Abstract
Non-traumatic orthopedic conditions are pathological conditions involving musculoskeletal system that includes muscles, tendons, bone and joints and associated with frequent medical and surgical care and high treatment costs. There is paucity of information on the pattern of non-traumatic orthopedic conditions in low and middle income countries. The purpose of this study was to determine the epidemiology of non-traumatic orthopedic conditions among inpatients at the Kenyatta National Hospital in Kenya. This was a cross-sectional study with a sample of 175 charts reviewed. Approximately, 70.3% of the inpatients were aged between 25 to 64 years of age with the mean age of 39.97 years (STD 18.78). Ever married tended to be older 53.5 (95% CI: 46.8–60.2) years than other marital statuses. Approximately, 60.6% were males, 38.9% had comorbidities and 49.1% were casuals or unemployed. All inpatients were Kenyans with Nairobi County comprising 52.6% of all inpatients. Approximately, 77.7% were self-referrals. The commonest non-trauma orthopaedic conditions were infection and non-union (35.4%) and spinal degenerative diseases (20.60%) and the least was limb deformities (1.70%). Compared to females, males were 3.703 (p<0.001) times more likely to have infection and non-union. Patients with primary, secondary and tertiary education were 88.2% (p<0.001), 75.6% (p<0.001) and 68.1% (p = 0.016) less likely to have infection and non-union compared to those with no or preschool education. Widows were 8.500 (p = 0.028) times more likely to have spinal degenerative disease than married. Males were 70.8% (p = 0.031) less likely to have osteoarthritis than females. Inpatients with secondary education were 5.250 (p = 0.040) times more likely to have osteoarthritis than those with no or preschool education. In conclusion, majority of inpatients were young and middle aged adults. Infection and non-union and spinal degenerative diseases were the most common non-trauma orthopedic conditions. While males and those with low education were more likely to have infection and non-union, married were more likely to have spinal degenerative disease. Osteoarthritis was more likely among female admissions.
Background
Non-traumatic orthopedic conditions are pathological conditions involving muscles, tendons, bone and joints in both appendicular and axial skeleton that could be congenital, developmental or acquired in nature. They are associated with significant morbidity that results in reduced productivity, chronic absenteeism at work, disability and generally high health care costs due to frequent medical and surgical care needed [1].
Non-traumatic orthopedic conditions such as low back pain, compressive neuropathies, and degenerative joint disorders affect mostly adults while orthopedic infections and musculoskeletal tumours affect all populations–young and the old. Non-traumatic orthopedic conditions are generally common morbidities at health facilities [2].
The most frequently occurring non-traumatic orthopedic conditions are osteoarthritis, back and neck pain, fragility fractures, and systemic inflammatory conditions such as rheumatoid arthritis. These are usually chronic disabling conditions with significant morbidity and compromised quality of life. They are more common in older populations, especially between 65 and 74 years of age [3].
A study on epidemiological patterns of traumatic musculoskeletal injuries and non-traumatic disorders in Japan Self-Defense Forces revealed that the most common were lumbar, tendon and joint disorders and the incidence increases with advancing age [4]. This study was comprised both outpatients and inpatients with musculoskeletal injuries in Japan Self-Defense Forces.
Studies on orthopedic admissions at a tertiary health facilities in Northern Tanzania and Nepal showed infection was the commonest non-trauma orthopedic condition comprising about 7% - 12% of all admissions [5, 6]. These studies looked at both trauma and non-trauma–related injuries admissions and did not look at the distribution and possible risk factors for non-trauma orthopedic admissions at the tertiary heath facilities.
Therefore there is a lack of literature on the occurrence of non-traumatic orthopedic conditions in inpatient settings in low and middle income countries, Kenya inclusive. The purpose of this study was to determine the epidemiology of non-traumatic orthopedic conditions among inpatient admissions in a tertiary health facility in Kenya. This will be important in hospital resource allocation and planning in the management of non-trauma orthopedic conditions in KNH and similar tertiary health facilities in Kenya and in the region.
Methods and materials
Study design
This was a retrospective cross-sectional study design.
Study area
The KNH is the largest teaching and referral hospital in East and Central Africa. KNH Orthopedic Wards were used as the study area. The KNH is based in Upperhill, Nairobi, the capital city of Kenya. It is located approximately 5 km from the city center. KNH has a bed capacity of 1,800, over 6,000 staff members, 50 wards, 22 outpatient clinics, 24 theaters (16 specialized) and an Accident & Emergency Department [7]. Of the 1800 bed capacity, 96 beds are allocated to orthopedic wards. KNH is a 10-floor storied building complex, and the orthopedic wards are located on the 6th floor; however, orthopedic admissions to private wings occurred on the 9th and 10th floors. Orthopedic patients with other comorbidities were also admitted to other wards in the KNH.
Study duration
The study duration was from 1st February 2021 to 31st December 2021. Data abstraction was done from 1st January 2022 to 31st March 2022.
Study population
Orthopedic inpatient admissions at the KNH in 2021.
Inclusion criteria
All non-trauma orthopedic conditions admitted at KNH from 1st February 2021 to 31st December, 2021.
Sample size
Fisher’s formula was used to calculate the sample size [8, 9]
The sample size was 175 charts after adjusting for study population fewer than 10,000.
Recruitment and sampling procedures
Three (3) research assistants (RAs) were recruited to collect and abstract patient data from patient files. The RAs were health care workers with a diploma in Orthopedic Trauma and with some experience in research data collection. The Principal Investigator (PI) was the research coordinator for the data collection. Orthopedic and trauma admissions were identified from the a) admission desk of the Health Information System at the KNH Accident and Emergency Unit (A&E), b) KNH Orthopedic Outpatient Clinic Records (OC), and c) KNH Corporate Outpatient Care (COC). The data were subsequently recorded in a logbook. This logbook served as a master register for all inpatients admitted and therefore the sampling frame for the study. All admissions were logged into the logbook from the admission books stationed at these three (3) services points. The proportional population-to-size (PPS) was subsequently used to determine the number of patients sampled per month from each of these three service points so that the sample size would be representative of the admissions by month from each of these three orthopedic admission entry points (Table 1).
