Abstract
Background
Human parasitic infections caused by Adenophorean nematodes encompass a range of diseases, including dioctophymiasis, trichuriasis, capillariasis, trichinellosis, and myositis. These infection can result in adverse impacts on human health and cause societal and economic concerns in tropical and subtropical regions.
Methods
This review conducted searches in PubMed, Embase and Google Scholar for relevant studies that published in established databases up to April 26, 2024. Studies that focused on the common morphology, life cycle, disease distribution, clinical manifestations, and prevention and control strategies for Adenophorean parasitic diseases in humans were included.
Results
Adenophorean nematodes exhibit shared morphological characteristics with a four-layered cuticle; uninucleate epidermal cells; pseudocoelom with six or more coelomocytes; generally three caudal glands; five esophageal glands; two testes in males with median-ventral supplementary glands in a single row; tail in males rarely possessing caudal alae; amphids always postlabial; presence of cephalic sensory organs; absence of phasmids; and a secretory-excretory system consisting of a single ventral gland cell, usually with a non-cuticularized terminal duct. Humans play two important roles in the life cycle of the nematode class, Adenophorea: 1) as a definitive host infected by ingesting undercooked paratenic hosts, embryonated eggs, infective larvae in fish tissue and meat contaminated with encysted or non-encysted larvae, and 2) as an accidental host infected by ingesting parasitic eggs in undercooked meat. Many organs are targeted by the Adenophorean nematode in humans such as the intestines, lungs, liver, kidneys, lymphatic circulation and blood vessels, resulting in gastrointestinal problems, excessive immunological responses, cell disruption, and even death. Most of these infections have significant incidence rates in the developing countries of Africa, Asia and Latin America; however, some parasitic diseases have restricted dissemination in outbreaks. To prevent these diseases, interventions together with education, sanitation, hygiene and animal control measures have been introduced in order to reduce and control parasite populations.
Conclusions
The common morphology, life cycle, global epidemiology and pathology of human Adenophorean nematode-borne parasitic diseases were highlighted, as well as their prevention and control. The findings of this review will contribute to improvement of monitoring and predicting human-parasitic infections, understanding the relationship between animals, humans and parasites, and preventing and controlling parasitic diseases.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s40249-024-01216-1.
Keywords: Adenophorea, Morphological, Life cycle, Global epidemiology, Pathology
Background
Adenophorea Chitwood, 1958 (also known as Enoplea Inglis, 1983 or Aphasmidia) is a class of phylum Nematoda (roundworms), initially classified into two classes by Chitwood [1]: Phasmidia and Aphasmidia, based on the presence and absence of phasmids, respectively. However, Chitwood [2] later proposed replacing these terms with Secernentea (= secretors, referring to the presence of an excretory system with lateral canals) and Adenophorea (= gland bearers, referring to the presence of caudal glands) as modifications of the term coined by von Linstow [3]. In some classifications, Adenophorea would be grouped with Enoplea, and Secernentea with Chromadorea Inglis, 1983, based on small subunit (SSU) rDNA sequences [4, 5]. Most Adenophoreans are free-living, aquatic, and microbotrophic nematodes. They also are species that cause parasitic disease in invertebrates, vertebrates and plants [6]. The Adenophorea class has three major genera; Trichinella Railliet, 1895, Capillaria Zeder, 1800 and Trichuris Roederer, 1761, all of which are infectious in humans and remain as important public health issues worldwide, particularly in developing countries [7]. Trichinella, Trichuris and Capillaria sensu lato belong to the superfamily, Trichinelloidea Ward, 1907, and their stichosome esophagus has a unique structure [8] that resembles a capillary tube equating to a stack of gland cells, known as stichocytes, which are arranged similarly to a stack of donuts. Based on complete mtDNA coding genes, the order Trichocephalida Spasski, 1954 is segregated into three well-defined clades, representing the families Trichinellidae Ward, 1907, Trichuridae Ransom, 1911 and Capillariidae Railliet, 1915, which include Trichinella, Trichuris and Capillaria, respectively [9].
Trichinella spp. has been identified as the causative agent for human trichinellosis in many regions globally [10]. Over the past two decades, reports on Trichinella spp. infections in animals and humans have emerged from 95 (48.5%) countries worldwide. These cases encompass both the wild cycle, documented in 75 countries (38.3%), and domestic cycle, noted in 32 countries (16.3%), as well as human infections in 47 countries (23.9%). Nevertheless, there remains a scarcity of recent epidemiological data in numerous countries, with some available information dating back to the previous century [10]. Trichinellosis had an estimated annual incidence rate of 469.2‒985.3 cases per billion individuals per year and a global mortality rate of 0.3‒0.8 per billion individuals per year [11]. While the Capillaria species primarily infest various vertebrate animals, only three of them are known to infect humans: Calodium hepaticum (syn. Capillaria hepatica Bancroft, 1893), Eucoleus aerophilus Dujardin, 1845 (Capillaria aerophila Creplin, 1839) and Capillaria philippinensis Velasquez, Chitwood and Salazar, 1968 [12]. Intestinal capillariasis, primarily caused by C. philippinensis, is the most significant disease, which exhibits a higher prevalence in humans when compared to other Capillaria species. Furthermore, human trichuriasis is an intestinal helminthic infection, widespread globally, and attributed to the whipworm parasite Trichuris trichiura Linnaeus, 1771 [13, 14]. It is estimated that approximately 25% of the global population is infected with this parasite. Trichuris trichiura is found more commonly in specific regions, particularly in tropical and subtropical areas like East Asia, China, sub-Saharan Africa, and the Americas [15]. Roughly 1.049 billion individuals are affected by T. trichiura, encompassing 114 and 233 million preschool- and school-age children, respectively. The occurrence of T. trichiura is elevated and can be as high as 95% among children in various regions worldwide. These areas often experience issues like protein energy malnutrition and anemia, together with limited access to healthcare and educational resources [16]. Trichuris species that have been identified in various mammals include Trichuris vulpis Froelich, 1789 (found in canines), Trichuris suis Schrank, 1788 (in swine), Trichuris skrjabini Baskakov, 1924 (in goats), Trichuris ovis Abildgaard, 1795 (in sheep) and Trichuris muris Schrank, 1788 (in mice). Among these, only T. suis [17] and T. vulpis [18, 19] are capable of causing persistent active infections in humans. In addition, Mohd-Shaharuddin [20] reported use of molecular methods to test for parasite eggs, and the presence of T. trichiura in dog feces was revealed. Interestingly, T. vulpis also has been identified in human feces (1.3%). These findings suggest that cross-infection between humans and animals in sympatric areas may contribute to infections in both hosts. Dioctophyme renale Goeze, 1782, and Haycocknema perplexum Spratt, Beveridge, Andrews & Dennett, 1999 are two species in the class that can infect humans, but they have not been reported widely [21, 22]. Dioctophyme renale can be found across the globe, but is seldom responsible for human infections [23]. So far, reports of human cases have only emerged from 10 countries. In China, a total of 21 human cases have been recorded since the initial report of dioctophymosis in humans in 1981, spanning at least 14 provinces and municipalities [22]. Furthermore, H. perplexum is a parasite that has been associated with infrequent cases of life-threatening myositis in humans. This condition has only been documented in nine patients in Australia from 1998 to 2016 [24]. Currently, its presence is extending beyond its original endemic regions in Australia, encompassing areas like tropical north Queensland and Tasmania [21, 24]. Millions of people aross approximately 145 countries have been affected by outbreaks of Adenophorean nematodes (ANs). These outbreaks occur when humans ingest food or water contaminated with the eggs or encysted larvae of these worms (Fig. 1). Among this class of parasitic nematodes, T. trichiura is the species known to parasitize humans [25], while others are predominantly zoonotic [26, 27]. Thus, the main focus of prevention and control has been on animal control and hygiene measures.
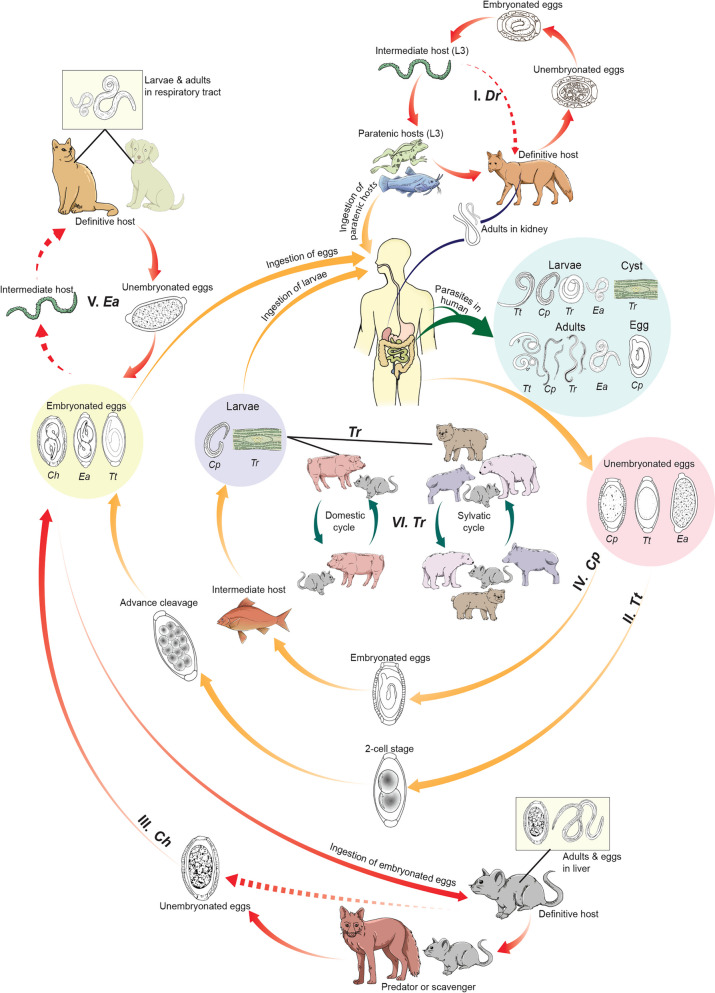
Fig. 1.
