Abstract
Background:
Traditional yoga texts describe “cross nostril breathing,” with inhalation and exhalation through different nostrils. Previous research reported no clear differences in oxygen consumption during uninostril breathing (i.e., inhalation and exhalation through the same nostril), hence not supporting right and left uninostril breathing as activating or relaxing, respectively, with no research on oxygen consumed in “cross nostril breathing.”
Methods:
Oxygen consumed during “cross nostril breathing” was measured in healthy participants (n = 47, males, 26.3 ± 6.4 years). Five sessions (viz., right nostril inspiration yoga breathing [RNIYB], left nostril inspiration yoga breathing [LNIYB], alternate nostril yoga breathing [ANYB], breath awareness (BAW), and quiet rest (QR) were conducted on separate days in random order. Sessions were 33 min in duration with pre, during, and post states.
Results:
Volume of oxygen consumed (VO2) and carbon dioxide eliminated (VCO2) increased during RNIYB (9.60% in VO2 and 23.52% in VCO2), LNIYB (9.42% in VO2 and 21.20% in VCO2) and ANYB (10.25% in VO2 and 22.72% in VCO2) with no significant change in BAW and QR. Diastolic blood pressure decreased during BAW and QR and after all five sessions (P < 0.05; in all cases). All comparisons were with the respective preceding state.
Conclusion:
During the three yoga breathing practices, the volume of oxygen consumed increased irrespective of the nostril breathed through, possibly associated with (i) conscious regulation of the breath; (ii) attention directed to the breath, and (iii) “respiration-locked cortical activation.” Restriction of the study to males reduces the generalizability of the findings.
Keywords: Alternate nostril, blood pressure, energy expenditure, nasal cycle, oxygen consumption, yoga breathing
Introduction
The nasal cycle is an ultradian rhythm of lateralized, alternating nostril mucosal engorgement varying every 30 min to 6 h.[1] This rhythm is believed to reflect dynamic lateralization of autonomic nervous system activity.[2,3] The nasal cycle is hence considered relevant to the basic rest–activity cycle, which enables organisms to alternate between rest and activity so as to use energy optimally.[4,5,6] In yoga, conscious regulation of the airflow through both nostrils either in isolation or alternately, was described as a means of consciously regulating a wide range of functions and behaviors.[7] In this description, the left nostril functions in synchrony with a lunar channel for subtle energy (ida nadi, in Sanskrit), whereas the functions of the right nostril are synchronized with the solar channel for life energy (surya nadi, in Sanskrit). According to this description, lateralized right uninostril yoga breathing was considered to be physiologically activating, whereas lateralized left uninostril yoga breathing was considered to have the reverse effect, whereas alternate nostril breathing was believed to achieve a balance between activation and rest.
The effects of nostril-regulated yoga breathing on oxygen consumption have been reported.[8,9] Oxygen consumption increases with physical activity, mental activity, and psychological distress, while it is lowest in basal resting conditions.[9,10,11,12,13] The influence of yoga practice on oxygen consumption varies with reports of reduced baseline oxygen consumption in experienced yoga practitioners[14] and individual practices causing either an increase or decrease in oxygen consumption.[8,15,16]
Early studies reported changes in baseline oxygen consumption after 30 days of daily practice of uninostril regulated yoga breathing practices compared to the baseline values, with a significant increase after a month of right uninostril breathing (37%), with nonsignificant increases following left uninostril breathing (24%) and alternate nostril breathing (18%).[17] Also, immediately, after 45 min of right uninostril yoga breathing, the oxygen consumption increased by 17% compared to the preceding baseline value.[18] These results support the traditional description of right uninostril yoga breathing as being physiologically activating, though changes related to left uninostril and alternate nostril yoga breathing were less clear. Conclusions about the effects were difficult to arrive at due to small sample sizes and variations in comparators.
An earlier study also reported the effect of right uni-nostril-regulated yoga breathing on blood pressure and sympathetic cutaneous vasomotor activity (based on a photoplethysmogram recording) following 45 min of practice.[18] The changes indicated increased systolic blood pressure (SBP) and increased cutaneous vasomotor activity, which is an index of sympathetic activity.[18,19] Blood pressure is regulated by multiple factors, including peripheral vascular resistance and cardiac output both of which are controlled by the autonomic nervous system, with raised sympathetic activity increasing both of them.[20] Hence, the results of the study,[18] suggest that right uninostril-regulated yoga breathing increases sympathetic activity based on the changes in cutaneous vasoconstrictor activity and blood pressure.[18,19]
These studies evaluated uninostril breathing, with both inhalation (I) and exhalation (E) through the same nostril. In contrast to this, in the traditional yoga texts (viz, Hatha Pradipika circa 1300 C. E.; Gheranda Samhita Circa 1600 C. E), nostril-regulated yoga breathing or pranayama, involves I through one nostril, with E through the other nostril. Hence, the traditional yoga breathing practices are right I-left E called suryabhedan pranayama, whereas left I-right E yoga breathing is called chandrabhedan pranayama.
To our knowledge, the effects of these “cross-nostril” (i.e., I through one nostril, E through the other) conventionally described yoga breathing practices on oxygen consumption have not been reported.