Table 1. Non-trauma orthopedic patients admitted to KNH stratified by point of admission, 2021.
| Month of the year, 2021` | Point of admission | |||
|---|---|---|---|---|
| A&E | Clinic | COC | Total | |
| February | 6 | 6 | 4 | 16 |
| March | 3 | 2 | 7 | 12 |
| April | 3 | 2 | 7 | 12 |
| May | 7 | 2 | 7 | 16 |
| June | 4 | 2 | 6 | 12 |
| August | 7 | 6 | 13 | 26 |
| September | 4 | 4 | 7 | 15 |
| October | 6 | 5 | 5 | 16 |
| November | 7 | 6 | 17 | 30 |
| December | 5 | 4 | 11 | 20 |
| Total | 52 | 39 | 84 | 175 |
The three (3) RAs were reporting to and working under the direction of the PI. The RAs were trained for two (2) days by the PI on the research protocol, data collection tools, and data collection procedures; pilot testing of the data collection tools was also performed before the actual data abstraction.
Variables
The variables extracted were admission date (dd/mm/yyyyy), age, sex, and marital status, religion, occupation, education level, referring health facility tier, nature of admission, type of admission, non-trauma orthopedic condition, Comorbidities.
Data collection procedures
The data were collected through a data abstraction form from the patient files. Missing data were collected by calling patients or their guardians using the mobile phones provided in the patients charts after obtaining their verbal consent.
Data abstraction form
The three (3) RAs were trained on the data abstraction using a data abstraction form as per the research protocol (S1 Text). The PI reviewed all the completed abstraction forms for completeness and accuracy daily during the entire data collection period and provided regular feedback to the RAs in a timely manner to ensure data quality and compliance with the study protocol. All the completed and verified data abstraction forms were then collected and filed by the PI at the end of every week in a locked cabinet.
Data management and analysis
The data abstraction tool was designed to collect both quantitative and qualitative data. While the author had access to information that could identify individual participants during or after data collection, for anonymity and confidentiality purposes, the data abstraction tools were marked only with the participant study numbers, and no names were used. The data were entered into a password-protected Redcap database (version 7.2.2; Vanderbilt, Nashville, TN, USA) maintained by the KNH Medical Research Department. The data were exported and then analyzed using SPSS version 27.0 (version 25.0; IBM, Ltd., North Carolina, USA) (S1 File). Descriptive statistics such as frequencies were calculated, while inferential statistics namely Pearson’s chi-square test and logistic regression were used. The calculations were performed at the 95% confidence level.
Ethics approval and consent to participate
The study protocol was presented to the UoN/KNH Ethics and Research Committee and was granted ethical approval (ERC No: P852/10/2021). Administrative approval was also granted by the KNH Medical Research Department and KNH Orthopedics Department. Written informed consent was obtained from the KNH Medical Research Department to have access to the patient’s health records in the Health Information Office (Room 19). Informed verbal consent was obtained from the discharged patients who had missing information in their charts as per the UoN/KNH ethics regulations. For minors, verbal consent was obtained from parents or guardians for charts with missing values. The verbal consent was obtained over the phone. The PI and RAs took into account the visual and auditory privacy during the telephone conversation with the discharged patients, parents or guardians.
Results
The socio-demographic profile of the sample population
A total of 175 charts were extracted and analyzed.
Approximately, 70.3% of the inpatient admissions were aged between 25 to 64 years of age, with children representing 11.4% and elderly being 8.6%. The mean age was 39.97 years (STD 18.78). Approximately, 60.6% of inpatients admissions were males. About 55.5% had secondary or tertiary education. About 56% were married and 12.6% were minors. Approximately, 49.1% were casuals or unemployed. About 54.3% of admissions are self-referrals. All admissions were Kenyans with Nairobi County comprising 52.6% of all inpatient admissions and this increased to 75.5% if Nairobi County and its environs are included. About 70.3% of the admissions were elective and admitted through the KNH clinic and COC. An emergency admission through accident and emergency department was 29.7%. Approximately, 77.7% of the inpatient admissions were self-referrals with the remaining 22.3% were health facility referrals. Approximately, 13.1% and 24.6% were smokers and took alcohol, respectively, at the time of admission to KNH. About 38.9% had a comorbidity of which the most prevalent were hypertension (41.2%), Diabetes Mellitus (23.5%), HIV (13.2%), Allergy/Asthma (7.4%) and Gastritis (5.9%) (Table 2).
Table 2. Socio-demographic profile of the sample population at KNH, 2021.
| Variable | Categories | Frequency, n (%) |
|---|---|---|
| Age | 0–14 years | 20 (11.4%) |
| 15–24 years | 17 (9.7%) | |
| 25–64 years | 123 (70.3%) | |
| Above 65 years | 15 (8.6%) | |
| Sex | Female | 69 (39.4%) |
| Male | 106 (60.6%) | |
| Education | None & Preschool | 14 (8.0%) |
| Primary | 58 (33.1%) | |
| Secondary | 40 (22.9%) | |
| Tertiary | 57 (32.6%) | |
| aMissing | 6 | |
| Marital status | Married | 98 (56.0%) |
| Minor | 22 (12.6%) | |
| Ever married | 18 (10.3%) | |
| Single | 37 (21.1%) | |
| Occupation | Business | 27 (15.4%) |
| Casual | 45 (25.7%) | |
| Employed | 41 (23.4%) | |
| Other | 16 (9.1%) | |
| Unemployed | 41 (23.4%) | |
| aMissing | 5 | |
| Country | Kenya | 175 (100%) |
| County | Others | 42 (24.0%) |
| Kajiado | 11 (6.3%) | |
| Kiambu | 19 (10.9%) | |
| Nairobi | 92 (52.6%) | |
| Others ‐ Eastern | 10 (5.7%) | |
| aMissing | 1 | |
| Type of admission | Elective | 123 (70.3%) |
| Emergency | 52 (29.7%) | |
| Point of admission | A&E | 52 (29.7%) |
| Clinic | 39 (22.3%) | |
| COC | 84 (48.0%) | |
| Type of referring health facility | Self-referrals | 95 (54.3%) |
| Government health facilities | 19 (10.9%) | |
| Private health facilities | 20 (11.4%) | |
| Nature of admission | Self-referrals | 136 (77.7%) |
| Facility referral | 39 (22.3%) | |
| Smoking | Yes | 23 (13.1%) |
| No | 138 (78.9%) | |
| aMissing | 14 | |
| Alcohol | Yes | 43 (24.6%) |
| No | 116 (66.3%) | |
| aMissing | 16 | |
| Comorbidities | No | 107 (61.1%) |
| Yes | 68 (38.9%) |
aMissing data were excluded from the computation of frequency distribution. Ever married includes widow, separated and divorced.
