Abstract
Objective
This study evaluates regularization variants in logistic regression (L1, L2, ElasticNet, Adaptive L1, Adaptive ElasticNet, Broken adaptive ridge [BAR], and Iterative hard thresholding [IHT]) for discrimination and calibration performance, focusing on both internal and external validation.
Materials and Methods
We use data from 5 US claims and electronic health record databases and develop models for various outcomes in a major depressive disorder patient population. We externally validate all models in the other databases. We use a train-test split of 75%/25% and evaluate performance with discrimination and calibration. Statistical analysis for difference in performance uses Friedman’s test and critical difference diagrams.
Results
Of the 840 models we develop, L1 and ElasticNet emerge as superior in both internal and external discrimination, with a notable AUC difference. BAR and IHT show the best internal calibration, without a clear external calibration leader. ElasticNet typically has larger model sizes than L1. Methods like IHT and BAR, while slightly less discriminative, significantly reduce model complexity.
Conclusion
L1 and ElasticNet offer the best discriminative performance in logistic regression for healthcare predictions, maintaining robustness across validations. For simpler, more interpretable models, L0-based methods (IHT and BAR) are advantageous, providing greater parsimony and calibration with fewer features. This study aids in selecting suitable regularization techniques for healthcare prediction models, balancing performance, complexity, and interpretability.
Keywords: logistic regression, electronic health records, regularization, discrimination, calibration
Introduction
A recent review of the use of clinical prediction models finds that in recent years 67% of studies use some kind of regression analysis.1 One common issue when developing clinical prediction models is the susceptibility to overfitting. Overfitting occurs when a model is overly complex such that it near perfectly fits the training data but is unable to generalize to new data. A common method to reduce overfitting when training regression models involves adding a regularization term to the model’s objective function. The regularization term adds a cost that aims to minimize model complexity. This is known as regularization. Studies on large observational health data commonly use L1 regularized logistic regression, otherwise known as Least Absolute Shrinkage and Selection Operator (LASSO) for its feature selection capabilities and good discriminative performance.2 As machine learning methods are advancing, pipelines to develop clinical prediction models, that work directly on large observational healthcare data (insurance claims and electronic healthcare records), are being developed. These pipelines develop models efficiently and improve model transparency. A recent study highlighting the use of a standardized analytical pipeline on observational health-data mapped to the Observational Health Data Sciences and Informatics (OHDSI) common data model (CDM) shows that logistic regression with LASSO often outperforms other machine learning models when externally validating the developed model.3 External validation is when the model is validated on a different dataset than it was trained on. It is common for developed models to have a drop in performance when transported to a different dataset and one of the outstanding issues in developing prediction models on observational data is to develop more generalizable models which do not suffer from this drop.4
LASSO regularization is a method developed at the end of the last century. It has enjoyed great success due to its interpretability and scalability5 and has been heavily used since its inception. Despite its success it has some limitations, especially regarding its feature selection capabilities. These limitations have led researchers to develop numerous other variants with differing theoretical properties. One such limitation is that if there is a group of features in the data with high pairwise correlations within the group, LASSO tends to select randomly one of the features as a representative of the whole group and push the rest to zero.6 Correlations between features are common when using standardized analytical pipelines in healthcare due to comorbidities and coding redundancies. Another limitation is that the LASSO feature selection is unstable unless specific conditions are met which rarely happens in practice.7 This means that the covariates selected will change drastically with minor changes in the data distribution. In practice this means that fitting models with LASSO regularization for example on different folds during cross validation can result in models selecting different features. Further there is an issue of false positives among the selected features. While LASSO is highly likely to select the relevant features, this is at the cost of features that are not relevant but end up in the model.8 This is worse when there is high collinearity among the features as is common in observational health data.9
To address these issues several variants of the LASSO have been developed. LASSO regularization incorporates an L1 penalty into a model’s objective function by considering the absolute value of the coefficients’ magnitude. This leads some coefficients to be pushed to precisely zero selecting some features while discarding others. L2 regularization on the other hand, known as Ridge,10 introduces a penalty based on the squared magnitude of the coefficients. Unlike L1, L2 does not force any coefficient to become exactly zero and all features are included in the final model. One of the first variants introduced to improve the LASSO was ElasticNet6 which use a mixture of L1 and L2 penalty. This means that in the presence of groups of correlated features it will select the whole group while still maintaining its feature selection capacity. ElasticNet has been shown to be more stable in feature selection than LASSO.11 Another developed variant is the adaptive LASSO12 where each feature is adaptively penalized according to an estimation of its coefficient magnitude. This means larger coefficients are penalized less, which reduces bias, and smaller coefficients are penalized more which results in sparser (ie, selects less features) and more stable models where fewer false positive features are selected.13,14 A more recent adaptive variant is the broken adaptive ridge (BAR).15,16 This is a version where ridge regression is iteratively fitted and in each iteration the coefficients are penalized according to the inverse of the magnitude of their coefficient in the previous iteration, this is repeated until convergence. This variant has the desired property that it is an approximation for L0 regularization, which is equal to best subset selection where every possible combination of features is tried to select the best subset. Finally, another L0 approximation method is often used; iterative hard thresholding (IHT).17 IHT has the advantage that a maximum number of selected features can be specified which can be attractive in a clinical setting.