Hence, the present randomized crossover study was conducted to determine the effects of (i) right nostril inspiration yoga breathing (RNIYB), (ii) left nostril inspiration yoga breathing (LNIYB), (iii) alternate nostril yoga breathing (ANYB), (iv) breath awareness (BAW) as an interventional control, and (v) quiet rest (QR) as control. It was hypothesized that RNIYB would increase oxygen consumption (VO2), LNIYB would reduce oxygen consumption, while the effect of ANYB would be not polarized in either direction. The blood pressure was also recorded during the sessions as an indicator of sympathetic activity.[21]
Methods
Participants
Forty-seven healthy male student volunteers aged between 18 and 46 years (group mean age ± standard deviation [SD]; 26.34 ± 6.38 years) were recruited from a yoga university in India. The sample size was not calculated a priori, however, the post-hoc power was determined from the change in VO2 during RNIYB using the G Power Program.[22] With n = 47, α =0.05, and Cohen’s d of 0.55, statistical power = 1.00. Participants were included if they: (i) had at least 6 months of experience of the yoga breathing techniques[23] and (ii) agreed to five consecutive days of testing. Participants were excluded if they (i) had any diagnosed health disorder, and (ii) required any medication or consumed tobacco in any form (none were excluded). Females were excluded from the trial to reduce inter-person variability, based on reported variations in oxygen consumption with the phases of the menstrual cycle.[24] Signed informed consent was obtained from each participant. The institution’s ethical committee approved the study (YRD-018/007).
Study design
The study was a randomized crossover trial. Randomization and allocation were carried out in three steps: (i) a person blinded to the study details allotted a serial number from 1 to 5 to each of the five sessions. (ii) An online randomizer (www.randomizer.org) generated fifty sets of random sequences of the five digits, i.e., 1, 2, 3, 4 and 5. (iii) Each participant was allotted one sequence of the digits, which determined the sequence of the five sessions for that participant. The participants were unaware of the order of sessions assigned. Assessments included (i) volume of oxygen consumed (VO2), (ii) volume of carbon dioxide eliminated (VCO2), (iii) energy expenditure (EE), and (iv) SBP and diastolic blood pressure (DBP): (i) for 5 min preceding the intervention or control sessions (baseline recording), (ii) for 18 min during the intervention or control sessions and (iii) for 10 min postintervention or control sessions. The duration of intervention was selected based on the clinical and research experience of the authors. The authors have found that the participants can practice various pranayamas efficiently and without fatigue if they have in between rest periods.[25,26] Three 5-min periods of practice with a 1-min rest period in between two consecutive 5 min practice periods were found to be the most feasible duration for participants to include in their daily practice. Therefore, the duration of this study is based on practical considerations, laboratory research, and discussion with participants, wherein they are asked to self-rate their level of comfort. Furthermore, in the present study, a familiarization session was not carried out considering that the participants were already required to come to the laboratory for five consecutive days at the same time of the day. In addition, the participants were aware of the laboratory conditions as they were students of the university and had visited the laboratory previously for assignments related to their coursework.
A schematic representation of the study design is provided in Figure 1.
Figure 1.
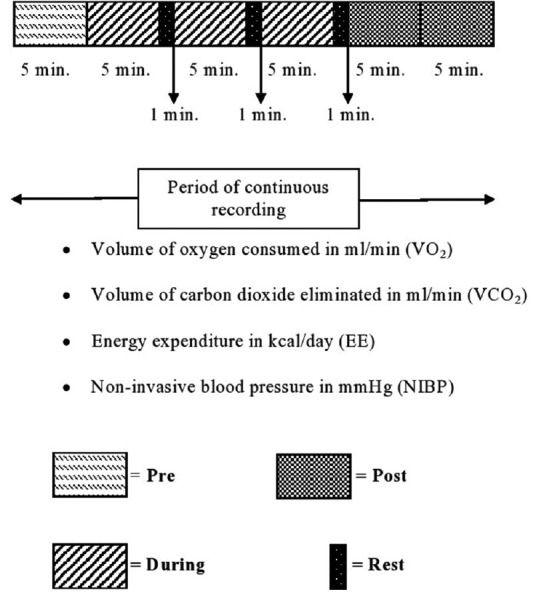
Schematic representation of the design of the study. VO2: Oxygen consumed, VCO2: Carbon dioxide eliminated, EE: Energy expenditure, NIBP: Non-invasive blood pressure
Assessment procedure
Participants were requested to avoid vigorous physical activity one night before and during testing. The participants were requested to come to the laboratory straight away after waking up in the morning for assessments following an overnight 12-h fast which was confirmed from them on their arrival at the laboratory. All participants reported that they adhered to this condition. Hence, they would not have carried out vigorous activity. However, in walking to the research laboratory they could walk briskly (150 m), which they were told to avoid. Furthermore, there was 15 min during which students filled in 24 h diet recall questionnaire, while seated. These 15 min gave time for the physiological changes (if any) related to walking to return to baseline.
