See Clinical Research on Page 1742
Kidney transplantation (KT) is the preferred treatment for patients with end-stage kidney disease; however, KT outcomes are highly dependent on several donor and recipient variables. Although donor quality and ischemia times mainly drive early and long-term graft outcomes, several recipient variables such as age, dialysis vintage, presence of diabetes mellitus, and obesity also contribute significantly. Another not so uncommon recipient risk factor noted in several studies is chronic systemic hypotension, which affects up to 5–10% of patients with dialysis, particularly those on hemodialysis.1 Although the exact mechanisms for chronic hypotension on dialysis remains unclear and likely vary among patients, it has been associated with higher mortality among patients on prevalent dialysis.2 Among KT recipients, pretransplant hypotension has been implicated as a risk factor for delayed graft function (DGF) and primary nonfunction (PNF).3, 4, 5, 6 However, data on long-term graft outcomes and changes in blood pressure (BP) following KT in patients with chronic hypotension are limited. The study by Auñón et al.7 in this issue of the journal therefore is an important addition to our understanding of KT outcomes among recipients with chronic hypotension.
This single center retrospective observational study involved 66 recipients with chronic hypotension who received a kidney transplant between 2004 and 2020. Chronic hypotension was defined as systolic BP ≤ 100 mm Hg using a single reading on the day of hospital admission for transplantation, among patients not receiving antihypertensive treatment. The study included a control cohort (systolic BP > 100) that consisted of either recipients of contralateral kidneys or recipients who were matched for age, kidney type, and time of transplantation. The hypotension cohort had significantly higher rates of DGF (85.9% vs. 53.2%, P < 0.001), PNF (8.2% vs. 6.1%, P = 0.03) and lower estimated glomerular filtration rate at the end of follow-up (35 ml/min per 1.73 m2 vs. 48 ml/min per 1.73 m2, P = 0.001). The hypotension cohort also had lower mean graft survival (81 vs. 105 months, P = 0.022) and worse 1, 3, 5, and 8-year graft survival. The graft survival differences were primarily driven by high incidence of PNF, a substantial proportion of which were due to allograft venous thrombosis. The authors reported a potential benefit of lower PNF rates with the use of prophylactic vasoactive drugs and anticoagulation. Finally, the presence of a functioning graft led to BP normalization in patients with chronic hypotension.
The study findings have important implications for KT. The higher DGF and PNF risks noted in this study are in line with findings from previous studies.3, 4, 5, 6,8 In addition, Auñón et al.7 provide useful data on long-term outcomes, BP trends, and potential benefit of anticoagulation. These data can inform future research and decision-making regarding donor and candidate selection and peri-transplant practices. The long-term graft survival rates noted in the study can be seen as a glass being either half empty or half full. The significantly lower graft survival in the hypotension cohort suggests that the outcomes are less than satisfactory. The high PNF rate also raises concerns about appropriate utilization of donor kidneys, a scare resource. Contrarily, despite the use of high proportion of extended criteria donor kidneys and a higher graft loss risk, the 3-year and 5-year graft survival rates among patients with hypotension could be considered acceptable when compared to the quality of life and survival rates of KT candidates on chronic dialysis. Selection of appropriate candidates for KT however remains challenging. The risk associated with low BP is a continuous one and categorizing based on a single threshold will not be clinically applicable. In a retrospective study by Wazir et al.,6 each 1 mm Hg decrease in preoperative mean arterial pressure was associated with a 2% higher DGF risk. Thus, chronic hypotension should be considered in the context of other coexisting risk factors. Most patients with chronic hypotension have poor outcomes on dialysis and thus, transplant options should be explored. However, careful consideration should be given to donor selection and peri-transplant practices. Although the use of marginal kidneys is necessary from a societal point of view, such kidneys will be at significantly higher risk for DGF or PNF when transplanted to patients with hypotension.4 When such organs are accepted for transplantation, every attempt should be made to keep ischemia times short and optimize the use of machine perfusion techniques.
