 2009–2019 |
Unadjusted OR (95% CI) |
Adjusted† OR (95% CI) |
Absolute % Difference 2009–2019 |
Unadjusted OR (95% CI) |
Adjusted† OR (95% CI) |
Absolute % Difference 2009–2019 |
Unadjusted OR (95% CI) |
Adjusted† OR (95% CI) |
|
| Overall | −21.2 | 0.42 (0.36–0.49)‡ |
0.36 (0.29–0.45)‡ |
13.6 | 1.86 (1.57–2.20)‡ |
1.96 (1.58–2.44)‡ |
8.6 | 2.31 (1.79–2.99)‡ |
2.59 (1.86–3.67)‡ |
| Race/ethnicity | |||||||||
| NH White | −16.6 | 0.49 (0.40–0.60)‡ |
0.41 (0.32–0.53)‡ |
8.9 | 1.54 (1.25–1.91)‡ |
1.70 (1.30–2.23)‡ |
5.5 | 1.91 (1.37–2.71)‡ |
2.21 (1.43–3.48)‡ |
| NH Black | −28.1 | 0.31 (0.19–0.49)‡ |
0.33 (0.16–0.67)‡ |
25.8 | 2.96 (1.85–2.40)‡ |
2.25 (1.14–4.50)‡ |
20.8 | 3.74 (2.05–7.16)‡ |
4.76 (1.99–12.52)‡ |
| Hispanic | −28.9 | 0.28 (0.17–0.44)‡ |
0.14 (0.07–0.28)‡ |
17.5 | 2.04 (1.32–3.18)‡ |
2.84 (1.52–5.44)‡ |
11.4 | 2.21 (1.23–4.11)‡ |
4.35 (1.78–12.11)‡ |
| NH Asian | −19.4 | 0.44 (0.22–0.86)‡ |
0.39 (0.16–0.91)‡ |
15.5 | 1.96 (0.99–3.99) |
2.31 (1.02–5.48)‡ |
8.0 | 2.64 (0.83–11.04) |
2.46 (0.65–11.90) |
| Age groups, y | |||||||||
| 25–34 | −41.3 | 0.17 (0.11–0.25)‡ |
0.19 (0.10–0.34)‡ |
26.0 | 3.14 (2.09–4.76)‡ |
3.25 (1.83–5.97)‡ |
19.1 | 6.16 (3.13–13.65)‡ |
4.04 (1.67–11.35)‡ |
| 35–44 | −18.1 | 0.48 (0.34–0.68)‡ |
0.47 (0.29–0.74)‡ |
9.4 | 1.52 (1.06–2.20)‡ |
1.34 (0.83–2.18) |
6.9 | 1.74 (1.07–2.88)‡ |
2.05 (1.05–4.10)‡ |
| 45–64 | −22.6 | 0.39 (0.30–0.51)‡ |
0.26 (0.19–0.37)‡ |
14.1 | 1.90 (1.45–2.50)‡ |
2.49 (1.75–3.57)‡ |
7.7 | 2.45 (1.57–3.92)‡ |
3.38 (1.88–6.35)‡ |
| ≥65 | −5.7 | 0.78 (0.55–1.09) |
1.37 (0.84–2.23) |
6.6 | 1.39 (0.96–2.02) |
0.86 (0.52–1.41) |
3.5 | 1.42 (0.84–2.43) |
1.11 (0.55–2.32) |
Data were weighted by age, race/ethnicity, educational attainment, household income, and region to reflect the composition of the US population of women ≥25 years of age who speak English according to distributions reported in the US Census Bureau’s March 2018 Current Population Survey.11 LCOD indicates leading cause of death; NH, non-Hispanic; and OR, odds ratio.
ORs interpreted as likelihood of identifying the cause of death as the LCOD in 2019 compared with 2009 (eg, the referent group is the prevalence in 2009).
Adjusted models include the following covariates: age (except in models stratified by age), race/ethnicity (except in models stratified by race/ethnicity), educational attainment, household income, history of heart attack, stroke, and diabetes mellitus (hypertension not available in 2009).
P<0.05.
Women in 2019 were 1.96-fold more likely to identify cancer (all) as the LCOD among women (OR, 1.96 [95% CI, 1.58–2.44]), 2.59-fold more likely to identify breast cancer as the LCOD among women (OR, 2.59 [95% CI, 1.86–3.67]), and 74% less likely to identify heart disease as the LCOD (OR, 0.36 [95% CI, 0.29–0.45]) compared with women in 2009 (Table 4). Non-Hispanic Black and Hispanic women and younger women (25–34 years of age) had greater increases over time than other groups in likelihood to identify cancer (all) or breast cancer as the LCOD.