On arrival at the laboratory, each participant was asked to empty the urinary bladder. Assessments were conducted at fixed times of the day (i.e., between 05:00 and 07:30 h) in a sound-attenuated air-conditioned laboratory (the temperature and humidity were maintained at 24.44 ± 2.14°C and 52.79 ± 5.87% on all days). The participants were recumbent with eyes closed during the session to allow the use of a canopy hood for recording (detailed below). Assessments were taken continuously in the 33 min session.
Assessments
Volume of oxygen consumed and carbon dioxide eliminated
An open-circuit oxygen consumption analyzer (Quark CPET [Cardio-Pulmonary Exercise Testing] COSMED, Italy) was used to assess VO2 and VCO2.[27] Before the assessment the equipment was calibrated for the volume and gas calibration using the method described elsewhere.[27] The calibrated equipment was used to measure: (i) VO2, (ii) VCO2, and (iii) EE.
The breathing techniques used in the study involved nostril manipulation with the thumb and ring finger; therefore, the participants were assessed for VO2 and VCO2 using a canopy hood, which ensures that exhaled air blends with ambient air.[28] The canopy was fitted around the waist and checked to be airtight.
Non-invasive blood pressure
The blood pressure was recorded with a TruscopeTM II Multiparameter monitor (Guangdong BiolightMeditech, China) from the left brachial artery when the participant was in a supine position with both arms extended and placed on the bed at the level of the heart with support. Baseline recordings were taken after 5 min of rest in this position. The mean arterial pressure (MAP) was calculated using the formula (MAP = DBP + 1/3 [SBP–DBP]).
Twenty-four-hour diet recall (energy intake/day)
The interview to determine the 24-h food recall was carried out by one of the authors (AS) using the following method: The participants were asked (i) to recall and list the food items they had eaten in the 24 h before the assessments, (ii) the process of preparation of each food item (e.g., raw, cooked, boiled or baked), (iii) the size of utensils used to consume the food, the researcher who interviewed the participants had four different types of utensils (i.e., bowl, cup, glass, and spoon), each with four sizes. Participants were asked to identify the size they had used. The volume of each of the utensils of different sizes for various food items consumed in India had already been determined.[29] The total energy intake/day as well as the amount of macronutrients was calculated based on norms for Indian foods.[29,30]
Interventions
During the assessments, participants were recumbent (i.e., savasana or corpse posture). The following interventions were given for 18 min each: RNIYB, LNIYB, ANYB, BAW, and QR. For all practices, the left nostril is occluded with the middle and ring fingers of the right hand and the right nostril is occluded with the thumb (the dominant hand for all participants).
Right nostril inspiration yoga breathing
The cycle begins with inhalation (right nostril), followed by exhaling (left nostril). The cycle is repeated.
Left nostril inspiration yoga breathing
The cycle begins with inhalation (left nostril) followed by exhaling (right nostril). The cycle is repeated.
Alternate nostril yoga breathing
The steps were: (i) exhaling (left nostril), (ii) inhaling (left nostril), (iii) followed by exhaling (right nostril), and (iv) finally, inhaling (right nostril). This is one complete one cycle. This sequence is repeated as mentioned above.
Breath awareness
Participants were asked to consciously direct their attention to the flow of air through the nasal passage, not altering their breathing. BAW was selected as an intervention because being aware of the breath is an inherent part of all yoga breathing techniques.
Quiet rest
During this practice, the participants were asked to avoid conscious regulation of their breath or of their thoughts, which were hence allowed to wander freely.
Quality of intervention and control sessions
At the end of each session, the participants were asked to rate their practice session on a 10 cm long horizontal analog scale (i.e., “how well were you able to follow the practice”) with the left and right extremes of the scale labeled as “Worst” and “Very well”, respectively. Sessions were included for analysis if the rating for the question was >7.5 cm. The cutoff (i.e., >7.5 cm) to be included in a session in the analyses was arbitrarily decided.
Data extraction
The mean values of the (i) VO2 (ml/min), (ii) VCO2 (ml/min), and (iii) EE were calculated for preintervention or control session (5 min), during the intervention (18 min; three 5 min active breathing intervention or control sessions with 1 min rest after each 1 min) and postintervention session (10 min; two 5 min periods).
Statistical analysis
Statistical analyses were separate repeated measures analyses of variance (RM-ANOVA) through IBM SPSS Version 24.0 followed by post-hoc analyses with Bonferroni adjustment. Each RM-ANOVA had two “Within subjects” factors, i.e., Sessions (with five levels; RNIYB, LNIYB, ANYB, BAW, and QR) and States (with six levels, i.e., pre, during 1, during 2, during 3, and post 1 and post 2). The level of significance (α) was set at 0.05 (two-tailed).
The energy intake/day (in kilocalories/day) and ratio of macronutrients (i.e., carbohydrates (in g/day), fat (in g/day), and protein (in g/day)) on the five recording days were compared using a one-way ANOVA.
Results
Forty-seven healthy male participants completed the study. The group mean ± SD, values of the quality of practice assessed with the visual analog scale were (i) 9.03 ± 1.27 for RNIYB, (ii) 8.99 ± 1.09 for LNIYB, (iii) 9.01 ± 0.90 for ANYB, (iv) 8.69 ± 1.28 for BAW, and (iv) 8.97 ± 1.33 for QR. The baseline characteristics of the participants are presented in Table 1.
