INTRODUCTION
Carbon monoxide (CO) is dubbed the silent killer, as it is colourless, odourless and tasteless. Clinical symptoms are non-specific, and many patients are unaware that they have been exposed to it until a CO detector sounds an alarm, or when the patient presents to the hospital and is found to have an elevated carboxyhaemoglobin (CoHb) level. Carbon monoxide is produced from the incomplete combustion of hydrocarbons, and malfunctioning heating systems, improperly ventilated vehicles, generators, grills, stoves and residential fires are the common sources of CO poisoning.[1] Anybody is at risk of CO poisoning, and vulnerable groups like infants, the elderly and those with chronic medical issues are especially at risk. More than 400 Americans die from unintentional CO poisoning not linked to fire annually, more than 20,000 end up in the emergency department (ED) and more than 4000 are hospitalised.[2] An American study found that majority (72.8%) of CO exposure occurred in homes; only 13.4% of CO poisoning was work related.[3] Locally, the most common cause of accidental CO poisoning was smoke inhalation from faulty vehicles (33%), followed by house fire (25%).[4]
This article describes an incident that occurred in a restaurant in Singapore in 2016, where some workers suffered CO poisoning due to a malfunctioning ventilation system in the kitchen. Thirty patients were sent to our ED, which was closest to the incident site and also houses the only Burns Unit in Singapore. Box 1 summarises the learning points from this incident.
Box 1.
Learning points
| 1. Emergency medical services, including the despatch centre, need to be vigilant of the possibility of a mass casualty event if there are requests for multiple ambulances from the same location. |
| 2. Consider equipping paramedics with a handheld portable pulse carbon monoxide (CO) oximetry for rapid diagnosis and treatment of patients with CO poisoning. |
| 3. Increase awareness of CO poisoning at work sites and consider installation of CO detector in high-risk confined areas involving machinery that can generate CO. |
| 4. Coordinated and prompt notification, and alerts to relevant regulatory and response agencies will help prevent escalation of the incident. |
NARRATIVE OF INCIDENT
The first four patients were brought in from 21:29 h to 21:35 h via separate ambulances. While they were being triaged, there was a standby call for a case of smoke inhalation, who arrived at our resuscitation area at 21:38 h. History was obtained from the paramedics, as the patient was agitated and hyperventilating. He was a chef in a restaurant kitchen preparing for a banquet when the exhaust fan malfunctioned. His CoHb level was 18.9% and lactate was 10.5 mmol/L, which confirmed the diagnosis of CO poisoning.
Given that there was a sudden influx of patients from the same restaurant, the attending emergency physicians deduced that they were all exposed to CO. Due to uncertainty of events and possibility of further influx of patients, two toxicologists who were off duty were recalled and the Emergency Medical Services (EMS) despatch centre was then informed of this incident. The hospital’s senior management, preparedness and response department and communications department were also notified in anticipation of a mass casualty incident (MCI) plan activation. All patients who were brought in from the same restaurant were initiated on 100% oxygen while waiting to be assessed by a doctor. Investigations included venous blood gas (including CoHb level), lactate, full blood count, renal panel, troponin T, electrocardiogram and chest X-ray.
A total of 30 patients, aged 22–63 years, from the restaurant were reviewed in the ED. There were two distinct waves of patient arrival — 20 cases from 21:29 h to 22:42 h and ten cases from 00:11 h to 01:09 h. The initial wave comprised seven casualties brought in via ambulances, while the rest were self-conveyed. All but two of the first group of patients presented with non-specific symptoms, which can be classified into neurological (headache, dizziness, numbness or tingling sensation, confusion, syncope), cardiorespiratory (breathlessness, chest discomfort) and irritative symptoms (eye or throat irritation, cough, nausea). The second group of patients were advised by the management of the restaurant to have a medical check-up, even though most were asymptomatic. Three had transient symptoms, which had resolved in the ED.
