Abstract
Introduction:
Spontaneous coronary artery dissection (SCAD) is a nonatherosclerotic cause of myocardial infarction. Migraine headache has been reported to be common among patients with SCAD, but the degree of migraine-related disability has not been quantified.
Methods:
Clinical data and headache variables were obtained from the baseline assessment of the prospective, multicenter iSCAD Registry. Migraine-related disability was quantified using the self-reported Migraine Disability Assessment (MIDAS). Demographic, clinical, psychosocial, and medical characteristics from data entry forms were compared between patients with and without migraine.
Results:
Of the 773 patients with available data, 46% reported previous or current migraines. Those with migraines were more likely to be women (96.9% vs 90.3%, p = 0.0003). The presence of underlying carotid fibromuscular dysplasia was associated with migraine (35% vs 27%, p = 0.0175). There was not a significant association with carotid artery dissection and migraine. Current migraine frequency was less than monthly (58%), monthly (24%), weekly (16%), and daily (3%). Triptan use was reported in 32.5% of patients, and 17.5% used daily migraine prophylactic medications. Using the MIDAS to quantify disability related to migraine, 60.2% reported little or no disability, 14.4% mild, 12.7% moderate, and 12.7% severe. The mean MIDAS score was 9.9 (mild to moderate disability). Patients with SCAD had higher rates of depression and anxiety (28.2% vs 17.7% [p = 0.0004] and 35.3% vs 26.7% [p = 0.0099], respectively).
Conclusions:
Migraines are common, frequent, and a source of disability in patients with SCAD. The association between female sex, anxiety, and depression may provide some insight for potential treatment modalities.
Keywords: fibromuscular dysplasia (FMD), migraine headache, myocardial infarction, spontaneous coronary artery dissection (SCAD)
Introduction
Spontaneous coronary artery dissection (SCAD) is a nonatherosclerotic cause of myocardial infarction. 1 Although migraine headaches are more common in women than men, the underlying prevalence of migraine headaches in patients with SCAD exceeds that of the general population and other cohorts of women with ischemia. For example, one SCAD cohort reported a lifetime prevalence of 40% 2 compared with a prevalence of 24% from the WISE (Women’s Ischemia Syndrome Evaluation) cohort. 3 The exact reason for the overrepresentation of migraine headaches in patients with SCAD is unknown but may be related to the underlying arteriopathies noted in this population. Fibromuscular dysplasia (FMD), an associated arteriopathy seen in about 40–80% of patients with SCAD,1,4 is also associated with migraine headaches, although the exact mechanism is unknown. 5 In addition, women with SCAD and migraines are more likely to have associated depression and chest pain. 2
Prior studies evaluating migraines in patients with SCAD have been limited by single-center data and smaller sample sizes. 2 In addition, little is known about the prevalence of conditions associated with migraine among patients with SCAD, including vascular abnormalities, anxiety, and depression. Additionally, the degree of disability due to migraine in patients with SCAD is not well known. This study describes migraine characteristics, associated demographic and clinical features, and quantifies migraine-related disability among patients with SCAD in the prospective, multicenter iSCAD Registry.
Methods
Registry design
The iSCAD Registry 6 is an independent, prospective, multicenter registry funded by the nonprofit patient organization SCAD Alliance. 7 As a patient-initiated, patient-funded registry, study design, case report forms and patient questionnaires were developed by the steering committee of the registry in collaboration with patient representatives from the SCAD Alliance. As the registry was developed, a patient survey was distributed through SCAD Alliance’s social media outlets using the REDCap (Research Electronic Data Capture) platform. 8 Patients were provided with a list of 11 topics identified as top priority questions to be answered by the registry and were asked to choose the five most important topics. Migraine headache was one of the topics selected. Each enrolling site and the coordinating center received local institutional review board approval to conduct this research.
This report of the iSCAD Registry includes data from patients enrolled in the first 18 US sites. Patients presenting with SCAD or with a history of SCAD were enrolled after confirmation of the diagnosis by angiography. Site investigators complete case report forms detailing patient demographics, medical history, and laboratory and imaging data. Patients complete online questionnaires regarding symptoms and medical, family, and psychosocial characteristics. Data are centrally coordinated by the Percutaneous-Pharmacologic Endoluminal Revascularization for Unstable Syndromes Evaluation (PERFUSE) group, which also performs core lab adjudication of coronary angiograms. Study data were collected and managed using REDCap electronic data capture tools hosted at Beth Israel Deaconess Medical Center. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources.8,9
Patients
Patients were eligible for inclusion if they were diagnosed with SCAD by coronary angiography with films available for adjudication, over the age of 18 years, were able to consent to be in the study, and had an electronic mail address to which they were able to receive patient questionnaires. Patients were enrolled during the acute SCAD event while hospitalized or from the outpatient cardiology clinic.
Data collection
Data were updated through case report forms and patient questionnaires up to five times in the first year after SCAD, depending on the date of enrollment in relation to the SCAD event, and yearly thereafter. Patient sex, age, race, past medical history, vascular manifestations, outcomes, depression, anxiety, and migraine headache-related data were collected as baseline data at the time of enrollment. Migraine characteristics were self-reported as a lifetime history of symptoms, including frequency and treatments, at the time of enrollment. Extracoronary vascular abnormalities (EVAs) were defined as FMD, dissection, aneurysm, or pseudoaneurysm detected by noncoronary vascular imaging including computed tomography angiography (CTA), magnetic resonance angiography (MRA), duplex ultrasound, and angiogram. Patient characteristics were compared between patients with and without migraine.
Migraine-related disability was quantified using the Migraine Disability Assessment (MIDAS) at baseline and at 1 year of follow-up. MIDAS is a self-administered questionnaire that has been validated to quantify disability over a 3-month period.10–12 A score of 0–5 indicates little to no disability, 6–10 is mild, 11–20 is moderate, and a score greater than 21 indicates severe disability. Follow-up data are collected, but only follow-up disability data were used for this manuscript.
