Abstract
A team of tribe-based behavioral health specialists and university-based researchers partnered to implement a cluster randomized trial for the prevention of drug misuse among adolescents attending public high schools on or near the Cherokee Nation Reservation in northeastern Oklahoma. The conceptual framework, which guided intervention and measurement design for the trial, incorporates indigenous knowledge and worldviews with empirically-based frameworks and evidence-based practices. Our goal is to serve multicultural youth, families, and schools and to provide a model of effective strategies for wide dissemination. This paper presents the conceptual model, survey design, and psychometric properties of scales to measure risk and protective factors for substance misuse. The survey includes common measures drawn from the PhenX Toolkit on substance use patterns—adolescent module, measured with standard items from the Monitoring the Future (MTF) study and items harmonized across ten NIH-funded research projects with diverse samples of youth. In our trial, brief (20-minute) self-report questionnaires were administered to 10th grade students in fall 2021 (n = 919, 87% response rate) and spring 2022 (n = 929, 89% response rate) in 20 participating high schools on or near the Cherokee Nation Reservation. The sample primarily fell into the following three categories of race/ethnicity identification: only American Indian (AI-only, 29%), AI and another race/ethnicity (AI+, 27%), and only White (35%). Results indicate that risk and protective factor scales were reliably and validly measured with 10 scales and 10 subscales. There were minimal differences between youth who identified as AI only, AI+, and White only, especially for the main scales, which provide confidence in the interpretation of trial outcomes across demographic groups. Study results may not be generalizable to AI/AN youth who live and attend school in more homogenous reservation lands, or alternatively, live in large diverse metropolitan areas.
Keywords: Risk factors, Protective factors, Measures, Psychometrics, Substance misuse, Adolescence, American Indian
The goal of this paper is to provide evidence of the reliability and validity of standard measures of substance misuse risk and protective factors for use with American Indian youth. The measures were designed to assess important risk and protective factors, as well as substance use and mental health outcomes, among a diverse sample of high school students living on or near the Cherokee Nation Reservation. A team of tribe-based behavioral health specialists and university-based researchers partnered to design and implement a cluster randomized trial for the prevention of substance misuse and promotion of mental health among adolescents. We have been collaborating and building our team’s partnership for over 10 years (Komro et al., 2017; Komro et al., 2015a), with some changes in team members over time (Komro et al., 2022b). Our collaboration has been built on mutual interests in optimal youth development and use of data to test effectiveness of efforts in the real world. Our values were aligned to support underserved youth and families directly with shared expertise and resources, as well as to contribute more broadly through dissemination of scientific findings.
Our trial was part of the Helping to End Addiction Long-Term (HEAL) Prevention Cooperative (HPC), a group of ten research projects and a coordinating center, funded by the National Institutes of Health and administered by the National Institute on Drug Abuse (Komro et al., 2022a; Ridenour et al., 2022). The HPC Coordinating Center at RTI International led efforts for core measure selection and harmonization across sites (Ridenour et al., 2022). Each research project developed a distinct intervention for specific populations and settings to prevent opioid misuse among older adolescents and young adults (Ridenour et al., 2022). In addition to our project in the Cherokee Nation, one additional project focused on American Indian/Alaska Native young adults (Komro et al., 2022b).
The goal of our trial was universal primary prevention of substance misuse and promotion of mental health among a cohort of high school students living on or near the Cherokee Nation Reservation in northeast Oklahoma (Komro et al., 2022a). We recruited 20 rural high schools and randomly assigned them to an intervention or delayed-intervention comparison condition. The Cherokee Nation Institutional Review Board (IRB) served as the IRB of record and approved the trial protocol, as well as each dissemination product. The intervention integrated family, school, and community strategies, based on our previous collaboration (Komro et al., 2017) and included (1) connect—a universal screening and brief motivational interviewing intervention within schools and (2) family action kits mailed directly to homes, with corresponding school and community dissemination.
In order to optimize cultural acceptability and intervention effectiveness, we relied on a collaborative approach between Cherokee Nation Behavioral Health specialists and prevention science expertise of university-based team members (Komro et al., 2022b). We designed a working conceptual model incorporating indigenous knowledge and worldviews with western frameworks and evidence-based practices. Our goal was to serve multicultural youth, families, and schools within and near the Cherokee Nation Reservation and to provide a model for community-based primary prevention for wide dissemination.
We first present our integrated conceptual framework, which guided intervention and measurement design. We then describe measures used to test the effectiveness of the intervention and an examination of how well the measures perform among a large sample of rural American Indian youth.
Conceptual Framework
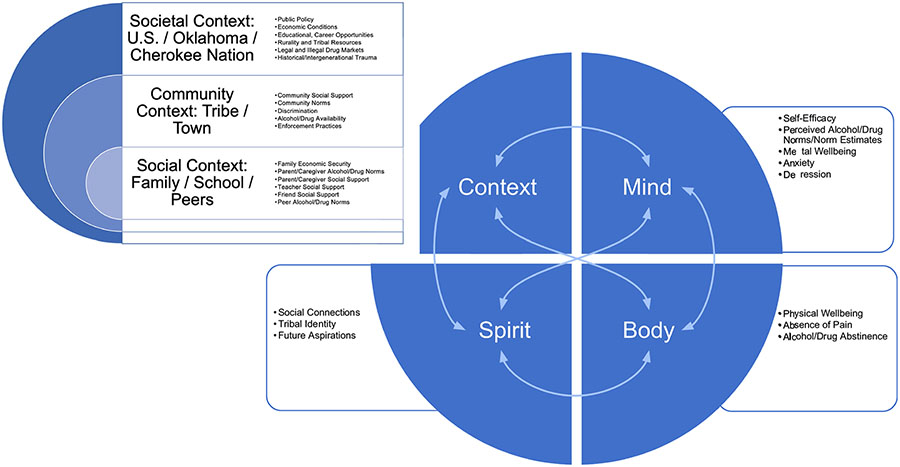
The conceptual framework guided selection of intervention objectives and measures and was based on merging socio-ecological and risk and protective frameworks (Hawkins et al., 1992; Keyes et al., 2014; Komro et al., 2016; Wagenaar & Perry, 1994) with an indigenous relational worldview perspective (Blackstock, 2019; Cross, 2007). The integrated conceptual framework is meant to highlight dynamic, multilevel, inter-relationships between contextual (i.e., societal, community, social) and intra- and inter-level (i.e., mind, body, spirit) factors that influence health and well-being as it relates to abstinence or initiation and escalation of substance misuse during adolescence into young adulthood.
Method
Participants
We recruited 20 rural high schools on or near the Cherokee Nation Reservation and randomly assigned them to an intervention or delayed-intervention comparison condition. In fall 2021, following Cherokee Nation IRB approved parent consent and student assent procedures, we enrolled and surveyed a cohort of 10th-grade students with the first follow-up survey conducted in spring 2022.
