Dear Editor,
Interscalene block, though widely used for shoulder surgeries, is associated with adverse effects.[1,2] The adverse effect may be mitigated by low volume and low concentration of local anaesthetic, but it limits the block duration.[3] Recently, erector spinae plane block (ESPB) has been favourable in shoulder surgery and partially qualifies as a phrenic-sparing block with effective analgesia for shoulder surgery.[4,5] Also, the shoulder is innervated by the C5–C6 nerve roots; hence, blocking it would provide postoperative analgesia after shoulder surgeries. We hypothesised that this combination of blocks would provide equivocal analgesia to a conventional interscalene block and have fewer adverse events (e.g., hoarseness of voice, Horner's syndrome, difficulty in breathing, and phrenic nerve involvement).
After approval of the ethical committee (Poona Medical Research Foundation, vide approval number RHC/BIOPMRF/EC/2020/256 dated 14 December 2020), 13 American Society of Anesthesiologists physical status I and II patients aged 18–65 years, undergoing major shoulder surgery under general anaesthesia were included. C5–C6 block was given using 7 ml of 0.375% ropivacaine at the start of surgery. All patients were then administered general anaesthesia with intravenous propofol 2 mg/kg, fentanyl 2 µg/kg, rocuronium 0.8 mg/kg and maintained on sevoflurane (minimum alveolar concentration 0.8–1). Multimodal analgesia was provided with intravenous paracetamol 1 g and diclofenac 75 mg. At the end of the surgery, an ultrasound-guided thoracic ESPB was performed at level T2, depositing 15 ml of 0.375% ropivacaine [Figure 1]. The spread of local anaesthetic was appreciated at the level of costotransverse junction in the axial plane, and the cephalon–caudad diffusion was noted. Diaphragm excursion was assessed before by a curvilinear probe – M mode) (Venue Go R2; GE, WI, USA) and 20 min after the blocks were instituted. Hemidiaphragmatic paralysis was considered if there was more than a 50% reduction in an excursion on deep breathing. A positive sniff test (a paradoxical diaphragm movement on asking the patient to sniff) was considered complete hemidiaphragmatic palsy.
Figure 1.
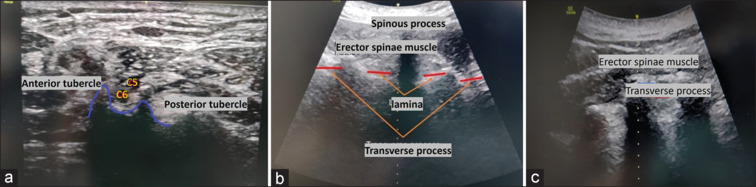
Sonoanatomy of cervical ventral rami and second thoracic vertebra. (a) Anterior and posterior tubercle of the sixth cervical vertebra seen with the cervical ventral rami five and six (C5–C6); (b) transverse view at the second thoracic vertebra; (c) paramedian sagittal image at the second thoracic vertebra
Five patients were female, while eight were male. Rescue analgesia with intravenous tramadol 50 mg was administered if the Visual Analogue Scale (VAS) score was more than or equal to 3; it was required by five patients once in 24 hours h (at 12, 13, 14, 16 and 18 hours) and one patient needed two rescue analgesics. The median duration of surgery was 140 min [range 130–150, interquartile range (IQR) 142.5–132.5 min]. VAS scores observed till 12 hours h was 0, whereas at 12, 18 and 24 hours, the median (IQR) was 0 (1–0), 2 (2.5–0.5) and 1.5 (2.5–1), respectively. The phrenic nerve was visualised in eight patients, near the C5–6 ventral rami in two of these patients. One of these patients reported hoarseness of voice. Diaphragm involvement was noted [Table 1].
Table 1.