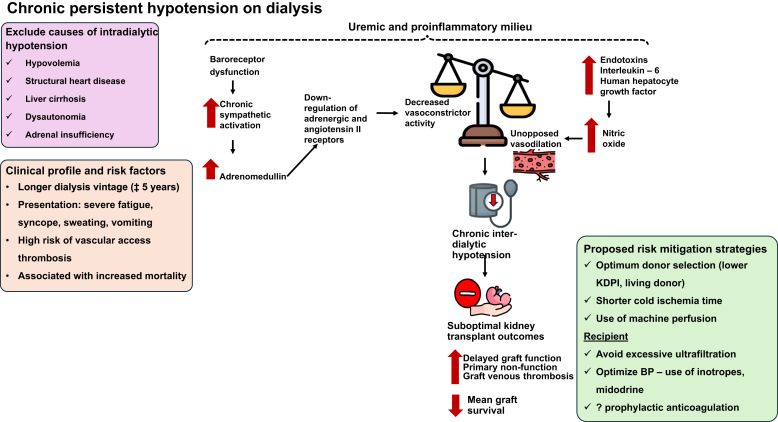
There are limited data to inform optimal therapeutic strategies for KT candidates with chronic hypotension. The pathophysiology of chronic hypotension in patients on dialysis remains poorly understood but a combination of autonomic dysregulation and excess activity of vasodilatory mediators likely play a role in lowering peripheral vascular resistance (Figure 1).9 The finding by Auñón et al.7 that hypotension improved significantly in the post-KT period, often within few weeks, suggests that the abnormal vascular milieu improves quickly after KT. In addition, in the absence of PNF, the finding that long-term kidney survival was similar between hypotensive and normotensive patients suggests that the predominant risks are perioperative in nature. Therefore, further research on mitigation measures that focus on the perioperative period are necessary. This is particularly important given that many of donor and recipient risk factors for DGF and PNF are nonmodifiable. Although measures such as careful assessment of cardiac status, avoiding excessive ultrafiltration, and attention to hypotension management may help improve outcomes, there is a dearth of clinical trials to inform clinical practice. The finding that PNF was mainly driven by venous thrombosis and that there was a suggestion of benefit from prophylactic anticoagulation is intriguing and requires additional investigation. Firm conclusions, however, cannot be drawn because the use of vasoactive agents and anticoagulation was not protocolized in this study. In addition, previous studies have not noted this significantly elevated risk of graft thrombosis.3, 4, 5, 6 The reasons for this discrepancy are not clear and more studies are warranted. The potential benefits of anticoagulation will need to be examined in prospective controlled studies before it can be recommended for all recipients with chronic hypotension.
Figure 1.
Pathophysiology and implications of chronic hypotension on dialysis. BP, blood pressure; KDPI, kidney donor profile index.
Other limitations of the study should also be noted. First, as a retrospective single center study, its external validity is limited to patients with similar geographical and risk profiles. Second, the definition of chronic hypotension was based on only one pretransplant blood pressure reading of systolic ≤ 100 mm Hg. Although a formal definition of chronic (interdialysis) hypotension is lacking, using more readings in the pretransplant period will aid in better understanding of the implications of chronic hypotension and KT outcomes. Third, the study cohort consisted of patients whose transplant dates spanned over 2 decades, during which immunosuppression and transplant practices have evolved considerably. Fourth, only a small proportion (∼5%) of transplants in this study was from living donors. Thus, the results are primarily applicable to deceased donor KT. Larger prospective studies are required to evaluate whether living donor KT can offer better outcomes for patients with chronic hypotension.
Despite the limitations, the study by Auñón et al.7 contributes to furthering our understanding of challenges to transplanting kidneys in patients with chronic hypotension. Although the study suggests that chronic persistent hypotension is not an absolute contraindication, it raises several questions, that is, the known unknowns, which will need to be answered by future studies.
Disclosure
CMP reports research funding from the National Institutes of Health and consulting fees from Replimune, Inc, outside of the submitted work. DB declared no competing interests.
References
- 1.Cases A., Coll E. Chronic hypotension in the dialysis patient. J Nephrol. 2002;15:331–335. [PubMed] [Google Scholar]
- 2.Port F.K., Hulbert-Shearon T.E., Wolfe R.A., et al. Predialysis blood pressure and mortality risk in a national sample of maintenance hemodialysis patients. Am J Kidney Dis. 1999;33:507–517. doi: 10.1016/s0272-6386(99)70188-5. [DOI] [PubMed] [Google Scholar]
- 3.Alhamad T., Brennan D.C., Brifkani Z., et al. Pretransplant midodrine use: a newly identified risk marker for complications after kidney transplantation. Transplantation. 2016;100:1086–1093. doi: 10.1097/tp.0000000000001113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dolla C., Mella A., Vigilante G., et al. Recipient pre-existing chronic hypotension is associated with delayed graft function and inferior graft survival in kidney transplantation from elderly donors. PLoS One. 2021;16 doi: 10.1371/journal.pone.0249552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webber A., Hambleton J., Chami A., et al. Mean arterial blood pressure while awaiting kidney transplantation is associated with the risk of primary nonfunction. Transplantation. 2012;93:54–60. doi: 10.1097/TP.0b013e3182398035. [DOI] [PubMed] [Google Scholar]
- 6.Wazir S., Abbas M., Ratanasrimetha P., Zhang C., Hariharan S., Puttarajappa C.M. Preoperative blood pressure and risk of delayed graft function in deceased donor kidney transplantation. Clin Transplant. 2022;36 doi: 10.1111/ctr.14776. [DOI] [PubMed] [Google Scholar]
- 7.Auñón P., Cavero T., García A., González J., Andrés A. Kidney transplantation outcomes of patients with chronic hypotension in dialysis. Kidney Int Rep. 2024;9:1742–1751. [Google Scholar]
- 8.Ozdemir F.N., Ibis A., Altunoglu A., Usluogullari A., Arat Z., Haberal M. Pretransplantation systolic blood pressure and the risk of delayed graft function in young living-related renal allograft recipients. Transplant Proc. 2007;39:842–845. doi: 10.1016/j.transproceed.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 9.Palmer B.F. Why are some dialysis patients chronically hypotensive in the absence of heart disease and volume depletion? Semin Dial. 2011;24:404–405. doi: 10.1111/j.1525-139X.2011.00915.x. [DOI] [PubMed] [Google Scholar]