Measures
The survey was designed to measure risk and protective factors at the individual to community levels as depicted in the conceptual model. The survey included common measures that we have used in previous studies (Komro et al., 2015b) and drawn from the PhenX Toolkit on substance use patterns—adolescent module (module #510301), measured with standard items from the Monitoring the Future (MTF) study (https://monitoringthefuture.org). PhenX uses a consensus process and inputs from the scientific community to provide well-established, high-quality, low-burden measurement protocols (https://www.phenx.org/).
Primary outcome measures included frequency (number of days) during the past 30 days of any: (1) alcohol use, (2) heavy alcohol use (defined as having at least four, among young women and those not disclosing gender, or five, among young men, standard alcoholic drinks within a couple of hours), (3) marijuana use, and (4) prescription opioid misuse (defined as “without a doctor’s prescription or differently than how a doctor or medical provider told you to use it”).
Measures of substance misuse-related problems included pain, depression, and anxiety. Pain was measured with the 4-item PROMIS Pediatric Pain Interference Scale (Cunningham et al., 2017; Varni et al., 2010). Depression was measured with the 8-item Patient Health Questionnaire depression scale (PHQ-8), established as a valid measure of current depression in the general population (Kroenke et al., 2009). Anxiety was measured with the Generalized Anxiety Disorder 7-item scale (GAD-7), found to have acceptable specificity and sensitivity and to differentiate between mild and moderate GAD among adolescents (Mossman et al., 2017).
Key risk and protective factors (and hypothesized mediators for intervention effects) included social support, perceived availability of drugs, social normative disapproval beliefs, self-efficacy, perceptions of getting in trouble for use, and normative estimates. Social support from community members, parents/caregivers, teachers, and friends were adapted from the School Support Scale (Hanson & Kim, 2007) and assessed with 24 items which are responded to on a 4-point scale where 0 = never and 3 = often. Adapted from the PhenX MTF items, ease or difficulty in accessing alcohol, marijuana, and prescription opioids was assessed with 12 items using a 4-point scale where 0 = very difficult to get and 3 = very easy to get. Adapted from MTF, participants were asked 12 items to assess if they think various social groups disapprove of young people drinking alcohol, using marijuana, and prescription opioid misuse (parents, community adults, peers, self). Responses were 0 = do not disapprove, 1 = disapprove, and 2 = strongly disapprove. Self-efficacy was assessed with 4 items asking how easy or hard it would be for participants to ask for help or refuse alcohol or drugs (Choi et al., 2013; Komro et al., 2015b). Responses were a 4-point scale, where 0 = very easy and 3 = very hard. Adapted from MTF, perceptions of getting into trouble with caregivers, teachers, or police for substance use (alcohol, marijuana, prescription opioid misuse) was measured with three items with response options of 0 = very little chance, 1 = little chance, 2 = some chance, and 3 = very good chance. Adapted from the PhenX Communities That Care items (Arthur et al., 2007), normative estimates of peer drug use (alcohol, marijuana, prescription opioid misuse) were assessed with 3 items asking how many of their peers in school used drugs in the past year. Possible responses were 0 = none or almost none, 1 = less than half, 2 = about half, 3 = more than half, and 4 = almost all or all. Tribal identity was measured with adaptations of three items from the 6-item Multigroup Ethnic Identity Measure–Revised (MEIM-R) (Phinney, 1992). Students who self-identified as American Indian/Alaska Native were asked three questions on a 5-point scale from strongly disagree to strongly agree: (1) I have a strong sense of belonging to my tribe, (2) I understand pretty well what my tribal identity means to me, and (3) I feel a strong attachment towards my tribe.
Survey Procedure
Brief (20 minute) self-report questionnaires were administered to 10th-grade students in fall 2021 (wave 1) and spring 2022 (wave 2) in 20 participating high schools. The response rate was 87% with 919 completed surveys in the fall 2021 survey, and 89% with 929 completed surveys in spring 2022. Reasons for nonresponse in order of frequency included (1) nonresponse from remote (i.e., off-site) students, (2) parent refusals, (3) parent consent undeliverable, (4) student absences, (5) student refusals, and (6) alternative education or vocational/technology students who were unable to be surveyed in school.
Nearly half of the sample identified as female (48%), nearly half as male (48%), and 4% selected “decline to answer.” The mean age was 15.5 years in fall 2021. The study sample is primarily American Indian (AI) and White. For the race/ethnicity item, which instructs participants to select all that apply, 28.9% reported being only AI, 26.7% reported being AI and another race/ethnicity (AI+), 35.1% reported being only White, and 9.2% reported being another racial/ethnic category.
Psychometric Analysis
We assessed reliability and validity of 10 scales, and a further 10 associated subscales, measuring risk and protective factors associated with substance use among those students identifying as AI only, AI+, or White only (n = 834). Specifically, we evaluated factor structure, concurrent validity, and predictive validity of each scale. We further evaluated measurement invariance across three AI identity categories. Finally, we tested differences in validity estimates by each AI identity group. The tribal identity scale was not used in validity analyses due to a lack of available appropriate criterion measures but was retained for all analyses of factor structure and invariance.
Factor Structure
We assessed the fit of the hypothesized factor structure for each scale using confirmatory factor analyses (CFA) using wave 1 survey data. Each scale was assessed in separate CFA measurement models. For models containing multiple subscales (social support, perceived substance use norms, and perceived substance use access), both first and second order CFA models were evaluated. Models were identified by standardizing the latent factor. To account for the ordinal nature of our Likert indicators, all CFA models were estimated using diagonally weighted least squares with mean and variance corrections (WLSMV). Model fit was assessed by both an inspection of factor loadings and the use of fit statistics. Fit statistics used included the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). To account for the mean and variance corrections used in our WLSMV estimation, robust CFI and RMSEA statistics were used. CFI values greater than 0.90 indicate reasonably good model fit. RMSEA values less than or equal to 0.05 indicate close approximate fit; values between 0.05 and 0.08 suggest reasonable fit, and values greater than or equal to 0.10 suggest poor model fit. SRMR values of less than 0.08 indicate reasonable model fit. Notably, some of our single factor CFA models contain only three indicators which will lead our fit statistics to indicate perfect fit regardless of the underlying structure. For these models, factor loadings are still informative, and they are retained in all reported analyses for consistency with subsequent measurement invariance testing.