Among the 30 patients, 11 (36.7%) were female and 19 (63.3%) were male. None of them had any pre-existing cardiorespiratory diseases. All were restaurant staff — ten chefs, seven kitchen staff, one cashier and the remaining were wait staff. No restaurant patrons attended. Figure 1 shows the layout of the restaurant. All chefs, kitchen staff and the cashier near or in the affected kitchen were seen in the first wave. Nineteen out of the 20 patients who attended during the first wave were admitted to hospital, with two of them admitted to the burns high-dependency unit for closer monitoring as they were symptomatic and 17 to the ED observation ward. The latter group received oxygen and had downtrending CoHb levels. Figure 2 shows the CoHb trend of all patients. All were asymptomatic when discharged at the end of the 8-h protocol. The two inpatients were also discharged uneventfully. None had airway burns or inhalational injuries, but three patients had elevated troponin with transient chest discomfort initially, which spontaneously resolved. They were given outpatient cardiology appointments. None received hyperbaric treatment and there were no fatalities. Findings from the regulatory authorities and workplace hygiene monitoring team at the incident site revealed that the CO levels were above the permissible exposure limit. Other toxic gases like methane were not detected.
Figure 1.
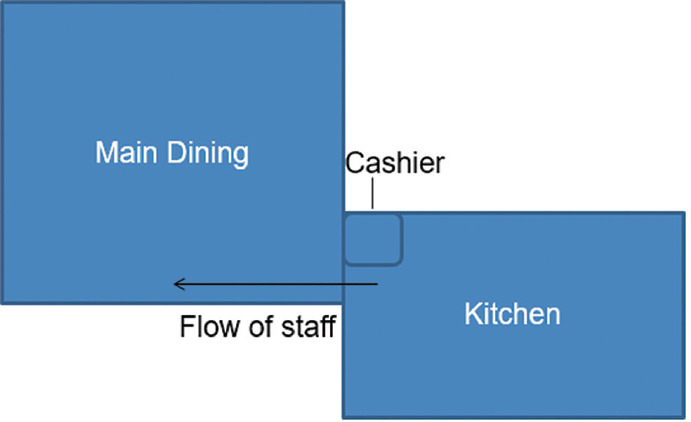
Diagram shows the restaurant’s kitchen and dining area with separate air conditioning and ventilation systems.
Figure 2.
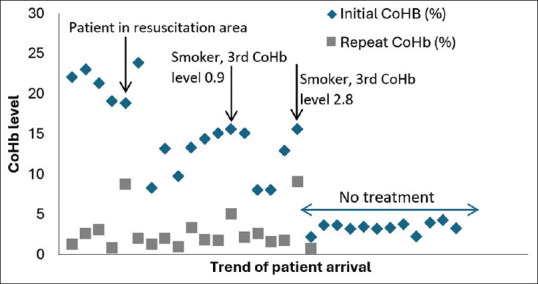
Carboxyhaemoglobin (CoHb) trend of all 30 patients. Three patients had elevated levels on repeat testing — the first being the patient in resuscitation whose CoHb was repeated after 1 h and the other two were smokers, with reduced CoHb levels during the third CoHb testing. It was noted that the last patient removed his non-breather mask during sleep, hence the elevated CoHb level of 9.1 during the second test.
DISCUSSION
This is the first local case series of mass CO poisoning from occupational exposure. This was only recognised after obtaining the history of smoke inhalation from the index case and multiple casualties from the same locality who presented simultaneously with multiple, non-specific symptoms. Carbon monoxide poisoning is readily treatable, simply by removing patients away from the source and providing supplemental oxygen via a non-rebreather mask, which reduces the CoHb half-life from 4–5 h to 40–80 min. However, the difficulty lies in diagnosing CO poisoning promptly.