DISCUSSION
The 2019 national AHA Survey of Women’s Cardiovascular Disease Awareness provides the most recent information on awareness of heart disease as the LCOD among women in the United States, as well as their knowledge about heart attack warning signs and what actions to take if someone were having a heart attack. The greatest proportion of women surveyed in both years indicated heart disease as the LCOD, but, concerningly, the proportion declined markedly between 2009 and 2019. Compared with 2009, after accounting for differences in participant characteristics across surveys, women in 2019 were 64% (95% CI, 55–71) less likely to know that heart disease is the LCOD among women. This decline in awareness was most evident among women 25 to 34 years of age and Hispanic women but was striking among women of every racial/ethnic group and in every age category except women ≥65 years of age. Women surveyed in 2019 were more than twice as likely as in 2009 to incorrectly identify breast cancer as the LCOD. In 2018, heart disease was the LCOD among women (300 977 deaths), all cancers (ie, malignant neoplasms) ranked as the second leading cause (283 721), and breast cancer was the cause of death for 42 466 US women.2 Thus, heart disease accounts for nearly 7 times as many deaths among women compared with breast cancer.
In both surveys, higher educational attainment was strongly related to awareness that heart disease is the LCOD. Women at high CVD risk (heart disease or stroke) had higher awareness than women without these conditions in 2009, but this was not seen in 2019. Diabetes mellitus was not associated with awareness in either survey, whereas in 2019 (not asked in 2009), women with hypertension had 30% lower awareness than women without hypertension.
Some findings on heart disease awareness were similar to those in the AHA’s 2012 survey7 in which awareness was lower among younger compared with older women and among non-Hispanic Black and Hispanic women compared with non-Hispanic Whites. In the current report, we extend these findings by examining differences in awareness across a 10-year span, showing lower awareness in 2019 in all non-White racial/ethnic groups and lower awareness among women with than without hypertension. In addition, the higher awareness among women with history of heart attack or stroke demonstrated in 2009 was not present in 2019.
The concerning marked decline in awareness of heart disease as the LCOD among women indicates a need for renewed efforts to educate women, particularly younger women, Hispanic and non-Hispanic Black women, those with lower levels of education, and women with history of heart attack, stroke, and cardiovascular risk factors. Observed trends may partly explain findings that the proportion of young women 35 to 54 years of age having an acute myocardial infarction increased over the past 2 decades, accompanied by a rising burden of risk factors such as hypertension and diabetes mellitus.13 In the current AHA survey, younger women were less likely to report leading a heart-healthy lifestyle and were more likely to identify multiple barriers to leading a heart-healthy lifestyle, including lack of time, stress, and lack of confidence (data not shown). According to NHANES (National Health and Nutrition Examination Survey) data, low percentages of people <40 years of age achieve ideal status on the 7 key health behaviors and factors espoused by AHA,1,14 pointing out the significant opportunity for improvement in this younger population.
Risk conversations with younger women are lacking and may contribute to decreasing rates of awareness. In the VIRGO study (Variation in Recover: Role of Gender on Outcomes of Young AMI Patients), only half of patients <55 years of age presenting with an acute myocardial infarction considered themselves at risk for heart disease before their event, despite a high overall prevalence of cardiac risk factors. Women were less likely than men to be told by their physician that they were at risk of CVD or to have a conversation about risk reduction.15 In the past decade, little progress has been made in increasing physician uptake of CVD risk assessment and preventive care for women.16 The lack of awareness and counseling is likely multi-factorial and may be related to lack of tools to assess cardiovascular risk in younger age groups,16,17 inconsistent use of preventive care,18 and misperceptions that young women are not at risk.18 Because obstetrician/gynecologists act as primary care providers for many young women, recent recommendations have encouraged obstetrician/gynecologists to incorporate cardiovascular screening and counseling into the well-woman examination.19,20
Multilevel interventions evaluating how to change behavior to prevent future CVD are urgently needed, especially among Hispanic, Black, and Asian women and women with lower educational attainment. Providing culturally appropriate education and care within community structures and community health worker interventions may be particularly effective for women.21-24
Limitations of this survey merit discussion. It was conducted entirely online, so generalizability to populations averse to online participation or without access should be considered. Potential limited internet access among women with lower household income may have resulted in limited representation among women experiencing the greatest socioeconomic disparities. Results were compared with the prior online survey sample to establish trends, but unmeasured characteristics of people tending to respond to online surveys might differ over time, especially by age, introducing potential bias. In 2019, the use of technology-enabled devices to improve health was common and was not associated with heart disease awareness, suggesting a small impact of this type of bias. Because the survey was performed only in English, we may have underestimated health-related awareness levels because limited English proficiency is associated with poorer health status.25,26 Although the results of the analyses were weighted by age, race/ethnicity, educational attainment, household income, and region to reflect the composition of the English-speaking US population of women ≥25 years of age, limitations still exist with regard to how well these approaches allow generalization of findings to the overall US population.