Schematic illustration of the life cycles of six parasites (redrawn from Centers for Disease Control and Prevention [28–32], including E. aerophilus, C. hepaticum, C. philippinensis, D. renale, Trichinella spp. and T. trichuira. Ea Eucoleus aerophilus; Ch Calodium hepaticum; Cp Capillaria philippinensis; Dr Dioctophyme renale; L3 third-stage larvae; Tr Trichinella spp.; Tt Trichuris trichuira
Previous studies have documented the prevalence, pathogenesis, and distribution of ANs [33]. However, due to extensive information needing collection, new data are required to update understanding of them. This review study focused on diverse parasite species and the global distribution of parasitic diseases involving ANs in humans. Moreover, deeper understanding of the basic biology of nematodes in the Adenophorea class and their reservoir is necessary in order to explain the expanding geographical distribution of these diseases [34, 35]. This review article aimed to provide a comprehensive overview of human parasitic infections involving ANs. To achieve this, a systematic review of existing literature was undertaken. The search focused on scholarly articles and publications that investigated the prevalence, pathogenesis, and clinical aspects of AN infections in humans. Additionally, studies exploring the common morphological features, life cycle characteristics of these parasites, as well as strategies for preventing and controlling AN-related diseases were included. Through the examination of these diverse aspects, this review aimed to enhance current knowledge and understanding of AN-related human parasitic infections.
Methods
Information sources and search strategy
This scoping review followed the recommendations outlined in the Preferred Reporting Items for Systematic Reviews, and Meta-analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines [36]. A combination of search terms was analyzed across various data sources, including PubMed, Embase, and Google Scholar, in order to conduct the scoping review from inception of the databases up until April 26, 2024. These sources were searched systematically for relevant books, articles, and other material. The scope of this review was centered around the Adenophorea class of nematodes, which has the potential to impact human health. The search strategy comprised a combination of keywords found in titles or abstracts, which were formulated as follows: Adenophorea (every genus such as Trichinella, Trichuris, Capillaria, etc.) AND (human parasites OR parasite infections OR parasite prevalence) AND (nematode morphology OR nematode life cycle OR global epidemiology of nematodes OR nematode pathology in humans OR prevention and control of nematodes) (see Additional file 1: Table S1 for detailed strategies).
Duplicated records were identified and removed using EndNote software X9 (Clarivate, Philadelphia, PA, USA). All of the papers underwent initial screening based on their titles and abstracts to identify the most relevant studies. If necessary, the morphological characteristics, life cycle, epidemiology, global distribution, pathogenesis, and prevention and control strategies relating to Adenophorea parasitic diseases were summarized.
Inclusion and exclusion criteria
The entire texts of these studies were examined to determine their suitability for inclusion in the review. The criteria for inclusion were as follows: 1) relevance to the Adenophorea class of nematodes, 2) explanation of the common morphology of the Adenophorea class of nematodes, 3) information related to the life cycle, epidemiology, pathogenicity, and prevention and control of human parasitic diseases caused by the Adenophorea class of nematodes, 4) no specified starting date for the databases, with a cutoff date of April 26, 2024, 5) cases or outbreaks occurring worldwide, and 6) publications written in English. In addition, studies presenting findings from the same source, conference abstracts, comments, resources without references, or studies that did not meet the relevant criteria were excluded.
Quality assessment of included literature
Critical appraisal was conducted by four reviewers (JI, CS, XL, SZG), who utilized the "Crowe Critical Appraisal Tool" (CCAT) to assess the quality of each study [37]. The CCAT, known for its reliability and validity in evaluating studies with diverse designs and implementation approaches, helped in reducing rater bias [37, 38]. To mitigate potential bias further, individual assessments were cross-checked, and any discrepancies were resolved by a fifth reviewer (NS). By following the established guidelines, the study team decided to categorize articles based on their CCAT scores, which used a six-point scale (ranging from 0 to 5 for each category), with a possible total score of 40.
Evidence extraction and analysis
Information was extracted from the studies included, based on the following categories: 1) morphology classification of Adenophorea, 2) life cycle of human Adenophorea parasitic diseases, 3) epidemiological trends and pathogenicity of human Adenophorea parasitic diseases, and 4) prevention and control strategies for human Adenophorea parasitic diseases. Five authors (JI, CS, XL, SZG and NS) independently evaluated the qualifications of the studies, compiled relevant information, and cross-validated the findings. Any disagreements were resolved through consensus among the authors.
Gap analysis
A gap analysis was conducted to identify areas that lacked research or had insufficient evidence. This analysis aimed to highlight knowledge gaps in current understanding of the Adenophorea class of nematodes and their impact on human health.
Results
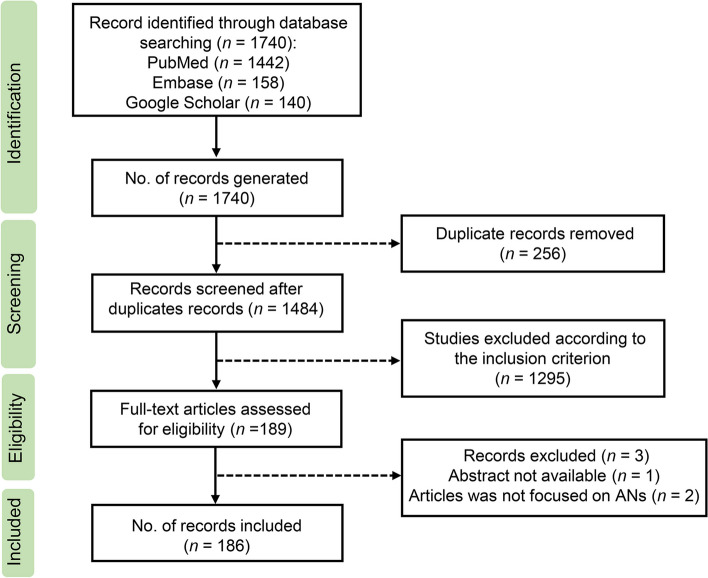
A total of 1740 records were retrieved initially for this review. After removing 256 duplicate records and excluding 1295 that did not meet the specified criteria, 186 were included in the analysis. Figure 2 presents a flowchart illustrating the selection process.
Fig. 2.
PRISMA flow diagram of the scoping review process for the Adenophorean class of nematodes
Common morphological characteristics of Adenophorea
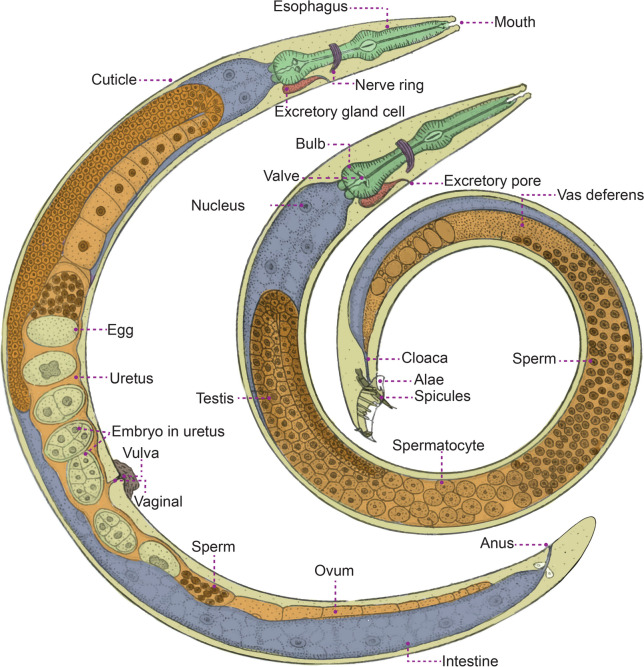
Adenophorea is characterized by specific morphological features encompassing the cuticle, epidermis, pseudocoelom, and the digestive, reproductive, sensory/nervous, and secretory-excretory systems [2, 6, 39–46]. Figure 3 details the morphological characteristics of the Adenophorea class, phylum Nematoda. The cuticle serves as a flexible exoskeleton, and exhibits invaginations at various points, including the mouth, amphids, aphasmids, and reproductive and excretory openings [39]. While generally smooth, the cuticle may display transverse or longitudinal striations that contain four layers of cuticle [6, 41]. Epidermal glands are often found beneath the cuticle, consisting of both unicellular epidermal glands and nonglandular cells [39]. Adenophoreans are non-segmented pseudocoelomates with a three-layered body, housing a pseudocoelom lined between the mesoderm and endoderm [39, 44], which contain six or more coelomocytes [46]. The digestive system typically lacks a rectal gland, but possesses three caudal and five esophageal glands [2, 6, 43]. The anterior portion of the specialized esophagus is a thin-walled, muscular tube in Trichinellida and Mermithida, while its posterior portion consists of a very thin tube surrounded by a column of single glandular cells called stichocytes. This entire structure is referred to as a stichosome. Stichocytes meet with the esophageal lumen via small ducts [47]. The stichosome may be homologous to the esophageal glands found in other nematodes, possibly arising from multiplication of the number of glands [48]. Eggs in the order, Trochocephalida (including Trichuris and Capillaria s.l.), typically have bipolar plugs (opercula), except in Trichinella spp. [49]. Similarly, eggs in the order, Dioctophymatida (Dioctophyme), are sculptured deeply or pitted and contain clear bipolar plugs [50]. The male reproductive system includes two testes, male tail with barely caudal alae (or bursae), and supplement glands that are median-ventral in a single row [6, 40, 43]. Adenophoreans feature paired lateral chemosensory organs known as amphids and lack deirids and phasmids [6, 40, 42]. Somatic and cephalic sensilla are distributed throughout the body, with cephalic sensilla positioned around the head [6, 42, 46]. The secretory-excretory system consists of a single ventral gland cell with a noncuticularized terminal duct lacking collecting tubules [6, 40, 45].
Fig. 3.
The common morphological characteristics of the Adenophorea class, phylum Nematoda (redrawn from Chitwood & Chitwood, 1950 [51]). Female (left) and male (right)
Life cycles of human Adenophorea parasitic diseases
Human parasitic diseases that are caused by ANs can be classified into seven groups, based on their genus and species (Fig. 1).