Patterns of non-trauma orthopedic conditions
Ever married tended to be older 53.5 (95% CI: 46.8–60.2) years than other marital statuses followed by married and single patients. Single are mostly young adults (Table 3).
Table 3. Marital status and mean age for non-trauma orthopaedic inpatient admissions at KNH, 2021.
| Marital categories | Mean age |
|---|---|
| Married | 48.5 (95% CI: 45.8–51.1) years |
| Minor | 8.1 (95% CI: 5.9–10.3) years |
| Ever married | 53.5 (95% CI: 46.8–60.2) years |
| Single | 29.9 (95% CI: 26.5–33.3) years |
95% confidence intervals were calculated from the mean age. Ever married includes widowed, widower, separated and divorced.
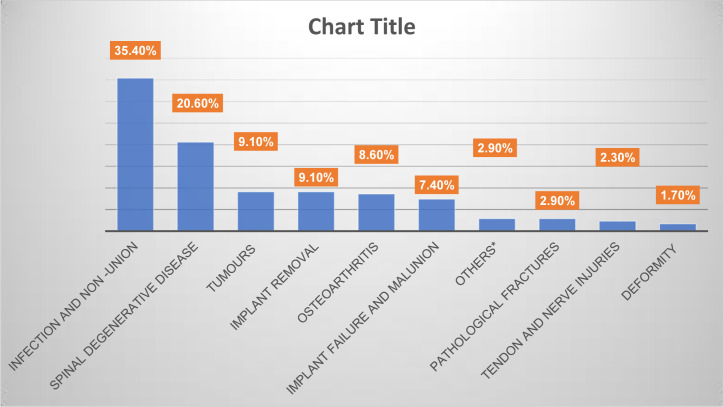
The commonest non-trauma orthopaedic admissions were infection and non-union, spinal degenerative disease comprising 56% of admissions. These were followed by tumors, implant removal, osteoarthritis and implant removal and mal-union. Pathological fractures, tendon and nerve injuries and deformity conditions were the least common admissions (Fig 1).
Fig 1. Graphical representation of common non-traumatic orthopaedic conditions admitted at KNH, 2021.
Frequency distribution tally for common non-traumatic orthopaedic conditions (n = 175).
Infection and non-unions
Compared to females, males were 3.703 (p<0.001) times more likely to have infection and non-union. Patients with primary, secondary and tertiary education were 88.2% (p<0.001), 75.6% (p<0.001) and 68.1% (p = 0.016) less likely to have infection and non-compared compared to those with no or preschool education. Minors were 2.776 times more likely to have infection and non as compared to married patients (p = 0.011). Patients with “Other” occupation were 2.922 (p = 0.034) times more likely to have infection and non-union than businessmen or women. Emergency admissions were 9.669 (p<0.001) times more likely to have infection than elective admissions. Admissions through clinic and COC were 92.6% (p<0.001) and 70.2% (p = 0.008) less likely to have infection and non-union, respectively, than Accident and Emergency admissions. Admissions through the government and private health facilities referrals were 77.7% (p = 0.023) and 87.7% (p = 0.008) less likely to have infection and non-union, respectively, than self-referrals (Table 4).
Table 4. Cluster differences in non-trauma orthopedic conditions according to logistic regression analysis of inpatients in KNH 2021.
