Abstract
Objectives
Healthcare providers employ heuristic and analytical decision-making to navigate the high-stakes environment of the emergency department (ED). Despite the increasing integration of information systems (ISs), research on their efficacy is conflicting. Drawing on related fields, we investigate how timing and mode of delivery influence IS effectiveness. Our objective is to reconcile previous contradictory findings, shedding light on optimal IS design in the ED.
Materials and methods
We conducted a systematic review following PRISMA across PubMed, Scopus, and Web of Science. We coded the ISs’ timing as heuristic or analytical, their mode of delivery as active for automatic alerts and passive when requiring user-initiated information retrieval, and their effect on process, economic, and clinical outcomes.
Results
Our analysis included 83 studies. During early heuristic decision-making, most active interventions were ineffective, while passive interventions generally improved outcomes. In the analytical phase, the effects were reversed. Passive interventions that facilitate information extraction consistently improved outcomes.
Discussion
Our findings suggest that the effectiveness of active interventions negatively correlates with the amount of information received during delivery. During early heuristic decision-making, when information overload is high, physicians are unresponsive to alerts and proactively consult passive resources. In the later analytical phases, physicians show increased receptivity to alerts due to decreased diagnostic uncertainty and information quantity. Interventions that limit information lead to positive outcomes, supporting our interpretation.
Conclusion
We synthesize our findings into an integrated model that reveals the underlying reasons for conflicting findings from previous reviews and can guide practitioners in designing ISs in the ED.
Keywords: emergency medical services, clinical decision-making, information systems, computer-assisted decision-making, clinical decision support systems, information overload
Background and significance
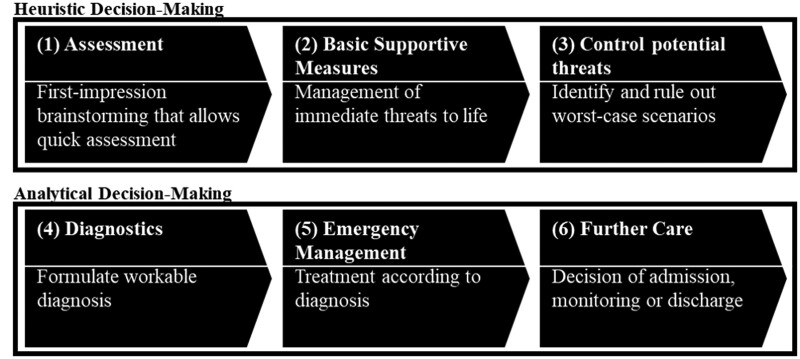
The emergency department (ED) is a critical yet volatile healthcare environment with varying patient volumes and acuity levels and a high density of decisions.1,2 Healthcare providers start with heuristic decision-making through pattern recognition and memorized checklists as tools for patient assessment and care.3,4 They then continue to a more analytical hypothetico-deductive approach, iterating through diagnostic hypotheses and treatment strategies1,5 (see Figure 1). However, this dual-model approach is susceptible to errors due to limited information,2 time pressure,6 interruptions and distractions,2 and multitasking.7
Figure 1.
Dual model of decision-making in the ED (adapted from3)
Information systems (ISs) have been posited as a potential solution to enhance clinical decision-making. ISs encompass any technical system that generates information enabling decision-makers to identify problems and needs, make evidence-based decisions, and allocate resources.8–10 Active and passive systems represent 2 distinct approaches within ISs.11–13 Active systems, such as Computerized Clinical Decision Support Systems (CCDSS), can be incorporated into electronic health record (EHR) systems or function as separate applications. These systems proactively assist physicians by offering recommendations based on patient data. Passive systems facilitate access to patient medical records and the latest evidence-based guidelines without actively interpreting the information. This category includes EHRs, which document patient interactions within a hospital, and Health Information Exchange (HIE) systems, which share patient information across healthcare facilities.14–23
Although ISs have shown promise to improve care quality in general clinical settings,24–26 their impact in the ED has shown mixed results. While some studies report improved efficiency and faster, better-informed decision-making,27,28 others indicate low adoption rates among physicians, decreased productivity, and increased burnout.29–31 Despite the growing research body on ISs in healthcare, extant literature lacks clarity regarding the contradictory impacts of ISs in the ED. Existing reviews focus on CCDSS and evaluate the methodological study quality without addressing the underlying reasons for the observed outcomes.32,33
Objective
Given the critical nature of decisions in emergency care, this research analyzes the impact of ISs on decision-making and why prior results are contradictory. The established understanding of heuristic and analytical decision-making and its effect on medical reasoning34–38 contrasts sharply with the limited exploration of its relevance to decision support systems. This gap persists despite IS research underscoring the importance of aligning the design of problem-solving aids with users’ mental representation to enhance problem-solving efficiency and effectiveness.39–41 Early evidence has identified passive summaries, graphics, and visual displays as advantageous for heuristic decision-making and active decision-support for analytical decision-making.42,43 Our study seeks to expand on these insights by testing 2 hypotheses (see Table 1).
Table 1.
Hypothesized effect matrix of technological intervention in the ED depending on their timing in the decision-making process and mode of delivery.
| Active mode of delivery | Passive mode of delivery | |
|---|---|---|
| Delivered during heuristic phases of decision-making | H: Passive ISs enhance the effectiveness of heuristic decision-making. | |
| Delivered during analytical phases of decision-making | H: Active ISs enhance the effectiveness of analytical decision-making. |
Methods
We followed the PRISMA guidelines for systematic reviews,44 including a forward search and a backward search.
Search strategy
We conducted a literature search across PubMed, Web of Science, and Scopus on April 26, 2023. The goal was to analyze the effects of the introduction of ISs in ED decision-making. Thus, our search string combined terms in 3 domains: technological intervention, decision support, and emergency care. We based the keywords on prior literature reviews on ED CCDSS to facilitate comparison.32,33 As the focus on CCDSS would omit established ISs like EHRs, we expanded the terms to include broader concepts, eg, “electronic” and “techn*” (see Supplementary Material S1). To ensure the robustness of our results, we focused on the most reputable medical informatics, emergency care, and IS journals in the initial search (see Supplementary Material S2).
Inclusion and exclusion criteria
We included primary research on technology implementation in the ED that compared IS-supported care with usual care. We thus excluded interventions that were (1) reviews, editorials, or perspectives, (2) nontechnological interventions, (3) outside the ED setting, or (4) did not compare outcome measures to non-IS-supported care. We refined our definition during the selection process and excluded systems (5) timed before patient assessment or after the admission/discharge decision (see Figure 1). This restriction facilitates the classification of whether physicians are in heuristic or analytical decision-making during delivery.
Study selection
Two authors independently screened titles and abstracts against the above criteria. If 1 author deemed an article relevant, we included it in the full-text screening. Two authors assessed publications for inclusion. Disagreements were resolved through discussion. One author performed forward and backward searches on the resulting publications. The eligibility of these articles was assessed similarly to the initial set, except that we did not filter on the predetermined journals.
Coding strategy
For each eligible study, we coded the intervention’s timing in the decision-making process, purpose, delivery mode, and effect on outcome variables. We started this process by extracting the verbatim descriptions for each variable, which we subsequently used for categorization. We assigned interventions to the heuristic phase if they provided information before physicians reached a diagnosis, to the analytical phase if information was provided after this point, and to both phases if they supplied information throughout the care pathway.3 Next, we coded the intervention’s purpose within each phase to capture how the IS was used. For the mode of delivery, we categorized, eg, “alerts”45 as active and “voluntary”46 interventions as passive. Lastly, for the outcome variables, we drew on decision support literature13,47 and assigned them to either “process outcomes,” where the change promoted by the IS alters a behavior; “economic outcomes,” where the change impacts hospital financial expenditures; or “clinical outcomes,” where the change translates into an impact on patients (see Table 2). Two authors independently coded the articles, resolving conflicts through discussion.
Table 2.