Measurement invariance testing was carried out using multi-group CFA models. We began by evaluating a simple model assuming configural invariance. Specifically, we estimated a model with the same underlying factor structure for all three identity groups, while allowing the factor loadings and indicator intercepts to freely vary across groups. When configural invariance was indicated, we then proceeded to test for weak invariance by holding the factor loadings equivalent across each of the three identity groups. When weak invariance was indicated, we then proceeded to test for strong invariance by holding both the factor loadings and intercepts equivalent across the identity groups. Strict invariance was not assessed due to guidance provided in both Little (2013) and Kline (2015) regarding the impact of random measurement error on residual error variance. To establish configural invariance, overall fit of the unrestricted multi-group CFA models were assessed similarly to the previously described single-group CFA models. For three item CFA models, configural variance is assumed given the lack of available degrees of freedom. To assess whether subsequent levels of invariance were met, we assessed changes in model fit with the additional group restrictions based on a change in the robust CFI statistic. A difference in the robust CFI statistic between the more restrictive and free models of less than 0.01 was considered adequate to establish invariance. All measurement invariance analyses were carried out using the “lavaan” package in R version 4.1.0.
Validity
Concurrent validity was estimated using the cross-sectional models at wave 1 of each scale with an applicable substance use outcome; predictive validity was estimated using each scale at wave 1 and the substance use outcome at wave 2. While no gold-standard is available in our data for the scales, we establish validity by estimating the relationship between the scales and a substance use criterion based on well-established behavioral theory, as presented in Fig. 1. To estimate validity, the majority of scales used an overall substance use criterion calculated by a participant indicating either past 30-day use of alcohol, marijuana, or opioids. For scales that were specific to a given substance, reports of past 30-day use of that specific substance were used as the criterion (e.g., marijuana use norms used past 30-day marijuana use for validity estimates). Odds ratios for the association between each scale and criterion were then estimated using mixed effects logistic regression models with a random intercept for study school. Wave 1 scales were standardized in each model to allow for easy comparisons for validity estimates across each scale.
Fig. 1.
Conceptual framework merging indigenous relational wordview and socio-ecological risk and protective factors for youth substance misuse
Differences in concurrent and predictive validity were estimated using mixed effects logistic regressions similar to validity estimates from the full sample. These models contained an interaction between the scale and AI identity group indicators. Odds ratios were then estimated for each identity group, and an F-test was used to test the statistical significance of the scale by AI identity group interaction. All models were estimated using “glmer” in R version 4.1.0.
Results
Substance Use Indices
Table 1 presents descriptive statistics for planned primary outcomes, scales for secondary outcomes, and scales for other substance use related problems. All descriptive results are presented at wave 1 for the full sample and by AI identity.
Table 1.
Baseline descriptive statistics for scales used for the overall sample and by AI identity
| Scale | Range | Overall mean (SD) (N = 834) |
White mean (SD) (N = 323) |
AI+ other mean (SD) (N = 245) |
AI only mean (SD) (N = 266) |
|---|---|---|---|---|---|
| Paina | 1–5 | 1.96 (0.99) | 1.95 (0.98) | 1.95 (0.99) | 1.97 (1.02) |
| Depression (PHQ-8) | 0–24 | 7.42 (6.02) | 7.14 (5.83) | 7.45 (5.91) | 7.73 (6.34) |
| Anxiety (GAD-7) | 0–21 | 6.68 (5.81) | 6.49 (5.68) | 6.75 (5.67) | 6.86 (6.10) |
| Social support—overalla | 1–4 | 3.36 (0.55) | 3.40 (0.53) | 3.35 (0.53) | 3.34 (0.58) |
| Parent/caregivera | 1–4 | 3.55 (0.57) | 3.59 (0.50) | 3.54 (0.54) | 3.52 (0.66) |
| Frienda | 1–4 | 3.40 (0.70) | 3.42 (0.70) | 3.40 (0.65) | 3.38 (0.74) |
| Teachera | 1–4 | 3.33 (0.76) | 3.34 (0.74) | 3.36 (0.73) | 3.30 (0.81) |
| Adult (community)a | 1–4 | 3.17 (0.94) | 3.24 (0.90) | 3.12 (0.94) | 3.14 (0.98) |
| Perceived substance use access—overalla | 1–4 | 1.76 (0.64) | 1.77 (0.64) | 1.82 (0.62) | 1.71 (0.65) |
| Alcohola | 1–4 | 2.01 (0.78) | 2.02 (0.79) | 2.06 (0.73) | 1.96 (0.81) |
| Marijuanaa | 1–4 | 1.87 (0.81) | 1.85 (0.81) | 1.92 (0.80) | 1.85 (0.82) |
| RX opioidsa | 1–4 | 1.41 (0.61) | 1.42 (0.60) | 1.47 (0.64) | 1.33 (0.61) |
| Normative disapproval beliefs—overalla | 1–3 | 2.28 (0.43) | 2.31 (0.40) | 2.27 (0.43) | 2.26 (0.46) |
| Alcohola | 1–3 | 2.14 (0.51) | 2.16 (0.48) | 2.11 (0.51) | 2.13 (0.54) |
| Marijuanaa | 1–3 | 2.19 (0.55) | 2.23 (0.52) | 2.17 (0.56) | 2.15 (0.56) |
| RX opioidsa | 1–3 | 2.53 (0.44) | 2.55 (0.40) | 2.54 (0.45) | 2.50 (0.49) |
| Self-efficacy to refuse alcohol and drugsa | 1–4 | 3.45 (0.74) | 3.49 (0.74) | 3.48 (0.66) | 3.37 (0.82) |
| Perception of getting in trouble for alcohol and drug usea | 1–4 | 3.50 (0.76) | 3.53 (0.72) | 3.53 (0.70) | 3.44 (0.85) |
| Normative estimates of peer alcohol and drug usea | 1–5 | 2.42 (0.85) | 2.44 (0.85) | 2.47 (0.85) | 2.34 (0.84) |
| Tribal identityab | 1–5 | 3.04 (0.99) | 3.33 (1.14) |
PHQ-8 Patient Health Questionnaire depression scale-8, GAD-7 Generalized Anxiety Disorder Scale-7, RX prescription
Scale coded as the mean of constituent Likert items
Only asked to those reporting as AI (American Indian) or AI+ other
Factor Structure
Confirmatory factor analysis was conducted to assess factor loadings, model fit indices, and overall reliability of each scale and subscale. Factor loadings and fit statistics for first order models can be found in Table 2. For scales measuring overall social support, perceived substance use access, and normative disapproval beliefs, no first order model was found to fit well. A second order CFA model was found to fit overall social support well (robust CFI = 0.996, robust RMSEA = 0.021, SRMR = 0.037), but not for perceived substance use access or normative disapproval beliefs. As a result, scales for overall perceived substance use access and normative disapproval beliefs were abandoned in favor of their substance-specific subscales in all remaining analyses.
Table 2.
