Abstract
The shipping fever (SF) and Kansas (Ka) strains of bovine parainfluenza virus type 3 (BPIV3) are restricted in their replication in rhesus monkeys 100- to 1,000-fold compared to human parainfluenza virus type 3 (HPIV3), and the Ka strain also was shown to be attenuated in humans. To initiate an investigation of the genetic basis of the attenuation of BPIV3 in primates, we produced viable chimeric HPIV3 recombinants containing the nucleoprotein (N) open reading frame (ORF) from either BPIV3 Ka or SF in place of the HPIV3 N ORF. These chimeric recombinants were designated cKa-N and cSF-N, respectively. Remarkably, cKa-N and cSF-N grew to titers comparable to those of their HPIV3 and BPIV3 parents in LLC-MK2 monkey kidney and Madin-Darby bovine kidney cells. Thus, the heterologous nature of the N protein did not impede replication in vitro. However, cKa-N and cSF-N were each restricted in replication in rhesus monkeys to a similar extent as Ka and SF, respectively. This identified the BPIV3 N protein as a determinant of the host range restriction of BPIV3 in primates. These chimeras thus combine the antigenic determinants of HPIV3 with the host range restriction and attenuation phenotype of BPIV3. Despite their restricted replication in rhesus monkeys, the chimeric viruses induced a level of resistance to HPIV3 challenge in these animals which was indistinguishable from that conferred by immunization with HPIV3. The infectivity, attenuation, and immunogenicity of these BPIV3/HPIV3 chimeras suggest that the modified Jennerian approach described in the present report represents a novel method to design vaccines to protect against HPIV3-induced disease in humans.
Human parainfluenza virus type 3 (HPIV3) and bovine parainfluenza virus type 3 (BPIV3) are enveloped, nonsegmented negative-strand RNA viruses within the Respirovirus genus of the family Paramyxoviridae (8). HPIV3 is a common cause of serious lower respiratory tract infection in infants and children less than 1 year of age (8, 9, 23), but a vaccine has not yet been licensed for HPIV3-induced disease. Since BPIV3 and HPIV3 have been shown to be 25% related antigenically by reciprocal cross-neutralization studies (6) and share neutralizing epitopes on their HN and F surface glycoproteins (7, 21), BPIV3 is being evaluated for use as a live-virus vaccine to protect humans against HPIV3-induced disease. The use of a naturally occurring animal pathogen to immunize humans against the counterpart human pathogen was pioneered by Jenner 200 years ago to control smallpox. In the Jennerian approach to vaccine development, an antigenically related animal virus that is restricted in replication in humans is used as a vaccine to protect against the related human disease. BPIV3 strains Kansas (Ka) and shipping fever (SF) were restricted in their replication in the upper and lower respiratory tracts of rhesus monkeys relative to HPIV3, induced antibodies that cross-neutralized HPIV3, and conferred resistance to challenge with HPIV3 (6). BPIV3 Ka was found to be attenuated, infectious, and immunogenic in chimpanzees (6), as well as in seronegative human infants (18), the primary population targeted for prophylaxis against HPIV3-induced disease. In addition, it retained its attenuation phenotype after replication in human vaccinees (18). Thus, BPIV3 was attenuated in three species of primates, evidence of an in vivo host range restriction.
HPIV3 and BPIV3 are essentially identical in genome organization. Both virus groups possess a single-stranded negative-sense RNA genome that encodes nine proteins: three nucleocapsid-associated proteins, the nucleoprotein (N), the phosphoprotein (P), and the large polymerase protein (L); an accessory protein (C) encoded by the second open reading frame (ORF) in the P mRNA; an internal matrix protein (M); and two envelope-associated proteins, the fusion (F) and the hemagglutinin-neuraminidase (HN) glycoproteins, which are the major neutralization and protective antigens (8). BPIV3 also encodes two other proteins by RNA editing of the P mRNA. The insertion of a single G residue at the editing site, located midway in the P locus, shifts the reading frame to fuse the upstream half of the P ORF to an internal ORF to encode the chimeric D protein (25). Insertion of two G residues fuses the upstream half of the P ORF to a second internal ORF to encode the chimeric V protein (25). HPIV3 also edits in the same way to encode a D protein (14). HPIV3 has a V ORF, but it is separated from the editing site by several stop codons. Biological data from gene knockout viruses suggest that the HPIV3 D and V ORFs encode significant proteins, albeit ones which are not essential for virus replication in vitro or in vivo (11).
A comparison of the nucleotide sequences of the genomes of three BPIV3 and two HPIV3 strains shows a high degree of identity in their leader, trailer, gene end, intergenic, and gene start sequences, whereas BPIV3 and HPIV3 protein sequences are more divergent; the five viruses display amino acid sequence identities ranging from 58.6% among P proteins to 89.6% among M proteins (1). It was of interest to determine which BPIV3 genes or genome regions are responsible for the host range restriction in replication in the respiratory tracts of rhesus monkeys, chimpanzees, and humans.
Our strategy to identify the genes or genome regions that confer the attenuation phenotype is to systematically substitute BPIV3 coding or noncoding sequences for their HPIV3 counterparts in a full-length infectious HPIV3 cDNA using the recently described reverse genetics techniques (10, 16), followed by evaluation of the recovered BPIV3/HPIV3 chimeric viruses in seronegative rhesus monkeys and, ultimately, in humans. As a first step, we have replaced the N ORF of wild-type (wt) HPIV3 strain JS with its counterpart from BPIV3 strain Ka or SF. The Ka and SF strains of BPIV3, which are 98.3% related in overall nucleotide sequence homology (1), were chosen as donors of the BPIV3 N ORF since (i) each virus was shown to be attenuated in primates and (ii) an attenuation phenotype identified in the BPIV3/HPIV3 chimeric viruses could be ascribed to the sequences shared by the two BPIV3 strains. The studies were initiated with the N ORF because, among the parainfluenza type 3 (PIV3) proteins, the BPIV3 and HPIV3 N proteins possess an intermediate level of amino acid sequence identity (84.7%), and it was thought that a BPIV3/HPIV3 N recombinant might be viable yet also might have novel properties. The N ORF substitution was accomplished using recombinant HPIV3 (JS strain) (10) as the recipient and the Ka or SF strain as the donor. In each case, a viable chimeric virus was successfully produced, designated cKa-N or cSF-N, respectively. Surprisingly, the two chimeric viruses replicated in vitro as efficiently as their HPIV3 and BPIV3 parents. However, in rhesus monkeys, cKa-N and cSF-N each replicated to a level comparable to that of their BPIV3 parents but to levels significantly lower than that of their HPIV3 parent. The restricted replication of cKa-N and cSF-N in monkeys but not in tissue culture identifies the BPIV3 N ORF as a host range determinant that attenuates BPIV3 in primates, a finding that has application for the design of a live attenuated vaccine for HPIV3.
