Abstract
Purpose
This review aimed to compare the postoperative outcomes of open reduction internal fixation (ORIF) versus excision in the surgical treatment of hook of hamate fractures.
Methods
A systematic review of PubMed and EMBASE databases from 1954 to 2023 was performed using the search term “hook of hamate fracture” to identify all publications regarding the use of ORIF or excision in the treatment of hook of hamate fractures. Outcomes included a return to sport, pain, ulnar nerve dysfunction, flexor tendon dysfunction, union rate, wrist range of motion (ROM; % of contralateral hand), grip strength (% of contralateral hand), and quick disabilities of arm, shoulder, and hand scores.
Results
Twenty-seven of the 705 total screened articles were included. Excision of the hook of hamate (n = 779) resulted in a shorter return to sport time (6 vs 7.8 weeks), lower rates of postoperative pain (6.1% vs 33.3%), higher rates of ulnar nerve sensory dysfunction (4.2% vs 0%), and higher rates of ulnar nerve motor dysfunction (1.5% vs 0%) relative to ORIF (n = 51). Chronic fractures had a longer return to sport time (7.2 vs 5.7 weeks) relative to nonchronic injuries.
Conclusions
Both surgical procedures appear to yield acceptable outcomes in the treatment of hook of hamate fractures. However, based on the sparsity of available data, we are unable to determine a consistent difference between hook of hamate excision and ORIF.
Clinical relevance
To our knowledge, no current consensus on the optimal surgical treatment for hook of hamate fractures exists. Our findings emphasize the need for a large prospective cohort study using standardized outcomes to provide strong evidence as to whether surgical excision or ORIF yields greater outcomes in the treatment of hook of hamate fractures.
Key words: Fracture, Hook of hamate, Nonunion, Return to sport, Ulnar nerve, Union
Hook of hamate fractures comprise approximately 2% to 4% of all carpal fractures.1, 2, 3 The hook of hamate fracture frequently occurs in sports where repeated impact exerting a direct force against the hamate exists, such as tennis, baseball, and golf.4, 5, 6 The hook of the hamate’s peculiar anatomy places it at risk of fracture. A fracture of this area can result in weakness of grip and persistent ulnar-sided wrist pain, hindering everyday tasks and sports.7,8 If not optimally treated, hook of hamate fractures can cause chronic pain, nonunion, ulnar nerve irritation, degenerative changes, and tendon rupture.5,9 These potential complications have made injuries to the hook of the hamate historically challenging to manage.
Multiple reports of nonunion have been noted, even in patients in whom the correct diagnosis and proper immobilization were initiated early on.10 As such, current treatment modalities are directed toward early surgical intervention in the form of excision or ORIF. Although extensive methods of surgical management have been described, few studies provide direct comparison among techniques,5,9 and there remains a lack of consensus on the best approach to fracture treatment, particularly among athletes.5,9 The purposes of this study were to review the current literature on hook of hamate surgical treatment (excision vs ORIF) and analyze validated clinical and functional outcomes. We hypothesize that excision will be superior to ORIF in both clinical and functional outcomes.
Materials and Methods
Study selection
A literature search was performed on July 31, 2023, via the electronic databases PubMed and EMBASE using the search term “hook of hamate fracture.” Articles in the literature searched ranged from 1954 through July 2023. All articles subsequently underwent a 2-step review process by 2 independent reviewers as follows: (1) article title and abstract were reviewed and (2) those articles meeting eligibility criteria underwent a full-text review. This systematic review of the relevant literature was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.11
Eligibility criteria
Inclusion criteria for articles included the following: English-language articles, levels of evidence I through IV, specification of a fracture, specification of treatment or lack thereof, and inclusion of clinical outcomes data. Exclusion criteria included the following: non-English articles, review articles, case reports, studies evaluating hamate body fractures, studies evaluating newly implemented surgical procedures or technique guides, studies, including multiple fractures, and no reporting data separated by type of treatment.
