Abstract
RNA methylation, a prevalent post-transcriptional modification, has garnered considerable attention in research circles. It exerts regulatory control over diverse biological functions by modulating RNA splicing, translation, transport, and stability. Notably, studies have illuminated the substantial impact of RNA methylation on tumor immunity. The primary types of RNA methylation encompass N6-methyladenosine (m6A), 5-methylcytosine (m5C), N1-methyladenosine (m1A), and N7-methylguanosine (m7G), and 3-methylcytidine (m3C). Compelling evidence underscores the involvement of RNA methylation in regulating the tumor microenvironment (TME). By affecting RNA translation and stability through the "writers", "erasers" and "readers", RNA methylation exerts influence over the dysregulation of immune cells and immune factors. Consequently, RNA methylation plays a pivotal role in modulating tumor immunity and mediating various biological behaviors, encompassing proliferation, invasion, metastasis, etc. In this review, we discussed the mechanisms and functions of several RNA methylations, providing a comprehensive overview of their biological roles and underlying mechanisms within the tumor microenvironment and among immunocytes. By exploring how these RNA modifications mediate tumor immune evasion, we also examine their potential applications in immunotherapy. This review aims to provide novel insights and strategies for identifying novel targets in RNA methylation and advancing cancer immunotherapy efficacy.
Keywords: RNA methylation, Tumor immunity, Immunotherapy, Tumor immune evasion, Tumor microenvironment (TME)
Introduction
RNA modification critically influences gene expression through chemical changes to RNA bases and ribose. To date, researchers have identified over 170 types of chemical modifications in various RNA classes across both prokaryotes and eukaryotes [1, 2]. Among these, RNA methylation, which accounts for more than 60% of all RNA modifications, plays a pivotal role in post-transcriptional gene regulation [1, 3, 4]. The major forms of RNA methylation include N1-methyladenosine (m1A), N6-methyladenosine (m6A), 5-methylcytosine (m5C), N7-methylguanosine (m7G), and 3-methylcytidine (m3C), highlighting its extensive presence and significance in shaping the complex landscape of gene regulation [1, 2, 5, 6]. RNA methylation is mediated by three types of proteins: "writers," which catalyze the addition of methyl groups; "readers," which identify these modifications; and "erasers," which remove them, each functioning through unique mechanisms [2, 5, 7] (Fig. 1). These proteins regulate a wide array of RNA types and signaling pathways, including mRNA, tRNA, IncRNA, sRNA, siRNA, snRNA, snoRNA, etc. As a dynamic and reversible process, RNA methylation regulates critical biological processes such as splicing, translation, transport, and RNA stability. Extensive studies have demonstrated that RNA methylation is crucial in the development and progression of various types of cancer, including breast cancer, lung cancer, colorectal cancer (CRC), hepatocellular carcinoma (HCC), gastric cancer (GC), esophageal cancer (EC), prostate cancer (PCa), bladder cancer, ovarian cancer, acute myeloid leukemia (AML), pancreatic cancer, etc. [1, 4, 8–16], underscoring its key role in malignant tumors.
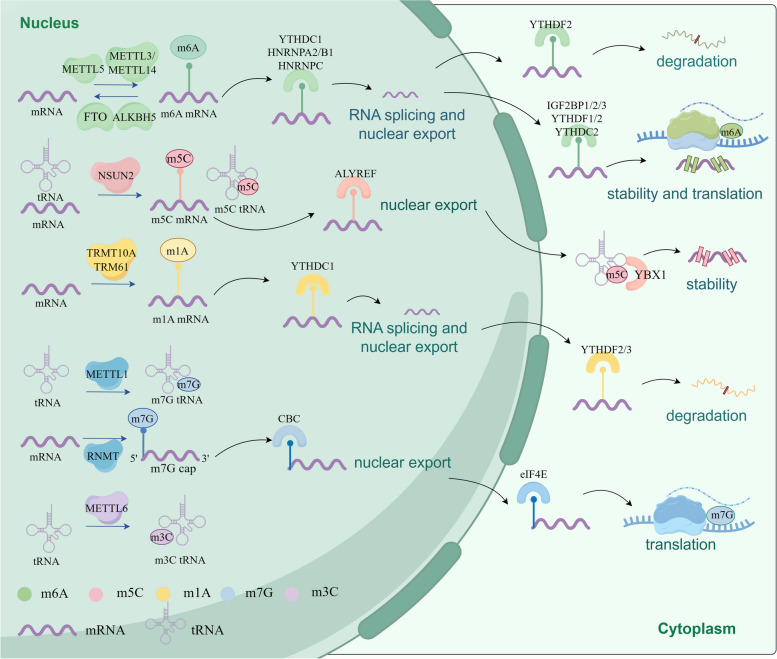
Fig. 1.
The machinery of RNA methylations and RNA fates regulated by RNA methylations. RNA methylations are modulated by their writers (such as METTL3/14 for m6A, NSUN2 for m5C, TRMT10A for m1A, METTL1 for m7G), and removed by their erasers (such as FTO and ALKBH5 for m6A). RNA methylations can regulate the fates of mRNA and mediate their biological functions including splicing, exportation, stability, degradation, translation and so on, after being recognized by their respective readers, including IGF2BP1/2/3, YTHDF1/2/3, YTHDC1/2/3, YBX1, ALYREF, CBC, eIF4E). m6A N6-methyladenosine, m5C 5-methylcytosine, m1A N1-methyladenosine, m7G 7-methylguanosine, m3C 3-Methylcytidine, METTL3 methyltransferase-like 3, FTO obesity-associated protein, ALKBH5 AlkB homolog 5, TET1/2/3 ten-eleven translocation proteins1/2/3, ALKBH1 α-ketoglutarate-dependent dioxygenase ABH1. Figure created with figdraw.com
In recent years, numerous studies have underscored the close association between RNA methylation and various immune biological processes, particularly within the context of tumor immunity [17, 18]. Additionally, abnormal expression of regulatory proteins has been linked to oncogenic activities and enhanced metastatic properties [19]. RNA methylation also plays a crucial role in maintaining homeostasis and in the metabolic reprogramming of the tumor microenvironment (TME), impacting the functionality of immune cells. The TME consists of a complex multicellular matrix that includes immune cells, stromal cells, the extracellular matrix, blood vessels, and other soluble factors [20]. RNA methylation contributes to tumor immune evasion by influencing oncogenic and metastatic capabilities, disrupting TME harmony, and impairing immune cell function. For instance, the m6A writer METTL3 is known to sustain high levels of glycolysis and to induce metabolic reprogramming in HCC [21]. This enzyme also affects macrophage polarization, dendritic cell activation, effector T cell differentiation and proliferation, and the expression of immune checkpoints [22–25]. These interactions highlight how RNA methylation connects the TME and immune cells with the mechanisms of tumor immune evasion. Currently, researchers are exploring potential inhibitors that target METTL3 and other RNA methylation regulators, with the hope that these compounds might be utilized in immunotherapy [26].
Components of the TME exhibit either anti-tumor or pro-tumor properties and play crucial roles in the initiation, progression, invasion, and metastasis of tumors. RNA methylation influences the biological processes of immune cells and other cellular components within the TME. Research has demonstrated that targeting these regulatory proteins can significantly advance cancer immunotherapy [11]. Immunotherapy seeks to boost anti-tumor immune responses by modulating the immune cells of the host's immune system, thereby aiding in the elimination of tumor cells. Focusing on the immune infiltrates within the TME has emerged as a promising approach that can decisively improve the clinical outcomes for cancer patients [27].
RNA methylation significantly influences cellular metabolism and plays a regulatory role in TME and immune cells, crucially impacting tumor immunity. Importantly, it is involved in the development and progression of various human diseases, including AML, CRC, GC, glioblastoma (GBM), renal cell carcinoma (RCC), HCC, etc. [28–31]. This paper will comprehensively explore the role of RNA methylation in tumor immunity and its potential applications in immunotherapy. Our discussion aims to offer new insights and strategies for the development of innovative targets for cancer diagnosis, treatment, and prognosis.
Classification of RNA methylation
N6-methyladenosine
N6-Methyladenosine (m6A), the predominant form of methylation in human mRNA, modifies adenosine at the N6 position and constitutes about 60% of RNA methylation events [4, 8, 32]. This modification is not only prevalent in mammalian mRNA but also occurs across a wide range of non-coding RNAs, including ribosomal RNAs (rRNAs), microRNAs (miRNAs), small nuclear RNAs (snRNAs), small nucleolar RNAs (snoRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) [7, 32–34]. m6A critically influences RNA stability, transport, splicing, and translation, thereby affecting overall RNA expression [2, 8, 32]. The dynamic regulation of m6A involves various components such as methyltransferases (writers), demethylases (erasers), and methylation reading proteins (readers). The m6A methyltransferase complex (MTC), which includes METTL3, METTL14, WTAP, RBM15/15B, ZC3H13, VIRMA, and KIAA1429, plays a vital role in catalyzing m6A modification on different RNA types [25, 35, 36]. The demethylation process is controlled by demethylases like FTO and ALKHB5, although METTL5, responsible for 18S rRNA m6A modification, currently has no known erasers or readers [37]. m6A methylation reader proteins encompass a diverse array of molecules, including insulin-like growth factor 2 mRNA-binding proteins 1/2/3 (IGF2BP1/2/3), YTH domain family proteins 1/2/3 (YTHDF1/2/3), embryonic Lethal Abnormal Vision Like 1 (ELAVL1), eukaryotic translation initiation factors 3 (eIF3), 4E (eIF4E), and 4G (eIF4G), poly(A) binding protein (PABP), etc. [38, 39]. These reader proteins possess the ability to recognize bases bearing m6A modifications, thereby initiating a cascade of downstream effects including translation, splicing, nuclear exportation, and degradation [38, 39] (Fig. 1). Moreover, they can specifically bind to m6A sites on RNA, thereby influencing disease onset and progression by modulating RNA stability and translation. For instance, IGF2BP3 has been implicated in promoting tumorigenesis and predicting poor prognosis in AML through its enhancement of regulator of chromosome condensation 2 (RCC2) stability [40]. Similarly, YTHDF1 has been shown to drive ovarian cancer progression by facilitating EIF3C translation [41]. Numerous studies have highlighted the involvement of m6A regulators in a wide range of human diseases, spanning psychiatric disorders, metabolic diseases, cardiovascular diseases, as well as specific cancers such as AML, brain tumors, bladder cancer, ovarian cancer, etc. [39–45] (Table 1).
Table 1.
The regulator proteins of RNA methylations
| Methylations | Regulator | Molecular | Cancer type | Biological function | References |
|---|---|---|---|---|---|
m6A
|
Writers | METTL3 | CRC | Promote oncogenesis via GLUT1 translation | [46] |
| AML | Promote oncogenesis via ITGA4 stability | [44] | |||
| Endometrial cancer | Inhibit oncogenesis via NLRC5 degradation | [47] | |||
| GC | Promote oncogenesis via HDGF stability | [48] | |||
| METTL14 | HCC | Promote oncogenesis via SIRT6 stability | [49] | ||
| METTL16 | CRC | Promote oncogenesis via PD-L1 translation | [50] | ||
| WTAP | HCC | Promote oncogenesis via HuR translation | [51] | ||
| ZC3H13 | CRC | Inhibit oncogenesis via snail and cyclin D1 translation | [52] | ||
| HCC | Inhibit oncogenesis via PKM2 stability | [53] | |||
| VIRMA | NSCLC | Promote oncogenesis via DAPK3 degradation | [54] | ||
| KIAA1429 | DLBCL | Promote oncogenesis via CHST11 translation | [55] | ||
| Erasers | FTO | CRC | Inhibit oncogenesis via PD-L1 translation | [56] | |
| Melanoma | Promote oncogenesis via PDCD1 translation | [57] | |||
| ALKBH5 | CRC | Promote oncogenesis via AXIN2 stability | [58] | ||
| HCC | Promote oncogenesis via MAP3K8 translation | [59] | |||
| Promote oncogenesis via GLUT4 mRNA stability | [60] | ||||
| Readers | IGF2BP3 | AML | Promote oncogenesis via RCC2 stability | [40] | |
| HCC | Promote oncogenesis via CCL5 translation | [61] | |||
| YTHDF1 | NSCLC | Promote oncogenesis via cyclin D1 translation | [62] | ||
| ELAVL1 | MPNSTs | Promote oncogenesis via HuR translation | [63] | ||
m5C
|
Writers | DNMT2 | AML | Promote oncogenesis via hnRNPK translation | [45] |
| NOP2 | HCC | Promote oncogenesis via c-Myc translation | [12] | ||
| NSUN2 | EC | Promote oncogenesis via GRB2 stability | [10] | ||
| GC | Promote oncogenesis via PIK3R1 translation | [9] | |||
| NSUN6 | Lung cancer | Promote oncogenesis via NM23-H1 translation | [11] | ||
| NSUN7 | HCC | Promote oncogenesis via CCDC9B stability | [12] | ||
| Erasers | ALKBH1 | CRC | Promote metastasis via SMAD7 translation | [64] | |
| Readers | ALYREF | Bladder cancer | Promote oncogenesis via PKM2 stability | [53] | |
| YBX1 | AML | Promote oncogenesis via BCL2 stability | [65] | ||
m1A
|
Writers | TRMT61A | HCC | Promote oncogenesis via PPARδ translation | [13] |
| TRM6 | GC | Promote oncogenesis via ErbB translation | [14] | ||
| Erasers | ALKBH1 | Pancreatic cancer | Promote oncogenesis via mTOR and ErbB translation | [15] | |
| ALKBH3 | Breast cancer | Promote oncogenesis via CSF-1 mRNA stability | [66] | ||
| Ovarian cancer | Promote oncogenesis via CSF-1 mRNA stability | [66] | |||
| Cervical cancer | Promote oncogenesis via ATP5D mRNA translation | [67] | |||
| Readers | YTHDF3 | Cervical cancer | Promote oncogenesis via ATP5D mRNA translation | [67] | |
| YTHDC1 | PDAC | Inhibit oncogenesis via miR-30d mRNA stability | [68] | ||
m7G
|
Writers | METTL1 | ACC | Promote oncogenesis via HK1 translation | [69] |
| HCC | Promote oncogenesis via Cyclin A2 and EGFR translation | [70] | |||
| HCC | Promote oncogenesis via TGF‐β2 mRNA translation | [71] | |||
| Bladder cancer | Promote oncogenesis via EGFR/EFEMP1 mRNA translation | [72] | |||
| WDR4 | HCC | Promote oncogenesis via Cyclin A2 and EGFR mRNA translation | [70] | ||
| RNMT | Gliomas | Promote oncogenesis via c-Myc mRNA translation | [73] | ||
| Breast cancer | Promote oncogenesis via PIK3CA translation | [74] | |||
| WBSCR22 | Pancreatic cancer | Inhibit oncogenesis via ISG15 translation | [16] | ||
| TRMT112 | Pancreatic cancer | Inhibit oncogenesis via ISG15 translation | [16] | ||
m3C
|
Writer | METTL6 | HCC | Promote oncogenesis | [75] |
Abbreviation: ACC Adrenocortical carcinoma, AML Acute myeloid leukemia, CRC Colorectal cancer, DLBCL Diffuse large B-cell lymphoma, EC Esophageal cancer, GC Gastric cancer, HCC Hepatocellular carcinoma, MPNSTs Malignant peripheral nerve sheath tumors, NSCLC Non-small cell lung cancer, PDAC Pancreatic ductal adenocarcinoma
5-methylcytosine
5-Methylcytosine (m5C) is a chemical modification found at the fifth carbon atom of cytosine in RNA molecules. This modification is extensively distributed across various RNA types, including transfer RNA (tRNA), ribosomal RNA (rRNA), messenger RNA (mRNA), non-coding RNA (ncRNA), enhancer RNA (eRNA), and microRNA (miRNA) [76, 77]. Despite its discovery over fifty years ago, the specific functions of m5C are still not fully elucidated [78]. RNA bisulfite sequencing, the most commonly used method to map m5C locations, has shown that these sites are predominantly enriched in the 3′-untranslated regions (3′-UTR) of mRNAs or near the translation initiation codon [79]. m5C plays multiple crucial roles in RNA biology: it enhances mRNA stability and structure, ensures translation accuracy, maintains integrity of tRNA fragments, influences the translation of stop codons in rRNA, and regulates the nuclear export of mature mRNAs [79–83] (Fig. 1).
m5C significantly impacts various biological processes including cell proliferation, differentiation, migration, and apoptosis [84, 85]. The enzymatic addition of m5C is facilitated by "writers" such as DNA methyltransferase 2 (DNMT2) and members of the NOP2/SUN RNA methyltransferase family, including NSUN1 through NSUN7 [85–87]. NSUN2, 3, 6, and DNMT2 have all been demonstrated to methylate tRNAs. Notably, NSUN2 is an essential RNA methyltransferase responsible for introducing m5C to RNA. It methylates most expressed tRNAs, along with other abundant non-coding RNAs and a few of mRNAs [82, 88, 89]. The cancer stem cell functions are controlled by global protein synthesis, but NSUN2 depletion induces decreased m5C level of tRNA and inhibits this process [83]. In budding yeast, NOP2/NSUN1 is essential for ribosome biogenesis, as it deposits m5C on 25S rRNA [90]. NSUN5 modulates protein synthesis by targeting m5C on 28S rRNA [91], while NSUN6 is crucial in regulating cell proliferation in pancreatic cancer and may serve as a potential biomarker for this disease [92]. The removal of m5C is performed by "erasers" such as the Ten-eleven translocation (TET) proteins (TET1-3) and α-ketoglutarate-dependent dioxygenase ABH1 (ALKBH1), which can oxidize m5C to 5-hydroxymethylcytidine (hm5C) [93–95]. Meanwhile, m5C is regulated by its reader proteins, specifically Aly/REF export factor (ALYREF) in mRNA and Y-box-binding protein 1 (YBX1) in tRNA [96] (Fig. 1). Research has shown that ALYREF can directly recognize and bind to the m5C sites in mRNA to promote the export of mRNA from the nucleus to the cytoplasm [97]. YBX1 also binds m5C to regulate its presence in both coding and non-coding RNA and affects rRNA maturation [98, 99]. Additionally, YBX1 interacts with hsa_circ_0062682 to modulate RNA metabolism and splicing, promoting proliferation and invasion in HCC cells, and contributing to sorafenib resistance [100]. Despite the significant roles of these proteins, research into m5C readers for tRNA and rRNA is still in its infancy. ALYREF and YBX1 are linked to the progression of HCC and AML through their influence on BCL2 mRNA stability, suggesting their potential as indicators of poor prognosis and reduced survival [65, 101] (Table 1).
N1-methyladenosine
First identified in the 1960s, N1-methyladenosine (m1A) results from the methylation of adenosine at position 1 and has been detected in tRNAs, rRNAs, mRNAs, and lncRNAs [102–104]. This reversible modification is catalyzed by several enzymes, including tRNA methyltransferase 10 homologue A (TRMT10A) at four specific positions and the TRM6–TRM61 complex, which targets mRNA and mitochondrial tRNA [105, 106]. Additional writers of m1A include nucleomethylin (NML, also known as RRP8) for rRNA, TRMT61A and TRMT61B for mitochondrial tRNA and rRNA, TRMT10B for tRNA, and TRMT10C for mitochondrial tRNA and mRNA [107, 108]. As a post-transcriptional modification, m1A significantly influences RNA stability by affecting base pairing [109]. The removal of m1A is facilitated by "erasers" such as FTO, ALKBH1, ALKBH3, ALKBH5, and ALKBH7, which demethylate various RNA types. Specifically, FTO, ALKBH1, and ALKBH7 target tRNA, whereas ALKBH3 is active on both tRNA and mRNA [57, 64, 110–112]. Although these m1A erasers share some functions with m6A erasers, the specific proteins that recognize m1A in RNA remain unidentified. However, several m6A readers, including YTHDF1/2/3 and YTHDC1, have been shown to detect m1A modifications and directly interact with them [113] (Fig. 1 and Table 1).
N7-methylguanosine
N7-methylguanosine (m7G) is an RNA methylation modification occurring at the N7 position of guanine, accounting for approximately 0.4% of all guanosine residues [114]. This modification is typically found at the 5’ caps and internal sites of mRNA, as well as within rRNA, tRNA, and miRNA [115–117]. The primary enzyme responsible for this modification is methyltransferase-like 1 (METTL1), which partners with the WD repeat domain 4 (WDR4) complex to insert m7G modifications into tRNA, miRNA, and mRNA, thus influencing miRNA structure and biogenesis [118, 119]. Additionally, RNA guanine-7 methyltransferase (RNMT) and RNMT-activating miniprotein (RAM) play critical roles in the efficient cap methylation of mRNA by applying the m7G modification [73, 120]. Furthermore, Williams–Beuren syndrome chromosome region 22 (WBSCR22) and tRNA methyltransferase activator subunit 112 (TRMT112) also contribute to m7G methylation in rRNA [119, 121]. eIF4E is known to recognize the m7G cap of mRNA and plays a crucial role in mediating mRNA translation. Together with the cap-binding complex (CBC), which includes CBP80 and CBP20, it significantly influences the nuclear export and translation of mRNA [122–124] (Fig. 1). Extensive research has linked m7G methylation to various aspects of tumor biology such as stress responses, and the initiation, progression, and prognosis of cancer [125]. Notably, the m7G modification, catalyzed by METTL1 and WDR4 on tRNA, is markedly increased in cancer patients, affecting a range of malignancies including AML, HCC, prostate cancer (PCa), and bladder cancer [71, 72, 126–128]. Additionally, abnormal expression patterns of RNMT have been observed in breast cancer and gliomas, highlighting its potential involvement in tumorigenesis and disease progression [74, 129] (Table 1).
3-Methylcytidine
3-Methylcytidine (m3C) is a modification found specifically in eukaryotic tRNA [130]. This modification occurs at position 32 and plays a crucial role in determining the structure and function of tRNA. Current research suggests that m3C methylation might be catalyzed by specific methyltransferases, with studies pointing to METTL2A, METTL6, and METTL8 as key enzymes involved in this process [75, 130, 131]. However, the understanding of m3C methylation is still limited, and further studies are essential to elucidate the underlying mechanisms and identify the associated regulatory proteins.
RNA Methylation Regulates Tumor Microenvironment (TME)
The tumor microenvironment (TME) comprises the surroundings of tumor cells, encompassing blood vessels, immunocytes, fibroblasts, cytokines, the extracellular matrix, and various stromal components [132, 133]. Immunological elements within the TME coordinate tumor immunity [134–136]. TME significantly influences tumor initiation, progression, metastasis, and response to treatment [134, 137].