MATERIALS AND METHODS
Viruses and cells.
BPIV3 wt strain Ka/15626/84 (clone 5-2-4, lot BPI3-1) was previously described (3, 19); the virus preparation used in the present work is identical in passage level to that currently undergoing clinical evaluation. The prototype BPIV3 wt strain SF (ATCC 281-VR) was obtained from the American Type Culture Collection, Manassas, Va. The JS wt recombinant virus (rJS) was described previously (10). The rJS, Ka, and SF viruses and the two BPIV3/HPIV3 chimeras were propagated at 32°C in LLC-MK2 rhesus monkey kidney cells (ATCC CCL-7) as described previously (15) or in Madin-Darby bovine kidney (MDBK) cells (ATCC CCL-22). The modified vaccinia (strain Ankara) recombinant virus that expresses bacteriophage T7 RNA polymerase (MVA-T7) was provided by B. Moss and L. Wyatt (31). HEp-2 (ATCC CCL-23), LLC-MK2, and MDBK cells were maintained in minimal essential medium (Life Technologies, Gaithersburg, Md.) supplemented with 5% fetal bovine serum, gentamicin at 50 μg/ml, and 4 mM glutamine at 37°C.
Construction of full-length chimeric BPIV3/HPIV3 antigenomic cDNA.
In previous work, the BPIV3 Ka and SF N genes were amplified from virion RNA (vRNA) isolated from virus amplified in LLC-MK2 cells and sequenced completely from reverse transcription (RT)-PCR products, yielding a complete consensus sequence for each genome (GenBank accession no. AF178654 and AF178655, respectively) (1). This information was used as a guide to prepare cDNA clones of the Ka and SF N genes. vRNA (0.5 μg) was reverse transcribed using the SuperScript Preamplification System (Life Technologies) and 200 ng of random hexamer primers. The PCR was carried out on the first-strand cDNA product using the Advantage cDNA PCR kit (Clontech Laboratories, Palo Alto, Calif.) and primers spanning nucleotides (nt) 1 to 26 (forward) and 1862 to 1898 (reverse) of the BPIV3 genome. The BPIV3 N cDNAs were cloned into pBluescript KS II (Stratagene, La Jolla, Calif.) using ClaI sites included in the PCR primers, producing plasmids pKa-N and pSF-N. The nucleotide sequences of cDNA inserts were determined by automated DNA sequencing using the Taq DYE Deoxy Terminator cycle sequencing kit (ABI, Foster City, Calif.). cDNA clones whose N ORF sequences exactly matched the above-mentioned consensus sequence for the BPIV3 Ka or SF genome were identified and used as templates for the mutagenesis preceding importation of the N ORF into the rJS backbone. The HPIV3 JS N gene represented in the complete antigenomic cDNA was subcloned as a 1,905-bp MluI/EcoRI fragment from previously described plasmid p(Left+2G) (10), which contains nt 1 to 7437 of the HPIV3 rJS antigenome, into pUC119 (Pharmacia Biotech, Uppsala, Sweden), producing pJS-N. Site-directed mutagenesis was then performed on pKa-N, pSF-N, and pJS-N using the method of Kunkel et al. (22) by the MUTA-GENE procedure (Bio-Rad, Hercules, Calif.) to introduce NcoI and AflII restriction enzyme sites at the N translation start and stop sites, respectively. The primers used to mutagenize the Ka and SF N gene were 5′-CGAATAGACTCACCATGGTTACAGTC (forward primer relative to positive sense) and 5′-CTCTTTGTGCTTAAGTGCTTCCG (italics identify the restriction enzyme site; the translation start and stop sites are in boldface), resulting in plasmids designated pKaN-NcoI/AflII and pSFN-NcoI/AflII, respectively. The mutagenic primers used to amplify the JS N gene were 5′-GGCTCACCATGGTTGAAATTATAGAG (forward) and 5′-GTTGATTCGCTTAAGTGCTTCC (reverse), producing pJSN-NcoI/AflII. The N ORFs of pKaN-NcoI/AflII and pSFN-NcoI/AflII were cloned individually in place of the JS N ORF in the NcoI/AflII window of pUC119JSN-NcoI/AflII, producing plasmids pB/HKaN-NcoI/AflII and pB/HSFN-NcoI/AflII. A second round of site-directed mutagenesis removed the NcoI and AflII sites and restored authentic HPIV3 and BPIV3 sequences adjacent to the start and stop codons using mutagenic primers 5′-CTCTATAATTTCAAAAATGTTGAGTCTATTCG and 5′-CGGAAGCAACTAGTCGAATCAAC, producing pB/HKa-N and pB/HSF-N. Existing MluI and EcoRI sites in the rJS sequence of pB/HKa-N and pB/HSF-N were used to clone the chimeric BPIV3/HPIV3 N genes into the rJS plasmid p(Left+2G) (10) using conventional cloning techniques, producing plasmids pLeftKa-N and pLeftSF-N. The XhoI-NgoMI fragment of p(Right+), containing an antigenomic copy of the rJS sequence from nt 7438 to nt 15,462 as previously described (10), was cloned into the XhoI/NgoMI window of pLeftKa-N and pLeftSF-N to produce pB/HPIV3Ka-N and pB/HPIV3SF-N, respectively. pB/HPIV3Ka-N and pB/HPIV3SF-N each encode a complete antigenomic analog of HPIV3 RNA, with the N ORF replaced with that of either Ka or SF, flanked by a T7 promoter and a delta ribozyme/T7 terminator at the 5′ and 3′ ends of the antigenomes, respectively.
Transfection.