| Infection and non-union OR (p-value) |
Spinal degenerative Disease OR (p-value) |
Tumors OR (p-value) |
Osteoarthritis OR (p-value) |
||
|---|---|---|---|---|---|
| Sex | Female | 1.0 | 1.0 | 1.0 | 1.0 |
| Male | 3.703 (p<0.001) | 0.538 (p = 0.097) | 0.622 (p = 0.367) | 0.292 (p = 0.031) | |
| Education | None and preschool | 1.0 | 1.0 | 1.0 | 1.0 |
| Primary | 0.118 (p = 0.001) | 2.143 (p = 0.353) | - | 2.437 (p = 0.418) | |
| Secondary | 0.244 (p = 0.001) | 1.714 (p = 0.241) | 0.641 (p = 0.429) | 5.250 (p = 0.040) | |
| Tertiary | 0.319 (p = 0.016) | 1.071 (p = 0.884) | 4.588 (p = 0.166) | 3.562 (p = 0.117) | |
| Marital status | Married | 1.0 | 1.0 | 1.0 | 1.0 |
| Minor | 2.776 (p = 0.011) | 0.221 (p = 0.019) | 2.255 (p = 0.246) | 0.182 (p = 0.106) | |
| Ever married | 1.847 (p = 0.266) | 1.211 (p = 0.998) | 0.412 (p = 0.227) | 0.583 (p = 0.708) | |
| Single | 1.319 (p = 0.631) | 0.176 (p = 0.027) | 0.970 (p = 0.973) | 0.249 (p = 0.999) | |
| Occupation | Business | 1.0 | 1.0 | 1.0 | 1.0 |
| Casual | 1.030 (p = 0.953) | 0.309 (p = 0.087) | 6.303 (p = 0.092) | 1.333 (p = 0.818) | |
| Employed | 0.885 (p = 0.780) | 0.378 (p = 0.127) | 5.212 (p = 0.045) | 0.718 (p = 0.724) | |
| Other | 2.922 (p = 0.034) | 0.295 (p = 0.054) | 2.242 (p = 0.219) | 0.249 (p = 0.096) | |
| Unemployed | 2.125 (p = 0.252) | 0.324 (p = 0.150) | 3.636 (p = 0.243) | 0.359 (p = 0.328) | |
| Type of admission | Elective | 1.0 | 1.0 | 1.0 | 1.0 |
| Emergency | 9.669 (p<0.001) | 0.227 (p = 0.008) | 0.518 (p = 0.321) | 0.338 (p = 0.164) | |
| Point of admission | A&E | 1.0 | 1.0 | 1.0 | 1.0 |
| Clinic | 0.074 (p<0.001) | 6.667 (p<0.001) | 1.719 (p = 0.440) | 3.767 (p = 0.093) | |
| COC | 0.298 (p = 0.008) | 6.667 (p = 0.003) | 0.716 (p = 0.581) | 2.788 (p = 0.197) | |
| Type of referring health facility | Self-referrals | 1.0 | 1.0 | 1.0 | 1.0 |
| Government health facilities | 0.223 (p = 0.023) | 2.303 (p = 0.120) | 2.218 (p = 0.281) | 2.528 (p = 0.305) | |
| Private health facilities | 0.123 (p = 0.008) | 2.872 (p = 0.179) | 1.500 (p = 0.678) | 0.944 (p = 0.957) | |
| Comorbidities | No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.891 (p = 0.723) | 1.450 (p = 0.321) | 0.939 (p = 0.907) | 2.568 (p = 0.088) |
OR refers to odds ratio. P-value calculated at 5% level of significance. 1.0 refers to reference group. A&E refers to the Accident and Emergency. COC refers to the Corporate Outpatient Clinic.
Spinal degenerative disease
Minors and singles were 77.9% (p = 0.019) and 0.176 (p = 0.027) less likely to have spinal degenerative disease compared to married patients, respectively. Emergency admissions were 77.3% (p = 0.008) less likely to have spinal degenerative disease than elective admissions. KNH clinic and COC admissions were 6.667 (p<0.001) and 6.667 (p = 0.003) times more likely to have spinal degenerative disease, respectively, than admissions through Accident and Emergency department (Table 4).
Tumours
Employed inpatient admissions were 5.212 (p = 0.045) times more likely to have tumors compared with businessmen and women. Emergency admissions were 48.2% less likely to have tumors than elective admissions. However, this was not statistically significant (Table 4).
Osteoarthritis
Males were 70.8% (p = 0.031) less likely to have osteoarthritis than females. Inpatients with secondary education were 5.250 (p = 0.040) times more likely to have osteoarthritis than those with no or preschool education (Table 4).
Discussion
Socio-demographic profile of the sample population
The study revealed that majority of admissions was aged between 25 to 64 years, with mean age of about 40 years and married or single. This compares with a study done in Malawi that showed musculoskeletal impairment was most common among 31–60 years of age with prevalence increasing with increasing age and majority are married or single [10, 11]. The non-traumatic musculoskeletal disorders are common among middle aged and becomes common with advancing age.
Overall, all admissions were Kenyans with Nairobi County comprising about half of the admissions. Nairobi County and its environs comprise about three-fourths of inpatients admissions at KNH. This finding is similar to studies performed in South Africa, Tanzania, Malawi and Iran, which revealed that the majority of patients admitted to tertiary hospitals were from regions co-located with the hospital [12–16]. This may be because of the proximity of the hospitals to patients’ area of residence and because patients, relatives and friends prefer their loved ones to be admitted closer home where they can easily visit their sick. About 4 out of every 10 admissions had comorbidity with the most prevalent ones being hypertension, diabetes mellitus, HIV and allergy/asthma. This compares with a study on prevalence and patterns of comorbidity among musculoskeletal disorders that revealed the prevalent comorbidities were hypertension and diabetes [17]. These are lifestyle diseases that are common with advancing age. However, these comorbidities had no influence on the occurrence of non-trauma orthopedic conditions in the current study.
Patterns of non-trauma orthopedic conditions
Over two-thirds of the admissions were electives, admitted mostly through the clinics. This parallels a study done in Brazil and UK that demonstrated elective admissions dominated non-traumatic orthopedic conditions [18–20]. A big proportion of non-traumatic orthopedic conditions are considered non-urgent medical conditions that are mostly managed electively and are usually seen and admitted from the outpatient clinics rather than accident and emergency department.
Over three-fourths of the admissions were self-referrals. This is in tandem with a longitudinal study done in Netherlands that revealed self-referral of patients with non-traumatic musculoskeletal conditions is common [21].
About one-tenth and a quarter of the inpatients admissions were smokers and took alcohol, respectively. This compares with a study done in Netherlands that showed musculoskeletal impairment is common among smokers [22]. Smoking and alcohol depresses body immunity and makes them prone to orthopedic infections, non-union, orthopedic tumours and pathological fractures.
This study showed that infection and non-union together with spinal degenerative disease were the most common non-trauma orthopaedic conditions admitted at KNH. This agrees with a study done in Nepal and Tanzania that showed infection is the most common form of non-trauma orthopaedic admissions [5, 6, 14]. However, it contrasts with a study done in India that showed spine conditions and implant removal were the most prevalent non-trauma orthopaedic conditions and infection was among the least common conditions [23]. This could be because Warangal Hospital in India is a multi-speciality teaching hospital that could be admitting patients of higher socio-economic status than is the case with the KNH. The study also contrasts with one done in PCEA Kikuyu Mission Hospital in Kenya that showed Osteoarthritis was the most common reason for non-trauma orthopaedic admission followed by limb deformities, infection and removal of implants [24]. This could be because the PCEA Kikuyu Mission Hospital had specialists’ orthopaedic surgeons for arthroplasty and tended to get referrals from other facilities for patients with hip and knee osteoarthritis.