Ultrasonography assessment of the diaphragm
| Number of patients | Diaphragm assessment 20 min after cervical 5 and 6 ventral rami block | Diaphragm assessment half an hour after extubation | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Quiet breathing | Deep breathing | Sniff test | Quiet breathing | Deep breathing | Sniff test | |
| 6 | No | No | Negative | No | No | Negative |
| 1 | No | No | Negative | No | <50% | Negative |
| 4 | No | <50% | Negative | No | <50% | Negative |
| 1 | No | < 50% | Negative | Yes | >50% | Positive |
| 1 | No | <50% | Negative | No | >50% | Positive |
Fredrickson et al.[3] elicited a direct correlation between the volume and concentration of the local anaesthetic with the duration of the interscalene block and is crucial in advocating a specific regional technique.[6] Few case reports have documented the use of cervical ESPB for shoulder surgery, and various case reports have observed that the local anaesthetic deposited at the T2–T3 level provided effective analgesia for shoulder surgery.[4] Ciftci et al.[7] studied ESPB for shoulder surgery in 60 patients and noted a reduction in VAS score and fewer rescue analgesics. A cephalad-directed, cervical ESPB injection at the first costotransverse junction showed a consistent effect on the dorsal spinal nerves of the thoracic and cervical areas, with spread noted in the paravertebral space dorsal to ventral roots.[4] In our series, the administration of two blocks (compounding) did not allow segregation of analgesia for either block. The cephalocaudal spread of the drug in the erector spinae plane could not be appreciated accurately without imaging or dye studies to advocate a particular pain relief modality. The low-volume C5–6 root block showed a lower incidence of phrenic nerve palsy than interscalene block and longer duration analgesia. Combining various site-specific blocks aids in lowering doses, limiting adverse events and giving an equivocal or longer duration of analgesia, and it may warrant further comparative studies.
Financial support and sponsorship
Ruby Hall Clinic, Pune.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Dr Abhay Kulkarni at Ruby Hall Clinic is acknowledged for trusting us with the care of his patients.
REFERENCES
- 1.Ayyanagouda B, Hosalli V, Kaur P, Ambi U, Hulkund SY. Hemi-diaphragmatic paresis following extrafascial versus conventional intrafascial approach for interscalene brachial plexus block: A double-blind randomised, controlled trial. Indian J Anaesth. 2019;63:375–81. doi: 10.4103/ija.IJA_69_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verelst P, van Zundert A. Respiratory impact of analgesic strategies for shoulder surgery. Reg Anesth Pain Med. 2013;38:50–3. doi: 10.1097/AAP.0b013e318272195d. [DOI] [PubMed] [Google Scholar]
- 3.Fredrickson MJ, Abeysekera A, White R. Randomised study of the effect of local anesthetic volume and concentration on the duration of peripheral nerve blockade. Reg Anesth Pain Med. 2012;37:495–501. doi: 10.1097/AAP.0b013e3182580fd0. [DOI] [PubMed] [Google Scholar]
- 4.Diwan S, Nair A. Erector spinae plane block for proximal shoulder surgery: A phrenic nerve sparing block! Turk J Anaesthesiol Reanim. 2020;48:331–3. doi: 10.5152/TJAR.2019.55047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Selvi O, Tulgar S, Ozer Z. Case report presentation of ultrasound-guided erector spinae plane block in shoulder surgery: Three patients and two different results. Cureus. 2018;10:e3538. doi: 10.7759/cureus.3538. doi: 10.7759/cureus. 3538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sivashanmugam T, Sripriya R, Jayaraman G, Ravindran C, Ravishankar M. Truncal injection brachial plexus block: A Description of a novel injection technique and dose finding study. Indian J Anaesth. 2020;64:415–21. doi: 10.4103/ija.IJA_803_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ciftci B, Ekinci M, Gölboyu BE, Kapukaya F, Atalay YO, Kuyucu E, et al. High thoracic erector spinae plane block for arthroscopic shoulder surgery: A randomised prospective double-blind study. Pain Med. 2021;22(Suppl 4):776–83. doi: 10.1093/pm/pnaa359. [DOI] [PubMed] [Google Scholar]


