To the Editor: Endoscopic retrograde cholangiopancreatography (ERCP) is strongly recommended for stone removal of choledocholithiasis. But there is still risk of complications such as post-ERCP cholangitis (PEC) and post-ERCP pancreatitis (PEP). Biliary drainage including endoscopic nasobiliary drainage (ENBD) and biliary stent is considered to reduce the occurrence of PEC and PEP. However, the ENBD tube will cause patient discomfort, and some patients may extract the tube by themselves. Furthermore, additional endoscopic stent removal is required after insertion of conventional biliary stent for short-term biliary drainage, increasing medical costs.
Therefore, we have developed a biliary spontaneous dislodgement spiral stent (BSDSS), which was made of thermoplastic polyurethane and can be dislodged and evacuated spontaneously after short-term biliary drainage [Figure 1].[1] Patients with common bile duct (CBD) stones from August 2018 to July 2020 at West China Hospital were consecutively prospectively enrolled. Its protocol was approved by the Chinese Ethics Committee of Registering Clinical Trials (No. ChiECRCT-20180104). It was registered at the Chinese Clinical Trial Registry (www.chictr.org.cn, ChiCTR180-0017387). Inclusion and exclusion criteria are shown in Supplementary Table 1, http://links.lww.com/CM9/B968. Informed consent was obtained from all patients included in this study. Eligible patients were 1:1 randomly assigned to the BSDSS group (inserting a BSDSS after complete stone removal for biliary drainage) or the control group (pulling back the endoscope directly after complete stone removal). Sealed envelopes with a serial number were used during the study period. After complete stone removal was confirmed, an envelope was serially selected to determine the group allocation. Blinding of the patients was not possible since they needed to confirm BSDSS dislodgement. Blinding of the endoscopists was also not possible since they needed to insert the BSDSS. Statistician was blinded to group allocation.
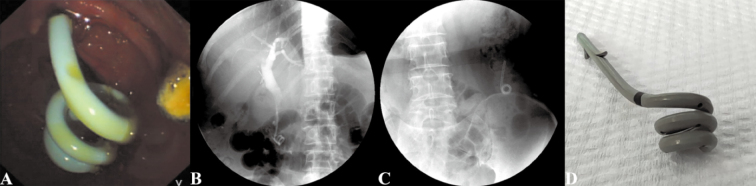
Figure 1.
Biliary spontaneous dislodgement spiral stent for short-term biliary drainage after complete stone removal. (A) The stent in situ under endoscopy. (B) The stent in situ under X-ray. (C) The stent dislodged to the bowel lumen under X-ray. (D) The stent expelled from the body.
All ERCP procedures were performed by one of the four experienced endoscopists (≥300 ERCPs per year) using a standard duodenoscope (TJF-260 V; Olympus, Tokyo, Honshu, Japan). After successful selective bile duct cannulation, cholangiography was performed by injecting 25% iohexol solution through the contrast catheter (PR-104Q-1; Olympus) to assess the common bile duct diameter and confirm the stone location, number, and size. Endoscopists chose papillary sphincterotomy (KD-V411M-0730; Olympus) for endoscopic sphincterotomy (EST), papillary balloon dilation (M00558400; Boston Scientific Corporation, Marlborough, Massachusetts, USA) for endoscopic papillary balloon dilation (EPBD), or a combination of both. The length of the EST was medium (about two-thirds of the full EST) or minimum (less than one-third of the full EST). As for EPBD, the extent of balloon dilation was less than 10 mm. The balloon was inflated slowly under endoscopy and was deflated immediately after the disappearance of the balloon waist. If ncessary, mechanical lithotripter (M00510890; Boston Scientific Corporation) was used for mechanical lithotripsy (ML) to assist stone extraction. Then, a stone-removal basket (FG-22Q-1; Olympus) or a stone-removal balloon (BV232P-A; Olympus) was used for stone extraction and bile duct cleaning. After stone removal, cholangiography was performed again for confirmation. After at least two endoscopists agreed that the stone was completely removed, the research assistant opened the envelope with group allocation.