In this study, we empirically examine these different regularization variants and investigate their discrimination and calibration performance both when evaluated on the same dataset as they are developed on (internal validation) and on a different dataset (external validation) and compare to the LASSO.
Methods
Data source
We use 5 US claims and electronic health record (EHR) databases (Table 1). We develop our models on 1 database and externally validate on the other 4, then repeat for all databases as the development database. The 5 databases in this study contain retrospectively collected deidentified patient healthcare data. The use of IBM and Optum databases were reviewed by the New England Institutional Review Board (IRB) and were determined to be exempt from broad IRB approval.
Table 1.
Overview of data sources used in the study.
| Name | Type | Description | Start | End | Size (million lives) |
|---|---|---|---|---|---|
| IBM® MarketScan® Commercial Claims and Encounters (CCAE) | US Claims | Patients aged 65 or younger. Employees who receive health insurance through their employer and their dependents | January 01, 2000 | July 31, 2021 | 152 |
| IBM® MarketScan® Medicare Supplemental (MDCR) | US Claims | Patients aged 65 or older with supplemental healthcare | January 01, 2000 | July 31, 2021 | 10 |
| IBM® MarketScan® Medicaid (MDCD) | US Claims | Patients with government subsidized healthcare | January 01, 2006 | May 31, 2021 | 33 |
| Optum® de-identified Electronic Health Record Dataset (Optum EHR) | US EHR | Patients of all ages | January 01, 2007 | December 31, 2021 | 106 |
| Optum® De-Identified Clinformatics® Data Mart Database (Clinformatics®) | US Claims | Patients of all ages | May 01, 2000 | March 31, 2022 | 93 |
All datasets used in this paper were mapped into the OHDSI Observational Medical Outcomes Partnership Common Data Model (OMOP-CDM) version 5.18 The OMOP-CDM was developed to enable researchers with diverse datasets to have a standard database structure and vocabulary. This enables analysis code and software to be shared among researchers and across data sources which facilitates external validation of prediction models.
Study population
The target population consists of patients with pharmaceutically treated major depressive disorder (MDD) and the index date is their first diagnosis of MDD. We use individual patient features from an observation window of 1 year prior to index, and attempt to predict 21 different outcomes from 1 day to 1 year after the index date (See Figure 1). These are the same prediction problems as have been used previously.20 The outcomes are acute liver injury, acute myocardial infarction, alopecia, constipation, decreased libido, delirium, diarrhea, fracture, gastrointestinal hemorrhage, hyponatremia, hypotension, hypothyroidism, insomnia, nausea, seizure, stroke, sudden cardiac death, suicide and suicidal ideation, tinnitus, ventricular arrhythmia, and vertigo.
Figure 1.
A patient level prediction problem. Conditions, drugs, procedures, and observations from an observation window prior to an index date are used to predict the outcome during a time-at-risk after index. Reproduced from John et al19 with permission from BMC Medical Research Methodology.
Features
The individual patient features included are continuous age at index, sex, conditions, drug ingredients, procedures, and observations. These are all extracted from an observation window of 1 year prior to the index date. Conditions, drug ingredients, procedures, and observations are extracted as binary indicator variables with the value 1 indicating the presence of the feature in the observation window. In the context of the OMOP-CDM, conditions indicate the presence of a disease, sign or symptom, either observed by the healthcare provider or reported by the patient. Drug codes indicate exposures to drugs and are combined under the active ingredient to reduce feature dimensionality. Procedures are activities or processes carried out by the healthcare provider and observations are clinical facts about a patient not captured by other clinical tables in the CDM.