HEp-2 cells (approximately 1.5 × 106 per well of a six-well dish) were grown to 90% confluence and transfected with two previously described support plasmids, 0.2 μg of pTM(P no C) (11) and 0.1 μg of pTM(L) (10), along with 5 μg of pB/HPIV3Ka-N or pB/HPIV3SF-N and 12 μl of LipofectACE (Life Technologies). Each transfection mixture also contained 1.5 × 107 PFU of MVA-T7, as previously described (10). The cultures were incubated at 32°C for 12 h, after which the medium was replaced with minimal essential medium (Life Technologies) containing 10% fetal bovine serum. The cultures were incubated at 32°C for an additional 3 days, after which the transfection harvests were passaged onto LLC-MK2 cell monolayers in T25 flasks and incubated for 5 days at 32°C. Viruses recovered in the supernatant were plaque purified three times prior to amplification and characterization. The chimeric viruses containing the Ka and SF N ORFs were designated cKa-N and cSF-N, respectively.
Molecular characterization of recovered chimeric recombinants.
The presence in cKa-N and cSF-N of a BPIV3 N ORF in the rJS backbone was confirmed by amplification of a region spanning nt 1 to 1898 of the HPIV3 genome from vRNA of plaque-purified recombinant viruses by RT-PCR followed by TaqI digestion. The nucleotide sequences on both sides of the BPIV3 N ORF start and stop sites were determined by automated DNA sequencing of the amplified products using the Taq DYE Deoxy Terminator cycle sequencing kit (ABI).
Replication of HPIV3/BPIV3 chimeras in cell culture.
The multicycle replication of rJS, Ka, SF, cKa-N, and cSF-N in MDBK and LLC-MK2 cells was determined by infecting cells in triplicate at a multiplicity of infection (MOI) of 0.01 and harvesting samples at 24-h intervals over a 6-day period as previously described (30). Samples were flash frozen and titers were determined simultaneously on LLC-MK2 cell monolayers in 96-well plates as previously described (11).
Monkey studies.
Rhesus monkeys, which were seronegative for PIV3 as determined by hemagglutination inhibition (HAI) assay (6), were inoculated intranasally and intratracheally in groups of four with 105 PFU of either cKa-N, cSF-N, rJS, Ka, or SF as previously described (13). Nasopharyngeal swabs were collected on 14 consecutive days, starting with the day of inoculation (day 0). Tracheal lavage samples were collected on days 2, 4, 6, 8, and 10 postinfection. Individual samples were flash frozen and stored at −70°C until all of the samples were available for titration. The virus titer in the specimens was determined on LLC-MK2 cell monolayers in 96-well plates as previously described (11). The mean log10 tissue culture-infective doses (TCID50) per milliliter were calculated per virus for each day sampled. Serum collected from monkeys on days 0 and 28 was tested by HAI assay using HPIV3 (JS strain) and BPIV3 (Ka strain) as the antigen as previously described (6). On day 42 postinoculation, the monkeys were challenged intranasally and intratracheally with 106 PFU of biologically derived wt HPIV3 strain JS. Nasopharyngeal swab samples were collected on days 3, 4, 5, 6, 7, and 8 postchallenge. Tracheal lavage samples were collected on days 4, 6, and 8 postchallenge. The virus titer in specimens was determined in a single assay as described above.
RESULTS
Recovery of chimeric BPIV3/HPIV3.
To initiate identification of the genetic determinants of the host range restriction of BPIV3 in primates, chimeric BPIV3/HPIV3 antigenomic cDNAs encoding a Ka or SF N ORF as a replacement for its HPIV3 counterpart in an HPIV3 JS backbone (pB/HPIV3Ka-N and pB/HPIV3SF-N, respectively) were constructed. The substitutions thus involved only the protein-coding sequences, and all of the noncoding flanking sequence, including the transcription start and stop signals, remained undisturbed. The chimeric antigenome plasmids were transfected along with support plasmids expressing the HPIV3 P and L proteins into HEp-2 cells with MVA-T7 as described previously (12). An N support plasmid was omitted from the transfections, as it was found to be dispensable for recovery of HPIV3 following cDNA transfection, presumably because the transfected, antigenomic plasmids pB/HPIV3Ka-N and pB/HPIV3SF-N express sufficient levels of the N protein, as was reported for wt HPIV3 cDNA (16).
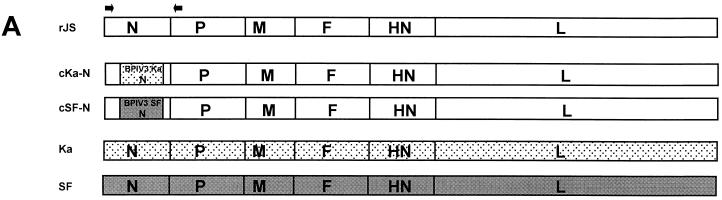
Both chimeric cDNAs directed the recovery of infectious viruses, which were designated cKa-N and cSF-N. To confirm that the recovered viruses were indeed chimeric recombinants possessing the correct structure, the N genes were amplified from vRNA by RT-PCR for analysis (Fig. 1). These amplified products and corresponding RT-PCR products from HPIV3 rJS and BPIV3 Ka or SF were subjected to TaqI digestion. TaqI digestion was predicted to produce a unique profile of digestion products for each of the three parental and two chimeric viruses, which would provide positive identification of each of the five viruses. The three parental viruses and the recovered cKa-N and cSF-N recombinants each produced the expected TaqI digestion pattern (Fig. 1). The chimeric identity of cKa-N and cSF-N was also analyzed by nucleotide sequence analysis of the RT-PCR products, which confirmed the presence of the Ka or SF N ORF flanked by JS noncoding sequence (data not shown).
FIG. 1.
Features of the BPIV3/HPIV3 chimeric genomes and their confirmation by TaqI digestion of RT-PCR products generated from vRNA. (A) The genomes of the chimeric cKa-N and cSF-N viruses are shown schematically (not to scale) relative to those of the HPIV3 and BPIV3 parents. Arrows above the rJS genome indicate the locations of primers used for RT-PCR amplification of chimeric and parent viruses for diagnostic TaqI digestion and sequence analysis. These primers were directed to regions conserved between HPIV3 and BPIV3 so that they could be used for the amplification of HPIV3, BPIV3, and BPIV3/HPIV3 chimeras. (B) Expected sizes of TaqI digestion products for each virus are shown. TaqI fragments which are unique to each virus and therefore serve in virus identification are indicated by stars. (C) TaqI profiles of RT-PCR products containing the PIV3 N coding region of chimeric cKa-N (left) and cSF-N (right) are shown flanked by those of the HPIV3 and BPIV3 parents. RT-PCR products (1.9 kb) containing the PIV3 N coding region and flanking sequence were amplified from virion RNA using primers whose locations are shown in (panel A) and subjected to digestion with TaqI. Unique TaqI fragments diagnostic of virus identity and corresponding to those identified in panel B are indicated by stars. Calculated lengths of DNA gel bands are indicated.