Confirmatory Factor Analysis (CFA)
| Scale | Factor loadings | Robust CFI | Robust RMSEA | Robust SRMR |
|---|---|---|---|---|
| Pain | 0.999 | 0.046 | 0.027 | |
| Trouble sleeping | 0.806 | |||
| Felt sad | 0.767 | |||
| Hard to pay attention | 0.859 | |||
| Hard to stay standing | 0.694 | |||
| Depression (PHQ-8) | 0.994 | 0.041 | 0.039 | |
| Little interest or pleasure in doing things | 0.684 | |||
| Feeling down, depressed, or hopeless | 0.786 | |||
| Trouble falling or staying asleep, or sleeping too much | 0.703 | |||
| Feeling tired or having little energy | 0.755 | |||
| Poor appetite or overeating | 0.677 | |||
| Feeling bad about yourself | 0.717 | |||
| Trouble concentrating on things | 0.648 | |||
| Moving or speaking so slowly/being so fidgety or restless | 0.645 | |||
| Anxiety (GAD-7) | 0.997 | 0.034 | 0.030 | |
| Feeling nervous, anxious or on edge | 0.816 | |||
| Not being able to stop or control worrying | 0.864 | |||
| Worrying too much about different things | 0.857 | |||
| Trouble relaxing | 0.821 | |||
| Being so restless that it is hard to sit still | 0.624 | |||
| Becoming easily annoyed or irritable | 0.655 | |||
| Feeling afraid as if something awful might happen | 0.751 | |||
| Parent/caregiver support | 0.991 | 0.039 | 0.054 | |
| Really cares about me | 0.680 | |||
| Tells me when I do a good job | 0.801 | |||
| Notices when I am not there | 0.648 | |||
| Always wants me to do my best | 0.658 | |||
| Listens to me when I have something to say | 0.792 | |||
| Believes that I will be a success | 0.783 | |||
| Teacher support | 1.000 | 0.012 | 0.017 | |
| Really cares about me | 0.864 | |||
| Tells me when I do a good job | 0.830 | |||
| Notices when I am not there | 0.766 | |||
| Always wants me to do my best | 0.830 | |||
| Listens to me when I have something to say | 0.808 | |||
| Believes that I will be a success | 0.869 | |||
| Friend support | 1.000 | 0.004 | 0.012 | |
| Really cares about me | 0.786 | |||
| Tells me when I do a good job | 0.779 | |||
| Notices when I am not there | 0.772 | |||
| Always wants me to do my best | 0.846 | |||
| Listens to me when I have something to say | 0.772 | |||
| Believes that I will be a success | 0.844 | |||
| Adult (community) support | 1.000 | 0.013 | 0.013 | |
| Really cares about me | 0.902 | |||
| Tells me when I do a good job | 0.901 | |||
| Notices when I am not there | 0.876 | |||
| Always wants me to do my best | 0.932 | |||
| Listens to me when I have something to say | 0.901 | |||
| Believes that I will be a success | 0.924 | |||
| Perceived alcohol access | 0.996 | 0.047 | 0.027 | |
| From the place where you live | 0.547 | |||
| From a store | 0.569 | |||
| From someone your age | 0.724 | |||
| From an older friend or another adult | 0.794 | |||
| Perceived marijuana access | 0.993 | 0.065 | 0.050 | |
| From the place where you live | 0.515 | |||
| From a dispensary without a doctor’s RX | 0.523 | |||
| From a dealer | 0.797 | |||
| From someone your age | 0.827 | |||
| From an older friend or another adult | 0.807 | |||
| Perceived RX opioid access | 0.996 | 0.041 | 0.049 | |
| From the place where you live | 0.545 | |||
| From a dispensary without a doctor’s RX | 0.595 | |||
| From a dealer | 0.791 | |||
| From someone your age | 0.862 | |||
| From an older friend or another adult | 0.837 | |||
| Alcohol normative disapproval beliefs | 0.989 | 0.068 | 0.031 | |
| Self | 0.671 | |||
| People your age | 0.489 | |||
| Adults | 0.630 | |||
| Parent(s)/caregiver(s) | 0.666 | |||
| Marijuana normative disapproval beliefs | 0.984 | 0.091 | 0.041 | |
| Self | 0.770 | |||
| People your age | 0.497 | |||
| Adults | 0.620 | |||
| Parent(s)/caregiver(s) | 0.679 | |||
| RX opioid normative disapproval beliefs | 0.988 | 0.065 | 0.041 | |
| Self | 0.652 | |||
| People your age | 0.463 | |||
| Adults | 0.747 | |||
| Parent(s)/caregiver(s) | 0.663 | |||
| Self-efficacy to refuse alcohol and drugs | 1.000 | 0.000 | 0.000 | |
| When you are feeling down | 0.759 | |||
| When you are celebrating or at a party | 0.960 | |||
| When offered by a friend | 0.705 | |||
| Perception of getting in trouble for alcohol and drug use | 1.000 | 0.000 | 0.000 | |
| Alcohol | 0.768 | |||
| Marijuana | 0.843 | |||
| RX opioid | 0.733 | |||
| Normative estimates of peer alcohol and drug use | 1.000 | 0.000 | 0.000 | |
| Alcohol | 0.771 | |||
| Marijuana | 0.810 | |||
| RX opioid | 0.539 | |||
| Tribal identity | 1.000 | 0.000 | 0.000 | |
| Strong sense of belonging to my tribe | 0.909 | |||
| Understand pretty well what my tribal identity means to me | 0.897 | |||
| Feel a strong attachment towards my tribe | 0.930 |
CFI comparative fit index, RMSEA root mean square error of approximation, SRMR standardized root mean square residual, GAD-7 Generalized Anxiety Disorder Scale-7, PHQ-8 Patient Health Questionnaire depression scale-8, RX prescription
Across the remaining first order CFA models for scales and subscales, there was a consistent pattern of well-fitting models (Table 2). With factor loadings ranging from 0.694 to 0.859, the pain scale items demonstrated strong associations with the latent construct. This suggests that each item effectively measures the concept of pain, contributing to the overall reliability of the scale. The model demonstrated an excellent fit to the data, as evidenced by a robust CFI of 0.99, a robust RMSEA of 0.046, and a robust SRMR of 0.027. The PHQ-8 and GAD-7 both had strong model fit statistics lending support for their use as measures of depressive symptoms and anxiety symptoms among this population. Factor loadings for the PHQ-8 and GAD-7 ranged from 0.645 to 0.786 and 0.624 to 0.864, respectively, with robust CFIs greater than 0.99 and robust RMSEA and robust SRMR values indicating close approximate fit on both scales. Scales measuring source specific social support from parents/caregivers, teachers, friends, and other adults in the community were tested using CFA on the subscale for each source. Results showed strong factor loadings ranging from 0.648 to 0.932 across subscales, with robust CFIs all greater than 0.99. All robust RMSEA values were below the cutoff for close approximate fit, and robust SRMRs reflect reasonable model fit across social support subscales. Similarly, scales measuring perceived access to alcohol, marijuana, and prescription opioids also had factor loadings and model fit statistics that lend support for their use as measures of the desired latent constructs among these youth. Factor loadings for alcohol access, marijuana access, and prescription opioid access were all high, ranging from 0.547 to 0.794, 0.515 to 0.827, and 0.545 to 0.862, respectively. Robust CFIs were greater than 0.99 for all three perceived access scales, reflecting excellent fit. Robust RMSEAs indicate close approximate fit with values less than 0.05 for alcohol and prescription opioid access and reasonable fit for marijuana access at 0.065. Robust SRMRs were similarly low (0.027–0.05). Items on the normative disapproval beliefs scales for alcohol, marijuana, and prescription opioids had generally strong factor loadings (alcohol: 0.489–0.671; marijuana: 0.497–0.770; prescription opioids: 0.463–0.747) and CFA model fit statistics. Robust CFIs across substance-specific scales were all greater than 0.98, robust SRMRs less than 0.05, and robust RMSEAs within (or close to, see marijuana robust RMSEA of 0.091) range for reasonable fit. The remaining scales (self-efficacy to refuse, perception of getting in trouble, normative estimates of peer use, and tribal identity) had strong factor loadings, but model fit could not be assessed given that these models were just identified.