As the features represent whether a patient has a condition/drug/procedure/observation record in the year prior to their prediction index, the values are never missing (0 = no record, 1 = record present). However, we do not impute missing records in the observational dataset, so in theory a patient may have a value of 0 for the feature “diabetes condition record in the prior year” but have diabetes unrecorded. Age is normalized by its max value in the training set and features rarer than 0.1% of observations are removed.
Further details about software used to extract features are in Supplementary Material.
Algorithms
We use 7 different prediction algorithms to develop our models. They are all integrated into the PatientLevelPrediction (version 5.4.5) R package (https://github.com/OHDSI/PatientLevelPrediction/) to facilitate ease of development and external validation on data from the OMOP-CDM. The following algorithms are used to develop models: LASSO,2 L2 penalized logistic regression (Ridge),10 L1/L2 penalized logistic regression (Elastic Net),6 adaptive L1 regularized logistic regression (Adaptive LASSO),12 adaptive L1/L2 penalized logistic regression (Adaptive ElasticNet), BAR,15 and IHT.17 Further details about software used for model development are in the Supplementary material.
We develop models using a train-test split of 75%/25%. Most algorithms use a 3-fold cross validation21 on the training set in combination with grid search to select the best hyperparameters, except for BAR-BIC and IHT-BIC which use the Bayesian information criteria (BIC). Algorithms that use Cyclops for model fitting (see Supplementary material) uses auto search instead of grid search to find the best hyperparameter.5 For all these algorithms the hyperparameters are the strength of the penalty. We also include a version of BAR that uses 3-fold cross validation and a simple grid search of 10 penalties, ranging from BIC to 0.1 * BIC, to select the best penalty based on the area-under-the-receiver-operating-characteristic curve (AUC). BAR and IHT require an initial fit of ridge regression which uses cross validation to find the optimal ridge regression penalty on the training set before refitting on the whole training set to get the initial regression coefficient estimates. Finally, all models are refit on the whole training set with fixed penalties set to the value from the hyperparameter search before internal validity is assessed on the test set. Since logistic regression models on this kind of data do not improve performance above around 3000 outcome events,18 if the training set includes more than 3000 events with a 75%-25% split the split was adjusted so the training set would only include 3000 events and the rest of the data would go to the test set to increase power in our performance estimates.
We use the AUC and the area under the precision-recall curve (AUPRC) to evaluate discriminative performance. The AUC is the most widely used and general metric to measure discrimination and does not depend on selecting a prediction threshold.22 AUPRC is another commonly used discrimination metric, particularly for rare outcomes.23 We evaluate calibration by computing the expected calibration error (ECE), also known as the E-avg.24 ECE measures the average difference of predicted versus expected risk in 10 equally spaced risk strata. We chose the ECE since we need a single metric for calibration that uses the whole range of risks. We develop the models on each database and then externally validate their performance on the other databases.
Statistical analysis
We use Friedman’s test to compare the performance of different algorithms.25 This is a non-parametric test that detects if the different algorithms are ranked differently to each other on the different prediction problems. If the null hypothesis is rejected for a difference in ranks between the algorithms, we proceed with a post-hoc test testing all pairwise differences controlling for multiplicity. We plot the results from the post-hoc test in a critical difference diagram which show the ranks of each algorithm with horizontal lines connecting algorithms that are not significantly different from each other (see Section 3.2.4 in Demsar25 for further details). We do this for discrimination and calibration. We then look at distributions of model sizes of each model and compare them to the achieved performance.
Results
Study population
Table 2 provides an overview of study population statistics across the 5 different data sources. The age distributions are quite different between databases. CCAE and MDCD have younger people while MDCR has older. Optum EHR and Clinformatics® are more spread in age.
Table 2.
