Abstract
Background
Stress and a sedentary lifestyle are major determinants of cardiovascular disease (CVD). As tai chi involves exercise and can help in stress reduction, it may be effective in the primary prevention of CVD.
Objectives
To determine the effectiveness of tai chi for the primary prevention of CVD.
Search methods
We searched the following electronic databases: the Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 11, 2013); MEDLINE (Ovid) (1946 to November week 3, 2013); EMBASE Classic + EMBASE (Ovid) (1947 to 6 December 2013); Web of Science (Thomson Reuters) (1970 to 6 December 2013); PsycINFO (Ovid) (1806 to December week 1, 2013); Database of Abstracts of Reviews of Effects (DARE); Health Technology Assessment Database and Health Economics Evaluations Database (Issue 4, 2013). We also searched the Allied and complementary Medicine Database (AMED) and OpenGrey (inception to October 2012) and several Asian databases. We searched trial registers and reference lists of reviews for further studies. We applied no language restrictions.
Selection criteria
Randomised controlled trials of tai chi lasting at least three months involving healthy adults or adults at high risk of CVD. The comparison group was no intervention or minimal intervention. The outcomes of interest were CVD clinical events and CVD risk factors. We excluded trials involving multifactorial lifestyle interventions or focusing on weight loss to avoid confounding.
Data collection and analysis
Two review authors independently selected trials for inclusion, abstracted the data and assessed the risk of bias.
Main results
We identified 13 small trials (1520 participants randomised) and three ongoing trials. All studies had at least one domain with unclear risk of bias, and some studies were at high risk of bias for allocation concealment (one study) and selective reporting (two studies). Duration and style of tai chi differed between trials. Seven studies recruited 903 healthy participants, the other studies recruited people with borderline hypertension or hypertension, elderly people at high risk of falling, and people with hypertension with liver and kidney yin deficiency syndrome.
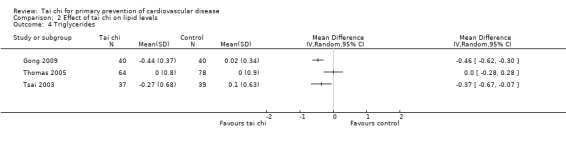
No studies reported on cardiovascular mortality, all‐cause mortality or non‐fatal events as most studies were short term (all studies had follow‐up of one year or less). There was also considerable heterogeneity between studies, which meant that it was not possible to combine studies statistically for cardiovascular risk (I2 statistic for systolic blood pressure (SBP) was 96%, for diastolic blood pressure (DBP) 96%, for total cholesterol 96%, low‐density lipoprotein‐cholesterol (LDL‐C) 95%, high‐density lipoprotein‐cholesterol (HDL‐C) 98%, triglycerides 75%). Nine trials measured blood pressure, six individual trials found reductions in SBP (reductions ranged from ‐22.0 mmHg (95% confidence interval (CI) ‐26.3 to ‐17.7) to ‐11.5 mmHg (95% CI ‐21.5 to ‐1.46)), two trials found no clear evidence of a difference (however, CIs were wide and an increase or decrease in SBP cannot be ruled out), and one trial found an increase in SBP with tai chi (increase 5.2 mmHg, 95% CI 3.73 to 6.67). A similar pattern was seen for DBP: three trials found a reduction in DBP (reductions ranged from ‐12.2 mmHg (95% CI ‐15.8 to ‐8.7) to ‐4.43 mmHg (95% CI ‐7.14 to ‐1.72)) and three trials found no clear evidence of a difference, however again with wide CIs. Three trials reported lipid levels and two found reductions in total cholesterol, LDL‐C and triglycerides (total cholesterol reductions ranged from ‐1.30 mmol/L (95% CI ‐1.57 to ‐1.03) to ‐0.50 mmol/L (95% CI ‐0.74 to ‐0.26): LDL‐C reductions ranged from ‐0.76 mmol/L (95% CI ‐0.93 to ‐0.59) to ‐0.59 mmol/L (95% CI ‐0.80 to ‐0.38): triglyceride reductions ranged from ‐0.46 mmol/L (95% CI ‐0.62 to ‐0.30) to ‐0.37 mmol/L (95% CI ‐0.67 to‐0.07)) and increased HDL‐C with the intervention (HDL‐C increases ranged from 0.61 mmol/L (95% CI 0.51 to 0.71) to 0.16 mmol/L (95% CI 0.02 to 0.30)), while the third study found no clear evidence of a difference between groups on lipid levels. Quality of life was measured in one trial: tai chi improved quality of life at three months. None of the included trials reported on adverse events, costs or occurrence of type 2 diabetes.
Authors' conclusions
There are currently no long‐term trials examining tai chi for the primary prevention of CVD. Due to the limited evidence available currently no conclusions can be drawn as to the effectiveness of tai chi on CVD risk factors. There was some suggestion of beneficial effects of tai chi on CVD risk factors but this was not consistent across all studies. There was considerable heterogeneity between the studies included in this review and studies were small and at some risk of bias. Results of the ongoing trials will add to the evidence base but additional longer‐term, high‐quality trials are needed.
Keywords: Adult, Humans, Tai Ji, Cardiovascular Diseases, Cardiovascular Diseases/prevention & control, Primary Prevention, Primary Prevention/methods, Randomized Controlled Trials as Topic, Risk Factors
Plain language summary
Tai Chi to prevent cardiovascular disease
Background
Cardiovascular diseases (CVD) are a group of conditions that affect the heart and blood vessels that are a worldwide health burden. However, it is thought that CVD risk can be lowered by changing a number of modifiable behaviours including increasing levels of exercise, and relaxation to reduce stress levels, and both of these comprise tai chi. This review assessed the effectiveness of tai chi interventions for healthy adults and adults at high risk of CVD at reducing cardiovascular death, all‐cause death, non‐fatal endpoints (such as heart attacks, strokes and angina) and CVD risk factors.
Study characteristics
We searched scientific databases for randomised controlled trials (clinical trials where people are allocated at random to one of two or more treatments) looking at the effects of tai chi on adults at high risk of developing CVD. We did not included people who had already had CVD (e.g. heart attacks and strokes). The evidence is current to December 2013.
Key results
We found 13 trials, none of them were large enough or of long enough duration to examine the effects of tai chi on reducing cardiovascular deaths or non‐fatal endpoints. There were variations in the duration and style of tai chi and the follow‐up of the interventions ranged from three to 12 months. Due to the small number of short‐term studies and the variability between them, we were unable to determine conclusively whether or not tai chi was beneficial at reducing cardiovascular risk in healthy adults and adults at increased risk of CVD, although beneficial effects for CVD risk factors were seen in some studies. None of the included studies reported on adverse events. Longer‐term, high‐quality trials are needed in order to determine the effectiveness of tai chi for CVD prevention.
Quality of the evidence
The results of this review should be treated with caution as the studies were small, of short duration and there was some risk of bias (where there was a risk of arriving at the wrong conclusions because of favouritism by the participants or researchers).
Background
Description of the condition
Cardiovascular diseases (CVD) are a group of conditions that affect the heart and blood vessels (WHO 2013). They include diseases such as coronary heart disease (CHD), hypertension and heart failure. According to the World Health Organization (WHO), CVDs were responsible for 17.3 million global deaths in 2008 and this is expected to rise to 23.6 million by 2030 (WHO 2013).
Many of the risk factors involved in the development of CVD are related to lifestyle choices, for example, an unhealthy diet, smoking, alcohol consumption and a lack of physical activity (WHO 2013). While clinical treatments are effective in treating and preventing CVD, other strategies involving making healthy lifestyle changes are also beneficial (Frishman 2005). One such beneficial strategy to use may be tai chi.
Description of the intervention
Tai chi originates from China and is a therapy that has evolved from a form of martial arts. It has been described as "a system of movements and postures used to enhance mental and physical health" (Ernst 2008). Tai chi has its foundations in Taoism and comprises three basic components, movement, meditation and deep breathing (Li 2001a), meaning that tai chi is not only a form of physical exercise but also mental exercise.
Tai chi has been shown to have a variety of physical and psychological effects (Han 2004): it can help to improve agility and balance (Tse 1991), improve lower extremity strength (Duncan 2001), and help to reduce stress (Jin 1992). Furthermore, tai chi is beneficial in improving general cardiorespiratory fitness, improving immune function and also in general pain management (Hong 2008; Verhagen 2004).
Interest in tai chi is growing as a consequence of increasing expenditure on chronic diseases, such as CVD, and due to ageing populations (Li 2001b). This is because tai chi is relatively inexpensive (Wolf 1996). Furthermore, tai chi is increasingly popular as a form of exercise, especially with older people, and as such may be an important intervention for the primary and secondary prevention of CVD. In fact, there are several studies that show tai chi to be effective for hypertension (Yeh 2008), and type 2 diabetes (Tsang 2008). Tai chi has also been shown to be beneficial in reducing stress (Hong 2008; Verhagen 2004), which is a determinant of CVD (WHO 2013).
How the intervention might work
Tai chi involves exercise and leads to stress reduction, both of which can be important in the prevention of CVD. Evidence suggests that exercise plays an important part in preventing CVD and diabetes (Mittal 2008). Regular exercise can reduce the risk of CVD mortality (USHHS 1996), and has favourable effects on CVD symptoms, quality of life and CVD risk factors (ACSM 2010; AHA 2011). Tai chi exercise is gentle, low impact and is of low intensity (Zhou 2012) and, therefore, may be a good choice of exercise for those individuals who are sedentary or less able to take more vigorous exercise.
Tai chi can help to reduce stress (Jin 1992), which is considered a determinant of CVD. While the exact mechanisms for this are unknown, some clinicians suggest that tai chi meditation acts as a distraction from the stressors (Bahrke 1978), while other clinicians suggest that the reduction in stress is due to the physical expenditure of tai chi (Zhou 1984). This is important since stress reduction has been shown to lead to a decrease in carotid atherosclerosis and hypertension, each being determinants in CVD development (Castillo‐Richmond 2000; Rainforth 2007).
Why it is important to do this review
There are a limited number of randomised controlled trials that have investigated the effectiveness of tai chi for the prevention of CVD. Moreover, few systematic reviews examining tai chi for the prevention of CVD exist and those reviews focus primarily on secondary prevention and not primary prevention (Dalusung‐Angosta 2011; Lee 2007a). As such, a comprehensive up‐to‐date systematic review is needed that thoroughly examines current evidence to determine the effectiveness of tai chi for the primary prevention of CVD.
Objectives
To determine the effectiveness of tai chi for the primary prevention of CVD.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials including cross‐over trials.
Types of participants
Adults aged 18 years and over from the general population and adults at high risk of CVD.
We excluded people who had experienced a previous myocardial infarction (MI), stroke, revascularisation procedure (coronary artery bypass grafting (CABG) or percutaneous transluminal coronary angioplasty (PTCA)), people with angina, or angiographically defined CHD.
Types of interventions
Trials investigating any style of tai chi.
We intended to stratify studies by tai chi style and duration, but there were insufficient studies for us to do this. We did not include multi‐factorial lifestyle intervention trials or trials involving weight loss in this review in order to avoid confounding. Furthermore, we focused on follow‐up periods of three months or more as these are the most relevant to public health interventions.
We only considered trials where the comparison group was either no intervention or minimal intervention (e.g. leaflets to promote increased physical activity or other more general health education with no face‐to‐face interaction or reinforcement).