BPIV3/HPIV3 chimeras replicate efficiently in cell culture.
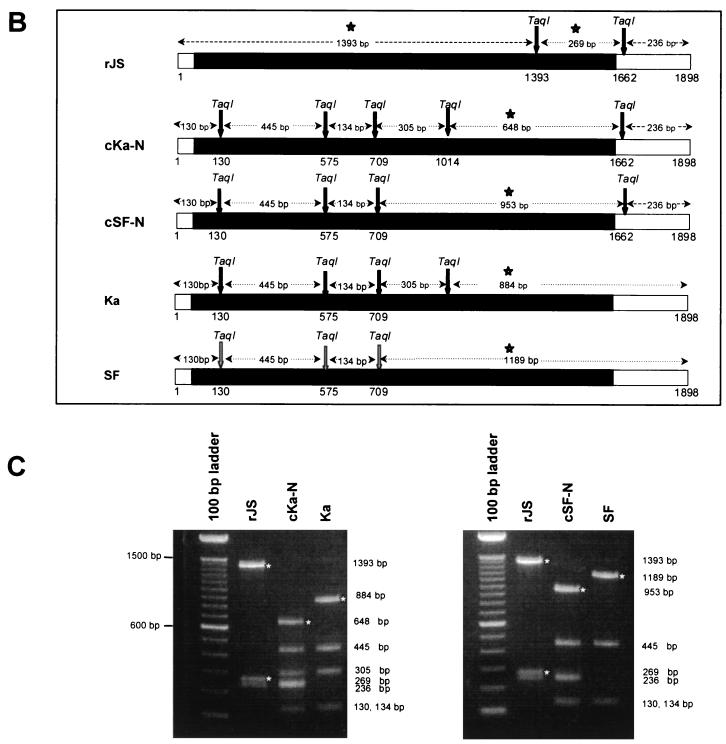
The multicycle replication of cKa-N, cSF-N, and their parental viruses rJS, Ka, and SF in a bovine cell line (MDBK) or in a rhesus monkey cell line (LLC-MK2) was analyzed by infecting parallel cultures of cells with the various individual viruses, each in triplicate at an MOI of 0.01, and harvesting samples over a 6-day period (Fig. 2). The chimeric viruses replicated to similar titers and with similar kinetics in both cell lines, like their human and bovine parental viruses. There was no evidence of a delay in replication or a significant reduction in the maximum virus titer achieved. In each case, cKa-N and cSF-N replicated to over 107.0 TCID50/ml, suggesting that the presence of the heterologous BPIV3 N protein in the HPIV3 background did not significantly reduce multicycle replication in either of the two cell lines studied.
FIG. 2.
Multicycle growth of parental and chimeric viruses in MDBK (A) or LLC-MK2 (B) cells. Monolayers of MDBK (A) or LLC-MK2 (B) cells in wells (9.6 cm2 each) of a six-well plate were infected at an MOI of 0.01 with the indicated parental or chimeric virus. Three replicate infections were performed with each virus. Samples were taken at the indicated time points and stored at −70°C, and the TCID50 of each sample was determined in one assay. Growth curves were constructed using the average of three replicate samples at each time point. The lower limit of virus detectability was 101.5 TCID50/ml, which is indicated by a horizontal dotted line.
The BPIV3 N ORF confers attenuation in rhesus monkeys.
The rJS, Ka, and SF parental viruses were compared to the cKa-N and cSF-N chimeric viruses for the ability to replicate in the upper and lower respiratory tracts of rhesus monkeys. Each virus was administered intranasally and intratracheally at a dose of 105.0 TCID50 per site. The kinetics of viral replication in the upper and lower respiratory tracts, as well as the mean peak titer at each site, were quantified for each virus and are presented in Table 1. The cKa-N and cSF-N recombinants were significantly attenuated in the upper respiratory tract, exhibiting a 60-fold or a 30-fold reduction, respectively, in mean peak virus titer compared to the level of replication of rJS (Table 1). The mean peak titer of each chimera in the upper respiratory tract was somewhat greater than that of its BPIV3 parent, but the difference was not statistically significant. Both cKa-N and cSF-N were also attenuated modestly in the lower respiratory tract compared to rJS, but this difference was statistically significant only for cSF-N. The low level of replication of rJS in the lower respiratory tract made it difficult to compare differences in replication at this site, but the mean peak titers of the two chimeric viruses were very similar to those of the two parental BPIV3 strains. Thus, the substitution of the N ORF of either Ka or SF into rJS attenuated the human virus in rhesus monkeys to a level resembling that of the BPIV3 parent.
TABLE 1.
Substitution of the BPIV3 N ORF into HPIV3 confers host range restriction in the upper and lower respiratory tracts of rhesus monkeys
| Immunizing virusa | Mean titerb (log10 TCID50/ml ± SE [Duncan grouping])f
|
Mean peak titere (log10 TCID50/ml ± SE [Duncan grouping])f
|
||||
|---|---|---|---|---|---|---|
| Nasopharyngeal swabc
|
Tracheal lavaged
|
Nasopharyngeal swab | Tracheal lavage | |||
| Day 6 | Day 7 | Day 4 | Day 6 | |||
| rJS | 5.3 ± 0.59 (A) | 3.9 ± 0.36 (A) | 1.7 ± 0.45 (A) | 1.7 ± 0.29 (A) | 5.3 ± 0.59 (A) | 2.5 ± 0.51 (A) |
| cKa-N | 3.0 ± 0.58 (B) | 2.9 ± 0.42 (AB) | 1.5 ± 0.40 (A) | 1.0 ± 0.19 (A) | 3.5 ± 0.54 (B) | 1.5 ± 0.18 (AB) |
| Ka | 2.0 ± 0.27 (B) | 2.4 ± 0.30 (B) | 1.3 ± 0.26 (A) | 1.3 ± 0.21 (A) | 2.5 ± 0.30 (B) | 1.6 ± 0.15 (AB) |
| cSF-N | 3.3 ± 0.40 (B) | 3.7 ± 0.57 (A) | 1.1 ± 0.25 (A) | 1.1 ± 0.24 (A) | 3.8 ± 0.46 (B) | 1.4 ± 0.26 (B) |
| SF | 2.8 ± 0.48 (B) | 2.6 ± 0.40 (AB) | 1.6 ± 0.46 (A) | 1.5 ± 0.40 (A) | 3.3 ± 0.28 (B) | 1.8 ± 0.41 (AB) |
Monkeys (four per group) were inoculated intranasally and intratracheally with 105 TCID50/ml in 1 ml at each site.