Study population characteristics.
| CCAEb | MDCRc | MDCDd | Optum EHRe | Clinformatics®f | |
|---|---|---|---|---|---|
| Study population | 2 220 724 | 181 912 | 628 293 | 3 140 079 | 1 649 138 |
| Age (mean ± std) | 41.1 ± 14.9 | 74.9 ± 7.8 | 33.6 ± 17.0 | 47.6 ± 19.1 | 50.7 ± 20.3 |
| Sex (% male) | 31.3% | 32.8% | 27.4% | 30.9% | 32.5% |
| No. of eventsa (median, first, and third quartile) | 12 358 (4619-27 575) | 2363 (1736-5030) | 5584 (2798-12 291) | 17 624 (7627-46 724) | 14 257 (8944-39 265) |
| Candidate predictors | 42 219 | 29 548 | 36 697 | 72 254 | 47 254 |
We have 21 different prediction problems per database, each with different number of outcome events.
IBM® MarketScan® Commercial Claims and Encounter.
IBM® MarketScan® Medicare Supplemental.
IBM® MarketScan® Medicaid.
Optum® de-identified Electronic Health Record Dataset.
Optum® De-Identified Clinformatics® Data Mart Database.
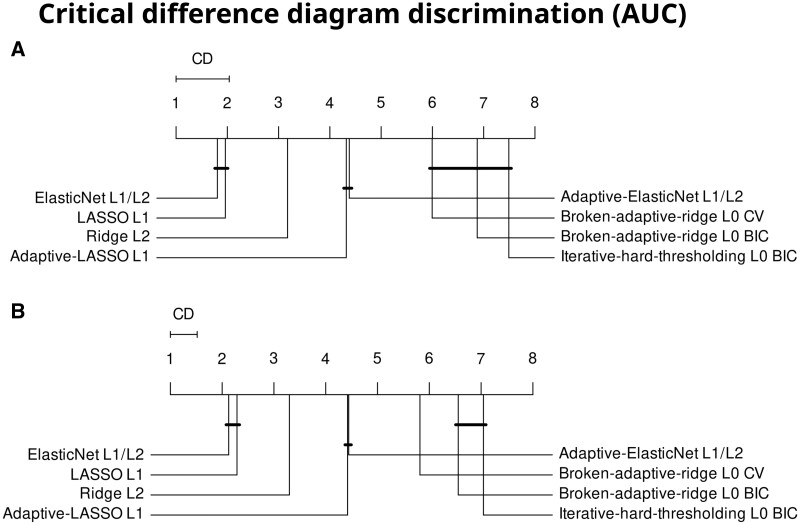
Discrimination
In total we develop 840 models across the 5 databases (7 different algorithms with 2 hyperparameter tuning strategies for 1; predicting 21 outcomes; in 5 databases: 8 × 21 × 5 = 840). The AUC on the test set between the different algorithms are significantly differently ranked (Q(7) = 555, P <.001). Figure 2A shows a critical difference diagram for the internal discrimination performance. The best ranked algorithms are the LASSO and ElasticNet with no statistically significant difference between their ranks. Ridge is in third place, then the adaptive LASSO and adaptive ElasticNet, then the L0-approximate methods, IHT, and BAR. The average AUC difference between the best and worst algorithm is 2.8% points. Practically this mean that when randomly selecting 1 person with and 1 without the outcome, the best algorithm will get the order correct (assign higher risk to person with outcome) on average 2.8% points more often than the worst algorithm. We then externally validate the 840 developed models across the other 4 databases resulting in 3360 external validations (840 models × 4 databases). We find that the external discrimination performance measured using AUCs is significantly different between the algorithms (Q(7) = 1678, P <.001). Figure 2B shows the critical difference diagram for the external discrimination performance. The ranks of algorithms are the same as during internal performance. LASSO and ElasticNet show the best performance while the approximate L0 methods rank last. The average difference between the best and worst algorithm is 2.8% points AUC. In Figure S1 results with the area under the precision-recall curve and in Tables S1 and S2 the ranks per each of the 21 outcomes are shown.
Figure 2.
(A) Critical difference diagram of the developed models ranked using internal AUC. (B) Critical difference diagram ranked using external AUC. The critical difference (CD) line indicates how big of a difference is needed to be significantly different. Solid lines connect algorithms with no significant difference between them. Abbreviations: BIC = Bayesian information criteria, CV = cross validation.