The presence of depression and anxiety prior to the SCAD event were self-reported as part of the medical history. Severity of depression and anxiety were assessed with the eight-item Patient Health Questionnaire depression scale (PHQ-8 13 ) and seven-item Generalized Anxiety Disorder scale (GAD-7 14 ), respectively. Patients indicated the extent to which they were bothered by symptoms of depression or anxiety in the last 2 weeks on a four-point Likert scale (0 = ‘not at all’ to 3 = ‘nearly every day’), and responses were summed to create total symptom severity scores. These brief measures have been found to be reliable and valid screening measures for depression and anxiety.13,14 Depressive symptom severity was categorized based on PHQ-8 total scores as follows: severe (20–24), moderately severe (15–19), moderate (10–14), mild (5–9), and none or minimal (0–4). Similarly, the severity of anxiety symptoms was categorized based on GAD-7 total scores: severe (15–21), moderate (10–14), mild (5–9), and none or minimal (0–4).
Statistical analysis
Demographic data, presenting signs and symptoms, underlying medical conditions, and psychosocial characteristics were expressed as means with SD for continuous variables and raw frequencies with percentages for categorical variables. Clinical variables were reported for patients with and without migraine headache. Differences between groups were determined using the chi-squared test with a p-value less than 0.05 considered significant. Migraine headache frequency was also reported. Migraine disability was reported using the MIDAS score. A nominal two-sided p-value threshold of 0.05 was used to determine statistical significance. The analyses were performed independently by the PERFUSE Study Group using SAS software version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
Patient characteristics
From March 2019 to February 2023, there were 773 patients enrolled in the iSCAD Registry with complete migraine data (Table 1). Of note, 29 (3.8%) of the patients included in this manuscript also participated in the Mayo registry that reported migraine headaches in SCAD patients. 2 The average age was 49 years, and the patient population was 86% White. Of these, 46% reported migraines (n = 354). Patients with migraines were more likely to be women (96.9% vs 90.2%, p = 0.0003) and younger at the time of the SCAD event (48.3 years vs 50.3 years, p = 0.0152) than patients without migraines. There was no difference in prevalence of chest pain at the time of the SCAD event among patients with migraines compared with those without migraines. Of the patients with migraines, 28% had hypertension, 16.7% had hyperlipidemia, and 24% had a history of smoking. Most had a history of oral contraceptive use (79.9%), and 14.1% reported a history of hormone therapy, although variables such as oral contraceptive use and hormone replacement therapy were not associated with migraines. There was a slight decrease in migraines in postmenopausal patients with SCAD (45.8% vs 48%, p ⩽ 0.0001). There was a low prevalence of connective tissue disease (2%) and systemic inflammatory disease (7.1%) in patients with migraines. There was no significant difference in these clinical variables between SCAD patients with and without migraines.
Table 1.
Baseline characteristics.
| Total (N = 773) |
History of migraine | |||
|---|---|---|---|---|
| Yes (n = 354) |
No (n = 419) |
p-value | ||
| Age, y | 0.015 a | |||
| Mean (SD) | 49.4 (11.0) | 48.3 (10.9) | 50.3 (11.0) | |
| Median (IQR) | 49.0 (41.6, 56.9) | 48.4 (40.3, 55.0) | 49.8 (43.0, 58.0) | |
| Sex, n (%) | < 0.001 b | |||
| Male | 51 (6.6) | 10 (2.8) | 41 (9.8) | |
| Female | 721 (93.3) | 343 (96.9) | 378 (90.2) | |
| Unknown | 1 (0.1) | 1 (0.3) | 0 (0.0) | |
| Race, n (%) | 0.599 b | |||
| American Indian/Alaska Native | 2 (0.3) | 0 (0.0) | 2 (0.5) | |
| Asian | 13 (1.7) | 6 (1.7) | 7 (1.7) | |
| Black/African American | 56 (7.2) | 25 (7.1) | 31 (7.4) | |
| Native Hawaiian/Pacific Islander | 1 (0.1) | 0 (0.0) | 1 (0.2) | |
| White | 662 (85.6) | 300 (84.7) | 362 (86.4) | |
| Multiracial | 8 (1.0) | 5 (1.4) | 3 (0.7) | |
| Other | 3 (0.4) | 2 (0.6) | 1 (0.2) | |
| Unknown | 28 (3.6) | 16 (4.5) | 12 (2.9) | |
| Ethnicity, n (%) | 0.389 b | |||
| Hispanic/Latino | 36 (4.7) | 19 (5.4) | 17 (4.1) | |
| Non-Hispanic/Latino | 737 (95.3) | 335 (94.6) | 402 (95.9) | |
| Symptoms of index SCAD, n (%) | ||||