Infection and non-union
The study showed that infection and non-union were more common among males inpatients. This is in tandem with studies in done USA, Pakistan, Iran and Germany that revealed men are more prone to bloodstream and surgical site infections including orthopaedic infections [25–28]. However, it differs with another study done in Germany that revealed no gender specific differences in surgical site infections were found in orthopaedic surgery. But it showed that if all specialities procedures were considered women had a lower rate of surgical site infections [29]. The differences in sex preposition to surgical site infections could be due to hormonal and immune response differences between male and female that accounts for lower occurrence of surgical site infections among females as compared to males. It is an established knowledge from numerous studies that infections are a major cause of fracture non-union and hence a lower occurrence of fracture non-union among female orthopaedic admissions, given the fact that they have low risk of surgical site infections.
Patients with higher education tended to have less infection and non-union than were those with no or preschool education. This parallels study done in Pakistan that revealed lower education and lower socio-economic status was strongly associated with risk of surgical site infections [28].
Minors were about three (3) times more likely to have infection and non-fracture union as compared to married patients. The mean age of minors was 8.1 years while married patients were 48.5 years. This means that younger age was associated with the risk of infection and hence fractures non-union. This is in tandem with a number of studies that have shown extremes of age–the very young and the elderly above 65 years ‐ are significantly associated with infections including surgical site infections [30–39]. This could be due to increased vulnerability resulting from immunosenescence, malnutrition as well as a variety of physiological and anatomical age-associated factors [31, 40, 41]. Married patients in this study were not elderly and hence low risk of infections and hence fracture non-union. The study also revealed that orthopaedic infections were associated with emergency admissions, admissions through accident and emergency department and self-referred patients. This is in tandem with studies done in UK that showed orthopaedic infections are associated with emergency admissions [42, 43]. Musculoskeletal infections have always been treated as one of the orthopaedic emergencies [44].
Spinal degenerative disease
Minors and singles were 77.9% (p = 0.019) and 0.176 (p = 0.027), respectively, less likely to have spinal degenerative disease compared to married patients. This study showed that spinal degenerative diseases were less likely among the young (minors and singles) as compared to the older age group (married patients). Minors had a mean age of 8.1 years, singles had a mean age of 29.9 years while married patients had a mean age of 48.5 years and the study therefore showed older patients were more prone to spinal degenerative disease as compared to younger patients‥ This agrees with a study done in China and Turkey that showed advancing age is associated with lumbar disc degeneration [10, 22, 45–50]. Also study in Italy revealed that chronic musculoskeletal degenerative conditions are associated with older age groups [10, 22].
The study also demonstrated that spinal degenerative disease were mostly elective admissions through the clinics. This is in tandem with a study done in Canada, USA that showed majority of degenerative spinal conditions were elective cases [51–53]. This is because they are degenerative conditions are common with advancing age and are usually chronic and non-urgent in nature.
Tumours
The study showed that inpatients admissions that were employed were more likely to have tumors. However, this study did not elicit the nature of employment of the inpatient admissions. Nevertheless, association between occupation and development of cancers has been documented in many studies over the century and has sometimes led to the identification of concerned carcinogens. This study agrees with a study done in USA that showed bone tumors are associated with those employed as blacksmiths, machine operators [54, 55].
Osteoarthritis
The study showed that females were more likely to have osteoarthritis. Sex bias in the prevalence and severity of osteoarthritis have been known for many years with females affected more than males with incidence increasing significantly after menopause [56–59]. Studies have been done that shows women have thinner articular cartilage than men and more predisposed not only to arthritis but also to severe forms of osteoarthritis.
The study also revealed that osteoarthritis was associated with secondary education. Several studies have shown low education, low socio-economic status is associated with increased prevalence of osteoarthritis [22, 60, 61]. This may be because low socio-economic status and low education levels are associated with occupation with strenuous activity level.
This study had several limitations. First, there is a possible effect of the COVID-19 pandemic on patients seeking health services at the KNH. The movement restrictions imposed during the COVID-19 pandemic could skew access to services at the KNH. This was mitigated by ensuring that the data collection period covered the COVID-19 period, during which inter-county movement restrictions were lifted by the Kenyan government. Second, this was a retrospective cross-sectional study design and hence was weak in determining causality. Third, there were missing data from the patient charts. This was mitigated by increasing the sample size by 10%. Fourth, this was a single health facility study and therefore may lack external validity. However, the tertiary health facility is the largest referral and teaching health facility in Kenya with a large catchment population and likely generalized to the Kenyan health facilities. Despite these limitations, given the dearth of information on non-trauma orthopedic conditions in Kenya, these findings could be used not only to help policy makers formulate public health preventive measures but also to help hospital management teams apportion resources appropriately for the care of these non-traumatic orthopedic conditions.
Conclusion
Majority of non-trauma orthopedic conditions inpatient admissions were young and middle aged adults who were either casuals or unemployed. Most of them were from within Nairobi County and its environs. Infection and non-union and spinal degenerative diseases were the most common non-trauma orthopedic conditions. Males and low education were more likely to have infection and non-union. Minors and singles were younger than other marital statuses and were less likely to have spinal degenerative diseases. Osteoarthritis was more likely among females than men inpatient admissions. Cardiovascular risk factors were the most prevalent comorbidities but they had no influence on occurrence of non-traumatic orthopedic conditions.