Virus titrations were performed by TCID50 assay on LLC-MK2 cells. Mean viral titers in each column were assigned to statistically similar groups (designated with a letter) using a Duncan multiple-range test (α = 0.05). Within each column, mean titers with different letters are statistically significantly different. Titers followed by AB are not significantly different from those followed by either A or B.
Nasopharyngeal swab samples were collected for 14 days; data from a subset of these days are shown.
Tracheal lavage samples were collected on days 2, 4, 6, 8, and 10 postinfection; data from a subset of these days are shown.
The mean peak titer was defined as the mean of the highest virus titer achieved by each of four animals in a virus group over the entire course of virus shedding.
The limit of virus titer detectability was 101 TCID50/ml.
Chimeric HPIV3 strains bearing a BPIV3 N ORF induce a high level of resistance to wt HPIV3 challenge.
To evaluate the protective efficacy of cKa-N and cSF-N, rhesus monkeys previously immunized with rJS, Ka, SF, cKa-N, or cSF-N were challenged intratracheally and intranasally with 106 TCID50 of biologically derived wt JS virus on day 42 postimmunization. Peak titers of the challenge virus were significantly reduced in the upper and lower respiratory tracts of monkeys previously immunized with parental or chimeric viruses compared to those of unimmunized animals (Table 2). The protection conferred by cKa-N or cSF-N against replication of HPIV3 challenge in the upper respiratory tract was statistically indistinguishable from that conferred by immunization with rJS or SF and was marginally greater than that conferred by the parental Ka strain. An increase in efficacy of a chimeric virus compared to that of its BPIV3 parent would not be unexpected, since the chimeric viruses bear the homologous HPIV3 HN and F protective antigens, whereas the SF and Ka BPIV3 parents are only 25% related antigenically to HPIV3, as shown by neutralization assays (6). The degree of protection conferred in the lower respiratory tract was high and was statistically indistinguishable among the chimeric and parental viruses. These data confirm that, despite their reduced growth in rhesus monkeys relative to rJS, the cKa-N and cSF-N chimeric viruses induced a protective immunity to HPIV3 infection that was comparable to that induced by rJS. Although cKa-N and cSF-N were highly attenuated in the upper and lower respiratory tracts of rhesus monkeys relative to rJS, each chimeric virus induced a HAI antibody response to HPIV3 that was 2.5- to 5-fold greater in magnitude than that induced by immunization with its respective BPIV3 parent. This likely is due to the presence of the HPIV3 HN protein in the chimeric viruses. Furthermore, the HPIV3-specific HAI responses induced by the chimeric viruses were statistically indistinguishable from that induced by immunization with rJS. One unexpected and favorable finding, which remains unexplained, is that, following challenge of the monkeys with HPIV3, the level of HAI antibody in monkeys initially immunized with cKa-N or cSF-N was significantly greater than levels observed in animals immunized with rJS, Ka, or SF.
TABLE 2.
Rhesus monkeys previously infected with chimeric BPIV3/HPIV3 manifest a high level of resistance to replication of wt HPIV3 challenge virus
| Virus used for initial infection (day 0)d | Mean peak JS challenge virus titer (log10 TCID50/ml ± SE [Duncan grouping])e in:
|
Mean reciprocal log2 serum HAI antibody titerc for HPIV3d
|
||
|---|---|---|---|---|
| Nasopharyngeal swaba (log10 TCID50/ml ± SE [Duncan grouping])e | Tracheal lavageb | Day 42 | Day 70 | |
| None | 5.1 ± 0.22 (A) | 4.6 ± 0.26 (A) | ≤1.0 ± 0 (D) | 11.0 ± 0 (AB) |
| rJS | 2.2 ± 0.18 (BC) | 1.6 ± 0.06 (B) | 9.2 ± 0.25 (AB) | 9.5 ± 0.29 (C) |
| cKa-N | 2.6 ± 0.57 (BC) | 1.5 ± 0 (B) | 9.8 ± 0.25 (A) | 12.0 ± 0 (A) |
| Ka | 3.0 ± 0.4 (B) | 1.6 ± 0.12 (B) | 7.5 ± 0.5 (C) | 9.0 ± 0.71 (C) |
| cSF-N | 1.8 ± 0.16 (C) | 1.6 ± 0.11 (B) | 9.8 ± 0.25 (A) | 11.2 ± 0.75 (A) |
| SF | 2.6 ± 0.57 (BC) | 1.5 ± 0 (B) | 8.5 ± 0.29 (B) | 9.8 ± 0.25 (BC) |
Nasopharyngeal swab samples were collected on days 3, 4, 5, 6, 7, and 8 postchallenge.
Tracheal lavage samples were collected on days 4, 6, and 8 postchallenge.
Serum samples used for the HAI assay were collected on the day of challenge (day 42) and on day 28 postchallenge (day 70).
Monkeys (four per group) were challenged with JS intranasally and intratracheally (106 TCID50 in 1 ml at each site) 42 days after initial immunization. All monkeys had a serum HAI titer to HPIV3 of ≤1.0 prior to the initial infection on day 0.
The titer (TCID50/ml) of virus present in each specimen was determined using LLC-MK2 cells, and the mean peak titers for four animals were determined as described for Table 1. Mean peak viral titers in each column were assigned to statistically similar groups (designated with a letter) using a Duncan multiple-range test (α = 0.05). Mean titers in each column with different letters are statistically significantly different.