| Chest pain | 692 (89.5) | 317 (89.5) | 375 (89.5) | 0.982 b |
| Arm/shoulder pain | 423 (54.7) | 197 (55.6) | 226 (53.9) | 0.634 b |
| Shortness of breath | 290 (37.5) | 145 (41.0) | 145 (34.6) | 0.069 b |
| Palpitations | 125 (16.2) | 59 (16.7) | 66 (15.8) | 0.731 b |
| Jaw pain | 195 (25.2) | 104 (29.4) | 91 (21.7) | 0.015 b |
| Cardiac arrest | 39 (5.0) | 18 (5.1) | 21 (5.0) | 0.963 b |
| Medical history, n (%) | ||||
| Diabetes | 15 (1.9) | 7 (2.0) | 8 (1.9) | 0.945 b |
| High cholesterol | 123 (15.9) | 59 (16.7) | 64 (15.3) | 0.598 b |
| Hypertension | 205 (26.5) | 99 (28.0) | 106 (25.3) | 0.403 b |
| Ischemic stroke | 7 (0.9) | 3 (0.8) | 4 (1.0) | 0.875 b |
| Hemorrhagic stroke | 5 (0.6) | 3 (0.8) | 2 (0.5) | 0.522 b |
| Transient ischemic attack | 6 (0.8) | 6 (1.7) | 0 (0.0) | 0.007 b |
| Known aneurysm c | 42 (5.4) | 23 (6.5) | 19 (4.5) | 0.230 b |
| Known dissection c | 112 (14.5) | 60 (16.9) | 52 (12.4) | 0.074 b |
| Smoking, n (%) | 0.056 b | |||
| Active or former smoker | 197 (25.5) | 84 (23.7) | 113 (27.0) | |
| Never smoker | 567 (73.4) | 269 (76.0) | 298 (71.1) | |
| Prefer not to say | 9 (1.2) | 1 (0.3) | 8 (1.9) | |
| Alcohol, n (%) | 0.141 b | |||
| Never drinker | 185 (23.9) | 92 (26.0) | 93 (22.2) | |
| Less than one drink per week | 327 (42.3) | 157 (44.4) | 170 (40.6) | |
| More than one drink per week | 251 (32.5) | 100 (28.2) | 151 (36.0) | |
| Prefer not to say | 10 (1.3) | 5 (1.4) | 5 (1.2) | |
| Menstrual cycle, n (%) | < 0.001 b | |||
| Premenopausal | 238 (30.8) | 112 (31.6) | 126 (30.1) | |
| Perimenopausal | 78 (10.1) | 39 (11.0) | 39 (9.3) | |
| Postmenopausal | 363 (47.0) | 162 (45.8) | 201 (48.0) | |
| Unsure | 42 (5.4) | 30 (8.5) | 12 (2.9) | |
| Not applicable | 52 (6.7) | 11 (3.1) | 41 (9.8) | |
| Hormone replacement therapy, n (%) | 0.372 b | |||
| Yes | 100 (12.9) | 50 (14.1) | 50 (11.9) | |
| No | 263 (34.0) | 112 (31.6) | 151 (36.0) | |
| Not applicable | 410 (53.0) | 192 (54.2) | 218 (52.0) | |
| Age of menopause | 0.775 a | |||
| Mean (SD) | 48.7 (6.6) | 48.4 (7.6) | 49.0 (5.7) | |
| Median (IQR) | 50.0 (46.0, 53.0) | 50.0 (46.0, 53.0) | 50.0 (46.0, 53.0) | |
| Oral contraceptive pills, n (%) | 0.266 b | |||
| Yes | 600 (77.6) | 283 (79.9) | 317 (75.7) | |
| No | 34 (4.4) | 16 (4.5) | 18 (4.3) | |
| Not applicable | 139 (18.0) | 55 (15.5) | 84 (20.0) | |
| Inherited connective tissue disorder, n (%) | 0.193 b | |||
| Yes | 10 (1.3) | 7 (2.0) | 3 (0.7) | |
| No | 516 (66.8) | 227 (64.1) | 289 (69.0) | |
| Not assessed | 243 (31.4) | 119 (33.6) | 124 (29.6) | |
| Missing | 4 (0.5) | 1 (0.3) | 3 (0.7) | |
| Systemic inflammatory disorder, n (%) | 0.449 b | |||
| Yes | 48 (6.2) | 25 (7.1) | 23 (5.5) | |
| No | 592 (76.6) | 262 (74.0) | 330 (78.8) | |
| Not assessed | 128 (16.6) | 64 (18.1) | 64 (15.3) | |
| Missing | 5 (0.6) | 3 (0.8) | 2 (0.5) | |
| PCI performed during hospitalization, n (%) | 0.381 b | |||
| Yes | 181 (23.4) | 81 (22.9) | 100 (23.9) | |
| No | 578 (74.8) | 267 (75.4) | 311 (74.2) | |
| Not assessed | 6 (0.8) | 1 (0.3) | 5 (1.2) | |
| Missing | 8 (1.0) | 5 (1.4) | 3 (0.7) | |
| CABG performed during hospitalization, n (%) | 0.275 b | |||
| Yes | 28 (3.6) | 12 (3.4) | 16 (3.8) | |
| No | 733 (94.8) | 335 (94.6) | 398 (95.0) | |
| Not assessed | 6 (0.8) | 2 (0.6) | 4 (1.0) | |
| Missing | 6 (0.8) | 5 (1.4) | 1 (0.2) | |
| Medical therapy only during hospitalization, n (%) | 0.853 b | |||
| Yes | 559 (72.3) | 256 (72.3) | 303 (72.3) | |
| No | 198 (25.6) | 91 (25.7) | 107 (25.5) | |
| Not assessed | 4 (0.5) | 1 (0.3) | 3 (0.7) | |
| Missing | 12 (1.6) | 6 (1.7) | 6 (1.4) | |
| Received beta-blockers during hospitalization, n (%) | 591 (76.5) | 274 (77.4) | 317 (75.7) | 0.569 b |
| Received beta-blockers at discharge, n (%) | 648 (83.8) | 300 (84.7) | 348 (83.1) | 0.525 b |
| Received beta-blockers at day 360, n (%) | 243/298 (81.5) | 116/140 (82.9) | 127/158 (80.4) | 0.582 b |
| In-hospital cerebrovascular accident, n (%) | 0.186 b | |||
| Yes | 4 (0.5) | 4 (1.1) | 0 (0.0) | |
| No | 725 (93.8) | 330 (93.2) | 395 (94.3) | |
| Not assessed | 14 (1.8) | 6 (1.7) | 8 (1.9) | |
| Missing | 30 (3.9) | 14 (4.0) | 16 (3.8) | |
| Taking NSAID regularly, n (%) | < 0.001 b | |||
| Yes | 228 (29.5) | 130 (36.7) | 98 (23.4) | |
| No | 436 (56.4) | 177 (50.0) | 259 (61.8) | |
| Not sure | 109 (14.1) | 47 (13.3) | 62 (14.8) | |
Kruskal–Wallis p-value; bchi-squared p-value; cprior to the index SCAD.