Types of outcome measures
Primary outcomes
Cardiovascular mortality.
All‐cause mortality.
Non‐fatal endpoints such as MI, CABG, PTCA, angina, or angiographically defined CHD, stroke, carotid endarterectomy, peripheral arterial disease (PAD).
Secondary outcomes
Changes in systolic blood pressure (SBP), diastolic blood pressure (DBP) and blood lipids (total cholesterol, high‐density lipoprotein cholesterol (HDL‐C), low‐density lipoprotein cholesterol (LDL‐C), triglycerides).
Occurrence of type 2 diabetes as a major CVD risk factor.
Health‐related quality of life.
Adverse effects.
Costs.
Search methods for identification of studies
Electronic searches
We searched the following databases on 9 December 2013:
Cochrane Central Register of Controlled Trials (CENTRAL) (Issue 11, 2013);
MEDLINE (Ovid) (1946 to November week 3, 2013);
EMBASE Classic + EMBASE (Ovid) (1947 to 6 December 2013);
PsycINFO (Ovid) (1806 to December week 1, 2013);
Web of Science (Thomson Reuters) (1970 to 6 December 2013);
Database of Abstracts of Reviews of Effects (DARE) (Issue 4, 2013);
NHS Economic Evaluation Database (NEED) (Issue 4, 2013);
NHS Centre for Reviews and Dissemination (CRD) databases Health Technology Assessment (HTA) (Issue 4, 2013).
We also searched the Allied and complementary Medicine Database (AMED) and OpenGrey (www.opengrey.eu) (inception to October 2012) as well as the following Asian databases from their inception to April 2013:
China National Knowledge Infrastructure (CNKI) (www.cnki.net/);
WanFang data (www.wanfangdata.com.cn/);
Korea med (www.koreamed.org);
DBPIA (www.dbpia.co.kr/);
Korean studies information service system (kiss.kstudy.com/index.asp).
We used medical subject headings (MeSH) or equivalent and text word terms. We designed searches in accordance with the Cochrane Heart Group methods and guidance. Searches were tailored to individual databases. The search strategy for MEDLINE is shown in Appendix 1. We also applied a search filter for randomised controlled studies to the MEDLINE search (Lefebvre 2011), and adaptations of it to EMBASE, PsycINFO and Web of Science.
We imposed no language restrictions.
Searching other resources
We checked the reference lists of reviews and retrieved articles for additional studies.
We searched the metaRegister of Controlled Trials (mRCT) (www.controlled‐trials.com/mrct), Clinical trials.gov (www.clinicaltrials.gov), and the WHO International Clinical Trials Registry platform (ICTRP) (apps.who.int/trialsearch/) for ongoing trials (inception to October 2012).
We performed citation searches on key articles by using the citation network in Web of Science and used Google Scholar to search for further studies.
We also contacted experts in the field for unpublished and ongoing trials, and contacted study authors where necessary for any additional information.
Data collection and analysis
Selection of studies
Two review authors (LH and NF or MSL) reviewed the title and abstract of each paper and retrieved potentially relevant references. We then obtained the full text of potentially relevant studies and two review authors (LH and NF or MSL) independently selected studies to be included in the review by using predetermined inclusion criteria. In all cases, we resolved all disagreements about study inclusion by consensus and consulted a third review author (KR) if disagreements persisted.
Data extraction and management
Two review authors (LH and NF or MSL) independently extracted data using a pro forma. We also contacted chief investigators to provide additional relevant information when necessary. We extracted details of the study design, participant characteristics, study setting, intervention and outcome data (including details of outcome assessment, adverse effects and methodological quality (randomisation, blinding and attrition)) from each included study. We resolved any disagreements about extracted data by consensus and consulted a third review author (KR) if disagreements persisted.
Assessment of risk of bias in included studies
We assessed risk of bias by examining the random sequence generation and allocation concealment, description of drop‐outs and withdrawals (including analysis by intention‐to‐treat), blinding (participants, personnel and outcome assessment) and selective outcome reporting in each trial (Higgins 2011). We also assessed the risk of bias from other sources such as adherence to the intervention, balance of baseline characteristics and funding sources.
Two review authors (LH and NF or MSL) independently assessed the risk of bias of included studies and rated each domain as having a low risk of bias, a high risk of bias or an unclear risk of bias.
Measures of treatment effect
We processed data in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For continuous outcomes, we compared net changes (i.e. intervention group minus control group differences) and calculated the mean difference (MD) plus 95% confidence interval (CI) for each study. We would have expressed dichotomous outcomes as odds ratios (ORs) or risk ratios (RRs), with 95% CIs calculated for each study.
Assessment of heterogeneity
We conducted tests of heterogeneity for each outcome (using the Chi2 test of heterogeneity and I2 statistic). For situations where there was no heterogeneity, we intended to perform a fixed‐effect meta‐analysis. Where substantial heterogeneity was detected, we looked for possible explanations for this (e.g. participants and intervention). If the heterogeneity could not be explained, we considered the following options: provide a narrative overview and not aggregating the studies at all or use a random‐effects model with appropriate cautious interpretation.
Subgroup analysis and investigation of heterogeneity
We intended to stratify results by style and duration of tai chi exercise where possible. It was also planned for trials to be stratified by baseline risk, that is, healthy participants versus participants at high risk of CVD. If possible, we also intended to examine the effects of age and gender and the nature of the comparison group on outcomes as pre‐specified subgroup analyses. However, there was an insufficient number of studies that met the inclusion criteria to perform these analyses.
Sensitivity analysis
We intended to carry out sensitivity analysis excluding studies with a high risk of bias. Similarly, we planned to examine the effects of publication bias using funnel plots and tests of asymmetry (Egger 1997). However, there was an insufficient number of studies that met the inclusion criteria to perform these analyses.
Results
Description of studies
Results of the search
The searches generated 955 hits and 681 after de‐duplication. Screening the titles and abstracts identified 169 papers for formal inclusion and exclusion. Of these, 13 RCTs (14 papers) met the inclusion criteria. We identified three ongoing trials. Details of the flow of studies through the review are given in Figure 1.
1.
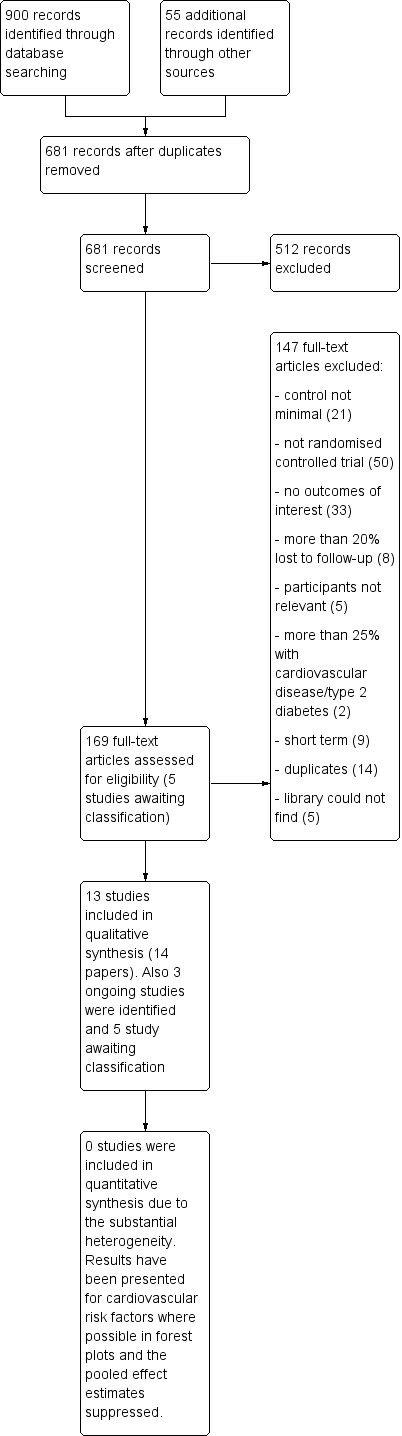
Study flow diagram.
Included studies
Details of the methods, participants, intervention, comparison group and outcome measures for each of the included studies in the review are provided in the Characteristics of included studies table. We included 13 trials that randomised 1520 participants (Atlanta FICSIT; Gao 2013; Gong 2009; Hui 2009; Logghe 2009; Luo 2006; Sun 1996; Sun 2010; Thomas 2005; Tsai 2003; Wang 2010; Wen 2005; Yang 2010). The health status of participants varied between studies; one study recruited participants with borderline hypertension (Tsai 2003); one study recruited older participants with a high risk of falling (Logghe 2009); two studies recruited people with essential hypertension (Luo 2006; Wen 2005); one study recruited people with hypertension with liver and kidney yin deficiency syndrome (Wang 2010); one study recruited people with hypertension (Sun 2010). The remaining studies recruited healthy people (903 participants) (Atlanta FICSIT; Gao 2013; Gong 2009; Hui 2009; Sun 1996; Thomas 2005; Yang 2010).
Nine trials recruited both male and female participants and four trials recruited only women (Gao 2013; Gong 2009; Wen 2005; Yang 2010). For one trial, no country information was available (36 participants) (Wen 2005), while two trials (156 participants) were conducted in the USA (Atlanta FICSIT; Sun 1996). The remaining studies were conducted in Hong Kong (581 participants randomised) (Hui 2009; Thomas 2005), Taiwan (88 participants) (Tsai 2003), China (390 participants) (Gao 2013; Gong 2009; Luo 2006; Sun 2010; Wang 2010; Yang 2010), and the Netherlands (269 participants) (Logghe 2009). The follow‐up periods varied between three months (Gao 2013; Hui 2009; Sun 1996; Tsai 2003), four months (Atlanta FICSIT; Wang 2010; Wen 2005; Yang 2010), five months (Gong 2009), six months (Luo 2006; Sun 2010) and 12 months (Logghe 2009; Thomas 2005).
The type of tai chi taught varied between the included studies. Four of the 13 included studies used the Yang style of tai chi (Hui 2009; Logghe 2009; Thomas 2005; Tsai 2003), one used tai chi breathing (Wen 2005), two used a simplified form of tai chi (Luo 2006; Sun 2010), and six studies did not state which style of tai chi they used (Atlanta FICSIT; Gao 2013; Gong 2009; Sun 1996; Wang 2010; Yang 2010). Duration of tai chi practice also varied between studies. Duration of classes ranged from 40 minutes to two hours with participants practising between one and seven times a week. Practice ranged from 12 weeks to one year. In two studies, no details were provided on the duration of tai chi practice (Sun 2010; Wang 2010). Five of the included studies stated that tai chi was taught by a qualified instructor (Atlanta FICSIT; Gao 2013; Hui 2009; Logghe 2009; Tsai 2003), and three studies stated that participants were encouraged to practice at home (Hui 2009; Logghe 2009; Thomas 2005).
We identified three ongoing trials. Details of these studies are shown in the Characteristics of ongoing studies table. The first study is examining the effect of tai chi practised for six months on change in heart rate complexity and change in centre of pressure complexity (Quilty 2011). The anticipated end date for this study is March 2014. The second study examined tai chi practised for eight weeks with four‐month follow‐up (Robins 2011), and the anticipated end date was June 2013. The third study examined tai chi practised for 12 weeks (Zheng 2011). No anticipated end date was provided for this study.