Data abstraction/analysis
Two independent reviewers examined the selected full-text articles after abstract review for inclusion. Data, including patient characteristics, treatment methodology, and functional outcomes, were extracted from the articles selected for inclusion. The outcomes commonly reported were return to sport, pain, union, and ulnar nerve dysfunction.
Posttreatment range of motion (ROM) was reported as the percentage of the contralateral uninjured wrist ROM. Grip strength was reported as a percentage of injured hand strength to contralateral uninjured extremity. The quick disabilities of arm, shoulder, and hand (QuickDASH) is a patient-reported questionnaire comprising 11 questions pertaining to disability and severity of symptoms totaling to a maximum score of 100 with higher scores correlating to increased disability and symptoms. Weighted averages were calculated using studies that provided 1 or more of the above metrics. Time to surgery/diagnosis was calculated as the majority of studies reported either time to surgery or time to diagnosis. In one study, both were reported, but time to surgery was used to calculate time to surgery/diagnosis. All studies were available for synthesis and variables of interest that were not reported were left blank for the respective study. A meta-analysis could not be performed because of the heterogeneity of the literature collected. The protocol for this systematic review was not registered.
A preplanned risk assessment was not assessed within this systematic review because of the lack of high-quality evidence investigating the clinical outcomes in the surgical management of hook of hamate fractures. The systematic review consists of case series and retrospective cohort studies that contain inherent biases and the lack of a control group.
Results
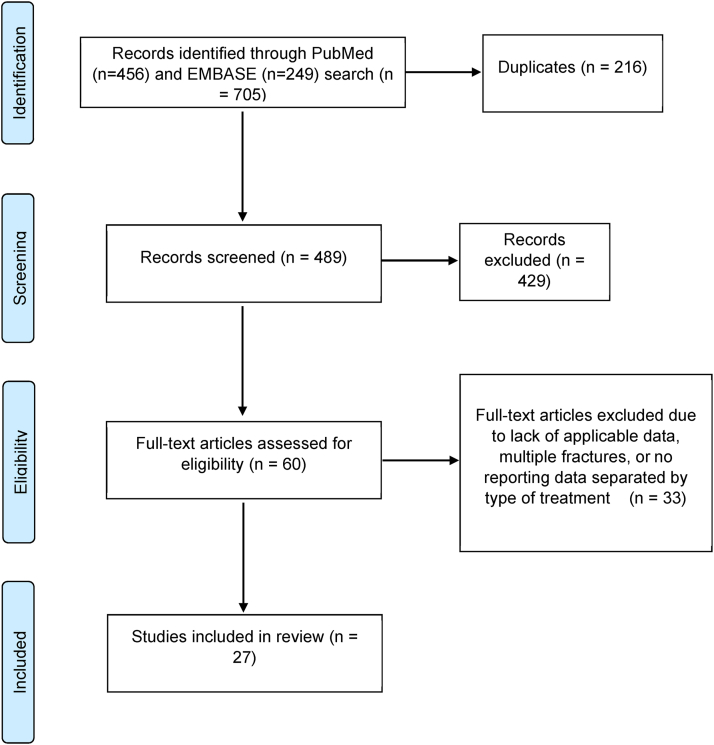
A total of 705 articles were identified, and 216 duplicates were removed. Subsequently, 60 articles met eligibility requirements in the first review of titles and abstracts. After full-text assessment, 27 articles were included in the current review. The literature review process is detailed in a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart (Fig).
Figure.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart depicting literature review methodology.
A total of 27 articles were included in the final review, 19 of which reported data on hook of hamate excision and 8 on ORIF.1,3, 4, 5,7,8,10,12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 Additionally, of the 27 articles included in the final review, 17 articles provided either time to diagnosis or time to procedure. In addition to stratification based on the type of operation, these articles were stratified based on the chronicity of the injury into 2 groups chronic (time to operation or time to diagnosis >12 weeks) and nonchronic (time to operation or time to diagnosis ≤12 weeks).