CABG, coronary artery bypass graft; NSAID, nonsteroidal antiinflammatory drug; PCI, percutaneous coronary intervention; SCAD, spontaneous coronary artery dissection.
EVAs were common (51.7%), and 43% had a diagnosis of FMD. EVAs overall were not associated with migraines in patients with SCAD; however, the presence of FMD in any vascular bed was more common in patients with migraine (47.9% vs 38.8%, p = 0.0214). Not all patients underwent brain-to-pelvis imaging to evaluate for FMD (Table 2). Patients with migraine were more likely to have experienced a transient ischemic attack (1.7% vs 0%, p = 0.0075). Patients with migraine were also more likely to have internal carotid artery FMD (33.8% vs 23.8%, p = 0.013). Cervical internal carotid artery dissection was not associated with the presence of migraines.
Table 2.
Extracoronary vascular abnormalities based on imaging after spontaneous coronary artery dissection (SCAD).
| Total (N = 773) |
History of migraine | p-value | ||
|---|---|---|---|---|
| Yes (n = 354) |
No (n = 419) |
|||
| Extracoronary vascular abnormalities, n (%) | 326/630 (51.7) | 160/290 (55.2) | 166/340 (48.8) | 0.112 a |
| Fibromuscular dysplasia, n (%) | 271/630 (43.0) | 139/290 (47.9) | 132/340 (38.8) | 0.021 a |
| Dissection, n (%) | 69/630 (11.0) | 35/290 (12.1) | 34/340 (10.0) | 0.407 a |
| Aneurysm, n (%) | 103/630 (16.3) | 36/290 (12.4) | 67/340 (19.7) | 0.014 a |
| Pseudoaneurysm, n (%) | 26/630 (4.1) | 12/290 (4.1) | 14/340 (4.1) | 0.990 a |
| Cervical internal carotid artery: Extracoronary vascular abnormalities, n (%) | 162/512 (31.6) | 84/231 (36.4) | 78/281 (27.8) | 0.037 a |
| Cervical internal carotid artery: Fibromuscular dysplasia, n (%) | 145/512 (28.3) | 78/231 (33.8) | 67/281 (23.8) | 0.013 a |
| Cervical internal carotid artery: Dissection, n (%) | 20/512 (3.9) | 8/231 (3.5) | 12/281 (4.3) | 0.639 a |
| Cervical internal carotid artery: Aneurysm, n (%) | 13/512 (2.5) | 7/231 (3.0) | 6/281 (2.1) | 0.522 a |
| Cervical internal carotid artery: Pseudoaneurysm, n (%) | 11/512 (2.1) | 5/231 (2.2) | 6/281 (2.1) | 0.982 a |
| Vertebral artery: Extracoronary vascular abnormalities, n (%) | 90/477 (18.9) | 47/218 (21.6) | 43/259 (16.6) | 0.168 a |
| Vertebral artery: Fibromuscular dysplasia, n (%) | 69/477 (14.5) | 36/218 (16.5) | 33/259 (12.7) | 0.243 a |
| Vertebral artery: Dissection, n (%) | 24/477 (5.0) | 11/218 (5.0) | 13/259 (5.0) | 0.989 a |
| Vertebral artery: Aneurysm, n (%) | 3/477 (0.6) | 0/218 (0.0) | 3/259 (1.2) | 0.111 a |
| Vertebral artery: Pseudoaneurysm, n (%) | 11/477 (2.3) | 5/218 (2.3) | 6/259 (2.3) | 0.987 a |
| Intracranial artery: Extracoronary vascular abnormalities, n (%) | 22/472 (4.7) | 8/221 (3.6) | 14/251 (5.6) | 0.314 a |
| Intracranial artery: Fibromuscular dysplasia, n (%) | 6/472 (1.3) | 5/221 (2.3) | 1/251 (0.4) | 0.071 a |
| Intracranial artery: Aneurysm, n (%) | 17/472 (3.6) | 4/221 (1.8) | 13/251 (5.2) | 0.050 a |
Not all patients underwent brain-to-pelvis imaging. The number of patients who had imaging of each vascular bed is as follows: cervical internal carotid (n = 512), vertebral artery (n = 477), intracranial artery (n = 472), thoracic aorta (n = 313), abdominal aorta (n = 486), renal (n = 533), mesenteric (n = 479), common iliac (n = 650), external iliac (n = 454).
Chi-squared p-value.
Patients with SCAD plus migraines were more likely to have higher rates of elevated symptoms of self-reported depression and anxiety (28.2% vs 17.7% [p = 0.0004] and 35.3% vs 26.7% [p = 0.0099], respectively) (Table 3). Patients with migraine were more likely to be taking medications for depression (18.4% vs 12.4%, p = 0.0016) and anxiety (12.4% vs 8.1%, p = 0.0266). The mean PHQ-8 score was higher in patients with migraines (5.4 vs 4.0, p ⩽ 0.001). Patients with migraine were more likely to have mild, moderate, and moderately severe depression when compared with patients without migraine. The mean GAD-7 anxiety score was 4.9 for patients with migraine and 3.5 for patients without migraine (p < 0.001). Patients with migraine were more likely to have severe, moderate, and mild anxiety when compared with patients without migraine.
Table 3.