In the BSDSS group, the BSDSS with 7 Fr in outer diameter was inserted for biliary drainage. Under the guidance of the guidewire, the endoscopist used a conveyer to place the BSDSS into the CBD and released the spiral stent under the radiation, ensuring that the spiral structure of the BSDSS was in the duodenum. The position of the BSDSS can be adjusted using conveyer or endoclip when necessary. In the control group, the endoscopist directly pulled back the endoscope after confirmation of complete stone removal.
The primary outcome was PEC. PEC was defined as fever (>38°C), hyperleukocytosis, and signs of cholestasis after ERCP. The severity grading criteria of PEC were referenced to the Tokyo Guidelines 2018. The secondary outcome included PEP, bleeding, perforation, BSDSS-related complications, postoperative hospital stays, and medical expenses. PEP was defined as persistent abdominal pain and elevation of blood amylase or lipase to more than three times the upper limit of normal after ERCP. The severity grading criteria of PEP were referenced to the Atlanta Guidelines 2012. Intraoperative bleeding was defined as bleeding after EST, EPBD, or stone removal and requiring additional hemostasis such as endoscopic clipping. Postoperative bleeding was defined as occurrence of hematemesis, melena, with or without hypovolemia after ERCP. Postoperative bleeding was classified into mild (bleeding stopped spontaneously after drug treatment), moderate (need for blood transfusion and hemostasis by endoscopy), and severe (need for vascular intervention or surgery). Perforation was identified by the occurrence of unexplained abdominal pain in patients during or after ERCP, with the detection of diaphragmatic or retroperitoneal gas on X-ray or CT images. Perforations resulting from BSDSS dislodgement were excluded from this definition. BSDSS-related complications include BSDSS retention, BSDSS related perforation, etc.
Statistical analysis was performed using SPSS 25.0 software (IBM Corp.; New York, USA). Student t-test, Mann Whitney U test, Chi-square test, or Fisher’s exact probability test was used for comparison between groups accordingly. P-value less than 0.05 was considered statistically significant.
A total of 1444 patients with CBD stones were enrolled during the study period. Finally, a total of 166 patients participated in randomization, including 83 patients in the BSDSS group and 83 patients in the control group [Supplementary Figure 1, http://links.lww.com/CM9/B968]. Comparisons of patient characteristics and ERCP procedures between groups are, respectively, shown in Supplementary Tables 2 and 3, http://links.lww.com/CM9/B968, and there were no significant differences in these characteristics.
PEC was noted in seven patients of the control group (8%), and there was no PEC in the BSDSS group (0). The difference between the two groups was statistically significant (P = 0.014) [Supplementary Table 4, http://links.lww.com/CM9/B968]. All patients with PEC in the control group were graded as mild and were treated by intravenous antibiotics. The number of patients needed to be treated was 12.
There were 4 patients (5%) with PEP in the BSDSS group and 12 patients (14%) with PEP in the control group. There was significant difference in the incidence of PEP between the two groups (P = 0.035) [Supplementary Table 4, http://links.lww.com/CM9/B968]. All patients with PEP were mild and were controlled by fluid infusion and anti-inflammatory therapy. The number of patients needed to be treated to prevent PEP was 10.
As for bleeding and perforation, there were no significant differences between the BSDSS group and the control group. All 15 patients (8 in the BSDSS group and 7 in the control group) with intraoperative bleeding were treated endoscopically. Postoperative bleeding was recorded only in one patient of the BSDSS group, which was mild and treated with conservative treatment, requiring no further endoscopic treatment nor blood transfusion. There was no perforation in the two groups.
BSDSS was dislodged and evacuated spontaneously in all patients of the BSDSS group, without BSDSS retention or BSDSS-related bowel injury. BSDSS evacuation was confirmed at the time of defecation in 60 patients, with a median duration of 4 (inter quartile range [IQR] = 2) days. The other 23 patients did not notice BSDSS evacuation, but that was confirmed by abdominal X-ray during follow-up.