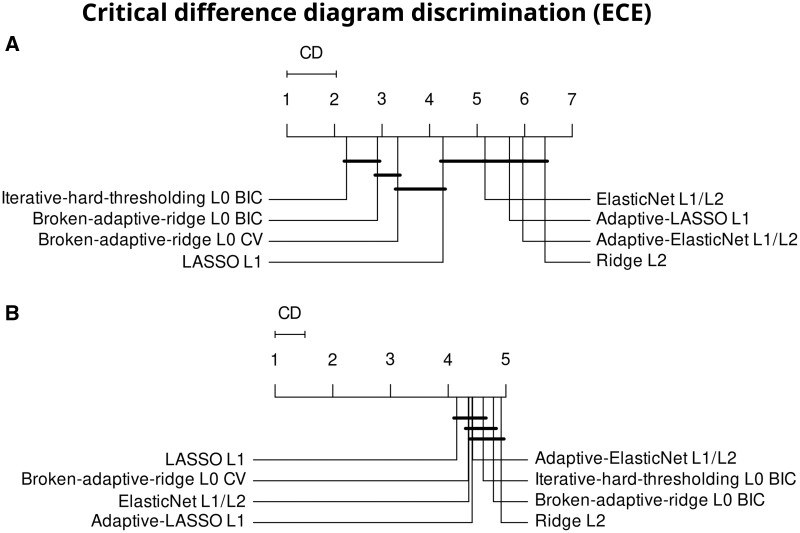
Calibration
Figure 3 shows the results for the ECE. The algorithms are ranked differently for internal calibration performance (Q(7)=286.7, P <.001). The approximate L0 methods, BAR, and IHT lead in calibration. The adaptive LASSO, adaptive ElasticNet, and Ridge regression rank worst. The magnitude of difference between the best and worst algorithm is small or only 0.001. Externally the algorithms rank differently (Q(7)=31, P <.001). However, there is more variation in the ranks, with all average ranks between 4 and 5, and the magnitude of difference between the best and worst algorithm is small or less than 0.001.
Figure 3.
Expected calibration error (ECE) ranked according to (A) internal and (B) external performance. Abbreviations: CD = critical difference, BIC = Bayesian information criteria, CV = cross validation.
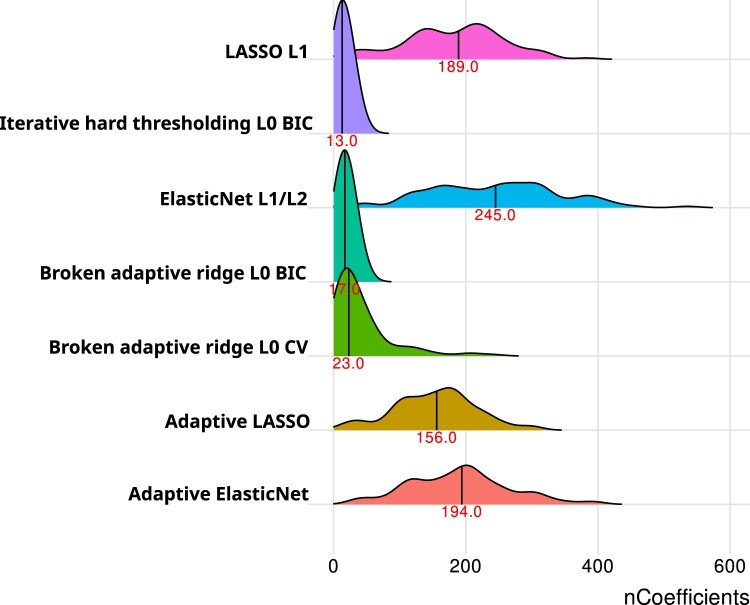
Model sizes
Figure 4 shows the model sizes. Ridge regression is not included since it always includes all features, and its average model size is 4013 coefficients. In Figure 4 while ElasticNet is equal in discriminative performance to LASSO it does so with larger model sizes. The 2 adaptive methods have slightly lower sizes than their non-adaptive counterparts. The BAR and IHT models have by far the smallest model sizes with an average of 17 and 13 coefficients in the model, respectively. When we used CV instead of BIC to determine penalty results we found slightly higher median model size for BAR as well as a longer tail towards higher model sizes.
Figure 4.
Distributions of model sizes for the 840 developed models. The vertical line and red number represent the median model size. Abbreviations: BIC = Bayesian information criteria, CV = cross validation.