Table 1.
Baseline characteristics of the participants
| Characteristics | Details |
|---|---|
| Sample | |
| Number of participants | 47 |
| Gender | Males |
| Age | |
| Age range (years) | 18–46 |
| Group mean age±SD (years) | 26.34±6.38 |
| Height (cm) | |
| Group mean age±SD | 166.94±6.20 |
| Weight (kg) | |
| Group mean age±SD | 58.95±6.87 |
| BMI (kg/m2) | |
| Group mean±SD | 21.16±2.22 |
| Education in years (n) | |
| 10–12 years of education | 27 |
| 15 years of education | 12 |
| 17 years of education | 8 |
| Yoga experience | |
| Group average yoga experience±SD (months) | 43.64±32.84 |
| Yoga experience range (months) | 6–144 |
| Time spent in practicing yoga in a day (min) | |
| Group mean±SD | 98.19±44.24 |
| Marital status | |
| Unmarried (n) | 47 |
| Health status | |
| Presence of any disease (n) | 0 |
| Taking any medication (n) | 0 |
| Diet | |
| Lacto-vegetarians | 47 |
| Sleep quality | |
| Self-rating of sleep quality on a 10 cm analog scale | 8.80±0.79 |
| Duration of sleep (min) | 338.44±4.22 |
| Duration of physical activity/day (min) | |
| Physical activity in a day (min) | 48.04±58.18 |
| Physical activity in a day range (min) | 8–244 |
| Tobacco and alcohol | |
| Consumption of tobacco including smoking (n) | 0 |
| Consumption of alcohol (n) | 0 |
SD: Standard deviation, BMI: Body mass index
Repeated measures analyses of variance
Volume of oxygen consumed, carbon dioxide eliminated, and Energy expenditure
The VO2 showed a significant difference for States (Huynh-Feldt: F2.31,106.46, =61.86, P < 0.001), Sessions (Huynh-Feldt: F4, 184 = 8.35, P < 0.001) and an interaction between Sessions and States (Huynh-Feldt: F7.84, 360.79 = 19.71, P < 0.001).
The VCO2 also showed a significant difference between States (Huynh-Feldt: F1.61, 74.20 = 67.27, P < 0.001), Sessions (Huynh-Feldt: F3.59, 165.00 = 10.09, P < 0.001) and interaction between Sessions and States (Huynh-Feldt: F5.41, 248.64 = 24.16, P < 0.001).
Furthermore, the EE showed a significant difference between States (Huynh-Feldt: F1.92, 88.19 = 65.75, P < 0.001), Sessions (Huynh-Feldt: F4, 184 = 10.37, P < 0.001) and interaction between Sessions and States (Huynh-Feldt: F6.41, 295.01 = 22.68, P < 0.001).
Non-invasive blood pressure
There was also a significant difference for States (Huynh-Feldt: F (3.39, 156.12 = 18.126, P < 0.001), Sessions (Huynh-Feldt: F4, 184 = 6.96, P < 0.001) and interaction between Sessions and States (Huynh-Feldt; F11.04, 507.91 = 4.58, P < 0.001) for SBP.
The DBP also showed a significant difference for States (Huynh-Feldt: F2.73, 125.36 = 29.44, P < 0.001), Sessions (Huynh-Feldt: F4, 184 = 7.42, P < 0.001) and interaction between Sessions and States (Huynh-Feldt: F10.53, 484.44 = 4.25, P < 0.001).
Furthermore, there was a significant difference for States (Huynh-Feldt: F2.77, 127.71 = 152.19, P < 0.001), Sessions (Huynh-Feldt: F4, 184 = 13.52, P < 0.001) and interaction between Sessions and States (Huynh-Feldt: F10.74, 494.02 = 255.09, P < 0.001) for MAP.
Post-hoc analyses
The VO2 increased in the three during states (i.e., during 1, during 2, and during 3) for (i) RNIYB, (ii) LNIYB, and (iii) ANYB (P < 0.05; in all cases). The BAW also showed an increase in VO2 during 1 (P < 0.05).
The VCO2 increased in the three during states (i.e., during 1, during 2, and during 3) and decreased in the two post states for (i) RNIYB, (ii) LNIYB, and (iii) ANYB (P < 0.05; in all cases). The BAW also showed an increase in VCO2 during 1 (P < 0.05).
The EE increased in the three during states (i.e., during 1, during 2, and during 3) for (i) RNIYB, (ii) LNIYB, and (iii) ANYB (P < 0.05; in all cases) and during 1 for BAW (P < 0.05).
SBP increased during 2 for LNIYB while decreasing in post 2 for BAW, and during 3 and post 1 and post 2 states for QR (P < 0.05; in all cases).
DBP decreased in the three during states and the two post states for (i) BAW and (ii) QR. Furthermore, DBP decreased during 3 and the two post states (i.e., post 1 and post 2) for ANYB (P < 0.05; in all cases).
MAP decreased in the three during states (i.e., during 1, during 2, and during 3) and the two post states (i.e., post 1 and post 2) for BAW, two during states and the two post states for QR, the post 2 for RNIYB, during 2 and post 2 for LNIYB, and post 2 for ANYB (P < 0.05; in all cases).