Patient characteristics
Appendix A (available on the Journal’s website at www.jhsgo.org) lists patient and study characteristics in more detail. Of the 27 articles included, data were available for 830 hands from 827 patients. In the ORIF group (51 patients; 51 hands; 8 papers), 15.6% of the patients were women and the average age for all patients was 40 years. The average time to surgery/diagnosis was 5.1 weeks, and the average time for follow-up was 25.1 months. Pain was present in 100% of the patients presenting with hook of hamate fractures. Sports-related injury was the cause of fracture in 30% of the patients who underwent ORIF. In the excision group (776 patients; 779 hands; 19 papers), 2.2% of the patients were women, and the average age for all patients was 23.2 years. The average time to surgery/diagnosis was 16.2 weeks, and the average time for follow-up was 13 months. Pain was present in 88% of the patients presenting with hook of hamate fracture. Sports-related injury was the cause of fracture in 93.7% of the patients who underwent hook of hamate excision.
Categorizing studies on chronicity of injury, in the chronic fracture group (135 patients; 135 hands; 8 papers), 7.1% of the patients were women, and the average age was 30.2 years. The average time to surgery/diagnosis was 20.8 weeks, and the average time for follow-up was 49.4 months. Pain was present in 100% of patients presenting with hook of hamate fractures. Sports-related injury was the cause of fracture in 77.8% of the patients with chronic injury. Hook of hamate excision was performed in 93.4% of these patients. In the nonchronic group (106 patients; 109 hands; 9 papers), 7.5% of the patients were women, and the average age was 26.4 years. The average time to surgery/diagnosis was 6.2 weeks, and the average time for follow-up was 23.1 months. Pain was present in 100% of the patients presenting with hook of hamate fractures. Sports-related injury was the cause of fracture in 41.5% of the patients with nonchronic injury. Hook of hamate excision was performed in 68.8% of these patients.
Clinical outcomes
The full list of outcomes was split by surgical intervention (Table 1) and chronicity of injury (Table 2). In ORIF studies, the ROM and grip strength were reported or calculated in 2 of 8 papers (19 hands), return to sport was reported in 1 of 8 paper (6 hands), final QuickDASH (average 13 months post-ORIF) score was reported in 3 of 8 papers (16 hands), pain was reported in 6 of 8 papers (39 hands), ulnar nerve and tendon dysfunction were reported in 3 of 8 papers (14 hands), and union was reported in 7 of 8 papers (38 hands). In excision studies, the ROM was not reported or calculable in any papers, grip strength was reported in 2 of 19 articles (32 hands), return to sport was reported in 14 of 19 papers (751 hands), final QuickDASH (average 19 months after excision) was reported in 1 of 19 papers (12 hands), pain was reported in 13 of 19 papers (444) hands, and ulnar nerve and tendon dysfunction were reported in 11 of 19 papers (432) hands.
Table 1.
Clinical Outcomes Stratified by Surgery Type
| Variable | ORIF | ORIF n = Hands (Papers) | Excision | Excision n = Hands (Papers) |
|---|---|---|---|---|
| ROM (%) | 92.7 | 19 (2) | - | 0 (0) |
| Grip strength (%) | 97.7 | 19 (2) | 92.9 | 32 (2) |
| Return to sport (wk) | 7.8 | 6 (1) | 6 | 751 (14) |
| QuickDASH | 2.3 | 16 (3) | 0.5 | 12 (1) |
| Pain (%) | 33.3 | 39 (6) | 6.1 | 444 (13) |
| Ulnar nerve sensory Dysfunction (%) | 0 | 14 (3) | 4.2 | 432 (11) |
| Ulnar nerve motor Dysfunction (%) | 0 | 14 (3) | 1.5 | 432 (11) |
| Tendon dysfunction (%) | 0 | 14 (3) | 0.8 | 432 (11) |
| Union (%) | 100 | 38 (7) | - | - |
Table 2.