Five studies are awaiting classification (see Characteristics of studies awaiting classification table). For two of these studies, we are waiting for information from the authors concerning the control group and for the three remaining papers, we are waiting for translations.
Excluded studies
Details and reasons for exclusion for the studies that most closely missed the inclusion criteria are presented in the Characteristics of excluded studies table. Reasons for exclusion for the majority of studies were alternative designs (not randomised controlled trials), the intervention was not relevant, studies were short term with less than three months of follow‐up, or the control group did not receive a minimal intervention or no intervention (see Figure 1).
Risk of bias in included studies
Details for each of the 13 included studies are presented in the 'Risk of bias' tables in the Characteristics of included studies and summaries are presented in Figure 2 and Figure 3.
2.
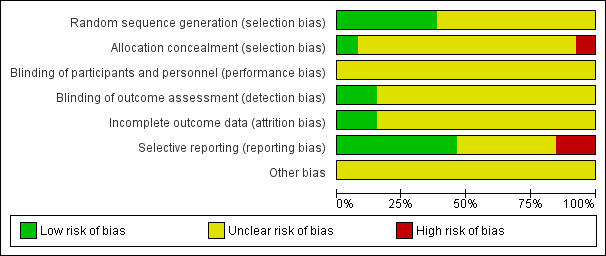
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
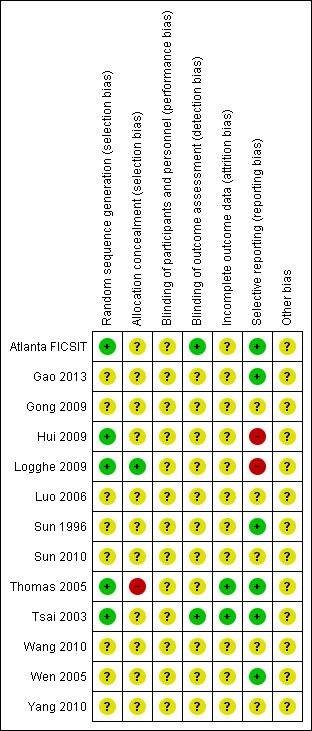
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
In five of the 13 included studies, random sequence generation methods were stated and we judged the methods to be of low risk of bias (Atlanta FICSIT; Hui 2009; Logghe 2009; Thomas 2005; Tsai 2003). In eight studies, the method of random sequence generation was unclear (Gao 2013; Gong 2009; Luo 2006; Sun 1996; Sun 2010; Wang 2010; Wen 2005; Yang 2010). The methods of allocation concealment were unclear in 11 of the included studies (Atlanta FICSIT; Gao 2013; Gong 2009; Hui 2009; Luo 2006; Sun 1996; Sun 2010; Tsai 2003; Wang 2010; Wen 2005; Yang 2010). In one study that stated the method of allocation concealment, we judged the method to be at low risk of bias (Logghe 2009), while in another study we judged the method to be at high risk of bias (Thomas 2005).
Blinding
The blinding of participants and personnel was not reported in all 13 of the included studies, so we have judged risk as unclear. However, it is difficult, if not impossible, to blind participants and personnel to behavioural interventions such as exercise. Two of the included studies reported blinding outcome assessors, which we judged to be at low risk of bias (Atlanta FICSIT; Tsai 2003).
Incomplete outcome data
We judged two of the 13 included studies to be at low risk of bias as losses to follow‐up were reported and reasons for drop‐puts were provided (Thomas 2005; Tsai 2003). In eight trials, we judged this as unclear as no information on losses to follow‐up was provided (Gao 2013; Gong 2009; Luo 2006; Sun 1996; Sun 2010; Wang 2010; Wen 2005; Yang 2010). We judged the remaining three trials as unclear because they either recorded the total number of losses but it was unclear from which treatment arm losses occurred (Atlanta FICSIT), or did not provide any or all reasons for drop‐outs (Hui 2009; Logghe 2009).
Selective reporting
Six of the included studies clearly stated the primary and secondary outcomes and reported the results of these (Atlanta FICSIT; Gao 2013; Sun 1996; Thomas 2005; Tsai 2003; Wen 2005). Two studies did not report all of their stated outcomes and so we judged these as having a high risk of bias (Hui 2009; Logghe 2009). In the remaining five trials, it was unclear if all outcomes had been reported and so we judged these as having an unclear risk of bias (Gong 2009; Luo 2006; Sun 2010; Wang 2010; Yang 2010).
Other potential sources of bias
In all cases, there was insufficient information to judge the risk of bias in other sources not covered above and we categorised all as unclear.
Effects of interventions
Cardiovascular events
We found no trials that reported cardiovascular mortality, all‐cause mortality or non‐fatal endpoints.
Cardiovascular risk factors
Blood pressure
Eleven of the included studies examined the effect of tai chi on blood pressure. In one study (Hui 2009), no data or information was provided as to blood pressure changes in the tai chi or control group. We contacted the authors but they did not respond. In another study (Wen 2005), blood pressure data were only provided for the tai chi group and no contact details were provided. However, it was stated that SBP decreased by 14.45 ± 5.64 mmHg (mean ± standard deviation) and DBP decreased by 8.85 ± 8.21 mmHg after 20 weeks in people performing tai chi. In the control group, there were no changes in SBP or DBP at 20 weeks.
Nine of the 13 studies provided useable data (Atlanta FICSIT; Gao 2013; Logghe 2009; Luo 2006: Sun 1996; Sun 2010; Thomas 2005; Tsai 2003; Wang 2010).
For SBP significant heterogeneity existed between trials (I2 = 96%) and we did not perform a meta‐analysis. In six trials, tai chi significantly reduced SBP (MD ‐11.5 mmHg, 95% CI ‐21.5 to ‐1.46 (Atlanta FICSIT); MD ‐22 mmHg, 95% CI ‐26.3 to ‐17.7 (Tsai 2003); MD ‐12.90 mmHg, 95% CI ‐17.87 to ‐7.93 (Luo 2006); MD ‐12.97 mmHg, 95% CI ‐22.71 to ‐3.23 (Sun 2010); MD ‐12.97, 95% CI ‐21.53 to ‐4.41 (Wang 2010); MD ‐11.76, 95% CI ‐16.48 to ‐7.04 (Gao 2013)), while in another two trials there was no statistically significant effect on SBP (MD ‐0.7 mmHg, 95% CI ‐5.0 to 3.6 (Thomas 2005); MD 2.10 mmHg, 95% CI ‐3.35 to 7.55 (Logghe 2009)). In the remaining trial, there was a statistically significant increase in SBP (MD 5.20 mmHg, 95% CI 3.73 to 6.67 (Sun 1996).
Seven of the 13 included studies measured DBP and had data that could have been combined in a meta‐analysis (Gao 2013; Logghe 2009; Luo 2006; Sun 1996; Sun 2010; Thomas 2005; Tsai 2003). However, significant heterogeneity existed between the trials (I2 = 96%) and so a meta‐analysis was not performed. In three trials, tai chi significantly reduced DBP (MD ‐12.2 mmHg, 95% CI ‐15.8 to ‐8.7 (Tsai 2003); MD ‐7.20 mmHg, 95% CI ‐12.11 to ‐2.29 (Sun 2010); MD ‐4.43, 95% CI ‐7.14 to ‐1.72 (Gao 2013)), while in another trial, tai chi significantly increased DBP (MD 5.20 mmHg, 95% CI 4.2 to 6.2) (Sun 1996). In the three remaining trials, tai chi had no statistically significant effect on DBP (MD 0.40 mmHg, 95% CI ‐2.27 to 3.07) (Logghe 2009); MD 1.10 mmHg, 95% CI ‐1.58 to 3.78 (Thomas 2005); MD ‐2.69 mmHg, 95% CI ‐6.30 to 0.92 (Luo 2006)).
Lipid levels
Five of the 13 included trials measured lipid levels. However, only three provided useable data (Gong 2009; Thomas 2005; Tsai 2003). The fourth trial provided no information or data for lipid levels (Hui 2009). We contacted the authors via email but they did not respond. The fifth trial provided LDL‐C levels at follow‐up but did not provide baseline values (Yang 2010). For this trial, no contact details were provided.
There was statistical heterogeneity between the three trials (that had usable data) for all lipid levels measured (total cholesterol: I2 = 96%, LDL‐C: I2 = 95%, HDL‐C: I2 = 98%, triglycerides: I2 = 75%), and so we did not perform meta‐analyses.
Two studies showed tai chi to significantly decrease total cholesterol (MD ‐0.50 mmol/L, 95% CI ‐0.74 to ‐0.26 (Tsai 2003); MD ‐1.30 mmol/L, 95% CI ‐1.57 to ‐1.03 (Gong 2009)). The remaining study found tai chi to have no effect on total cholesterol (MD 0 mmol/L, 95% CI ‐0.25 to 0.25) (Thomas 2005). A similar pattern was seen for LDL‐C. In two studies, LDL‐C was significantly reduced by tai chi (MD ‐0.59 mmol/L, 95% CI ‐0.80 to ‐0.38 (Tsai 2003); MD ‐0.76 mmol/L, 95% CI ‐0.93 to ‐0.59 (Gong 2009)). In the third study, tai chi had no effect on LDL‐C (MD 0 mmol/L, 95% CI ‐0.17 to 0.17) (Thomas 2005). In the trial that did not provide useable data, LDL‐ C was significantly lower in the tai chi group than in the control group (P value < 0.05) (Yang 2010).
For HDL‐C, one study found tai chi to have no effect (MD 0 mmol/L, 95% CI ‐0.07 to 0.07) (Thomas 2005), and the remaining two studies found tai chi to increase HDL‐C (MD 0.16 mmol/L, 95% CI 0.02 to 0.30 (Tsai 2003); MD 0.61 mmol/L, 95% CI 0.51 to 0.71 (Gong 2009)). One study also found tai chi to have no effect on triglycerides (MD 0 mmol/L, 95% CI ‐0.28 to 0.28) (Thomas 2005), while in the other two studies, tai chi significantly decreased triglyceride levels (MD ‐0.37 mmol/L, 95% CI ‐0.67 to ‐0.07 (Tsai 2003); MD ‐0.46 mmol/L, 95% CI ‐0.62 to ‐0.30 (Gong 2009)).
Quality of life was measured in one of the trials (Sun 2010). Tai chi for six days a week for people aged 40 to 70 years with hypertension significantly improved quality of life at three months (as assessed by 36 item Short Form (SF‐36) questionnaires).
None of the studies reported the occurrence of type 2 diabetes, adverse effects or costs.
Discussion
Summary of main results
We included 13 studies (1520 participants randomised) with durations of three months or more in this review from the 681 papers screened. However, only 10 of the 13 included studies provided useable data. For the remaining three studies, one provided no control group data and had no contact details, one only provided follow‐up results with no baseline data and had no contact details, and in the other, we contacted the authors for extra data but they did not respond. We identified three ongoing trials.
None of the included studies measured clinical events, as most were relatively short term and conducted in mainly healthy participants. There was also significant heterogeneity between studies, which meant that it was not possible to combine studies for blood pressure or lipid level measurements statistically. There was some evidence of beneficial effects of tai chi on CVD risk factors but this was not consistent across all studies. Nine trials measured SBP, six showed a statistically significant decrease in SBP with tai chi, two showed no effect and one showed an increase in SBP with the intervention. Similar results were seen for DBP. Three trials measured lipid levels, two showed beneficial effects of tai chi while the other showed no effects of the intervention.