The group mean ± SD for (i) VO2, (ii) VCO2, (iii) EE, (iv) SBP, (v) DBP, and (vi) MAP during different states of each session are given in Table 2.
Table 2.
Values of the (i) volume of oxygen consumed, (ii) volume of carbon dioxide eliminated, (iii) energy expenditure, and (iv) blood pressure in the five sessions
| Variables | States | RNIYB | LNIYB | ANYB | BAW | QR |
|---|---|---|---|---|---|---|
| VO2 (mL/min) | Pre | 278.69±42.96 | 275.60±45.35 | 270.93±48.79 | 268.57±46.30 | 266.61±47.42 |
| During 1 | 303.76±47.96*** | 303.58±51.95*** | 298.93±53.99*** | 276.68±47.01** | 269.32±45.90 | |
| During 2 | 306.32±47.78*** | 302.00±52.67*** | 298.17±54.22*** | 274.05±48.75 | 267.94±45.93 | |
| During 3 | 306.28±48.38*** | 299.12±54.12*** | 299.05±55.36*** | 273.55±45.15 | 267.41±47.40 | |
| Post 1 | 279.78±43.99 | 273.87±47.72 | 271.42±49.14 | 270.17±45.26 | 268.50±47.92 | |
| Post 2 | 283.49±43.92 | 278.26±48.15 | 278.54±50.31* | 273.16±43.10 | 267.37±47.54 | |
| VCO2 (mL/min) | Pre | 164.43±30.13 | 167.08±37.19 | 164.36±44.21 | 160.02±33.16 | 162.01±28.89 |
| During 1 | 212.38±51.17*** | 215.86±55.44*** | 213.16±56.73*** | 173.03±44.65* | 161.59±28.60 | |
| During 2 | 202.89±47.22*** | 201.04±49.70*** | 200.23±52.48*** | 165.32±43.04 | 161.62±30.80 | |
| During 3 | 193.99±43.46*** | 190.61±47.73** | 191.72±51.02*** | 164.69±40.32 | 161.97±30.16 | |
| Post 1 | 143.06±38.46*** | 142.63±44.32*** | 138.69±49.17*** | 154.17±34.18 | 160.82±30.91 | |
| Post 2 | 153.82±35.72** | 151.82±40.86** | 151.76±47.94* | 159.34±35.50 | 160.98±31.60 | |
| EE (kcal/day) | Pre | 1810.28±267.04 | 1798.18±297.87 | 1767.90±325.05 | 1747.27±293.97 | 1740.19±295.17 |
| During 1 | 2032.16±327.44*** | 2037.41±364.17*** | 2007.26±372.74*** | 1814.65±317.89** | 1754.21±285.99 | |
| During 2 | 2029.21±319.93*** | 2002.38±362.29*** | 1980.11±370.83*** | 1786.60±327.81 | 1746.73±289.87 | |
| During 3 | 2013.11±318.84*** | 1968.16±368.03*** | 1969.72±375.37*** | 1782.73±300.49 | 1744.49±299.84 | |
| Post 1 | 1778.83±284.46 | 1745.21±317.97 | 1724.83±331.99 | 1745.58±292.73 | 1748.38±302.83 | |
| Post 2 | 1817.47±279.51 | 1785.49±317.47 | 1786.85±338.24 | 1771.08±280.11 | 1742.49±302.14 | |
| Systolic BP (mmHg) | Pre | 106.97±5.75 | 105.86±5.82 | 106.59±6.69 | 106.09±6.89 | 106.09±6.89 |
| During 1 | 108.58±6.93 | 106.88±5.67 | 107.75±5.76 | 105.11±6.34 | 105.11±6.34 | |
| During 2 | 108.67±7.25 | 107.66±6.70** | 107.86±6.59 | 104.80±6.22 | 104.80±6.22 | |
| During 3 | 108.97±7.97 | 107.02±5.81 | 107.83±6.00 | 104.80±6.39 | 104.80±6.39* | |
| Post 1 | 106.86±6.30 | 105.32±5.98 | 105.70±6.47 | 104.81±6.34 | 104.81±6.34** | |
| Post 2 | 105.86±5.67 | 105.10±6.49 | 107.15±5.94 | 104.02±5.86** | 104.02±5.86*** | |
| Diastolic BP (mmHg) | Pre | 67.15±4.68 | 66.89±4.89 | 67.14±5.24 | 66.77±4.71 | 67.01±4.81 |
| During 1 | 67.36±5.02 | 66.74±5.76 | 67.02±4.41 | 65.59±4.91** | 66.17±4.88* | |
| During 2 | 67.41±5.62 | 67.10±5.41 | 67.00±4.68 | 64.94±4.55*** | 65.22±5.19*** | |
| During 3 | 67.63±5.16 | 67.12±5.20 | 67.31±4.43 | 64.82±4.78*** | 64.48±4.19*** | |
| Post 1 | 66.48±5.04 | 65.77±5.19 | 65.86±4.80* | 64.54±4.62*** | 64.19±5.08*** | |
| Post 2 | 65.00±4.30*** | 65.11±5.54** | 65.24±4.81** | 63.82±4.52*** | 62.97±5.00*** | |
| Mean arterial BP (mmHg) | Pre | 80.42±4.83 | 79.88±4.94 | 80.29±5.52 | 79.87±5.24 | 80.14±4.95 |
| During 1 | 81.10±5.44 | 63.89±4.50*** | 80.59±4.66 | 78.77±5.12** | 79.47±5.00 | |
| During 2 | 81.16±6.01 | 80.62±5.56 | 80.62±4.99 | 78.23±4.90** | 78.81±5.57** | |
| During 3 | 81.41±5.85 | 80.42±5.14 | 80.82±4.72 | 78.15±5.11*** | 77.97±5.06*** | |
| Post 1 | 79.94±5.19 | 78.96±5.15 | 79.14±5.10 | 77.97±4.87** | 77.65±5.31*** | |
| Post 2 | 78.62±4.56** | 78.44±5.56** | 64.80±4.12*** | 77.22±4.68*** | 76.48±5.33*** |
*P<0.05, **P<0.01, ***P<0.001; repeated-measures analysis of variance with Bonferroni adjustment comparing during and postvalues with prevalues. Values are group mean±SD . SD: Standard deviation, BP: Blood pressure, EE: Energy expenditure, VO2: Volume of oxygen consumed, VCO2: Volume of carbon dioxide eliminated, RNIYB: Right nostril inspiration yoga breathing, LNIYB: Left nostril inspiration yoga breathing, ANYB: Alternate nostril yoga breathing, BAW: Breath awareness, QR: Quiet rest
One-way analysis of variance