RNA methylation plays a pivotal role in shaping the complexity and diversity of the TME, exerting regulatory control over the initiation, progression, and metastasis of various cancers, including HCC, PCa, GC, CRC, pancreatic ductal adenocarcinoma (PDAC), non-small cell lung cancer (NSCLC), small-cell lung cancer (SCLC), malignant peripheral nerve sheath tumors (MPNSTs), etc. [33, 51–54, 63, 138] (Table 1). The m6A modification, a prominent form of RNA methylation, is implicated in a plethora of RNA biology processes, spanning RNA processing, translation, stabilization, splicing, and degradation. Consequently, it exerts influence over the dynamic landscape of the TME, impacting the metabolic and biological functions of tumor cells [138, 139]. Interactions between tumor cells and the TME significantly contribute to processes such as proliferation, differentiation, invasion, metastasis, and development of drug resistance [138]. The TME is typified by three key features: hypoxia, metabolic reprogramming, and immune evasion, which collectively foster the establishment of an immunosuppressive microenvironment and regulate tumor immune evasion through various mechanisms [28, 133, 140] (Fig. 2). Substantial evidence suggests that m6A methylation actively participates in tumor immune evasion by modulating the immunosuppressive TME [132, 141, 142]. Thus, we comprehensively explore the composition of the TME, elucidate the molecular mechanisms governing RNA methylation regulation, and delineate its role in mediating the biological effects of tumor immunosuppression (Fig. 2).
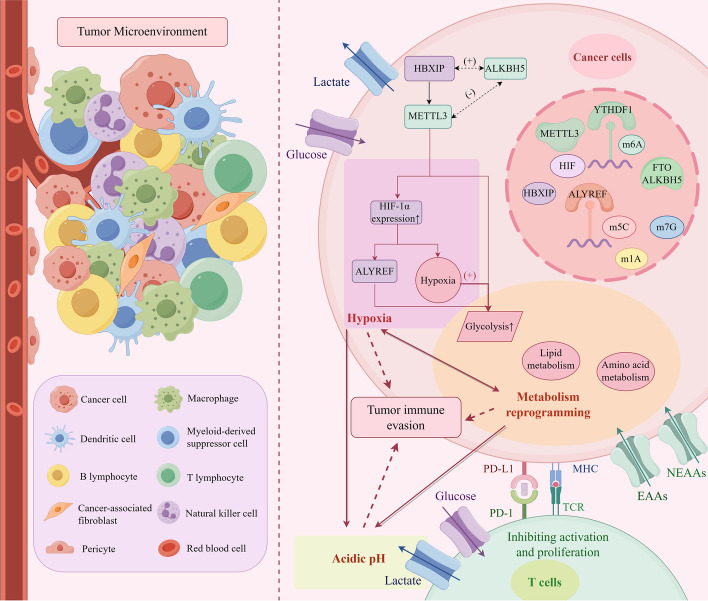
Fig. 2.
The compositions of tumor microenvironment (TME) and RNA methylations promote tumor immune evasion through hypoxia, metabolic reprogramming and acidic pH environment. Hypoxia-inducible factor (HIF) regulates the formation of immunosuppressive TME and promotes tumor immune escape by m6A, m5C, m1A, and m7G RNA methylations. RNA methylations regulate biological metabolism, including glucose metabolism, lipid metabolism and amino acid metabolism, leading to immune cell dysfunction and the formation of an acidic environment, which promotes tumorigenesis, angiogenesis, and tumor cell proliferation. This further aggravates tissue hypoxia and promotes tumor progression. Hypoxia, metabolic reprogramming, and acidic environment interact with each other and work together to contribute to tumor immune escape. TME, tumor microenvironment; HIF, hypoxia-inducible factors. NEAAs, non-essential amino acids; EAAs, essential amino acids. Figure created with figdraw.com
Hypoxic
Hypoxia stands out as a prominent feature within the tumor microenvironment, tightly interlinked with tumorigenesis, angiogenesis, metabolism, and immune response [143, 144]. Excessive hypoxia within tissues disrupts microenvironmental homeostasis, fostering the emergence of a hypoxic, hypoglycemic, and acidic TME conducive to tumor initiation and growth [145, 146]. The rapid proliferation of tumor cells exacerbates oxygen depletion within the tissue, exacerbating microenvironmental hypoxia. Hypoxia-inducible factors (HIF) play a pivotal role in activating genes associated with cellular oxygen homeostasis, including those involved in glucose and lactate metabolism. This activation favors glycolysis over oxidative metabolism, creating a conducive environment for tumor cell proliferation [142, 145–147]. HIF is intricately linked to tumor metabolism and plays a crucial role in immune evasion.
m6A methylation plays a pivotal role in shaping the hypoxic, hypoglycemic, and acidic tumor microenvironment, with the levels of its regulators closely linked to tumor cell content [20, 124, 127]. For instance, YTHDF1, an m6A reader protein, collaborates with other m6A-specific mRNA binding and translation proteins to regulate the methylation and expression of HIF genes, thereby promoting hypoxia-associated tumor progression [62]. Additionally, under hypoxic conditions, HBx-interacting protein (HBXIP) enhances METTL3 expression, a component of the m6A methyltransferase complex. This upregulation of METTL3 results in increased expression of HIF-1α and maintenance of elevated glycolysis levels, thereby accelerating the progression of HCC [21] (Fig. 2). METTL3 and its downstream reader YTHDF1 have been shown to participate in the upregulation of HIF expression and the acceleration of glycolysis [146, 148]. Furthermore, studies indicate that hypoxia suppresses FTO protein expression, correlating with a high recurrence rate and poor prognosis in patients with CRC [56]. Additionally, the overexpression of ALKBH5 promotes tumor progression by establishing a positive feedback loop with HBx protein. This loop leads to the upregulation of ALKBH5 via H3K4me3 epigenetic modification of the ALKBH5 promoter, resulting in the removal of m6A [149]. However, some investigations propose that METTL3 and ALKBH5 contribute to the establishment of opposing hypoxia and reoxygenation conditions, thereby regulating m6A methylation in ischemic heart disease [150]. Therefore, a coordinated interplay between m6A methylation and hypoxia, forming a positive feedback loop, is essential to promote tumor proliferation (Fig. 2).
In summary, m6A methylation promotes the formation of a hypoxic microenvironment, triggering a cascade of downstream biological reactions that influence immune cell functions and tumor biological behaviors. This intricate interplay significantly impacts the onset and progression of malignancies [21, 56, 149, 150]. In bladder cancer, HIF-1α promotes the upregulation of m5C expression by activating ALYREF. This induction of glycolysis accelerates tumor growth, contributing to the establishment of a hypoxic tumor immune microenvironment (TIME) that facilitates immune evasion [97]. Addressing hypoxia represents an effective strategy to enhance the antitumor immune response [151].
Metabolic reprogramming
Metabolic reprogramming stands out as a significant mechanism for tumor immune evasion [151]. The process of RNA modification within metabolic reprogramming encompasses three types of metabolites: glucose, lipid, and amino acids (Fig. 3). Extensive evidence has illustrated that RNA methylation regulates the homeostasis of TME through these three substance metabolisms, subsequently influencing tumor immune evasion [135] (Fig. 2).
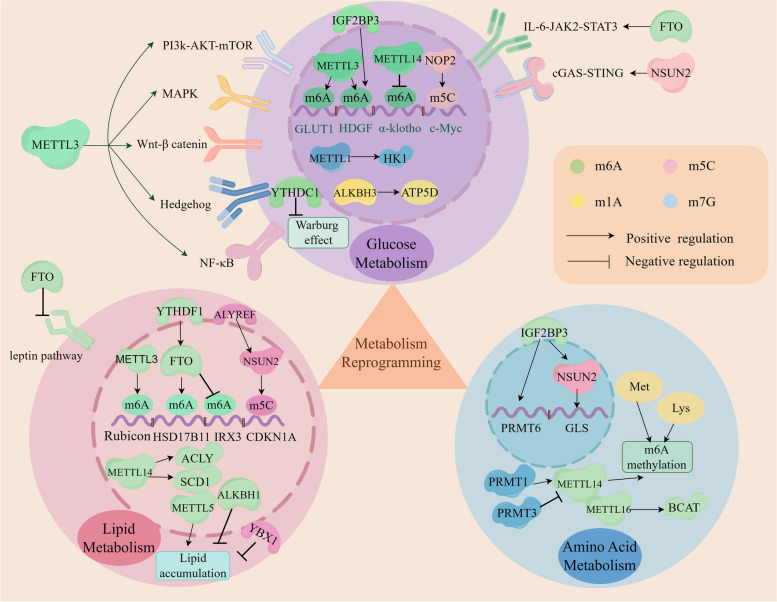
Fig. 3.
RNA methylations participate in metabolic reprogramming of the TME, including glucose metabolism, lipid metabolism and amino acid metabolism. RNA methylations regulate the expression of glycolysis-associated genes (GLUT1, Gys2, HDGF) and signal pathways (PI3K-AKT, mTORC1, MAPK, Wnt-β catenin, Hedgehog, NF-κB, IL-6/JAK2/STAT3, cGAS/STING) and enhance Warburg effect through their regulators, such as METTL1, METTL3, METTL14, NOP2, NSUN2, FTO, ALKBH3, IGF2BP3, YTHDC1 and. m6A and m5C accelerate lipid accumulation. m6A, m5C and m7G modulate the metabolisms of glutamine, arginine, methionine and lysine. These methylations impact tumor cell immunogenicity, proliferation, immune escape as well as tumor progression. ACLY, ATP citrate lyase; SCD1, stearoyl-CoA desaturase1; BCAT1, branched-chain amino acid transaminase 1; Met, methionine; Lys, lysine; PRMT1, protein arginine methyltransferase1. Figure created with figdraw.com
Glucose metabolism
Glucose metabolism serves as a pivotal pathway for tumor cells. A notable metabolic trait, termed the Warburg effect, describes the preference of tumor cells for glycolytic pathways over oxidative phosphorylation (OXPHOS), even in oxygen-rich environments [152]. This metabolic signature is closely intertwined with the immune functions of the TIME, impacting the biological characteristics of various immune cells, including activated T cells, dendritic cells (DCs), natural killer (NK) cells, and M1 macrophages. Furthermore, cancer cells can outcompete immune cells for nutrients, thereby suppressing the tumor immune response [153, 154].
Studies have demonstrated that m6A regulators promote glycolytic reprogramming through various glycolytic-associated genes and signaling pathways in multiple cancers [142]. For instance, METTL3 can induce GLUT1 mRNA translation and facilitate glucose uptake and lactate generation, thus activating mTORC1 signaling in colorectal cancer [46] (Fig. 3). Furthermore, METTL3 exerts a significant influence on the progression of colorectal cancer through glycose metabolism via an m6A-IGF2BP3-dependent mechanism [155]. Additionally, in gastric cancer, IGF2BP3 directly recognizes the m6A site on HDGF (Heparin Binding Growth Factor) mRNA, a process initiated by METTL3. This recognition promotes tumor angiogenesis and glycolysis [48] (Fig. 3). Additionally, METTL3 can also activates others signal pathways, including the mitogen activated protein kinase (MAPK) signaling pathway, the Wnt-β catenin pathway, the Hedgehog signaling pathway, the NF-κB signaling pathway, as well as METTL3-IGF2BP2-Gys2 (the liver-specific glycogen synthase) axis [156–161]. Consequently, glycolysis process accelerates, and hepatic glycogenesis continues, providing essential conditions for tumor proliferation (Fig. 3). There is evidence indicating that METTL14 efficiently utilizes glucose to induce glomerular endothelial cell injury by modifying m6A methylation, resulting in the downregulation of α-klotho expression [49, 162].
The demethylase FTO has been shown to be responsible for decreasing m6A methylation of Apolipoprotein E (APOE) mRNA and modulating the IL-6/JAK2/STAT3 signaling pathway, thereby inhibiting tumor glycolysis and abrogating tumor growth [163] (Fig. 3). Furthermore, the m6A reader YTHDC1 contributes to suppressing glycolysis by attenuating the Warburg effect, ultimately impeding pancreatic tumorigenesis [68].
It has been reported that NSUN2, the methylase responsible for m5C modification, can bind with glucose to sustain the oncogenic activity of tumor cells. This process occurs through the promotion of three prime repair exonuclease 2 (TREX2) mRNA expression and activation of the cGAS/STING pathway, thereby mediating immunotherapy resistance [164]. Additionally, NOP2 can enhance glycolysis by upregulating the expression of glycolytic genes and increasing the m5C content of c-Myc mRNA [165].
Additionally, studies have demonstrated that ALKBH3, an m1A demethylase, positively regulates the translation of ATP5D mRNA, thereby accelerating glycolysis [67]. METTL1 has also been found to upregulate the expression of the glycolysis rate-limiting enzyme HK1 [69]. Numerous pieces of evidence highlight the critical role of RNA methylation regulators in cancer cell glycolysis (Fig. 3).
Lipid metabolism
Fatty acids, as a significant metabolic pattern, play crucial roles in maintaining essential cellular physiological functions and participating in various cellular activities. Aberrant lipid metabolism has emerged as a key factor in tumorigenesis [166]. Dysregulated lipid metabolism not only suppresses the anti-tumor capabilities of immune cells but also facilitates immune evasion by cancer cells, thus impairing the immune response and reshaping the immunosuppressive TME. This alteration is characterized by both catabolic and anabolic processes closely associated with tumor immune evasion [167, 168]. Lipid metabolism encompasses processes such as synthesis, degradation, and storage of lipids. Tumor cells utilize these metabolites for membrane assembly and energy generation, significantly contributing to tumor cell proliferation [168].
Several pieces of evidence suggest that RNA methylation plays a crucial role in lipid metabolism in various cancers. Specifically, research indicates that YTHDF1 can bind to m6A-marked Rubicon mRNA, a process mediated by METTL3, ultimately impeding the fusion of autophagosomes with lysosomes and obstructing the clearance of lipid droplets (LDs) [169]. Additionally, overexpression of METTL14 enhances the protein levels of ATP citrate lyase (ACLY) and stearoyl-CoA desaturase 1 (SCD1), leading to increased production of triglycerides and cholesterol and accumulation of LDs [170] (Fig. 3). Moreover, the demethylase FTO promotes the formation of LDs in EC cells by facilitating the expression of the HSD17B11 gene via a YTHDF1-dependent mechanism [171]. Additionally, FTO enhances adipogenesis and fat deposition while inhibiting lipolysis by suppressing IRX3 expression and the leptin pathway, thereby promoting the progression of lipid disorder diseases [172] (Fig. 3). However, the demethylase ALKBH1 reduces the uptake and synthesis of lipids, leading to a decrease in hepatic lipid accumulation, thereby alleviating hepatic steatosis and the progression of nonalcoholic fatty liver disease (NAFLD) [173]. In vitro and mouse models have shown that METTL5 knockdown significantly reduces the levels of triglycerides, cholesterol, and intracellular free fatty acids, effectively blocking the progression of HCC [174]. Knockdown of NSUN2 decreases the protein expression of cyclin-dependent kinase inhibitor 1A (CDKN1A) in a m5C-ALYREF-dependent manner, indicating that the NSUN2-m5C-ALYREF signaling pathway plays a significant role in suppressing adipogenesis [81]. Similarly, m5C inhibits adipogenesis via the ALYREF-m5C-YBX2 and ALYREF-m5C-SMO pathways [175]. These findings suggest that various RNA modification proteins regulate the lipid metabolism of cancer cells through multiple mechanisms and signaling pathways, potentially serving as promising therapeutic targets and providing a research direction for immunotherapy.
Amino acid metabolism
Abnormal amino acid metabolism has been shown to suppress the anti-tumor immune capacity of immune cells and mediate tumor immune evasion [176]. Specifically, the reprogramming of glutamine metabolism plays a vital role in the anti-tumor immune response within TME [177]. Glutamine synthesis, as a critical proliferative metabolite, is widely upregulated in cancer-associated fibroblasts (CAFs) and is essential for lymphocyte proliferation, protein synthesis, and antibody production. Studies have demonstrated that blockade of glutamine metabolism alleviates the immunosuppressive TME and overcomes tumor immune evasion, ultimately inhibiting tumor growth [178, 179].
In the context of AML, branched-chain amino acid (BCAA) transaminase 1 (BCAT1) and BCAT2 drive carcinogenesis by reprogramming BCAA metabolism. METTL16 promotes BCAT expression in an m6A-dependent manner, thereby regulating metabolism to facilitate cancer progression [180]. Additionally, IGF2BP2 recognizes m6A to regulate the expression of critical targets in glutamine metabolism, making it a potential therapeutic target in AML [181]. Moreover, IGF2BP3 stabilizes PRMT6 (protein arginine methyltransferase 6) mRNA, which in turn mediates histone H3R2me2a methylation and maintains the function of leukemia stem cells (LSCs) [182, 183]. Additionally, PRMT3 interacts with METTL14 and is involved in its arginine methylation, leading to the downregulation of METTL14 expression levels. Depletion of PRMT3 enhances sensitivity of EC cells to ferroptosis by increasing m6A levels of Glutathione peroxidase 4 (GPX4) mRNA [184]. METTL14 also recognizes histone H3 trimethylation at lysine-36 (H3K36me3) to interact with the m6A methyltransferase complex (MTC) and affect m6A methylation [185]. Furthermore, Protein arginine N-methyltransferase 1 (PRMT1) catalyzes the methylation of METTL14 at arginine 255 (R255), stabilizing the m6A methyltransferase complex METTL3/METTL14 and facilitating m6A methylation [186].
It has been shown that metabolites originating from methionine metabolism contribute to m6A methylation and the translation of immune checkpoints. Furthermore, restricting methionine in the diet inhibits tumor growth and improves the anti-tumor immune response by enhancing the abundance and cytotoxicity of CD8+ T cells [187] (Fig. 3).
Therapies utilizing glutamine blockade to inhibit tumor cell metabolism have been proposed; however, these approaches equally damage immune cell metabolism, and as of yet, none have been approved for practical application [188]. Furthermore, depletion of the m6A-specific reader YTHDF1 in combination with PD-1 blockade has shown enhanced efficacy in anti-tumor therapy. A low protein diet supplemented with methionine and lysine has been found to enhance the expression of m6A and reduce the expression of FTO and ALKBH5, possibly through regulation by the transcription factor PPARγ [189]. Additionally, NSUN2-methylated lncRNA enhances the stability of glutaminase (GLS) mRNA by upregulating glutaminase expression through interaction with the IGF2BP3/HUR complex, thus facilitating reprogramming of glutamine metabolism and accelerating gastric cancer progression [190] (Fig. 3). In m7G-associated molecular subtypes of sepsis, subtypes with higher amino acid metabolism activity are characterized by more abundant activated macrophages, M0 and NK cells, and higher expression of immune regulatory genes [191]. Not only is RNA methylation able to regulate multiple types of amino acid metabolism, but conversely, amino acid metabolism plays a critical role in RNA methylation [70].
Taken together, abnormal metabolism can result in immune system dysfunction, tumor oncogenesis, progression, invasion, and immune evasion. The hypoxic microenvironment promotes glycolysis, exacerbating tissue hypoxia. Methylation, hypoxia, and glycolysis form a positive feedback loop that impacts various downstream responses (Fig. 2). These aberrant conditions suppress immune cell functions and promote tumor biological behavior.
RNA methylation regulates tumor innate immunity
The oncogenic process triggers the host innate immunity, which encompasses a variety of immune cells, including macrophages, monocytes, neutrophils, myeloid-derived suppressor cells (MDSCs), dendritic cells (DCs), and others. The characteristics of these immune cells are also influenced by features of the TME, such as hypoxia and metabolic abnormalities [192, 193]. Therefore, we will explore several immune cells closely associated with RNA methylation and tumor innate immunity.
Tumor-associated macrophages
Macrophages play a critical role in the immune response, encompassing both innate and adaptive immunity through activities such as phagocytosis of foreign material, antigen presentation, and secretion of proteins and cytokines across various phenotypes [194]. Tumor-associated macrophages (TAMs) represent a major infiltrating cell type within tumors and contribute significantly to the formation of the tumor microenvironment [195, 196]. TAMs originate from bone marrow monocytes, including resident macrophages and circulating monocytes recruited to the TME [197]. M-MDSCs (monocyte-related myeloid-derived suppressor cells) serve as the primary circulating precursors of TAMs and can be induced into TAMs by chemokines, as well as by the immunosuppressive programming of MDSCs [198].
TAMs are typically categorized into two distinct functional subtypes: classical activated M1 macrophages and alternatively activated M2 macrophages [199]. These infiltrating macrophages are widely considered to be involved in various aspects of tumorigenesis, including progression, invasion, angiogenesis, metastasis, and drug resistance [199, 200]. High levels of infiltration are closely associated with poor prognosis and therapeutic response, including targeted therapy, radiotherapy, and chemotherapy [201]. Within the TME, elements such as fibrosis, hypoxia, metabolic reprogramming, and cytokines contribute to the phenotypic variation of TAMs, inducing polarization toward M1/M2 phenotypes [195]. Initially, macrophages exhibit a pro-inflammatory M1 secretion profile during the early healing stage, which transitions to an anti-inflammatory M2 secretory profile in the later stage [195]. While M1 macrophages are generally considered anti-tumorigenic, and M2 macrophages are considered pro-tumorigenic [195, 202]. It's worth noting that M1 macrophages can also express M2 markers and vice versa [203]. TAMs demonstrate a high degree of plasticity, capable of polarizing pro-tumor M2-type macrophages into M1 TAMs and altering their functions, thereby exerting a role in suppressing tumor progression [204].
Research has demonstrated that RNA methylation regulates macrophage polarization through reprogramming of the TME and various signaling pathways [204]. METTL3 plays a crucial role in macrophage polarization [22]. Yin et al. showed that depletion of METTL3 increased the expression of M1/M2-associated genes and promoted the polarization of bone marrow-derived macrophages (BMDMs) toward both M1 and M2 TAMs via NF-κB and STAT3 pathways, thereby enhancing the infiltration of TAMs into tumors [205, 206]. In models with METTL3 depletion, the therapeutic efficacy of PD-1 blockade was reduced, leading to accelerated tumor progression and distant metastasis [205]. Shu et al. demonstrated that METTL3 drove M1 polarization of macrophages and accelerated liver fibrosis through m6A methylation [207]. Similarly, Liu et al. found that upregulation of METTL3 expression was accompanied by an increase in M1 macrophages and a decrease in M2 macrophages, a process mediated by STAT1 mRNA [208]. Furthermore, lactic acid facilitated M2 polarization by activating METTL3 via the Trib1/ERK/STAT3 pathway [209]. Knockdown of METTL3/METTL14 significantly inhibited macrophage activation and secretion and slowed the progression of liver fibrosis [210, 211]. Additionally, WTAP and RBM15 interact with M1 macrophages and mediate downstream inflammatory responses [212] (Fig. 4).