Recommendations
KNH and other similar tertiary health facilities should apportion more resources and supplies towards infection prevention and treatment in orthopedic wards;
KNH and the county governments should allocate more resources towards training of health care workers, patients and caregivers on infection prevention measures, early detection and treatment of orthopedic infections;
Aggressive infection prevention measures be instituted for emergency admissions and self-referred patients;
Further studies need to be done to determine the nature of employments and their predisposition for tumours to help in developing orthopedic tumours prevention guidelines;
Supporting information
(SAV)
(DOCX)
(DOC)
(DOCX)
Acknowledgments
I would like to sincerely acknowledge the work of Brian Okinyi and Micah J. Kipkemei for their commitment and assistance in the data collection process.
List of abbreviations
- COVID-19
Coronavirus Disease
- ERC
Ethics Review Committee
- KNH
Kenyatta National Hospital
- UoN/KNH
University of Nairobi/Kenyatta National Hospital
- RA
Research Assistant
- SPSS
Statistical Package for the Social Sciences
- SOPs
Standard operating procedures
- USA
United States of America
- PCEA
Presbyterian Church of East Africa
- PI
Principal Investigator
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Kenyatta National Hospital. RFA 2020/21. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Neumann PJ, Stone PW, Chapman RH, Sandberg EA, Bell CM. The quality of reporting in published cost-utility analyses, 1976–1997. Ann Intern Med. 2000. Jun 20;132(12):964–72. [DOI] [PubMed] [Google Scholar]
- 2.Brenna J, McCarney D. Nontraumatic Musculoskeletal Disorders. Oxford; 2019. [cited. Available from: https://academic.oup.com/book/24830/chapter-abstract/188514935?redirectedFrom=fulltext&login=false. [Google Scholar]
- 3.Yelin E, Weinstein S, King T. The burden of musculoskeletal diseases in the United States. Semin Arthritis Rheum. 2016. Dec;46(3):259–60. doi: 10.1016/j.semarthrit.2016.07.013 [DOI] [PubMed] [Google Scholar]
- 4.Amako M, Yato Y, Yoshihara Y, Arino H, Sasao H, Nemoto O, et al. Epidemiological patterns of traumatic musculoskeletal injuries and non-traumatic disorders in Japan Self-Defense Forces. Inj Epidemiol. 2018. May 1;5(1):19. doi: 10.1186/s40621-018-0150-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mishra BN, Jha A, Gupta. Epidemiology of Orthopaedic Admissions at A Teaching Hospital of Eastern Nepal. Journal of Nobel Medical College. 2017;6(1):56–62. [Google Scholar]
- 6.Hardaker WM, Jusabani M, Massawe H, Pallangyo A, Temu R, Masenga G, et al. The burden of orthopaedic disease presenting to a tertiary referral center in Moshi, Tanzania: a cross-sectional study. Pan African Medical Journal 2022;42:96. 2022;42(96). doi: 10.11604/pamj.2022.42.96.30004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MoH. Nairobi; 2021 [updated 2021; cited 2021 10th May ]; Available from: https://knh.or.ke/index.php/history/
- 8.Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013. Apr;35(2):121–6. doi: 10.4103/0253-7176.116232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jung SH. Stratified Fisher’s exact test and its sample size calculation. Biom J. 2014. Jan;56(1):129–40. doi: 10.1002/bimj.201300048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ngoie LB, Dybvik E, Hallan G, Gjertsen JE, Mkandawire N, Varela C, et al. Prevalence, causes and impact of musculoskeletal impairment in Malawi: A national cluster randomized survey. PLoS One. 2021;16(1):e0243536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atijosan O, Rischewski D, Simms V, Kuper H, Linganwa B, Nuhi A, et al. A national survey of musculoskeletal impairment in Rwanda: prevalence, causes and service implications. PLoS One. 2008. Aug 6;3(7):e2851. doi: 10.1371/journal.pone.0002851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jergesen H, Oloruntoba D, Edward Aluede G, M., Phillips J, Caldwell A. Analysis of Outpatient Trauma Referrals in a Sub-Saharan African Orthopedic Center. World Journal of Surgery. 2011;35:956–61 doi: 10.1007/s00268-011-1001-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simba DO, Mbembati NA, Museru LM, Lema LE. Referral pattern of patients received at the national referral hospital: challenges in low income countries. East Afr J Public Health. 2008. Apr;5(1):6–9. doi: 10.4314/eajph.v5i1.38969 [DOI] [PubMed] [Google Scholar]
- 14.Premkumar A, Massawe HH, Mshabaha DJ, R.Foran J, XiaohanYing, Sheth NP. The burden of orthopaedic disease presenting to a referral hospital in northern Tanzania. Global Surgery. 2015;2(1):70–5. [Google Scholar]
- 15.Pittalis C, Brugha R, Bijlmakers L, Mwapasa G, Borgstein E, Gajewski J. Patterns, quality and appropriateness of surgical referrals in Malawi. Trop Med Int Health. 2020. Jul;25(7):824–33. doi: 10.1111/tmi.13406 [DOI] [PubMed] [Google Scholar]
- 16.Soleymanha M, Mobayen M, Asadi K, Adeli A, Haghparast-Ghadim-Limudahi Z. Survey of 2582 cases of acute orthopedic trauma. Trauma Mon. 2014. Nov;19(4):e16215. doi: 10.5812/traumamon.16215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ziade N, El Khoury B, Zoghbi M, Merheb G, Abi Karam G, Mroue K, et al. Prevalence and pattern of comorbidities in chronic rheumatic and musculoskeletal diseases: the COMORD study. Sci Rep. 2020. May 6;10(1):7683. doi: 10.1038/s41598-020-64732-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luciano AP, Almeida T, Dos Santos Figueiredo FW, Schoueri JHM, Abreu LC, Adami F. Study of the evolution and variability of nontraumatic orthopedic surgeries in Brazil-9 years of follow-up: A database study. Medicine (Baltimore). 2018. May;97(21):e10703. doi: 10.1097/MD.0000000000010703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blom AW, Donovan RL, Beswick AD, Whitehouse MR, Kunutsor SK. Common elective orthopaedic procedures and their clinical effectiveness: umbrella review of level 1 evidence. BMJ. 2021. Jul 7;374:n1511. doi: 10.1136/bmj.n1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasta G, Polizzi A, Annunziata S, Klersy C, Fenech L, Dermenaki Farahani MR, et al. Patients with Musculoskeletal Disorders Presenting to the Emergency Department: The COVID-19 Lesson. Int J Environ Res Public Health. 2022. May 12;19(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lankhorst NE, Barten JA, Meerhof R, Bierma-Zeinstra SMA, van Middelkoop M. Characteristics of patients with knee and ankle symptoms accessing physiotherapy: self-referral vs general practitioner’s referral. Physiotherapy. 2020. Sep;108:112–9. doi: 10.1016/j.physio.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 22.Cimmino MA, Ferrone C, Cutolo M. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2011. Apr;25(2):173–83. doi: 10.1016/j.berh.2010.01.012 [DOI] [PubMed] [Google Scholar]