Clinical Outcomes Stratified by Injury Chronicity
| Variable | Chronic | Chronic n = Hands (Papers) | Nonchronic | Nonchronic n = Hands (Papers) |
|---|---|---|---|---|
| ROM (%) | - | 0 (0) | 92.7 | 19 (2) |
| Grip strength (%) | 92.9 | 32 (2) | 97.7 | 19 (2) |
| Return to sport (wk) | 7.2 | 119 (5) | 5.7 | 74 (5) |
| QuickDASH | 0.8 | 4 (1) | 1.7 | 24 (3) |
| Pain (%) | 2.5 | 118 (7) | 15.7 | 89 (6) |
| Ulnar nerve sensory Dysfunction (%) | 1.8 | 110 (6) | 4.5 | 67 (4) |
| Ulnar nerve motor Dysfunction (%) | 0.9 | 110 (6) | 0 | 67 (4) |
| Tendon dysfunction (%) | 2.7 | 110 (6) | 0 | 67 (4) |
| Union (%) | 100 | 8 (2) | 100 | 21 (3) |
In chronic fractures, the ROM was not reported or calculable. Grip strength was reported or evaluated in 2 of 8 papers (32 hands), return to sport was evaluated in 5 of 8 papers (119 hands), final QuickDASH (average 6 months posttreatment) was reported in 1 of 8 papers (4 hands), pain was reported in 7 of 8 papers (118 hands), ulnar nerve and tendon dysfunction were reported in 6 of 8 papers (110 hands), and union was reported in 2 of 8 papers (38 hands). In nonchronic fractures, the ROM and grip strength were reported or calculated in 2 of 9 papers (19 hands), return to sport was reported in 5 of 9 papers (74 hands), and final QuickDASH (average 18 months posttreatment) was reported in 3 of 9 papers (24 hands), pain was reported in 6 of 9 papers (89) hands, ulnar nerve and tendon dysfunction were reported in 4 of 9 papers (67 hands), and union was reported in 3 of 9 papers (21 hands).
Excision of the hook of the hamate resulted in a return to sport time of 6 weeks, postoperative pain in 6.1% of the patients, ulnar nerve sensory dysfunction in 4.2% of the patients, and ulnar nerve motor dysfunction in 1.5% of the patients. Treatment with ORIF was associated with a return to sport time of 7.8 weeks, postoperative pain in 33.3% of the patients, ulnar nerve sensory dysfunction, and ulnar nerve motor dysfunction were not present among the ORIF group.
Treatment of chronic fractures resulted in a return to sport time of 7.2 weeks, postoperative pain in 2.5% of the patients, ulnar nerve sensory dysfunction in 1.8% of the patients, and ulnar nerve motor dysfunction in 0.9% of the patients. Treatment of nonchronic fractures was associated with a return to sport time of 5.7 weeks, postoperative pain in 15.7% of the patients, ulnar nerve sensory dysfunction in 4.5% of the patients, and ulnar nerve motor dysfunction was not present among the nonchronic group.
Discussion
This study provides an extensive literature review of treatment approaches in the setting of hook of hamate fracture care. We found that neither ORIF nor excision yielded consistently improved outcomes. Additionally, ORIF yielded the greatest average grip strength and lowest rates of ulnar nerve and flexor tendon dysfunction after surgery. Excision yielded a decreased return to sport time, postoperative QuickDASH score, and rates of postoperative pain. The cause of injury was much more likely to be related to sport in those who underwent hook of hamate excision.