Group I
Humans serve as definitive hosts of D. renale following the consumption of undercooked paratenic hosts, such as fish or frogs [52]. Eggs of the parasite are excreted in urine, hatch into first-stage larvae (L1) in water, and are then ingested by oligochaete worms (intermediate hosts). These larvae develop to the third stage (L3) and encyst within paratenic hosts, which can subsequently infect carnivorous mammals and humans through their consumption. Humans can become infected by consuming either the paratenic or intermediate host [53, 54].
Group II
Humans are the definitive hosts of T. trichuira, which has no intermediate host in its life cycle. It releases unembryonated eggs into the soil together with feces, from which a 2-cell, advanced cleavage develops into embryonated eggs [55]. Humans are infected by ingesting the embryonated eggs in soil-contaminated food. Upon ingestion, the eggs hatch in the small intestine of the human, and the larvae mature in the colon [53].
Group III
Humans are the second accidental host of C. hepaticum. They are infected through the ingestion of parasitic eggs present in fecally contaminated water, food, or soil. C. hepaticum has a direct life cycle without an intermediate host [56, 57]. Eggs hatch in the intestine of rodents, thus releasing L1 larvae that develop and lay eggs in their livers [53]. The eggs are retained in the liver until the animal dies, and then released into the environment, as predators or scavengers (first accidental host) ingest the definitive host, and the cycle continues repeatedly [58]. In humans, the larvae hatch in the intestine, and juveniles migrate to the liver, mature, mate, and lay eggs, causing granuloma formation, liver necrosis [58, 59] and lesions [60].
Group IV
Humans are the definitive hosts for C. philippinensis. They are infected by consuming larvae in fish tissue. Unembryonated eggs are discharged in human feces and develop in water. When fish ingest these eggs, larvae develop in their tissues, and humans consume the infected raw or undercooked fish. Adult worms live in the small intestine, and females lay unembryonated and shell-less embryonated eggs. Released larvae can re-invade the small intestine in an autoinfection cycle [61, 62].
Group V
Humans may act as definitive hosts of E. aerophilus. They are infected by ingesting embryonated eggs from soil. This worm has a direct life cycle. The larvae hatch in the small intestine, then perforate the mucosa, migrate to the lungs, penetrate the alveoli, relocate to the air passages as they develop, and eventually reach maturity to live in the respiratory epithelium. Females lay eggs, which are excreted into the soil to mature. E. aerophilus may also have an indirect life cycle involving earthworms as intermediate hosts, which become infected after consumption by a mammalian host [63].
Group VI
Humans are the definitive host of Trichinella spp. They become infected by swallowing meat contaminated by encysted larvae (except for T. pseudospiralis and T. papuae, which do not encyst). The larvae develop into adult worms in the small intestine, in which they release larvae that migrate to muscle cells. Adults remain in the intestine until they die, and are then excreted [33]. Infection sources include domestic and wild animals [64].
Group VII
H. perplexum is a small muspiceoid nematode found within human skeletal muscle cells [65]. Its life cycle is still unknown. Potential sources of human infection encompass vertebrates, invertebrates, plants, soil, and water [5, 66]. Speculation suggests that it may rely on an intermediary arthropod host, with humans serving as incidental hosts; or that humans contract the infection through consuming of undercooked bush-meat from infected native fauna [21].
In summary, humans are accidental hosts of C. hepaticum but serve as definitive hosts of D. renale, T. trichuira, C. philippinensis, E. aerophilus, and Trichinella. It remains unclear whether humans are the host for H. perplexum. These parasites undergo various developmental stages within humans and other hosts, demonstrating the complexity of their life cycles. Similarities in these parasites include humans often acting as definitive hosts and common infection routes through ingestion of contaminated food or water. However, there are differences in life cycle complexity, with some parasites having direct cycles without intermediate hosts (T. trichiura, C. hepaticum), while others involve multiple hosts (D. renale, C. philippinensis, E. aerophilus). Additionally, infection mechanisms and adult worm locations vary, affecting organs such as the kidneys, colon, liver, small intestines, lungs, and muscle cells.
Epidemiology and pathogenesis of human Adenophorea parasitic diseases
The Adenophorea class of nematodes remains a public health concern of importance regarding humans. The distribution of human infection caused by 15 parasite species and 5 families in this class are described in Table 1.
Table 1.
Distribution of Adenophorean nematodes that can transmit parasitic diseases, human infection cases, host range and source of infection in humans
| Categories | Distribution | Distribution of human cases | Host range or host infection | Source of infection in humans | References |
|---|---|---|---|---|---|
| Capillaridae Railliet, 1915 | |||||
| Eucoleus aerophilus Dujardin, 1845 (syn. Capillaria aerophila Creplin, 1839) | Worldwide | Wild carnivores, dogs, cats, humans | Ingestion of embryonated eggs | [67] | |
| France, Iran, Morocco, Russia, Serbia, Ukraine | Carnivorous mammals | Cats | [68] | ||
| Calodium hepaticum (Bancroft, 1893) Moravec, 1982 (syn. Capillaria hepatica Bancroft, 1893) | Worldwide | Murid rodents and various other mammals | Consumption of unembryonated eggs in soil or infected game | [69] | |
| Argentina, France | Human, rodent, camelid | ND | [70] | ||
| Brazil, Canada, Czechoslovakia, England, Germany, Greece, Italy, Mexico, New Zealand, Nigeria, India, Ivory Coast, Japan, Republic of Korea, South Africa, Switzerland, Thailand, Turkey, USA, Yugoslavia | Marsupials, carnivores, hominids and other mammals | The consumption of infected game or from soil | [58] | ||
| China | Human | – | [60] | ||
| Israel | Human | – | [59] | ||
| Iran | Human | – | [57] | ||
| C. philippinensis Velasquez, Chitwood and Salazar, 1968 | The Philippines, Thailand, Japan, Iran, Egypt, China | Human | Raw fish | [71] | |
| China | Human | Fish | [72] | ||
| Colombia | Human | Fish | [73] | ||
| Egypt | Human | Fish | [74–76] | ||
| India | Human | Fish | [77] | ||
| Indonesia | Human | – | [78] | ||
| Japan | Human | Fish | [79] | ||
| Republic of Korea | Human | Fish | [80, 81] | ||
| Lao People's Democratic Republic | Human | Fish | [82] | ||
| The Philippines | Human | Fish | [62, 83, 84] | ||
| China (Taiwan Province) | Human | Fish | [85, 86] | ||
| Thailand | Human | Fish | [87–89] | ||
| Dioctophymatidae Castellani & Chalmers, 1910 | |||||
| Dioctophyme renale Goeze, 1782 | Worldwide | Mustelids, wild carnivores, domestic animals | Ingestion of raw or undercooked fish or frogs | [22, 54] | |
| Australia, China, Greece, India, Iran, Indonesia, Japan, Thailand, the United States, and Yugoslavia | Mustelids, wild carnivores, domestic animals | Fish or frogs | [22, 54] | ||
| Robertdollfusidae Chabaud & Campana, 1950 | |||||
| Haycocknema perplexum Spratt, Beveridge, Andrews & Dennett, 1999 | ND | Queensland and Tasmania in Australia | ND | ND | [21, 90] |
| Trichinellidae Ward, 1907 | |||||
| Trichinella britovi (T3) Pozio, la-Rosa, Murrell & Lichtenfels, 1992 | Temperate areas of Europe and Asia, Northern and Western Africa | Sylvatic mammals and seldomly domestic pigs |
Wild boars, domestic pigs horses, foxes, jackals |
[33] | |
| Algeria | Human | Golden jackal (Canis aureus) | [91] | ||
| Bulgaria | Human | Wild boar and backyard pig | [92] | ||
| Human | Domestic pig | [93] | |||
| France | Human | Wild boar | [94] | ||
| Greece | Human | Wild boar meat products | [95] | ||
| Italy | Human | Wild boar meat products | [96] | ||
| Human | Wild boar and pig | [97] | |||
| Serbia | Human | Wild boars | [98] | ||
| Slovakia | Human | Red foxes and wild boars | [99] | ||
| Spain | Human | Wild boar | [100] | ||
| Human | Wild boar | [101] | |||
| Sweden | Human | Wild boar | [101] | ||
| Turkey | Human | Raw meat balls of beef-mixed pork | [102] | ||
| T. murrelli (T5) Pozio & La Rosa, 2000 | United States and southern Canada | Sylvatic carnivores | Bears, horses | [33] | |
| France | Human | Horse | [103] | ||
| T. nativa (T2) Britov & Boev, 1972 | Arctic and subarctic areas of America, Asia, Europe | Sylvatic carnivores | Bears, walruses | [33] | |
| Canada (northern Ontario) | Human | Black bear meat | [104] | ||
| Canada (northern Saskatchewan) | Human | Bear meat | [105] | ||
| China | Human | Dog | [106] | ||
| United States | Human | Cougar jerky | [107] | ||
| T. nelsoni (T7) Britov and Boev, 1972 | Eastern-southern Africa | Sylvatic mammals | Warthogs, bush pigs | [33] | |
| Ethiopia, Kenya, Tanzania and Senegal | Human | – | [108] | ||
| T. papuae (T10) Pozio et al., 1999 | Papua New Guinea, Thailand | Wild pigs, saltwater crocodiles | Wild pigs | [33] | |
| Cambodia | Human | Wild pig | [109] | ||
| Malaysia | Human | Wild boar | [110] | ||
| Thailand | Human | Wild pig | [111] | ||
| Wild boar | [112] | ||||
| T. pseudospiralis (T4) Garkavi, 1972 | Cosmopolitan | Sylvatic mammals and birds, domestic pigs | Domestic and wild pigs | [33] | |
| France | Human | Wild boar | [113] | ||
| Italy | Human | The ‘beef’ steak tartare | [114] | ||
| Russia (Kamchatka) | Human | – | [115] | ||
| Tasmania | Human | – | [116] | ||
| Thailand | Human | Wild pig | [117] | ||
| T. spiralis (T1) Owen, 1835 | Cosmopolitan | Domestic and sylvatic mammals | Domestic and sylvatic swine horses | [33] | |
| Austria | Human | Pork belly | [118] | ||
| Bulgaria | Human | Backyard pig | [92] | ||
| Domestic pigs | [93] | ||||
| Insufficiently cooked meat | [119] | ||||
| Canada | Human | Sheep and pigs | [120] | ||
| Chile | Human | Wild boar | [121] | ||
| Croatia | Human | Smoked sausages | [122] | ||
| – | [123] | ||||
| Insufficiently cooked meat | [119] | ||||
| Egypt | Human | Pigs | [124] | ||
| Estonia | Human | – | [125] | ||
| Ethiopia | Human | Raw pork meat | [126] | ||