The median post-ERCP hospital stay was 4 days (IQR = 3) in the BSDSS group and 3 days (IQR = 2) in the control group, without significant difference (P = 0.184). In terms of medical expenses, there was also no significant difference between the BSDSS group (RMB 22.6 thousand yuan, IQR = 14.3) and the control group (RMB 22.6 thousand yuan, IQR = 13.9), (P = 0.954).
This single-center, prospective, and randomized controlled study showed that placement of BSDSS after complete stone removal in patients with CBD stones significantly reduced the incidence of PEC and PEP, without additional complications and medical costs. These results confirm the necessity, efficacy, and safety of temporary biliary drainage with BSDSS after complete stone removal.
Previous studies suggested that temporary biliary drainage not only reduced the possibility of bile entering the pancreatic duct by reducing the bile duct pressure, but also avoided biliary and pancreatic obstruction caused by residual debris, thereby reducing the risk of PEP.[2] Compared to patient discomfort with the ENBD tube, and additional endoscopic stent removal of conventional stent, BSDSS can dislodge spontaneously requiring no additional endoscopy. Besides, compared with the conventional stent, the spiral part and the soft material of the BSDSS help reduce stent-related complications. The price of BSDSS is also comparable to that of conventional stents. Therefore, routine placement of BSDSS for preventing PEC and PEP is efficient and necessary, especially for patients with high risk of PEC and PEP. The difference in the incidence of cholangitis and pancreatitis between our cohort and previous studies may be related to the demographic characteristics of the cohort, endoscopist experience, and other factors. As for subtle differences of auxiliary stone-removal methods between two groups, it may not have an effect on outcomes based on previous literature.[3] There are some limitations in the study. As for a single-center clinical study, a multicenter study with large sample size is required to further evaluate the BSDSS. Due to the blank control group, the study of comparison of BSDSS and routine therapy should be carried out. Finally, the lack of long-term follow-up for stone recurrence, comparison with other biliary stent, and details of ERCP such as difficult cannulation are also limitations.
In conclusion, placement of BSDSS after complete stone removal in patients with choledocholithiasis can significantly reduce PEC and PEP, without extract hospital stay or medical cost. BSDSS should be routinely inserted, especially for patients with high risk of PEC and PEP. Future multicenter studies are warranted to confirm this conclusion.
Funding
We acknowledge the funding support from the National Natural Science Foundation of China (No. 82003156), 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (Nos. 2020HXFH016 and 2020HXFH040), Med-X Innovation Programme of Med-X Center for Materials, Sichuan University (No. MCM202302) and West China Nursing Discipline Development Special Fund Project, Sichuan University (No. HXHL21029).
Conflicts of interest
None.
Supplementary Material
Footnotes
Liansong Ye and Lifan Zhang contributed equally to this work.
How to cite this article: Ye LS, Zhang LF, Mou Y, Yuan XL, Liu W, Wu CC, Luo YH, Du J, Bai S, Xie J, Zhang QY, Tan QH, Liu L, Hu B. Biliary spontaneous dislodgement spiral stent for short-term biliary drainage in patients undergoing complete stone removal: A randomized controlled study. Chin Med J 2024;137:1363–1365. doi: 10.1097/CM9.0000000000003089
References
- 1.Ye LS Yuan XL Wu CC Liu W Du J Yao MH, et al. Biliary spontaneous dislodgement spiral stent for patients who underwent mechanical lithotripsy. World J Gastroenterol 2020;26:740–748. doi: 10.3748/wjg.v26.i7.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang J, Peng J, Pang E, Chen W. Efficacy of endoscopic nasobiliary drainage for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis and cholangitis after repeated clearance of common bile duct stones: Experience from a Chinese center. Dig Endosc 2013;25:453–458. doi: 10.1111/den.12013. [DOI] [PubMed] [Google Scholar]
- 3.Liu Y Su P Lin S Xiao K Chen P An S, et al. Endoscopic papillary balloon dilatation versus endoscopic sphincterotomy in the treatment for choledocholithiasis: A meta-analysis. J Gastroenterol Hepatol 2012;27:464–471. doi: 10.1111/j.1440-1746.2011.06912.x. [DOI] [PubMed] [Google Scholar]