Discussion
This empirical study helps researchers developing models choose whether to pick a regularization technique that maximizes discriminative performance (ie, use LASSO or ElasticNet) or whether they would be happy to achieve a slightly less discriminative model that requires fewer features and is therefore easier to understand and implement (ie, use IHT or BAR). Most researchers tend to use ridge, LASSO, or ElasticNet as regularization techniques, but our results empirically investigate the impact of regularization technique across 21 prediction problems and 5 databases. These results now provide guidance into the impact of regularization choice on discrimination, calibration, and model parsimony.
Our results show that logistic regression with the LASSO and ElasticNet regularization techniques lead to improved discrimination over the other techniques investigated. This discrimination remains consistent between the internal performance and external performance. However, the approximate L0 based techniques lead to improved parsimony and internal calibration. Internal and external calibration patterns differed, where internally IHT and BAR have better calibration but externally it was harder to see a superior technique, although LASSO and BAR tend to be slightly better calibrated. Overall, our results stand consistent with prior theoretical work, that shows L0 techniques lead to improved parsimony and calibration.26 One novel insight is that the improvement in calibration of the L0 techniques does not hold when models are externally validated.
If model discrimination is the only important criterion for a model developer using logistic regression, then the developer would likely want to pick either ElasticNet or LASSO regularization. These 2 regularization techniques resulted in similar AUC across the prediction problems and the AUC was higher than alternative regularization techniques investigated. ElasticNet results in more features being included in the final model compared to LASSO, with medians of 245 and 189, respectively. Therefore, if model discrimination is very important, but the developer still has some constraint on model complexity, the developer may prefer LASSO over ElasticNet. Implementing such a model with a few hundred features would not be feasible manually, but it could be implemented as part of an EHR system.
If a researcher developing models knows that implementing a model with hundreds of features would be difficult, for example if it requires manually inserting features into a form or they value understanding the model, then the researcher may prefer to use L0 based regularization such as IHT or BAR. A median of 13 and 17 features were required across the prediction task for IHT and BAR, respectively. This means these models would be simple to implement and clinicians would be able to understand the models more compared to the LASSO models that required a median of 189 features. Most developed models are not clinically implemented, and these simpler models could be an attractive choice for clinicians.27
While the ranks in discrimination are statistically significant and the average AUC difference is 2.8% points between best and worst algorithm, it is difficult to say what this means for a specific clinical use case. One tool to do such things is decision curve analysis where the gain to detecting one more true positive is compared to the cost of increased false positives.28 This requires selecting a threshold or range of thresholds which depend on the intended clinical use case or even preference of the patient. That is not possible at the large scale of comparisons done in this article.
Exploring the potential reasons behind the underperformance of adaptive LASSO and ElasticNet compared to their standard counterparts in our study, we identify several factors that might influence these findings. First, the initial coefficient estimates crucial for these methods are derived from ridge regression, which, while helpful in high-dimensional and collinear settings, introduces bias that could affect subsequent adaptive penalization. Despite utilizing a gamma value of one, as typically recommended, the possibility remains that an alternate gamma setting might yield better performance in our data context. Furthermore, the choice of using 3-fold cross-validation for determining the optimal penalization parameter was informed by prior studies focused on LASSO but could be suboptimal for adaptive methods. Future research could investigate some of these factors to improve model fitting performance with adaptive LASSO and ElasticNet in similar high-dimensional analyses.
Our study’s strengths include comparing multiple regularization techniques across 21 prediction problems and 5 databases. In addition, we investigated calibration, discrimination, and model parsimony both internally and externally. However, our study has some weaknesses. Firstly, we only investigated one target population and future work should expand this study to more target populations. Secondly, we focused on logistic regression, but the regularization techniques can be applied to different supervised learning methods and the results found for logistic regression may not generalize to other supervised learning methods. In future work it would be interesting to explore whether the results generalize to other supervised learning methods. We do not explore all possible penalties, we select penalties to investigate based on if they are commonly used in the literature and have performant implementations available suitable for our large scale comparison. Other penalties such as SLOPE or SCAD could be interesting to investigate as well in the future.29,30 Finally, we focused mostly on binary features and it is unknown whether the results would generalize to continuous features. However, most of the implemented clinical prediction models use binary features, such as Well’s criteria, CHA2DS2VASc, HAS-BLED, and Charlson comorbidity index.31–34
The literature shows that logistic regression is a common modelling technique used by researchers developing healthcare prediction models. When using big healthcare data to develop prediction models, a situation that is becoming more common, regularization is required to limit overfitting. Our large-scale empirical study can be used to guide researchers who need to select which regularization techniques to implement. If model parsimony and understanding is not important, that LASSO regularization is a good tradeoff between performance and number of features, but if model parsimony and understanding is important, then BAR often performs well while only including a manageable number of features.