Coding structure.
| Coded variable | Distinct values | Description | Exemplary indicators |
|---|---|---|---|
| Timing in the ED decision-making process | Heuristic | Intervention provides information before the healthcare providers reach a diagnosis3, ie, phases (1) to (3) in Figure 1 | “assessed the patient for the presence of sepsis,”48 “diagnostic suggestions were displayed”49 |
| Analytical | Intervention provides information after the healthcare providers reach a diagnostic working hypothesis3, ie, phases (4) to (6) in Figure 1 | “initiation of buprenorphine,”50 “promote take-home naloxone prescription”51 | |
| Both | Intervention provides information across the care pathway3, ie, phases (1) to (6) in Figure 1 | “real time virtual patient record available at all points of care,”52 “available […] when diagnosing and admitting patients”53 | |
| Purpose | Verbatim descriptions | Aim of the technological intervention | “guides medication dosing for the elderly,”54 “automatically recognizes systemic inflammatory response syndrome”45 |
| Mode of delivery | Active | Information appears automatically11 | “interruptive,”55 “alert,”45 “notification,”56 “pop-up”57 |
| Passive | Users must proactively seek out the information they need11 | “voluntary,”46 “optional,”58 “at the clinician’s discretion”58 | |
| Type of outcome variable | Process | Variable measures a change in behavior13,47 | Adherence to proposed Management Plan, Adherence to Medication Guidelines13,47 |
| Economic | Variable measures an impact on financial expenditures13,47 | Cost, Cost-effectiveness13,47 | |
| Clinical | Variable measures an impact on patients13,47 | Mortality, Length of Stay13,47 | |
|
+ | Intervention results in a significant increase on a certain outcome variable | “usage was increased,”59 “significant increase was achieved”60 |
| ⦁ | Intervention has no significant effect on a certain outcome variable | “we did not observe such an effect,”61 “there was not a statistically significant change”62 | |
| — | Intervention results in a significant decrease on a certain outcome variable | “reduces the amount,”63 “was associated with a decrease”64 | |
|
↑ | Intervention was aimed at a significant increase | Decision Quality ↑, Adherence to Medication Guidelines ↑ |
| ↓ | Intervention was aimed at a significant decrease | Mortality ↓, Length of Stay ↓ | |
|
Black | Desired effect | Measured effect in line with expected effect |
| Grey | No effect | Intervention has no significant effect (⦁) | |
| White | Undesired effect | Measured effect not in line with expected effect |
Synthesis strategy
We first clustered similar purposes into groups by iteratively abstracting the verbatim descriptions.65 Supplementary Material S4 provides descriptions for every purpose group and outcome variable. We compared ISs carried out at the same phase and with the same purpose and timing to reveal what outcomes they affect. We summarized these effects across interventions to assess the consistency of the results. Finally, we synthesized the interventions across purposes to test how the timing and the mode of delivery affect the efficacy of IS interventions.
Results
Our initial search (left section in Figure 2) yielded 7766 hits, with 365 studies remaining after removing duplicates and filtering for relevant outlets. We identified 39 relevant studies through abstract and full-text screening. Forward and backward searches on these yielded 2387 articles (right section). Forty-four publications met the inclusion criteria, resulting in a total of 83 included studies. The main reasons for exclusion were nontechnological interventions (n = 388) and studies that did not compare outcome measures with non-IS-supported care (n = 248).
Figure 2.
Study selection process.
Clustering of purposes
We assigned the 83 interventions to the heuristic, analytical, or both phases and detailed their purpose. We coded their delivery mode as active or passive and how the intervention affected process, economic, or clinical outcomes. Table 3 visualizes how interventions affect outcomes at the purpose level. For example, the first row documents active interventions identifying medical conditions and recommending actions during heuristic decision-making. At the intersection with the outcome measure “adherence to proposed management plan,” we observe that 5 publications measure no significant impact, while 3 other ISs improve compliance. As less than 60% of the interventions have the desired effect (37.5%), we mark the cell grey. We used this granular analysis to prepare the test of our main hypotheses.
Table 3.
Effects of ISs in ED.
| Legend: |
Process outcomes |
Economic outcomes |
Clinical outcomes |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Docu-men-tation |
Clinical decision-making |
Adherence to clinical guidelines |
Clinical efficiency |
Clinical outcomes |
||||||||||||

|
At least 60% of interventions achieve the desired effect. | Quality of documentation ↑ | Information comprehension ↑ | Decision quality ↑ | Time to decision ↓ | Adherence to proposed management plan ↑ | Adherence to medication guidelines ↑ | Time to intervention ↓ | Utilization of imaging and testing resources ↓ | Yield of imaging and testing resources ↑ | Costs ↓ | Hospital Readmission ↓ | Hospital admission ↓ | Mortality ↓ | Length of stay ↓ | |

|
Less than 60% of interventions achieve the desired effect. | |||||||||||||||

|
The intervention leads to undesired effects. | |||||||||||||||
|
| ||||||||||||||||
| Timing | Purpose groups | Mode | ||||||||||||||
| Heuristic | Detection and Management Recommendations for Medical Conditions | Active | • (5)/ + (3)a | − (3) | • (1) | • (4) | • (4) | |||||||||
| Passive | + (1) | + (4) | − (1)/ • (1) | − (1) | − (1) | |||||||||||
| Analytical | Risk-Stratification for Imaging | Active | + (5) | − (9)/ • (1) | • (2)/ + (4) | |||||||||||
| Passive | • (2) | |||||||||||||||
| Proposal of Substitute Medication or Dosage Adjustment | Active | + (10) | + (1) | |||||||||||||
| Passive | • (1)/ + (1) | • (1) | ||||||||||||||
| Standardization of Admission and Discharge Process | Active | − (1) | − (2) | − (2) | − (2)/ • (1) | |||||||||||
| Both | Access to patients’ medical history | Passive | + (1) | − (2) | + (1) | − (1)/ • (1) | − (3) | − (4) | • (1) | − (2) | ||||||
| Emphasis Framing | Passive | + (3) | + (1) | − (1) | ||||||||||||
| Graphical Representation | Passive | + (2) | + (1) | − (1) | ||||||||||||
Used as example in text.
Interventions during heuristic decision-making
Twenty-seven interventions provided information while physicians mitigate threats to life and generate diagnostic hypotheses, ie, during heuristic decision-making. All aimed to support providers in (1.1) detecting a specific medical condition and recommending measures for its management.
Purpose group 1.1: detection and management recommendations for medical conditions (32.5% of identified interventions)
The 27 ISs in this group suggested diagnoses and actions based on evidence-based guidelines usually listed in order sets that include, eg, laboratory tests. These ISs provided active or passive guidance before physicians make a diagnosis.
Among the 27 articles, 18 had an active mode of delivery, ie, they alerted physicians to at-risk patients. Six reported positive effects. Three studies aimed to improve the timeliness of countermeasures for sepsis or acute coronary syndrome and found significant decreases in the time-to-intervention.56,66,67 Three studies improved guideline adherence by focusing on a single countermeasure, ie, lactate testing,45 blood culture collection,68 and child services reporting.69
The remaining 12 papers with active guidance failed to demonstrate positive results. Seven publications did not find significant effects on LOS,55,70–72 mortality,48,55,73,74 and hospital admission.73 Five studies on improving guideline adherence did not yield significant positive outcomes.75–79 In contrast to the successful studies above, these interventions proposed multiple measures. For example, Rosenthal et al78 demanded multiple tests, scans, and consultations.
Nine studies had a passive mode of delivery, ie, they provided information for physicians when experiencing diagnostic uncertainty. Eight reported positive effects. Five studies improved guideline adherence through antibiotic prescribing guidelines46,80–82 or medical calculators.83 Masica et al84 embedded voluntary medical calculators and showed a decrease in hospital admissions. Ramnarayan et al49 improve documentation quality through a diagnostic support system. Nam et al85 decreased time-to-thrombolysis when physicians proactively notified a stroke team.
One study with a passive delivery mode reported no significant results. Fargo et al58 provided a voluntary order set that did not improve time-to-antibiotics.
Interventions during analytical decision-making
Forty interventions provided information while physicians treat patients according to their diagnosis and decide whether to admit, monitor, or discharge patients, ie, during analytical decision-making. This phase is further subdivided into (2.1) risk-stratification for imaging, (2.2) proposal of substitute medication or dosage adjustment, and (2.3) standardization of the admission and discharge process.
Purpose group 2.1: risk-stratification for imaging (22.9%)
This group includes 19 studies that facilitated risk-stratification for imaging. These interventions supported clinicians actively or passively in deciding whether a patient requires imaging based on clinical guidelines.
Seventeen studies had an active mode of delivery, ie, they alerted physicians that an ordered imaging study is unnecessary. Each intervention, except one, improved outcome variables. The authors focused on head injury,86–92 pulmonary embolism,93–95 headache,96 ankle97 or wrist63 injury, or renal colic.98 Three studies introduced multiple guidelines.59,64,99 All 16 studies either decreased utilization rates,63,64,86–89,92,94,98 increased diagnostic yield,59,92,93,99 or improved documentation quality.89–91,95,97 Royuela et al96 found only decreased utilization but no effect on yield. Raja et al’s94 intervention impacted neither.
The remaining 2 studies had a passive mode of delivery, ie, they provided voluntary education on risk factors, but imaging utilization rates and yield were unaffected.61,62
Purpose group 2.2: proposal of substitute medication or dosage adjustment (16.9%)
The second group during analytical decision-making encompasses 14 interventions that actively or passively suggested medication substitution or dosage adjustment.
Among the 14 studies, 11 had an active mode of delivery, ie, they alerted physicians to reconsider their order placement. All 11 interventions had a positive effect on the outcome variables. Four studies improved naloxone prescription for opioid-related overdose.51,60,100,101 Griffey et al54 and Terrell et al102 reduced inappropriate medication for elderly patients. Two studies increased ketorolac prescribing103 or decreased excessive dosing104 in renal impairment. Dutta et al105 alerted physicians of duplicate vaccines. Bernstein et al106 reduced the use of proprietary antibiotics by displaying patients’ insurance status. Green et al107 demanded patient reverification and decreased wrong-patient orders.