Psychosocial characteristics.
| Total (N = 773) |
History of migraine | p-value | ||
|---|---|---|---|---|
| Yes (n = 354) |
No (n = 419) |
|||
| Depression, n (%) | 174 (22.5) | 100 (28.2) | 74 (17.7) | < 0.001 a |
| Taking medication for depression, n (%) | 0.002 a | |||
| Yes | 117 (15.1) | 65 (18.4) | 52 (12.4) | |
| No | 57 (7.4) | 35 (9.9) | 22 (5.3) | |
| Not applicable | 599 (77.5) | 254 (71.8) | 345 (82.3) | |
| Anxiety, n (%) | 237 (30.7) | 125 (35.3) | 112 (26.7) | 0.010 a |
| Taking medication for anxiety, n (%) | 0.027 a | |||
| Yes | 78 (10.1) | 44 (12.4) | 34 (8.1) | |
| No | 36 (4.7) | 22 (6.2) | 14 (3.3) | |
| Not applicable | 536 (69.3) | 229 (64.7) | 307 (73.3) | |
| Unknown | 123 (15.9) | 59 (16.7) | 64 (15.3) | |
| PHQ-8 score | < 0.001b | |||
| Mean (SD) | 4.6 (4.7) | 5.4 (4.8) | 4.0 (4.6) | |
| Median (IQR) | 3.0 (1.0, 7.0) | 4.0 (2.0, 8.0) | 2.0 (1.0, 6.0) | |
| Depression severity by PHQ-8 score, n (%) | < 0.001 a | |||
| Severe (20–24) | 8 (1.0) | 1 (0.3) | 7 (1.7) | |
| Moderately severe (15–19) | 30 (3.9) | 17 (4.8) | 13 (3.1) | |
| Moderate (10–14) | 74 (9.6) | 49 (13.8) | 25 (6.0) | |
| Mild (5–9) | 191 (24.7) | 98 (27.7) | 93 (22.2) | |
| None or minimal (0–4) | 470 (60.8) | 189 (53.4) | 281 (67.1) | |
| GAD-7 score | < 0.001 b | |||
| Mean (SD) | 4.1 (4.8) | 4.9 (5.1) | 3.5 (4.5) | |
| Median (IQR) | 3.0 (0.0, 6.0) | 3.5 (0.0, 7.0) | 2.0 (0.0, 5.0) | |
| Anxiety severity by GAD-7 score, n (%) | 0.002 a | |||
| Severe (15–21) | 43 (5.6) | 26 (7.3) | 17 (4.1) | |
| Moderate (10–14) | 55 (7.1) | 35 (9.9) | 20 (4.8) | |
| Mild (5–9) | 185 (23.9) | 90 (25.4) | 95 (22.7) | |
| None or minimal (0–4) | 490 (63.4) | 203 (57.3) | 287 (68.5) | |
| MIDAS score | 0.431b | |||
| Mean (SD) | 9.8 (22.3) | 9.9 (22.4) | 2.5 (4.4) | |
| Median (IQR) | 2.5 (0.0, 11.0) | 3.0 (0.0, 11.0) | 0.5 (0.0, 5.0) | |
| MIDAS grade, n (%) | < 0.001 a | |||
| Little or no disability | 216 (27.9) | 213 (60.2) | 3 (0.7) | |
| Mild disability | 52 (6.7) | 51 (14.4) | 1 (0.2) | |
| Moderate disability | 45 (5.8) | 45 (12.7) | 0 (0.0) | |
| Severe disability | 45 (5.8) | 45 (12.7) | 0 (0.0) | |
| Missing | 415 (53.7) | 0 (0.0) | 415 (99.0) | |
| MIDAS score at 1 year | 0.322 b | |||
| Mean (SD) | 9.8 (22.1) | 9.7 (22.1) | 10.6 (22.4) | |
| Median (IQR) | 3.0 (0.0, 11.0) | 3.0 (0.0, 11.0) | 0.0 (0.0, 15.0) | |
| MIDAS grade at 1 year, n (%) | < 0.001 a | |||
| Little or no disability | 117 (15.1) | 103 (29.1) | 14 (3.3) | |
| Mild disability | 24 (3.1) | 23 (6.5) | 1 (0.2) | |
| Moderate disability | 28 (3.6) | 26 (7.3) | 2 (0.5) | |
| Severe disability | 24 (3.1) | 20 (5.6) | 4 (1.0) | |
| Missing | 580 (75.0) | 182 (51.4) | 398 (95.0) | |
Chi-squared p-value; bKruskal–Wallis p-value.
GAD-7, seven-item Generalized Anxiety Disorder scale; MIDAS, Migraine Disability Assessment; PHQ-8, eight-item Patient Health Questionnaire depression scale; SCAD, spontaneous coronary artery dissection.
Migraine frequency and severity
Among those reporting migraine, migraine frequency was less than monthly (58%), monthly (24%), weekly (15%), and daily (3%) (Figure 1). A total of 32.5% of patients reported triptan use and 17.5% used daily prophylactic medications for migraines. The percentage of patients who had never received treatment (or were unsure) for migraines was high at 53% (Figure 2). Beta-blocker use was not different at the time of discharge from the hospital (84.7% vs 83.1%, p = 0.52) and at 1-year follow-up (82.9% vs 80.4%, p = 0.58).
Figure 1.
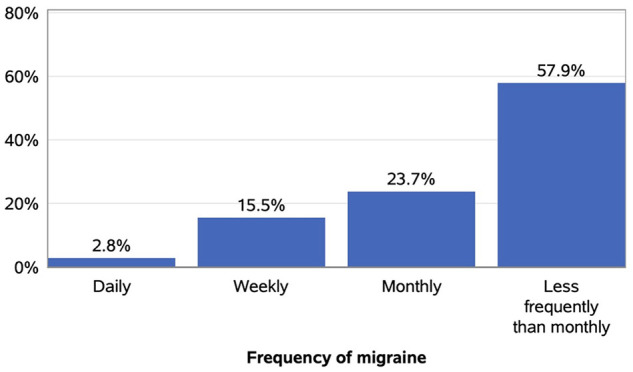
Distribution of migraine frequency among patients reporting migraines (n = 354).