|
France Serbia |
Human | Backyard pigs | [127] | ||
| Insufficiently cooked meat | [119] | ||||
| Germany, Latvia, Lithuania, Russia, Spain | Human | Insufficiently cooked meat | [119] | ||
| China (Hong Kong Special Administrative Region) | Human | Inadequately cooked pork | [128] | ||
| Hungary | Human | Backyard pigs and wild boars | [129] | ||
| India | Human | Pork | [130] | ||
| Indonesia | Human | – | [131] | ||
| Italy | Human | Pigs, wild boars and horses | [97] | ||
| Insufficiently cooked meat | [119] | ||||
| Republic of Korea | Human | Wild boar | [132] | ||
| Badger | [133] | ||||
| Lao People's Democratic Republic | Human | Uncooked or fermented pork | [134] | ||
| Lebanon | Human | Pork | [135] | ||
| Mexico | Human | – | [136] | ||
| New Zealand | Human | Pigs | [137] | ||
| Poland | Human | Sausage made of wild boar | [138] | ||
| Insufficiently cooked meat | [119] | ||||
| Romania | Human | Pig meat and products (including wild boar) | [123] | ||
| Insufficiently cooked meat | [119] | ||||
| Slovakia | Human | Pork and/or smoked pork products | [139] | ||
| Insufficiently cooked meat | [119] | ||||
| Thailand | Human | Pigs | [140] | ||
| United States | Human | Pork sausage | [141] | ||
| Vietnam | Human | Raw pork | [142] | ||
| Pork | [143] | ||||
| Trichinella T6 | Canada, Alaska, Rocky Mountains, and Appalachian Mountains in the United States | Sylvatic carnivores | Carnivores | [33] | |
| United States | Cougar jerky | [107] | |||
| Trichinella T9 | Japan | Sylvatic carnivores | ND | [33] | |
| Japan | Human | Bear meat | [144] | ||
| Trichinella spp. | Argentina | Human | Puma, armadillo and wild boar | [145] | |
| Austria, Bulgaria, Croatia, Estonia, France, Germany, Greece, Hungary, Italy, Latvia, Lithuania, Netherlands, Poland, Portugal, Romania, Slovakia, Spain, Sweden | Human | Pig and wild boar | [123] | ||
| Bosnia-Herzegovina | Human | Domestic and wild animals | [146] | ||
| Belarus | Human | Domestic and sylvatic mammals | [147] | ||
| China | Human | Pork | [148] | ||
| Czech Republic | Human | – | [149] | ||
| Georgia | Human | Pork | [150] | ||
| Greenland | Human | Polar bear | [151] | ||
| Iran Islamic Rep | Human | Boar meat | [152] | ||
| Ireland | Human | – | [153] | ||
| Israel | Human | Wild pig | [154] | ||
| Wild boar | [155] | ||||
| Kazakhstan | Human | Wild boars | [147] | ||
| Kyrgyzstan | Human | – | [149] | ||
| Lao People's Democratic Republic | Human | Raw pork | [156] | ||
| Lithuania | Human | Pork and wild boar | [157] | ||
| Macedonia | Human | – | [149] | ||
| Montenegro, Yugoslavia | Human | Pork | [158] | ||
| Russia | Human | Pork and wild animals (bear, badger, dog) | [159] | ||
| Pork | [160] | ||||
| Senegal | Human | Smoked warthog (Phacochoerus africanus) | [161] | ||
| Slovakia | Human | Red foxes and wild boars | [99] | ||
| Slovenia | Human | – | [149] | ||
| Switzerland | Human | – | [149] | ||
| China (Taiwan Province) | Human | Soft-shelled turtles | [162] | ||
| Ukraine | Human | Infected game | [163] | ||
| United Kingdom | Human | – | [149] | ||
| Uzbekistan | Human | Wild boar | [147] | ||
| Trichuridae, Ransom, 1911 | |||||
| Trichuris trichiura Linnaeus, 1771 | Worldwide | Developing regions of Asia, Africa, and Latin America | Human | Ingesting parasitic eggs contaminated in soil, water, vegetables, fruits, etc. | [164, 165] |
ND None documented
Dioctophymiasis
The geographical distribution of D. renale infection in mammals has been reported in at least 33 countries across Asia, Africa, Europe and South and North America, with Argentina and Brazil each reporting more than 1000 cases. The life cycle involves various paratenic hosts, primarily fish, frogs, and toads. Mustelids and canids predominantly serve as definitive hosts that play a crucial role in sustaining the parasite’s life cycle. At least 49 different mammals have been recognized as definitive hosts for D. renale, such as golden jackal, coyote, gray wolf, domestic dog, red wolf, capuchin monkey, fox, wolf, horse, brown rat, brown bear, racoon, mink, and squirrel monkey [166]. The American mink (Neovison vison), predominantly found in North America, is identified as the primary definitive host and reservoir, due to the abundant presence of adult parasites of both genders within a single animal host [167].
Dioctophymiasis is a zoonotic disease caused by Dioctophyme (or Dioctophyma) renale (giant kidney worm), and one of the largest known parasitic nematodes infecting humans [168]. This parasite infects humans relatively rarely, and to date, only 10 countries have reported cases of this infection [22] (see Additional file 1: Figure S1). Human infection of D. renale usually manifests as nonspecific clinical symptoms including mainly hematuria [22, 169], loin pain [22], nephritis, intermittent kidney pain [169], and renal cyst [170] that may result in worms migrating through the ureter [171]. Sometimes it manifests as weight loss, frequent and urgent urination, fever, anemia, and abdominal pain [22].
Trichuriasis
Trichuriasis is caused by infection of Trichuris trichuira, also known as the human whipworm, and a member of the Trichuridae family. This worm is found worldwide, notably in Asia, Africa and Latin America [164, 165] (see Additional file 1: Figure S2). T. trichuira has infected approximately 795 million individuals worldwide [172]. Infection often presents subclinically and moderately, however severe infections, especially among children, can result in weight loss, malnutrition, anemia, and rectal prolapse in addition to watery stools, mucoid mucus, abdominal pain, nausea, and vomiting [173].
Capillariasis
Capillariasis is caused by Capillaria, a genus of the family, Capillaridae, that has 300 species, of which only three are well-known human parasites, including Capillaria philippinensis (syn. Paracapillaria philippinensis), Calodium hepaticum (syn. Capillaria hepatica), and Eucoleus aerophilus (syn. Capillaria aerophila) [12]. Over 300 capillariid species parasitize diverse vertebrate groups worldwide. Identifying them is challenging due to limited taxonomically informative structures, leading to laborious classification and controversial genus definitions that render capillariid taxonomy among the most intricate within Nematoda. An update on a study by Borba [174] focused on examining capillariid eggshell structure via scanning electron microscopy, which compared patterns among 12 species and enhanced taxonomy and species identification. In addition, the study introduced an innovative taxonomic approach by merging biological data with artificial intelligence techniques to characterize capillariid eggs. This method not only aimed to advance current understanding, but also give support for future research, particularly in the taxonomy and diagnosis of both contemporary and ancient capillariids [175].
Hepatic capillariasis
Calodium hepaticum infection causes hepatic capillariasis, which is a zoonotic disease that affects the liver of rodents (main hosts) and various other mammals worldwide [58]. Multiple rodent species that belong to the Muroidea superfamily act as primary hosts for this pathogen. Calodium hepaticum has been detected in Muroidean hosts across over 60 countries spanning Africa; Asia; Europe; Oceania; and North, Central and South America. Rattus norvegicus (Norway rat) exhibits the highest global prevalence of infection, with rates exceeding 50% reported in various regions across Asia, Europe and South and North America. Other murid species exhibit high prevalence rates in specific regions. For instance, in Asia, Rattus tanezumi and Niviventer fuloscens (white bellied rat) have been documented with prevalence rates exceeding 50%. Furthermore, Ondatra zibethicus serves as a significant host for C. hepaticum in North America, while in the UK, Apodemus sylvaticus (long-tailed field mice) and Myodes glareolus (bank vole) exhibit elevated prevalence rates [176]. While murid rodents act as primary hosts, a wide range of other mammals, including Insectivora (e.g. European hedgehog, shrew), Marsupialia (e.g. opossum, wallaby, kangaroo), Chiroptera (e.g. bat), Artiodactyla (e.g. antelope, peccary, cattle, pig), Lagomorpha (e.g. hare, rabbit, cottontail, pika), Hyracoidea (e.g. hyrax), Perissodactyla (e.g. horse, tapir), Primates (e.g. lemur, monkey, macaque, saki, gorilla, chimpanzee, human), and Carnivora (e.g. skunk, dog, wolf, fox, cat), can also be affected by hepatic capillariasis. In total, over 180 mammalian species, including humans, are recognized as suitable hosts for this parasite [69]. In humans, this worm is responsible for uncommon cases of hepatic capillariosis and spurious infections in patients [177]. It is found throughout the world, and human infection cases of C. hepaticum have been documented in different regions of Africa, Asia, Europe, North and South America, and Oceania (see Additional file 1: Figure S3), with 163 individuals affected [58, 59].
Sustained fever, respiratory disorder, abdominal discomfort, diarrhea, leukocytosis, and eosinophilia are common clinical symptoms of C. hepaticum infection. Moreover, egg deposition in the liver can result in septal fibrosis and necrotized parasitic granulomas, from which high-intensity infections can induce liver cell disruption and damage [178].
Intestinal capillariasis
Capillaria philippinensis is a pathogen that causes human intestinal capillariasis as well as an emerging zoonotic parasite that has been increasingly evident in the past two decades [12]. Chitwood et al. [179] found the first case of C. philippinensis infection in The Philippines, and the parasite became endemic in Thailand in 1973 [180]. Intestinal capillariasis has now spread from endemic areas to several other Asian countries, such as China [72, 85, 86], India [77], Indonesia [78], Japan [79], Republic of Korea [80, 81], and the Lao People’s Democratic Republic [82] (see Additional file 1: Figure S4), and Egypt in Africa [74, 75]. In addition, two cases of infection have been revealed in Europe, one from a Colombian man infected in a nonendemic area, and another from an Italian man who visited an endemic area in Indonesia [73, 78]. More than 2000 residents worldwide have been infected with C. philippinensis, resulting in nearly 200 fatalities [62].