Despite receiving requests for multiple ambulances at the same location, the EMS did not send a standby call to the hospital to inform this potential MCI. One should consider a potential chemical exposure when there are multiple casualties with irritative and cardiorespiratory symptoms from the same locality, failing which the paramedics and hospital staff may not be appropriately protected and there may be increased morbidity and mortality as they become unwell and this surge in victims may overwhelm the local healthcare system. The lack of decontamination at the scene of the Tokyo subway Sarine attack and the lack of personal protective equipment (PPE) usage resulted in 9.9% of fire department personnel (135 out of 1364) being exposed secondarily while transporting victims.[5] It is thus imperative to seal off the incident site and decontaminate victims to avoid medical facilities from being contaminated, especially if the chemical agent is unknown.[6] The HAZMAT team will usually be activated in these circumstances and their advanced detector will detect the presence of any toxic and combustible gas. Once the agent is known, for example, CO, the level of PPE can be adjusted and the appropriate treatment or antidote may also be administered immediately.
Our paramedics were also not equipped with a portable CO detector or a pulse CO-oximeter, despite their unpredictable and occasional risky job nature. This resulted in the delay in the diagnosis of mass CO poisoning, and more importantly, this could also have endangered them, should they perform a prolonged resuscitation in the closed confines of the restaurant kitchen. An analysis of smoke inhalation cases from house fires can possibly shed some light on the caseload and justify the provision of this useful device for our frontline paramedics.
Among the first wave of patients who presented to the ED, some were aware that the kitchen exhaust fan was malfunctioning. However, they continued working as they were asymptomatic initially. Moreover, there was no CO detector as there is no legal requirement to install it in industrial kitchens or residential homes locally. In the USA, 27 states as well as the district of Columbia have enacted statutes requiring CO detectors in residences. Data from the National Poison Data from the National Poison Data System have shown that the odds of CO poisoning were 3.2 times higher (95% confidence interval 1.5, 6.9) among individuals whose residences had no CO detectors as compared to those whose residences had CO detectors sounded the alarm, and at a higher degree of poisoning severity.[7] Following three incidents of CO poisoning in UK residences, which arose from activities in neighbouring restaurants, CO alarms are now mandated in residences with solid fuel appliances.[8]
Smoke detectors, which are known to reduce the risk of injury or death from home fires by 88%,[9] have been mandated in all new local residences since June 2018.[10] However, a study on awareness, perception and knowledge of CO poisoning has revealed that more than one-third of the interviewees believe that CO can be identified by its odour, smoke or the smoke alarm signal.[11] As such, this may convey a false sense of security, and the public should be educated on the differences between smoke and CO detectors. The cost of a CO detector is low (USD 15–60), and has a lifespan of 5–10 years with no maintenance cost.[12] However, CO detectors are not as popular as smoke alarms. In a survey, 97.6% of respondents reported having at least one smoke alarm in their home, but only 51.4% had a CO alarm.[13] Given the availability of combination smoke and CO detectors, they should be considered for residential use instead, as the price difference between these and smoke alarms is marginal.
Local studies should also be performed to look at the risk of CO exposure in Singapore, for example, vessels for recreational or industrial purposes, where there is an inherent risk due to the use of fossil fuels in confined spaces. By identifying areas of high risk of CO poisoning, there can be a tiered strategy by legislating CO detectors in high-risk areas and encouraging other places with lower risk to consider installation due to low cost and maintenance. As EDs are sentinel outposts in the frontline, it would be prudent to have contingency plans built in for a coordinated and prompt alert system that is triggered early to prevent escalation of the incident. In this case, although the hospital authorities were notified early, communication among the different agencies involved in emergency response to disasters could improve to better integrate and coordinate the response at the national level. This incident can also be used to teach EMS about identification of incidents involving potential hazardous materials.