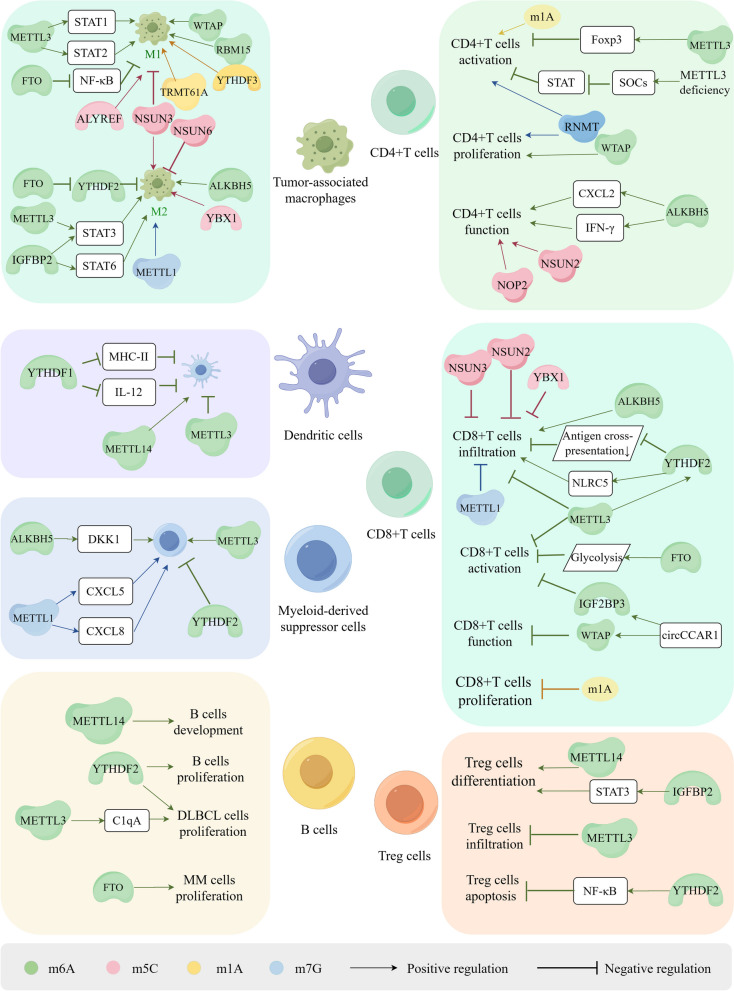
Fig. 4.
Mechanisms of RNA methylations regulate of the biological functions of immune cells in the TME, including immune cell differentiation, development, infiltration, activation, proliferation and apoptosis. RNA methylations promote tumor-associated macrophages (TAMs) polarization towards M1 macrophage or M2 macrophage and regulate the proliferation and infiltration of dendritic cells (DCs), Myeloid-derived suppressor cells (MDSCs) and regulatory T (Treg) cells. Furthermore, RNA methylations play a significant role in the differentiation and development of T cells. m6A and m5C suppress the infiltration and activation of CD8+ T cells as well as mediating their dysfunction. m1A and m7G also participate in the activation, infiltration and proliferation of CD4+T cells and CD8+T cells, however, the regulators of m1A and m7G in these processes remain further investigation. RNA methylations regulate tumor immune response and evasion through impacting various biological functions of immune cells, such as the differentiation, development, infiltration, activation, proliferation and apoptosis of immune cells. Figure created with figdraw.com
Knockdown of the demethylase FTO inhibited the polarization of both M1 and M2 macrophages by dysregulating the expression of STAT1 in M1 macrophages and STAT6 in M2 macrophages. This dysregulation occurred via suppression of the NF-κB signaling pathway and silencing of YTHDF2 [212]. Additionally, knockdown of ALKBH5 resulted in decreased infiltration of M2 macrophages [59, 213]. Studies have indicated that IGFBP2 plays a crucial role in shifting M1 macrophages towards M2 polarization through the STAT3 or STAT6 pathways, thereby contributing to the formation of an immunosuppressive microenvironment [196, 214, 215] (Fig. 4).
The polarization of TAMs is also regulated by other RNA modifications. In a prognostic score model, NSUN3 knockdown has been shown to decrease the infiltration of M2 macrophages while increasing the infiltration of M1 macrophages [216, 217]. Intriguingly, NSUN6 inhibits the expression of macrophage-associated chemokines by promoting HDAC10 expression, thereby suppressing the recruitment of M2 macrophages and improving prognosis in bladder cancer patients [218]. High expression of YBX1 is associated with the infiltration of M2 macrophages and T cell depletion, which could potentially be targeted using M1 polarization agents in synergy with immunotherapy [219]. In Abdominal Aortic Aneurysm (AAA), immune infiltration analysis has shown that YTHDF1/2/3, YTHDC1, RRP8, and TRMT61A are upregulated genes associated with the infiltration of M1 macrophages, while FTO and ALKBH1 are downregulated [220].
The m1A reader, YTHDF3, facilitates the polarization of M1 macrophages and exacerbates inflammation [220]. ALKBH3-mediated m1A demethylation stabilizes the cytokine macrophage colony-stimulating factor (CSF-1) mRNA, promoting the progression of breast and ovarian cancer [66].
Moreover, m7G methylation is positively correlated with the abundance of M2 macrophages [69]. METTL1 also plays a role in the polarization of TAMs. Elevated METTL1 expression correlates with increased infiltration of M2-like macrophages, while inhibition of METTL1 and decreased m7G methylation of tRNAs induce TAMs towards an M1-like endotype in preclinical models of PCa [128]. Data from The Cancer Genome Atlas (TCGA) database indicates that ALYREF, ZC3H13, WTAP, and METTL1 are negatively associated with M1 macrophages [221] (Fig. 4).
Taken together, these findings underscore the significant role of RNA methylation in the polarization of TAMs. These RNA methylation regulators have the ability to catalyze and modulate the phenotypes of TAM polarization, thereby influencing the infiltration of TAMs within tumors and ultimately shaping the immunosuppressive microenvironment. Moreover, these insights provide novel targets and strategies for immunotherapy.
Dendritic cells
Dendritic cells (DCs) are pivotal antigen-presenting cells that play a crucial role in both innate and adaptive immune responses [222]. As part of the antigen-presenting cell (APC) population, which also includes macrophages and B lymphocytes, DCs are capable of uptaking, processing, and presenting antigens to T cells [223]. However, within the TME, the function and activity of DCs are regulated by immunosuppressive factors and interactions with other immune cells, potentially leading to immune evasion and exacerbating oncogenesis [223, 224].
Recent studies have shed light on the involvement of m6A methylation in DC-mediated anti-tumor responses. Knockdown of YTHDF1 has been shown to enhance the expression of MHC-II on DCs and increase the secretion of interleukin-12 (IL-12), thereby bolstering adaptive immune responses [225]. METTL3 has been implicated in the regulation of DC activation and the mediation of immune dysfunction through m6A methylation [23, 226] (Fig. 4). Additionally, the tumor suppressor gene METTL14 is positively correlated with DCs, and its knockdown has been found to promote immunosuppression in breast cancer [227, 228]. Researchers have also demonstrated that the m6A-YTHDF1 axis restricts the cross-priming capacity of DCs, and loss of YTHDF1 enhances antigen presentation capacity [229]. The infiltration of DCs has been correlated with the ALKB family; however, further exploration is warranted to elucidate the interaction between them [230].
Myeloid-derived suppressor cells
As a significant component of TME, myeloid-derived suppressor cells (MDSCs) originate from the bone marrow and serve as precursors to dendritic cells, macrophages, and granulocytes. These cells possess the ability to inhibit T cell-mediated immune responses, thereby impacting cancer outcomes [231, 232]. Studies have revealed that expression levels of METTL3 are closely associated with the expansion of MDSCs, and loss of METTL3 inhibits the accumulation and immunosuppressive capacity of MDSCs, resulting in increased infiltration of CD4+ and CD8+ T cells [233, 234]. Furthermore, the expansion and suppressive function of MDSCs are enhanced in YTHDF2-knockout mice [235, 236]. Additionally, ALKBH5 facilitates MDSCs accumulation by inducing the expression of Dickkopf-related protein 1 (DKK1) [58, 237] (Fig. 4). Moreover, METTL1 upregulates the expression of chemokines CXCL5 and CXCL8 in an m7A-dependent manner, leading to MDSCs accumulation and immunosuppression in HCC and intrahepatic cholangiocarcinoma (ICC) [238, 239] (Fig. 4).
RNA methylation regulates tumor adaptive immunity
RNA methylation has emerged as a critical regulator of adaptive immunity, shaping the outcome of the host immune response [240, 241]. Adaptive immunity in tumor immune responses primarily involves T lymphocytes and B lymphocytes. Research indicates that RNA methylation plays a pivotal role in the development, differentiation, activation, exhaustion processes, and therapeutic responses of these immune cells by modulating the translation and expression of RNA and proteins [242]. Below, we delve into the specific regulatory mechanisms of RNA methylation in adaptive immunity and immune cells.
T lymphocytes
T lymphocytes, critical components of adaptive immunity, originate from bone marrow progenitors and undergo maturation in the thymus, where they play pivotal roles. Naïve T cells possess the ability to differentiate into various subsets, such as T helper (Th) cells, depending on their stem cell features [243]. During thymic development, T cell precursors undergo positive or negative selection, leading to differentiation into CD4+ or CD8+ T cells in the thymic cortex and regulatory T (Treg) cells in the thymic medulla [244]. Numerous studies have highlighted the role of RNA methylation in mediating various functions of T cells, including proliferation, activation, and apoptosis, through the involvement of multiple RNA methylation regulators [245, 246] (Fig. 4).
CD4+T cells
Researchers have demonstrated that inhibiting METTL3 facilitates the activation of CD4+ T cells while suppressing the differentiation of effector T cells, particularly Treg cells, by reducing the expression of Foxp3 in a m6A-dependent manner [247]. Inhibition of METTL3 reduces m6A methylation levels, promotes cell apoptosis, hinders effector T cell differentiation, and inhibits allogeneic CD4+ T cell responses [24]. In naïve T cells deficient in METTL3, the activity of the SOCs family is enhanced, which encodes STAT inhibitory proteins, thus suppressing STAT activation and impeding the proliferation and differentiation of T cells [248]. Similarly, WTAP and METTL3 exhibit similar characteristics in regulating mRNA stability. CD4+ T cells deficient in WTAP undergo apoptosis and exhibit reduced proliferation upon TCR signal activation [249]. The presence of m6A methylase is essential for T cells to exert immune functions. Additionally, the m6A demethylase ALKBH5 enhances the stability of CXCL2 and IFN-γ mRNA and proteins by reducing m6A modification expression, thereby preserving CD4+ T cell immune function [250] (Fig. 4).
During HIV-1 infection of CD4+ T cells, m6A levels are upregulated, potentially mediated by variations in the activity of m6A writers or erasers in T-cells [251, 252]. Overexpression of YTHDF3 has been shown to decrease the production and infection of HIV-1 by incorporating into viral particles [253, 254]. Evidence suggests that NOP2 promotes m5C methylation in HIV-1 and interacts with TAR by competing with Tat protein, thereby inhibiting HIV-1 replication and transcription, prolonging the incubation period [255]. Additionally, IL-17 treatment reduces the posttranslational modification of YBX1 in CD4+ T cells, inhibiting HIV infection by suppressing HIV reverse transcription [256].
In patients with Systemic lupus erythematosus (SLE), the levels of m5C and NSUN2 expression are decreased in CD4+ T cells, and hypermethylated m5C is involved in immune-related and inflammatory pathways, including the immune system, cytokine signaling, and interferon (IFN) signaling [257]. m7G methylation is essential for T cell activation. RNMT, a key regulator of T cell activation, controls ribosome generation, enhances mRNA translation efficiency, and promotes proliferation and differentiation [258]. Although tRNA modification is a dynamic process during T cell activation, the m1A methylation at position 58 of tRNA remains constant, suggesting its involvement in the translation of T cell activation [259] (Fig. 4).
CD8+T cells
Numerous studies have highlighted a close association between RNA methylation and the infiltration of CD8+ T cells in cancers [260–262] (Fig. 4). Tumors exhibiting high m6A expression demonstrate stronger immunogenicity by increasing HLA-A content, which enhances immunosurveillance and activates immune cell infiltration [263]. For instance, YTHDF2 depletion enhances the activation and antitumor response of CD8+ T cells by augmenting their antigen cross-presentation ability and the abundance of infiltrating immune cells [229, 264, 265]. Moreover, METTL3 knockdown inhibits the generation of MDSCs, leading to the activation and proliferation of CD4+ and CD8+ T cells [234]. Conversely, a study has shown that METTL3 overexpression increases CD8+ T cell proportions, attenuates immune evasion, and inhibits the progression of EC by promoting m6A modifications of NLRC5 via a YTHDF2-dependent mechanism [47]. Evidence has shown that IGF2BP3 inhibits the activation of CD8+ T cells and facilitates tumor immune evasion [61, 266]. A recent study has demonstrated that exosome-derived circCCAR1 upregulates WTAP expression by binding with IGF2BP3, thereby enhancing its stability through increased m6A expression. CircCCAR1 can be ingested by CD8+ T cells, causing them to malfunction by stabilizing the PD-1 protein [267]. Furthermore, tumor cells utilize glycolysis promoted by FTO to inhibit the activation and effector states of CD8+ T cells, which can be reversed by combining an FTO inhibitor with anti-PD-L1 blockade [268]. These findings suggest a promising therapeutic strategy for multiple types of cancers. However, as an m6A demethylase, elevated levels of ALKBH5 have been shown to enhance the infiltration of CD8+ T cells [269]. The mechanisms underlying the relationship between demethylases and the activation of CD8+ T cells require further exploration.
NSUN2 boosts m5C methylation to stabilize TREX2 mRNA, reducing the infiltration of CD8+ T cells and fostering resistance to anti-PD-L1 immunotherapy through activation of the cGAS/STING pathway [164]. Additionally, NSUN3 expression inversely correlates with the infiltration of CD8+ T cells [217, 270]. Knockdown of the m5C reader YBX1 decreases the infiltration of MDSCs and Tregs while increasing the infiltration of CD8+ T cells, thereby enhancing the anti-tumor immune response [271]. m1A negatively regulates the proliferation of CD8+ T effector cells in colon cancer [272]. Similarly, high expression of m7G is associated with decreased cytotoxic CD8+ T cell infiltration and increased M2 macrophage infiltration [69, 128, 273] (Fig. 4). Together, these findings suggest that RNA methylation could be a promising therapeutic target for enhancing the tumor immune response.
Treg cells
m6A methylation has been demonstrated to regulate the proliferation of immunosuppressive Treg cells [43]. METTL14 deficiency inhibits the differentiation of naïve T cells into Treg cells, and METTL14-deficient Treg cells exhibit impaired function in suppressing inflammation induced by naïve T cells. However, adoptive transfer of Treg cells can alleviate this impaired function [274, 275]. Additionally, there is a negative correlation between METTL3 expression levels and Treg infiltration [276]. Insulin-like growth factor binding protein 2 (IGFBP2) contributes to the activation of the STAT3 signaling pathway, leading to Treg differentiation and the creation of a suppressive tumor environment [277]. Studies have shown that the loss of YTHDF2 in Tregs promotes Treg apoptosis and suppresses their function in the TME, thereby inhibiting tumor progression through the YTHDF2-m6A-NF-κB pathway [278, 279] (Fig. 4).
B lymphocytes
B lymphocytes are integral to the adaptive immune response, functioning by producing antibodies, which include memory B cells and plasma cells [280]. Evidence has verified that RNA methylation and its regulatory factors are involved in various B cell-associated diseases [281, 282]. RNA m6A methylation plays a critical role in the development, maturation, and antibody secretion of B cells [281, 283–285] (Fig. 4). The deletion of METTL14 constrains the development from large pre-B cells to small pre-B cells by reducing m6A methylation levels, and the deletion of YTHDF2 results in a significant block of pro-B cell proliferation [283]. Studies have shown that METTL3 inhibits the complement pathway by mediating C1qA methylation and enhances resistance to Rituximab, thereby facilitating the progression of diffuse large B-cell lymphoma (DLBCL) [286]. In AML, METTL3 also plays a role in pre-B cell to macrophage trans-differentiation, and this effect can be inhibited by the METTL3 inhibitor [287]. The writer KIAA1429 also plays a role in DLBCL progression [55]. Additionally, YTHDF2 can identify m6A sites on alkaline ceramidase 2 (ACER2) mRNA, promoting the proliferation of DLBCL cells and contributing to disease progression [282]. METTL14-mediated YTHDF2 activity facilitates the formation of germinal centers and regulates positive selection and cell cycle regulation of germinal center B cells in an m6A-dependent manner [288, 289]. Furthermore, the m6A reader YTHDF1 recognizes and destabilizes Epstein–Barr virus (EBV) mRNA, thereby suppressing EBV infection and replication, which is significant in B-cell malignancies [290]. Expression levels of m6A are decreased in plasma cells of patients with multiple myeloma (MM) due to FTO-mediated demethylation, and inhibiting FTO suppresses MM cell proliferation, migration, and invasion [291].
Accordingly, RNA methylation serves a crucial role in both innate and adaptive immune responses, influencing various biological processes within immune cells. These include guiding macrophage polarization towards the M2 phenotype, promoting the accumulation of MDSCs, affecting the function of DCs in antigen presentation, reducing the infiltration and activation of effector T cells, influencing the differentiation of Tregs, and contributing to abnormal proliferation of B cells.
RNA Methylation Mediates Tumor Immune Evasion
The tumor microenvironment is distinguished by an immunosuppressive state that is instrumental in both the downregulation of immune cell functions and the facilitation of tumor immune evasion [135, 292]. This evasion significantly contributes to the creation of an immunosuppressive environment that not only promotes oncogenesis but also allows for its uncontrolled proliferation [293]. Antitumor responses primarily involve activated CD8+ T cells, which specifically recognize and target tumor antigens presented by APCs. These cells then exert cytotoxic effects to destroy tumor cells [294]. However, tumor cells have the ability to emit suppressive signals that impair the immune functions of T cells, thus hindering effective immune responses [293].
The immune system is critical in mounting anti-tumor responses. Yet, tumor cells often evade immune surveillance and elimination via various mechanisms, such as creating an immunosuppressive TME, downregulating HLA-1, and upregulating immune checkpoint proteins [295, 296]. Tumor immune evasion is characterized by the continuous and uncontrolled expansion of the tumor immune microenvironment [293]. Tumor cells manipulate intrinsic regulators to forge an immunosuppressive microenvironment and alter tumor metabolism, thereby impairing immune cell functions and promoting immune evasion [297, 298]. Furthermore, the interaction between PD-1 and PD-L1 facilitates tumor evasion of immunosurveillance by fostering immune tolerance and curtailing the proliferation, survival, and effector functions of CD8+ cytotoxic T lymphocytes (CTLs), as well as triggering apoptosis in tumor-infiltrating T cells [299]. The aforementioned details highlight the role of RNA methylation in enhancing hypoxic and metabolic reprogramming within tumors.
RNA methylation plays a pivotal role in regulating tumor immunosuppressive factors, thereby modulating tumor immune evasion mechanisms. For instance, m6A methylation significantly influences the regulation of PD-1/PD-L1 through mechanisms such as splicing, stability, and translation, ultimately facilitating immune evasion [300, 301]. Specifically, m6A methylation enhances PD-1/PD-L1 expression via the METTL3-JNK signaling pathway [302]. In this pathway, JNK interacts with and binds to METTL3, which increases the m6A modification of mRNA, thereby elevating PD-1 levels and reducing the cytotoxic effectiveness of CD8+ T cells, leading to tumor immune evasion [302]. Moreover, the expression of PD-L1 is linked to both METTL3 and IGF2BP3; the latter recognizes m6A sites and blocks PD-1 degradation to promote immune evasion [25, 303]. Additionally, METTL3 is known to augment the immunosuppressive abilities of tumor-infiltrating myeloid cells [304]. In the context of EC, Serine hydroxymethyltransferase 2 (SHMT2) utilizes the METTL3/FTO/ALKBH5/IGF2BP2 pathway to mediate immune evasion by modifying c-myc through m6A [305]. These findings further indicate that IGF2BP3 plays a crucial role in the regulation of PD-1/PD-L1 degradation and impacts tumor immune responses. Moreover, overexpression of METTL16, by decreasing mRNA stability via m6A modification, cooperatively inhibits tumor immune evasion along with PD-1 suppression [50]. Deficiencies in ALKBH5 or FTO can also suppress PD-L1 expression by hindering YTHDF2-mediated mRNA stability [306, 307]. Additionally, YTHDF1 promotes tumor immune evasion by enhancing PD-L1 expression [308] (Fig. 5). The expression of PD-L1 is upregulated by the m5C reader protein YBX1, which when interacting with PD-1, can significantly inhibit the proliferation and function of cytotoxic CD8+ T cells. This interaction thereby suppresses the immune response in patients [309]. These findings underscore the critical role of RNA methylation in facilitating tumor immune evasion, highlighting the potential of targeting this biochemical process as a promising therapeutic strategy.
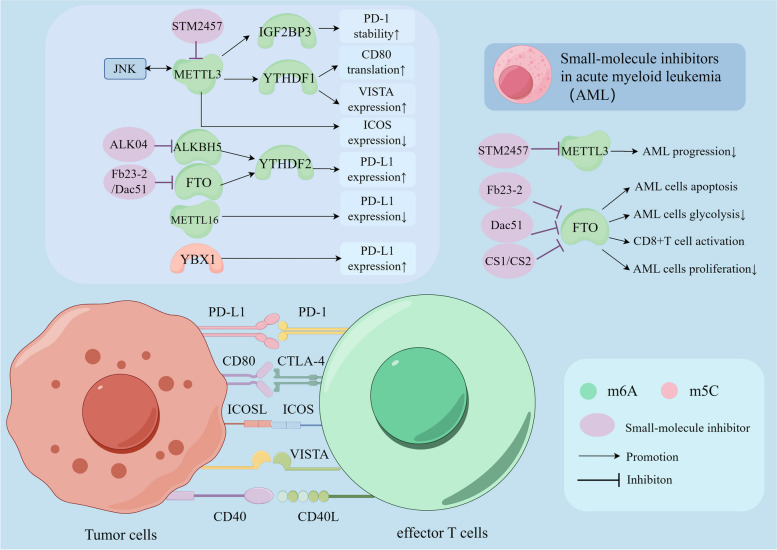
Fig. 5.