There was no significant difference between participants’ diet on the five recording days for (i) energy intake (F4,230 = 0.694, P = 0.597), (ii) carbohydrate (F4,230 = 1.492, P = 0.205), (iii) fat (F4,230 = 1.221, P = 0.303) and (iv) protein (F4,230 = 0.047, P = 0.996) intake (one way ANOVA).
Discussion
During RNIYB, LNIYB, and ANYB there were comparable increases in VO2 (i.e., 9.60%, 9.42% and 10.25%, respectively), compared to the respective preceding values. There were no changes during BAW or QR. These results are contrary to the hypothesized increase in VO2 during RNIYB, with a decrease in VO2 during LNIYB and no polarized change during ANYB.
These findings suggest that the increase in VO2 during these yoga breathing practices was not an effect of the nostril breathed through, but of a physiological change common to the three yoga breathing practices, which is comparable to previous early reports of effects of uninostril yoga breathing practices (i.e., inhale-exhale through the same nostril).[17]
All three yoga breathing practices required the participants to volitionally regulate their respiration, consciously breathing through either one nostril or both nostrils alternately, depending on the practice. Furthermore, all yoga breathing practices required participants to be aware of their breathing during the practice, regulating their breathing with conscious awareness.[23] Previously, the brain activity during volitional breathing and BAW was assessed with intracranial electroencephalogram (EEG) recorded simultaneously with the respiration showed brain activity in both volitional breathing and attentional breathing.[31] Since yoga breathing includes both volitional and attentional breathing, these brain areas may be active during yoga breathing. Cortical activation during yoga breathing practices is supported by previous research reporting improved performance in attention or memory tasks following episodes of yoga breathing.[16] Hence, increased activity in these brain areas could contribute to the increase in oxygen consumption during the three yoga breathing practices assessed here.
Yoga breathing may influence brain activity in other ways. During normal respiration, respiratory movements, respiratory sensations, or chemosensitive signals increase brain activity as “respiration-locked cortical activation.”[32] Which may be increased if the person is aware of the signals arising from respiration.[33,34] Yoga breathing requires the participant to maintain open-minded attention to each moment and to the sensations arising from respiration.[35] Hence, yoga breathing could contribute to increased “respiration-locked cortical activation,” which in turn may lead to an increase in oxygen consumption.
No increase in oxygen consumption was noted during BAW which suggests that being aware of the breath alone does not have the same effect as yoga breathing with conscious modification of nostril regulation. This speculation is supported by previously reported increases in oxygen consumption during several yoga breathing practices which use volition to modify specific characteristics of breathing.[8]
The yoga breathing practices studied here are unlikely to have increased the work of breathing. Previously, oxygen consumption was recorded in patients with chronic obstructive pulmonary disease during physical therapy breathing (viz., diaphragmatic breathing or pursed lip breathing) to assess the work of breathing during the breathing exercises.[36] Oxygen consumption decreased by an average of 8.4 ml/min during physical therapy breathing compared with spontaneous breathing, hence indicating no increase in work of breathing during these physical therapy breath exercises in patients with COPD.[36] Hence it appears unlikely that in the present healthy persons, an increase in work of breathing during the three yoga breathing practices (which are comparable to the physical therapy breathing exercises) accounted for the increase in oxygen consumption.
The present results are comparable to a previous early report of increased baseline oxygen consumption after a month of right uninostril yoga breathing, with nonsignificant increases in oxygen consumed after a month of left uninostril and alternate nostril yoga breathing.[17] Minor differences in the magnitude of change may be related to differences in the spirometer used for assessment, participants’ characteristics, and study design, among other factors.