Strengths of this study include longitudinal survey administration in predominant US racial/ethnic groups and the ability to adjust for differences in survey respondent characteristics within and across time.
CONCLUSIONS
Awareness that heart disease is the LCOD among women was lower in 2019 than 2009 according to standardized AHA surveys and independent of differences in participant characteristics over time. This concerning decline was observed in women of all ages except those ≥65 years of age and in all racial/ethnic groups and was greatest among women <34 years of age and racial/ethnic groups.
FUTURE DIRECTIONS
Results suggest an urgent call to action to identify underlying causes of the concerning trends in women’s awareness and to redouble efforts to reverse them. Escalation of efforts to educate women through awareness campaigns, cardiovascular screening, and counseling is needed. Ultimately, these efforts may reduce the ranking of heart disease as the leading cause of death in US women.
Supplementary Material
Footnotes
The American Heart Association makes every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
Supplemental material is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/CIR.0000000000000907.
Disclosures
| Writing Group Member |
Employment | Research Grant |
Other Research Support |
Speakers’ Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Mary Cushman | University of Vermont | None | None | None | None | None | None | None |
| Virginia J. Howard |
University of Alabama at Birmingham | NIH-NINDS† | None | None | None | None | None | None |
| Monik C. Jiménez |
Brigham and Women’s Hospital | NIH-NINDS† | None | None | None | None | None | Salary: Brigham and Women’s Hospital/Harvard Medical School† |
| Jennifer Lewey | University of Pennsylvania | None | None | None | None | None | None | None |
| Jean C. McSweeney | University of Arkansas for Medical Sciences | None | None | None | None | None | None | None |
| Lori J. Mosca | Columbia University | AHA* | None | Amarin* | None | Amarin* | Amarin* | AHA* |
| L. Kristin Newby | Duke University, Duke Clinical Research Institute |
Boehringer Ingelheim* |
None | None | None | None | None | None |
| Ram Poudel | American Heart Association |
None | None | None | None | None | None | None |
| Kathryn M. Rexrode | Brigham and Women’s Hospital, Harvard Medical School | NIH† | None | None | None | None | None | None |
| Harmony R. Reynolds | New York University | None | None | None | None | None | None | None |
| Christina M. Shay |
American Heart Association |
None | None | None | None | None | None | None |
| Mario Sims | University of Mississippi | None | None | None | None | None | None | None |
| Reviewer | Employment | Research Grant |
Other Research Support |
Speakers’ Bureau/ Honoraria |
Expert Witness |
Ownership Interest |
Consultant/ Advisory Board |
Other |
|---|---|---|---|---|---|---|---|---|
| Norrina B. Allen | Northwestern University |
None | None | None | None | None | None | None |
| Matthew A. Allison | University of California, San Diego | None | None | None | None | None | None | None |
| Laxmi S. Mehta | The Ohio State University | None | None | None | None | None | None | None |
| Tochi M. Okwuosa | Rush University Medical Center | None | None | None | None | None | None | None |
REFERENCES
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. ; on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2019 update: a report from the American Heart Association [published correction appears in Circulation. 2020;141:e33]. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999–2018 on CDC WONDER Online Database, released in 2020. http://wonder.cdc.gov/ucd-icd10.html. Accessed April 28, 2020. [Google Scholar]
- 3.Robertson RM. Women and cardiovascular disease: the risks of misperception and the need for action. Circulation. 2001;103:2318–2320. doi: 10.1161/01.cir.103.19.2318 [DOI] [PubMed] [Google Scholar]
- 4.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women’s awareness of heart disease: an American Heart Association national study. Circulation. 2004;109:573–579. doi: 10.1161/01.CIR.0000115222.69428.C9 [DOI] [PubMed] [Google Scholar]
- 5.Christian AH, Rosamond W, White AR, Mosca L. Nine-year trends and racial and ethnic disparities in women’s awareness of heart disease and stroke: an American Heart Association national study. J Womens Health (Larchmt). 2007;16:68–81. doi: 10.1089/jwh.2006.M072 [DOI] [PubMed] [Google Scholar]
- 6.Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelveyear follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3:120–127. doi: 10.1161/CIRCOUTCOMES.109.915538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mosca L, Hammond G, Mochari-Greenberger H, Towfighi A, Albert MA; on behalf of the American Heart Association Cardiovascular Disease and Stroke in Women and Special Populations Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on High Blood Pressure Research, and Council on Nutrition, Physical Activity and Metabolism. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013;127:1254–1263, e1-e9. doi: 10.1161/CIR.0b013e318287cf2f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wendelboe AM, McCumber M, Hylek EM, Buller H, Weitz JI, Raskob G; ISTH Steering Committee for World Thrombosis Day. Global public awareness of venous thromboembolism. J Thromb Haemost. 2015;13:1365–1371. doi: 10.1111/jth.13031 [DOI] [PubMed] [Google Scholar]