Figure 2.
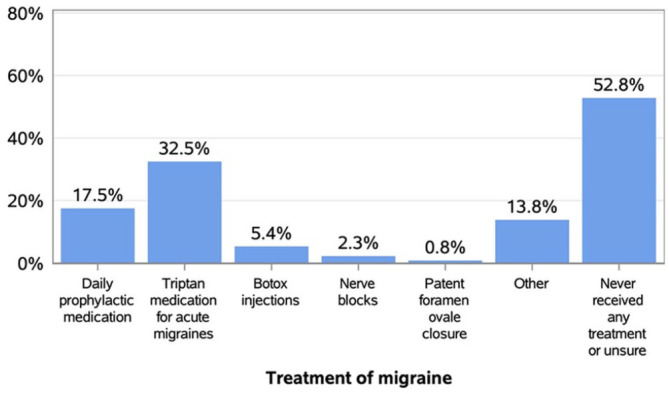
Distribution of migraine treatment among patients reporting migraines (n = 354).
Disability
Using the MIDAS to quantify disability related to migraine, 60.2% reported little or no disability, 14.4% mild, 12.7% moderate, and 12.7% severe (n = 354 patients). The mean MIDAS score was 9.9 (mild to moderate disability). The severity of disability at 1 year after follow-up was overall unchanged (Figure 3).
Figure 3.
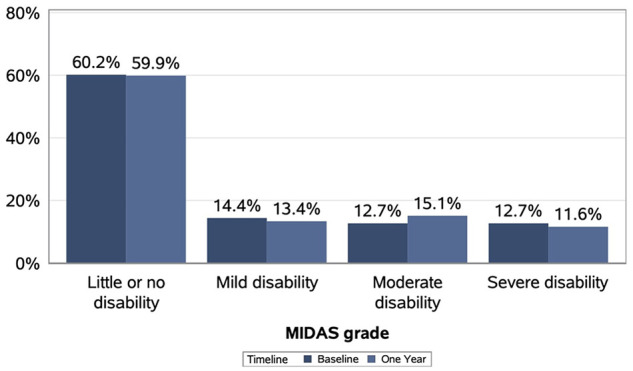
Distribution of Migraine Disability Assessment (MIDAS) grade in patients reporting migraines at baseline (n = 354) and 1 year (n = 172).
Discussion
In patients with a history of SCAD, migraine headaches are common 2 and have been reported in 37–46% of patients with SCAD compared with a 24% lifetime prevalence in American women with stable angina from the WISE cohort. 3 The iSCAD Registry data are similar, with 45% of patients with SCAD reporting migraines. In our study, over 50% of patients with migraine reported not receiving treatment or were unsure of having received treatment and 17% had been treated with prophylactic medication. This finding is common in the general population, where only 40% of patients with migraine have seen a provider for their symptoms. Of those, 44% received a correct diagnosis of migraine and 24% of those received appropriate treatment. 15
Migraines are associated with increased risk for cardiovascular events and are increased in patients with other vascular abnormalities.3,16 The relationship with migraines and vascular disorders is not well understood, but there are likely genetic, hormonal, vascular, and environmental factors that contribute to this predisposition. Our study did not show a significant difference in migraines in patients with SCAD taking exogenous hormone therapy. However, it did show a decrease in migraines in the postmenopausal period. The decrease in migraines postmenopause has been described in population-based studies. 17 Women in the general population are more likely to experience migraines, 18 and the SCAD patient population is predominantly women. Genetic risk factors for SCAD and other arteriopathies have been identified. These gene variants further support the relationship between arterial disease and migraine headaches. The PHACTR1 gene variant has been associated with FMD, cervical artery dissections, SCAD, and migraines. 19 Another variant in the LRP1 gene established a locus for migraine and SCAD. 20 Further, a genome-wide meta-analysis showed multiple loci to be associated with SCAD and neurovascular disease, including migraine. 21
The prevalence of migraine headaches in this SCAD cohort was not associated with traditional cardiovascular risk factors such as hypertension, hyperlipidemia, and diabetes. In addition, hormonal variables such as oral contraceptive use, hormone therapy, and menopause status were not associated with migraines. Given the clear predominance of women with SCAD, it is thought that hormones play a role in migraines. However, this has not been directly studied. In a prior study, patients with migraine experienced SCAD at a slightly younger age. 2 This was also shown in our study. It has also been shown that SCAD patients with migraines have a higher prevalence of EVAs. 2 Similarly, FMD patients with migraines experienced more carotid aneurysms and dissections. 5 In this study, EVAs were not associated with migraines in SCAD patients, with the exception of FMD and internal carotid artery FMD. The reason for these differences is not clear and deserves further investigation.
In the iSCAD Registry, 18.3% of patients with SCAD experienced at least weekly migraines. Prophylactic medication was used approximately 17.5% of the time, but most patients (53%) never received treatment. With the reported disability in this patient population due to headache, more attention to abortive and prophylactic therapy for migraines should be emphasized to improve quality of life in this patient population. One concern is that triptan use was common, reported in 32.5% of patients. Triptans are contraindicated in this patient population due to the side effect of vasoconstriction. Newer agents, such as calcitonin gene-related peptide (CGRP) inhibitors appear to be safe in patients with vascular conditions. 22 There should be an emphasis on increased use of prophylactic medications to reduce the frequency and severity of migraines in SCAD patients. Also, beta-blockers may reduce the recurrence of SCAD events 23 but also are utilized as migraine prophylaxis. 24 Thus, beta-blockers may be particularly useful in patients with SCAD for their potential to treat angina, reduce SCAD recurrence, and prevent migraine headaches.