The 3 remaining studies had a passive mode of delivery, ie, they provided decision support only when launched at the physician’s discretion. One study demonstrated positive effects. Holland et al50 increased the rate of buprenorphine prescription. The other 2 publications showed no or mixed effects. The authors50 above could not replicate the results on a larger scale.108 Horng et al’s109 study highlighted that previous prescriptions did not decrease duplicate medication orders.
Purpose group 2.3: standardization of admission and discharge process (8.4%)
Seven studies expedited the execution of the admission or discharge process by digitizing substeps. All interventions delivered content actively.
Five studies showed positive effects. Mahler et al110 and Stoypra et al57 computerized the HEART pathway to identify low-risk patients for discharge, reducing hospital admission. Cho et al111 and Kim et al112 reduced LOS by automating specialty consultations. Desai et al113 implemented a review loop after the admission decision, decreasing admission.
Two studies measured mixed or negative effects. While Liu et al114 confirmed the positive impact of the HEART pathway on hospital admission, they measured no difference in LOS. Driver et al115 implemented a “hard stop”115 when clinicians discharged patients without reviewing all lab results. However, this led to an increase in test results after discharge.
Interventions during both heuristic and analytical decision-making
The remaining 16 publications describe (3.1) accessing patients’ medical history or facilitating the extraction of information from these records through (3.2) emphasis framing or (3.3) graphical representation. Although the publications did not specify the timing, usage patterns indicate that medical records are consulted during both heuristic and analytical decision-making.28,52,53,116–119
Purpose group 3.1: access to patients’ medical history (12.0%)
This group encompasses 10 publications investigating the impact of access to medical records from previous encounters. Access to this data was either limited to visits at the designated hospital (EHRs) or extended to nearby hospitals (HIE). All interventions passively provided access.
Eight studies show positive effects on LOS,120,121 hospital admission,52,53,121,122 hospital readmission,52,53,119 and guideline adherence.123 Everson et al121 additionally reported a decrease in imaging utilization. Saef et al124 approximated a reduction in costs.
The remaining 2 studies reported mixed or no effects. Bailey et al125 found improvements in imaging utilization and yield, but these did not translate to cost reductions. von Wedel et al126 found no impact on mortality.
Purpose group 3.2: emphasis framing (4.2%)
Four studies focused on emphasis framing, ie, highlighting aspects of information to make it easier or more likely to be processed.127,128
All 4 interventions in this group had a passive mode delivery, ie, they highlighted certain information without alerts. Three author groups reported positive outcomes. Hwang et al129 and Kim et al130 highlighted radiographic abnormalities, improving their detection. Munigala et al131 retained only 1 test in the “frequently ordered” section, decreasing urine culture utilization. One study demonstrated mixed results. Laker et al132 emphasized the most critical information and summarized a patient’s EHR. They improved decision quality, but the time-to-decision also increased.
Purpose group 3.3: graphical representation (2.1%)
Two publications described interventions that visualize textual or tabular information to enhance information comprehension, as quantified, eg, by the NASA Task Load Index.
Both interventions had a passive delivery mode and reported positive effects. Kim et al133 converted the textual results of microbiological cultures into a visual representation, enhancing information comprehension. Thayer et al134 developed an asthma timeline, increasing information comprehension and reducing task time.
Summary
Summarizing the interventions across purpose groups and outcome types, we observe that active interventions failed to achieve the desired effects on 70% of the outcome variables during the heuristic phase. In contrast, passive interventions achieved the desired effects on 89% of the outcome variables. During the analytical phase, active interventions achieved desired effects on 87% of outcome variables, while passive interventions did not affect 80%. Passive EHR- and HIE-related interventions achieved positive results 88% of the time in both phases (Table 4).
Table 4.
Effects of technological intervention in the ED on outcome measures depending on their timing in the decision-making process and mode of delivery.
| Active mode of delivery | Passive mode of delivery | |
|---|---|---|
| Delivered during heuristic phases of decision-making | 6 Desired effect (30%), 14 No effect (70%) | 8 Desired effect (89%), 1 No effect (11%) |
| Delivered during analytical phases of decision-making | 35 Desired effect (87%), 4 No effect (10%), 1 Undesired effect (3%) | 1 Desired effect (20%), 4 No effect (80%) |
| Delivered during both phases | — | 22 Desired effect (88%), 2 No effect (8%), 1 Undesired effect (4%) |
Discussion
This review evaluated 83 IS interventions designed to support decision-making in the ED based on their timing in the decision-making process, ie, heuristic or analytical, and their mode of delivery, ie, active or passive. In the heuristic phase, active interventions did not achieve the desired effect in 70% of the measured outcome variables, whereas passive interventions met 89% of intended outcomes. Conversely, active interventions realized 87% of desired outcomes in analytical decision-making, while passive ISs had no impact on 80%. Across both phases, passive interventions that facilitate the extraction of information achieved positive outcomes 88% of the time.
Two systematic reviews paved the way for our exploration. Bennet and Hardiker’s32 and Patterson et al’s33 reviews assessed the impact of CCDSS and the researchers’ methodological rigor. Our active interventions have substantive overlap with the included studies. Bennet and Hardiker found that half of the studies reported positive outcomes, but their review did not categorize the interventions or examine the reasons for these results. Patterson et al highlighted positive effects in 83% of the included investigations. Their findings corroborate our own, emphasizing that improvements predominantly center around imaging and medication interventions.
Our study extends beyond CCDSS to encompass a broader spectrum of technological interventions. We explicitly included EHRs and HIEs in our search string and identified interventions that facilitate information extraction.
ISs in the heuristic decision-making phase
We hypothesize that information overload in the early stages of patient encounters, and the mismatch between heuristic thinking patterns and alerts explain the contrasting effectiveness of active and passive interventions. Decision theory suggests that increasing information quality improves decision quality. However, the relationship between information quantity and decision quality follows an inverted U-curve. Information overload occurs when the information quantity impedes decision quality more than the quality of information enhances it.135,136
Upon encountering a patient in the ED, physicians are met with abundant information, which they process under time pressure and high diagnostic uncertainty. To navigate this complexity and expedite care, clinicians revert to pattern recognition and algorithms, ie, heuristic decision-making.34–38
ISs add to this information in quality and quantity. However, active systems, eg, automatic sepsis detection,45,48,55,58,67,74,76 represent another information stream that doctors must process alongside diagnosing and treating patients. For most active interventions, the adverse impact of increased information quantity overshadows the benefits of enhanced information quality, leading to mixed outcomes in process measures and no discernible effect on clinical outcomes. The few successful interventions focused on a single recommendation,45,68,69 minimizing information quantity. In contrast, physicians consult passive systems, eg, databases with pneumonia treatment advice,46,80,82 when experiencing diagnostic uncertainty, ie, information deficit. Thus, there is no information overload, and the interventions consistently improve outcomes.
Several factors inherent to the environment and tasks during heuristic decision-making contribute to the reduced effectiveness of active systems. The complexity of diagnosing patients from EHR data causes false positives, leading to alert fatigue.55 Addressing immediate life threats requires direct interaction with patients, while alerts are generated on nearby PCs.70,71 Alerts may be triggered after treatment has already been administered due to the reliance on outdated information.55 These factors, ie, alert fatigue mitigation and decision support at the appropriate place and time, correlate with improved clinical practice.137,138 The drawbacks of the difficulty of their implementation in the ED are exacerbated by the heuristic thinking patterns, characterized by passive responsiveness, low cognitive awareness, and high automaticity.34–38 This can lead to notifications being viewed as noise.
ISs in the analytical decision-making phase
We hypothesize that the reason for the overwhelmingly positive effects of active interventions in analytical decision-making is the significant reduction in information overload. In contrast, physicians are reluctant to use passive resources because they do not perceive an information deficit in their tasks.
At this point in the care pathway, clinicians have managed immediate threats. They now want to confirm their diagnostic hypothesis and treat patients accordingly. The stability of patients allows providers to engage in more time-consuming but less error-prone analytical decision-making using the commonly employed hypothetico-deductive model.4,5,139,140
The identified interventions ask clinicians to reconsider their imaging, medication, or admission orders if they contradict evidence-based guidelines. We hypothesize that the reason for the consistently positive effects of active interventions is the significant decrease in diagnostic uncertainty and, thus, information quantity after physicians reach a working hypothesis.4,141–144 Clinicians do not seem to experience information overload from the IS-generated information, and the studies demonstrate a significant increase in guideline adherence. In contrast, the low adoption rates62,108 suggest physicians are reluctant to engage with passive resources. We attribute this reluctance to clinicians not perceiving an information deficit. They have already derived a decision, even if it diverges from the latest guidelines.