RNA methylations regulate expression of immune checkpoints through their regulators, and several small-molecule inhibitors combined with immune checkpoint blockade are applied in acute myeloid leukemia (AML). Co-inhibitory receptor-ligand complexes includes PD-1/PD-L1, CTLA-4/CD80, VISTA and so on. Co-stimulatory receptor-ligand complexes includes CD40/CD40L, ICOS/ICOSL and so on. m6A and m5C regulate the expression, translation, and stability of immune checkpoints as well as their sensibilities to immunotherapy. Immune checkpoints such as PD-1, CTLA-4, ICOS, VISTA, CD40L bind with their respective ligands on tumor cells, triggering a negative or positive signal to T cells response. This process can be impacted by several regulator proteins of RNA methylations, such as METTL3, ALKBH5, FTO and METTL16. Several small-molecular inhibitions targeting METTL3 and FTO, including STM2457, Alk-04, FB23-2, Dac51 and so on, can inhibit m6A methylation process and can be applied in AML. Figure created with figdraw.com
Targeting RNA Methylation Enhances the Therapeutic Effects of Immune Checkpoint Blockade
Immune checkpoint blockade (ICB) has shown significant success in clinical trials and has been approved for the treatment of various cancers. These include GC, HCC, CRC, NSCLC, SCLC, triple-negative breast cancer, urothelial carcinoma, melanoma, etc. [310–322]. Immune checkpoint inhibitors (ICIs) are designed to block the function of immune checkpoints, effectively alleviating the immunosuppressive state of T cells, reversing T cell exhaustion, and reactivating effector T cells within the TME. This action significantly boosts anti-tumor immune responses [323, 324]. Specifically, targeting PD-1 and its ligands, along with CTLA-4 the two principal immune checkpoints—has substantially improved outcomes in cancer treatment [323, 325–327]. Additionally, there is a growing body of evidence supporting the use of PD-L1 small-molecule inhibitors in combination with RNA modification modulators to enhance the effectiveness of ICB in clinical treatments [328, 329] (Table 2). Furthermore, the inhibition of methylases has been shown to significantly enhance the effectiveness of ICB therapy. For instance, inhibiting METTL1 has been demonstrated to improve responses to ICB therapy in preclinical models of PCa, and low expression of METTL1 is associated with favorable outcomes from ICB therapy [128].
Table 2.
Small-molecule inhibitors targeting N6-Methyladenosine regulators and immune checkpoints
| Small-molecule inhibitors | Target | Cancer type | References |
|---|---|---|---|
| STM2457 | METTL3 | CESC; AML | [330, 331] |
| FB23-2 | FTO | AML | [332] |
| Dac51 | FTO | AML | [332] |
| CS1 | FTO | AML | [333] |
| CS2 | FTO | AML | [333] |
| 18097 | FTO | Breast cancer | [334] |
| Alk-04 | ALKBH5 | CRC; Melanoma | [237] |
| Atezolizumab | PD-L1 | SCLC; Triple-negative breast cancer | [311, 316] |
| Avelumab | PD-L1 | Urothelial carcinoma | [320] |
| Durvalumab | PD-L1 | SCLC | [321] |
| Nivolumab | PD-1 | Advanced HCC | [310] |
| Ipilimumab | CTLA-4 | Advanced Melanoma | [319] |
| Pembrolizumab | PD-1 | Metastatic squamous cell carcinoma | [322] |
Abbreviation: AML acute myeloid leukemia, CESC cervical squamous cell carcinoma, CRC colorectal cancer, SCLC small-cell lung cancer
The use of m6A regulator inhibitors in enhancing ICB therapies has been extensively explored in recent studies [335, 336]. m6A methylases play a crucial role in modulating the expression levels of PD-L1 and enhancing tumor sensitivity to anti-PD-1 and anti-CTLA-4 therapies, thereby improving the outcomes of ICB treatments [50, 234, 337]. Additionally, YTHDF1 is implicated in inducing resistance to ICIs by promoting the degradation of MHC-I molecules; inhibiting YTHDF1 can transform immunologically "cold" tumors into "hot" ones, making them more amenable to therapy [60]. YTHDF1 also contributes to the dysfunction of cytotoxic CD8+ T cells by encouraging the accumulation of MDSCs through IL-6 secretion, presenting a novel target for ICB immunotherapy [338]. Furthermore, both methionine metabolites and YTHDF1 are known to enhance the translation of immune checkpoints such as PD-L1 and VISTA, suggesting that targeting these processes could be an innovative strategy for ICB [187]. Depleting METTL3 in myeloid cells has been shown to reduce the efficacy of PD-1 blockade therapies by decreasing the translation efficiency of YTHDF1 [205]. Moreover, IGF2BP1 enhances PD-L1 mRNA stability and promotes tumor immune evasion by reducing CD8+ T cell-mediated cytotoxicity. This mechanism is potentiated by fibroblast growth factor receptor 4 (FGFR4), and targeting IGF2BP1 in conjunction with anti-PD-L1 therapy can inhibit the proliferation and invasion of HCC cells [339, 340].
Moreover, upregulation of m6A regulators has been observed in patients exhibiting resistance to immunotherapy. Notable among these regulators are METTL3, METTL16, ALKBH5, etc., suggesting their potential roles in the development of resistance mechanisms [341–343]. Overall, to enhance the efficacy of ICB in cancer immunotherapy, it is crucial to explore small-molecule inhibitors targeting RNA methylation regulators. This approach necessitates a thorough understanding of the complex interactions between immune checkpoints and RNA methylation mechanisms.
Several small-molecule inhibitors have been developed and are being used in conjunction with ICB (Fig. 5 and Table 2). Notably, STM2457, an inhibitor of METTL3, has been demonstrated to reduce m6A levels and inhibit the progression of AML [287, 330]. STM2457, when used in conjunction with anti-PD-1 antibodies, has been shown to significantly improve treatment outcomes in cervical squamous cell carcinoma (CESC) [331]. This METTL3 inhibitor is particularly noteworthy because it can eliminate AML cells without significantly harming normal hematopoiesis [330]. Additionally, substrate-competitive FTO inhibitors such as FB23-2 and Dac51 have been effective in promoting apoptosis in AML cells and reactivating CD8+T cells by inhibiting tumor glucose metabolism, respectively [332, 333]. Moreover, two other inhibitors, CS1 and CS2, have been documented to drastically reduce the proliferation of human AML cells by suppressing PD-L1 expression through the MYC pathway. Their therapeutic efficacy is reported to be over ten times greater than that of FB23-2 [334]. Another FTO inhibitor, named 18,097, has been successful in inhibiting the proliferation and migration of breast cancer cells and enhancing their chemosensitivity [344]. Furthermore, Alk-04, a specific inhibitor of ALKBH5, boosts the effectiveness of anti-PD-1 therapy and reduces the infiltration of Tregs and MDSCs in TME [237]. Beyond PD-1 and PD-L1, methylation regulators also affect other immune checkpoints such as CD80, ICOS, and VISTA. For instance, METTL3-mediated YTHDF1 recognition of m6A in CD80 transcripts enhances CD80 translation [23], and METTL3 deficiency correlates with reduced expression of the inducible co-stimulatory molecule (ICOS) [148]. YTHDF1 also increases the expression levels of PD-L1 and the PD-1 homolog VISTA [187]. Additionally, it has been reported that targeting modifications like m5C and m1A methylation can further enhance the effectiveness of ICB immunotherapy [345, 346]. These findings illustrate a broad and potent application of small-molecule inhibitors in cancer treatment, particularly when combined with established ICB strategies.
In conclusion, the inhibition of RNA methylation regulators is currently under investigation for its potential to curb tumor progression. Experimental evidence from animal studies has confirmed that combining immune checkpoint blockade with small-molecule inhibitors can effectively suppress tumor growth. The ongoing development and refinement of RNA methylation regulator inhibitors and ICIs are poised to yield significant advancements and offer promising new treatments for cancer patients in the foreseeable future.
Conclusions and perspectives
In this review, we explored four types of RNA methylation and their regulatory roles: writers, erasers, and readers, within the TME. These regulators are involved in crucial biological processes including hypoxia and metabolic reprogramming, and they influence the development, differentiation, proliferation, infiltration, activation, and apoptosis of immune cells in tumor immunity. Furthermore, they mediate the expression of immune checkpoints, thereby facilitating tumor immune evasion. These modifications influence RNA fate through mechanisms such as splicing, transport, translation, stability, and degradation. Given these roles, RNA methylation significantly impacts the initiation, proliferation, invasion, and metastasis of cancer. By regulating the translation of immune checkpoints and mediating tumor immune evasion, these modifications highlight a promising area for targeting the interactions between RNA modification and immune checkpoints in cancer immunotherapy.
RNA methylation has been extensively studied for its varied biological functions, and its regulators have been widely examined in the context of cancer research. Interestingly, some regulators, such as METTL3, have been found to perform opposing functions depending on the disease type or even within different aspects of the same disease. For example, low expression of METTL3 is associated with resistance to anti-PD-1 antibodies in thyroid cancer [266], whereas inhibitors of METTL3 can improve treatment outcomes in AML [330]. These findings underscore the importance of thoroughly understanding the complex biological effects of methylation regulators in different cancers.
Overall, the prospects of RNA methylation in the field of cancer immunotherapy are promising. These regulators can be utilized to estimate the diagnosis and prognosis of cancer by assessing the upregulation or downregulation of expression levels. Furthermore, there is potential to exploit cancer vaccines targeting the regulators' functions in tumor immunity, as RNA methylation plays a crucial role in regulating RNA fate. These regulators also modulate the function of immune cells, the invasion capacity of tumor cells, and the expression of immune checkpoints, thereby influencing tumor progression, resistance, and recurrence. In conclusion, targeting these biological functions and developing more small-molecule inhibitors, especially in combination with ICB immunotherapy, holds great promise for clinical treatment and offers encouraging prospects in the field of cancer immunotherapy.
Acknowledgements
Not applicable.
Abbreviations
- AAA
Abdominal Aortic Aneurysm
- ACC
Adrenocortical carcinoma
- ACER2
Alkaline ceramidase 2
- ALKBH1
α-Ketoglutarate-dependent dioxygenase ABH1
- ALKBH5
AlkB homolog 5
- ALYREF
Aly/REF export factor
- AML
Acute myeloid leukemia
- APC
Antigen presenting cells
- APOE
Apolipoprotein E
- BCAA
Branched-chain amino acid
- BCAT1
Branched-chain amino acid transaminase 1
- BMDMs
Bone marrow-derived macrophages
- CAFs
Cancer-associated fibroblasts
- CBC
Cap-binding complex
- CDKN1A
Cyclin-dependent kinase inhibitor 1A
- CESC
Cervical squamous cell carcinoma
- CRC
Colorectal cancer
- CSF-1
Cytokine macrophage colony-stimulating factor
- CTLs
Cytotoxic T lymphocytes
- DKK1
Dickkopf-related protein 1
- DLBCL
Diffuse large B-cell lymphoma
- DNMT2
DNA methyltransferase 2
- EBV
Epstein–Barr virus
- EC
Esophageal cancer
- eIF3
Eukaryotic translation initiation factor 3
- ELAVL1
Embryonic Lethal Abnormal Vision Like 1
- FTO
Obesity-associated protein
- GBM
Glioblastoma
- GC
Gastric cancer
- GLS
Glutaminase
- Gys2
The liver-specific glycogen synthase
- HBXIP
HBx-interacting protein
- HCC
Hepatocellular carcinoma
- HDGF
Heparin Binding Growth Factor
- HIF
Hypoxia-inducible factors
- hm5C
5-Hydroxymethylcytidine
- ICC
Intrahepatic cholangiocarcinoma
- ICIs
Immune checkpoint inhibitors
- ICOS
Inducible co-stimulatory
- IFN
Interferon
- IGF2BP1
Insulin-like growth factor 2 mRNA-binding protein 1
- IL-12
Interleukin-12
- LSCs
Leukemia stem cells
- m1A
N1-methyladenosine
- m3C
3-Methylcytidine
- m5C
5-Methylcytosine
- m6A
N6-methyladenosine
- m7G
N7-methylguanosine
- MAPK
Mitogen activated protein kinase
- MDSCs
Myeloid-derived suppressor cells
- METTL3
Methyltransferase-like 3
- MM
Multiple myeloma
- M-MDSCs
Monocyte-related myeloid-derived suppressor cells
- MPNSTs
Malignant peripheral nerve sheath tumors
- MTC
Methyltransferase complex
- NAFLD
Nonalcoholic fatty liver disease
- NML
Nucleomethylin
- NSCLC
Non-small cell lung cancer
- OXPHOS
Oxidative phosphorylation
- PABP
Poly(A) binding protein
- PCa
Prostate cancer
- PDAC
Pancreatic ductal adenocarcinoma
- PRMT1
Protein arginine N-methyltransferases 1
- R255
Arginine 255
- RAM
RNMT-activating miniprotein
- RCC
Renal cell carcinoma
- RCC2
Regulator of chromosome condensation 2
- RNMT
RNA guanine-7 methyltransferase
- SCD1
Stearoyl-CoA desaturase1
- SCLC
Small-cell lung cancer
- SHMT2
Serine hydroxymethyltransferase 2
- SLE
Systemic lupus erythematosus
- TAMs
Tumor-associated macrophages
- TET1/2/3
Ten-eleven translocation proteins1/2/3
- TIME
Tumor immune microenvironment
- TME
Tumor microenvironment
- TREX2
Three prime repair exonuclease 2
- TRM61
TRNA methyltransferase catalytic subunit 61
- TRMT10A
TRNA methyltransferase 10 homologue A
- TRMT112
TRNA methyltransferase activator subunit 11–2
- WBSCR22
Williams–Beuren syndrome chromosome region 22
- WDR4
WD repeat domain 4
- YBX1
Y-box-binding protein 1
- YTHDF1
YTH N6-methyladenosine RNA binding protein 1
Authors’ contributions
LZ provided direction and guidance throughout the preparation of this manuscript. YL, HJ, QL and LS finished the manuscript and YL designed the figures. YM and LZ reviewed and made significant revisions to the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the Natural Science Foundation of Hunan Province (2022JJ30794), Changsha Municipal Natural Science Foundation (kq2202126), Research Project on Teaching Reform in Ordinary Higher Education Institutions in Hunan Province (HNJG-20230120), Graduate Education and Teaching Reform Project of Central South University (2022YJSKS018, 2023JGB118, 2023jy153, 2024ALK005).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have approved to publish this manuscript.
Competing interests
All authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yitao Mao, Email: maoyt@csu.edu.cn.
Luqing Zhao, Email: luqingzhao@csu.edu.cn.
References
- 1.Cui L, Ma R, Cai J, Guo C, Chen Z, Yao L, et al. RNA modifications: importance in immune cell biology and related diseases. Sig Transduct Target Ther. 2022;7:334. doi: 10.1038/s41392-022-01175-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbieri I, Kouzarides T. Role of RNA modifications in cancer. Nat Rev Cancer. 2020;20:303–322. doi: 10.1038/s41568-020-0253-2. [DOI] [PubMed] [Google Scholar]
- 3.Li X, Ma S, Deng Y, Yi P, Yu J. Targeting the RNA m6A modification for cancer immunotherapy. Mol Cancer. 2022;21:76. doi: 10.1186/s12943-022-01558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xue C, Chu Q, Zheng Q, Jiang S, Bao Z, Su Y, et al. Role of main RNA modifications in cancer: N6-methyladenosine, 5-methylcytosine, and pseudouridine. Sig Transduct Target Ther. 2022;7:142. doi: 10.1038/s41392-022-01003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han D, Xu MM. RNA Modification in the Immune System. Annu Rev Immunol. 2023;41:73–98. doi: 10.1146/annurev-immunol-101921-045401. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y, Jiang Z, Yang Y, Zhang C, Liu H, Wan J. The functions and mechanisms of post-translational modification in protein regulators of RNA methylation: Current status and future perspectives. Int J Biol Macromol. 2023;253:126773. doi: 10.1016/j.ijbiomac.2023.126773. [DOI] [PubMed] [Google Scholar]
- 7.Shi H, Wei J, He C. Where, When, and How: Context-Dependent Functions of RNA Methylation Writers, Readers, and Erasers. Mol Cell. 2019;74:640–650. doi: 10.1016/j.molcel.2019.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deng X, Qing Y, Horne D, Huang H, Chen J. The roles and implications of RNA m6A modification in cancer. Nat Rev Clin Oncol. 2023;20:507–526. doi: 10.1038/s41571-023-00774-x. [DOI] [PubMed] [Google Scholar]
- 9.Hu Y, Chen C, Tong X, Chen S, Hu X, Pan B, et al. NSUN2 modified by SUMO-2/3 promotes gastric cancer progression and regulates mRNA m5C methylation. Cell Death Dis. 2021;12:842. doi: 10.1038/s41419-021-04127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su J, Wu G, Ye Y, Zhang J, Zeng L, Huang X, et al. NSUN2-mediated RNA 5-methylcytosine promotes esophageal squamous cell carcinoma progression via LIN28B-dependent GRB2 mRNA stabilization. Oncogene. 2021;40:5814–5828. doi: 10.1038/s41388-021-01978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu Z, Liu B, Kong D, Zhou X, Pei D, Liu D. NSUN6 regulates NM23-H1 expression in a m5C manner to affect epithelial-mesenchymal transition in lung cancer. Med Princ Pract. 2024;33:56-65. [DOI] [PMC free article] [PubMed]
- 12.Ortiz-Barahona V, Soler M, Davalos V, García-Prieto CA, Janin M, Setien F, et al. Epigenetic inactivation of the 5-methylcytosine RNA methyltransferase NSUN7 is associated with clinical outcome and therapeutic vulnerability in liver cancer. Mol Cancer. 2023;22:83. doi: 10.1186/s12943-023-01785-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Y, Wang J, Li X, Xiong X, Wang J, Zhou Z, et al. N1-methyladenosine methylation in tRNA drives liver tumourigenesis by regulating cholesterol metabolism. Nat Commun. 2021;12:6314. doi: 10.1038/s41467-021-26718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao Y, Zhao Q, Kaboli PJ, Shen J, Li M, Wu X, et al. m1A Regulated Genes Modulate PI3K/AKT/mTOR and ErbB Pathways in Gastrointestinal Cancer. Transl Oncol. 2019;12:1323–1333. doi: 10.1016/j.tranon.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng Q, Yu X, Zhang Q, He Y, Guo W. Genetic characteristics and prognostic implications of m1A regulators in pancreatic cancer. Bioscience Reports. 2021;41:BSR20210337. doi: 10.1042/BSR20210337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan AA, Huang H, Zhao Y, Li H, Pan R, Wang S, et al. WBSCR22 and TRMT112 synergistically suppress cell proliferation, invasion and tumorigenesis in pancreatic cancer via transcriptional regulation of ISG15. Int J Oncol. 2022;60:24. doi: 10.3892/ijo.2022.5314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lan Q, Liu PY, Haase J, Bell JL, Hüttelmaier S, Liu T. The Critical Role of RNA m6A Methylation in Cancer. Cancer Res. 2019;79:1285–1292. doi: 10.1158/0008-5472.CAN-18-2965. [DOI] [PubMed] [Google Scholar]
- 18.Zhou W, Wang X, Chang J, Cheng C, Miao C. The molecular structure and biological functions of RNA methylation, with special emphasis on the roles of RNA methylation in autoimmune diseases. Crit Rev Clin Lab Sci. 2022;59:203–218. doi: 10.1080/10408363.2021.2002256. [DOI] [PubMed] [Google Scholar]
- 19.Orsolic I, Carrier A, Esteller M. Genetic and epigenetic defects of the RNA modification machinery in cancer. Trends Genet. 2023;39:74–88. doi: 10.1016/j.tig.2022.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Bejarano L, Jordāo MJC, Joyce JA. Therapeutic Targeting of the Tumor Microenvironment. Cancer Discov. 2021;11:933–959. doi: 10.1158/2159-8290.CD-20-1808. [DOI] [PubMed] [Google Scholar]
- 21.Yang N, Wang T, Li Q, Han F, Wang Z, Zhu R, et al. HBXIP drives metabolic reprogramming in hepatocellular carcinoma cells via METTL3-mediated m6A modification of HIF-1α. J Cell Physiol. 2021;236:3863–3880. doi: 10.1002/jcp.30128. [DOI] [PubMed] [Google Scholar]