The results of this review highlight gaps in the published literature. There is a lack of good evidence on the effects of tai chi on CVD risk factors and a lack of any trials reporting clinical events. Most trials included in this review were relatively small and short term, and larger, longer‐term trials should be conducted to determine the potential benefits of tai chi for the primary prevention of CVD.
Overall completeness and applicability of evidence
This review included adults with varying levels of CVD risk and included both men and women. Most included trials were carried out in developed countries. None of the 13 included trials examined our primary outcomes as most of the trials had relatively short follow‐up and recruited predominantly healthy participants. We were unable to examine the duration and type of tai chi and the effects of age, gender and the nature of the comparison group on outcomes due to the limited number of included trials.
The effectiveness of tai chi could not be rigorously assessed since only four trials (640 participants) assessed CVD risk factors at six months. The remaining nine studies were shorter term so it is unclear whether any effects of the intervention could be sustained. Significant heterogeneity was also found between trials for blood pressure and lipid levels meaning that meta‐analyses could not be performed. There was considerable variability in the interventions, participants recruited and outcomes measured in the included trials. The three ongoing trials will add to the evidence base but more trials are needed.
Quality of the evidence
The results of this review should be treated with caution as the studies included were at some risk of bias. In seven studies, the methods of random sequence generation were stated. In 11 of the studies, the details of allocation concealment were not stated, in one study this was judged as low risk of bias while in one study allocation concealment was judged as high risk of bias. Twelve of the 13 included trials did not state if participants, personnel or outcome assessors were blinded. However, it is difficult, if not impossible, to blind participants and personnel to behavioural lifestyle interventions such as tai chi. The risk of bias related to incomplete outcome data was unclear in 11 studies but low in two. Bias due to selective reporting was judged as high in two studies, low in six studies and unclear in the remaining five studies. For all studies, there was insufficient information to judge the risk of other biases.
This review is also at risk of small‐study bias since most of the included trials were small. We were unable to examine the effects of publication bias in funnel plots because of the limited number of included studies. However, small trials are often conducted with less methodological rigour, more likely to be carried out in selected populations and have been shown to report larger beneficial effects than larger trials (Nüesch 2010; Sterne 2000; Sterne 2001). The results of this review need to be interpreted with this in mind.
Potential biases in the review process
We conducted a comprehensive search across major databases for interventions involving tai chi. We also screened systematic review reference lists and contacted study authors where necessary. However, from corresponding with study authors, we did not receive further unreported data from two trials, which limited our analyses. Two review authors independently conducted all screening, inclusion and exclusion, and data abstraction. Two review authors also conducted data entry and analysis.
Our decision to restrict this review to interventions only investigating tai chi avoided the potential confounding effects of other behavioural interventions on our outcomes (e.g. interventions that focused on weight loss). However, this may have limited the number of trials eligible for inclusion. In addition, the small number of trials on which this review is based, limitations in the reporting of methodological quality, an unclear risk of bias in most of the included trials, and no data for primary outcomes and limited data for secondary outcomes means that the findings to date are limited. In addition, most of the included trials were relatively short term at three months of follow‐up with only four reporting outcomes at six months or more, which was our original inclusion criteria. Hence, it is unclear whether any potential benefits of tai chi on CVD risk factors would be sustained in the longer term.
Agreements and disagreements with other studies or reviews
To our knowledge, no other systematic review including only randomised controlled trials has been carried out solely to examine the effects of tai chi in adults for the primary prevention of CVD. Other systematic reviews have looked at tai chi in relation to cancer, osteoarthritis and type 2 diabetes (Lee 2007b; Lee 2008a; Lee 2008b) or have looked at tai chi for the secondary prevention of CVD (Yeh 2008; Yeh 2009).
Other reviews have examined the effects of tai chi only in people with hypertension (Lee 2007a; Lee 2010). One review found limited evidence for the effectiveness of tai chi on blood pressure in older people (Lee 2010). Another review did find some evidence indicating that tai chi reduced blood pressure in people with hypertension but this review was based on only a small number of trials with small sample sizes and consequently no firm conclusions about the effectiveness of tai chi could be drawn (Lee 2007a). In this review, there was some suggestion of beneficial effects of tai chi on blood pressure and lipids but this was not consistent across all of the included studies.
In this current review, heterogeneity of included participants and the nature, intensity and duration of the interventions precluded meta‐analyses so the effects of tai chi on CVD risk factors are inconclusive to date. While it would be helpful to explore the impact of the different intervention components, such as tai chi intensity on our outcomes we currently do not have enough trials to do so. This will be investigated in future updates of this review.
Authors' conclusions
Implications for practice.
Few trials met the inclusion criteria for our review and none reported our primary outcomes. Significant heterogeneity was also found between the included trials meaning that meta‐analysis was not possible. Studies included in this review were also at risk of bias and as such the results should be treated with caution. Given the limited evidence to date, this review cannot make definitive conclusions about tai chi for the primary prevention of cardiovascular disease (CVD).
Implications for research.
There is a lack of randomised controlled trials looking at the effects of tai chi for the primary prevention of CVD. In particular, there is a shortage of well‐conducted randomised controlled trials that examine the effects of tai chi over the long term to determine the effects of such interventions on CVD events. We also found no trials reporting economic evaluations of tai chi interventions.
Acknowledgements
We are grateful to Nicole Martin and Jo Abbot for conducting the searches for this review.
Appendices
Appendix 1. Search strategies December 2013
The Cochrane Library
#1 MeSH descriptor: [Cardiovascular Diseases] explode all trees #2 cardio* #3 cardia* #4 heart* #5 coronary* #6 angina* #7 ventric* #8 myocard* #9 pericard* #10 isch?em* #11 emboli* #12 arrhythmi* #13 thrombo* #14 atrial next fibrillat* #15 tachycardi* #16 endocardi* #17 (sick near/2 sinus) #18 MeSH descriptor: [Stroke] explode all trees #19 (stroke or stokes) #20 cerebrovasc* #21 cerebral next vascular #22 apoplexy #23 (brain near/2 accident*) #24 ((brain* or cerebral or lacunar) near/2 infarct*) #25 MeSH descriptor: [Hypertension] explode all trees #26 hypertensi* #27 peripheral next arter* next disease* #28 ((high or increased or elevated) near/2 blood near/2 pressure) #29 MeSH descriptor: [Hyperlipidemias] explode all trees #30 hyperlipid* #31 hyperlip?emia* #32 hypercholesterol* #33 hypercholester?emia* #34 hyperlipoprotein?emia* #35 hypertriglycerid?emia* #36 MeSH descriptor: [Arteriosclerosis] explode all trees #37 MeSH descriptor: [Cholesterol] explode all trees #38 cholesterol #39 coronary next risk next factor* #40 MeSH descriptor: [Blood Pressure] this term only #41 "blood pressure" #42 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 #43 MeSH descriptor: [Tai Ji] this term only #44 MeSH descriptor: [Martial Arts] this term only #45 tai chi #46 tai ji #47 chi tai #48 taji* #49 tai chi #50 tai‐chi #51 taiji #52 #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 #53 #42 and #52
MEDLINE Ovid
1. exp Cardiovascular Diseases/ 2. cardio*.tw. 3. cardia*.tw. 4. heart*.tw. 5. coronary*.tw. 6. angina*.tw. 7. ventric*.tw. 8. myocard*.tw. 9. pericard*.tw. 10. isch?em*.tw. 11. emboli*.tw. 12. arrhythmi*.tw. 13. thrombo*.tw. 14. atrial fibrillat*.tw. 15. tachycardi*.tw. 16. endocardi*.tw. 17. (sick adj sinus).tw. 18. exp Stroke/ 19. (stroke or stokes).tw. 20. cerebrovasc*.tw. 21. cerebral vascular.tw. 22. apoplexy.tw. 23. (brain adj2 accident*).tw. 24. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 25. exp Hypertension/ 26. hypertensi*.tw. 27. peripheral arter* disease*.tw. 28. ((high or increased or elevated) adj2 blood pressure).tw. 29. exp Hyperlipidemias/ 30. hyperlipid*.tw. 31. hyperlip?emia*.tw. 32. hypercholesterol*.tw. 33. hypercholester?emia*.tw. 34. hyperlipoprotein?emia*.tw. 35. hypertriglycerid?emia*.tw. 36. exp Arteriosclerosis/ 37. exp Cholesterol/ 38. cholesterol.tw. 39. cholesterol.tw. 40. "coronary risk factor*".tw. 41. Blood Pressure/ 42. blood pressure.tw. 43. or/1‐42 44. Tai Ji/ 45. Martial Arts/ 46. tai chi.tw. 47. tai ji.tw. 48. chi tai.tw. 49. taji$.tw. 50. t'ai chi.tw. 51. tai‐chi.tw. 52. taiji.tw. 53. or/44‐52 54. 43 and 53 55. randomized controlled trial.pt. 56. controlled clinical trial.pt. 57. randomized.ab. 58. placebo.ab. 59. drug therapy.fs. 60. randomly.ab. 61. trial.ab. 62. groups.ab. 63. 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 64. exp animals/ not humans.sh. 65. 63 not 64 66. 54 and 65