In our study, patients with SCAD plus migraines were more likely to report elevated symptoms of anxiety and depression in the past 2 weeks compared to patients without migraines. The median time from the SCAD event to the patient questionnaire completion was 326 days. This parallels previous research demonstrating evidence for comorbidity of migraine with depression and anxiety in the general population.25,26 Furthermore, it has been shown that intense emotional stress can be a precipitating factor for SCAD, 1 and high levels of emotional stress have been reported by patients with SCAD. 27 Patients with SCAD and migraines are more likely to have a history of depression. 2 Similarly, patients with FMD with a history of depression were more likely to have frequent migraines. 5 More research is needed to determine the temporal relationship between depression and anxiety with SCAD.
The iSCAD Registry study is the first to report disability due to migraine in patients with SCAD. Although it is reassuring that 60% of patients reported little to no disability, 25.4% of patients reported moderate or severe disability and 40% reported significant disability. The average MIDAS score was 10, indicating overall mild to moderate disability among all patients with SCAD and migraines. Migraines are a common symptom among patients with SCAD and other arteriopathies.2,5 Providers should be aware of the commonly used treatment modalities for migraine headaches and adopt a multidisciplinary approach to the patient with SCAD who may benefit from specialist referral to headache neurology.
Study limitations
There are several limitations that should be noted. First, the iSCAD Registry is an observational study and, as such, the reported relationships between migraine headaches and clinical findings are associations and do not suggest causality. The registry data are a ‘real-life’ representation of patient care at many SCAD centers across the United States and also reflect symptoms and measures derived directly from patient questionnaires and are subject to recall and reporting bias. The descriptive nature of this study lacks a true comparator group. Migraine headache symptoms were self-reported by patients rather than by physicians and medical records. It is possible that patients with anxiety and depression may over-report migraine symptoms, but this cannot be confirmed. The registry also does not capture clinician diagnoses of or treatment for depression or anxiety. Unfortunately, important clinical variables in migraine headache research, including the presence of aura, were not captured in this version of the iSCAD Registry. The presence of extracoronary abnormalities was evaluated in approximately two-thirds of these patients. This reflects the ‘real world’ nature of the data collected and likely represents some practical limitation of obtaining complete brain-to-pelvis imaging after a SCAD event in these patients. Additionally, use of newer treatments for migraine headache, including CGRP inhibitors, 22 were also not collected.
Conclusions
Migraines are common, frequent, and a source of disability in patients with SCAD. The association between female sex, anxiety, and depression may provide some insight for potential treatment modalities.
Supplemental Material
Supplemental material, sj-pdf-1-vmj-10.1177_1358863X241252444 for Migraine headache in patients with spontaneous coronary artery dissection: A report of the iSCAD Registry by Bryan J Wells, Malissa J Wood, Anne E O’Duffy, Jennifer A Sumner, Gerald Chi, Anna Grodzinsky, Heather L Gornik, Daniella Kadian-Dodov, Angela Taylor, Connie N Hess, Monika Sanghavi, Stanislav Henkin, Gretchen Wells, Lori Tam, James Orford, Kathryn Lindley, Dharam J Kumbhani, Clara Vitarello, Fahad Alkhalfan, C Michael Gibson, Katherine K Leon, Sahar Naderi and Esther SH Kim in Vascular Medicine
Acknowledgments
The iSCAD Registry was developed in partnership with patients with SCAD who recognized the need for a collaborative research model accessible to patients and investigators nationwide. Patients simultaneously raised funds to support the registry, answered surveys to develop the study questions, have selflessly shared their medical and personal information as active enrolled participants in the registry, and have reviewed the content of this manuscript. The authors would like to acknowledge these patients, without whose generosity this work would not have been possible. Please see the Patient Perspective for this manuscript in the online supplemental material.
Footnotes
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Malissa Wood is a member of the Scientific Advisory Board of SCAD Alliance; she has no relationships with industry. Dr Gerald Chi receives unrelated research grant support paid to the Beth Israel Deaconess Medical Center, Harvard Medical School from Portola Pharmaceuticals, Bayer, Janssen Scientific Affairs, and CSL Behring. Dr Daniella Kadian-Dodov receives unrelated research support from Philips Healthcare; she is a consultant for Boston Scientific; and receives honoraria for participation in educational conferences from Abbott Laboratories and Boston Scientific. Katherine Leon is co-founder and Board Chair of SCAD Alliance; she has no relationships with industry. Dr Sahar Naderi is a member of the Scientific Advisory Board of SCAD Alliance; she has no relationships with industry. Dr Esther Kim is the Chair of the Scientific Advisory Board of SCAD Alliance; she has no relationships with industry. All remaining authors have no disclosures.
Funding: This work was funded by the SCAD Alliance, which is a 501(3)c nonprofit organization. Malissa Wood, Katherine Leon, Sahar Naderi, and Esther Kim serve on the SCAD Alliance Scientific Advisory Board (unpaid roles) and were involved with the study design and manuscript preparation.
ORCID iDs: Bryan J Wells  https://orcid.org/0000-0001-9994-7947
https://orcid.org/0000-0001-9994-7947
Gerald Chi  https://orcid.org/0000-0002-8371-1689
https://orcid.org/0000-0002-8371-1689
Heather L Gornik  https://orcid.org/0000-0002-5849-4010
https://orcid.org/0000-0002-5849-4010
Daniella Kadian-Dodov  https://orcid.org/0000-0002-6748-7728
https://orcid.org/0000-0002-6748-7728
Stanislav Henkin  https://orcid.org/0000-0001-5968-1216
https://orcid.org/0000-0001-5968-1216
Fahad Alkhalfan  https://orcid.org/0000-0002-6268-5629
https://orcid.org/0000-0002-6268-5629
Supplementary material: The supplementary material is available online with the article.