- 22.Song B, Zeng Y, Cao Y, Zhang J, Xu C, Pan Y, et al. Emerging role of METTL3 in inflammatory diseases: mechanisms and therapeutic applications. Front Immunol. 2023;14:1221609. doi: 10.3389/fimmu.2023.1221609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang H, Hu X, Huang M, Liu J, Gu Y, Ma L, et al. Mettl3-mediated mRNA m6A methylation promotes dendritic cell activation. Nat Commun. 2019;10:1898. doi: 10.1038/s41467-019-09903-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li S, Zou D, Chen W, Britz GW, Liu Z, Weng Y-L. METTL3 inhibition reduces N6-methyladenosine levels and prevents allogeneic CD4+ T-cell responses. Immunol Cell Biol. 2022;100:718–730. doi: 10.1111/imcb.12581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wan W, Ao X, Chen Q, Yu Y, Ao L, Xing W, et al. METTL3/IGF2BP3 axis inhibits tumor immune surveillance by upregulating N6-methyladenosine modification of PD-L1 mRNA in breast cancer. Mol Cancer. 2022;21:60. doi: 10.1186/s12943-021-01447-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sun Y, Shen W, Hu S, Lyu Q, Wang Q, Wei T, et al. METTL3 promotes chemoresistance in small cell lung cancer by inducing mitophagy. J Exp Clin Cancer Res. 2023;42:65. doi: 10.1186/s13046-023-02638-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Zhang Z. The history and advances in cancer immunotherapy: understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell Mol Immunol. 2020;17:807–821. doi: 10.1038/s41423-020-0488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang F, Liu H, Duan M, Wang G, Zhang Z, Wang Y, et al. Crosstalk among m6A RNA methylation, hypoxia and metabolic reprogramming in TME: from immunosuppressive microenvironment to clinical application. J Hematol Oncol. 2022;15:84. doi: 10.1186/s13045-022-01304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang T, Kong S, Tao M, Ju S. The potential role of RNA N6-methyladenosine in Cancer progression. Mol Cancer. 2020;19:88. doi: 10.1186/s12943-020-01204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han X, Wang M, Zhao Y-L, Yang Y, Yang Y-G. RNA methylations in human cancers. Semin Cancer Biol. 2021;75:97–115. doi: 10.1016/j.semcancer.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Zhang Y, Zhang W, Zhao J, Ito T, Jin J, Aparicio AO, et al. m6A RNA modification regulates innate lymphoid cell responses in a lineage-specific manner. Nat Immunol. 2023;24:1256–1264. doi: 10.1038/s41590-023-01548-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang H, Weng H, Chen J. m6A Modification in Coding and Non-coding RNAs: Roles and Therapeutic Implications in Cancer. Cancer Cell. 2020;37:270–288. doi: 10.1016/j.ccell.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Y, Lin Y, Shu Y, He J, Gao W. Interaction between N6-methyladenosine (m6A) modification and noncoding RNAs in cancer. Mol Cancer. 2020;19:94. doi: 10.1186/s12943-020-01207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song P, Tayier S, Cai Z, Jia G. RNA methylation in mammalian development and cancer. Cell Biol Toxicol. 2021;37:811–831. doi: 10.1007/s10565-021-09627-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oerum S, Meynier V, Catala M, Tisné C. A comprehensive review of m6A/m6Am RNA methyltransferase structures. Nucleic Acids Res. 2021;49:7239–7255. doi: 10.1093/nar/gkab378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou H, Yin K, Zhang Y, Tian J, Wang S. The RNA m6A writer METTL14 in cancers: Roles, structures, and applications. Biochim Biophys Acta Rev Cancer. 2021;1876:188609. doi: 10.1016/j.bbcan.2021.188609. [DOI] [PubMed] [Google Scholar]
- 37.van Tran N, Ernst FGM, Hawley BR, Zorbas C, Ulryck N, Hackert P, et al. The human 18S rRNA m6A methyltransferase METTL5 is stabilized by TRMT112. Nucleic Acids Res. 2019;47:7719–7733. doi: 10.1093/nar/gkz619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fang Z, Mei W, Qu C, Lu J, Shang L, Cao F, et al. Role of m6A writers, erasers and readers in cancer. Exp Hematol Oncol. 2022;11:45. doi: 10.1186/s40164-022-00298-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiang X, Liu B, Nie Z, Duan L, Xiong Q, Jin Z, et al. The role of m6A modification in the biological functions and diseases. Signal Transduct Target Ther. 2021;6:74. doi: 10.1038/s41392-020-00450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang N, Shen Y, Li H, Chen Y, Zhang P, Lou S, et al. The m6A reader IGF2BP3 promotes acute myeloid leukemia progression by enhancing RCC2 stability. Exp Mol Med. 2022;54:194–205. doi: 10.1038/s12276-022-00735-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu T, Wei Q, Jin J, Luo Q, Liu Y, Yang Y, et al. The m6A reader YTHDF1 promotes ovarian cancer progression via augmenting EIF3C translation. Nucleic Acids Res. 2020;48:3816–3831. doi: 10.1093/nar/gkaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.X H, J G, Z F. Interactions between m6A modification and miRNAs in malignant tumors. Cell death & disease. 2021 [cited 2023 Aug 12];12. Available from: https://pubmed.ncbi.nlm.nih.gov/34108450/ [DOI] [PMC free article] [PubMed]
- 43.Wang L, Zhang S, Li H, Xu Y, Wu Q, Shen J, et al. Quantification of m6A RNA methylation modulators pattern was a potential biomarker for prognosis and associated with tumor immune microenvironment of pancreatic adenocarcinoma. BMC Cancer. 2021;21:876. doi: 10.1186/s12885-021-08550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li M, Ye J, Xia Y, Li M, Li G, Hu X, et al. METTL3 mediates chemoresistance by enhancing AML homing and engraftment via ITGA4. Leukemia. 2022;36:2586–2595. doi: 10.1038/s41375-022-01696-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cheng JX, Chen L, Li Y, Cloe A, Yue M, Wei J, et al. RNA cytosine methylation and methyltransferases mediate chromatin organization and 5-azacytidine response and resistance in leukaemia. Nat Commun. 2018;9:1163. doi: 10.1038/s41467-018-03513-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen H, Gao S, Liu W, Wong C-C, Wu J, Wu J, et al. RNA N6-Methyladenosine Methyltransferase METTL3 Facilitates Colorectal Cancer by Activating the m6A-GLUT1-mTORC1 Axis and Is a Therapeutic Target. Gastroenterology. 2021;160:1284–1300.e16. doi: 10.1053/j.gastro.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 47.Zhan L, Zhang J, Zhang J-H, Liu X-J, Guo B, Chen J-H, et al. METTL3 facilitates immunosurveillance by inhibiting YTHDF2-mediated NLRC5 mRNA degradation in endometrial cancer. Biomark Res. 2023;11:43. doi: 10.1186/s40364-023-00479-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Q, Chen C, Ding Q, Zhao Y, Wang Z, Chen J, et al. METTL3-mediated m 6 A modification of HDGF mRNA promotes gastric cancer progression and has prognostic significance. Gut. 2020;69:1193–1205. doi: 10.1136/gutjnl-2019-319639. [DOI] [PubMed] [Google Scholar]
- 49.Du L, Li Y, Kang M, Feng M, Ren Y, Dai H, et al. USP48 Is Upregulated by Mettl14 to Attenuate Hepatocellular Carcinoma via Regulating SIRT6 Stabilization. Cancer Res. 2021;81:3822–3834. doi: 10.1158/0008-5472.CAN-20-4163. [DOI] [PubMed] [Google Scholar]
- 50.Wang A, Sun Y, Wang X, Yan Z, Wang D, Zeng L, et al. m6A methyltransferase METTL16 mediates immune evasion of colorectal cancer cells via epigenetically regulating PD-L1 expression. Aging (Albany NY) 2023;15:8444–8457. doi: 10.18632/aging.204980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Y, Peng C, Chen J, Chen D, Yang B, He B, et al. WTAP facilitates progression of hepatocellular carcinoma via m6A-HuR-dependent epigenetic silencing of ETS1. Mol Cancer. 2019;18:127. doi: 10.1186/s12943-019-1053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhu D, Zhou J, Zhao J, Jiang G, Zhang X, Zhang Y, et al. ZC3H13 suppresses colorectal cancer proliferation and invasion via inactivating Ras-ERK signaling. J Cell Physiol. 2019;234:8899–8907. doi: 10.1002/jcp.27551. [DOI] [PubMed] [Google Scholar]
- 53.Wang Q, Xie H, Peng H, Yan J, Han L, Ye G. ZC3H13 Inhibits the Progression of Hepatocellular Carcinoma through m6A-PKM2-Mediated Glycolysis and Enhances Chemosensitivity. Wang F, editor. J Oncol. 2021;2021:1–15. doi: 10.1155/2021/1328444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu Y, Chen Y, Yao Y, Xie H, Lu G, Du C, et al. VIRMA contributes to non-small cell lung cancer progression via N6-methyladenosine-dependent DAPK3 post-transcriptional modification. Cancer Lett. 2021;522:142–154. doi: 10.1016/j.canlet.2021.08.027. [DOI] [PubMed] [Google Scholar]
- 55.Chen X, Lu T, Cai Y, Han Y, Ding M, Chu Y, et al. KIAA1429-mediated m6A modification of CHST11 promotes progression of diffuse large B-cell lymphoma by regulating Hippo-YAP pathway. Cell Mol Biol Lett. 2023;28:32. doi: 10.1186/s11658-023-00445-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ruan D-Y, Li T, Wang Y-N, Meng Q, Li Y, Yu K, et al. FTO downregulation mediated by hypoxia facilitates colorectal cancer metastasis. Oncogene. 2021;40:5168–5181. doi: 10.1038/s41388-021-01916-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang S, Wei J, Cui Y-H, Park G, Shah P, Deng Y, et al. m6A mRNA demethylase FTO regulates melanoma tumorigenicity and response to anti-PD-1 blockade. Nat Commun. 2019;10:2782. doi: 10.1038/s41467-019-10669-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhai J, Chen H, Wong CC, Peng Y, Gou H, Zhang J, et al. ALKBH5 Drives Immune Suppression Via Targeting AXIN2 to Promote Colorectal Cancer and Is a Target for Boosting Immunotherapy. Gastroenterology. 2023;165:445–462. doi: 10.1053/j.gastro.2023.04.032. [DOI] [PubMed] [Google Scholar]
- 59.You Y, Wen D, Zeng L, Lu J, Xiao X, Chen Y, et al. ALKBH5/MAP3K8 axis regulates PD-L1+ macrophage infiltration and promotes hepatocellular carcinoma progression. Int J Biol Sci. 2022;18:5001–5018. doi: 10.7150/ijbs.70149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lin W, Chen L, Zhang H, Qiu X, Huang Q, Wan F, et al. Tumor-intrinsic YTHDF1 drives immune evasion and resistance to immune checkpoint inhibitors via promoting MHC-I degradation. Nat Commun. 2023;14:265. doi: 10.1038/s41467-022-35710-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ma L, Jiang J, Si Q, Chen C, Duan Z. IGF2BP3 Enhances the Growth of Hepatocellular Carcinoma Tumors by Regulating the Properties of Macrophages and CD8+ T Cells in the Tumor Microenvironment. J Clin Transl Hepatol. 2023;11:1308–1320. doi: 10.14218/JCTH.2023.00184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi Y, Fan S, Wu M, Zuo Z, Li X, Jiang L, et al. YTHDF1 links hypoxia adaptation and non-small cell lung cancer progression. Nat Commun. 2019;10:4892. doi: 10.1038/s41467-019-12801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Palomo-Irigoyen M, Pérez-Andrés E, Iruarrizaga-Lejarreta M, Barreira-Manrique A, Tamayo-Caro M, Vila-Vecilla L, et al. HuR/ELAVL1 drives malignant peripheral nerve sheath tumor growth and metastasis. J Clin Invest. 2020;130:3848–3864. doi: 10.1172/JCI130379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chen W, Wang H, Mi S, Shao L, Xu Z, Xue M. ALKBH1-mediated m1 A demethylation of METTL3 mRNA promotes the metastasis of colorectal cancer by downregulating SMAD7 expression. Mol Oncol. 2023;17:344–364. doi: 10.1002/1878-0261.13366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Feng M, Xie X, Han G, Zhang T, Li Y, Li Y, et al. YBX1 is required for maintaining myeloid leukemia cell survival by regulating BCL2 stability in an m6A-dependent manner. Blood. 2021;138:71–85. doi: 10.1182/blood.2020009676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Woo H-H, Chambers SK. Human ALKBH3-induced m1A demethylation increases the CSF-1 mRNA stability in breast and ovarian cancer cells. Biochim Biophys Acta Gene Regul Mech. 2019;1862:35–46. doi: 10.1016/j.bbagrm.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 67.Wu Y, Chen Z, Xie G, Zhang H, Wang Z, Zhou J, et al. RNA m1A methylation regulates glycolysis of cancer cells through modulating ATP5D. Proc Natl Acad Sci U S A. 2022;119:e2119038119. doi: 10.1073/pnas.2119038119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hou Y, Zhang Q, Pang W, Hou L, Liang Y, Han X, et al. YTHDC1-mediated augmentation of miR-30d in repressing pancreatic tumorigenesis via attenuation of RUNX1-induced transcriptional activation of Warburg effect. Cell Death Differ. 2021;28:3105–3124. doi: 10.1038/s41418-021-00804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xu F, Cai D, Liu S, He K, Chen J, Qu L, et al. N7-methylguanosine regulatory genes well represented by METTL1 define vastly different prognostic, immune and therapy landscapes in adrenocortical carcinoma. Am J Cancer Res. 2023;13:538–568. [PMC free article] [PubMed] [Google Scholar]
- 70.Ruiz-Arroyo VM, Raj R, Babu K, Onolbaatar O, Roberts PH, Nam Y. Structures and mechanisms of tRNA methylation by METTL1-WDR4. Nature. 2023;613:383–390. doi: 10.1038/s41586-022-05565-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen Z, Zhu W, Zhu S, Sun K, Liao J, Liu H, et al. METTL1 promotes hepatocarcinogenesis via m7 G tRNA modification-dependent translation control. Clin Transl Med. 2021;11:e661. doi: 10.1002/ctm2.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ying X, Liu B, Yuan Z, Huang Y, Chen C, Jiang X, et al. METTL1-m7 G-EGFR/EFEMP1 axis promotes the bladder cancer development. Clin Transl Med. 2021;11:e675. doi: 10.1002/ctm2.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Osborne MJ, Volpon L, Memarpoor-Yazdi M, Pillay S, Thambipillai A, Czarnota S, et al. Identification and Characterization of the Interaction Between the Methyl-7-Guanosine Cap Maturation Enzyme RNMT and the Cap-Binding Protein eIF4E. J Mol Biol. 2022;434:167451. doi: 10.1016/j.jmb.2022.167451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dunn S, Lombardi O, Lukoszek R, Cowling VH. Oncogenic PIK3CA mutations increase dependency on the mRNA cap methyltransferase, RNMT, in breast cancer cells. Open Biol. 2019;9:190052. doi: 10.1098/rsob.190052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang F, Yoon K, Zhang DY, Kim N-S, Ming G-L, Song H. Epitranscriptomic regulation of cortical neurogenesis via Mettl8-dependent mitochondrial tRNA m3C modification. Cell Stem Cell. 2023;30:300–311.e11. doi: 10.1016/j.stem.2023.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen X, Li A, Sun B-F, Yang Y, Han Y-N, Yuan X, et al. 5-methylcytosine promotes pathogenesis of bladder cancer through stabilizing mRNAs. Nat Cell Biol. 2019;21:978–990. doi: 10.1038/s41556-019-0361-y. [DOI] [PubMed] [Google Scholar]
- 77.García-Vílchez R, Sevilla A, Blanco S. Post-transcriptional regulation by cytosine-5 methylation of RNA. Biochim Biophys Acta Gene Regul Mech. 2019;1862:240–252. doi: 10.1016/j.bbagrm.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 78.Nombela P, Miguel-López B, Blanco S. The role of m6A, m5C and Ψ RNA modifications in cancer: Novel therapeutic opportunities. Mol Cancer. 2021;20:18. doi: 10.1186/s12943-020-01263-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Boo SH, Kim YK. The emerging role of RNA modifications in the regulation of mRNA stability. Exp Mol Med. 2020;52:400–408. doi: 10.1038/s12276-020-0407-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Trixl L, Lusser A. The dynamic RNA modification 5-methylcytosine and its emerging role as an epitranscriptomic mark. WIREs RNA. 2019;10:e1510. doi: 10.1002/wrna.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu Y, Zhao Y, Wu R, Chen Y, Chen W, Liu Y, et al. mRNA m5C controls adipogenesis by promoting CDKN1A mRNA export and translation. RNA Biol. 2021;18:711–721. doi: 10.1080/15476286.2021.1980694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Blanco S, Dietmann S, Flores JV, Hussain S, Kutter C, Humphreys P, et al. Aberrant methylation of tRNAs links cellular stress to neuro-developmental disorders. EMBO J. 2014;33:2020–2039. doi: 10.15252/embj.201489282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Blanco S, Bandiera R, Popis M, Hussain S, Lombard P, Aleksic J, et al. Stem cell function and stress response are controlled by protein synthesis. Nature. 2016;534:335–340. doi: 10.1038/nature18282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Q Z, F L, W C, H M, H L, Z L, et al. The role of RNA m5C modification in cancer metastasis. International journal of biological sciences. 2021 [cited 2023 Sep 2];17. Available from: https://pubmed.ncbi.nlm.nih.gov/34512153/ [DOI] [PMC free article] [PubMed]
- 85.Li M, Tao Z, Zhao Y, Li L, Zheng J, Li Z, et al. 5-methylcytosine RNA methyltransferases and their potential roles in cancer. J Transl Med. 2022;20:214. doi: 10.1186/s12967-022-03427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chellamuthu A, Gray SG. The RNA Methyltransferase NSUN2 and Its Potential Roles in Cancer. Cells. 2020;9:1758. doi: 10.3390/cells9081758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Selmi T, Hussain S, Dietmann S, Heiß M, Borland K, Flad S, et al. Sequence- and structure-specific cytosine-5 mRNA methylation by NSUN6. Nucleic Acids Res. 2021;49:1006–1022. doi: 10.1093/nar/gkaa1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huang T, Chen W, Liu J, Gu N, Zhang R. Genome-wide identification of mRNA 5-methylcytosine in mammals. Nat Struct Mol Biol. 2019;26:380–388. doi: 10.1038/s41594-019-0218-x. [DOI] [PubMed] [Google Scholar]
- 89.Hussain S, Sajini AA, Blanco S, Dietmann S, Lombard P, Sugimoto Y, et al. NSun2-mediated cytosine-5 methylation of vault noncoding RNA determines its processing into regulatory small RNAs. Cell Rep. 2013;4:255–261. doi: 10.1016/j.celrep.2013.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Liao H, Gaur A, McConie H, Shekar A, Wang K, Chang JT, et al. Human NOP2/NSUN1 regulates ribosome biogenesis through non-catalytic complex formation with box C/D snoRNPs. Nucleic Acids Res. 2022;50:10695–10716. doi: 10.1093/nar/gkac817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Janin M, Ortiz-Barahona V, de Moura MC, Martínez-Cardús A, Llinàs-Arias P, Soler M, et al. Epigenetic loss of RNA-methyltransferase NSUN5 in glioma targets ribosomes to drive a stress adaptive translational program. Acta Neuropathol. 2019;138:1053–1074. doi: 10.1007/s00401-019-02062-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yang R, Liang X, Wang H, Guo M, Shen H, Shi Y, et al. The RNA methyltransferase NSUN6 suppresses pancreatic cancer development by regulating cell proliferation. EBioMedicine. 2021;63:103195. doi: 10.1016/j.ebiom.2020.103195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shen H, Ontiveros RJ, Owens MC, Liu MY, Ghanty U, Kohli RM, et al. TET-mediated 5-methylcytosine oxidation in tRNA promotes translation. J Biol Chem. 2021;296:100087. doi: 10.1074/jbc.RA120.014226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yang H, Wang Y, Xiang Y, Yadav T, Ouyang J, Phoon L, et al. FMRP promotes transcription-coupled homologous recombination via facilitating TET1-mediated m5C RNA modification demethylation. Proc Natl Acad Sci U S A. 2022;119:e2116251119. doi: 10.1073/pnas.2116251119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Xu B, Wang H, Tan L. Dysregulated TET Family Genes and Aberrant 5mC Oxidation in Breast Cancer: Causes and Consequences. Cancers (Basel) 2021;13:6039. doi: 10.3390/cancers13236039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xue C, Gu X, Zheng Q, Shi Q, Yuan X, Su Y, et al. ALYREF mediates RNA m5C modification to promote hepatocellular carcinoma progression. Signal Transduct Target Ther. 2023;8:130. doi: 10.1038/s41392-023-01395-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang J-Z, Zhu W, Han J, Yang X, Zhou R, Lu H-C, et al. The role of the HIF-1α/ALYREF/PKM2 axis in glycolysis and tumorigenesis of bladder cancer. Cancer Commun (Lond) 2021;41:560–575. doi: 10.1002/cac2.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jayavelu AK, Schnöder TM, Perner F, Herzog C, Meiler A, Krishnamoorthy G, et al. Splicing factor YBX1 mediates persistence of JAK2-mutated neoplasms. Nature. 2020;588:157–163. doi: 10.1038/s41586-020-2968-3. [DOI] [PubMed] [Google Scholar]
- 99.Dai X, Gonzalez G, Li L, Li J, You C, Miao W, et al. YTHDF2 Binds to 5-Methylcytosine in RNA and Modulates the Maturation of Ribosomal RNA. Anal Chem. 2020;92:1346–1354. doi: 10.1021/acs.analchem.9b04505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Razpotnik R, Vidmar R, Fonović M, Rozman D, Režen T. Circular RNA hsa_circ_0062682 Binds to YBX1 and Promotes Oncogenesis in Hepatocellular Carcinoma. Cancers (Basel) 2022;14:4524. doi: 10.3390/cancers14184524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Xu J, Ji L, Liang Y, Wan Z, Zheng W, Song X, et al. CircRNA-SORE mediates sorafenib resistance in hepatocellular carcinoma by stabilizing YBX1. Signal Transduct Target Ther. 2020;5:298. doi: 10.1038/s41392-020-00375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhou H, Rauch S, Dai Q, Cui X, Zhang Z, Nachtergaele S, et al. Evolution of a reverse transcriptase to map N1-methyladenosine in human messenger RNA. Nat Methods. 2019;16:1281–1288. doi: 10.1038/s41592-019-0550-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shi L, Chen W, Zhang Z, Chen J, Xue M. N1-methyladenosine profiling of long non-coding RNA in colorectal cancer. IUBMB Life. 2021;73:1235–1243. doi: 10.1002/iub.2534. [DOI] [PubMed] [Google Scholar]
- 104.Li J, Zhang H, Wang H. N1-methyladenosine modification in cancer biology: Current status and future perspectives. Comput Struct Biotechnol J. 2022;20:6578–6585. doi: 10.1016/j.csbj.2022.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wiener D, Schwartz S. The epitranscriptome beyond m6A. Nat Rev Genet. 2021;22:119–131. doi: 10.1038/s41576-020-00295-8. [DOI] [PubMed] [Google Scholar]