EMBASE Ovid
1. exp Cardiovascular Diseases/ 2. cardio*.tw. 3. cardia*.tw. 4. heart*.tw. 5. coronary*.tw. 6. angina*.tw. 7. ventric*.tw. 8. myocard*.tw. 9. pericard*.tw. 10. isch?em*.tw. 11. emboli*.tw. 12. arrhythmi*.tw. 13. thrombo*.tw. 14. atrial fibrillat*.tw. 15. tachycardi*.tw. 16. endocardi*.tw. 17. (sick adj sinus).tw. 18. exp Stroke/ 19. (stroke or stokes).tw. 20. cerebrovasc*.tw. 21. cerebral vascular.tw. 22. apoplexy.tw. 23. (brain adj2 accident*).tw. 24. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 25. exp Hypertension/ 26. hypertensi*.tw. 27. peripheral arter* disease*.tw. 28. ((high or increased or elevated) adj2 blood pressure).tw. 29. exp Hyperlipidemias/ 30. hyperlipid*.tw. 31. hyperlip?emia*.tw. 32. hypercholesterol*.tw. 33. hypercholester?emia*.tw. 34. hyperlipoprotein?emia*.tw. 35. hypertriglycerid?emia*.tw. 36. exp arteriosclerosis/ 37. exp cholesterol/ 38. cholesterol.tw. 39. "coronary risk factor*".tw. 40. Blood Pressure/ 41. blood pressure.tw. 42. or/1‐41 43. Tai Chi/ 44. tai chi.tw. 45. tai ji.tw. 46. chi tai.tw. 47. taji$.tw. 48. t'ai chi.tw. 49. tai‐chi.tw. 50. taiji.tw. 51. or/43‐50 52. 42 and 51 53. random$.tw. 54. factorial$.tw. 55. crossover$.tw. 56. cross over$.tw. 57. cross‐over$.tw. 58. placebo$.tw. 59. (doubl$ adj blind$).tw. 60. (singl$ adj blind$).tw. 61. assign$.tw. 62. allocat$.tw. 63. volunteer$.tw. 64. crossover procedure/ 65. double blind procedure/ 66. randomized controlled trial/ 67. single blind procedure/ 68. 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 69. (animal/ or nonhuman/) not human/ 70. 68 not 69 71. 52 and 70
PsycINFO Ovid
1. exp Cardiovascular Disorders/ 2. cardio*.tw. 3. cardia*.tw. 4. heart*.tw. 5. coronary*.tw. 6. angina*.tw. 7. ventric*.tw. 8. myocard*.tw. 9. pericard*.tw. 10. isch?em*.tw. 11. emboli*.tw. 12. arrhythmi*.tw. 13. thrombo*.tw. 14. atrial fibrillat*.tw. 15. tachycardi*.tw. 16. endocardi*.tw. 17. (sick adj sinus).tw. 18. exp Stroke/ 19. (stroke or stokes).tw. 20. cerebrovasc*.tw. 21. cerebral vascular.tw. 22. apoplexy.tw. 23. (brain adj2 accident*).tw. 24. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 25. exp Hypertension/ 26. hypertensi*.tw. 27. peripheral arter* disease*.tw. 28. ((high or increased or elevated) adj2 blood pressure).tw. 29. exp Hyperlipidemias/ 30. hyperlipid*.tw. 31. hyperlip?emia*.tw. 32. hypercholesterol*.tw. 33. hypercholester?emia*.tw. 34. hyperlipoprotein?emia*.tw. 35. hypertriglycerid?emia*.tw. 36. exp Arteriosclerosis/ 37. exp Cholesterol/ 38. cholesterol.tw. 39. "coronary risk factor*".tw. 40. exp blood pressure/ 41. blood pressure.tw. 42. or/1‐41 43. Martial Arts/ 44. tai chi.tw. 45. tai ji.tw. 46. chi tai.tw. 47. taji$.tw. 48. t'ai chi.tw. 49. tai‐chi.tw. 50. taiji.tw. 51. or/43‐50 52. 42 and 51 53. random$.tw. 54. factorial$.tw. 55. crossover$.tw. 56. cross‐over$.tw. 57. placebo$.tw. 58. (doubl$ adj blind$).tw. 59. (singl$ adj blind$).tw. 60. assign$.tw. 61. allocat$.tw. 62. volunteer$.tw. 63. control*.tw. 64. "2000".md. 65. or/53‐64 66. 52 and 65
Web of Science
#32 #31 AND #30 AND #29 #31 TS=((random* or blind* or allocat* or assign* or trial* or placebo* or crossover* or cross‐over*)) #30 TS=((tai chi) or (tai ji) or (taji*) or (t'ai chi) or (tai‐chi) or (taiji) or (chi tai)) #29 #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 #28 TS=(arteriosclerosis or cholesterol or "coronary risk factor*" or "blood pressure") #27 TS=(hyperlipoprotein?emia* or hypertriglycerid?emia*) #26 TS=(hypercholester?emia*) #25 TS=(hypercholesterol*) #24 Topic=(hyperlip?emia*) #23 Topic=(hyperlipid*) #22 Topic=(((brain* or cerebral or lacunar) near/2 infarct*)) #21 Topic=(brain near/2 accident*) #20 Topic=(apoplexy) #19 Topic=("cerebral vascular") #18 Topic=(cerebrovasc*) #17 Topic=(stroke or strokes) #16 Topic=("sick sinus") #15 Topic=(endocardi*) #14 Topic=(tachycardi*) #13 Topic=((atrial fibrillat*)) #12 Topic=(thrombo*) #11 Topic=(arrhythmi*) #10 Topic=(emboli*) #9 Topic=(isch?em*) #8 Topic=(pericard*) #7 Topic=(myocard*) #6 Topic=(ventric*) #5 Topic=(angina*) #4 Topic=(coronary*) #3 Topic=(heart*) #2 Topic=(cardia*) #1 Topic=(cardio*)
AMED
1. cardio*.tw. 2. cardia*.tw. 3. heart*.tw. 4. coronary*.tw. 5. angina*.tw. 6. ventric*.tw. 7. myocard*.tw. 8. pericard*.tw. 9. isch?em*.tw. 10. emboli*.tw. 11. arrhythmi*.tw. 12. thrombo*.tw. 13. atrial fibrillat*.tw. 14. tachycardi*.tw. 15. endocardi*.tw. 16. (sick adj sinus).tw. 17. exp Stroke/ 18. (stroke or strokes).tw. 19. cerebrovasc*.tw. 20. cerebral vascular.tw. 21. apoplexy.tw. 22. (brain adj2 accident*).tw. 23. ((brain* or cerebral or lacunar) adj2 infarct*).tw. 24. exp Hypertension/ 25. hypertensi*.tw. 26. peripheral arter* disease*.tw. 27. ((high or increased or elevated) adj2 blood pressure).tw. 28. hyperlipid*.tw. 29. hyperlip?emia*.tw. 30. hypercholesterol*.tw. 31. hypercholester?emia*.tw. 32. hyperlipoprotein?emia*.tw. 33. hypertriglycerid?emia*.tw. 34. arteriosclerosis.tw. 35. cholesterol.tw. 36. cholest*.tw. 37. or/1‐36 38. Tai Ji/ 39. Martial Arts/ 40. tai chi.tw. 41. tai ji.tw. 42. chi tai.tw. 43. taji$.tw. 44. t'ai chi.tw. 45. tai‐chi.tw. 46. taiji.tw. 47. or/38‐46 48. 37 and 47 49. randomized controlled trial.pt. 50. controlled clinical trial.pt. 51. randomized.ab. 52. placebo.ab. 53. randomly.ab. 54. trial.ab. 55. groups.ab. 56. 49 or 50 or 51 or 52 or 53 or 54 or 55 57. exp animals/ not humans.sh. 58. 56 not 57 59. 48 and 58
Clinicaltrials.gov
1. Cardio* 2. Tai Chi
WHO ICTRP
1. Cardio* 2. Tai Chi
ISRCTN Register
1. Cardio* 2. Tai Chi
OpenGrey
1. Cardio* 2. Tai Chi
CNKI (Chinese Medical Database of the China Academic Journal)
1. 太极
2. 太极拳
3. 1 or 2
4. 心血管疾病
5. 冠心病
6. 高血压
7. 高血脂
8. 心绞痛
9. 心肌梗死
10. 心律失常
11. 心力衰竭
12. 心肌缺血
13. 动脉粥样硬化
14. 冠状动脉疾病
15. 中风
16. 脑卒中
17. 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
18. 对照
19. 随机
20. 18 and 19
21. 3 and 17 and 20 (49)
WanFang Data
1. 太极拳
2. 心血管疾病
3. 对照
4. 1 and 2 and 3 (3)
Korea med
1.태극
2.태극권
3.Taichi
4.Taiji
DBPIA
.태극권
2.Tai chi 운동
3.Taiji
Korean Studies Information Service System
1.태극권
2.Tai chi 운동
Data and analyses
Comparison 1. Effect of tai chi on blood pressure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Systolic blood pressure | 9 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Diastolic blood pressure | 7 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
1.1. Analysis.
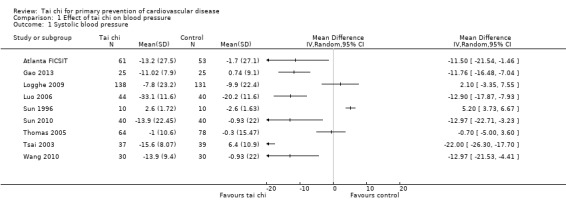
Comparison 1 Effect of tai chi on blood pressure, Outcome 1 Systolic blood pressure.
1.2. Analysis.
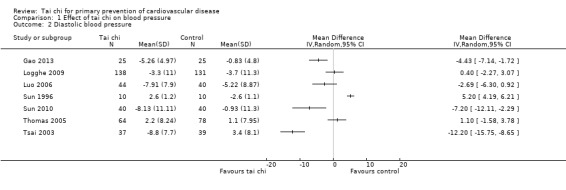
Comparison 1 Effect of tai chi on blood pressure, Outcome 2 Diastolic blood pressure.
Comparison 2. Effect of tai chi on lipid levels.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Total cholesterol | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Low‐density lipoprotein cholesterol | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 High‐density lipoprotein cholesterol | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Triglycerides | 3 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
2.1. Analysis.
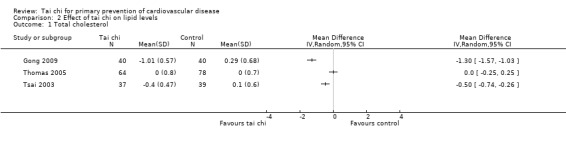
Comparison 2 Effect of tai chi on lipid levels, Outcome 1 Total cholesterol.
2.2. Analysis.
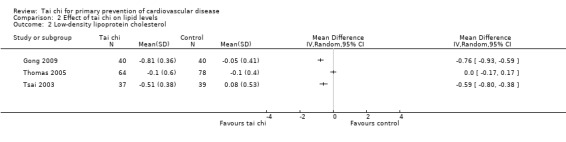
Comparison 2 Effect of tai chi on lipid levels, Outcome 2 Low‐density lipoprotein cholesterol.
2.3. Analysis.
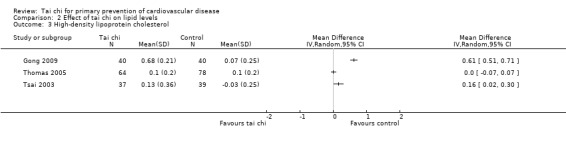
Comparison 2 Effect of tai chi on lipid levels, Outcome 3 High‐density lipoprotein cholesterol.
2.4. Analysis.
Comparison 2 Effect of tai chi on lipid levels, Outcome 4 Triglycerides.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Atlanta FICSIT.
| Methods | RCT with parallel group design | |
| Participants | Participants: 200 older people living in the community were recruited through local adverts and by direct contact. Mean age: 76.2 years Inclusion criteria: 70 years of age or older, live in unsupervised environments, ambulatory Exclusion criteria: presence of debilitating condition such as severe cognitive impairments, metastatic cancer, severe arthritis, Parkinson's disease or major stroke, profound visual deficits that could compromise balance or ambulation Country of publication: USA |
|
| Interventions | Participants were randomly assigned to control (education) or tai chi or computerised balance training Tai chi group (n = 72): classes were a synthesis of the existing 108 forms into 10 that could be completed during the 15 weeks. Forms emphasised all components of movement that typically become limited with age. Participants were encouraged to practice at home for at least 15 minutes twice a day Control group (n = 64): instructed not to change their exercise levels. Met weekly for 1 hour with a researcher/gerontological nurse to discuss topics of interest to older people such as pharmacological management, sleep disorders, cognitive deficits, coping with bereavement and other issues of interest Follow‐up: 4 months |
|
| Outcomes | Blood pressure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated fixed randomisation procedure was used |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data collectors were blind to the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Details of drop‐outs were provided but numbers were not provided by group |
| Selective reporting (reporting bias) | Low risk | All main outcomes reported but states measured blood pressure but only reports SBP not DBP |
| Other bias | Unclear risk | Insufficient information to judge |
Gao 2013.