Human intestinal capillariasis can present clinically as watery stools, diarrhea, lower limb edema, vomiting, crampy abdominal pain, weight loss, anorexia, and borborygmi [72, 74, 75, 87], which if left untreated can worsen into a serious condition. The severe symptoms of C. philippinensis, which include protein-losing enteropathy, hypokalemia (electrolyte loss), and chronic diarrhea [76, 79, 88], can be deadly to humans.
Pulmonary capillariasis
Eucoleus aerophilus is a nematode with a worldwide geographical distribution. It causes lung capillariosis in both wild and domestic animals, including coyote, fox, wolf, cat and dog [181], and sporadic reports have shown its zoonotic potential in humans [182, 183]. The precise life cycle of this parasite, whether direct or indirect, remains unclear, with suggestions that earthworms could serve as potential intermediate or paratenic hosts. The occurrence of E. aerophilus has been reported in 36 animal species, encompassing both wild and domestic animals across 38 countries worldwide. The highest prevalence of E. aerophilus was detected predominantly in fox, cat and dog, and documented in Lithuania (97.12%), Uruguay (50%) and Italy (19.51%), respectively [184].
The trichuroid parasitic nematode, E. aerophilus, is the cause of pulmonary capillariasis. This parasite has been regarded as the most significant respiratory parasite of domestic cat in terms of worldwide distribution over the past three decades, but it rarely infects humans, with only 12 cases being reported in six countries including Russia, France, Iran, Morocco, Serbia and Ukraine [68, 185] (see Additional file 1: Figure S5). Clinical symptoms of E. aerophilus infection are coughing, fever, bronchitis, mucoid mucus or blood-tinged sputum, eosinophilia, and dyspnea [183].
Trichinellosis
Trichinellosis (or trichinosis) is a devastating zoonotic disease caused by members of the genus Trichinella, family Trichinellidae, that has a worldwide distribution in domestic and/or sylvatic animals, as well as among humans. An update of this genus in wildlife worldwide was reviewed by Crisóstomo-Jorquera and Landaeta-Aqueveque in 2022 [186]. They found that Trichinella spp. had been documented across 129 host species of wild or feral animals in 64 countries. It comprises 13 genotypes, each restricted to specific geographical regions. Europe has the highest number of animals studied, with wild boar being the host species mostly researched. Interestingly, the prevalence of Trichinella does not correlate with research efforts, suggesting more focus is needed on animals higher in food chains. Invasive species such as raccoon dog, wild boar, and American mink can serve as important reservoirs. Ultimately, the geographical spread appears to be the primary driver influencing the distribution of Trichinella species among hosts. In humans, Trichinella infection is related to the consumption of undercooked or raw meat and raw meat derivatives. Each year, 10,000 human incidences of infection from Trichinella species are reported from 55 different countries. Nine species of Trichinella are suspected currently of infecting humans, including encapsulated (T. spiralis, Trichinella britovi, Trichinella murrelli, Trichinella nativa, Trichinella nelsoni and two unnamed genotypes: Trichinella T6 and T9), and non-encapsulated (Trichinella papuae and Trichinella pseudospiralis) species [147], with T. spiralis being the most pervasive in pig, alongside widespread species of this genus [187]. An update in the literature reported almost 64 countries with human Trichinella infection (see Additional file 1: Figure S6), particularly T. spiralis, the most frequent species distributed internationally.
Trichinella britovi is found widespread in temperate sylvatic carnivores in Europe and Asia. According to reports from Algeria, Bulgaria, France, Greece, Italy, Serbia, Slovakia, Spain, Sweden and Turkey, the majority of T. britovi infections in humans have been caused by ingesting raw meat or raw meat products from wild boar and wolf. Trichinella murrelli also is present in sylvatic carnivores that dwell in temperate climates in the Nearctic realm. Human infection with T. murrelli was first reported in 1985 after feeding infected horses imported into France from Connecticut, resulting in a massive human outbreak [103, 188]. Moreover, sylvatic predators that inhabit frigid regions of Asia, Europe, and North America, including wolf, black and grizzly bear, mountain lion, lynx, fox, and raccoon dog, are known to transmit Trichinella nativa [108, 188]. Human infections from T. nativa have been confirmed in Canada (northern Ontario and northern Saskatchewan), China (northeast), and the United States between 1996 and 2017 through eating raw meat from bear, dog or mountain lion [104–107]. Trichinella nelsoni is found in sylvatic carnivores inhabiting eastern and southern Africa (Kenya, Tanzania, and South Africa), of which spotted hyena is the main reservoir. Less than 100 human infections have been documented with this species in Ethiopia, Kenya, Tanzania, and Senegal spanning the last decade [108]. In addition, Trichinella T6 was recognized in carnivores (e.g., fox, bear and walrus) in several Arctic ecosystems in Canada and the United States [33]. Infections in humans have been associated with eating raw game meat, according to 1995 evidence from Idaho in the United States [107]. Sylvatic carnivores in Japan were discovered transmitting Trichinella T9. The intake of raw bear meat correlated with Trichinella T9 infection, causing an outbreak of trichinellosis in 2016, which affected 21 individuals across Japan [144]. Trichinella papuae was discovered by Pozio et al. in 1999, and is the most recent species infecting sylvatic swine in Papua New Guinea [189]. Mammals and reptiles are the principal reservoir hosts for this species [33]. It is interesting to note that during outbreaks from 2006 to 2020, human infections for this species have been reported in Thailand [111, 112], Malaysia [110], and Cambodia [109]. In Tasmania, Trichinella pseudospiralis has been detected in both mammals and birds [147]. Human infections from eating domestic or sylvan animals have been revealed in Tasmania, Thailand, France, Italy, and Kamchatka Krai. Besides, this parasite was the causative agent of the 2015 trichinellosis epidemic in northern Italy [114].
Patients in the gastrointestinal phase of Trichinella spp. infection are generally asymptomatic or present mild clinical manifestations, such as nausea, diarrhea, vomiting and abdominal pain after 1–2 days, as a result of the first stage larvae penetrating the small intestine [190]. Skeletal muscles, periorbital edema, fevers, myalgias, myositis, encephalitis, myocarditis, high levels of eosinophils, white blood cells, and muscle enzymes are among the classic clinical symptoms of the subsequent systemic and muscular phase, which is brought on by larvae entering the lymphatic circulation and blood vessels [161, 190]. Clinical symptoms might range from moderate to severe, depending on the number of parasitic worms taken from meat. Severe infections, however, ultimately result in death [117, 190].
Parasitic myositis
Parasitic myositis is caused by the muspiceoid nematode, Haycocknema perplexum, family Robertdollfusidae, and is suspected of being a zoonotic disease. It was reported initially in 1998 and isolated from a man in Tasmania, Australia [65]. Human myositis has now spread from endemic areas in Australia, including tropical north Queensland and Tasmania [21, 90] (see Additional file 1: Figure S7), and its global distribution remains unclear. This worm is a rare cause of myositis in humans, with only 9 patients being publicized in Australia between 1998 and 2016 [90]. Human infection with H. perplexum generates mild eosinophilia, elevated creatine kinase, muscular weakness, dysphagia, and weight loss [24, 90, 191].
Disease prevention and control
While the majority of human parasites in the Adenophorea class are zoonotic and propagate through the ingestion of undercooked meats by humans, some species (T. trichiura and E. aerophilus) infect by consumption of embryonated eggs from soil. However, due to the unclear life cycle of H. perplexum, there are no specific recommendations for its prevention and control. Since no vaccines are available, prevention relies on education, hygiene measures, and managing animal hosts (Table 2).
Table 2.
Summary of major prevention and control measures for human parasitic diseases of the Adenophorea class of nematodes
| Measure | Details |
|---|---|
| Education and hygiene |
- Educate consumers on the risks of eating raw/undercooked meat from domestic/wild animals (fish, frog, pig, etc.). - Promote hand washing with soap before eating. |
| Food safety |
- Cook meat at no less than 71 °C (160 °F). - Freeze meat at no less than -15 °C (5 °F) (not recommended for wild game due to freeze-resistant parasites). - Use irradiation (0.3 kGy). |
| Sanitation (WASH Program) |
- Improve water quality and quantity. - Increase access to latrines. - Manage fecal waste. - Promote personal hygiene. |
| Preventive chemotherapy |
- Administer single doses of oral mebendazole or albendazole. - Target children, women of reproductive age, and at-risk populations. - Aim for at least 75% coverage. |
| Animal control |
- Regular deworming of animals. - Prevent animals from accessing contaminated environments. - Regular testing/treatment for parasitic infections. - Rodent control. |
| Research and development |
- Vaccines. - Probiotics (e.g., Lactobacillus to prevent T. spiralis and T. britovi). - Chemicals such as OX02983 to inhibit egg development and hatching. |
WASH Water, sanitation, and hygiene
In minimizing parasitic infection, consumers should be informed about the risks of eating raw or undercooked meat from domestic and wild animal carriers of parasites (such as D. renale, Capillarea and Trichinella) [22, 33, 192]. The International Commission on Trichinellosis advises using test-and-slaughter techniques, cooking, or irradiating to prevent infection [193]. However, freezing is ineffective for wild game, due to freeze-resistant Trichinella taxa such as T. britovi and T. nativa [194]. Furthermore, the Global Water, Sanitation, and Hygiene (WASH) program, guided by the World Health Organization (WHO), helps in reducing trichuriasis and other soil-transmitted helminth infections by improving water quality and quantity, access to latrines, fecal waste management, and personal sanitation and hygiene. Preventive chemotherapy significantly reduces the prevalence and impact of soil-transmitted helminthiases, with an up to 80% decrease in parasite burden and prevalence in endemic areas [195–197]. In 2017, the WHO revised guidelines for preventive chemotherapy against soil-transmitted helminth infections (STHs) in endemic regions [198]. These programs, which administer single doses of mebendazole or albendazole to at-risk groups, aim to reduce trichuriasis prevalence [199]. By 2017, 598 million children (69% of the at-risk population) were treated, nearing the 2020 target of 75% coverage [200]. However, reinfection in areas with poor sanitation and hygiene remains a problem [201], emphasizing the need for better WASH programs to control STH infections [200].