Additionally, this study analyzed postoperative outcomes among acute versus chronic fractures of the hook of the hamate. Chronic fractures were much more likely to be treated with excision relative to nonchronic fractures. Chronic fractures had lower postoperative QuickDASH scores, lower rates of postoperative pain, and lower rates of ulnar nerve sensory dysfunction. Treatment of acute fractures resulted in greater grip strength, lower return to sport time, lower rates of ulnar nerve motor dysfunction, and lower rates of flexor tendon dysfunction.
Two studies have examined postoperative results among hook of hamate management treatments and compared the use of immobilization, hook of hamate excision, and ORIF.9,32 Neither surgical approach resulted in superior postoperative measures, whereas immobilization resulted in nonunion rates of 24% and 83% in each study. This is in accordance with the current review of literature where neither surgical intervention proved to be consistently superior.
The goal of surgery for hook of hamate excision was removal of the fracture while avoiding ulnar nerve structures. Indications for surgical treatment of these injuries include chronic nonunion fractures in addition to acute fractures in younger athletes. Therefore, ORIF is indicated for acute hook of hamate fractures in older adults. Although each method has general indications as noted above, great variability exists for each fracture based on the fracture characteristics and surgeon preference and experience. Postoperative rehabilitation after hook of hamate fracture also varies greatly by surgeon and institution; however, general mainstays of treatment include early passive ROM exercises as allowed by stability of the fixation construct. Disparity in postoperative rehabilitation is a potential source of variation in the results of this review.
This literature review has several limitations. Although only validated data were included, the heterogeneous composition of the articles reviewed made direct comparisons challenging. Particularly, the reported outcome measures displayed an enormous range of variation between articles, making it difficult to make definitive conclusions regarding the superiority of either surgical technique. Lack of standardized outcome measures not only resulted in reporting variability but also in the presentation of reported information. The relatively small sample sizes, because of data missingness, within ROM, grip strength, and QuickDASH score variables made these values unreliable in the comparison of surgical techniques. Direct comparisons were made even more challenging by the relatively low volume of studies investigating ORIF in the treatment of hook of hamate fractures. In addition, upon comparing nonchronic and chronic fractures, we found that the timing of surgery strongly impacted the type of surgery with which these patients were treated. As a result, our findings regarding the outcome differences between nonchronic and chronic fractures are confounded by the relatively high number of hook of hamate excision procedures performed in the chronic fracture cohort relative to the nonchronic fracture cohort. We elected not to exclude ORIF patients from this comparison because of the already low availability of data. The selection of only English-language articles imports a selection bias that may limit the generalizability of our findings. This review is also limited to a literature body of predominately case series with inherent biases that lack a control group. Because of this, we are unable to determine the causality of our findings. Therefore, future control studies are required to assess beyond correlation.
In this review, we report that no surgical approach to hook of hamate fracture management yielded consistently higher average postoperative outcomes. Treatment of this fracture is ultimately based on fracture chronicity, patient functional status, and ulnar nerve involvement. However, our data were limited by data missingness and demonstrated that no robust comparison of hook of hamate excision and ORIF is feasible with the existing literature. We recommend a robust prospective cohort or randomized trial with standardized outcomes, such as average postoperative pain, return to sport, ulnar nerve dysfunction, flexor tendon dysfunction, ROM, grip strength, and QuickDASH score.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly to this article.