| Methods | RCT | |
| Participants | Participants: 50 older women from the Donghu Lake District of Shanghai Inclusion criteria: 61‐71 years old without recent regular exercise, healthy without any disability, took no pills that could influence the results of the study, agreed to the trial Country of publication: China |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 25): learned tai chi for 1 week before the study began. After mastering tai chi, the group practised tai chi for 50‐60 minutes per session, 5 times a week for 3 months. Tai chi was organised and executed collectively and with instructions provided by specialists Control (n = 25): no exercise Follow‐up: 3 months |
|
| Outcomes | Blood pressure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All outcomes stated were reported |
| Other bias | Unclear risk | Insufficient information to judge |
Gong 2009.
| Methods | RCT | |
| Participants | Participants: 80 older women who were community residents Inclusion criteria: no bone metabolic disease, cerebrovascular diseases or family history of these diseases Country of publication: China |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi group (n = 40): exercise in the morning at 7‐8 am for 60 minutes for 20 weeks. 10 minutes' preparation and warm‐up activity before tai chi practice and 10 minutes' organisational activities at the end Control (n = 40): no information provided Follow‐up: 20 weeks |
|
| Outcomes | Lipids | |
| Notes | This article was translated and data abstracted by 1 review author (MS) who could speak Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Intention‐to‐treat analysis was used but no other information provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
Hui 2009.
| Methods | RCT of parallel group design | |
| Participants | Participants: 374 sedentary, middle‐aged men and women were recruited from a large housing estate Inclusion criteria: no known cardiovascular or pulmonary diseases, neurological disorders or musculoskeletal disorders Country of publication: Hong Kong |
|
| Interventions | Participants were randomly assigned to control or tai chi or walking exercises Tai chi group (n = 129): 12‐week training programme with 5 days of exercise a week. This was led by a qualified instructor for 3 days and for 2 days participants were to practice on their own. A modified Yang style of tai chi was selected that had 32 movements Control group (n = 124): no exercise intervention |
|
| Outcomes | Lipid levels | |
| Notes | Author was contacted for data and information on blood pressure, lipid levels and quality of life for each group at baseline and follow‐up. This was done 3 times via email. The author did not respond | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by locations using simple random drawing procedure |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No reasons for losses to follow‐up provided |
| Selective reporting (reporting bias) | High risk | States CVD risk factors were examined through blood tests but data on lipid levels were not reported |
| Other bias | Unclear risk | Insufficient information to judge |
Logghe 2009.
| Methods | RCT of parallel group design | |
| Participants | Participants: 269 older men and women identified and recruited using patient registration files of participating general practitioners Mean age: 77 years Inclusion criteria: aged 70 years and older, living at home, have a high fall risk, disturbed balance, mobility problems, dizziness and use benzodiazepines or diuretics Country of publication: the Netherlands |
|
| Interventions | Participants were randomly assigned to control or tai chi chuan At baseline both groups received a brochure explaining how to prevent fall incidents in and around the house Tai chi (n = 138): 1 hour of tai chi chuan training twice a week for 13 weeks. 4 professional tai chi chuan instructors gave the lessons using a pre‐defined protocol. The core of the lessons consisted of 10 positions from the Yang style. Chi kung exercises were used during the warm up and cool down periods and group size ranged from 7 to 14 people. Participants were also asked to practice at home at least twice a week for about 15 minutes. Control (n = 131): usual care and could use or apply for available services in the area as before Follow‐up: 12 months |
|
| Outcomes | Blood pressure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used pre‐stratified block randomisation using a computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Independent research assistant stratified participants |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinded research assistant performed baseline measures |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Used an intention‐to‐treat analysis and reported losses to follow‐up but did not provide all the reasons for losses or drop‐outs |
| Selective reporting (reporting bias) | High risk | No information provided on forced expiratory volume and peak expiratory flow even though these were measured but reasons provided as to why not reported. Also blood pressure not reported at 6 months |
| Other bias | Unclear risk | Insufficient information to judge |
Luo 2006.
| Methods | RCT | |
| Participants | Participants: 84 adults with primary hypertension Age: 36‐68 years Exclusion criteria: people with secondary hypertension; aged below 35 years old; aged over 70 years; women who were pregnant or lactating; people with heart, brain, liver or kidney dysfunction44 Country of publication: China |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 44): 24 simplified tai ji quan exercises every day for 45 minutes for 6 months. Also received angiotensin‐converting enzyme inhibitors once daily Control (n = 40): received only angiotensin‐converting enzyme inhibitors for 6 months Follow‐up: 6 months |
|
| Outcomes | Blood pressure | |
| Notes | This paper was translated and data abstracted by 1 review author (MS), who spoke Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Used intention‐to‐treat analysis but no other information was provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
Sun 1996.
| Methods | RCT of parallel group design | |
| Participants | Participants: 20 Hmong adults recruited from door‐to‐door interviews Age: ≥ 60 years Exclusion criteria: severe cardiovascular conditions or taking medication for cardiovascular conditions Country of publication: USA |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 10): participation was once a week for 12 weeks. The programme comprised of 10 × 2 hour sessions including mini lectures on simple human physiological systems, common diseases in older adults, information on emotional and mental health and stress management. The sessions also included a review of tai chi chuan movements from previous week and the teaching of new movements. Participants were also provided with an assignment of tai chi exercises to practice until the next session Control (n = 10): asked to continue with their routine physical activities Follow‐up: 12 weeks |
|
| Outcomes | Blood pressure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on the number of participants eligible |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Unclear risk | Insufficient information to judge |
Sun 2010.
| Methods | RCT | |
| Participants | Participants: 80 middle‐aged and older people with hypertension Age: 40‐70 years Inclusion criteria: primary hypertension with unused blood pressure medication or oral antihypertensive drugs, SBP 140‐179 mmHg and DBP 90‐109 mmHg, no systematic exercise habits at ordinary times (< 20 minutes per time, less that twice a week), no serious liver or kidney dysfunction, no joint disease, knee arthritis, limb motor or sensory dysfunction caused by trauma and no movement of other diseases Country of publication: China |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 40): 24 simplified taijiquan exercises for 3 months Control (n = 40): did not change lifestyle and did not receive an exercise intervention Follow‐up: 6 months |
|
| Outcomes | Blood pressure, quality of life | |
| Notes | This paper was translated and data abstracted by 1 review author (MS) who could speak Chinese | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
Thomas 2005.
| Methods | RCT of parallel group design | |
| Participants | Participants: 207 healthy older adults of either sex Age: 65‐74 years Exclusion criteria: people with impaired mobility, dementia, known CVD or uncontrolled/newly diagnosed hypertension, people regularly performing exercise. Country of publication: Hong Kong |
|
| Interventions | Participants were randomly assigned to control or tai chi or resistance training exercise Tai chi (n = 64): attended a health centre for 1‐hour sessions 3 times a week where tai chi was performed using the 24 forms of movements of the simplified yang style. There was a 15‐minute warm‐up followed by a 45‐minute period of tai chi that was supervised by a registered tai chi master. The participants were encouraged to practice between classes Control (n = 78): requested to maintain their usual levels of physical activity for the duration of the study Follow‐up: 12 months |
|
| Outcomes | Blood pressure and lipid levels | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list stratified by sex |
| Allocation concealment (selection bias) | High risk | List held by a study member and as participants were recruited they were allocated to groups by a study nurse |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis performed and there were a similar number of losses between the intervention and control group. Reasons for drop‐outs were also provided |
| Selective reporting (reporting bias) | Low risk | Clearly stated primary and secondary outcomes and reported results |
| Other bias | Unclear risk | Insufficient information to judge |
Tsai 2003.
| Methods | RCT of parallel group design | |
| Participants | Participants: 88 men and women with documented borderline hypertension recruited from a university campus and 2 teaching hospitals Age (mean ± standard deviation): control 50.5 ± 9.8 years, tai chi 51.6 ± 16.3 years Inclusion criteria: documented borderline hypertension, not on medication and not engaged in an exercise programme prior to study Exclusion criteria: a personal history of coronary artery disease, strokes, limiting orthopaedic problems or any other major health problems Country of publication: Taiwan |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 44): prior to participation the tai group participants practised 108 postures of Yang style tai chi following instructions and movements provided by qualified masters. They then performed this exercise 3 times a week. Each session included 10 minutes of warm up, 30 minutes of tai chi practice and 10 minutes of cool down. Each posture was performed according to a pre‐recorded form sequence on a tape to ensure the same time course. Control (n = 44): maintained their usual lifestyle with regular follow‐up through outpatient department or by telephone every 4 weeks Follow‐up: 12 weeks |
|
| Outcomes | Blood pressure and lipid levels | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | States randomly assigned by drawing |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research assistant taking blood pressure measurements was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for losses were reported and there was a similar number of losses between groups |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcomes reported |
| Other bias | Unclear risk | Insufficient information to judge |
Wang 2010.
| Methods | RCT | |
| Participants | Participants: 60 people with primary and secondary hypertension (SBP 140‐179 mmHg and DBP 90‐109 mmHg) and liver and kidney yin deficiency syndrome Age: 50‐70 years Country of publication: China |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 30): performed therapeutic exercise prescription in tai chi movements for 16 weeks Control (n = 30): no exercise Follow‐up: 16 weeks |
|
| Outcomes | SBP | |
| Notes | This article was translated by 1 review author (MS) who could speak Chinese. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
Wen 2005.
| Methods | RCT of parallel group design | |
| Participants | Participants: 36 women with essential hypertension Age: 50‐62 years Country of publication: not stated |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 20): 40 minutes of tai chi breathing 3 times a week for 20 weeks Control (n = 16): no information provided Follow‐up: period was 20 weeks |
|
| Outcomes | Blood pressure | |
| Notes | This is an abstract. Authors could not be contacted to provide extra information as no contact details were provided on the abstract. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on losses to follow‐up was given |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | Insufficient information to judge |
Yang 2010.
| Methods | RCT | |
| Participants | Participants: 36 healthy women Age (mean ± standard deviation): tai chi: 47.09 ± 2.3 years, control: 49.4 ± 5.0 years Country of publication: China |
|
| Interventions | Participants were randomly assigned to control or tai chi Tai chi (n = 25): morning exercise with taijiquan practitioners in the park. Practised taijiquan weekly for > 14 hours for 8.6‐14.7 months Control (n = 11): no sports activities Follow‐up: 16 weeks |
|
| Outcomes | Lipids | |
| Notes | This article was translated and data abstracted by 1 author (MS) who speaks Chinese. Only follow‐up data for low‐density lipoprotein cholesterol was reported with no baseline values provided. No contact details were given | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | No information provided |
| Other bias | Unclear risk | No information provided |
DBP: diastolic blood pressure; RCT: randomised controlled trial; SBP: systolic blood pressure.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Barbat‐Artigas 2011 | Not an RCT |
| Brown 1995 | No outcomes of interest |
| Frishman 2009 | Not an RCT |
| Gemmell 2006 | Short‐term follow‐up (6 weeks) |
| Jin 1992 | Short‐term follow‐up (1 hour) |
| Li 2012 | No outcomes of interest and not relevant population |
| Mao 2006 | Short‐term follow‐up (8 weeks) |
| Nedelijkovic 2012 | No outcomes of interest |
| Sattin 2005 | No outcomes of interest |
| Song 2003 | No outcomes of interest |
| Thumwaree 2011 | Short‐term follow‐up (8 weeks) |
| Wayne 2010 | No outcomes of interest |
| Wu 2010 | Control group not minimal |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
Lee 2004.
| Methods | Article written in Korean with no English abstract ‐ awaiting translation |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Lu 2012.