Animal control measures reduce animal-to-human transmission through deworming regularly, preventing access to contaminated environments, and treating infected animals. Regular testing and treatment can eliminate fecal contamination in animals reared in uncontaminated areas [202, 203]. Treating infected cats with parasiticide (1% spot-on moxidectin) effectively reduces Capillaria spp. eggs [204]. Rodent control and appropriate sanitation help to prevent the transmission of C. hepaticum, Trichinella, and D. renale. In addition to current measures, other prevention methods are being researched, such as vaccines [205] and probiotics to prevent T. spiralis [206] and T. britovi [207] infections. The chemical, dihydrobenzoxazepinone OX02983, can inhibit egg development and hatching by breaking the life cycle of T. trichiura [208]. These innovative techniques have the potential for employment as efficient prevention and control measures.
Conclusions
Human infection by ANs remains an important worldwide health concern. Approximately 15 nematode species from diverse tropical and subtropical regions have been linked to human infections. Dioctophymiasis, trichuriasis, capillariasis, trichinellosis, and myositis are human parasitic diseases caused by ANs, each with a distinct geographical distribution. These diseases pose significant threats to human health, due to their multifaceted effects on various organs, which often lead to severe complications and even mortality.
Humans serve as definitive and accidental hosts of ANs, and are infected by ingesting undercooked or raw meat and food contaminated with parasitic eggs. To interrupt the cycle of disease transmission, significant progress has been made in preventive and control measures, primarily focusing on animal control. Additionally, efforts have been made to emphasize the importance of education, sanitation, and hygiene practices to mitigate the risk of contracting these infections.
Based on epidemiological data and studies of the parasitic life cycle, the updated information in this review supports the prevention and control of parasitic infections, as well as further surveillance and forecasting of human-parasite infection outbreaks in both endemic and non-endemic areas. However, the life cycle and particular host of H. perplexum are still unknown, hence, no recommendations for avoiding and managing them are currently available. Comprehensive molecular epidemiology research should be a component of further studies to better understand of the distribution, parasitic ecology and parasitic infections in animals and humans, potentially leading to the establishment of new strategies for monitoring, predicting, preventing, and actively managing parasitic diseases caused by ANs.
Supplementary Information
Acknowledgements
The authors would like to thank all of the participants in this study as well as the staff at Hainan General Hospital and Sun Yat-Sen University for their support.
Abbreviations
- ANs
Adenophorean nematodes
- Ch
Calodium hepaticum
- Cp
Capillaria philippinensis
- Dr
Dioctophyme renale
- Ea
Eucoleus aerophilus
- Hp
Haycocknema perplexum
- L1
First-stage larvae
- L3
Third-stage larvae
- Tr
Trichinella spp.
- Tt
Trichuris trichuira
Authors’ contributions
JI, CS, XL, SG and NS conceived and designed the study. JI, XL, CS, SG and NS conducted the literature search, and managed and analyzed the data. JI and CS drafted the first version of the manuscript. TC and ZL contributed to writing, editing, and revising the review. All of the authors have read the manuscript and given their consent for its submission to Infectious Diseases of Poverty.
Funding
This study was supported by Hainan Province Science and Technology Special Fund (grant number ZDKJ2021035 and ZDKJ202003), the Key Research and Development Program of Hainan Province (grant number ZDYF2020120), the Academician Innovation Platform Special Project of Hainan Province (grant number YSPTZX202133), the Open Project Program of Hainan Tropical Diseases Research Center (Hainan Sub-Center, Chinese Center for Tropical Diseases Research) (grant number HNTDC202301), Postdoctoral Fund of Hainan General Hospital (grant number 2022BSH01), Key R&D Plan Projects of Hainan Province (grant number ZDYF2021SHFZ091), and the National Parasitic Resources Center of China (grant number NPRC-2019-194-30). This work was Supported by the Construction Project of Hainan Province Clinical Medical Center and Science, and The Innovation Platform for Academicians of Hainan Province. The study design, data collection and analysis, data interpretation, and manuscript writing were not influenced by the funding bodies.
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Footnotes
Jitrawadee Intirach and Chang Shu are joint first authors with equal contribution.
Contributor Information
Tao Chen, Email: ctxwyc@163.com.
Zhiyue Lv, Email: lvzhiyue@mail.sysu.edu.cn.
References
- 1.Chitwood BG. A revised classification of the Nematoda. In: Anon, editor. Papers of helminthology, 30 year jubileum K.J. Skrjabin. Moscow: All-Union Lenin Academy of Agricultural Sciences; 1937. p. 67–79.
- 2.Chitwood BG. The designation of official names for higher taxa of invertebrates. Bull Zool Nomencl. 1958;15:860–895. doi: 10.5962/bhl.part.19410. [DOI] [Google Scholar]
- 3.von Linstow O. Helminthen der Russischen Polarexpedition (1900–1903) Mem Acad Imp Sci St Petersb Ser 8 Class Phys Math. 1905;18:17. [Google Scholar]
- 4.Blaxter ML, De Ley P, Garey JR, Liu LX, Scheldeman P, Vierstraete A, et al. A molecular evolutionary framework for the phylum Nematoda. Nature. 1998;392:71–75. doi: 10.1038/32160. [DOI] [PubMed] [Google Scholar]
- 5.De Ley P, Blaxter ML. Systematic position and phylogeny. In: Lee DL, editor. The biology of nematodes. London: Taylor & Francis; 2002. pp. 1–30. [Google Scholar]
- 6.Bogitsh BJ, Carter CE, Oeltmann TN. Human parasitology. New York: Academic; 2018. [Google Scholar]
- 7.Berman JJ. Taxonomic guide to infectious diseases: understanding the biologic classes of pathogenic organisms. 2nd ed. Cambridge: Elsevier; 2019.
- 8.Ali MI, El-Dib NA, Abdel-Latif M, Arafa WM, Abdel Gawad SS. Screening of Capillaria philippinensis infection using Trichuris muris and Trichinella spiralis antigens. Parasitol United J. 2021;14:178–182. doi: 10.21608/puj.2021.76982.1121. [DOI] [Google Scholar]
- 9.Calvani NED, Wright M, White J, Stepkovitch B, Francis E, Rivory P, et al. What the fox? Cryptic Eucoleus [Capillaria] sp. in the respiratory tract of a cat from Australia. Curr Res Parasitol Vector Borne Dis. 2021;1:100028. doi: 10.1016/j.crpvbd.2021.100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pozio E. Epidemiology. In: Bruschi F, editor. Trichinella and Trichinellosis. London: Academic; 2021. [Google Scholar]
- 11.Devleesschauwer B, Praet N, Speybroeck N, Torgerson PR, Haagsma JA, De Smet K, Murrell KD, Pozio E, Dorny P. The low global burden of trichinellosis: evidence and implications. Int J Parasitol. 2015;45:95–99. doi: 10.1016/j.ijpara.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy J, Moore TA. Emerging helminth zoonoses. Int J Parasitol. 2000;30:1351–1360. doi: 10.1016/S0020-7519(00)00122-3. [DOI] [PubMed] [Google Scholar]
- 13.Viswanath A, Yarrarapu SNS, Williams M. Trichuris trichiura Infection. Treasure Island: StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- 14.Al Amin ASM, Wadhwa R. Helminthiasis. Treasure Island: StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- 15.Parvaiz Y, Semran P, Shahid R, Nisheet Z. Trichuris: A Critical Review. In: Dogan N, editor. Roundworms - A Survey From Past to Present. London: IntechOpen; 2022.
- 16.Stephenson LS, Holland CV, Cooper ES. The public health significance of Trichuris trichiura. Parasitology. 2000;121:S73–95. doi: 10.1017/S0031182000006867. [DOI] [PubMed] [Google Scholar]
- 17.Kradin RL, Badizadegan K, Auluck P, Korzenik J, Lauwers GY. Iatrogenic Trichuris suis infection in a patient with Crohn disease. Arch Pathol Lab Med. 2006;130:718–720. doi: 10.5858/2006-130-718-ITSIIA. [DOI] [PubMed] [Google Scholar]
- 18.Dunn JJ, Columbus ST, Aldeen WE, Davis M, Carroll KC. Trichuris vulpis recovered from a patient with chronic diarrhea and five dogs. J Clin Microbiol. 2002;40:2703–2704. doi: 10.1128/JCM.40.7.2703-2704.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Márquez-Navarro A, García-Bracamontes G, Alvarez-Fernández BE, Ávila-Caballero LP, Santos-Aranda I, Díaz-Chiguer DL, et al. Trichuris vulpis (Froelich, 1789) infection in a child: a case report. Korean J Parasitol. 2012;50:69–71. doi: 10.3347/kjp.2012.50.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohd-Shaharuddin N, Lim YAL, Hassan NA, Nathan S, Ngui R. Molecular characterization of Trichuris species isolated from humans, dogs and cats in a rural community in Peninsular Malaysia. Acta Trop. 2019;190:269–272. doi: 10.1016/j.actatropica.2018.11.026. [DOI] [PubMed] [Google Scholar]
- 21.Koehler AV, Spratt DM, Norton R, Warren S, McEwan B, Urkude R, et al. More parasitic myositis cases in humans in Australia, and the definition of genetic markers for the causative agents as a basis for molecular diagnosis. Infect Genet Evol. 2016;44:69–75. doi: 10.1016/j.meegid.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 22.Yang F, Zhang W, Gong B, Yao L, Liu A, Ling H. A human case of Dioctophyma renale (giant kidney worm) accompanied by renal cancer and a retrospective study of dioctophymiasis. Parasite. 2019;26:22. doi: 10.1051/parasite/2019023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chauhan S, Kaval S, Tewari S. Dioctophymiasis: a rare case report. J Clin Diagn Res. 2016;10:Dd01–02. doi: 10.7860/JCDR/2016/17394.7305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Basuroy R, Pennisi R, Robertson T, Norton R, Stokes J, Reimers J, Archer J. Parasitic myositis in tropical Australia. Med J Aust. 2008;188:254–256. doi: 10.5694/j.1326-5377.2008.tb01601.x. [DOI] [PubMed] [Google Scholar]
- 25.Rivero J, Cutillas C, Callejón R. Trichuris trichiura (Linnaeus, 1771) from human and non-human primates: morphology, biometry, host specificity, molecular characterization, and phylogeny. Front Vet Sci. 2020;7:626120. doi: 10.3389/fvets.2020.626120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaewpitoon N, Kaewpitoon SJ, Pengsaa P. Food-borne parasitic zoonosis: distribution of trichinosis in Thailand. World J Gastroenterol. 2008;14:3471–3475. doi: 10.3748/wjg.14.3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Camargo LMA, de Souza Almeida Aranha Camargo J, Vera LJ, di Tarique Crispim Barreto P, Tourinho EK, de Souza MM. Capillariaisis (Trichurida, Trichinellidae, Capillaria hepatica) in the Brazilian amazon: low pathogenicity, low infectivity and a novel mode of transmission. Parasit Vectors. 2010;3:11. doi: 10.1186/1756-3305-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DPDx. Intestinal Capillariasis [Capillaria philippinensis]. 2020. https://www.cdc.gov/dpdx/intestinalcapillariasis/index.html. Accessed 26 Apr 2024.