Carbon dioxide elimination (VCO2) indicates efficiency in alveolar ventilation, pulmonary perfusion, CO2 production, and ventilation optimization.[37] VCO2 was greater during the three yoga breathing practices (when oxygen consumption increased as well) compared to the respective preceding state, suggesting that ventilation during the yoga breathing practices was adequate. Following the three yoga breathing practices, when oxygen consumption was not higher than the preceding state, the VCO2 decreased. The physiological state after an episode of yoga breathing is described as associated with mental calm and rest,[38] which could be reflected in no change in oxygen consumption and a decrease in VCO2.
SBP is determined chiefly by the stroke volume, whereas peripheral vascular resistance largely determines the DBP, both of which increase with increased sympathetic activity.[21] The changes in systolic and DBP during and after both BAW and QR indicate a decrease in sympathetic activity.[19,20,21] Contrary to our hypothesis, there was an increase in SBP during chandrabheda pranayama, suggesting an increase in sympathetic activity.[19,20,21] The mechanisms underlying this are less easy to explain but could include the fact that chandrabhedan is a cross-over breathing requiring inhalation through the left nostril and exhalation through the right nostril. Hence, the effect may be considered to be of right nostril exhale, though this remains a speculation. The DBP decreased not only after the BAW and QR sessions but also after the three breathing sessions. This reduction may be attributed to the recumbent posture assumed in all five sessions.
Conclusion
In summary, the present study found comparable increases in oxygen consumption during RNIYB, LNIYB, and ANYB, compared to the respective preceding states speculated to be due to increased activity in the brain during yoga breathing related to (i) attention directed to the breath and (ii) “respiration-locked cortical activation.” The results are limited in generalizability since the results and conclusions were restricted to males alone.
Ethical statement
The approval of the Institutional Ethics Committee was obtained (approval number YRD-018/007).
Consent to participate statement
The signed informed consent of each participant was obtained.
Data availability statement
The datasets generated during analysis for the current study are available from the corresponding author on reasonable request.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pendolino AL, Lund VJ, Nardello E, Ottaviano G. The nasal cycle: A comprehensive review. Rhinol Online. 2018;1:67–76. [Google Scholar]
- 2.Werntz DA, Bickford RG, Bloom FE, Shannahoff-Khalsa DS. Alternating cerebral hemispheric activity and the lateralization of autonomic nervous function. Hum Neurobiol. 1983;2:39–43. [PubMed] [Google Scholar]
- 3.Backon J, Matamoros N, Ramirez M, Sanchez RM, Ferrer J, Brown A, et al. Afunctional vagotomy induced by unilateral forced right nostril breathing decreases intraocular pressure in open and closed angle glaucoma. Br J Ophthalmol. 1990;74:607–9. doi: 10.1136/bjo.74.10.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shannahoff-Khalsa D. Lateralized rhythms of the central and autonomic nervous systems. Int J Psychophysiol. 1991;11:225–51. doi: 10.1016/0167-8760(91)90017-r. [DOI] [PubMed] [Google Scholar]
- 5.Kleitman N. Basic rest-activity cycle –22 years later. Sleep. 1982;5:311–7. doi: 10.1093/sleep/5.4.311. [DOI] [PubMed] [Google Scholar]
- 6.Aschoff J, Gerkema MP. On diversity and uniformity of ultradian rhythms. In: Schulz H, Lavie P, editors. Ultradian Rhythms in Physiology and Behavior. Berlin: Springer; 1985. pp. 321–34. [Google Scholar]
- 7.Muktibodhananda S. Swara yoga: The Tantric Science of Brain Breathing. Munger: Bihar School of Yoga; 1999. [Google Scholar]
- 8.Tyagi A, Cohen M. Oxygen consumption changes with yoga practices: A systematic review. J Evid Based Complement Altern Med. 2013;18:290–308. [Google Scholar]
- 9.Wright J. A consideration of the vascular mechanism of the nasal mucous membrane and its relations to certain pathological processes. Am J Med Sci. 1895;109:516. [Google Scholar]
- 10.Lillie HI. Some practical considerations of the physiology of the upper respiratory tract. J Iowa Med Soc. 1923;13:403–8. [Google Scholar]
- 11.Heetderks DR. Observations of the reaction of normal nasal mucous membrane. [[Last accessed on 2024 Apr 13]];Am J Med Sci. 1927 174:231–44. Available from: https://eurekamag.com/research/025/129/025129614.php . [Google Scholar]
- 12.Eccles RB. The nasal cycle in respiratory defence. Acta Otorhinolaryngol Belg. 2000;54:281–6. [PubMed] [Google Scholar]
- 13.Gungor A, Moinuddin R, Nelson RH, Corey JP. Detection of the nasal cycle with acoustic rhinometry: Techniques and applications. Otolaryngol Head Neck Surg. 1999;120:238–47. doi: 10.1016/S0194-5998(99)70413-4. [DOI] [PubMed] [Google Scholar]