Supplementary Data
References
- 1.Aldridge J.M., III, Mallon W.J. Hook of the hamate fractures in competitive golfers: results of treatment by excision of the fractured hook of the hamate. Orthopedics. 2003;26(7):717–719. doi: 10.3928/0147-7447-20030701-17. [DOI] [PubMed] [Google Scholar]
- 2.Boulas H.J., Milek M.A. Hook of the hamate fractures. Diagnosis, treatment, and complications. Orthop Rev. 1990;19(6):518–529. [PubMed] [Google Scholar]
- 3.Devers B.N., Douglas K.C., Naik R.D., Lee D.H., Watson J.T., Weikert D.R. Outcomes of hook of hamate fracture excision in high-level amateur athletes. J Hand Surg Am. 2013;38(1):72–76. doi: 10.1016/j.jhsa.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Bachoura A., Wroblewski A., Jacoby S.M., Osterman A.L., Culp R.W. Hook of hamate fractures in competitive baseball players. Hand (N Y) 2013;8(3):302–307. doi: 10.1007/s11552-013-9527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheufler O., Radmer S., Andresen R. Dorsal percutaneous cannulated mini-screw fixation for fractures of the hamate hook. Hand Surg. 2012;17(2):287–293. doi: 10.1142/S0218810412970039. [DOI] [PubMed] [Google Scholar]
- 6.Wharton D.M., Casaletto J.A., Choa R., Brown D.J. Outcome following coronal fractures of the hamate. J Hand Surg Eur. 2010;35(2):146–149. doi: 10.1177/1753193408098907. [DOI] [PubMed] [Google Scholar]
- 7.Bansal A., Carlan D., Moley J., Goodson H., Goldfarb C.A. Return to play and complications after hook of the hamate fracture surgery. J Hand Surg Am. 2017;42(10):803–809. doi: 10.1016/j.jhsa.2017.06.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barber J.A., Loeffler B., Gaston R.G., Lourie G.M. Excision of incomplete hook of the hamate fractures. Orthopedics. 2019;42(2):e232–e235. doi: 10.3928/01477447-20190125-05. [DOI] [PubMed] [Google Scholar]
- 9.Kadar A., Bishop A.T., Suchyta M.A., Moran S.L. Diagnosis and management of hook of hamate fractures. J Hand Surg Eur Vol. 2018;43(5):539–545. doi: 10.1177/1753193417729603. [DOI] [PubMed] [Google Scholar]
- 10.Tolat A.R., Humphrey J.A., McGovern P.D., Compson J. Surgical excision of ununited hook of hamate fractures via the carpal tunnel approach. Injury. 2014;45(10):1554–1556. doi: 10.1016/j.injury.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aso K. A comparison of the outcomes of excision of the fractured hook of hamate via a carpal tunnel approach versus a lateral approach. J Hand Surg Asian Pac. 2022;27(1):117–123. doi: 10.1142/S2424835522500126. [DOI] [PubMed] [Google Scholar]
- 13.Burleson A., Shin S. Return to play after hook of hamate excision in baseball players. Orthop J Sports Med. 2018;6(10) doi: 10.1177/2325967118803090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter P.R., Eaton R.G., Littler J.W. Ununited fracture of the hook of the hamate. J Bone Joint Surg Am. 1977;59(5):583–588. [PubMed] [Google Scholar]
- 15.Ceccarelli R., Dumontier C., Camuzard O. Minimally invasive fixation with a volar approach using a cannulated compression screw for acute hook of hamate fractures. J Hand Surg Am. 2019;44(11):993.e991–993.e996. doi: 10.1016/j.jhsa.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 16.David T.S., Zemel N.P., Mathews P.V. Symptomatic, partial union of the hook of the hamate fracture in athletes. Am J Sports Med. 2003;31(1):106–111. doi: 10.1177/03635465030310010201. [DOI] [PubMed] [Google Scholar]
- 17.Engler I.D., Barrazueta G., Colacchio N.D., Ruchelsman D.E., Belsky M.R., Leibman M.D. Excision of hook of hamate fractures in elite baseball players: surgical technique and return to play. Orthop J Sports Med. 2022;10(3) doi: 10.1177/23259671211038028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Erickson B.J., McElheny K., Chalmers P.N., et al. Performance and return to sport after excision of the fractured hook of the hamate in professional baseball players. Am J Sports Med. 2020;48(12):3066–3071. doi: 10.1177/0363546520949204. [DOI] [PubMed] [Google Scholar]