Formal invariance testing was carried out for all scales and subscales with the exception of overall social support, overall perceived substance use access, and normative disapproval beliefs. Measurement invariance for overall social support was not assessed due to lack of convergence in the 2nd order configural model. Measurement invariance was not assessed for overall perceived substance use access and normative disapproval beliefs due to lack of a well-fitting model in the full sample. All remaining scales were found to be strongly invariant based on the criterion that the change in robust CFI across more restrictive models did not exceed 0.01 (Table 3). Additionally, all fit statistics for weak and strong invariance models indicated good fit with all robust CFIs in excess of 0.95, robust RMSEAs below 0.08, and all SRMRs below 0.08 (Appendix 1).
Table 3.
Measurement invariance
| Scale | Configural invariance CFI |
Weak invariance CFI |
Strong invariance CFI |
Delta CFI weak invariance |
Delta CFI strong invariance |
|
|---|---|---|---|---|---|---|
| Pain | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Depression (PHQ-8) | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Anxiety (GAD-7) | 0.997 | 0.997 | 0.997 | 0.000 | 0.000 | |
| Social support—overall | a | a | a | a | a | |
| Parent/caregiver support | 0.990 | 0.977 | 0.971 | 0.013 | 0.006 | |
| Friend support | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Teacher support | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Adult (community) support | 0.999 | 0.999 | 0.999 | 0.000 | 0.000 | |
| Perceived substance use access—overall | b | b | b | b | b | |
| Perceived alcohol access | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Perceived marijuana access | 0.995 | 0.997 | 0.999 | −0.002 | −0.002 | |
| Perceived RX opioid access | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Normative disapproval beliefs—overall | b | b | b | b | b | |
| Alcohol normative disapproval beliefs | 0.994 | 0.997 | 0.992 | −0.003 | 0.005 | |
| Marijuana normative disapproval beliefs | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| RX opioid normative disapproval beliefs | 0.994 | 0.999 | 1.000 | −0.005 | −0.001 | |
| Self-efficacy to refuse alcohol and drugs | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Perception of getting in trouble for alcohol and drug use | 1.000 | 1.000 | 1.000 | 0.000 | 0.000 | |
| Normative estimates of peer alcohol and drug use | 1.000 | 0.999 | 0.999 | 0.001 | 0.000 | |
| Tribal identity | 1.000 | 0.999 | 0.999 | 0.001 | 0.000 |
Invariance not assessed due to lack of convergence in configural invariance model
invariance not assessed due to poor model fit in the full sample
CFI comparative fit index, PHQ-8 Patient Health Questionnaire depression scale-8, GAD-7 Generalized Anxiety Disorder Scale-7, RX prescription
Validity
Concurrent Validity
Table 4 presents overall and by group concurrent validity estimates for each scale using cross-sectional models at wave 1 Overall, every standard deviation increase in pain, depression, and anxiety scales was associated with 1.35, 1.55, and 1.38 times the odds of overall substance use. Additionally, every standard deviation increase in overall perceived substance use access was associated with 2.3 times the odds of overall substance use. Similar results were found for all three substance-specific subscales with the highest odds with marijuana use (3.41). Also, every standard deviation increase in normative estimates of peer alcohol and drug use was associated with 1.92 times the odds of overall substance use. Conversely, every standard deviation increase in overall social support was associated with 0.68 times the odds of overall substance use. Similar results were found in all three subscales of social support with the lowest odds of overall substance use with parent/caregiver support (0.63). Similarly, every standard deviation increase in overall normative disapproval beliefs was associated with 0.44 times the odds of overall substance use. Similar results were found for all three substance-specific subscales with the lowest odds with marijuana use (0.28). Finally, every standard deviation increase in self-efficacy to refuse alcohol and drugs and the perception of getting in trouble for substance use was associated with 0.43 and 0.52 times the odds of overall substance use.
Table 4.