| Methods | Awaiting details about the control group |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Rosardo‐Pérez 2012.
| Methods | Awaiting details about the control group |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Si 2006.
| Methods | Article written in Chinese with no English abstract ‐ awaiting translation |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Zhang 1997.
| Methods | Article written in Chinese with no English abstract ‐ awaiting translation |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes |
Characteristics of ongoing studies [ordered by study ID]
Quilty 2011.
| Trial name or title | Tai Chi, Physiologic Complexity, and Healthy Aging |
| Methods | Randomised, single‐blind, parallel group design |
| Participants | Inclusion criteria:
Exclusion criteria:
Age minimum: 50 years Age maximum: 79 years Gender: men or women |
| Interventions | Tai chi: community‐based tai chi class twice a week for 6 months as well as practice tai chi outside of class twice a week for the same 6‐month period Control: wait list receiving standard medical care |
| Outcomes | Primary:
|
| Starting date | March 2011 Estimated primary completion date: March 2013 (final data collection date for primary outcome measure) |
| Contact information | Mary Teresa Quilty Beth Israel Deaconess Medical Center Brookline Massachusetts 02215, USA Tel: 617‐432‐1602 Email: maryteresa_quilty@hms.harvard.edu Jacquelyn Walsh Beth Israel Deaconess Medical Center Brookline Massachusetts 02215, USA Tel: 617‐732‐6508 Email: jwalsh19@partners.org |
| Notes |
Robins 2011.
| Trial name or title | Reduce Cardiovascular Risk in Women Through Tai Chi Intervention |
| Methods | Randomised, open‐label, parallel group design |
| Participants | Inclusion criteria:
Exclusion criteria:
Age minimum: 35 years Age maximum: 50 years Gender: female |
| Interventions | Tai chi: 8‐week tai chi intervention will be led by Project PI. A focused short form of tai chi involving 12 movements will be used. Each 8‐weekly 60‐minute session will begin with a 10‐minute guided meditation session. Movements learned the previous week will be reviewed prior to introducing new movements. Training DVDs will be produced and provided to participants for weekly and ongoing practice of the techniques Control: wait list |
| Outcomes | Primary:
Secondary:
|
| Starting date | June 2011 Estimated primary completion date: December 2012 (final data collection date for primary outcome measure) |
| Contact information | Jo Robins Virginia Commonwealth University Richmond Virginia 23298, USA Tel: 804‐828‐0776 Email: jwrobins@vcu.edu |
| Notes |
Zheng 2011.
| Trial name or title | The Effect of Six Weeks of Tai Ji Practice on Anxiety in Healthy but Stressed People Compared to an Exercise Only Comparison Group |
| Methods | Randomised, 3‐arm parallel group design. |
| Participants | Inclusion criteria:
Exclusion criteria:
Age minimum: 18 years Age maximum: 60 years Gender: men and women |
| Interventions | Tai chi: the tai ji sessions will take place for the first 6 weeks when there will be 5 tai ji sessions per week (1 hour each) available for participants to attend. Participants must complete at least 5 hours of tai ji training a week (minimum 1800 minutes during the initial 6 weeks) and at least 2 of these must be in the contact sessions. The contact session will be conducted as a group with a trainer and non‐contact practice will self practice and monitored by a log book. There is no limit on how many contact tai ji sessions any individual attends, but the minimum of 2 contact sessions must be completed per week. After the initial 6 weeks, there will only be 1 contact session a week for the remaining 6 weeks to revise any forgotten movements and check completion of log books. The emphasis on home tai ji practice (non‐contact) will be strongly reinforced and the minimum of 5 hours of tai ji training a week still applies. Participants will be asked to follow the DVD they were given at the commencement of the trial in regards to the training Control: will be idle for the 12 weeks of the trial; however, they will be given 6 weeks of tai ji practice and the DVD after the 12 weeks as appreciation for their involvement in this trial Active control: provided with gym membership for the duration of the trial (12 weeks). It is expected that they complete 5 hours of exercise per week including at least 2 hours at the UTS Fitness Centre. They will be assessed by the staff at the UTS Fitness Centre and will be required to attend at least 1 of the scheduled exercise classes inclusive in the 2 hours they spend at the UTS Fitness Centre. There will be a weekly meeting with this group to check progress of journals Follow‐up: 12 weeks |
| Outcomes | Primary:
Secondary:
|
| Starting date | 1 July 2011 |
| Contact information | Mr Shuai Zheng Room 44 level 3 building 4 City Campus University of Technology Sydney 2007 New South Wales Australia Tel: +61 2 9514 1780 Email: shuai.zheng@student.uts.edu.au Associate Professor Chris Zaslawski Science Building University of Technology Sydney ‐ City Campus Corner of Harris and Thomas Street Broadway 2007 New South Wales Australia Tel: +61 2 9514 7856 Email: Chris.Zaslawski@uts.edu.au |
| Notes |
bpm: beats per minute; BMI: body mass index; CVD: cardiovascular disease; DBP: diastolic blood pressure; ECG: electrocardiogram; HR: heart rate; LDL‐C: low‐density lipoprotein cholesterol; SBP: systolic blood pressure.
Differences between protocol and review
It was our intention to include only studies with a six‐month follow‐up. However, as such, studies were lacking, we changed the review to include studies with a follow‐up of three months or more.
It was also our intention to perform stratified analyses to examine the effects of duration, nature of the comparison group and type of tai chi but the review included an insufficient number of trials to do this. Similarly, the lack of included studies meant that we were unable to examine the effects of gender and age. We also intended to perform funnel plots to assess publication bias. These will be addressed in future updates of this review when more evidence is available.
In the protocol, it was stated that we would search SCI‐EXPANDED; however, this was not done for this review. Furthermore, we searched a number of Asian databases that were not stated in the protocol.
Contributions of authors
All authors contributed to the protocol development. The Trials Search Co‐ordinators of the Cochrane Heart Group ran the searches and MSL conducted the searches for the Asian databases. LH and NF or MSL screened titles and abstracts and assessed studies for formal inclusion and exclusion. LH and NF or MSL abstracted data and assessed methodological rigour. LH analysed the data, which were checked by KR. LH wrote the first draft of the review and all review authors contributed to later drafts.
Sources of support
Internal sources
Warwick Medical School, University of Warwick, UK.
Complementary Medicine, Peninsula Medical School, Exeter, UK.
-
Korea Institute of Oriental Medicine, Korea, South.
K13281 and K13400
External sources
NIHR Cochrane Programme Grant, UK.
Declarations of interest
None known.
New
References
References to studies included in this review
Atlanta FICSIT {published data only}
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T, et al. Reducing frailty and falls in older persons: an investigation of tai chi and computerised balance training. Journal of the American Geriatrics Society 1996;44:489‐97. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T, et al. Selected as the best paper in the 1990s: reducing frailty and falls in older persons: an investigation of tai chi and computerised balance training. Journal of the American Geriatrics Society 2003;51:1794‐803. [DOI] [PubMed] [Google Scholar]
Gao 2013 {published data only}
- Gao DQ. Effect of 3‐month tai chi exercise on heart and lung capability of elder people. Proceedings of the 2013 International Conference on Educational Research and Sports Education. Paris: Atlantis Press, 2013; Vol. 39:86‐8.
Gong 2009 {published data only}
- Gong JC, Liu YD, Zhao DM, Zhao ML. Taijishan effect on community indicators of blood lipid in middle aged and old women. Journal of Community Medicine 2009;7(17):34‐5. [Google Scholar]
Hui 2009 {published data only}
- Hui SSC, Woo J, Kwok T. Evaluation of energy expenditure and cardiovascular health effects from tai chi and walking exercise. Hong Kong Medical Journal 2009;15:S4‐7. [PubMed] [Google Scholar]
Logghe 2009 {published data only}
- Logghe IHJ, Zeeuwe PEM, Verhagen AP, Wijnen‐Sponselee RMT, Willemsen SP, Bierma‐Zeinstra SMA, et al. Lack of effect of tai chi chuan in preventing falls in elderly people living at home: a randomised clinical trial. Journal of the American Geriatrics Society 2009;57:70‐5. [DOI] [PubMed] [Google Scholar]
Luo 2006 {published data only}
- Luo H. Tai Chi combined with drug in treatment of essential hypertension: a clinical study. China Medical Herald 2006;3(33):43‐4. [Google Scholar]
Sun 1996 {published data only}
- Sun WY, Dosch M, Gilmore GD, Pemberton W, Scarseth T. Effects of a tai chi chuan program on Hmong American older adults. Educational Gerontology 1996;22:161‐7. [Google Scholar]
Sun 2010 {published data only}
- Sun QQ. Research on the effect of middle‐aging and elderly high blood pressure patients quality of life by practice Taichi. Beijing Sport University 2010:1‐62. [Google Scholar]
Thomas 2005 {published data only}
- Thomas GN, Hong AWL, Tomlinson B, Lau E, Lam CWK, Sanderson JE, et al. Effects of tai chi and resistance training on cardiovascular risk factors in the elderly Chinese subjects: a 12‐month longitudinal, randomised, controlled intervention study. Clinical Endocrinology 2005;63:663‐9. [DOI] [PubMed] [Google Scholar]
Tsai 2003 {published data only}
- Tsai JC, Wang WH, Chan P, Lin LJ, Wang CH, Tomlinson B, et al. The beneficial effects of tai chi chuan on blood pressure and lipid profile and anxiety status in a randomised controlled trial. Journal of Alternative and Complementary Medicine 2003;9(5):747‐54. [DOI] [PubMed] [Google Scholar]
Wang 2010 {published data only}
- Wang XJ, Li YJ, Liu NN. Empirical study of taijiquan interventions on the prevention and cure of hypertension. Journal of Beijing Sport University 2011;34(9):75‐7. [Google Scholar]
Wen 2005 {published data only}
- Wen J, Kang YS. Tai chi breathing on BP, HR, EEG and mood in seniors with essential hypertension. Medicine and Science in Sports and Exercise 2005;37(5):S255. [Google Scholar]
Yang 2010 {published data only}
- Yang Q, Fu RD. Study on antioxidant effect of taijiquan to the middle‐aged and elderly women. Liaoning Sport Science and Technology 2010;32(4):38‐9. [Google Scholar]
References to studies excluded from this review
Barbat‐Artigas 2011 {published data only}
- Barbat‐Artigas S, Filion ME, Dupontgand S, Karelis AD, Aubertin‐Leheudre M. Effects of tai chi training in dynapenic and nondynapenic postmenopausal women. Menopause 2011;18(9):974‐9. [DOI] [PubMed] [Google Scholar]
Brown 1995 {published data only}
- Brown DR, Wang Y, Ward A, Ebbeling CB, Fortlage L, Puleo E, et al. Chronic psychological effects of exercise and exercise plus cognitive strategies. Medicine and Science in Sports and Exercise 1995;27(5):765‐75. [PubMed] [Google Scholar]