Supplementary Material
Contributor Information
Egill A Fridgeirsson, Department of Medical Informatics, Erasmus University Medical Center, 3015 GD Rotterdam, The Netherlands.
Ross Williams, Department of Medical Informatics, Erasmus University Medical Center, 3015 GD Rotterdam, The Netherlands.
Peter Rijnbeek, Department of Medical Informatics, Erasmus University Medical Center, 3015 GD Rotterdam, The Netherlands.
Marc A Suchard, Department of Biostatistics, University of California, Los Angeles, Los Angeles, CA 90095-1772, United States; VA Informatics and Computing Infrastructure, United States Department of Veterans Affairs, Salt Lake City, UT 84148, United States.
Jenna M Reps, Department of Medical Informatics, Erasmus University Medical Center, 3015 GD Rotterdam, The Netherlands; Observational Health Data Analytics, Janssen Research and Development, Titusville, NJ 08560, United States.
Author contributions
Egill A. Fridgeirsson and Jenna M. Reps designed the study with input from Peter Rijnbeek and Marc A. Suchard. Egill A. Fridgeirsson performed the analysis and drafted the first version. All authors reviewed the results and the final manuscript.
Supplementary material
Supplementary material is available at Journal of the American Medical Informatics Association online.
Funding
This work was supported by the Innovative Medicines Initiative 2 Joint Undertaking (JU) grant agreement No 806968. The JU receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA.
Conflicts of interest
E.A.F. and P.R. work for a research group who received unconditional research grants from Boehringer-Ingelheim, GSK, Janssen Research & Development, Novartis, Pfizer, Yamanouchi, Servier. None of these grants result in a conflict of interest to the content of this paper. J.M.R. is an employee of Janssen R&D and shareholder of JNJ. M.A.S. receives contracts and grants from the US National Institutes of Health, the US Food & Drug Administration and Janssen Research & Development, all outside the scope of this work.
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals whose data was used in the study. Aggregated data to support the findings of this study can be made available upon a reasonable request from the corresponding author.
References
- 1. Yang C, Kors JA, Ioannou S, et al. Trends in the conduct and reporting of clinical prediction model development and validation: a systematic review. J Am Med Inform Assoc. 2022;29(5):983-989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tibshirani R. Regression shrinkage and selection via the LASSO. J R Stat Soc B. 1996;58(1):267-288. [Google Scholar]
- 3. Khalid S, Yang C, Blacketer C, et al. A standardized analytics pipeline for reliable and rapid development and validation of prediction models using observational health data. Comput Methods Programs Biomed. 2021;211:106394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Siontis GCM, Tzoulaki I, Castaldi PJ, et al. External validation of new risk prediction models is infrequent and reveals worse prognostic discrimination. J Clin Epidemiol. 2015;68(1):25-34. [DOI] [PubMed] [Google Scholar]
- 5. Suchard MA, Simpson SE, Zorych I, et al. Massive parallelization of serial inference algorithms for a complex generalized linear model. ACM Trans Model Comput Simul. 2013;23(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zou H, Hastie T. Regularization and variable selection via the elastic net. J R Stat Soc B. 2005;67(2):301-320. [Google Scholar]
- 7. Markus AF, Rijnbeek PR, Reps JM. Why predicting risk can’t identify ‘risk factors’: empirical assessment of model stability in machine learning across observational health databases. In: Proceedings of the 7th Machine Learning for Healthcare Conference. PMLR;2022:828- 1514–1521..