- 23.Saikiran V., Laxmi P. G, Nagaraju V., Bharath K. D, Shyam S. A. Epidemiology of orthopedic trauma admissions in a multispecialty hospital in Warangal-A retrospective study. Clinical Practice. 2019;16(6). [Google Scholar]
- 24.Kihuba E. Epidemiology and medical costs of orthopedic conditions in a tertiary hospital in Kenya; A five-year analysis of admission data. BMJ Yale. 2022. [Google Scholar]
- 25.Cohen B, Choi YJ, Hyman S, Furuya EY, Neidell M, Larson E. Gender differences in risk of bloodstream and surgical site infections. J Gen Intern Med. 2013. Oct;28(10):1318–25. doi: 10.1007/s11606-013-2421-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang B, Wang Q, Hamushan M, Yu J, Jiang F, Li M, et al. Trends in microbiological epidemiology of orthopedic infections: a large retrospective study from 2008 to 2021. BMC Infect Dis. 2023. Aug 31;23(1):567. doi: 10.1186/s12879-023-08471-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taherpour N, Mehrabi Y, Seifi A, Eshrati B, Hashemi Nazari SS. Epidemiologic characteristics of orthopedic surgical site infections and under-reporting estimation of registries using capture-recapture analysis. BMC Infect Dis. 2021. Jan 4;21(1):3. doi: 10.1186/s12879-020-05687-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.East LA, Arudo J, Loefler M, Evans CM. Exploring the potential for advanced nursing practice role development in Kenya: a qualitative study. BMC Nurs. 2014;13(1):33. doi: 10.1186/s12912-014-0033-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langelotz C, Mueller-Rau C, Terziyski S, Rau B, Krannich A, Gastmeier P, et al. Gender-Specific Differences in Surgical Site Infections: An Analysis of 438,050 Surgical Procedures from the German National Nosocomial Infections Surveillance System. Viszeralmedizin. 2014. Apr;30(2):114–7. doi: 10.1159/000362100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bischoff P, Kramer TS, Schroder C, Behnke M, Schwab F, Geffers C, et al. Age as a risk factor for surgical site infections: German surveillance data on total hip replacement and total knee replacement procedures 2009 to 2018. Euro Surveill. 2023. Mar;28(9). doi: 10.2807/1560-7917.ES.2023.28.9.2200535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gavazzi G, Krause KH. Ageing and infection. Lancet Infect Dis. 2002. Nov;2(11):659–66. doi: 10.1016/s1473-3099(02)00437-1 [DOI] [PubMed] [Google Scholar]
- 32.Katz MJ, Roghmann MC. Healthcare-associated infections in the elderly: what’s new. Curr Opin Infect Dis. 2017. Aug;29(4):388–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cruz E, Cano JR, Benitez-Parejo N, Rivas-Ruiz F, Perea-Milla E, Guerado E. Age as a risk factor of nosocomial infection after hip fracture surgery. Hip Int. 2010;20 Suppl 7:S19–25. doi: 10.1177/11207000100200s704 [DOI] [PubMed] [Google Scholar]
- 34.Cheadle WG. Risk factors for surgical site infection. Surg Infect (Larchmt). 2006;7 Suppl 1:S7–11. doi: 10.1089/sur.2006.7.s1-7 [DOI] [PubMed] [Google Scholar]
- 35.Kaye KS, Schmit K, Pieper C, Sloane R, Caughlan KF, Sexton DJ, et al. The effect of increasing age on the risk of surgical site infection. J Infect Dis. 2005. Apr 1;191(7):1056–62. doi: 10.1086/428626 [DOI] [PubMed] [Google Scholar]
- 36.Fisichella L, Fenga D, Rosa MA. Surgical Site Infection In Orthopaedic Surgery: Correlation Between Age, Diabetes, Smoke And Surgical Risk. Folia Med (Plovdiv). 2014. Oct-Dec;56(4):259–63. doi: 10.1515/folmed-2015-0005 [DOI] [PubMed] [Google Scholar]
- 37.Autore G, Bernardi L, Esposito S. Update on Acute Bone and Joint Infections in Paediatrics: A Narrative Review on the Most Recent Evidence-Based Recommendations and Appropriate Antinfective Therapy. Antibiotics (Basel). 2020. Aug 6;9(8). doi: 10.3390/antibiotics9080486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Riise OR, Kirkhus E, Handeland KS, Flato B, Reiseter T, Cvancarova M, et al. Childhood osteomyelitis-incidence and differentiation from other acute onset musculoskeletal features in a population-based study. BMC Pediatr. 2008. Oct 20;8:45. doi: 10.1186/1471-2431-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Walter N, Bartl S, Alt V, Rupp M. The Epidemiology of Osteomyelitis in Children. Children (Basel). 2021. Nov 3;8(11). doi: 10.3390/children8111000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guerra-Laso JM, Gonzalez-Garcia S, Gonzalez-Cortes C, Diez-Tascon C, Lopez-Medrano R, Rivero-Lezcano OM. Macrophages from elders are more permissive to intracellular multiplication of Mycobacterium tuberculosis. Age (Dordr). 2013. Aug;35(4):1235–50. doi: 10.1007/s11357-012-9451-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grudzinska FS, Brodlie M, Scholefield BR, Jackson T, Scott A, Thickett DR, et al. Neutrophils in community-acquired pneumonia: parallels in dysfunction at the extremes of age. Thorax. 2020. Feb;75(2):164–71. doi: 10.1136/thoraxjnl-2018-212826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Howell A, Parker S, Tsitskaris K, Oddy MJ. The burden of bone, native joint and soft tissue infections on orthopaedic emergency referrals in a city hospital. Ann R Coll Surg Engl. 2016. Jan;98(1):34–9. doi: 10.1308/rcsann.2015.0050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee A, May A, Obremskey WT. Necrotizing Soft-tissue Infections: An Orthopaedic Emergency. J Am Acad Orthop Surg. 2019. Mar 1;27(5):e199–e206. doi: 10.5435/JAAOS-D-17-00616 [DOI] [PubMed] [Google Scholar]
- 44.Babu J. Orthopedic Emergencies. In: In: Eltorai A, Eberson, C., Daniels, A. (eds) editor. Essential Orthopedic Review: Springer, Cham; 2018.