The effectiveness of active systems is enhanced by providing recommendations immediately after order placement based on if-then rules. This temporal and contextual immediacy ensures high accuracy and workflow integration.137,138 The increased receptivity to alerts also indicates the shift to analytical thinking, characterized by active responsiveness, high cognitive awareness, and low automaticity.34–38
ISs in both decision-making phases
The overwhelmingly positive effects of providing passive access to patients’ medical histories and passively facilitating information extraction support our hypotheses above. Discharge summaries and previous lab reports offer valuable information to guide diagnosis and treatment. Physicians access EHRs and HIEs from a desire to incorporate historical patient information into their decision-making, ie, from a perceived information deficit. Interventions that prepare information through emphasis framing or visual representation, eg, removing all but 1 order set from the “frequently ordered” section,131 show favorable outcomes because they reduce information quantity or increase comprehension through visualization.137,138,145
Future work
Our research suggests that the under-researched concept of information overload strongly influences the effectiveness of ISs. Only 1 prior study explicitly examined its perception and impact. Most physicians surveyed agreed that information overload is a severe problem and impairs decision-making.146 Other studies briefly mention information overload as a by-product of overcrowding.147,148 Beyond the ED, information overload due to the electronic availability of patient information is gaining traction in the discourse. Several publications find an association between EHR use and provider burnout.149–151 Nijor et al152 suggest that information overload may result in more medical errors and negatively impact patient safety.
We suggest researchers tackle information overload in the ED through the lens of the systems’ timing and delivery mode. In heuristic decision-making, physicians consult passive systems to reduce their diagnostic uncertainty. Researchers could identify and visualize the most contextually relevant information by timing and user group based on established guidelines and usage patterns.28,52,53,116–119 Another angle for future research is to investigate automatic data aggregation and visualization techniques to address information quantity and comprehension in passive systems, building on studies outside the ED context.153–155 An intriguing method for implementing these avenues is the cooperative delivery mode—an iterative “back and forth” of requesting and modifying information.156 For example, recent studies have demonstrated the ability of large language models to generate diagnosis lists for common chief complaints.157,158
In the analytical phase, clinicians are receptive to active alerts issued at the time and place of the decision. Most analyzed IS are integrated into the medication or imaging ordering systems.51,86 Future research could explore methods to maintain this workflow integration when clinicians are away from their workstations, potentially through wearables or augmented reality. Ensuring that only the most important information is relayed through these devices, future research should prevent sensory overflow and integrate rest periods away from the PC for recovery.146 For example, the alerts’ appropriateness could be derived from clinicians’ physiological measures and environmental factors such as overcrowding.
Last, future research should strengthen the robustness of our results. We suggest empirically testing our hypothesis that passive interventions are more effective than active interventions during heuristic decision-making. We propose an RCT where EDs will be randomly assigned to implement a clinical guideline passively (databases), actively (alerting), or to control groups. A similar design is also suitable for testing the superiority of active over passive interventions in the analytical phase, eg, when prescribing medication.
Limitations
Our search strategy initially filtered studies based on decision support keywords and predetermined outlets, which could potentially miss relevant studies. We coded interventions as either heuristic or analytical, while physicians typically blend these strategies, with the dominant approach being influenced not only by the timing but also, eg, experience. Our analysis does not account for several factors that contribute to the effectiveness of interventions, such as the accuracy, time, and place of decision support. We did not assess the quality of the study design, considering all studies to contribute equally to the evidence base. The imbalance of delivery modes during the heuristic (9 passive/20 active) and analytical phases (5/40) affects the generalizability of our conclusions.
Conclusion
ISs have shown great promise in improving decision quality in general clinical settings,24–26 but their impact in the ED has shown mixed results. We assessed 83 studies from 2 angles: their timing during heuristic or analytical decision-making and their active or passive mode of delivery. We synthesize the findings into an integrated model (Tables 3 and 4), which we provide as a printable tool (Supplementary Material S5). It reveals underlying reasons for the mixed results of prior reviews and can serve as a reference tool for practitioners involved in designing ISs in the ED (see Supplementary Material S6 for practical implications).
Supplementary Material
Contributor Information
Cornelius Born, School of Computation, Information and Technology, Technical University of Munich, 85748 Garching bei München, Germany.
Romy Schwarz, School of Computation, Information and Technology, Technical University of Munich, 85748 Garching bei München, Germany.
Timo Phillip Böttcher, School of Computation, Information and Technology, Technical University of Munich, 85748 Garching bei München, Germany.
Andreas Hein, Institute of Information Systems and Digital Business, University of St. Gallen, 9000 St. Gallen, Switzerland.
Helmut Krcmar, School of Computation, Information and Technology, Technical University of Munich, 85748 Garching bei München, Germany.
Author contributions
Cornelius Born, Timo Böttcher, and Andreas Hein designed the review. Cornelius Born and Romy Schwarz performed the study selection and coding process. Cornelius Born synthesized and interpreted the findings, and drafted and revised the manuscript. Timo Böttcher, Andreas Hein, and Helmut Krcmar reviewed the drafts and provided feedback.
Supplementary material
Supplementary material is available at Journal of the American Medical Informatics Association online.
Funding
This work was supported by the German Ministry of Education and Research (Bundesministerium für Bildung und Forschung) under grant number 16SV9048.
Conflicts of interest
None declared.
Data availability
The list of all articles identified by our search strategy with their inclusion/exclusion criteria and the detailed coding of all studies (summarized in Supplementary Material S3), including the verbatim descriptions for each variable and the rationale for their categorization, will be provided upon request.
References
- 1. Kovacs G, Croskerry P. Clinical decision making: an emergency medicine perspective. Acad Emerg Med. 1999;6(9):947-952. 10.1111/j.1553-2712.1999.tb01246.x [DOI] [PubMed] [Google Scholar]
- 2. Croskerry P, Sinclair D. Emergency medicine: a practice prone to error? Can J Emerg Med. 2001;3(4):271-276. 10.1017/S1481803500005765 [DOI] [PubMed] [Google Scholar]
- 3. Al-Azri NH. How to think like an emergency care provider: a conceptual mental model for decision making in emergency care. Int J Emerg Med. 2020;13(1):17. 10.1186/s12245-020-00274-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9(11):1184-1204. 10.1197/aemj.9.11.1184 [DOI] [PubMed] [Google Scholar]
- 5. Tierney WM. Improving clinical decisions and outcomes with information: a review. Int J Med Inform. 2001;62(1):1-9. 10.1016/S1386-5056(01)00127-7 [DOI] [PubMed] [Google Scholar]
- 6. Flowerdew L, Brown R, Russ S, Vincent C, Woloshynowych M. Teams under pressure in the emergency department: an interview study. Emerg Med J. 2012;29(12):e2. 10.1136/emermed-2011-200084 [DOI] [PubMed] [Google Scholar]
- 7. Laxmisan A, Hakimzada F, Sayan OR, Green RA, Zhang J, Patel VL. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2007;76(11-12):801-811. 10.1016/j.ijmedinf.2006.09.019 [DOI] [PubMed] [Google Scholar]
- 8. Haux R. Health information systems—past, present, future. Int J Med Inform. 2006;75(3-4):268-281. 10.1016/j.ijmedinf.2005.08.002 [DOI] [PubMed] [Google Scholar]
- 9. AbouZahr C, Boerma T. Health information systems: the foundations of public health. Bull World Health Organ. 2005;83(8):578-583. [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization. Health Information Systems and Rehabilitation. 2017. Accessed January 29, 2024. https://cdn.who.int/media/docs/default-source/documents/health-topics/rehabilitation/call-for-action/healthinformationsystemsandrehaboctober17.pdf?sfvrsn=a0461dd9_5 [Google Scholar]
- 11. Perreault LE, Metzger JB. A pragmatic framework for understanding clinical decision support. J Healthc Inf Manag. 1999;13(2):5-22. [Google Scholar]