References
- 1. Hayes SN, Kim CESH, Saw J, et al. Spontaneous coronary artery dissection: Current state of the science: A scientific statement from the American Heart Association. Circulation 2018; 137: e523–e557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kok SN, Hayes SN, Cutrer FM, et al. Prevalence and clinical factors of migraine in patients with spontaneous coronary artery dissection. J Am Heart Assoc 2018; 7: e010140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ahmed B, Bairey Merz CN, McClure C, et al. Migraines, angiographic coronary artery disease and cardiovascular outcomes in women. Am J Med 2006; 119: 670–675. [DOI] [PubMed] [Google Scholar]
- 4. Saw J, Ricci D, Starovoytov A, et al. Spontaneous coronary artery dissection: Prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc Interv 2013; 6: 44–52. [DOI] [PubMed] [Google Scholar]
- 5. Wells BJ, Modi RD, Gu X, et al. Clinical associations of headaches among patients with fibromuscular dysplasia: A Report from the US Registry for Fibromuscular Dysplasia. Vasc Med 2020; 25: 348–350. [DOI] [PubMed] [Google Scholar]
- 6. Kim E. International Spontaneous Coronary Artery Dissection (SCAD) “iSCAD” Registry, https://clinicaltrials.gov/study/NCT04496687 (2023, accessed 7 October 2023).
- 7. SCAD Alliance website. https://scadalliance.org (accessed 7 October 2023).
- 8. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019; 95: 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stewart WF, Lipton R, Kolodner K, et al. Reliability of the migraine disability assessment score in a population-based sample of headache sufferers. Cephalalgia 1999; 19: 107–114. [DOI] [PubMed] [Google Scholar]
- 11. Stewart WF, Lipton RB, Kolodner KB, et al. Validity of the Migraine Disability Assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain 2000; 88: 41–52. [DOI] [PubMed] [Google Scholar]
- 12. Stewart WF, Lipton RB, Whyte J, et al. An international study to assess reliability of the Migraine Disability Assessment (MIDAS) score. Neurology 1999; 53: 988–994. [DOI] [PubMed] [Google Scholar]
- 13. Kroenke K, Strine TW, Spitzer RL, et al. The PHQ-8 as a measure of current depression in the general population. J Affect Disord 2009; 114: 163–173. [DOI] [PubMed] [Google Scholar]
- 14. Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 15. Dodick DW, Loder EW, Manack Adams A, et al. Assessing barriers to chronic migraine consultation, diagnosis, and treatment: Results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache 2016; 56: 821–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014; 7: 645–655. [DOI] [PubMed] [Google Scholar]
- 17. Neri I, Granella F, Nappi R, et al. Characteristics of headache at menopause: A clinico-epidemiologic study. Maturitas 1993; 17: 31–37. [DOI] [PubMed] [Google Scholar]
- 18. Stewart WF, Linet MS, Celentano DD, et al. Age- and sex-specific incidence rates of migraine with and without visual aura. Am J Epidemiol 1991; 134: 1111–1120. [DOI] [PubMed] [Google Scholar]
- 19. Turley TN, O’Byrne MM, Kosel ML, et al. Identification of susceptibility loci for spontaneous coronary artery dissection. JAMA Cardiol 2020; 5: 929–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Amrani-Midoun A, Adlam D, Bouatia-Naji N. Recent advances on the genetics of spontaneous coronary artery dissection. Circ Genom Precis Med 2021; 14: e003393. [DOI] [PubMed] [Google Scholar]
- 21. Adlam D, Berrandou T-E, Georges A, et al. Genome-wide association meta-analysis of spontaneous coronary artery dissection identifies risk variants and genes related to artery integrity and tissue-mediated coagulation. Nat Genet 2023; 55: 964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Favoni V, Giani L, Al-Hassany L, et al. CGRP and migraine from a cardiovascular point of view: What do we expect from blocking CGRP? J Headache Pain 2019; 20: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Saw J, Humphries K, Aymong E, et al. Spontaneous coronary artery dissection: Clinical outcomes and risk of recurrence. J Am Coll Cardiol 2017; 70: 1148–1158. [DOI] [PubMed] [Google Scholar]
- 24. Linde K, Rossnagel K. WITHDRAWN: Propranolol for migraine prophylaxis. Cochrane Database Syst Rev 2017; 2: CD003225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Buse DC, Silberstein SD, Manack AN, et al. Psychiatric comorbidities of episodic and chronic migraine. J Neurol 2013; 260: 1960–1969. [DOI] [PubMed] [Google Scholar]
- 26. Merikangas KR, Stevens DE. Comorbidity of migraine and psychiatric disorders. Neurol Clin 1997; 15: 115–123. [DOI] [PubMed] [Google Scholar]
- 27. Saw J, Starovoytov A, Humphries K, et al. Canadian spontaneous coronary artery dissection cohort study: In-hospital and 30-day outcomes. Eur Heart J 2019; 40: 1188–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-vmj-10.1177_1358863X241252444 for Migraine headache in patients with spontaneous coronary artery dissection: A report of the iSCAD Registry by Bryan J Wells, Malissa J Wood, Anne E O’Duffy, Jennifer A Sumner, Gerald Chi, Anna Grodzinsky, Heather L Gornik, Daniella Kadian-Dodov, Angela Taylor, Connie N Hess, Monika Sanghavi, Stanislav Henkin, Gretchen Wells, Lori Tam, James Orford, Kathryn Lindley, Dharam J Kumbhani, Clara Vitarello, Fahad Alkhalfan, C Michael Gibson, Katherine K Leon, Sahar Naderi and Esther SH Kim in Vascular Medicine