- 9.Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. American Heart Association Women’s Heart Disease and Stroke Campaign Task Force. Arch Fam Med. 2000;9:506–515. doi: 10.1001/archfami.9.6.506 [DOI] [PubMed] [Google Scholar]
- 10.Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, Burdick KA, Simpson SL. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–534. doi: 10.1161/CIRCULATIONAHA.105.588103 [DOI] [PubMed] [Google Scholar]
- 11.US Census Bureau. Current Population Survey (CPS). https://www.census.gov/programs-surveys/cps.html. Accessed November 9, 2019. [Google Scholar]
- 12.R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2014. https://www.R-project.org/. Accessed January 6, 2020. [Google Scholar]
- 13.Arora S, Stouffer GA, Kucharska-Newton AM, Qamar A, Vaduganathan M, Pandey A, Porterfield D, Blankstein R, Rosamond WD, Bhatt DL, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139:1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003-2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leifheit-Limson EC, D’Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM, Lichtman JH. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol. 2015;66:1949–1957. doi: 10.1016/j.jacc.2015.08.859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bairey Merz CN, Andersen H, Sprague E, Burns A, Keida M, Walsh MN, Greenberger P, Campbell S, Pollin I, McCullough C, et al. Knowledge, attitudes, and beliefs regarding cardiovascular disease in women: the Women’s Heart Alliance. J Am Coll Cardiol. 2017;70:123–132. doi: 10.1016/j.jacc.2017.05.024 [DOI] [PubMed] [Google Scholar]
- 17.Gooding HC, Ning H, Gillman MW, Shay C, Allen N, Goff DC Jr, Lloyd-Jones D, Chiuve S. Application of a lifestyle-based tool to estimate premature cardiovascular disease events in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) study. JAMA Intern Med. 2017;177:1354–1360. doi: 10.1001/jamainternmed.2017.2922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lichtman JH, Leifheit-Limson EC, Watanabe E, Allen NB, Garavalia B, Garavalia LS, Spertus JA, Krumholz HM, Curry LA. Symptom recognition and healthcare experiences of young women with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2015;8(suppl 1):S31–S38. doi: 10.1161/CIRCOUTCOMES.114.001612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown HL, Warner JJ, Gianos E, Gulati M, Hill AJ, Hollier LM, Rosen SE, Rosser ML, Wenger NK; on behalf of the American Heart Association and the American College of Obstetricians and Gynecologists. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory from the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137:e843–e852. doi: 10.1161/CIR.0000000000000582 [DOI] [PubMed] [Google Scholar]
- 20.Petterson SM, Bazemore AW, Phillips RL, Rayburn WF. Trends in office-based care for reproductive-aged women according to physician specialty: a ten-year study. J Womens Health (Larchmt). 2014;23:1021–1026. doi: 10.1089/jwh.2014.4765 [DOI] [PubMed] [Google Scholar]
- 21.Altman R, Nunez de Ybarra J, Villablanca AC. Community-based cardiovascular disease prevention to reduce cardiometabolic risk in Latina women: a pilot program. J Womens Health (Larchmt). 2014;23:350–357. doi: 10.1089/jwh.2013.4570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Villablanca AC, Warford C, Wheeler K. Inflammation and cardiometabolic risk in African American women is reduced by a pilot community-based educational intervention. J Womens Health (Larchmt). 2016;25:188–199. doi: 10.1089/jwh.2014.5109 [DOI] [PubMed] [Google Scholar]
- 23.Hurtado M, Spinner JR, Yang M, Evensen C, Windham A, Ortiz G, Tracy R, Ivy ED. Knowledge and behavioral effects in cardiovascular health: Community Health Worker Health Disparities Initiative, 2007-2010. Prev Chronic Dis. 2014;11:E22. doi: 10.5888/pcd11.130250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kangovi S, Mitra N, Norton L, Harte R, Zhao X, Carter T, Grande D, Long JA. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: a randomized clinical trial. JAMA Intern Med. 2018;178:1635–1643. doi: 10.1001/jamainternmed.2018.4630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jacobs EA, Karavolos K, Rathouz PJ, Ferris TG, Powell LH. Limited English proficiency and breast and cervical cancer screening in a multiethnic population. Am J Public Health. 2005;95:1410–1416. doi: 10.2105/AJPH.2004.041418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gee GC, Ponce N. Associations between racial discrimination, limited English proficiency, and health-related quality of life among 6 Asian ethnic groups in California. Am J Public Health. 2010;100:888–895. doi: 10.2105/AJPH.2009.178012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.