- 12. Berner ES, ed. Clinical Decision Support Systems. Springer; 2007. 10.1007/978-0-387-38319-4 [DOI] [Google Scholar]
- 13. Osheroff J, Pifer E, Teich J, Sittig D, Jenders R. Improving Outcomes with Clinical Decision Support: An Implementer’s Guide. Healthcare Information & Management Systems Society; 2005. [Google Scholar]
- 14. Gefen D, Ben-Assuli O, Stehr M, Rosen B, Denekamp Y. Governmental intervention in Hospital Information Exchange (HIE) diffusion: a quasi-experimental ARIMA interrupted time series analysis of monthly HIE patient penetration rates. Eur J Inf Syst. 2019;28(6):627-645. [Google Scholar]
- 15. Noblin A, Cortelyou-Ward K, Cantiello J, et al. EHR implementation in a new clinic: a case study of clinician perceptions. J Med Syst. 2013;37(4):9955. 10.1007/s10916-013-9955-2 [DOI] [PubMed] [Google Scholar]
- 16. Ben-Assuli O, Leshno M. Assessing electronic health record systems in emergency departments: using a decision analytic Bayesian model. Health Informatics J. 2016;22(3):712-729. 10.1177/1460458215584203 [DOI] [PubMed] [Google Scholar]
- 17. Sittig DF, Gonzalez D, Singh H. Contingency planning for electronic health record-based care continuity: a survey of recommended practices. Int J Med Inform. 2014;83(11):797-804. 10.1016/j.ijmedinf.2014.07.007 [DOI] [PubMed] [Google Scholar]
- 18. Ben-Assuli O. Electronic health records, adoption, quality of care, legal and privacy issues and their implementation in emergency departments. Health Policy. 2015;119(3):287-297. 10.1016/j.healthpol.2014.11.014 [DOI] [PubMed] [Google Scholar]
- 19. Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med. 2011;365(9):825-833. 10.1056/NEJMsa1102519 [DOI] [PubMed] [Google Scholar]
- 20. Kazley AS, Simpson AN, Simpson KN, Teufel R. Association of electronic health records with cost savings in a national sample. Am J Manag Care. 2014;20(6):e183-e190. [PubMed] [Google Scholar]
- 21. Heart T, Ben-Assuli O, Shabtai I. A review of PHR, EMR and EHR integration: a more personalized healthcare and public health policy. Health Policy Technol. 2017;6(1):20-25. 10.1016/j.hlpt.2016.08.002 [DOI] [Google Scholar]
- 22. Knepper MM, Castillo EM, Chan TC, Guss DA. The effect of access to electronic health records on throughput efficiency and imaging utilization in the emergency department. Health Serv Res. 2018;53(2):787-802. 10.1111/1475-6773.12695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kannampallil TG, Denton CA, Shapiro JS, Patel VL. Efficiency of emergency physicians: insights from an observational study using EHR log files. Appl Clin Inform. 2018;9(1):99-104. 10.1055/s-0037-1621705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff (Millwood). 2011;30(3):464-471. 10.1377/hlthaff.2011.0178 [DOI] [PubMed] [Google Scholar]
- 25. Goldzweig CL, Towfigh A, Maglione M, Shekelle PG. Costs and benefits of health information technology: new trends from the literature. Health Aff (Millwood). 2009;28(2):w282-w293. 10.1377/hlthaff.28.2.w282 [DOI] [PubMed] [Google Scholar]
- 26. Kruse CS, Beane A. Health information technology continues to show positive effect on medical outcomes: systematic review. J Med Internet Res. 2018;20(2):e8793. 10.2196/jmir.8793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baumlin KM, Shapiro JS, Weiner C, Gottlieb B, Chawla N, Richardson LD. Clinical information system and process redesign improves emergency department efficiency. Jt Comm J Qual Patient Saf. 2010;36(4):179-185. 10.1016/s1553-7250(10)36030-2 [DOI] [PubMed] [Google Scholar]
- 28. Callen J, Li L, Georgiou A, et al. Does an integrated emergency department information system change the sequence of clinical work? A mixed-method cross-site study. Int J Med Inform. 2014;83(12):958-966. 10.1016/j.ijmedinf.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 29. Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: an evaluation of information system impact and contingency factors. Int J Med Inform. 2014;83(11):779-796. 10.1016/j.ijmedinf.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 30. Mullins A, O’Donnell R, Morris H, et al. The effect of my health record use in the emergency department on clinician-assessed patient care: results from a survey. BMC Med Inform Decis Mak. 2022;22(1):1. 10.1186/s12911-022-01920-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hill RG, Sears LM, Melanson SW. 4000 clicks: a productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med. 2013;31(11):1591-1594. 10.1016/j.ajem.2013.06.028 [DOI] [PubMed] [Google Scholar]
- 32. Bennett P, Hardiker NR. The use of computerized clinical decision support systems in emergency care: a substantive review of the literature. J Am Med Inform Assoc. 2017;24(3):655-668. 10.1093/jamia/ocw151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Patterson BW, Pulia MS, Ravi S, et al. Scope and influence of electronic health record-integrated clinical decision support in the emergency department: a systematic review. Ann Emerg Med. 2019;74(2):285-296. 10.1016/j.annemergmed.2018.10.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84(8):1022-1028. 10.1097/ACM.0b013e3181ace703 [DOI] [PubMed] [Google Scholar]
- 35. Croskerry P, Norman G. Overconfidence in clinical decision making. Am J Med. 2008;121(Suppl 5):S24-S29. 10.1016/j.amjmed.2008.02.001 [DOI] [PubMed] [Google Scholar]
- 36. Coughlan JJ, Mullins CF, Kiernan TJ. Diagnosing, fast and slow. Postgrad Med J. 2021;97(1144):103-109. 10.1136/postgradmedj-2019-137412 [DOI] [PubMed] [Google Scholar]
- 37. Corrao S, Argano C. Rethinking clinical decision-making to improve clinical reasoning. Front Med. 2022;9:900543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bate L, Hutchinson A, Underhill J, Maskrey N. How clinical decisions are made. Br J Clin Pharmacol. 2012;74(4):614-620. 10.1111/j.1365-2125.2012.04366.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vessey I. Cognitive fit: a theory-based analysis of the graphs versus tables literature. Decis Sci. 1991;22(2):219-240. 10.1111/j.1540-5915.1991.tb00344.x [DOI] [Google Scholar]
- 40. Speier C, Vessey I, Valacich JS. The effects of interruptions, task complexity, and information presentation on computer-supported decision-making performance. Decis Sci. 2003;34(4):771-797. 10.1111/j.1540-5414.2003.02292.x [DOI] [Google Scholar]
- 41. Zigurs I, Buckland B. A theory of task/technology fit and group support systems effectiveness. Manag Inf Syst Q. 1998;22(3):313-334. [Google Scholar]
- 42. Islam R, Weir CR, Jones M, Del Fiol G, Samore MH. Understanding complex clinical reasoning in infectious diseases for improving clinical decision support design. BMC Med Inform Decis Mak. 2015;15(1):101. 10.1186/s12911-015-0221-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wu HW, Davis PK, Bell DS. Advancing clinical decision support using lessons from outside of healthcare: an interdisciplinary systematic review. BMC Med Inform Decis Mak. 2012;12(1):90. 10.1186/1472-6947-12-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Berger T, Birnbaum A, Bijur P, Kuperman G, Gennis P. A computerized alert screening for severe sepsis in emergency department patients increases lactate testing but does not improve inpatient mortality. Appl Clin Inform. 2010;1(4):394-407. 10.4338/ACI-2010-09-RA-0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Buising KL, Thursky KA, Black JF, et al. Improving antibiotic prescribing for adults with community acquired pneumonia: does a computerised decision support system achieve more than academic detailing alone?—a time series analysis. BMC Med Inform Decis Mak. 2008;8(1):35. 10.1186/1472-6947-8-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lobach D, Sanders GD, Bright TJ, et al. Enabling health care decision-making through clinical decision support and knowledge management. Evid Rep Technol Assess. 2012;(703):1-784. [PMC free article] [PubMed] [Google Scholar]
- 48. Arabi YM, Al-Dorzi HM, Alamry A, et al. The impact of a multifaceted intervention including sepsis electronic alert system and sepsis response team on the outcomes of patients with sepsis and septic shock. Ann Intensive Care. 2017;7(1):57. 10.1186/s13613-017-0280-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ramnarayan P, Winrow A, Coren M, et al. Diagnostic omission errors in acute paediatric practice: impact of a reminder system on decision-making. BMC Med Inform Decis Mak. 2006;6(1):37. 10.1186/1472-6947-6-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Holland WC, Nath B, Li F, et al. Interrupted time series of user-centered clinical decision support implementation for emergency department-initiated buprenorphine for opioid use disorder. Acad Emerg Med. 2020;27(8):753-763. 10.1111/acem.14002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Jennings LK, Ward R, Pekar E, et al. The effectiveness of a noninterruptive alert to increase prescription of take-home naloxone in emergency departments. J Am Med Inform Assoc. 2023;30(4):683-691. 10.1093/jamia/ocac257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ben-Assuli O, Shabtai I, Leshno M. The impact of EHR and HIE on reducing avoidable admissions: controlling main differential diagnoses. BMC Med Inform Decis Mak. 2013;13(1):49. 10.1186/1472-6947-13-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ben-Assuli O, Shabtai I, Leshno M, Hill S. EHR in emergency rooms: exploring the effect of key information components on main complaints. J Med Syst. 2014;38(4):36. 10.1007/s10916-014-0036-y [DOI] [PubMed] [Google Scholar]