Overall and by AI identity group concurrent validity estimates for each scale at wave 1
| Scale | Overall criterion OR (95%) | Criterion OR (95%)— White |
Criterion OR (95%)— AI+O |
Criterion OR (95%)—AI only |
p-values |
|---|---|---|---|---|---|
| Pain | 1.35 (1.16, 1.57) | 1.29 (1.00, 1.67) | 1.23 (0.94, 1.62) | 1.55 (1.19, 2.02) | 0.456 |
| Depression (PHQ-8) | 1.55 (1.32, 1.81) | 1.47 (1.13, 1.92) | 1.48 (1.11, 1.97) | 1.67 (1.28, 2.18) | 0.768 |
| Anxiety (GAD-7) | 1.38 (1.19, 1.61) | 1.26 (0.97, 1.63) | 1.39 (1.05, 1.85) | 1.51 (1.16, 1.96) | 0.635 |
| Social support—overall | 0.68 (0.58, 0.79) | a | a | a | |
| Parent/caregiver | 0.63 (0.54, 0.73) | 0.49 (0.37, 0.66) | 0.67 (0.50, 0.88) | 0.71 (0.57, 0.89) | 0.146 |
| Friend | 0.94 (0.81, 1.09) | 0.90 (0.70, 1.15) | 0.93 (0.69, 1.25) | 1.00 (0.77, 1.29) | 0.846 |
| Teacher | 0.73 (0.63, 0.84) | 0.57 (0.44, 0.74) | 0.88 (0.66, 1.17) | 0.78 (0.61, 1.00) | 0.068 |
| Adult (community) | 0.77 (0.66, 0.89) | 0.60 (0.46, 0.78) | 0.98 (0.74, 1.30) | 0.80 (0.62, 1.03) | 0.037 |
| Perceived substance use access—overall | b | b | b | b | |
| Alcohol | 2.30 (1.89, 2.80) | 2.19 (1.58, 3.02) | 2.66 (1.82, 3.89) | 2.18 (1.58, 3.02) | 0.678 |
| Marijuana | 3.41 (2.68, 4.34) | 3.52 (2.32, 5.34) | 4.46 (2.75, 7.24) | 2.75 (1.90, 3.98) | 0.284 |
| RX opioids | 2.34 (1.78, 3.09) | 1.96 (1.17, 3.29) | 2.58 (1.50, 4.42) | 2.48 (1.62, 3.78) | 0.728 |
| Normative disapproval beliefs—overall | b | b | b | b | |
| Alcohol | 0.40 (0.32, 0.49) | 0.49 (0.34, 0.70) | 0.28 (0.18, 0.42) | 0.45 (0.32, 0.63) | 0.095 |
| Marijuana | 0.28 (0.22, 0.36) | 0.24 (0.15, 0.38) | 0.23 (0.14, 0.37) | 0.37 (0.25, 0.55) | 0.200 |
| RX opioids | 0.54 (0.40, 0.73) | 0.47 (0.26, 0.86) | 0.66 (0.38, 1.16) | 0.52 (0.33, 0.81) | 0.699 |
| Self-efficacy to refuse alcohol and drugs | 0.43 (0.36, 0.50) | 0.45 (0.34, 0.58) | 0.23 (0.15, 0.35) | 0.54 (0.42, 0.69) | 0.003 |
| Perception of getting in trouble for alcohol and drug use | 0.52 (0.45, 0.61) | 0.52 (0.40, 0.67) | 0.46 (0.33, 0.64) | 0.56 (0.44, 0.71) | 0.655 |
| Normative estimates of peer alcohol and drug use | 1.92 (1.61, 2.28) | 1.77 (1.33, 2.36) | 2.20 (1.59, 3.04) | 1.86 (1.37, 2.53) | 0.604 |
Group specific ORs were not estimated due to lack of confirmation of scale invariance
overall and group specific ORs not estimated due to poor model fit in the overall sample
p-values in bold: < 0.05
PHQ-8 Patient Health Questionnaire depression scale-8, GAD-7 Generalized Anxiety Disorder Scale-7, RX prescription
Concurrent validity differed significantly based on the F-test by identity groups in one scale and one subscale. The association between self-efficacy to refuse alcohol and drugs and overall substance use differed significantly between identity groups (p < 0.05) where AI+ youth had the lowest odds (0.23) of overall substance use with every standard deviation increase in the self-efficacy to refuse alcohol and drugs scale. The association between adult support and overall substance use also differed significantly between identity groups (p < 0.05) where White youth had the lowest odds (0.60) of overall substance use with every standard deviation increase in adult support.
Predictive Validity
Table 5 presents overall and by group predictive validity estimates using each scale at wave 1 and the substance use outcome at wave 2. Predictive validity estimates reflect similar associations in the same direction as observed for concurrent validity. Overall, every standard deviation increase in pain, depression, and anxiety scales at wave 1 was associated with 1.41, 1.74, and 1.61 times the odds of overall substance use, i.e., either past 30-day use of alcohol, marijuana, or opioids at wave 2. Additionally, every standard deviation increase in overall perceived substance use access at wave 1 was associated with 1.97 times the odds of overall substance use at wave 2. Similar results were found for all 3 substance-specific subscales with the highest odds with marijuana use (2.52). Also, every standard deviation increase in normative estimates of peer alcohol and drug use at wave 1 was associated with 1.50 times the odds of overall substance use at wave 2. Conversely, every standard deviation increase in overall social support at wave 1 was associated with 0.61 times the odds of overall substance use at wave 2 Similar results were found in all 3 subscales of social support with the lowest odds of overall substance use with parent/caregiver support (0.64). Similarly, every standard deviation increase in overall normative disapproval beliefs at wave 1 was associated with 0.54 times the odds of overall substance use at wave 2. Similar results were found for all three substance-specific subscales with the lowest odds with marijuana use (0.29). Finally, every standard deviation increase in self-efficacy to refuse alcohol and drugs and the perception of getting in trouble for substance use at wave 1 was associated with 0.54 and 0.59 times the odds of overall substance use at wave 2.
Table 5.
Overall and by AI identity group predictive validity estimates using each scale at wave 1 and substance use outcomes at wave 2
| Scale | Overall criterion estimate | Criterion estimate— White |
Criterion estimate— AI+O |
Criterion estimate—AI only |
p-values |
|---|---|---|---|---|---|
| Pain | 1.41 (1.19, 1.67) | 1.47 (1.10, 1.95) | 1.36 (1.02, 1.83) | 1.40 (1.04, 1.88) | 0.937 |
| Depression (PHQ-8) | 1.74 (1.46, 2.07) | 1.87 (1.38, 2.52) | 1.74 (1.25, 2.42) | 1.62 (1.22, 2.16) | 0.805 |
| Anxiety (GAD-7) | 1.61 (1.36, 1.90) | 1.56 (1.18, 2.07) | 1.60 (1.17, 2.19) | 1.66 (1.25, 2.21) | 0.955 |
| Social support—overall | 0.61 (0.51, 0.72) | a | a | a | |
| Parent/caregiver | 0.64 (0.54, 0.75) | 0.62 (0.45, 0.84) | 0.60 (0.43, 0.82) | 0.69 (0.54, 0.88) | 0.738 |
| Friend | 0.81 (0.69, 0.96) | 0.92 (0.70, 1.22) | 0.77 (0.56, 1.06) | 0.74 (0.56, 0.97) | 0.501 |
| Teacher | 0.66 (0.56, 0.78) | 0.57 (0.43, 0.76) | 0.68 (0.50, 0.94) | 0.74 (0.56, 0.97) | 0.445 |
| Adult (community) | 0.75 (0.63, 0.88) | 0.81 (0.61, 1.07) | 0.74 (0.55, 0.99) | 0.71 (0.54, 0.93) | 0.795 |
| Perceived substance use access—overall | b | b | b | b | |
| Alcohol | 2.02 (1.63, 2.51) | 2.24 (1.55, 3.23) | 2.20 (1.46, 3.31) | 1.75 (1.24, 2.46) | 0.566 |
| Marijuana | 2.52 (2.02, 3.15) | 1.97 (1.39, 2.80) | 4.21 (2.47, 7.19) | 2.53 (1.77, 3.62) | 0.066 |
| RX opioids | 1.20 (0.79, 1.83) | 1.94 (0.84, 4.46) | 1.10 (0.58, 2.08) | 0.80 (0.26, 2.42) | 0.398 |
| Normative disapproval beliefs—overall | b | b | b | b | |
| Alcohol | 0.62 (0.50, 0.77) | 0.74 (0.51, 1.07) | 0.56 (0.38, 0.82) | 0.58 (0.41, 0.83) | 0.518 |
| Marijuana | 0.29 (0.23, 0.38) | 0.39 (0.26, 0.58) | 0.16 (0.09, 0.30) | 0.31 (0.21, 0.47) | 0.069 |
| RX opioids | 0.84 (0.54, 1.32) | 0.93 (0.36, 2.39) | 0.62 (0.31, 1.24) | 1.08 (0.47, 2.47) | 0.580 |
| Self-efficacy to refuse alcohol and drugs | 0.54 (0.45, 0.64) | 0.60 (0.45, 0.79) | 0.34 (0.23, 0.51) | 0.62 (0.48, 0.81) | 0.034 |
| Perception of getting in trouble for alcohol and drug use | 0.59 (0.50, 0.70) | 0.65 (0.50, 0.86) | 0.54 (0.39, 0.75) | 0.57 (0.43, 0.74) | 0.643 |