- 19.Futami T., Aoki H., Tsukamoto Y. Fractures of the hook of the hamate in athletes. 8 cases followed for 6 years. Acta Orthop Scand. 1993;64(4):469–471. doi: 10.3109/17453679308993670. [DOI] [PubMed] [Google Scholar]
- 20.Gómez B.O., Olea Á.G., Sierra V.H. Percutaneous dorsal approach for fractures of the hook of the hamate: a less common but effective option. Rev Iberoam Cir Mano. 2021;49(2):e90–e96. [Google Scholar]
- 21.Jie F., Hui Z., Dawei Z., Weiya Q. Treatment of the hook of hamate fracture with robot navigation: a note on technique. Acta Orthop Traumatol Turc. 2022;56(4):296–299. doi: 10.5152/j.aott.2022.21310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kimura H., Sato K., Suzuki T., Matsumura N., Iwamoto T. Excision of the hook of hamate in athletes using the carpal tunnel approach. J Orthop Sci. 2023;28(1):143–146. doi: 10.1016/j.jos.2021.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Lamas-Gómez C., Velasco-González L., González-Osuna A., Almenara-Fernández M., Trigo-Lahoz L., Aguilera-Roig X. Evaluation of grip strength in hook of hamate fractures treated with osteosynthesis. Is this surgical treatment necessary? Acta Orthop Traumatol Turc. 2019;53(2):115–119. doi: 10.1016/j.aott.2018.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milek M.A., Boulas H.J. Flexor tendon ruptures secondary to hamate hook fractures. J Hand Surg Am. 1990;15(5):740–744. doi: 10.1016/0363-5023(90)90147-j. [DOI] [PubMed] [Google Scholar]
- 25.Parker R.D., Berkowitz M.S., Brahms M.A., Bohl W.R. Hook of the hamate fractures in athletes. Am J Sports Med. 1986;14(6):517–523. doi: 10.1177/036354658601400617. [DOI] [PubMed] [Google Scholar]
- 26.Satake H., Naganuma Y., Shibuya J., Honma R., Nito T., Takagi M. Unsuccessful intervention of ct-assisted osteosynthesis for stress fractures of the hook of the hamate: a report of 3 cases. JBJS Case Connect. 2021;11(2) doi: 10.2106/JBJS.CC.20.00871. [DOI] [PubMed] [Google Scholar]
- 27.Sheridan J., Sheridan D., Sheridan D. Hook of hamate fractures in major and minor league baseball players. J Hand Surg Am. 2021;46(8):653–659. doi: 10.1016/j.jhsa.2021.03.015. [DOI] [PubMed] [Google Scholar]
- 28.Stark H.H., Chao E.K., Zemel N.P., Rickard T.A., Ashworth C.R. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71(8):1202–1207. [PubMed] [Google Scholar]
- 29.Teissier J., Escare P., Asencio G., Gomis R., Allieu Y. Rupture of the flexor tendons of the little finger in fractures of the hook of the hamate bone. Report of two cases. Ann Chir Main. 1983;2(4):319–327. doi: 10.1016/s0753-9053(83)80029-5. [DOI] [PubMed] [Google Scholar]
- 30.van Rijckevorsel V.A.J.I.M., Selles C.A., van der Vlies C.H., Cleffken B.I., Schep N.W.L. Functional outcome following headless compression screw fixation for hamate fractures. J Wrist Surg. 2020;9(2):164–169. doi: 10.1055/s-0039-1695765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watson H.K., Rogers W.D. Nonunion of the hook of the hamate: an argument for bone grafting the nonunion. J Hand Surg Am. 1989;14(3):486–490. doi: 10.1016/s0363-5023(89)80008-5. [DOI] [PubMed] [Google Scholar]
- 32.Scheufler O., Andresen R., Radmer S., Erdmann D., Exner K., Germann G. Hook of hamate fractures: critical evaluation of different therapeutic procedures. Plast Reconstr Surg. 2005;115(2):488–497. doi: 10.1097/01.prs.0000149480.25248.20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.