- 54. Griffey RT, Lo HG, Burdick E, Keohane C, Bates DW. Guided medication dosing for elderly emergency patients using real-time, computerized decision support. J Am Med Inform Assoc. 2012;19(1):86-93. 10.1136/amiajnl-2011-000124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Austrian JS, Jamin CT, Doty GR, Blecker S. Impact of an emergency department electronic sepsis surveillance system on patient mortality and length of stay. J Am Med Inform Assoc. 2018;25(5):523-529. 10.1093/jamia/ocx072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Nelson JL, Smith BL, Jared JD, Younger JG. Prospective trial of real-time electronic surveillance to expedite early care of severe sepsis. Ann Emerg Med. 2011;57(5):500-504. 10.1016/j.annemergmed.2010.12.008 [DOI] [PubMed] [Google Scholar]
- 57. Stopyra JP, Snavely AC, Lenoir KM, et al. HEART pathway implementation safely reduces hospitalizations at one year in patients with acute chest pain. Ann Emerg Med. 2020;76(5):555-565. 10.1016/j.annemergmed.2020.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Fargo EL, D’Amico F, Pickering A, Fowler K, Campbell R, Baumgartner M. Impact of electronic physician order-set on antibiotic ordering time in septic patients in the emergency department. Appl Clin Inform. 2018;9(4):869-874. 10.1055/s-0038-1676040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Poeran J, Mao LJ, Zubizarreta N, et al. Effect of clinical decision support on appropriateness of advanced imaging use among physicians-in-training. AJR Am J Roentgenol. 2019;212(4):859-866. 10.2214/AJR.18.19931 [DOI] [PubMed] [Google Scholar]
- 60. Lowenstein M, Perrone J, Xiong RA, et al. Sustained implementation of a multicomponent strategy to increase emergency department-initiated interventions for opioid use disorder. Ann Emerg Med. 2022;79(3):237-248. 10.1016/j.annemergmed.2021.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Carnevale TJ, Meng D, Wang JJ, Littlewood M. Impact of an emergency medicine decision support and risk education system on computed tomography and magnetic resonance imaging use. J Emerg Med. 2015;48(1):53-57. 10.1016/j.jemermed.2014.07.033 [DOI] [PubMed] [Google Scholar]
- 62. Andruchow JE, Grigat D, McRae AD, et al. Decision support for computed tomography in the emergency department: a multicenter cluster-randomized controlled trial. CJEM. 2021;23(5):631-640. 10.1007/s43678-021-00170-3 [DOI] [PubMed] [Google Scholar]
- 63. Mulders MAM, Walenkamp MMJ, Sosef NL, et al. The Amsterdam Wrist Rules to reduce the need for radiography after a suspected distal radius fracture: an implementation study. Eur J Trauma Emerg Surg. 2020;46(3):573-582. 10.1007/s00068-019-01194-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bookman K, West D, Ginde A, et al. Embedded clinical decision support in electronic health record decreases use of high-cost imaging in the emergency department: EmbED study. Acad Emerg Med. 2017;24(7):839-845. 10.1111/acem.13195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Corbin JM, Strauss A. Grounded theory research: procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3-21. 10.1007/BF00988593 [DOI] [Google Scholar]
- 66. Alhejily WA. Implementing “Chest Pain Pathway” using smartphone messaging application “WhatsApp” as a corrective action plan to improve ischemia time in “ST-Elevation Myocardial Infarction” in primary PCI capable center “WhatsApp-STEMI Trial”. Crit Pathw Cardiol. 2021;20(4):179-184. 10.1097/HPC.0000000000000264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hayden GE, Tuuri RE, Scott R, et al. Triage sepsis alert and sepsis protocol lower times to fluids and antibiotics in the ED. Am J Emerg Med. 2016;34(1):1-9. 10.1016/j.ajem.2015.08.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Dutta S, McEvoy DS, Rubins DM, Dighe AS, Filbin MR, Rhee C. Clinical decision support improves blood culture collection before intravenous antibiotic administration in the emergency department. J Am Med Inform Assoc. 2022;29(10):1705-1714. 10.1093/jamia/ocac115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Rumball-Smith J, Fromkin J, Rosenthal B, et al. Implementation of routine electronic health record-based child abuse screening in general emergency departments. Child Abuse Negl. 2018;85:58-67. 10.1016/j.chiabu.2018.08.008 [DOI] [PubMed] [Google Scholar]
- 70. Dexheimer JW, Abramo TJ, Arnold DH, et al. An asthma management system in a pediatric emergency department. Int J Med Inform. 2013;82(4):230-238. 10.1016/j.ijmedinf.2012.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Dexheimer JW, Abramo TJ, Arnold DH, et al. Implementation and evaluation of an integrated computerized asthma management system in a pediatric emergency department: a randomized clinical trial. Int J Med Inform. 2014;83(11):805-813. 10.1016/j.ijmedinf.2014.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Roukema J, Steyerberg EW, van der Lei J, Moll HA. Randomized trial of a clinical decision support system: impact on the management of children with fever without apparent source. J Am Med Inform Assoc. 2008;15(1):107-113. 10.1197/jamia.M2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Dean NC, Jones BE, Jones JP, et al. Impact of an electronic clinical decision support tool for emergency department patients with pneumonia. Ann Emerg Med. 2015;66(5):511-520. 10.1016/j.annemergmed.2015.02.003 [DOI] [PubMed] [Google Scholar]
- 74. Narayanan N, Gross AK, Pintens M, Fee C, MacDougall C. Effect of an electronic medical record alert for severe sepsis among ED patients. Am J Emerg Med. 2016;34(2):185-188. 10.1016/j.ajem.2015.10.005 [DOI] [PubMed] [Google Scholar]
- 75. Asaro PV, Sheldahl AL, Char DM. Embedded guideline information without patient specificity in a commercial emergency department computerized order-entry system. Acad Emerg Med. 2006;13(4):452-458. 10.1197/j.aem.2005.09.015 [DOI] [PubMed] [Google Scholar]
- 76. Kim Y-J, Lee J-H, Lee S-W, Kim WY. Use of quick sequential organ failure assessment score-based sepsis clinical decision support system may be helpful to predict sepsis development. SV. 2021;17(5):86-94. 10.22514/sv.2021.082 [DOI] [Google Scholar]
- 77. Rocha BHSC, Christenson JC, Evans RS, Gardner RM. Clinicians’ response to computerized detection of infections. J Am Med Inform Assoc. 2001;8(2):117-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Rosenthal B, Skrbin J, Fromkin J, et al. Integration of physical abuse clinical decision support at 2 general emergency departments. J Am Med Inform Assoc. 2019;26(10):1020-1029. 10.1093/jamia/ocz069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Suresh S, Saladino RA, Fromkin J, et al. Integration of physical abuse clinical decision support into the electronic health record at a Tertiary Care Children’s Hospital. J Am Med Inform Assoc. 2018;25(7):833-840. 10.1093/jamia/ocy025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Dean NC, Vines CG, Carr JR, et al. A pragmatic, stepped-wedge, cluster-controlled clinical trial of real-time pneumonia clinical decision support. Am J Respir Crit Care Med. 2022;205(11):1330-1336. 10.1164/rccm.202109-2092OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Demonchy E, Dufour J-C, Gaudart J, et al. Impact of a computerized decision support system on compliance with guidelines on antibiotics prescribed for urinary tract infections in emergency departments: a multicentre prospective before-and-after controlled interventional study. J Antimicrob Chemother. 2014;69(10):2857-2863. 10.1093/jac/dku191 [DOI] [PubMed] [Google Scholar]
- 82. Wang HY, Treu CN, Cocca M, Felton D, Gatton B. Appropriateness of antibiotic selection for pneumonia in the emergency department: pre- and post-order set changes. Int J Pharm Pract. 2021;29(5):493-498. 10.1093/ijpp/riab043 [DOI] [PubMed] [Google Scholar]
- 83. Morgan KL, Kukhareva PV, Warner PB, et al. Using CDS Hooks to increase SMART on FHIR app utilization: a cluster-randomized trial. J Am Med Inform Assoc. 2022;29(9):1461-1470. 10.1093/jamia/ocac085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Masica A, Brown R, Farzad A, et al. Effectiveness of an algorithm-based care pathway for patients with non-valvular atrial fibrillation presenting to the emergency department. J Am Coll Emerg Physicians Open. 2022;3(1):e12608. 10.1002/emp2.12608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Nam HS, Han SW, Ahn SH, et al. Improved time intervals by implementation of computerized physician order entry-based stroke team approach. Cerebrovasc Dis. 2007;23(4):289-293. 10.1159/000098329 [DOI] [PubMed] [Google Scholar]
- 86. Ballard DW, Kuppermann N, Vinson DR, et al. ; Partners HealthCare. Implementation of a clinical decision support system for children with minor blunt head trauma who are at nonnegligible risk for traumatic brain injuries. Ann Emerg Med. 2019;73(5):440-451. 10.1016/j.annemergmed.2018.11.011 [DOI] [PubMed] [Google Scholar]