- 106.Dégut C, Ponchon L, Folly-Klan M, Barraud P, Tisné C. The m1A(58) modification in eubacterial tRNA: An overview of tRNA recognition and mechanism of catalysis by TrmI. Biophys Chem. 2016;210:27–34. doi: 10.1016/j.bpc.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 107.Safra M, Sas-Chen A, Nir R, Winkler R, Nachshon A, Bar-Yaacov D, et al. The m1A landscape on cytosolic and mitochondrial mRNA at single-base resolution. Nature. 2017;551:251–255. doi: 10.1038/nature24456. [DOI] [PubMed] [Google Scholar]
- 108.Howell NW, Jora M, Jepson BF, Limbach PA, Jackman JE. Distinct substrate specificities of the human tRNA methyltransferases TRMT10A and TRMT10B. RNA. 2019;25:1366–1376. doi: 10.1261/rna.072090.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhou H, Kimsey IJ, Nikolova EN, Sathyamoorthy B, Grazioli G, McSally J, et al. m(1)A and m(1)G disrupt A-RNA structure through the intrinsic instability of Hoogsteen base pairs. Nat Struct Mol Biol. 2016;23:803–810. doi: 10.1038/nsmb.3270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chen Z, Qi M, Shen B, Luo G, Wu Y, Li J, et al. Transfer RNA demethylase ALKBH3 promotes cancer progression via induction of tRNA-derived small RNAs. Nucleic Acids Res. 2019;47:2533–2545. doi: 10.1093/nar/gky1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Xu B, Liu D, Wang Z, Tian R, Zuo Y. Multi-substrate selectivity based on key loops and non-homologous domains: new insight into ALKBH family. Cell Mol Life Sci. 2021;78:129–141. doi: 10.1007/s00018-020-03594-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wei J, Liu F, Lu Z, Fei Q, Ai Y, He PC, et al. Differential m6A, m6Am, and m1A Demethylation Mediated by FTO in the Cell Nucleus and Cytoplasm. Mol Cell. 2018;71:973–985.e5. doi: 10.1016/j.molcel.2018.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dai X, Wang T, Gonzalez G, Wang Y. Identification of YTH Domain-Containing Proteins as the Readers for N1-Methyladenosine in RNA. Anal Chem. 2018;90:6380–6384. doi: 10.1021/acs.analchem.8b01703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen Y, Lin H, Miao L, He J. Role of N7-methylguanosine (m7G) in cancer. Trends Cell Biol. 2022;32:819–824. doi: 10.1016/j.tcb.2022.07.001. [DOI] [PubMed] [Google Scholar]
- 115.Tomikawa C. 7-Methylguanosine Modifications in Transfer RNA (tRNA) Int J Mol Sci. 2018;19:4080. doi: 10.3390/ijms19124080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Enroth C, Poulsen LD, Iversen S, Kirpekar F, Albrechtsen A, Vinther J. Detection of internal N7-methylguanosine (m7G) RNA modifications by mutational profiling sequencing. Nucleic Acids Res. 2019;47:e126. doi: 10.1093/nar/gkz736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kouzarides T, Pandolfini L, Barbieri I, Bannister AJ, Andrews B. Further Evidence Supporting N7-Methylation of Guanosine (m7G) in Human MicroRNAs. Mol Cell. 2020;79:201–202. doi: 10.1016/j.molcel.2020.05.023. [DOI] [PubMed] [Google Scholar]
- 118.Pandolfini L, Barbieri I, Bannister AJ, Hendrick A, Andrews B, Webster N, et al. METTL1 Promotes let-7 MicroRNA Processing via m7G Methylation. Mol Cell. 2019;74:1278–1290.e9. doi: 10.1016/j.molcel.2019.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Luo Y, Yao Y, Wu P, Zi X, Sun N, He J. The potential role of N7-methylguanosine (m7G) in cancer. J Hematol Oncol. 2022;15:63. doi: 10.1186/s13045-022-01285-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Varshney D, Lombardi O, Schweikert G, Dunn S, Suska O, Cowling VH. mRNA Cap Methyltransferase, RNMT-RAM, Promotes RNA Pol II-Dependent Transcription. Cell Rep. 2018;23:1530–1542. doi: 10.1016/j.celrep.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhao H, Su W, Sun Y, Wu Z. WBSCR22 Competes with Long Non-coding RNA Linc00346 for miR-509-5p Binding Site to Regulate Cancer Stem Cell Phenotypes of Colorectal Cancer. Biochem Genet. 2020;58:384–398. doi: 10.1007/s10528-020-09949-y. [DOI] [PubMed] [Google Scholar]
- 122.Mars J-C, Ghram M, Culjkovic-Kraljacic B, Borden KLB. The Cap-Binding Complex CBC and the Eukaryotic Translation Factor eIF4E: Co-Conspirators in Cap-Dependent RNA Maturation and Translation. Cancers (Basel) 2021;13:6185. doi: 10.3390/cancers13246185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dou Y, Kalmykova S, Pashkova M, Oghbaie M, Jiang H, Molloy KR, et al. Affinity proteomic dissection of the human nuclear cap-binding complex interactome. Nucleic Acids Res. 2020;48:10456–10469. doi: 10.1093/nar/gkaa743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Jensen KB, Dredge BK, Toubia J, Jin X, Iadevaia V, Goodall GJ, et al. capCLIP: a new tool to probe translational control in human cells through capture and identification of the eIF4E-mRNA interactome. Nucleic Acids Res. 2021;49:e105. doi: 10.1093/nar/gkab604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.García-Vílchez R, Añazco-Guenkova AM, López J, Dietmann S, Tomé M, Jimeno S, et al. N7-methylguanosine methylation of tRNAs regulates survival to stress in cancer. Oncogene. 2023;42:3169–3181. doi: 10.1038/s41388-023-02825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Du D, He J, Ju C, Wang C, Li H, He F, et al. When N7-methyladenosine modification meets cancer: Emerging frontiers and promising therapeutic opportunities. Cancer Lett. 2023;562:216165. doi: 10.1016/j.canlet.2023.216165. [DOI] [PubMed] [Google Scholar]
- 127.Orellana EA, Liu Q, Yankova E, Pirouz M, De Braekeleer E, Zhang W, et al. METTL1-mediated m7G modification of Arg-TCT tRNA drives oncogenic transformation. Mol Cell. 2021;81:3323–3338.e14. doi: 10.1016/j.molcel.2021.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.García-Vílchez R, Añazco-Guenkova AM, Dietmann S, López J, Morón-Calvente V, D’Ambrosi S, et al. METTL1 promotes tumorigenesis through tRNA-derived fragment biogenesis in prostate cancer. Mol Cancer. 2023;22:119. doi: 10.1186/s12943-023-01809-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chen H, Guo Y, Sun J, Dong J, Bao Q, Zhang X, et al. Preferential Expression of B7–H6 in Glioma Stem-Like Cells Enhances Tumor Cell Proliferation via the c-Myc/RNMT Axis. J Immunol Res. 2020;2020:1–12. doi: 10.1155/2020/2328675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lentini JM, Alsaif HS, Faqeih E, Alkuraya FS, Fu D. DALRD3 encodes a protein mutated in epileptic encephalopathy that targets arginine tRNAs for 3-methylcytosine modification. Nat Commun. 2020;11:2510. doi: 10.1038/s41467-020-16321-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ignatova VV, Kaiser S, Ho JSY, Bing X, Stolz P, Tan YX, et al. METTL6 is a tRNA m3C methyltransferase that regulates pluripotency and tumor cell growth. Sci Adv. 2020;6:eaaz4551. doi: 10.1126/sciadv.aaz4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Guo L, Yang H, Zhou C, Shi Y, Huang L, Zhang J. N6-Methyladenosine RNA Modification in the Tumor Immune Microenvironment: Novel Implications for Immunotherapy. Front Immunol. 2021;12:773570. doi: 10.3389/fimmu.2021.773570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Riera-Domingo C, Audigé A, Granja S, Cheng W-C, Ho P-C, Baltazar F, et al. Immunity, Hypoxia, and Metabolism-the Ménage à Trois of Cancer: Implications for Immunotherapy. Physiol Rev. 2020;100:1–102. doi: 10.1152/physrev.00018.2019. [DOI] [PubMed] [Google Scholar]
- 134.Binnewies M, Roberts EW, Kersten K, Chan V, Fearon DF, Merad M, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24:541–550. doi: 10.1038/s41591-018-0014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cao X, Geng Q, Fan D, Wang Q, Wang X, Zhang M, et al. m6A methylation: a process reshaping the tumour immune microenvironment and regulating immune evasion. Mol Cancer. 2023;22:42. doi: 10.1186/s12943-022-01704-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fu T, Dai L-J, Wu S-Y, Xiao Y, Ma D, Jiang Y-Z, et al. Spatial architecture of the immune microenvironment orchestrates tumor immunity and therapeutic response. J Hematol Oncol. 2021;14:98. doi: 10.1186/s13045-021-01103-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Surendran V, Rutledge D, Colmon R, Chandrasekaran A. A novel tumor-immune microenvironment (TIME)-on-Chip mimics three dimensional neutrophil-tumor dynamics and neutrophil extracellular traps (NETs)-mediated collective tumor invasion. Biofabrication. 2021;13. [DOI] [PMC free article] [PubMed]
- 138.Gu Y, Wu X, Zhang J, Fang Y, Pan Y, Shu Y, et al. The evolving landscape of N6-methyladenosine modification in the tumor microenvironment. Mol Ther. 2021;29:1703–1715. doi: 10.1016/j.ymthe.2021.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhang B, Wu Q, Li B, Wang D, Wang L, Zhou YL. m6A regulator-mediated methylation modification patterns and tumor microenvironment infiltration characterization in gastric cancer. Mol Cancer. 2020;19:53. doi: 10.1186/s12943-020-01170-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wang Y, Wang Y, Ren Y, Zhang Q, Yi P, Cheng C. Metabolic modulation of immune checkpoints and novel therapeutic strategies in cancer. Semin Cancer Biol. 2022;86:542–565. doi: 10.1016/j.semcancer.2022.02.010. [DOI] [PubMed] [Google Scholar]
- 141.van den Homberg DAL, van der Kwast RVCT, Quax PHA, Nossent AY. N-6-Methyladenosine in Vasoactive microRNAs during Hypoxia; A Novel Role for METTL4. Int J Mol Sci. 2022;23:1057. doi: 10.3390/ijms23031057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.An Y, Duan H. The role of m6A RNA methylation in cancer metabolism. Mol Cancer. 2022;21:14. doi: 10.1186/s12943-022-01500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bhandari V, Hoey C, Liu LY, Lalonde E, Ray J, Livingstone J, et al. Molecular landmarks of tumor hypoxia across cancer types. Nat Genet. 2019;51:308–318. doi: 10.1038/s41588-018-0318-2. [DOI] [PubMed] [Google Scholar]
- 144.Shen X, Zhong J, He J, Han J, Chen N. Identification of m6A modification patterns and development of m6A–hypoxia prognostic signature to characterize tumor microenvironment in triple-negative breast cancer. Front Immunol. 2022;13:978092. doi: 10.3389/fimmu.2022.978092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Li Y, Zhao L, Li X-F. Hypoxia and the Tumor Microenvironment. Technol Cancer Res Treat. 2021;20:15330338211036304. doi: 10.1177/15330338211036304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gilkes DM, Semenza GL, Wirtz D. Hypoxia and the extracellular matrix: drivers of tumour metastasis. Nat Rev Cancer. 2014;14:430–439. doi: 10.1038/nrc3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Liu Y, Yan W, Tohme S, Chen M, Fu Y, Tian D, et al. Hypoxia induced HMGB1 and mitochondrial DNA interactions mediate tumor growth in hepatocellular carcinoma through Toll-like receptor 9. J Hepatol. 2015;63:114–121. doi: 10.1016/j.jhep.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Yao Y, Yang Y, Guo W, Xu L, You M, Zhang Y-C, et al. METTL3-dependent m6A modification programs T follicular helper cell differentiation. Nat Commun. 2021;12:1333. doi: 10.1038/s41467-021-21594-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kostyusheva A, Brezgin S, Glebe D, Kostyushev D, Chulanov V. Host-cell interactions in HBV infection and pathogenesis: the emerging role of m6A modification. Emerg Microbes Infect. 2021;10:2264–2275. doi: 10.1080/22221751.2021.2006580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Song H, Feng X, Zhang H, Luo Y, Huang J, Lin M, et al. METTL3 and ALKBH5 oppositely regulate m6A modification of TFEB mRNA, which dictates the fate of hypoxia/reoxygenation-treated cardiomyocytes. Autophagy. 2019;15:1419–1437. doi: 10.1080/15548627.2019.1586246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.DePeaux K, Delgoffe GM. Metabolic barriers to cancer immunotherapy. Nat Rev Immunol. 2021;21:785–797. doi: 10.1038/s41577-021-00541-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Reinfeld BI, Madden MZ, Wolf MM, Chytil A, Bader JE, Patterson AR, et al. Cell-programmed nutrient partitioning in the tumour microenvironment. Nature. 2021;593:282–288. doi: 10.1038/s41586-021-03442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Xia L, Oyang L, Lin J, Tan S, Han Y, Wu N, et al. The cancer metabolic reprogramming and immune response. Mol Cancer. 2021;20:28. doi: 10.1186/s12943-021-01316-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Guerra L, Bonetti L, Brenner D. Metabolic Modulation of Immunity: A New Concept in Cancer Immunotherapy. Cell Rep. 2020;32:107848. doi: 10.1016/j.celrep.2020.107848. [DOI] [PubMed] [Google Scholar]
- 155.Shen C, Xuan B, Yan T, Ma Y, Xu P, Tian X, et al. m6A-dependent glycolysis enhances colorectal cancer progression. Mol Cancer. 2020;19:72. doi: 10.1186/s12943-020-01190-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Chen L, Lin X, Lei Y, Xu X, Zhou Q, Chen Y, et al. Aerobic glycolysis enhances HBx-initiated hepatocellular carcinogenesis via NF-κBp65/HK2 signalling. J Exp Clin Cancer Res. 2022;41:329. doi: 10.1186/s13046-022-02531-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Zhang X, Yin H, Zhang X, Jiang X, Liu Y, Zhang H, et al. N6-methyladenosine modification governs liver glycogenesis by stabilizing the glycogen synthase 2 mRNA. Nat Commun. 2022;13:7038. doi: 10.1038/s41467-022-34808-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Wang F, Qi X-M, Wertz R, Mortensen M, Hagen C, Evans J, et al. p38γ MAPK Is Essential for Aerobic Glycolysis and Pancreatic Tumorigenesis. Cancer Res. 2020;80:3251–3264. doi: 10.1158/0008-5472.CAN-19-3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Xu X, Zhang M, Xu F, Jiang S. Wnt signaling in breast cancer: biological mechanisms, challenges and opportunities. Mol Cancer. 2020;19:165. doi: 10.1186/s12943-020-01276-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hinshaw DC, Hanna A, Lama-Sherpa T, Metge B, Kammerud SC, Benavides GA, et al. Hedgehog Signaling Regulates Metabolism and Polarization of Mammary Tumor-Associated Macrophages. Cancer Res. 2021;81:5425–5437. doi: 10.1158/0008-5472.CAN-20-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Spannl S, Buhl T, Nellas I, Zeidan SA, Iyer KV, Khaliullina H, et al. Glycolysis regulates Hedgehog signalling via the plasma membrane potential. EMBO J. 2020;39:e101767. doi: 10.15252/embj.2019101767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Li M, Deng L, Xu G. METTL14 promotes glomerular endothelial cell injury and diabetic nephropathy via m6A modification of α-klotho. Mol Med. 2021;27:106. doi: 10.1186/s10020-021-00365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Huang J, Sun W, Wang Z, Lv C, Zhang T, Zhang D, et al. FTO suppresses glycolysis and growth of papillary thyroid cancer via decreasing stability of APOE mRNA in an N6-methyladenosine-dependent manner. J Exp Clin Cancer Res. 2022;41:42. doi: 10.1186/s13046-022-02254-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Chen T, Xu Z-G, Luo J, Manne RK, Wang Z, Hsu C-C, et al. NSUN2 is a glucose sensor suppressing cGAS/STING to maintain tumorigenesis and immunotherapy resistance. Cell Metabolism. 2023 [cited 2023 Sep 14]; Available from: https://www.sciencedirect.com/science/article/pii/S155041312300267X [DOI] [PMC free article] [PubMed]
- 165.Zhang H, Zhai X, Liu Y, Xia Z, Xia T, Du G, et al. NOP2-mediated m5C Modification of c-Myc in an EIF3A-Dependent Manner to Reprogram Glucose Metabolism and Promote Hepatocellular Carcinoma Progression. Research (Wash D C) 2023;6:0184. doi: 10.34133/research.0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Li Z, Zhang H. Reprogramming of glucose, fatty acid and amino acid metabolism for cancer progression. Cell Mol Life Sci. 2016;73:377–392. doi: 10.1007/s00018-015-2070-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yu W, Lei Q, Yang L, Qin G, Liu S, Wang D, et al. Contradictory roles of lipid metabolism in immune response within the tumor microenvironment. J Hematol Oncol. 2021;14:187. doi: 10.1186/s13045-021-01200-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Fan C, Zhang S, Gong Z, Li X, Xiang B, Deng H, et al. Emerging role of metabolic reprogramming in tumor immune evasion and immunotherapy. Sci China Life Sci. 2021;64:534–547. doi: 10.1007/s11427-019-1735-4. [DOI] [PubMed] [Google Scholar]
- 169.Peng Z, Gong Y, Wang X, He W, Wu L, Zhang L, et al. METTL3-m6A-Rubicon axis inhibits autophagy in nonalcoholic fatty liver disease. Mol Ther. 2022;30:932–946. doi: 10.1016/j.ymthe.2021.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Yang Y, Cai J, Yang X, Wang K, Sun K, Yang Z, et al. Dysregulated m6A modification promotes lipogenesis and development of non-alcoholic fatty liver disease and hepatocellular carcinoma. Mol Ther. 2022;30:2342–2353. doi: 10.1016/j.ymthe.2022.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Duan X, Yang L, Wang L, Liu Q, Zhang K, Liu S, et al. m6A demethylase FTO promotes tumor progression via regulation of lipid metabolism in esophageal cancer. Cell Biosci. 2022;12:60. doi: 10.1186/s13578-022-00798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Yang Z, Yu G-L, Zhu X, Peng T-H, Lv Y-C. Critical roles of FTO-mediated mRNA m6A demethylation in regulating adipogenesis and lipid metabolism: Implications in lipid metabolic disorders. Genes Dis. 2022;9:51–61. doi: 10.1016/j.gendis.2021.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Luo L, Liu Y, Nizigiyimana P, Ye M, Xiao Y, Guo Q, et al. DNA 6mA Demethylase ALKBH1 Orchestrates Fatty Acid Metabolism and Suppresses Diet-Induced Hepatic Steatosis. Cell Mol Gastroenterol Hepatol. 2022;14:1213–1233. doi: 10.1016/j.jcmgh.2022.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Peng H, Chen B, Wei W, Guo S, Han H, Yang C, et al. N6-methyladenosine (m6A) in 18S rRNA promotes fatty acid metabolism and oncogenic transformation. Nat Metab. 2022;4:1041–1054. doi: 10.1038/s42255-022-00622-9. [DOI] [PubMed] [Google Scholar]
- 175.Liu Y, Yang Y, Wu R, Gao C, Liao X, Han X, et al. mRNA m5C inhibits adipogenesis and promotes myogenesis by respectively facilitating YBX2 and SMO mRNA export in ALYREF-m5C manner. Cell Mol Life Sci. 2022;79:481. doi: 10.1007/s00018-022-04474-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wang Z, Li B, Li S, Lin W, Wang Z, Wang S, et al. Metabolic control of CD47 expression through LAT2-mediated amino acid uptake promotes tumor immune evasion. Nat Commun. 2022;13:6308. doi: 10.1038/s41467-022-34064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Ma G, Zhang Z, Li P, Zhang Z, Zeng M, Liang Z, et al. Reprogramming of glutamine metabolism and its impact on immune response in the tumor microenvironment. Cell Commun Signal. 2022;20:114. doi: 10.1186/s12964-022-00909-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Leone RD, Zhao L, Englert JM, Sun I-M, Oh M-H, Sun I-H, et al. Glutamine blockade induces divergent metabolic programs to overcome tumor immune evasion. Science. 2019;366:1013–1021. doi: 10.1126/science.aav2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yang W-H, Qiu Y, Stamatatos O, Janowitz T, Lukey MJ. Enhancing the Efficacy of Glutamine Metabolism Inhibitors in Cancer Therapy. Trends Cancer. 2021;7:790–804. doi: 10.1016/j.trecan.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Han L, Dong L, Leung K, Zhao Z, Li Y, Gao L, et al. METTL16 drives leukemogenesis and leukemia stem cell self-renewal by reprogramming BCAA metabolism. Cell Stem Cell. 2023;30:52–68.e13. doi: 10.1016/j.stem.2022.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Weng H, Huang F, Yu Z, Chen Z, Prince E, Kang Y, et al. The m6A reader IGF2BP2 regulates glutamine metabolism and represents a therapeutic target in acute myeloid leukemia. Cancer Cell. 2022;40:1566–1582.e10. doi: 10.1016/j.ccell.2022.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Kim S, Kim NH, Park JE, Hwang JW, Myung N, Hwang K-T, et al. PRMT6-mediated H3R2me2a guides Aurora B to chromosome arms for proper chromosome segregation. Nat Commun. 2020;11:612. doi: 10.1038/s41467-020-14511-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cheng Y, Gao Z, Zhang T, Wang Y, Xie X, Han G, et al. oding m6A RNA methylome identifies PRMT6-regulated lipid transport promoting AML stem cell maintenance. Cell Stem Cell. 2023;30:69–85.e7. doi: 10.1016/j.stem.2022.12.003. [DOI] [PubMed] [Google Scholar]
- 184.Wang Y, Wang C, Guan X, Ma Y, Zhang S, Li F, et al. PRMT3-Mediated Arginine Methylation of METTL14 Promotes Malignant Progression and Treatment Resistance in Endometrial Carcinoma. Adv Sci (Weinh). 2023;10(36):e2303812. doi: 10.1002/advs.202303812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Huang H, Weng H, Zhou K, Wu T, Zhao BS, Sun M, et al. Histone H3 trimethylation at lysine 36 guides m6A RNA modification co-transcriptionally. Nature. 2019;567:414–419. doi: 10.1038/s41586-019-1016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Liu X, Wang H, Zhao X, Luo Q, Wang Q, Tan K, et al. Arginine methylation of METTL14 promotes RNA N6-methyladenosine modification and endoderm differentiation of mouse embryonic stem cells. Nat Commun. 2021;12:3780. doi: 10.1038/s41467-021-24035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Li T, Tan Y-T, Chen Y-X, Zheng X-J, Wang W, Liao K, et al. Methionine deficiency facilitates antitumour immunity by altering m6A methylation of immune checkpoint transcripts. Gut. 2023;72:501–511. doi: 10.1136/gutjnl-2022-326928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.DeBerardinis RJ. Tumor Microenvironment, Metabolism, and Immunotherapy. N Engl J Med. 2020;382:869–871. doi: 10.1056/NEJMcibr1914890. [DOI] [PubMed] [Google Scholar]