- 8. Su W, Bogdan M, Candès E. False discoveries occur early on the LASSO path. Ann Stat. 2017;45(5):2133-2150. [Google Scholar]
- 9. Kumar A, Bhattacharyya S, Bouchard K. Numerical characterization of support recovery in sparse regression with correlated design. Commun Stat Simul Comput. 2024;53(3):1504-1518. [Google Scholar]
- 10. Hoerl AE, Kennard RW. Ridge regression: biased estimation for nonorthogonal problems. Technometrics. 1970;12(1):55-67. [Google Scholar]
- 11. Nogueira S, Sechidis K, Brown G. On the stability of feature selection algorithms. J Mach Learn Res. 2018;18(174):1-54. [Google Scholar]
- 12. Zou H. The adaptive LASSO and its oracle properties. J Am Stat Assoc. 2006;101(476):1418-1429. [Google Scholar]
- 13. Freijeiro-González L, Febrero-Bande M, González-Manteiga W. A critical review of LASSO and its derivatives for variable selection under dependence among covariates. Int Stat Rev. 2022;90(1):118-145. [Google Scholar]
- 14. Wahid A, Khan DM, Iqbal N, et al. A generalized stability estimator based on inter-intrastability of subsets for high-dimensional feature selection. Chemom Intell Lab Syst. 2022;220:104457. [Google Scholar]
- 15. Dai L, Chen K, Sun Z, et al. Broken adaptive ridge regression and its asymptotic properties. J Multivar Anal. 2018;168:334-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Li N, Peng X, Kawaguchi E, et al. A scalable surrogate L0 sparse regression method for generalized linear models with applications to large scale data. J Stat Plan Inference. 2021;213:262-281. [Google Scholar]
- 17. Blumensath T, Davies ME. Iterative hard thresholding for compressed sensing. Appl Comput Harmon Anal. 2009;27(3):265-274. [Google Scholar]
- 18. John LH, Kors JA, Reps JM, et al. Logistic regression models for patient-level prediction based on massive observational data: do we need all data? Int J Med Inform. 2022;163:104762. [DOI] [PubMed] [Google Scholar]
- 19. John LH, Kors JA, Fridgeirsson EA, et al. External validation of existing dementia prediction models on observational health data. BMC Med Res Methodol. 2022;22(1):311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reps JM, Schuemie MJ, Suchard MA, et al. Design and implementation of a standardized framework to generate and evaluate patient-level prediction models using observational healthcare data. J Am Med Inform Assoc. 2018;25(8):969-975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reps JM, Ryan P, Rijnbeek PR. Investigating the impact of development and internal validation design when training prognostic models using a retrospective cohort in big US observational healthcare data. BMJ Open. 2021;11(12):e050146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moons KGM, Altman DG, Reitsma JB, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162(1):W1-W73. [DOI] [PubMed] [Google Scholar]
- 23. Saito T, Rehmsmeier M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS One. 2015;10(3):e0118432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Austin PC, Steyerberg EW. The integrated calibration index (ICI) and related metrics for quantifying the calibration of logistic regression models. Stat Med. 2019;38(21):4051-4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Demsar J. Statistical comparisons of classifiers over multiple data sets. J Mach Learn Res. 2006;7:1-30. [Google Scholar]
- 26. Hastie T, Tibshirani R, Tibshirani R. Best subset, forward stepwise or LASSO? Analysis and recommendations based on extensive comparisons. Stat Sci. 2020;35(4):579-592. [Google Scholar]
- 27. Cowley LE, Farewell DM, Maguire S, et al. Methodological standards for the development and evaluation of clinical prediction rules: a review of the literature. Diagn Progn Res. 2019;3:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fan J, Li R. Variable selection via nonconcave penalized likelihood and its oracle properties. J Am Stat Assoc. 2001;96(456):1348-1360. [Google Scholar]
- 30. Bogdan M, van den Berg E, Sabatti C, et al. Slope—adaptive variable selection via convex optimization. Ann Appl Stat. 2015;9(3):1103-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med. 2001;135(2):98-107. [DOI] [PubMed] [Google Scholar]
- 32. Lip GYH, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro heart survey on atrial fibrillation. Chest. 2010;137(2):263-272. [DOI] [PubMed] [Google Scholar]
- 33. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093-1100. [DOI] [PubMed] [Google Scholar]
- 34. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly due to the privacy of individuals whose data was used in the study. Aggregated data to support the findings of this study can be made available upon a reasonable request from the corresponding author.