- 87. Arora R, White EN, Niedbala D, et al. Reducing computed tomography scan utilization for pediatric minor head injury in the emergency department: a quality improvement initiative. Acad Emerg Med. 2021;28(6):655-665. 10.1111/acem.14177 [DOI] [PubMed] [Google Scholar]
- 88. Dayan PS, Ballard DW, Tham E, et al. ; for the Pediatric Emergency Care Applied Research Network (PECARN). Use of traumatic brain injury prediction rules with clinical decision support. Pediatrics. 2017;139(4):e20162709. 10.1542/peds.2016-2709 [DOI] [PubMed] [Google Scholar]
- 89. Engineer RS, Podolsky SR, Fertel BS, et al. A pilot study to reduce computed tomography utilization for pediatric mild head injury in the emergency department using a clinical decision support tool and a structured parent discussion tool. Pediatr Emerg Care. 2021;37(12):e1670-e1674. 10.1097/PEC.0000000000001501 [DOI] [PubMed] [Google Scholar]
- 90. Gupta A, Ip IK, Raja AS, Andruchow JE, Sodickson A, Khorasani R. Effect of clinical decision support on documented guideline adherence for head CT in emergency department patients with mild traumatic brain injury. J Am Med Inform Assoc. 2014;21(e2):e347-e351. 10.1136/amiajnl-2013-002536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Ip IK, Raja AS, Gupta A, Andruchow J, Sodickson A, Khorasani R. Impact of clinical decision support on head computed tomography use in patients with mild traumatic brain injury in the ED. Am J Emerg Med. 2015;33(3):320-325. 10.1016/j.ajem.2014.11.005 [DOI] [PubMed] [Google Scholar]
- 92. Sharp AL, Huang BZ, Tang T, et al. Implementation of the Canadian CT head rule and its association with use of computed tomography among patients with head injury. Ann Emerg Med. 2018;71(1):54-63.e2. 10.1016/j.annemergmed.2017.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Drescher FS, Chandrika S, Weir ID, et al. Effectiveness and acceptability of a computerized decision support system using modified Wells criteria for evaluation of suspected pulmonary embolism. Ann Emerg Med. 2011;57(6):613-621. 10.1016/j.annemergmed.2010.09.018 [DOI] [PubMed] [Google Scholar]
- 94. Raja AS, Ip IK, Prevedello LM, et al. Effect of computerized clinical decision support on the use and yield of CT pulmonary angiography in the emergency department. Radiology. 2012;262(2):468-474. 10.1148/radiol.11110951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Raja AS, Gupta A, Ip IK, Mills AM, Khorasani R. The use of decision support to measure documented adherence to a national imaging quality measure. Acad Radiol. 2014;21(3):378-383. 10.1016/j.acra.2013.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Royuela A, Abad C, Vicente A, et al. Implementation of a computerized decision support system for computed tomography scan requests for nontraumatic headache in the emergency department. J Emerg Med. 2019;57(6):780-790. 10.1016/j.jemermed.2019.08.026 [DOI] [PubMed] [Google Scholar]
- 97. Silveira PC, Ip IK, Sumption S, Raja AS, Tajmir S, Khorasani R. Impact of a clinical decision support tool on adherence to the Ottawa Ankle Rules. Am J Emerg Med. 2016;34(3):412-418. 10.1016/j.ajem.2015.11.028 [DOI] [PubMed] [Google Scholar]
- 98. Raja AS, Pourjabbar S, Ip IK, et al. Impact of a health information technology-enabled appropriate use criterion on utilization of emergency department CT for renal colic. AJR Am J Roentgenol. 2019;212(1):142-145. 10.2214/AJR.18.19966 [DOI] [PubMed] [Google Scholar]
- 99. Ip IK, Schneider LI, Hanson R, et al. Adoption and meaningful use of computerized physician order entry with an integrated clinical decision support system for radiology: ten-year analysis in an urban teaching hospital. J Am Coll Radiol. 2012;9(2):129-136. 10.1016/j.jacr.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 100. Funke M, Kaplan MC, Glover H, et al. Increasing naloxone prescribing in the emergency department through education and electronic medical record work-aids. Jt Comm J Qual Patient Saf. 2021;47(6):364-375. 10.1016/j.jcjq.2021.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Marino R, Landau A, Lynch M, Callaway C, Suffoletto B. Do electronic health record prompts increase take-home naloxone administration for emergency department patients after an opioid overdose? Addiction. 2019;114(9):1575-1581. 10.1111/add.14635 [DOI] [PubMed] [Google Scholar]
- 102. Terrell KM, Perkins AJ, Dexter PR, Hui SL, Callahan CM, Miller DK. Computerized decision support to reduce potentially inappropriate prescribing to older emergency department patients: a randomized, controlled trial. J Am Geriatr Soc. 2009;57(8):1388-1394. 10.1111/j.1532-5415.2009.02352.x [DOI] [PubMed] [Google Scholar]
- 103. Netherton SJ, Lonergan K, Wang D, McRae A, Lang E. Computerized physician order entry and decision support improves ED analgesic ordering for renal colic. Am J Emerg Med. 2014;32(9):958-961. 10.1016/j.ajem.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 104. Terrell KM, Perkins AJ, Hui SL, Callahan CM, Dexter PR, Miller DK. Computerized decision support for medication dosing in renal insufficiency: a randomized, controlled trial. Ann Emerg Med. 2010;56(6):623-629. 10.1016/j.annemergmed.2010.03.025 [DOI] [PubMed] [Google Scholar]
- 105. Dutta S, McEvoy DS, Stump T, et al. Clinical decision support reduces unnecessary tetanus vaccinations in the emergency department. Ann Emerg Med. 2021;78(3):370-380. 10.1016/j.annemergmed.2021.02.021 [DOI] [PubMed] [Google Scholar]
- 106. Bernstein SL, Whitaker D, Winograd J, Brennan JA. An electronic chart prompt to decrease proprietary antibiotic prescription to self-pay patients. Acad Emerg Med. 2005;12(3):225-231. 10.1197/j.aem.2004.09.021 [DOI] [PubMed] [Google Scholar]
- 107. Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system. Ann Emerg Med. 2015;65(6):679-686.e1. 10.1016/j.annemergmed.2014.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Melnick ER, Nath B, Dziura JD, et al. User centered clinical decision support to implement initiation of buprenorphine for opioid use disorder in the emergency department: EMBED pragmatic cluster randomized controlled trial. BMJ. 2022;9(5):e069271. 10.1136/bmj-2021-069271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Horng S, Joseph JW, Calder S, et al. Assessment of unintentional duplicate orders by emergency department clinicians before and after implementation of a visual aid in the electronic health record ordering system. JAMA Netw Open. 2019;2(12):e1916499. 10.1001/jamanetworkopen.2019.16499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Mahler SA, Lenoir KM, Wells BJ, et al. Safely identifying emergency department patients with acute chest pain for early discharge: the HEART pathway accelerated diagnostic protocol. Circulation. 2018;138(22):2456-2468. 10.1161/CIRCULATIONAHA.118.036528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Cho SJ, Jeong J, Han S, et al. Decreased emergency department length of stay by application of a computerized consultation management system. Acad Emerg Med. 2011;18(4):398-402. 10.1111/j.1553-2712.2011.01039.x [DOI] [PubMed] [Google Scholar]
- 112. Kim MJ, Park JM, Je SM, et al. Effects of a short text message reminder system on emergency department length of stay. Int J Med Inform. 2012;81(5):296-302. 10.1016/j.ijmedinf.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 113. Desai S, Gruber PF, Eiting E, et al. The effect of utilization review on emergency department operations. Ann Emerg Med. 2017;70(5):623-631.e1. 10.1016/j.annemergmed.2017.03.043 [DOI] [PubMed] [Google Scholar]
- 114. Liu T-Y, Tsai M-T, Chen F-C, et al. Impact of coronary risk scores on disposition decision in emergency patients with chest pain. Am J Emerg Med. 2021;48:165-169. 10.1016/j.ajem.2021.04.029 [DOI] [PubMed] [Google Scholar]
- 115. Driver BE, Scharber SK, Fagerstrom ET, Klein LR, Cole JB, Dhaliwal RS. The effect of a clinical decision support for pending laboratory results at emergency department discharge. J Emerg Med. 2019;56(1):109-113. 10.1016/j.jemermed.2018.10.002 [DOI] [PubMed] [Google Scholar]
- 116. Hripcsak G, Sengupta S, Wilcox A, Green RA. Emergency department access to a longitudinal medical record. J Am Med Inform Assoc. 2007;14(2):235-238. 10.1197/jamia.M2206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Johnson KB, Unertl KM, Chen Q, et al. Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc. 2011;18(5):690-697. 10.1136/amiajnl-2011-000308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Politi L, Codish S, Sagy I, Fink L. Use patterns of health information exchange systems and admission decisions: reductionistic and configurational approaches. Int J Med Inform. 2015;84(12):1029-1038. 10.1016/j.ijmedinf.2015.06.012 [DOI] [PubMed] [Google Scholar]
- 119. Ben-Assuli O, Arazy O, Kumar N, Shabtai I. Too much information? The use of extraneous information to support decision-making in emergency settings. Decis Sci. 2022;54(6):632-650. 10.1111/deci.12585 [DOI] [Google Scholar]
- 120. Ayer T, Ayvaci MUS, Karaca Z, Vlachy J. The impact of health information exchanges on emergency department length of stay. Prod Oper Manag. 2019;28(3):740-758. 10.1111/poms.12953 [DOI] [Google Scholar]