DISCUSSION
BPIV3 and HPIV3 replicate efficiently in bovine and primate cells in vitro, but BPIV3 is highly restricted for replication in the respiratory tracts of primates compared to HPIV3. This constitutes an in vivo host range restriction, one which is of considerable interest for the development of a vaccine against HPIV3. On one hand, efficient growth in vitro is necessary for the manufacture of a vaccine virus, and on the other hand, the host range restriction attenuates virus replication and virulence in the human vaccinee. We wanted to identify the genetic determinant(s) of the host range restriction of BPIV3 and determine whether this phenotype could be transferred to HPIV3. As a first step in the present study, we replaced the N ORF of HPIV3 strain JS with its counterpart from BPIV3 strain SF or Ka.
One possible and undesirable outcome might have been that these N replacement chimeric viruses would be defective for growth due to incompatibility between the BPIV3 and HPIV3 components. However, this was not observed. Instead, the two BPIV3/HPIV3 chimeric viruses replicated efficiently in multicycle growth in vitro in cells of bovine or rhesus monkey origin. Indeed, these viruses could not be distinguished from their HPIV3 and BPIV3 parents on the basis of growth fitness in vitro.
Analysis of in vivo host range restriction was performed with rhesus monkeys. This is a suitable animal model because both SF and Ka are attenuated in the upper and lower respiratory tracts of rhesus monkeys compared to HPIV3 (6), and this restriction correlates with attenuation in fully susceptible seronegative infants and children (19). In rhesus monkeys, the two chimeric viruses were highly restricted compared to HPIV3 and the level of attenuation was nearly equivalent to that of the BPIV3 parent. This indicates that the N ORF is a determinant of the host range restriction of BPIV3. Since the N ORFs from two distinct strains of BPIV3 conferred similar levels of host range restriction, it is likely that this phenotype is an authentic host range property. The observation that the chimeric viruses were slightly less attenuated than their BPIV3 parents suggests that one or more additional genes or genetic elements also contribute to the host range restriction. Despite their restricted replication, the chimeric viruses induced a level of HPIV3-specific serum antibodies which equalled or exceeded that induced by wt HPIV3 and provided a high level of resistance to replication of the challenge virus, wt HPIV3.
The basis for the host range restriction of cKa-N and cSF-N presumably lies in the encoded BPIV3 N protein. The formal possibility exists that nucleotide differences within the ORF are involved, but this seems highly unlikely since the cis-acting elements of paramyxoviruses have largely been defined and do not lie in the N ORF. The N proteins of HPIV3 and BPIV3 are 85% identical, with an average of 79 differences in a total of 515 amino acids (1). In a five-way comparison of two HPIV3 and three BPIV3 N protein sequences, 58 of the 79 variable amino acids were designated “host specific” by virtue of the presence of a specific amino acid assignment in the three BPIV3 sequences and a different assignment at that position in both HPIV3 sequences (1). These differences were distributed over the length of the protein, with a concentration in the C terminus (1). Although some of these 58 host-specific residues might be coincidental, they also presumably include ones which arose during the evolution of HPIV3 and BPIV3 in their respective natural hosts and represent adaptation to those hosts. Thus, these differences presumably include ones responsible for the host range restriction of BPIV3 in the nonnatural primate host. However, residues that do not fit this host-specific definition might also be involved, particularly if they are conserved between Ka and SF irrespective of their conservation among the HPIV3 strains. It will be important to define the specific amino acids responsible for the host range restriction by constructing chimeric viruses containing defined portions of BPIV3 N.
The use of animal viruses that are attenuated in humans because of a host range restriction is the basis of the Jennerian approach to vaccine development. The identification of genetic determinants, other than those encoding protective epitopes, that specify the host range phenotype of an animal virus has made it possible to create modified Jennerian vaccine viruses (i.e., animal-human chimeras) that are attenuated in humans due to host range restriction but possess the protective antigens of the human virus. For example, the recently licensed quadrivalent rotavirus vaccine exploits the host range restriction of rhesus rotavirus (RRV) in humans. Since there is a need for a multivalent vaccine that induces resistance to each of the four major human rotavirus serotypes, three single gene reassortant viruses each containing 10 RRV genes plus a single human rotavirus gene that coded for the major neutralization antigen (VP7) of serotype 1, 2, or 4 were combined with RRV itself, which is highly related antigenically to the serotype 3 human rotavirus (17). The quadrivalent vaccine provided a high level of efficacy against human rotavirus infection in infants and young children (26).
As another example, reassortant viruses possessing the gene segments encoding the hemagglutinin and neuraminidase surface glycoproteins from a human influenza A virus and the six remaining gene segments from an avian influenza A virus were attenuated in humans (4, 24, 28). This indicated that one or more of the six gene segments of the avian virus attenuated the avian-human influenza A viruses for humans. The genetic determinants of this attenuation were mapped using reassortant viruses possessing a single gene segment from an attenuating avian influenza A virus and the remaining genes from a human strain. This analysis revealed that the nonstructural, polymerase (PB1 and PB2), and M genes contributed to the attenuation phenotype of avian influenza A viruses in humans (5). This illustrates that a number of genes contribute to the host range restriction phenotype of avian influenza A virus in primates. We expect that multiple determinants will typically specify the host range phenotypes of Jennerian and modified Jennerian vaccines, although this has not been well studied. Thus, although introduction of the BPIV3 N ORF into the HPIV3 background resulted in a level of host range restriction nearly equivalent to that of BPIV3, it is premature to conclude that N is the primary determinant of this phenotype. Instead, it is equally possible that strong attenuation effects will also be observed when other BPIV3 genes or genetic elements are transferred individually into HPIV3. The transfer of other individual BPIV3 ORFs into HPIV3 is in progress.