| Normative estimates of peer alcohol and drug use | 1.50 (1.26, 1.80) | 1.18 (0.88, 1.59) | 1.63 (1.17, 2.27) | 1.86 (1.35, 2.57) | 0.102 |
Group specific ORs were not estimated due to lack of confirmation of scale invariance
overall and group specific ORs not estimated due to poor model fit in the overall sample
p-values in bold: < 0.05
PHQ-8 Patient Health Questionnaire depression scale-8, GAD-7 Generalized Anxiety Disorder Scale-7, RX prescription
Predictive validity differed significantly based on the F-test by identity groups in only one scale. The association between self-efficacy to refuse alcohol and drugs at wave 1 and overall substance use at wave 2 differed significantly between identity groups (p < 0.05) where AI+ youth had the lowest odds (0.34) of overall substance use at wave 2 with every standard deviation increase in self-efficacy to refuse alcohol and drugs at wave 1.
Discussion
The multi-item scales to measure risk and protective factors targeted by our multilevel preventive intervention performed well among AI and White youth attending high schools on or near the Cherokee Nation Reservation. Factor analyses in the overall sample demonstrated adequate model fit across almost all scales, and item loadings indicated that our measured items reasonably measure the proposed constructs. Results from the overall sample support the use of these scales in planned intervention evaluation analyses for the parent trial. Notably, these scales exhibited remarkable measurement invariance across AI identity groups in our sample, supporting their use in comparing potential intervention effects by AI status.
Concurrent and predictive validity was also evident for each scale based on correspondence between our criterion results and those predicted by our theoretical framework. For criterion validity, all but one of our scales and subscales were significantly associated with substance use in the theoretically aligned direction as risk or protective factors. Social support from friends was not associated with reductions in substance use and may indicate heterogeneous effects based on peer substance use norms. Two of our scales exhibited differential concurrent validity across AI identity groups. Adult social support was protective for White youth, but not AI only and AI+ groups. While self-efficacy to refuse alcohol and drugs was strongly associated with reductions in substance use for all groups, this association was stronger among AI+ youth. Similarly, the majority of predictive validity estimates were significant and in the theorized direction. Notably, the associations between both perceived access to prescription opioids and normative disapproval beliefs for prescription opioids with our opioid use criterion were attenuated in predictive validity models and no longer statistically significant. Only self-efficacy to refuse drugs and alcohol exhibited differential predictive validity across AI identity groups, with patterns similar to those observed in concurrent validity models.
Overall, all our scales performed well for the full sample and for the three subgroups defined by identity, providing support for their use in measuring changes in risk and protective factors over time and for measurement of effectiveness of the multilevel preventive intervention.
Limitations and Future Directions
The results of this study may not generalize outside the context of the ongoing trial due to the uniqueness of this study’s sample of AI youth. With forced removal of Cherokee people from their once vast ancestral lands in what is now the southeastern US, to Indian country, in what is now the State of Oklahoma, jurisdictional boundaries of the Cherokee Nation were set. However, when Oklahoma became a state in 1907, the tribe’s land was allotted to individual land owners, with much of the land quickly acquired by non-Indians (for additional historical details, see https://www.cherokee.org/about-the-nation/history/). Consequently, the land within the 14-county jurisdictional boundaries of the Cherokee Nation Reservation is primarily owned by non-Indians with the geographic area being racially mixed but majority White, as is evident by the demographic characteristics of the study sample. Therefore, our study results may not be generalizable to AI/AN youth who live and attend school in more homogenous reservation lands, or alternatively, live in large diverse metropolitan areas. In future research with either more homogenous or diverse samples, there may be a need to adapt measures.
Despite limitations, results provide confidence in the use of this brief survey instrument to reliably and validly measure targeted risk and protective factors and for outcome assessments of preventive interventions. The comprehensive survey was completed within 20 minutes, with approximately 30 minutes of class time used for complete survey administration. The survey included core measures of substance use, pain, depression, and anxiety that were harmonized across ten research projects as part of the HEAL prevention initiative, which will facilitate even greater understanding of developmental trajectories and intervention effectiveness across various distinct populations of adolescents and young adults.
Conclusion
Our conceptual framework, which guided selection of intervention objectives and measures, merged socio-ecological and risk and protective frameworks (Hawkins et al., 1992; Keyes et al., 2014; Komro et al., 2016; Wagenaar & Perry, 1994) with an indigenous relational worldview perspective (Blackstock, 2019; Cross, 2007). The majority of targeted risk and protective factors were deemed reliably and validly measured across our 10 scales and 10 subscales included in a brief 20-minute survey. While measures of perceived substance use access and normative disapproval beliefs aggregated across alcohol, marijuana, and prescription opioid misuse were not able to be validated, substance-specific subscale performed well. Factor analysis demonstrated strong invariance of validated scale across youth who identified as AI-only, AI and another race/ethnicity, and White-only providing confidence in the use of these scales across demographic groups. Observed differences in criterion and predictive validity of each scale were also minimal across race/ethnicity further reinforcing the use of these scales in our heterogeneous study population.
Supplementary Material
Acknowledgements
We acknowledge the trust and partnership of school districts, community members, and study participants to engage with us in this trial. Research reported in this publication was supported by the National Institute On Drug Abuse (NIDA) of the National Institutes of Health (NIH) through the NIH HEAL Initiative under Award Numbers UG3DA050234 and UH3DA050234. This research was also funded in part by NIDA Award Number T32DA050552. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, its NIH HEAL Initiative, or NIDA. The award was issued as a cooperative agreement in which NIH scientific involvement is anticipated in the performance of the trial. The funding sources played no role in the study design, data analysis, and writing of the manuscript.