- 121. Everson J, Kocher KE, Adler-Milstein J. Health information exchange associated with improved emergency department care through faster accessing of patient information from outside organizations. J Am Med Inform Assoc. 2017;24(e1):e103-e110. 10.1093/jamia/ocw116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Vest JR, Kern LM, Campion TR, Silver MD, Kaushal R. Association between use of a health information exchange system and hospital admissions. Appl Clin Inform. 2014;5(1):219-231. 10.4338/ACI-2013-10-RA-0083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Appari A, Eric Johnson M, Anthony DL. Meaningful use of electronic health record systems and process quality of care: evidence from a panel data analysis of U.S. acute-care hospitals. Health Serv Res. 2013;48(2 Pt 1):354-375. 10.1111/j.1475-6773.2012.01448.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Saef SH, Melvin CL, Carr CM. Impact of a health information exchange on resource use and Medicare-allowable reimbursements at 11 emergency departments in a midsized city. West J Emerg Med. 2014;15(7):777-785. 10.5811/westjem.2014.9.21311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Bailey JE, Wan JY, Mabry LM, et al. Does health information exchange reduce unnecessary neuroimaging and improve quality of headache care in the emergency department? J Gen Intern Med. 2013;28(2):176-183. 10.1007/s11606-012-2092-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. von Wedel P, Hagist C, Liebe J-D, Esdar M, Hübner U, Pross C. Effects of hospital digitization on clinical outcomes and patient satisfaction: nationwide multiple regression analysis across German hospitals. J Med Internet Res. 2022;24(11):e40124. 10.2196/40124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Druckman JN. The implications of framing effects for citizen competence. Polit Behav. 2001;23(3):225-256. 10.1023/A:1015006907312 [DOI] [Google Scholar]
- 128. Entman RM. Framing: toward clarification of a fractured paradigm. J Commun. 1993;43(4):51-58. 10.1111/j.1460-2466.1993.tb01304.x [DOI] [Google Scholar]
- 129. Hwang EJ, Nam JG, Lim WH, et al. Deep learning for chest radiograph diagnosis in the emergency department. Radiology. 2019;293(3):573-580. 10.1148/radiol.2019191225 [DOI] [PubMed] [Google Scholar]
- 130. Kim JH, Han SG, Cho A, Shin HJ, Baek S-E. Effect of deep learning-based assistive technology use on chest radiograph interpretation by emergency department physicians: a prospective interventional simulation-based study. BMC Med Inform Decis Mak. 2021;21(1):311. 10.1186/s12911-021-01679-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Munigala S, Jackups RR, Poirier RF, et al. Impact of order set design on urine culturing practices at an academic medical centre emergency department. BMJ Qual Saf. 2018;27(8):587-592. 10.1136/bmjqs-2017-006899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Laker LF, Froehle CM, Windeler JB, Lindsell CJ. Quality and efficiency of the clinical decision-making process: information overload and emphasis framing. Prod Oper Manag. 2018;27(12):2213-2225. 10.1111/poms.12777 [DOI] [Google Scholar]
- 133. Kim EY, Grossestreuer AV, Safran C, Nathanson LA, Horng S. A visual representation of microbiological culture data improves comprehension: a randomized controlled trial. J Am Med Inform Assoc. 2021;28(9):1826-1833. 10.1093/jamia/ocab056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Thayer JG, Ferro DF, Miller JM, et al. Human-centered development of an electronic health record-embedded, interactive information visualization in the emergency department using fast healthcare interoperability resources. J Am Med Inform Assoc. 2021;28(7):1401-1410. 10.1093/jamia/ocab016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Iselin ER. The effects of information load and information diversity on decision quality in a structured decision task. Account Organ Soc. 1988;13(2):147-164. 10.1016/0361-3682(88)90041-4 [DOI] [Google Scholar]
- 136. Keller KL, Staelin R. Effects of quality and quantity of information on decision effectiveness. J Consum Res. 1987;14(2):200-213. 10.1086/209106 [DOI] [Google Scholar]
- 137. Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3(17):1-10. 10.1038/s41746-020-0221-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330(7494):765. 10.1136/bmj.38398.500764.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Kassirer JP, Wong JB, Kopelman RI. Learning Clinical Reasoning. Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 140. Sackett DL, Haynes RB, Tugwell P, Guyatt GH. Clinical Epidemiology: A Basic Science for Clinical Medicine. 2nd ed. Little Brown & Co; 1991. [Google Scholar]
- 141. Woodruff JN. Accounting for complexity in medical education: a model of adaptive behaviour in medicine. Med Educ. 2019;53(9):861-873. 10.1111/medu.13905 [DOI] [PubMed] [Google Scholar]
- 142. Zavala AM, Day GE, Plummer D, Bamford-Wade A. Decision-making under pressure: medical errors in uncertain and dynamic environments. Aust Health Rev. 2018;42(4):395-402. 10.1071/AH16088 [DOI] [PubMed] [Google Scholar]
- 143. Thammasitboon S, Thammasitboon S, Singhal G. System-related factors contributing to diagnostic errors. Curr Probl Pediatr Adolesc Health Care. 2013;43(9):242-247. 10.1016/j.cppeds.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 144. Peacock WF, Soto-Ruiz KM. Risk stratification for suspected acute coronary syndromes and heart failure in the emergency department. Acute Card Care. 2009;11(3):138-145. 10.1080/17482940902989068 [DOI] [PubMed] [Google Scholar]
- 145. Henrion M, Breese JS, Horvitz EJ. Decision analysis and expert systems. AI Mag. 1991;12(4):64-64. 10.1609/aimag.v12i4.919 [DOI] [Google Scholar]
- 146. Sbaffi L, Walton J, Blenkinsopp J, Walton G. Information overload in emergency medicine physicians: a multisite case study exploring the causes, impact, and solutions in four North England National Health Service Trusts. J Med Internet Res. 2020;22(7):e19126. 10.2196/19126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Hwang U, Weber EJ, Richardson LD, et al. A research agenda to assure equity during periods of emergency department crowding. Acad Emerg Med. 2011;18(12):1318-1323. 10.1111/j.1553-2712.2011.01233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Ouyang H, Wang J, Sun Z, Lang E. The impact of emergency department crowding on admission decisions and patient outcomes. Am J Emerg Med. 2022;51:163-168. 10.1016/j.ajem.2021.10.049 [DOI] [PubMed] [Google Scholar]
- 149. Kruse CS, Mileski M, Dray G, Johnson Z, Shaw C, Shirodkar H. Physician burnout and the electronic health record leading up to and during the first year of COVID-19: systematic review. J Med Internet Res. 2022;24(3):e36200. 10.2196/36200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Li C, Parpia C, Sriharan A, Keefe DT. Electronic medical record-related burnout in healthcare providers: a scoping review of outcomes and interventions. BMJ Open. 2022;12(8):e060865. 10.1136/bmjopen-2022-060865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Tajirian T, Stergiopoulos V, Strudwick G, et al. The influence of electronic health record use on physician burnout: cross-sectional survey. J Med Internet Res. 2020;22(7):e19274. 10.2196/19274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Nijor S, Rallis G, Lad N, Gokcen E. Patient safety issues from information overload in electronic medical records. J Patient Saf. 2022;18(6):e999-e1003. 10.1097/PTS.0000000000001002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Pivovarov R, Elhadad N. Automated methods for the summarization of electronic health records. J Am Med Inform Assoc. 2015;22(5):938-947. 10.1093/jamia/ocv032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. West VL, Borland D, Hammond WE. Innovative information visualization of electronic health record data: a systematic review. J Am Med Inform Assoc. 2015;22(2):330-339. 10.1136/amiajnl-2014-002955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Waller RG, Wright MC, Segall N, et al. Novel displays of patient information in critical care settings: a systematic review. J Am Med Inform Assoc. 2019;26(5):479-489. 10.1093/jamia/ocy193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Hättenschwiler P. Neues erfolgreiches Konzept der Entscheidungsunterstützung. In: Mey H, Pollheimer DL, Affentranger B, eds. Absturz Im Freien Fall—Anlauf Zu Neuen Höhenflügen Gutes Entscheiden in Wirtschaft, Politik und Gesellschaft. Zurich, Switzerland: vdf Hochschulverlag; 2001:. 189-208. [Google Scholar]
- 157. Rao A, Pang M, Kim J, et al. 2023. Assessing the utility of ChatGPT throughout the entire clinical workflow: development and usability study. J Med Internet Res. 2023;25(1):e48659. 10.2196/48659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Hirosawa T, Harada Y, Yokose M, Sakamoto T, Kawamura R, Shimizu T. Diagnostic accuracy of differential-diagnosis lists generated by generative pretrained transformer 3 chatbot for clinical vignettes with common chief complaints: a pilot study. Int J Environ Res Public Health. 2023;20(4):3378. 10.3390/ijerph20043378 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The list of all articles identified by our search strategy with their inclusion/exclusion criteria and the detailed coding of all studies (summarized in Supplementary Material S3), including the verbatim descriptions for each variable and the rationale for their categorization, will be provided upon request.