Chimeric recombinant viruses containing genetically stable, attenuating sequences from BPIV3 and the protective epitopes of HPIV3 are novel vaccine candidates that might overcome the potential limitations of two promising existing candidate vaccines, namely, cold-adapted HPIV3 strain cp45 (2, 20) and BPIV3 strain Ka (18). The attenuation phenotype of cp45 is specified by at least 5 of the 20 nt that vary between cp45 and its wt parent (27, 29). Although the attenuation phenotype of cp45 has been stable in vitro and in vivo in studies to date, it is possible that evidence of instability will emerge when this candidate vaccine is administered to larger numbers of individuals. If attenuation of BPIV3/HPIV3 chimeras based on host range restriction involves more amino acids than were found to contribute to the attenuation of cp45, it is likely that these chimeric viruses would be more stable genetically. This can be better evaluated when more information is available on the specific amino acids within BPIV3 N which are involved in the host range restriction of cKa-N and cSF-N and when other BPIV3 genes have been evaluated for their host range effects. With regard to the use of BPIV3 itself as a vaccine virus for HPIV3, this has the drawback that BPIV3 and HPIV3 are only 25% related antigenically based on in vitro neutralization (6). This drawback is overcome by a recombinant virus such as cKa-N or cSF-N, which combines the host range restriction of BPIV3 with the major protective HN and F antigens of HPIV3.
The level of replication of cKa-N and cSF-N in the upper and lower respiratory tracts of rhesus monkeys was statistically indistinguishable from that of their BPIV3 parent. Since Ka has proven to be safe and infectious in infants younger than 6 months (18), it is possible that cKa-N and cSF-N would also be well tolerated in this age group, which constitutes the target population for prophylaxis against HPIV3 disease. Thus, these chimeric viruses might be suitable HPIV3 vaccines. It is also possible that cKa-N and cSF-N will replicate to a slightly higher level than Ka, as they did in rhesus monkeys in the present study, and retain some residual virulence for human infants. This could be reduced by the importation of additional BPIV3 genes or other attenuating mutations. The data reported in the present study, which demonstrate the attenuation and protective efficacy of cKa-N and cSF-N in rhesus monkeys, provide a foundation for the evaluation of these chimeric viruses as candidate vaccines in humans.
ACKNOWLEDGMENTS
We thank Ernest Williams, Jr., and Chris Cho for expert technical assistance in performing serological assays. We are grateful to Robert Chanock and Alex Schmidt for review of the manuscript.
REFERENCES
- 1.Bailly, J. E., J. M. McAuliffe, M. H. Skiadopoulos, P. L. Collins, and B. R. Murphy. Sequence determination and molecular analysis of two strains of bovine parainfluenza virus type 3 that are attenuated for primates. Virus Genes, in press. [DOI] [PubMed]
- 2.Belshe R B, Hissom F K. Cold adaptation of parainfluenza virus type 3: induction of three phenotypic markers. J Med Virol. 1982;10:235–242. doi: 10.1002/jmv.1890100403. [DOI] [PubMed] [Google Scholar]
- 3.Clements M L, Belshe R B, King J, Newman F, Westblom T U, Tierney E L, London W T, Murphy B R. Evaluation of bovine, cold-adapted human, and wild-type human parainfluenza type 3 viruses in adult volunteers and in chimpanzees. J Clin Microbiol. 1991;29:1175–1182. doi: 10.1128/jcm.29.6.1175-1182.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clements M L, Sears S D, Christina K, Murphy B R, Snyder M H. Comparison of the virologic and immunologic responses of volunteers to live avian-human influenza A H3N2 reassortant virus vaccines derived from two different avian influenza virus donors. J Clin Microbiol. 1989;27:219–222. doi: 10.1128/jcm.27.1.219-222.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clements M L, Subbarao E K, Fries L F, Karron R A, London W T, Murphy B R. Use of single-gene reassortant viruses to study the role of avian influenza A virus genes in attenuation of wild-type human influenza A virus for squirrel monkeys and adult human volunteers. J Clin Microbiol. 1992;30:655–662. doi: 10.1128/jcm.30.3.655-662.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coelingh K, Winter C C, Tierney E L, London W T, Murphy B R. Attenuation of bovine parainfluenza virus type 3 in nonhuman primates and its ability to confer immunity to human parainfluenza virus type 3 challenge. J Infect Dis. 1988;157:655–662. doi: 10.1093/infdis/157.4.655. [DOI] [PubMed] [Google Scholar]
- 7.Coelingh K J, Winter C C, Murphy B R, Rice J M, Kimball P C, Olmsted R A, Collins P L. Conserved epitopes on the hemagglutinin-neuraminidase proteins of human and bovine parainfluenza type 3 viruses: nucleotide sequence analysis of variants selected with monoclonal antibodies. J Virol. 1986;60:90–96. doi: 10.1128/jvi.60.1.90-96.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collins P L, Chanock R M, McIntosh K. Parainfluenza viruses. In: Fields B N, Knipe D M, Howley P M, Chanock R M, Melnick J L, Monath T P, Roizman B, Straus S E, editors. Fields virology. 3rd ed. Vol. 1. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 1205–1243. [Google Scholar]
- 9.Crowe J E., Jr Current approaches to the development of vaccines against disease caused by respiratory syncytial virus (RSV) and parainfluenza virus (PIV). A meeting report of the WHO Programme for Vaccine Development. Vaccine. 1995;13:415–421. doi: 10.1016/0264-410x(95)98266-d. [DOI] [PubMed] [Google Scholar]
- 10.Durbin A P, Hall S L, Siew J W, Whitehead S S, Collins P L, Murphy B R. Recovery of infectious human parainfluenza virus type 3 from cDNA. Virology. 1997;235:323–332. doi: 10.1006/viro.1997.8697. [DOI] [PubMed] [Google Scholar]
- 11.Durbin A P, McAuliffe J M, Collins P L, Murphy B R. Mutations in the C, D, and V open reading frames of human parainfluenza virus type 3 attenuate replication in rodents and primates. Virology. 1999;261:319–330. doi: 10.1006/viro.1999.9878. [DOI] [PubMed] [Google Scholar]