- 189.Gebeyew K, Yang C, Mi H, Cheng Y, Zhang T, Hu F, et al. Lipid metabolism and m6A RNA methylation are altered in lambs supplemented rumen-protected methionine and lysine in a low-protein diet. J Anim Sci Biotechnol. 2022;13:85. doi: 10.1186/s40104-022-00733-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Fang L, Huang H, Lv J, Chen Z, Lu C, Jiang T, et al. m5C-methylated lncRNA NR_033928 promotes gastric cancer proliferation by stabilizing GLS mRNA to promote glutamine metabolism reprogramming. Cell Death Dis. 2023;14:520. doi: 10.1038/s41419-023-06049-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Gong J, Yang J, He Y, Chen X, Yang G, Sun R. Construction of m7G subtype classification on heterogeneity of sepsis. Front Genet. 2022;13:1021770. doi: 10.3389/fgene.2022.1021770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Maiorino L, Daßler-Plenker J, Sun L, Egeblad M. Innate Immunity and Cancer Pathophysiology. Annu Rev Pathol. 2022;17:425–457. doi: 10.1146/annurev-pathmechdis-032221-115501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Demaria O, Cornen S, Daëron M, Morel Y, Medzhitov R, Vivier E. Harnessing innate immunity in cancer therapy. Nature. 2019;574:45–56. doi: 10.1038/s41586-019-1593-5. [DOI] [PubMed] [Google Scholar]
- 194.Niu Y, Chen J, Qiao Y. Epigenetic Modifications in Tumor-Associated Macrophages: A New Perspective for an Old Foe. Front Immunol. 2022;13:836223. doi: 10.3389/fimmu.2022.836223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Pan Y, Yu Y, Wang X, Zhang T. Tumor-Associated Macrophages in Tumor Immunity. Front Immunol. 2020;11:583084. doi: 10.3389/fimmu.2020.583084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wen Z, Sun H, Zhang Z, Zheng Y, Zheng S, Bin J, et al. High baseline tumor burden-associated macrophages promote an immunosuppressive microenvironment and reduce the efficacy of immune checkpoint inhibitors through the IGFBP2-STAT3-PD-L1 pathway. Cancer Commun (Lond) 2023;43:562–581. doi: 10.1002/cac2.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wu K, Lin K, Li X, Yuan X, Xu P, Ni P, et al. Redefining Tumor-Associated Macrophage Subpopulations and Functions in the Tumor Microenvironment. Front Immunol. 2020;11:1731. doi: 10.3389/fimmu.2020.01731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Tcyganov E, Mastio J, Chen E, Gabrilovich DI. Plasticity of myeloid-derived suppressor cells in cancer. Curr Opin Immunol. 2018;51:76–82. doi: 10.1016/j.coi.2018.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Xiang X, Wang J, Lu D, Xu X. Targeting tumor-associated macrophages to synergize tumor immunotherapy. Signal Transduct Target Ther. 2021;6:75. doi: 10.1038/s41392-021-00484-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.DeNardo DG, Ruffell B. Macrophages as regulators of tumour immunity and immunotherapy. Nat Rev Immunol. 2019;19:369–382. doi: 10.1038/s41577-019-0127-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Zhang Q, He Y, Luo N, Patel SJ, Han Y, Gao R, et al. Landscape and Dynamics of Single Immune Cells in Hepatocellular Carcinoma. Cell. 2019;179:829–845.e20. doi: 10.1016/j.cell.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 202.Boutilier AJ, Elsawa SF. Macrophage Polarization States in the Tumor Microenvironment. Int J Mol Sci. 2021;22:6995. doi: 10.3390/ijms22136995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Orecchioni M, Ghosheh Y, Pramod AB, Ley K. Macrophage Polarization: Different Gene Signatures in M1(LPS+) vs. Classically and M2(LPS-) vs. Alternatively Activated Macrophages. Front Immunol. 2019;10:1084. doi: 10.3389/fimmu.2019.01084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Shrivastava R, Asif M, Singh V, Dubey P, Ahmad Malik S, Lone MUD, et al. M2 polarization of macrophages by Oncostatin M in hypoxic tumor microenvironment is mediated by mTORC2 and promotes tumor growth and metastasis. Cytokine. 2019;118:130–43. doi: 10.1016/j.cyto.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 205.Yin H, Zhang X, Yang P, Zhang X, Peng Y, Li D, et al. RNA m6A methylation orchestrates cancer growth and metastasis via macrophage reprogramming. Nat Commun. 2021;12:1394. doi: 10.1038/s41467-021-21514-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wang J, Yan S, Lu H, Wang S, Xu D. METTL3 Attenuates LPS-Induced Inflammatory Response in Macrophages via NF-κB Signaling Pathway. Mediators Inflamm. 2019;2019:3120391. doi: 10.1155/2019/3120391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Shu B, Zhou Y-X, Li H, Zhang R-Z, He C, Yang X. The METTL3/MALAT1/PTBP1/USP8/TAK1 axis promotes pyroptosis and M1 polarization of macrophages and contributes to liver fibrosis. Cell Death Discov. 2021;7:368. doi: 10.1038/s41420-021-00756-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Liu Y, Liu Z, Tang H, Shen Y, Gong Z, Xie N, et al. The N6-methyladenosine (m6A)-forming enzyme METTL3 facilitates M1 macrophage polarization through the methylation of STAT1 mRNA. Am J Physiol Cell Physiol. 2019;317:C762–C775. doi: 10.1152/ajpcell.00212.2019. [DOI] [PubMed] [Google Scholar]
- 209.Gou Y, Wang H, Wang T, Wang H, Wang B, Jiao N, et al. Ectopic endometriotic stromal cells-derived lactate induces M2 macrophage polarization via Mettl3/Trib1/ERK/STAT3 signalling pathway in endometriosis. Immunology. 2023;168:389–402. doi: 10.1111/imm.13574. [DOI] [PubMed] [Google Scholar]
- 210.Feng Y, Dong H, Sun B, Hu Y, Yang Y, Jia Y, et al. METTL3/METTL14 Transactivation and m6A-Dependent TGF-β1 Translation in Activated Kupffer Cells. Cell Mol Gastroenterol Hepatol. 2021;12:839–856. doi: 10.1016/j.jcmgh.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Li Q, Yu L, Gao A, Ren R, Zhang J, Cao L, et al. METTL3 (Methyltransferase Like 3)-Dependent N6-Methyladenosine Modification on Braf mRNA Promotes Macrophage Inflammatory Response and Atherosclerosis in Mice. Arterioscler Thromb Vasc Biol. 2023;43:755–773. doi: 10.1161/ATVBAHA.122.318451. [DOI] [PubMed] [Google Scholar]
- 212.Gu X, Zhang Y, Li D, Cai H, Cai L, Xu Q. N6-methyladenosine demethylase FTO promotes M1 and M2 macrophage activation. Cell Signal. 2020;69:109553. doi: 10.1016/j.cellsig.2020.109553. [DOI] [PubMed] [Google Scholar]
- 213.Zhao Y, Sun J, Jin L. The N6-Methyladenosine Regulator ALKBH5 Mediated Stromal Cell-Macrophage Interaction via VEGF Signaling to Promote Recurrent Spontaneous Abortion: A Bioinformatic and In Vitro Study. Int J Mol Sci. 2022;23:15819. doi: 10.3390/ijms232415819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Wang X, Ji Y, Feng P, Liu R, Li G, Zheng J, et al. The m6A Reader IGF2BP2 Regulates Macrophage Phenotypic Activation and Inflammatory Diseases by Stabilizing TSC1 and PPARγ. Adv Sci (Weinh) 2021;8:2100209. doi: 10.1002/advs.202100209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sun L, Zhang X, Song Q, Liu L, Forbes E, Tian W, et al. IGFBP2 promotes tumor progression by inducing alternative polarization of macrophages in pancreatic ductal adenocarcinoma through the STAT3 pathway. Cancer Lett. 2021;500:132–146. doi: 10.1016/j.canlet.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Yu G, Bao J, Zhan M, Wang J, Li X, Gu X, et al. Comprehensive Analysis of m5C Methylation Regulatory Genes and Tumor Microenvironment in Prostate Cancer. Front Immunol. 2022;13:914577. doi: 10.3389/fimmu.2022.914577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Jin S, Li J, Shen Y, Wu Y, Zhang Z, Ma H. RNA 5-Methylcytosine Regulator NSUN3 promotes tumor progression through regulating immune infiltration in head and neck squamous cell carcinoma. Oral Diseases. 2022 [cited 2023 Oct 12];n/a. Available from: 10.1111/odi.14357 [DOI] [PubMed]
- 218.Yan D, Xie Y, Huang L, Zhang Y, Gu R, Xie H, et al. RNA m5C methylation orchestrates BLCA progression via macrophage reprogramming. J Cell Mol Med. 2023;27:2398–2411. doi: 10.1111/jcmm.17826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Lv Z, Xue C, Zhang L, Sun J, Bo C. Elevated mRNA Level of Y-Box Binding Protein 1 Indicates Unfavorable Prognosis Correlated with Macrophage Infiltration and T Cell Exhaustion in Luminal Breast Cancer. Cancer Manag Res. 2021;13:6411–6428. doi: 10.2147/CMAR.S311650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Wu Y, Jiang D, Zhang H, Yin F, Guo P, Zhang X, et al. N1-Methyladenosine (m1A) Regulation Associated With the Pathogenesis of Abdominal Aortic Aneurysm Through YTHDF3 Modulating Macrophage Polarization. Front Cardiovasc Med. 2022;9:883155. doi: 10.3389/fcvm.2022.883155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zheng P, Li N, Zhan X. Ovarian cancer subtypes based on the regulatory genes of RNA modifications: Novel prediction model of prognosis. Front Endocrinol (Lausanne) 2022;13:972341. doi: 10.3389/fendo.2022.972341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Wang Y, Xiang Y, Xin VW, Wang X-W, Peng X-C, Liu X-Q, et al. Dendritic cell biology and its role in tumor immunotherapy. J Hematol Oncol. 2020;13:107. doi: 10.1186/s13045-020-00939-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Verneau J, Sautés-Fridman C, Sun C-M. Dendritic cells in the tumor microenvironment: prognostic and theranostic impact. Semin Immunol. 2020;48:101410. doi: 10.1016/j.smim.2020.101410. [DOI] [PubMed] [Google Scholar]
- 224.Diamond MS, Lin JH, Vonderheide RH. Site-Dependent Immune Escape Due to Impaired Dendritic Cell Cross-Priming. Cancer Immunol Res. 2021;9:877–890. doi: 10.1158/2326-6066.CIR-20-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Bai X, Wong CC, Pan Y, Chen H, Liu W, Zhai J, et al. Loss of YTHDF1 in gastric tumors restores sensitivity to antitumor immunity by recruiting mature dendritic cells. J Immunother Cancer. 2022;10:e003663. doi: 10.1136/jitc-2021-003663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Cheng L, Li H, Zhan H, Liu Y, Li X, Huang Y, et al. Alterations of m6A RNA methylation regulators contribute to autophagy and immune infiltration in primary Sjögren’s syndrome. Front Immunol. 2022;13:949206. doi: 10.3389/fimmu.2022.949206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Gong P-J, Shao Y-C, Yang Y, Song W-J, He X, Zeng Y-F, et al. Analysis of N6-Methyladenosine Methyltransferase Reveals METTL14 and ZC3H13 as Tumor Suppressor Genes in Breast Cancer. Front Oncol. 2020;10:578963. doi: 10.3389/fonc.2020.578963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Chen Y, Lei J, He S. m6A Modification Mediates Mucosal Immune Microenvironment and Therapeutic Response in Inflammatory Bowel Disease. Front Cell Dev Biol. 2021;9:692160. doi: 10.3389/fcell.2021.692160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Han D, Liu J, Chen C, Dong L, Liu Y, Chang R, et al. Anti-tumour immunity controlled through mRNA m6A methylation and YTHDF1 in dendritic cells. Nature. 2019;566:270–274. doi: 10.1038/s41586-019-0916-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Cai Y, Wu G, Peng B, Li J, Zeng S, Yan Y, et al. Expression and molecular profiles of the AlkB family in ovarian serous carcinoma. Aging (Albany NY) 2021;13:9679–9692. doi: 10.18632/aging.202716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Aarts CEM, Hiemstra IH, Béguin EP, Hoogendijk AJ, Bouchmal S, van Houdt M, et al. Activated neutrophils exert myeloid-derived suppressor cell activity damaging T cells beyond repair. Blood Adv. 2019;3:3562–3574. doi: 10.1182/bloodadvances.2019031609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Adewunmi O, Shen Y, Zhang XH-F, Rosen JM. Targeted Inhibition of lncRNA Malat1 Alters the Tumor Immune Microenvironment in Preclinical Syngeneic Mouse Models of Triple-Negative Breast Cancer. Cancer Immunol Res. 2023;11:1462–79. doi: 10.1158/2326-6066.CIR-23-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Ni H-H, Zhang L, Huang H, Dai S-Q, Li J. Connecting METTL3 and intratumoural CD33+ MDSCs in predicting clinical outcome in cervical cancer. J Transl Med. 2020;18:393. doi: 10.1186/s12967-020-02553-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Chen H, Pan Y, Zhou Q, Liang C, Wong C-C, Zhou Y, et al. METTL3 Inhibits Antitumor Immunity by Targeting m6A-BHLHE41-CXCL1/CXCR2 Axis to Promote Colorectal Cancer. Gastroenterology. 2022;163:891–907. doi: 10.1053/j.gastro.2022.06.024. [DOI] [PubMed] [Google Scholar]
- 235.Lyu Z, Huang B, Zhang J, Qian Q, Pu X, Cui N, et al. Suppression of YTHDF2 attenuates autoimmune hepatitis by expansion of myeloid-derived suppressor cells. J Autoimmun. 2023;135:102993. doi: 10.1016/j.jaut.2023.102993. [DOI] [PubMed] [Google Scholar]
- 236.Wang L, Dou X, Chen S, Yu X, Huang X, Zhang L, et al. YTHDF2 inhibition potentiates radiotherapy antitumor efficacy. Cancer Cell. 2023;41:1294–1308.e8. doi: 10.1016/j.ccell.2023.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Li N, Kang Y, Wang L, Huff S, Tang R, Hui H, et al. ALKBH5 regulates anti-PD-1 therapy response by modulating lactate and suppressive immune cell accumulation in tumor microenvironment. Proc Natl Acad Sci U S A. 2020;117:20159–20170. doi: 10.1073/pnas.1918986117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Liu H, Zeng X, Ren X, Zhang Y, Huang M, Tan L, et al. Targeting tumour-intrinsic N7-methylguanosine tRNA modification inhibits MDSC recruitment and improves anti-PD-1 efficacy. Gut. 2023;72:1555–1567. doi: 10.1136/gutjnl-2022-327230. [DOI] [PubMed] [Google Scholar]
- 239.Zeng X, Liao G, Li S, Liu H, Zhao X, Li S, et al. Eliminating METTL1-mediated accumulation of PMN-MDSCs prevents hepatocellular carcinoma recurrence after radiofrequency ablation. Hepatology. 2023;77:1122–1138. doi: 10.1002/hep.32585. [DOI] [PubMed] [Google Scholar]
- 240.Shulman Z, Stern-Ginossar N. The RNA modification N6-methyladenosine as a novel regulator of the immune system. Nat Immunol. 2020;21:501–512. doi: 10.1038/s41590-020-0650-4. [DOI] [PubMed] [Google Scholar]
- 241.Dong L, Chen C, Zhang Y, Guo P, Wang Z, Li J, et al. The loss of RNA N6-adenosine methyltransferase Mettl14 in tumor-associated macrophages promotes CD8+ T cell dysfunction and tumor growth. Cancer Cell. 2021;39:945–957.e10. doi: 10.1016/j.ccell.2021.04.016. [DOI] [PubMed] [Google Scholar]
- 242.Frias AB, Boi SK, Lan X, Youngblood B. Epigenetic regulation of T cell adaptive immunity. Immunol Rev. 2021;300:9–21. doi: 10.1111/imr.12943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Davenport MP, Smith NL, Rudd BD. Building a T cell compartment: how immune cell development shapes function. Nat Rev Immunol. 2020;20:499–506. doi: 10.1038/s41577-020-0332-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Takaba H, Takayanagi H. The Mechanisms of T Cell Selection in the Thymus. Trends Immunol. 2017;38:805–816. doi: 10.1016/j.it.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 245.Calis JJA, van Loosdregt J. N6-adenosine methylation (m6A) is involved in the life and death decisions of T cells. Cell Mol Immunol. 2023;20:316–317. doi: 10.1038/s41423-022-00958-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Chao Y, Li H-B, Zhou J. Multiple Functions of RNA Methylation in T Cells: A Review. Front Immunol. 2021;12:627455. doi: 10.3389/fimmu.2021.627455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Lu S, Wei X, Zhu H, Hu Z, Zheng M, Wu J, et al. m6A methyltransferase METTL3 programs CD4+ T-cell activation and effector T-cell differentiation in systemic lupus erythematosus. Mol Med. 2023;29:46. doi: 10.1186/s10020-023-00643-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Li H-B, Tong J, Zhu S, Batista PJ, Duffy EE, Zhao J, et al. m6A mRNA methylation controls T cell homeostasis by targeting the IL-7/STAT5/SOCS pathways. Nature. 2017;548:338–342. doi: 10.1038/nature23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Ito-Kureha T, Leoni C, Borland K, Cantini G, Bataclan M, Metzger RN, et al. The function of Wtap in N6-adenosine methylation of mRNAs controls T cell receptor signaling and survival of T cells. Nat Immunol. 2022;23:1208–1221. doi: 10.1038/s41590-022-01268-1. [DOI] [PubMed] [Google Scholar]
- 250.Zhou J, Zhang X, Hu J, Qu R, Yu Z, Xu H, et al. m6A demethylase ALKBH5 controls CD4+ T cell pathogenicity and promotes autoimmunity. Sci Adv. 2021;7:eabg0470. doi: 10.1126/sciadv.abg0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Tirumuru N, Wu L. HIV-1 envelope proteins up-regulate N6-methyladenosine levels of cellular RNA independently of viral replication. J Biol Chem. 2019;294:3249–3260. doi: 10.1074/jbc.RA118.005608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Pendleton KE, Chen B, Liu K, Hunter OV, Xie Y, Tu BP, et al. The U6 snRNA m6A Methyltransferase METTL16 Regulates SAM Synthetase Intron Retention. Cell. 2017;169:824–835.e14. doi: 10.1016/j.cell.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Jurczyszak D, Zhang W, Terry SN, Kehrer T, Bermúdez González MC, McGregor E, et al. HIV protease cleaves the antiviral m6A reader protein YTHDF3 in the viral particle. PLoS Pathog. 2020;16:e1008305. doi: 10.1371/journal.ppat.1008305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Lu W, Tirumuru N, St Gelais C, Koneru PC, Liu C, Kvaratskhelia M, et al. N6-Methyladenosine-binding proteins suppress HIV-1 infectivity and viral production. J Biol Chem. 2018;293:12992–13005. doi: 10.1074/jbc.RA118.004215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Kong W, Biswas A, Zhou D, Fiches G, Fujinaga K, Santoso N, et al. Nucleolar protein NOP2/NSUN1 suppresses HIV-1 transcription and promotes viral latency by competing with Tat for TAR binding and methylation. PLoS Pathog. 2020;16:e1008430. doi: 10.1371/journal.ppat.1008430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Poudyal D, Yang J, Chen Q, Goswami S, Adelsberger JW, Das S, et al. IL-27 posttranslationally regulates Y-box binding protein-1 to inhibit HIV-1 replication in human CD4+ T cells. AIDS. 2019;33:1819–1830. doi: 10.1097/QAD.0000000000002288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Guo G, Wang H, Shi X, Ye L, Yan K, Chen Z, et al. Disease Activity-Associated Alteration of mRNA m5 C Methylation in CD4+ T Cells of Systemic Lupus Erythematosus. Front Cell Dev Biol. 2020;8:430. doi: 10.3389/fcell.2020.00430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.A G, A K, D D, A A, H Y, C G-M, et al. Upregulation of RNA cap methyltransferase RNMT drives ribosome biogenesis during T cell activation. Nucleic acids research. 2021 [cited 2023 Oct 26];49. Available from: https://pubmed.ncbi.nlm.nih.gov/34125914/ [DOI] [PMC free article] [PubMed]
- 259.Rak R, Polonsky M, Eizenberg-Magar I, Mo Y, Sakaguchi Y, Mizrahi O, et al. Dynamic changes in tRNA modifications and abundance during T cell activation. Proc Natl Acad Sci U S A. 2021;118:e2106556118. doi: 10.1073/pnas.2106556118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Tsuchiya K, Yoshimura K, Inoue Y, Iwashita Y, Yamada H, Kawase A, et al. YTHDF1 and YTHDF2 are associated with better patient survival and an inflamed tumor-immune microenvironment in non-small-cell lung cancer. Oncoimmunology. 2021;10:1962656. doi: 10.1080/2162402X.2021.1962656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Zhao Y, Sun H, Zheng J, Shao C. Analysis of RNA m6A methylation regulators and tumour immune cell infiltration characterization in prostate cancer. Artif Cells Nanomed Biotechnol. 2021;49:407–435. doi: 10.1080/21691401.2021.1912759. [DOI] [PubMed] [Google Scholar]
- 262.Tian L, Wang Y, Tian J, Song W, Li L, Che G. Prognostic Value and Genome Signature of m6A/m5C Regulated Genes in Early-Stage Lung Adenocarcinoma. Int J Mol Sci. 2023;24:6520. doi: 10.3390/ijms24076520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.He X, Tan L, Ni J, Shen G. Expression pattern of m6A regulators is significantly correlated with malignancy and antitumor immune response of breast cancer. Cancer Gene Ther. 2021;28:188–196. doi: 10.1038/s41417-020-00208-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Ma S, Sun B, Duan S, Han J, Barr T, Zhang J, et al. YTHDF2 orchestrates tumor-associated macrophage reprogramming and controls antitumor immunity through CD8+ T cells. Nat Immunol. 2023;24:255–266. doi: 10.1038/s41590-022-01398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Chen G, Ren D, Wang Y, Wang H, Zhang J, Yang S. YTHDF2 negatively correlates with tumor immune infiltration in small cell lung cancer. J Mol Histol. 2023;54:365–377. doi: 10.1007/s10735-023-10129-6. [DOI] [PubMed] [Google Scholar]