Frishman 2009 {published data only}
- Frishman WH, Beravol P, Carosella C. Alternative and complementary medicine for preventing and treating cardiovascular disease. Disease‐a‐Month 2009;55(3):121‐92. [DOI] [PubMed] [Google Scholar]
Gemmell 2006 {published data only}
- Gemmell C, Leathem JM. A study investigating the effects of tai chi chuan: individuals with traumatic brain injury compared to controls. Brain Injury 2006;20(2):151‐6. [DOI] [PubMed] [Google Scholar]
Jin 1992 {published data only}
- Jin P. Efficacy of tai chi, brisk walking, meditation, and reading in reducing mental and emotional stress. Journal of Psychosomatic Research 1991;36(4):361‐70. [DOI] [PubMed] [Google Scholar]
Li 2012 {published data only}
- Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, et al. Tai chi and postural stability in patients with Parkinson's disease. New England Journal of Medicine 2012;366(6):511‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mao 2006 {published data only}
- Mao HN, Sha P. Effect of tai chi exercise on blood pressure, plasma nitrogen monoxidum and endothelin in hypertensive patients. Chinese Journal of Clinical Rehabilitation 2006;10(48):65‐7. [Google Scholar]
Nedelijkovic 2012 {published data only}
- Nedeljkovic M, Ausfeld‐Hafter B, Streitberger K, Seiler R, Wirtz PH. Taiji practice attenuates psychobiological stress reactivity ‐ a randomized controlled trial in healthy subjects. Psychoneuroendocrinology 2012;37(8):1171‐80. [DOI] [PubMed] [Google Scholar]
Sattin 2005 {published data only}
- Sattin RW, Easley KA, Wolf SL, Chen Y, Kutner MH. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. Journal of the American Geriatrics Society 2005;53(7):1168‐78. [DOI] [PubMed] [Google Scholar]
Song 2003 {published data only}
- Song R, Lee, EO, Lam P, Bae SC. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. Journal of Rheumatology 2003;30(9):2039‐44. [PubMed] [Google Scholar]
Thumwaree 2011 {published data only}
- Thumwaree B, Nana A, Limroongreungrat W, Laksanakorn W. Effects of 8‐week wheelchair tai chi training on cardiorespiratory fitness in individuals with spinal cord injury. Journal of Science and Medicine in Sport 2011;14:e109. [Google Scholar]
Wayne 2010 {published data only}
- Wayne PM, Buring JE, Davis RB, Connors EM, Bonato P, Patritti B, et al. Tai chi for osteopenic women: design and rationale of a pragmatic randomized controlled trial. BMC Musculoskeletal Disorders 2010;11(40):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2010 {published data only}
- Wu G, Keyes L, Callas P, Ren X, Bookchin B. Comparison of telecommunication, community, and home‐based tai chi exercise programs on compliance and effectiveness in elders at risk for falls. Archives of Physical Medicine and Rehabilitation 2010;91(6):849‐56. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Lee 2004 {published data only}
- Lee EN. The effects of tai chi exercise program on blood pressure, total cholesterol and cortisol level in patients with essential hypertension. Taehan Kanho Hakhoe Chi 2004;34:829‐37. [DOI] [PubMed] [Google Scholar]
Lu 2012 {published data only}
- Lu WA, Kuo CD. Effect of 3‐month tai chi chuan on heart rate variability, blood lipid and cytokine profiles in middle‐aged and elderly individuals. International Journal of Gerontology 2012;6:267‐72. [Google Scholar]
Rosardo‐Pérez 2012 {published data only}
- Rosado‐Pérez J, Santiago‐Osorio E, Ortiz R, Mendoza‐Núñez VM. Tai chi diminishes oxidative stress in Mexican older adults. Journal of Nutrition, Health & Aging 2012;16:642‐6. [DOI] [PubMed] [Google Scholar]
Si 2006 {published data only}
- Si CJ. The effect of taijiquan exercise on the constitution of mid and old age people. Journal of Liaoning Normal University (Natural Science Edition) 2006;29(3):379‐81. [Google Scholar]
Zhang 1997 {published data only}
- Zhang Q, Wei X, Zhao SY. The effect of Tai Chi on microcirculation system in elderly. Journal of Binzhou Medical College 1997;20(5):11. [Google Scholar]
References to ongoing studies
Quilty 2011 {published data only}
- NCT01340365. Tai chi, physiologic complexity, and healthy aging. clinicaltrials.gov/show/NCT01340365 (accessed 31 March 2014).
Robins 2011 {published data only}
- NCT01467544. Reduce cardiovascular risk in women through tai chi intervention. clinicaltrials.gov/show/NCT01467544 (accessed 31 March 2014).
Zheng 2011 {published data only}
- ACTRN12611000810910. The effect of six weeks of tai ji practice on anxiety in healthy but stressed people compared to an exercise only comparison group. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=343090 (accessed 31 March 2014).
Additional references
ACSM 2010
- American College of Sports Medicine. ACSM's Resource Manual for Guidelines for Exercise Testing and Prescription. 6th Edition. Philadelphia: Wolters Kluwer Health/Lippincott Williams and Wilkins, 2010. [Google Scholar]
AHA 2011
- American Heart Association (AHA). Physical activity improves quality of life. www.heart.org/HEARTORG/GettingHealthy/Physical Activity/StartWalking/Physical‐activity‐improves‐quality‐of‐life_UCM_307977_Article.jsp (accessed 31 March 2014).
Bahrke 1978
- Bahrke MS, Morgan WP. Anxiety reduction following exercise and meditation. Cognitive Therapy and Research 1978;2:323‐34. [Google Scholar]
Castillo‐Richmond 2000
- Castillo‐Richmond A, Schneider RH, Alexander CN, Cook R, Myers H, Nidich S, et al. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke 2000;31:568‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dalusung‐Angosta 2011
- Dalusung‐Angosta A. The impact of tai chi exercise on coronary heart disease: a systematic review. Journal of the American Academy of Nurse Practitioners 2011;23(7):376‐81. [DOI] [PubMed] [Google Scholar]
Duncan 2001
- Duncan TE, Duncan SC, Chaumeton N, Fisher KJ. An evaluation of the effects of tai chi exercise on physical function among older persons: a randomized controlled trial. Annals of Behavioral Medicine 2001;23(2):139‐46. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ernst 2008
- Ernst E, Pittler MH, Wider B, Boddy K. Oxford Handbook of Complementary Medicine. Oxford: Oxford University Press, 2008. [Google Scholar]
Frishman 2005
- Frishman WH, Weintraub MI, Micozzi MS. Complementary and Integrative Therapies for Cardiovascular Disease. St Louis, MO: Elsevier/Mosby, 2005. [Google Scholar]
Han 2004
- Han A, Judd M, Welch V, Wu T, Tugwell P, Wells GA. Tai Chi for treating rheumatoid arthritis. Cochrane Database of Systematic Reviews 2004, Issue 3. [DOI: 10.1002/14651858.CD004849] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). The Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hong 2008
- Hong Y. Tai Chi Chuan: State of the Art in International Research. New York: Karger, 2008. [Google Scholar]
Lee 2007a
- Lee MS, Pittler MH, Taylor‐Piliae RE, Ernst E. Tai chi for cardiovascular disease and its risk factors: a systematic review. Journal of Hypertension 2007;25(9):1974‐5. [DOI] [PubMed] [Google Scholar]
Lee 2007b
- Lee MS, Pittler MH, Ernst E. Is tai chi an effective adjunct in cancer care? A systematic review of controlled clinical trials. Supportive Care in Cancer 2007;15:597‐601. [DOI] [PubMed] [Google Scholar]
Lee 2008a
- Lee MS, Pittler MH, Ernst E. Tai chi for osteoarthritis: a systematic review. Clinical Rheumatology 2008;27:211‐8. [DOI] [PubMed] [Google Scholar]
Lee 2008b
- Lee MS, Pittler MH, Kim MS, Ernst E. Tai chi for type 2 diabetes: a systematic review. Diabetic Medicine 2008;25:240‐1. [DOI] [PubMed] [Google Scholar]
Lee 2010
- Lee MS, Lee EN, Kim JI, Ernst E. Tai chi for lowering resting blood pressure in the elderly: a systematic review. Journal of Evaluation in Clinical Practice 2010;16:818‐24. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Li 2001a
- Li Y. Fitness function and principles of tai chi. Journal of Liaoning College of Traditional Chinese Medicine 2001;3:82‐3. [Google Scholar]
Li 2001b
- Li JY, Hong Y, Chan KM. Tai chi: physiological characteristics and beneficial effects on health. British Journal of Sports Medicine 2001;35:148‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mittal 2008
- Mittal S. The Metabolic Syndrome in Clinical Practice. London: Springer, 2008. [Google Scholar]
Nüesch 2010
- Nüesch E, Trelle S, Reichenbach S, Rutjes AW, Tschannen B, Altman DG, et al. Small study effects in meta‐analyses of osteoarthritis trials: meta‐epidemiological study. BMJ 2010;341:c3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rainforth 2007
- Rainforth MV, Schneider RH, Nidich SI, Gaylord‐King C, Salerno JW, Anderson JW. Stress reduction programs in patients with elevated blood pressure: a systematic review and meta‐analysis. Current Hypertension Reports 2007;9(6):520‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2000
- Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta‐analysis: power of statistical tests and prevalence in the literature. Journal of Clinical Epidemiology 2000;53:1119‐29. [DOI] [PubMed] [Google Scholar]
Sterne 2001
- Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta‐analysis. BMJ 2001;323:101‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsang 2008
- Tsang T, Orr R, Lam P, Comino E, Singh MF. Effects of tai chi on glucose homeostasis and insulin sensitivity in older adults with type 2 diabetes: a randomised double‐blind sham‐exercise ‐controlled trial. Age and Ageing 2008;37(1):64‐71. [DOI] [PubMed] [Google Scholar]
Tse 1991
- Tse S, Bailey DM. T'ai chi and postural control in the well elderly. American Journal of Occupational Therapy 1991;29:263‐88. [DOI] [PubMed] [Google Scholar]
USHHS 1996
- US Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, 1996. [Google Scholar]
Verhagen 2004
- Verhagen AP, Immink M, Meulen, Bierma‐Zeinstra SM. The efficacy of tai chi chuan in older adults: a systematic review. Family Practice 2004;21(1):107‐13. [DOI] [PubMed] [Google Scholar]
WHO 2013
- World Health Organization. Media centre: cardiovascular diseases (CVDs). www.who.int/mediacentre/factsheets/fs317/en/index.html (accessed 31 March 2014).
Wolf 1996
- Wolf SL. Reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. Atlanta FICSIT Group. Frailty and injuries: cooperative studies of intervention techniques. Journal of the American Geriatrics Society 1996;44(5):498‐506. [DOI] [PubMed] [Google Scholar]
Yeh 2008
- Yeh GY, Wang C, Wayne PM, Phillips RS. The effect of tai chi exercise on blood pressure: a systematic review. Preventive Cardiology 2008;11(2):82‐9. [DOI] [PubMed] [Google Scholar]
Yeh 2009
- Yeh GY, Wang C, Wayne PM, Phillips R. Tai chi exercise for patients with cardiovascular conditions and risk factors: a systematic review. Journal of Cardiopulmonary Rehabilitation and Prevention 2009;29:152‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhou 1984
- Zhou D, Shephard RJ, Phyley MJ, Davis GM. Cardiorespiratory and metabolic responses during tai chi chuan exercise. Canadian Journal of Applied Sport Sciences 1984;9:7‐10. [PubMed] [Google Scholar]
Zhou 2012
- Zhou J, Zhang L, Liu H, Mallampati T, Xu M, Yang J. Tai Chi for type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD009717] [DOI] [Google Scholar]