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s42844-023-00112-1.
Ethics Approval and Consent to Participate This project was approved by the Cherokee Nation Institutional Review Board (US Federal Wide Assurance #0000047). Emory University and Cherokee Nation signed a reliance agreement, which designated Cherokee Nation as the organization providing IRB review.
Consent for Publication The Cherokee Nation IRB reviewed and approved this manuscript for publication. A model consent form is available on request.
Competing Interests The authors declare no competing interests.
Data Availability
Underlying primary data will be made available to outside individuals via written request to the Emory University PIs (Livingston and Komro) and with approval of a data sharing agreement with the Cherokee Nation.
References
- Arthur MW, Briney JS, David Hawkins J, Abbott RD, Brooke-Weiss BL, & Catalano RF (2007). Measuring risk and protection in communities using the Communities That Care Youth Survey. In Evaluation and Program Planning 30, 2 197–211. 10.1016/j.evalprogplan.2007.01.009 [DOI] [PubMed] [Google Scholar]
- Blackstock C. (2019). Revisiting the breath of life theory. British Journal of Social Work, 49(4), 854–859. [Google Scholar]
- Choi HJ, Krieger JL, & Hecht ML (2013). Reconceptualizing efficacy in substance use prevention research: Refusal response efficacy and drug resistance self-efficacy in adolescent substance use. Health Communication, 28(1), 40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross T. (2007). Through indigenous eyes: Rethinking theory and practice. Presented at National Aboriginal and Islander Child Care (SNAICC) National Conference September 20, 2007. https://www.snaicc.org.au/through-indigenous-eyes-rethinking-theory-and-practice-keynote-address-2007-cross-t-snaicc-conf-2007-2/ [Google Scholar]
- Cunningham NR, Kashikar-Zuck S, Mara C, Goldschneider KR, Revicki DA, Dampier C, Sherry DD, Crosby L, Carle A, Cook KF, & Morgan EM (2017). Development and validation of the self-reported PROMIS pediatric pain behavior item bank and short form scale. Pain, 158(7), 1323–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson TL, & Kim J-O (2007). Measuring resilience and youth development: The psychometric properties of the Healthy Kids Survey Issues & Answers Report, REL. https://ies.ed.gov/ncee/edlabs/regions/west/pdf/REL_2007034_body.pdf [Google Scholar]
- Hawkins JD, Catalano RF, & Miller JY (1992). Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin, 112(1), 64–105. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Cerdá M, Brady JE, Havens JR, & Galea S (2014). Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, D’Amico EJ, Dickerson DL, Skinner JR, Johnson CL, Kominsky TK, & Etz K (2022a). Culturally Responsive Opioid and Other Drug Prevention for American Indian/Alaska Native People: a Comparison of Reservation- and Urban-Based Approaches. Prevention Science: The Official Journal of the Society for Prevention Research. 10.1007/s11121-022-01396-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, Kominsky TK, Skinner JR, Livingston MD, Livingston BJ, Avance K, Lincoln AN, Barry CM, Walker AL, Pettigrew DW, Merlo LJ, Cooper HLF, & Wagenaar AC (2022b). Study protocol for a cluster randomized trial of a school, family, and community intervention for preventing drug misuse among older adolescents in the Cherokee Nation. Trials, 23(1), 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, Livingston MD, Garrett BA, & Boyd ML (2016). Similarities in the Etiology of Alcohol Use Among Native American and Non-Native Young Women. Journal of Studies on Alcohol and Drugs, 77(5), 782–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, Livingston MD, Kominsky TK, Livingston BJ, Garrett BA, Molina MM, & Boyd ML (2015a). Fifteen-Minute Comprehensive Alcohol Risk Survey: Reliability and Validity Across American Indian and White Adolescents. In Journal of Studies on Alcohol and Drugs 76(1):133–142. 10.15288/jsad.2015.76.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, Livingston MD, Wagenaar AC, Kominsky TK, Pettigrew DW, Garrett BA, & Cherokee Nation Prevention Trial Team. (2017). Multilevel Prevention Trial of Alcohol Use Among American Indian and White High School Students in the Cherokee Nation. American Journal of Public Health, 107(3), 453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro KA, Wagenaar AC, Boyd M, Boyd BJ, Kominsky T, Pettigrew D, Tobler AL, Lynne-Landsman SD, Livingston MD, Livingston B, & Molina MMM (2015b). Prevention trial in the Cherokee Nation: design of a randomized community trial. Prevention Science: The Official Journal of the Society for Prevention Research, 16(2), 291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling. Guildford Press. [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1-3), 163–173. [DOI] [PubMed] [Google Scholar]
- Little TD (2013). Longitudinal structural equation modeling. New York, NY: Guilford Press. [Google Scholar]
- Mossman SA, Luft MJ, Schroeder HK, Varney ST, Fleck DE, Barzman DH, Gilman R, DelBello MP, & Strawn JR (2017). The Generalized Anxiety Disorder 7-item scale in adolescents with generalized anxiety disorder: Signal detection and validation. Annals of Clinical Psychiatry: Official Journal of the American Academy of Clinical Psychiatrists, 29(4), 227–234A. [PMC free article] [PubMed] [Google Scholar]
- Phinney JS (1992). The multigroup ethnic identity measure: A new scale for use with diverse groups. Journal of Adolescent Research, 7(2), 156–176. [Google Scholar]
- Ridenour TA, Cruden G, Yang Y, Bonar EE, Rodriguez A, Saavedra LM, Hussong AM, Walton MA, Deeds B, Ford JL, Knight DK, Haggerty KP, Stormshak E, Kominsky TK, Ahrens KR, Woodward D, Feng X, Fiellin LE, Wilens TE, & Fernandes C-S (2022). Methodological strategies for prospective harmonization of studies: Application to 10 distinct outcomes studies of preventive interventions targeting opioid misuse. Prevention Science: The Official Journal of the Society for Prevention Research. 10.1007/s11121-022-01412-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni JW, Stucky BD, Thissen D, Dewitt EM, Irwin DE, Lai J-S, Yeatts K, & Dewalt DA (2010). PROMIS Pediatric Pain Interference Scale: An item response theory analysis of the pediatric pain item bank. The Journal of Pain: Official Journal of the American Pain Society, 11(11), 1109–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenaar AC, & Perry CL (1994). Community strategies for the reduction of youth drinking: Theory and application. Journal of Research on Adolescence: The Official Journal of the Society for Research on Adolescence, 4(2), 319–345. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Underlying primary data will be made available to outside individuals via written request to the Emory University PIs (Livingston and Komro) and with approval of a data sharing agreement with the Cherokee Nation.