- 45.Lou C, Chen H, Mei L, Yu W, Zhu K, Liu F, et al. Association between menopause and lumbar disc degeneration: an MRI study of 1,566 women and 1,382 men. Menopause. 2017. Oct;24(10):1136–44. doi: 10.1097/GME.0000000000000902 [DOI] [PubMed] [Google Scholar]
- 46.Muscat Baron Y. Menopause and the intervertebral disc. Menopause. 2017. Oct;24(10):1118–21. doi: 10.1097/GME.0000000000000964 [DOI] [PubMed] [Google Scholar]
- 47.Lou C, Chen HL, Feng XZ, Xiang GH, Zhu SP, Tian NF, et al. Menopause is associated with lumbar disc degeneration: a review of 4230 intervertebral discs. Climacteric. 2014. Dec;17(6):700–4. doi: 10.3109/13697137.2014.933409 [DOI] [PubMed] [Google Scholar]
- 48.Ozcan-Eksi EE, Eksi MS, Akcal MA. Severe Lumbar Intervertebral Disc Degeneration Is Associated with Modic Changes and Fatty Infiltration in the Paraspinal Muscles at all Lumbar Levels, Except for L1-L2: A Cross-Sectional Analysis of 50 Symptomatic Women and 50 Age-Matched Symptomatic Men. World Neurosurg. 2019. Feb;122:e1069–e77. doi: 10.1016/j.wneu.2018.10.229 [DOI] [PubMed] [Google Scholar]
- 49.Machino M, Nakashima H, Ito K, Tsushima M, Ando K, Kobayashi K, et al. Influence of Age and Gender on Intervertebral Disk Degeneration and Height in the Thoracolumbar Spine. Spine Surg Relat Res. 2022;6(4):379–87. doi: 10.22603/ssrr.2021-0187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976). 2002. Dec 1;27(23):2631–44. doi: 10.1097/00007632-200212010-00002 [DOI] [PubMed] [Google Scholar]
- 51.Dandurand C, Hindi MN, Laghaei PF, Mashayekhi MS, Kwon BK, Dea N, et al. Degenerative spinal conditions requiring emergency surgery: an evolving crisis in a publicly funded health care system. Can J Surg. 2023. May-Jun;66(3):E274–E81. doi: 10.1503/cjs.012122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kukreja S, Ambekar S, Ahmed OI, Menger RP, Sin AH, Nanda A. Impact of elective versus emergent admission on perioperative complications and resource utilization in lumbar fusion. Clin Neurol Neurosurg. 2015. Sep;136:52–60. doi: 10.1016/j.clineuro.2015.05.015 [DOI] [PubMed] [Google Scholar]
- 53.Ingraham AM, Cohen ME, Raval MV, Ko CY, Nathens AB. Comparison of hospital performance in emergency versus elective general surgery operations at 198 hospitals. J Am Coll Surg. 2011. Jan;212(1):20–8 e1. doi: 10.1016/j.jamcollsurg.2010.09.026 [DOI] [PubMed] [Google Scholar]
- 54.Burningham Z, Hashibe M, Spector L, Schiffman JD. The epidemiology of sarcoma. Clin Sarcoma Res. 2012. Oct 4;2(1):14. doi: 10.1186/2045-3329-2-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Merletti F, Richiardi L, Bertoni F, Ahrens W, Buemi A, Costa-Santos C, et al. Occupational factors and risk of adult bone sarcomas: a multicentric case-control study in Europe. Int J Cancer. 2006. Feb 1;118(3):721–7. doi: 10.1002/ijc.21388 [DOI] [PubMed] [Google Scholar]
- 56.Maleki-Fischbach M, Jordan JM. New developments in osteoarthritis. Sex differences in magnetic resonance imaging-based biomarkers and in those of joint metabolism. Arthritis Res Ther. 2010;12(4):212. doi: 10.1186/ar3091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007. Jan;34(1):172–80. [PubMed] [Google Scholar]
- 58.Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009. Apr;36(4):809–15. doi: 10.3899/jrheum.080677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005. Sep;13(9):769–81. doi: 10.1016/j.joca.2005.04.014 [DOI] [PubMed] [Google Scholar]
- 60.Hannan MT, Anderson JJ, Pincus T, Felson DT. Educational attainment and osteoarthritis: differential associations with radiographic changes and symptom reporting. J Clin Epidemiol. 1992. Feb;45(2):139–47. doi: 10.1016/0895-4356(92)90006-9 [DOI] [PubMed] [Google Scholar]
- 61.Lee JY, Han K, Park YG, Park SH. Effects of education, income, and occupation on prevalence and symptoms of knee osteoarthritis. Sci Rep. 2021. Jul 7;11(1):13983. doi: 10.1038/s41598-021-93394-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
(DOCX)
(DOC)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.