- 266.Liu Z, Wang T, She Y, Wu K, Gu S, Li L, et al. N6-methyladenosine-modified circIGF2BP3 inhibits CD8+ T-cell responses to facilitate tumor immune evasion by promoting the deubiquitination of PD-L1 in non-small cell lung cancer. Mol Cancer. 2021;20:105. doi: 10.1186/s12943-021-01398-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Hu Z, Chen G, Zhao Y, Gao H, Li L, Yin Y, et al. Exosome-derived circCCAR1 promotes CD8 + T-cell dysfunction and anti-PD1 resistance in hepatocellular carcinoma. Mol Cancer. 2023;22:55. doi: 10.1186/s12943-023-01759-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Liu Y, Liang G, Xu H, Dong W, Dong Z, Qiu Z, et al. Tumors exploit FTO-mediated regulation of glycolytic metabolism to evade immune surveillance. Cell Metab. 2021;33:1221–1233.e11. doi: 10.1016/j.cmet.2021.04.001. [DOI] [PubMed] [Google Scholar]
- 269.Ge J, Liu S-L, Zheng J-X, Shi Y, Shao Y, Duan Y-J, et al. RNA demethylase ALKBH5 suppresses tumorigenesis via inhibiting proliferation and invasion and promoting CD8+ T cell infiltration in colorectal cancer. Transl Oncol. 2023;34:101683. doi: 10.1016/j.tranon.2023.101683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Pan J, Huang Z, Xu Y. m5C RNA Methylation Regulators Predict Prognosis and Regulate the Immune Microenvironment in Lung Squamous Cell Carcinoma. Front Oncol. 2021;11:657466. doi: 10.3389/fonc.2021.657466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.H R, L B, Z T, K C. Flightless I Homolog Reverses Enzalutamide Resistance through PD-L1-Mediated Immune Evasion in Prostate Cancer. Cancer immunology research. 2021 [cited 2023 Nov 1];9. Available from: https://pubmed.ncbi.nlm.nih.gov/34011528/ [DOI] [PubMed]
- 272.Gao Y, Wang H, Li H, Ye X, Xia Y, Yuan S, et al. Integrated analyses of m1A regulator-mediated modification patterns in tumor microenvironment-infiltrating immune cells in colon cancer. Oncoimmunology. 2021;10:1936758. doi: 10.1080/2162402X.2021.1936758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Huang X, Zhu B, Qian C, Feng Y. The prognostic index of m7G-related genes in CRC correlates with immune infiltration. Sci Rep. 2022;12:21282. doi: 10.1038/s41598-022-25823-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Lu TX, Zheng Z, Zhang L, Sun H-L, Bissonnette M, Huang H, et al. A New Model of Spontaneous Colitis in Mice Induced by Deletion of an RNA m6A Methyltransferase Component METTL14 in T Cells. Cell Mol Gastroenterol Hepatol. 2020;10:747–761. doi: 10.1016/j.jcmgh.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Xu T, Gao S, Ruan H, Liu J, Liu Y, Liu D, et al. METTL14 Acts as a Potential Regulator of Tumor Immune and Progression in Clear Cell Renal Cell Carcinoma. Front Genet. 2021;12:609174. doi: 10.3389/fgene.2021.609174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Ning J, Hou X, Hao J, Zhang W, Shi Y, Huang Y, et al. METTL3 inhibition induced by M2 macrophage-derived extracellular vesicles drives anti-PD-1 therapy resistance via M6A-CD70-mediated immune suppression in thyroid cancer. Cell Death Differ. 2023;30:2265–2279. doi: 10.1038/s41418-023-01217-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Sun L, Zhang Y, Yang T, Chen J, Zhang X, Liang X. IGFBP2 Drives Regulatory T Cell Differentiation through STAT3/IDO Signaling Pathway in Pancreatic Cancer. J Pers Med. 2022;12:2005. doi: 10.3390/jpm12122005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Zhang L, Dou X, Zheng Z, Ye C, Lu TX, Liang HL, et al. YTHDF2/m6A/NF-κB axis controls anti-tumor immunity by regulating intratumoral Tregs. EMBO J. 2023;42:e113126. doi: 10.15252/embj.2022113126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Liu Z, Liu H, Li D, Ma L, Lu T, Sun H, et al. Comprehensive analysis of m6A RNA methylation modification patterns and the immune microenvironment in osteoarthritis. Front Immunol. 2023;14:1128459. doi: 10.3389/fimmu.2023.1128459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Cancro MP, Tomayko MM. Memory B cells and plasma cells: The differentiative continuum of humoral immunity. Immunol Rev. 2021;303:72–82. doi: 10.1111/imr.13016. [DOI] [PubMed] [Google Scholar]
- 281.Wang S, Li H, Lian Z, Deng S. The Role of m6A Modifications in B-Cell Development and B-Cell-Related Diseases. Int J Mol Sci. 2023;24:4721. doi: 10.3390/ijms24054721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Chen X, Lu T, Ding M, Cai Y, Yu Z, Zhou X, et al. Targeting YTHDF2 inhibits tumorigenesis of diffuse large B-cell lymphoma through ACER2-mediated ceramide catabolism. J Adv Res. 2023;S2090–1232(23):00314–324. doi: 10.1016/j.jare.2023.10.010. [DOI] [PubMed] [Google Scholar]
- 283.Zheng Z, Zhang L, Cui X-L, Yu X, Hsu PJ, Lyu R, et al. Control of Early B Cell Development by the RNA N6-Methyladenosine Methylation. Cell Rep. 2020;31:107819. doi: 10.1016/j.celrep.2020.107819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Zhao C, Xu G, Zhang X, Ye Y, Cai W, Shao Q. RNA m6A modification orchestrates the rhythm of immune cell development from hematopoietic stem cells to T and B cells. Front Immunol. 2022;13:839291. doi: 10.3389/fimmu.2022.839291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Wang W, Huang H, Jiang H, Tian C, Tang Y, Gan D, et al. A Cross-Tissue Investigation of Molecular Targets and Physiological Functions of Nsun6 Using Knockout Mice. Int J Mol Sci. 2022;23:6584. doi: 10.3390/ijms23126584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Li J, Zhu Z, Zhu Y, Li J, Li K, Zhong W. METTL3-mediated m6A methylation of C1qA regulates the Rituximab resistance of diffuse large B-cell lymphoma cells. Cell Death Discov. 2023;9:405. doi: 10.1038/s41420-023-01698-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Bueno-Costa A, Piñeyro D, García-Prieto CA, Ortiz-Barahona V, Martinez-Verbo L, Webster NA, et al. Remodeling of the m6A RNA landscape in the conversion of acute lymphoblastic leukemia cells to macrophages. Leukemia. 2022;36:2121–2124. doi: 10.1038/s41375-022-01621-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Huang H, Zhang G, Ruan G-X, Li Y, Chen W, Zou J, et al. Mettl14-Mediated m6A Modification Is Essential for Germinal Center B Cell Response. J Immunol. 2022;208:1924–1936. doi: 10.4049/jimmunol.2101071. [DOI] [PubMed] [Google Scholar]
- 289.Grenov A, Hezroni H, Lasman L, Hanna JH, Shulman Z. YTHDF2 suppresses the plasmablast genetic program and promotes germinal center formation. Cell Rep. 2022;39:110778. doi: 10.1016/j.celrep.2022.110778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Xia T-L, Li X, Wang X, Zhu Y-J, Zhang H, Cheng W, et al. N(6)-methyladenosine-binding protein YTHDF1 suppresses EBV replication and promotes EBV RNA decay. EMBO Rep. 2021;22:e50128. doi: 10.15252/embr.202050128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Xu A, Zhang J, Zuo L, Yan H, Chen L, Zhao F, et al. FTO promotes multiple myeloma progression by posttranscriptional activation of HSF1 in an m6A-YTHDF2-dependent manner. Mol Ther. 2022;30:1104–1118. doi: 10.1016/j.ymthe.2021.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Lundø K, Trauelsen M, Pedersen SF, Schwartz TW. Why Warburg Works: Lactate Controls Immune Evasion through GPR81. Cell Metab. 2020;31:666–668. doi: 10.1016/j.cmet.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 293.Li W, Hao Y, Zhang X, Xu S, Pang D. Targeting RNA N6-methyladenosine modification: a precise weapon in overcoming tumor immune escape. Mol Cancer. 2022;21:176. doi: 10.1186/s12943-022-01652-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol. 2020;20:651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Kong Y, Yu J, Ge S, Fan X. el insight into RNA modifications in tumor immunity: Promising targets to prevent tumor immune escape. Innovation (Camb) 2023;4:100452. doi: 10.1016/j.xinn.2023.100452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Al Zein M, Boukhdoud M, Shammaa H, Mouslem H, El Ayoubi LM, Iratni R, et al. Immunotherapy and immunoevasion of colorectal cancer. Drug Discov Today. 2023;28:103669. doi: 10.1016/j.drudis.2023.103669. [DOI] [PubMed] [Google Scholar]
- 297.Riaz N, Havel JJ, Makarov V, Desrichard A, Urba WJ, Sims JS, et al. Tumor and Microenvironment Evolution during Immunotherapy with Nivolumab. Cell. 2017;171:934–949.e16. doi: 10.1016/j.cell.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Hugo W, Zaretsky JM, Sun L, Song C, Moreno BH, Hu-Lieskovan S, et al. Genomic and Transcriptomic Features of Response to Anti-PD-1 Therapy in Metastatic Melanoma. Cell. 2016;165:35–44. doi: 10.1016/j.cell.2016.02.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Xu C, Fillmore CM, Koyama S, Wu H, Zhao Y, Chen Z, et al. Loss of Lkb1 and Pten leads to lung squamous cell carcinoma with elevated PD-L1 expression. Cancer Cell. 2014;25:590–604. doi: 10.1016/j.ccr.2014.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Xiao W, Adhikari S, Dahal U, Chen Y-S, Hao Y-J, Sun B-F, et al. Nuclear m(6)A Reader YTHDC1 Regulates mRNA Splicing. Mol Cell. 2016;61:507–519. doi: 10.1016/j.molcel.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 301.Liu L, Liang L, Li H, Shao W, Yang C, Lin F, et al. The role of m6A-mediated PD-1/PD-L1 in antitumor immunity. Biochem Pharmacol. 2023;210:115460. doi: 10.1016/j.bcp.2023.115460. [DOI] [PubMed] [Google Scholar]
- 302.Ni Z, Sun P, Zheng J, Wu M, Yang C, Cheng M, et al. JNK Signaling Promotes Bladder Cancer Immune Escape by Regulating METTL3-Mediated m6A Modification of PD-L1 mRNA. Can Res. 2022;82:1789–1802. doi: 10.1158/0008-5472.CAN-21-1323. [DOI] [PubMed] [Google Scholar]
- 303.Guan H, Tian K, Luo W, Li M. m6A-modified circRNA MYO1C participates in the tumor immune surveillance of pancreatic ductal adenocarcinoma through m6A/PD-L1 manner. Cell Death Dis. 2023;14:120. doi: 10.1038/s41419-023-05570-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Xiong J, He J, Zhu J, Pan J, Liao W, Ye H, et al. Lactylation-driven METTL3-mediated RNA m6A modification promotes immunosuppression of tumor-infiltrating myeloid cells. Mol Cell. 2022;82:1660–1677.e10. doi: 10.1016/j.molcel.2022.02.033. [DOI] [PubMed] [Google Scholar]
- 305.Qiao Z, Li Y, Cheng Y, Li S, Liu S. SHMT2 regulates esophageal cancer cell progression and immune Escape by mediating m6A modification of c-myc. Cell Biosci. 2023;13:203. doi: 10.1186/s13578-023-01148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Tang W, Xu N, Zhou J, He Z, Lenahan C, Wang C, et al. ALKBH5 promotes PD-L1-mediated immune escape through m6A modification of ZDHHC3 in glioma. Cell Death Discov. 2022;8:497. doi: 10.1038/s41420-022-01286-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Tsuruta N, Tsuchihashi K, Ohmura H, Yamaguchi K, Ito M, Ariyama H, et al. RNA N6-methyladenosine demethylase FTO regulates PD-L1 expression in colon cancer cells. Biochem Biophys Res Commun. 2020;530:235-39. [DOI] [PubMed]
- 308.Wang Y, Jin P, Wang X. N6-methyladenosine regulator YTHDF1 represses the CD8 + T cell-mediated antitumor immunity and ferroptosis in prostate cancer via m6A/PD-L1 manner. Apoptosis. 2023; [DOI] [PubMed]
- 309.Tao Z, Ruan H, Sun L, Kuang D, Song Y, Wang Q, et al. Targeting the YB-1/PD-L1 Axis to Enhance Chemotherapy and Antitumor Immunity. Cancer Immunol Res. 2019;7:1135–1147. doi: 10.1158/2326-6066.CIR-18-0648. [DOI] [PubMed] [Google Scholar]
- 310.El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Horn L, Mansfield AS, Szczęsna A, Havel L, Krzakowski M, Hochmair MJ, et al. First-Line Atezolizumab plus Chemotherapy in Extensive-Stage Small-Cell Lung Cancer. N Engl J Med. 2018;379:2220–2229. doi: 10.1056/NEJMoa1809064. [DOI] [PubMed] [Google Scholar]
- 312.Zou Y, Zou X, Zheng S, Tang H, Zhang L, Liu P, et al. Efficacy and predictive factors of immune checkpoint inhibitors in metastatic breast cancer: a systematic review and meta-analysis. Ther Adv Med Oncol. 2020;12:1758835920940928. doi: 10.1177/1758835920940928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Cortellini A, Tucci M, Adamo V, Stucci LS, Russo A, Tanda ET, et al. Integrated analysis of concomitant medications and oncological outcomes from PD-1/PD-L1 checkpoint inhibitors in clinical practice. J Immunother Cancer. 2020;8:e001361. doi: 10.1136/jitc-2020-001361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Tong H, Wei H, Smith AO, Huang J. The Role of m6A Epigenetic Modification in the Treatment of Colorectal Cancer Immune Checkpoint Inhibitors. Front Immunol. 2021;12:802049. doi: 10.3389/fimmu.2021.802049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.West H, McCleod M, Hussein M, Morabito A, Rittmeyer A, Conter HJ, et al. Atezolizumab in combination with carboplatin plus nab-paclitaxel chemotherapy compared with chemotherapy alone as first-line treatment for metastatic non-squamous non-small-cell lung cancer (IMpower130): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:924–937. doi: 10.1016/S1470-2045(19)30167-6. [DOI] [PubMed] [Google Scholar]
- 316.Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N Engl J Med. 2018;379:2108–2121. doi: 10.1056/NEJMoa1809615. [DOI] [PubMed] [Google Scholar]
- 317.Fuchs CS, Doi T, Jang RW, Muro K, Satoh T, Machado M, et al. Safety and Efficacy of Pembrolizumab Monotherapy in Patients With Previously Treated Advanced Gastric and Gastroesophageal Junction Cancer: Phase 2 Clinical KEYNOTE-059 Trial. JAMA Oncol. 2018;4:e180013. doi: 10.1001/jamaoncol.2018.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Weng J, Li S, Zhu Z, Liu Q, Zhang R, Yang Y, et al. Exploring immunotherapy in colorectal cancer. J Hematol Oncol. 2022;15:95. doi: 10.1186/s13045-022-01294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Rohaan MW, Borch TH, van den Berg JH, Met Ö, Kessels R, Geukes Foppen MH, et al. Tumor-Infiltrating Lymphocyte Therapy or Ipilimumab in Advanced Melanoma. N Engl J Med. 2022;387:2113–2125. doi: 10.1056/NEJMoa2210233. [DOI] [PubMed] [Google Scholar]
- 320.Powles T, Park SH, Voog E, Caserta C, Valderrama BP, Gurney H, et al. Avelumab Maintenance Therapy for Advanced or Metastatic Urothelial Carcinoma. N Engl J Med. 2020;383:1218–1230. doi: 10.1056/NEJMoa2002788. [DOI] [PubMed] [Google Scholar]
- 321.Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet. 2019;394:1929–1939. doi: 10.1016/S0140-6736(19)32222-6. [DOI] [PubMed] [Google Scholar]
- 322.Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394:1915–1928. doi: 10.1016/S0140-6736(19)32591-7. [DOI] [PubMed] [Google Scholar]
- 323.Boussiotis VA. Molecular and Biochemical Aspects of the PD-1 Checkpoint Pathway. N Engl J Med. 2016;375:1767–1778. doi: 10.1056/NEJMra1514296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Budimir N, Thomas GD, Dolina JS, Salek-Ardakani S. Reversing T-cell Exhaustion in Cancer: Lessons Learned from PD-1/PD-L1 Immune Checkpoint Blockade. Cancer Immunol Res. 2022;10:146–153. doi: 10.1158/2326-6066.CIR-21-0515. [DOI] [PubMed] [Google Scholar]
- 325.Zongyi Y, Xiaowu L. Immunotherapy for hepatocellular carcinoma. Cancer Lett. 2020;470:8–17. doi: 10.1016/j.canlet.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 326.Kirchhammer N, Trefny MP, Auf der Maur P, Läubli H, Zippelius A. Combination cancer immunotherapies: Emerging treatment strategies adapted to the tumor microenvironment. Sci Transl Med. 2022;14:eabo3605. doi: 10.1126/scitranslmed.abo3605. [DOI] [PubMed] [Google Scholar]
- 327.Wu Q, Qian W, Sun X, Jiang S. Small-molecule inhibitors, immune checkpoint inhibitors, and more: FDA-approved novel therapeutic drugs for solid tumors from 1991 to 2021. J Hematol Oncol. 2022;15:143. doi: 10.1186/s13045-022-01362-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Zwergel C, Fioravanti R, Mai A. PD-L1 small-molecule modulators: A new hope in epigenetic-based multidrug cancer therapy? Drug Discov Today. 2023;28:103435. doi: 10.1016/j.drudis.2022.103435. [DOI] [PubMed] [Google Scholar]
- 329.Pan J, Huang T, Deng Z, Zou C. Roles and therapeutic implications of m6A modification in cancer immunotherapy. Front Immunol. 2023;14:1132601. doi: 10.3389/fimmu.2023.1132601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Yankova E, Blackaby W, Albertella M, Rak J, De Braekeleer E, Tsagkogeorga G, et al. Small-molecule inhibition of METTL3 as a strategy against myeloid leukaemia. Nature. 2021;593:597–601. doi: 10.1038/s41586-021-03536-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Yu R, Wei Y, He C, Zhou P, Yang H, Deng C, et al. Integrative Analyses of m6A Regulators Identify that METTL3 is Associated with HPV Status and Immunosuppressive Microenvironment in HPV-related Cancers. Int J Biol Sci. 2022;18:3874–3887. doi: 10.7150/ijbs.70674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Huang Y, Xia W, Dong Z, Yang C-G. Chemical Inhibitors Targeting the Oncogenic m6A Modifying Proteins. Acc Chem Res. 2023;56:3010–3022. doi: 10.1021/acs.accounts.3c00451. [DOI] [PubMed] [Google Scholar]
- 333.Huang Y, Su R, Sheng Y, Dong L, Dong Z, Xu H, et al. Small-Molecule Targeting of Oncogenic FTO Demethylase in Acute Myeloid Leukemia. Cancer Cell. 2019;35:677–691.e10. doi: 10.1016/j.ccell.2019.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Su R, Dong L, Li Y, Gao M, Han L, Wunderlich M, et al. Targeting FTO Suppresses Cancer Stem Cell Maintenance and Immune Evasion. Cancer Cell. 2020;38:79–96.e11. doi: 10.1016/j.ccell.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Kong J, Lu S, Zhang L, Yao Y, Zhang J, Shen Z, et al. m6A methylation regulators as predictors for treatment of advanced urothelial carcinoma with anti-PDL1 agent. Front Immunol. 2022;13:1014861. doi: 10.3389/fimmu.2022.1014861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Liu W, Liu C, Wang H, Xu L, Zhou J, Li S, et al. Targeting N6-methyladenosine RNA modification combined with immune checkpoint Inhibitors: A new approach for cancer therapy. Comput Struct Biotechnol J. 2022;20:5150–5161. doi: 10.1016/j.csbj.2022.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Wang L, Hui H, Agrawal K, Kang Y, Li N, Tang R, et al. m6 A RNA methyltransferases METTL3/14 regulate immune responses to anti-PD-1 therapy. EMBO J. 2020;39:e104514. doi: 10.15252/embj.2020104514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Wang L, Zhu L, Liang C, Huang X, Liu Z, Huo J, et al. Targeting N6-methyladenosine reader YTHDF1 with siRNA boosts antitumor immunity in NASH-HCC by inhibiting EZH2-IL-6 axis. J Hepatol. 2023;79:1185–1200. doi: 10.1016/j.jhep.2023.06.021. [DOI] [PubMed] [Google Scholar]
- 339.Peng Y, Zhang Z, Yang G, Dai Z, Cai X, Liu Z, et al. N6-methyladenosine reader protein IGF2BP1 suppresses CD8 + T cells-mediated tumor cytotoxicity and apoptosis in colon cancer. Apoptosis. 2023; [DOI] [PubMed]
- 340.Guo C, Zhou N, Lu Y, Mu M, Li Z, Zhang X, et al. FGF19/FGFR4 signaling contributes to hepatocellular carcinoma survival and immune escape by regulating IGF2BP1-mediated expression of PD-L1. Biomed Pharmacother. 2024;170:115955. doi: 10.1016/j.biopha.2023.115955. [DOI] [PubMed] [Google Scholar]
- 341.Liu H, Lyu H, Jiang G, Chen D, Ruan S, Liu S, et al. ALKBH5-Mediated m6A Demethylation of GLUT4 mRNA Promotes Glycolysis and Resistance to HER2-Targeted Therapy in Breast Cancer. Cancer Res. 2022;82:3974–3986. doi: 10.1158/0008-5472.CAN-22-0800. [DOI] [PubMed] [Google Scholar]
- 342.Chen Y, Lu Z, Qi C, Yu C, Li Y, Huan W, et al. N6-methyladenosine-modified TRAF1 promotes sunitinib resistance by regulating apoptosis and angiogenesis in a METTL14-dependent manner in renal cell carcinoma. Mol Cancer. 2022;21:111. doi: 10.1186/s12943-022-01549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Wang J, Yu H, Dong W, Zhang C, Hu M, Ma W, et al. N6-Methyladenosine-Mediated Up-Regulation of FZD10 Regulates Liver Cancer Stem Cells’ Properties and Lenvatinib Resistance Through WNT/β-Catenin and Hippo Signaling Pathways. Gastroenterology. 2023;164:990–1005. doi: 10.1053/j.gastro.2023.01.041. [DOI] [PubMed] [Google Scholar]
- 344.Xie G, Wu X-N, Ling Y, Rui Y, Wu D, Zhou J, et al. A novel inhibitor of N6-methyladenosine demethylase FTO induces mRNA methylation and shows anti-cancer activities. Acta Pharmaceutica Sinica B. 2022;12:853–866. doi: 10.1016/j.apsb.2021.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Xu Z, Chen S, Zhang Y, Liu R, Chen M. Roles of m5C RNA Modification Patterns in Biochemical Recurrence and Tumor Microenvironment Characterization of Prostate Adenocarcinoma. Front Immunol. 2022;13:869759. doi: 10.3389/fimmu.2022.869759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Zhou B, Bie F, Zang R, Zhang M, Song P, Liu L, et al. RNA modification writer expression profiles predict clinical outcomes and guide neoadjuvant immunotherapy in non-small cell lung cancer. EBioMedicine. 2022;84:104268. doi: 10.1016/j.ebiom.2022.104268. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.