In conclusion, CO poisoning is difficult to detect due to non-specific symptoms, and one should have a high index of suspicion. The HAZMAT team should be activated in a suspected MCI to identify any causative agents, with management of casualties following a predetermined workflow. As most CO exposures are accidental, increased public awareness and CO detectors will help prevent and reduce the incidence.[11] Local studies should also be performed to look at the risk of CO exposure in Singapore to assist authorities in considering the mandate of CO detectors in high-risk areas to reduce the risk of accidental CO poisoning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to thank LTC Janice Oh and COL (Dr) Ng Yih Yng from the Singapore Civil Defence Force for their contribution towards the publication of this paper.
REFERENCES
- 1.Wu PE, Juurlink DN. Carbon monoxide poisoning. CMAJ. 2014;186:611. doi: 10.1503/cmaj.130972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Centers for Disease Control and Prevention. Carbon monoxide poisoning: General information – frequently asked questions. [[Last accessed on 2020 Oct 12]]. Available from: https://www.cdc.gov/co/faqs.htm .
- 3.Centers for Disease Control and Prevention (CDC) Nonfatal, unintentional, non-fire-related carbon monoxide exposures--United States, 2004-2006. MMWR Morb Mortal Wkly Rep. 2008;57:896–9. [PubMed] [Google Scholar]
- 4.Handa PK, Tai DYH. Carbon monoxide poisoning: A five-year review at Tan Tock Seng Hospital, Singapore. Ann Acad Med Singap. 2005;34:611–4. [PubMed] [Google Scholar]
- 5.Okumura T, Suzuki K, Fukuda A, Kohama A, Takasu N, Ishimatsu S, et al. The Tokyo Subway sarin attack:Disaster management, part I:Community emergency response. Acad Emerg Med. 1998;5:613–7. doi: 10.1111/j.1553-2712.1998.tb02470.x. [DOI] [PubMed] [Google Scholar]
- 6.Okumura S, Okumura T, Ishimatsu S, Miura K, Maekawa H, Naito T. Clinical review:Tokyo –protecting the health care worker during a chemical mass casualty event:An important issue of continuing relevance. Crit Care. 2005;9:397–400. doi: 10.1186/cc3062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christensen GM, Creswell PD, Theobald J, Meiman JG. Carbon monoxide detector effectiveness in reducing poisoning, Wisconsin 2014-2016. Clin Toxicol (Phila) 2020;58:1335–41. doi: 10.1080/15563650.2020.1733592. [DOI] [PubMed] [Google Scholar]
- 8.Keshishian C, Sandle H, Meltzer M, Young Y, Ward R, Balasegaram S, et al. Carbon monoxide from restaurants:The need for an integrated multi-agency response. J Public Health (Oxf) 2012;34:477–82. doi: 10.1093/pubmed/fds023. [DOI] [PubMed] [Google Scholar]
- 9.Ahrens M. Smoke alarms in U.S. home fires. National Fire Protection Association. [[Last accessed 2020 Sep 14]]. Available from: https://www.nfpa.org/News-and-Research/Data-research-and-tools/Detection-and-Signaling/Smoke-Alarms-in-USHome-Fires .
- 10.Ng JS. Smoke detectors mandatory in all new homes from June 2018; existing home owners also urged to comply. The Straits Times. 2017. [[Last accessed on 2020 Oct 14]]. Jun 16. Available from: https://www.straitstimes.com/singapore/smoke-detectorsmandatory-in-all-new-homes-from-june-2018-existing-homeowners-alsourged .
- 11.Jungnickel K, Lohmann M, Böl GF. Carbon monoxide –an underestimated risk?Awareness, perception, knowledge and prevention activities. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2019;62:1324–31. doi: 10.1007/s00103-019-03019-4. [German] [DOI] [PubMed] [Google Scholar]
- 12.Hampson NB. Cost of accidental carbon monoxide poisoning: A preventable expense. Prev Med Rep. 2015;3:21–4. doi: 10.1016/j.pmedr.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hampson NB, Weaver LK. Residential carbon monoxide alarm use:Opportunities for poisoning prevention. J Environ Health. 2011;73:30–3. [PubMed] [Google Scholar]