- 29.DPDx. Dioctophymiasis [Dioctophyme renale]. 2019. https://www.cdc.gov/dpdx/dioctophymiasis/index.html. Accessed 26 Apr 2024.
- 30.CDC. Parasites - Trichinellosis (also known as Trichinosis). 2023. https://www.cdc.gov/parasites/trichinellosis/index.html. Accessed 26 Apr 2024.
- 31.DPDx. Hepatic Capillariasis [Capillaria hepatica]. 2019. https://www.cdc.gov/dpdx/hepaticcapillariasis/index.html. Accessed 26 Apr 2024.
- 32.DPDx. Trichuriasis [Trichuris trichiura]. 2017. https://www.cdc.gov/dpdx/trichuriasis/index.html. Accessed 26 Oct 2023.
- 33.Gottstein B, Pozio E, Nöckler K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clin Microbiol Rev. 2009;22:127–145. doi: 10.1128/CMR.00026-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burke R, Masuoka P, Murrell KD. Swine trichinella infection and geographic information system tools. Emerg Infect Dis. 2008;14:1109–1111. doi: 10.3201/eid1407.071538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pozio E, Gomez Morales MÁ. Trichinella and Trichinellosis: from wildlife to the human beings. In: Sing A, editor. Zoonoses: infections affecting humans and animals. Cham: Springer; 2023. pp. 529–544. [Google Scholar]
- 36.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 37.Crowe M, Sheppard L, Campbell A. Reliability analysis for a proposed critical appraisal tool demonstrated value for diverse research designs. J Clin Epidemiol. 2012;65:375–383. doi: 10.1016/j.jclinepi.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 38.Crowe M, Sheppard L. A general critical appraisal tool: an evaluation of construct validity. Int J Nurs Stud. 2011;48:1505–1516. doi: 10.1016/j.ijnurstu.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Lee DL. The biology of nematodes. 1st ed. Boca Raton: CRC Press; 2002.
- 40.Eisenback J. Nematology laboratory investigations morphology and taxonomy. Blacksburg: Mactode Publications; 2003. [Google Scholar]
- 41.Adenophorea MH. In: Encyclopedia of parasitology. Mehlhorn H, editor. Heidelberg: Springer, Berlin; 2008. pp. 49–50. [Google Scholar]
- 42.Bird AF, Bird J. The structure of nematodes. 2. New York: Academic; 2012. [Google Scholar]
- 43.Ravichandra NG. Fundamentals of plant pathology. New Delhi: PHI Learning; 2013.
- 44.Basyoni MM, Rizk EM. Nematodes ultrastructure: complex systems and processes. J Parasit Dis. 2016;40:1130–1140. doi: 10.1007/s12639-015-0707-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schratzberger M, Holterman M, van Oevelen D, Helder J. A Worm’s World: ecological flexibility pays off for free-living nematodes in sediments and soils. Bioscience. 2019;69:867–876. doi: 10.1093/biosci/biz086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nickle WR. Manual of agricultural nematology. 1st ed. Boca Raton: CRC Press; 2020.
- 47.Sheffield HG. Electron microscopy of the bacillary band and stichosome of Trichuris muris and T. vulpis. J Parasitol. 1963;49:998–1009. doi: 10.2307/3275740. [DOI] [PubMed] [Google Scholar]
- 48.Adamson ML. Phylogenetic analysis of the higher classification of the Nematoda. Can J Zool. 1987;65:1478–1482. doi: 10.1139/z87-230. [DOI] [Google Scholar]
- 49.Roberts LS, Janovy J, Schmidt GD. Gerald D. Schmidt & Larry S. Roberts’ Foundations of Parasitology. 8th ed. New York: McGraw-Hill; 2009.
- 50.Pedrassani D, Lux Hoppe EG, Avancini N, do Nascimento AA. Morphology of eggs of Dioctophyme renale Goeze, 1782 (Nematoda: Dioctophymatidae) and influences of temperature on development of first-stage larvae in the eggs. Rev Bras Parasitol Vet. 2009;18:15–9. doi: 10.4322/rbpv.01801003. [DOI] [PubMed] [Google Scholar]
- 51.Chitwood BG, Chitwood MBH. An introduction to nematology. Rev. 1950. Baltimore: Monumental Printing Company; 1950.
- 52.Berman JJ. Chapter 27 - Nematoda (roundworms) In: Berman JJ, editor. Taxonomic guide to infectious diseases. Boston: Academic; 2012. pp. 147–159. [Google Scholar]
- 53.Hugot JP, Quentin JC. Nemacycle: a coding system for representation of nematode life-cycles. Res Rev Parasitol. 1999;60:57–67. [Google Scholar]
- 54.Angelou A, Tsakou K, Mpranditsas K, Sioutas G, Moores DA, Papadopoulos E. Giant kidney worm: novel report of Dioctophyma renale in the kidney of a dog in Greece. Helminthologia. 2020;57:43–48. doi: 10.2478/helm-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DPDx. Trichuriasis (also known as whipworm infection). 2013. https://www.cdc.gov/parasites/whipworm/biology.html. Accessed 26 Oct 2023.
- 56.Tesana S, Puapairoj A, Saeseow O. Granulomatous, hepatolithiasis and hepatomegaly caused by Capillaria hepatica infection: first case report of Thailand. Southeast Asian J Trop Med Public Health. 2007;38:636–640. [PubMed] [Google Scholar]
- 57.Kazemi Aghdam M, Karimi A, Amanati A, Ghoroubi J, Khoddami M, Shamsian BS, et al. Capillaria hepatica, a case report and review of the literatures. Arch Pediatr Infect Dis. 2015;3:e19398. [Google Scholar]
- 58.Fuehrer HP, Igel P, Auer H. Capillaria hepatica in man–an overview of hepatic capillariosis and spurious infections. Parasitol Res. 2011;109:969–979. doi: 10.1007/s00436-011-2494-1. [DOI] [PubMed] [Google Scholar]
- 59.Manor U, Doviner V, Kolodziejek J, Weidinger P, Dagan A, Ben-Haim M, et al. Capillaria hepatica (syn. Calodium hepaticum) as a cause of asymptomatic liver mass. Am J Trop Med Hyg. 2021;105:204–6. doi: 10.4269/ajtmh.21-0120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li CD, Yang HL, Wang Y. Capillaria hepatica in China. World J Gastroenterol. 2010;16:698–702. doi: 10.3748/wjg.v16.i6.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cross JH, Banzon T, Singson C. Further studies on Capillaria philippinensis: development of the parasite in the Mongolian gerbil. J Parasitol. 1978;64:208–213. doi: 10.2307/3279658. [DOI] [PubMed] [Google Scholar]
- 62.Cross JH. Intestinal capillariasis. Clin Microbiol Rev. 1992;5:120–129. doi: 10.1128/CMR.5.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Di Cesare A, Castagna G, Otranto D, Meloni S, Milillo P, Latrofa MS, et al. Molecular detection of Capillaria aerophila, an agent of canine and feline pulmonary capillariosis. J Clin Microbiol. 2012;50:1958–1963. doi: 10.1128/JCM.00103-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.DPDx. Trichinellosis (also known as Trichinosis). 2019. https://www.cdc.gov/parasites/trichinellosis/biology.html. Accessed 26 Oct 2023.