- 12.Durbin A P, Siew J W, Murphy B R, Collins P L. Minimum protein requirements for transcription and RNA replication of a minigenome of human parainfluenza virus type 3 and evaluation of the rule of six. Virology. 1997;234:74–83. doi: 10.1006/viro.1997.8633. [DOI] [PubMed] [Google Scholar]
- 13.Durbin A P, Wyatt L S, Siew J, Moss B, Murphy B R. The immunogenicity and efficacy of intranasally or parenterally administered replication-deficient vaccinia-parainfluenza virus type 3 recombinants in rhesus monkeys. Vaccine. 1998;16:1324–1330. doi: 10.1016/s0264-410x(98)00010-3. [DOI] [PubMed] [Google Scholar]
- 14.Galinski M S, Troy R M, Banerjee A K. RNA editing in the phosphoprotein gene of the human parainfluenza virus type 3. Virology. 1992;186:543–550. doi: 10.1016/0042-6822(92)90020-P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall S L, Stokes A, Tierney E L, London W T, Belshe R B, Newman F C, Murphy B R. Cold-passaged human parainfluenza type 3 viruses contain ts and non-ts mutations leading to attenuation in rhesus monkeys. Virus Res. 1992;22:173–184. doi: 10.1016/0168-1702(92)90049-f. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman M A, Banerjee A K. An infectious clone of human parainfluenza virus type 3. J Virol. 1997;71:4272–4277. doi: 10.1128/jvi.71.6.4272-4277.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kapikian A Z, Vesikari T, Ruuska T, Madore H P, Christy C, Dolin R, Flores J, Green K Y, Davidson B L, Gorziglia M, et al. An update on the “Jennerian” and modified “Jennerian” approach to vaccination of infants and young children against rotavirus diarrhea. Adv Exp Med Biol. 1992;327:59–69. doi: 10.1007/978-1-4615-3410-5_8. [DOI] [PubMed] [Google Scholar]
- 18.Karron R A, Makhene M, Gay K, Wilson M H, Clements M L, Murphy B R. Evaluation of a live attenuated bovine parainfluenza type 3 vaccine in two- to six-month-old infants. Pediatr Infect Dis J. 1996;15:650–654. doi: 10.1097/00006454-199608000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Karron R A, Wright P F, Hall S L, Makhene M, Thompson J, Burns B A, Tollefson S, Steinhoff M C, Wilson M H, Harris D O, Clements M L, Murphy B R. A live attenuated bovine parainfluenza virus type 3 vaccine is safe, infectious, immunogenic, and phenotypically stable in infants and children. J Infect Dis. 1995;171:1107–1114. doi: 10.1093/infdis/171.5.1107. [DOI] [PubMed] [Google Scholar]
- 20.Karron R A, Wright P F, Newman F K, Makhene M, Thompson J, Samorodin R, Wilson M H, Anderson E L, Clements M L, Murphy B R, Belshe R B. A live human parainfluenza type 3 virus vaccine is attenuated and immunogenic in healthy infants and children. J Infect Dis. 1995;172:1445–1450. doi: 10.1093/infdis/172.6.1445. [DOI] [PubMed] [Google Scholar]
- 21.Klippmark E, Rydbeck R, Shibuta H, Norrby E. Antigenic variation of human and bovine parainfluenza virus type 3 strains. J Gen Virol. 1990;71:1577–1580. doi: 10.1099/0022-1317-71-7-1577. [DOI] [PubMed] [Google Scholar]
- 22.Kunkel T A, Roberts J D, Zakour R A. Rapid and efficient site-specific mutagenesis without phenotypic selection. Methods Enzymol. 1987;154:367–382. doi: 10.1016/0076-6879(87)54085-x. [DOI] [PubMed] [Google Scholar]
- 23.Marx A, Torok T J, Holman R C, Clarke M J, Anderson L J. Pediatric hospitalizations for croup (laryngotracheobronchitis): biennial increases associated with human parainfluenza virus 1 epidemics. J Infect Dis. 1997;176:1423–1427. doi: 10.1086/514137. [DOI] [PubMed] [Google Scholar]
- 24.Murphy B R, Clements M L, Tierney E L, Black R E, Stienberg J, Chanock R M. Dose response of influenza A/Washington/897/80 (H3N2) avian-human reassortant virus in adult volunteers. J Infect Dis. 1985;152:225–229. doi: 10.1093/infdis/152.1.225. [DOI] [PubMed] [Google Scholar]
- 25.Pelet T, Curran J, Kolakofsky D. The P gene of bovine parainfluenza virus 3 expresses all three reading frames from a single mRNA editing site. EMBO J. 1991;10:443–448. doi: 10.1002/j.1460-2075.1991.tb07966.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perez-Schael I, Guntinas M J, Perez M, Pagone V, Rojas A M, Gonzalez R, Cunto W, Hoshino Y, Kapikian A Z. Efficacy of the rhesus rotavirus-based quadrivalent vaccine in infants and young children in Venezuela. N Engl J Med. 1997;337:1181–1187. doi: 10.1056/NEJM199710233371701. [DOI] [PubMed] [Google Scholar]
- 27.Skiadopoulos M H, Surman S, Tatem J M, Paschalis M, Wu S-L, Udem S A, Durbin A P, Collins P L, Murphy B R. Identification of mutations contributing to the temperature-sensitive, cold-adapted, and attenuation phenotypes of the live-attenuated cold-passage 45 (cp45) human parainfluenza virus 3 candidate vaccine. J Virol. 1999;73:1374–1381. doi: 10.1128/jvi.73.2.1374-1381.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snyder M H, Clements M L, Betts R F, Dolin R, Buckler-White A J, Tierney E L, Murphy B R. Evaluation of live avian-human reassortant influenza A H3N2 and H1N1 virus vaccines in seronegative adult volunteers. J Clin Microbiol. 1986;23:852–857. doi: 10.1128/jcm.23.5.852-857.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stokes A, Tierney E L, Sarris C M, Murphy B R, Hall S L. The complete nucleotide sequence of two cold-adapted, temperature-sensitive attenuated mutant vaccine viruses (cp12 and cp45) derived from the JS strain of human parainfluenza virus type 3 (PIV3) Virus Res. 1993;30:43–52. doi: 10.1016/0168-1702(93)90014-e. [DOI] [PubMed] [Google Scholar]
- 30.Tao T, Durbin A P, Whitehead S S, Davoodi F, Collins P L, Murphy B R. Recovery of a fully viable chimeric human parainfluenza virus (PIV) type 3 in which the hemagglutinin-neuraminidase and fusion glycoproteins have been replaced by those of PIV type 1. J Virol. 1998;72:2955–2961. doi: 10.1128/jvi.72.4.2955-2961.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wyatt L S, Moss B, Rozenblatt S. Replication-deficient vaccinia virus encoding bacteriophage T7 RNA polymerase for transient gene expression in mammalian cells. Virology. 1995;210:202–205. doi: 10.1006/viro.1995.1332. [DOI] [PubMed] [Google Scholar]