- 14.Chaya MS, Nagendra HR. Long-term effect of yogic practices on diurnal metabolic rates of healthy subjects. Int J Yoga. 2008;1:27–32. doi: 10.4103/0973-6131.36761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ray US, Pathak A, Tomer OS. Hatha yoga practices: Energy expenditure, respiratory changes and intensity of exercise. Evid Based Complement Alternat Med. 2011;2011:241294. doi: 10.1093/ecam/neq046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saoji AA, Raghavendra BR, Manjunath NK. Effects of yogic breath regulation: A narrative review of scientific evidence. J Ayurveda Integr Med. 2019;10:50–8. doi: 10.1016/j.jaim.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 18.Telles S, Nagarathna R, Nagendra HR. Physiological measures of right nostril breathing. J Altern Complement Med. 1996;2:479–84. doi: 10.1089/acm.1996.2.479. [DOI] [PubMed] [Google Scholar]
- 19.Özbay PS, Chang C, Picchioni D, Mandelkow H, Moehlman TM, Chappel-Farley MG, et al. Contribution of systemic vascular effects to fMRI activity in white matter. Neuroimage. 2018;176:541–9. doi: 10.1016/j.neuroimage.2018.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall JE. Pocket Companion to Guyton and Hall Textbook of Medical Physiology E- Book. Philadelphia, PA: Elsevier Health Sciences; 2015. [Google Scholar]
- 21.Frese EM, Fick A, Sadowsky HS. Blood pressure measurement guidelines for physical therapists. Cardiopulm Phys Ther J. 2011;22:5–12. [PMC free article] [PubMed] [Google Scholar]
- 22.Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 23.Ramdev S. Pranayama Rahasya with Scientific Factual Evidence. Revised ed. Haridwar, India: Divya Prakashan Divya Yog Mandir (Trust); 2009. p. 76. [Google Scholar]
- 24.Das TK, Jana H. Basal oxygen consumption during different phases of menstrual cycle. Indian J Med Res. 1991;94:16–9. [PubMed] [Google Scholar]
- 25.Telles S, Singh N, Balkrishna A. Heart rate variability changes during high frequency yoga breathing and breath awareness. Biopsychosoc Med. 2011;5:4. doi: 10.1186/1751-0759-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Telles S, Sharma SK, Balkrishna A. Blood pressure and heart rate variability during yoga-based alternate nostril breathing practice and breath awareness. Med Sci Monit Basic Res. 2014;20:184–93. doi: 10.12659/MSMBR.892063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Telles S, Singh N, Balkrishna A. Metabolic and ventilatory changes during and after high-frequency yoga breathing. Med Sci Monit Basic Res. 2015;21:161–71. doi: 10.12659/MSMBR.894945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parimbelli M, Pezzotti E, Negro M, Calanni L, Allemano S, Bernardi M, et al. Nutrition and exercise in a case of carnitine palmitoyl-transferase II deficiency. Front Physiol. 2021;12:637406. doi: 10.3389/fphys.2021.637406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Telles S, Bhardwaj AK, Gupta RK, Kumar A, Balkrishna A. Development of a food frequency questionnaire to assess dietary intake for the residents of the Northern region of India. Indian J Anc Med Yoga. 2016;9:139–47. [Google Scholar]
- 30.National Institute of Nutrition (NIN) Dietary Guidelines for Indians -A Manual. 2nd ed. Hyderabad, India: National Institute of Nutrition; 2011. p. 174. [Google Scholar]
- 31.Herrero JL, Khuvis S, Yeagle E, Cerf M, Mehta AD. Breathing above the brain stem: Volitional control and attentional modulation in humans. J Neurophysiol. 2018;119:145–59. doi: 10.1152/jn.00551.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heck DH, McAfee SS, Liu Y, Babajani-Feremi A, Rezaie R, Freeman WJ, et al. Breathing as a fundamental rhythm of brain function. Front Neural Circuits. 2016;10:115. doi: 10.3389/fncir.2016.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farb N, Daubenmier J, Price CJ, Gard T, Kerr C, Dunn BD, et al. Interoception, contemplative practice, and health. Front Psychol. 2015;6:763. doi: 10.3389/fpsyg.2015.00763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gibson J. Mindfulness, interoception, and the body: A contemporary perspective. Front Psychol. 2019;10:2012. doi: 10.3389/fpsyg.2019.02012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hepburn SJ, McMahon M. Pranayama meditation (yoga breathing) for stress relief: Is it beneficial for teachers? Aust J Teach Educ. 2017;42:142–59. [Google Scholar]
- 36.Jones AY, Dean E, Chow CC. Comparison of the oxygen cost of breathing exercises and spontaneous breathing in patients with stable chronic obstructive pulmonary disease. Phys Ther. 2003;83:424–31. [PubMed] [Google Scholar]
- 37.Smallwood CD, Walsh BK, Bechard LJ, Mehta NM. Carbon dioxide elimination and oxygen consumption in mechanically ventilated children. Respir Care. 2015;60:718–23. doi: 10.4187/respcare.03605. [DOI] [PubMed] [Google Scholar]
- 38.Muktibodhananda S. Hatha Yoga Pradipika: Light on Hatha Yoga. Munger, India: Yoga Publications Trust; 2002. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during analysis for the current study are available from the corresponding author on reasonable request.