- 65.Spratt DM, Beveridge I, Andrews JR, Dennett X. Haycocknema perplexum n. g., n. sp. (Nematoda: Robertdollfusidae): an intramyofibre parasite in man. Syst Parasitol. 1999;43:123–31. doi: 10.1023/A:1006158218854. [DOI] [PubMed] [Google Scholar]
- 66.Spratt D, Nicholas WL. Morphological evidence for the systematic position of the Order Muspiceida (Nematoda) Trans R Soc S Aust. 2002;126:51–62. [Google Scholar]
- 67.Elhamiani Khatat S, Rosenberg D, Benchekroun G, Polack B. Lungworm Eucoleus aerophilus (Capillaria aerophila) infection in a feline immunodeficiency virus-positive cat in France. JFMS Open Rep. 2016;2:2055116916651649. doi: 10.1177/2055116916651649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stepanović P, Despotović D, Dimitrijević S, Ilić T. Clinical-parasitological screening for respiratory capillariosis in cats in urban environments. Helminthologia. 2020;57:322–334. doi: 10.2478/helm-2020-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fuehrer HP. An overview of the host spectrum and distribution of Calodium hepaticum (syn. Capillaria hepatica): part 2-Mammalia (excluding Muroidea) Parasitol Res. 2014;113:641–51. doi: 10.1007/s00436-013-3692-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borba VH, Machado-Silva JR, Le Bailly M, Iñiguez AM. Worldwide paleodistribution of capillariid parasites: paleoparasitology, current status of phylogeny and taxonomic perspectives. PLoS One. 2019;14:e0216150. doi: 10.1371/journal.pone.0216150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Saichua P, Nithikathkul C, Kaewpitoon N. Human intestinal capillariasis in Thailand. World J Gastroenterol. 2008;14:506–510. doi: 10.3748/wjg.14.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fan Z, Huang Y, Qian S, Lv G, Chen Y, Yang B, et al. Serious diarrhea with weight loss caused by Capillaria philippinensis acquired in China: a case report. BMC Res Notes. 2012;5:554. doi: 10.1186/1756-0500-5-554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dronda F, Chaves F, Sanz A, Lopez-Velez R. Human intestinal capillariasis in an area of nonendemicity: case report and review. Clin Infect Dis. 1993;17:909–912. doi: 10.1093/clinids/17.5.909. [DOI] [PubMed] [Google Scholar]
- 74.el-Karaksy H, el-Shabrawi M, Mohsen N, Kotb M, el-Koofy N, el-Deeb N. Capillaria philippinensis: a cause of fatal diarrhea in one of two infected Egyptian sisters. J Trop Pediatr. 2004;50:57–60. doi: 10.1093/tropej/50.1.57. [DOI] [PubMed] [Google Scholar]
- 75.Abdel Salam N, Hassany SM, Medhat A, Hussein HI, Blum HE. Capillaria philippinensis: a cause of chronic diarrhea in Upper Egypt. JASMR. 2012;7:10–13. [Google Scholar]
- 76.Attia RA, Tolba ME, Yones DA, Bakir HY, Eldeek HE, Kamel S. Capillaria philippinensis in upper Egypt: has it become endemic? Am J Trop Med Hyg. 2012;86:126–133. doi: 10.4269/ajtmh.2012.11-0321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vasantha PL, Girish N, Leela KS. Human intestinal capillariasis: a rare case report from non-endemic area (Andhra Pradesh, India) Indian J Med Microbiol. 2012;30:236–239. doi: 10.4103/0255-0857.96708. [DOI] [PubMed] [Google Scholar]
- 78.Chichino G, Bernuzzi AM, Bruno A, Cevini C, Atzori C, Malfitano A, et al. Intestinal capillariasis (Capillaria philippinensis) acquired in Indonesia: a case report. Am J Trop Med Hyg. 1992;47:10–12. doi: 10.4269/ajtmh.1992.47.10. [DOI] [PubMed] [Google Scholar]
- 79.Nawa Y, Imai JI, Abe T, Kisanuki H, Tsuda K. A case report of intestinal capillariasis - the second case found in Japan. Kisechugaku Zasshi. 1988;37:113–118. [Google Scholar]
- 80.Jung WT, Kim HJ, Min HJ, Ha CY, Kim HJ, Ko GH, et al. An indigenous case of intestinal capillariasis with protein-losing enteropathy in Korea. Korean J Parasitol. 2012;50:333–337. doi: 10.3347/kjp.2012.50.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ha M, Jun DH, Kim JH, Kim YJ, Kwon KA, Park DK, et al. Intestinal capillariasis diagnosed by endoscopic biopsy. Clin Endosc. 2013;46:675–678. doi: 10.5946/ce.2013.46.6.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Soukhathammavong P, Sayasone S, Harimanana AN, Akkhavong A, Thammasack S, Phoumindr N, et al. Three cases of intestinal capillariasis in Lao People’s Democratic Republic. Am J Trop Med Hyg. 2008;79:735–738. doi: 10.4269/ajtmh.2008.79.735. [DOI] [PubMed] [Google Scholar]
- 83.Belizario VY, Jr, Totañes FIG, de Leon WU, Migriño JR, Jr, Macasaet LY. Intestinal capillariasis, western Mindanao, the Philippines. Emerg Infect Dis. 2010;16:736–8. doi: 10.3201/eid1604.080483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Manalo M, Bañez V, Belizario V. A case of chronic diarrhea secondary to Capillaria philippinensis in Occidental Mindoro: possibly a newly-described endemic area? Acta Med Philipp. 2012;46:81–84. doi: 10.47895/amp.v46i3.2107. [DOI] [Google Scholar]
- 85.Hwang KP. Human intestinal capillariasis (Capillaria philippinensis) in Taiwan. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1998;39:82–85. [PubMed] [Google Scholar]
- 86.Lu LH, Lin MR, Choi WM, Hwang KP, Hsu YH, Bair MJ, et al. Human intestinal capillariasis (Capillaria philippinensis) in Taiwan. Am J Trop Med Hyg. 2006;74:810–813. doi: 10.4269/ajtmh.2006.74.810. [DOI] [PubMed] [Google Scholar]
- 87.Sadaow L, Sanpool O, Intapan PM, Sukeepaisarnjaroen W, Prasongdee TK, Maleewong W. A hospital-based study of intestinal capillariasis in thailand: clinical features, potential clues for diagnosis, and epidemiological characteristics of 85 patients. Am J Trop Med Hyg. 2018;98:27–31. doi: 10.4269/ajtmh.17-0465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Thewjitcharoen Y, Medhajirapat S, Sanprasert V, Saksirisampant W, Nuchprayoon S. A fatal case of intestinal capillariasis due to misleading investigations. Asian Biomed. 2017;6:781–785. [Google Scholar]
- 89.Limsrivilai J, Pongprasobchai S, Apisarnthanarak P, Manatsathit S. Intestinal capillariasis in the 21st century: clinical presentations and role of endoscopy and imaging. BMC Gastroenterol. 2014;14:207. doi: 10.1186/s12876-014-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vos LJ, Robertson T, Binotto E. Haycocknema perplexum: an emerging cause of parasitic myositis in Australia. Commun Dis Intell Q Rep. 2016;40:E496–E499. [PubMed] [Google Scholar]
- 91.Nezri M, Ruer J, De Bruyne A, Cohen-Valensi R, Pozio E, Dupouy-Camet J. First report of a human case of trichinellosis due to T richinella britovi after jackal (C anis aureus) meat consumption in Algeria. Bull Soc Pathol Exot. 2006;99:94–95. [PubMed] [Google Scholar]
- 92.Petkova S, Mihov L, Vutova K, Tsenov I, La Rosa G, Pozio E. Epidemiological and clinical patterns of trichinellosis in Bulgaria from 1995 to 2002. Parasite. 2008;15:86–88. doi: 10.1051/parasite/2008151086. [DOI] [PubMed] [Google Scholar]
- 93.Vutova K, Velev V, Chipeva R, Yancheva N, Petkova S, Tomov T, et al. Clinical and epidemiological descriptions from trichinellosis outbreaks in Bulgaria. Exp Parasitol. 2020;212:107874. doi: 10.1016/j.exppara.2020.107874. [DOI] [PubMed] [Google Scholar]
- 94.Gari-Toussaint M, Tieulié N, Baldin J, Dupouy-Camet J, Delaunay P, Fuzibet JG, et al. Human trichinellosis due to Trichinella britovi in southern France after consumption of frozen wild boar meat. Euro Surveill. 2005;10:117–118. doi: 10.2807/esm.10.06.00550-en. [DOI] [PubMed] [Google Scholar]
- 95.Dimzas D, Diakou A, Koutras C, Gómez Morales MA, Psalla D, Keryttopoulos P, et al. Human trichinellosis caused by Trichinella britovi in Greece, and literature review. J Helminthol. 2019;94:e33. doi: 10.1017/S0022149X19000075. [DOI] [PubMed] [Google Scholar]
- 96.Stroffolini G, Rossi L, Faraoni S, Calcagno A, Bonora S, Perri GD, et al. Trichinella britovi outbreak in north-west Italy, 2019–2020: beware of wild boar. Int J Infect Dis. 2022;116:S77–S78. doi: 10.1016/j.ijid.2021.12.183. [DOI] [PubMed] [Google Scholar]
- 97.Troiano G, Nante N. Human trichinellosis in Italy: an epidemiological review since 1989. J Prev Med Hyg. 2019;60:E71–E75. doi: 10.15167/2421-4248/jpmh2019.60.2.891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dmitric M, Debeljak Z, Vidanovic D, Sekler M, Vaskovic N, Matovic K, et al. Trichinella britovi in game meat linked to human trichinellosis outbreak in Serbia. J Parasitol. 2018;104:557–559. doi: 10.1645/18-42. [DOI] [PubMed] [Google Scholar]
- 99.Dubinský P, Antolová D, Reiterová K. Human trichinella infection outbreaks in Slovakia, 1980–2008. Acta Parasitol. 2016;61:205–211. doi: 10.1515/ap-2016-0029. [DOI] [PubMed] [Google Scholar]
- 100.Rodríguez-Osorio M, Gómez-Garcia V, Benito R, Gil J. Trichinella britovi human infection in Spain: antibody response to surface, excretory/secretory and somatic antigens. Parasite. 2003;10:159–164. doi: 10.1051/parasite/2003102159. [DOI] [PubMed] [Google Scholar]
- 101.Gallardo MT, Mateos L, Artieda J, Wesslen L, Ruiz C, García MA, et al. Outbreak of trichinellosis in Spain and Sweden due to consumption of wild boar meat contaminated with Trichinella britovi. Euro Surveill. 2007;12:E070315.070311. doi: 10.2807/esw.12.11.03154-en. [DOI] [PubMed] [Google Scholar]
- 102.Akkoc N, Kuruuzum Z, Akar S, Yuce A, Onen F, Yapar N, et al. A large-scale outbreak of trichinellosis caused by Trichinella britovi in Turkey. Zoonoses Public Health. 2009;56:65–70. doi: 10.1111/j.1863-2378.2008.01158.x. [DOI] [PubMed] [Google Scholar]
- 103.Ancelle T, Dupouy-Camet J, Bougnoux ME, Fourestie V, Petit H, Mougeot G, et al. Two outbreaks of trichinosis caused by horsemeat in France in 1985. Am J Epidemiol. 1988;127:1302–1311. doi: 10.1093/oxfordjournals.aje.a114923. [DOI] [PubMed] [Google Scholar]
- 104.Dalcin D, Zarlenga DS, Larter NC, Hoberg E, Boucher DA, Merrifield S, et al. Trichinella Nativaoutbreak with rare thrombotic complications associated with meat from a black bear hunted in northern Ontario. Clin Infect Dis. 2017;64:1367–1373. doi: 10.1093/cid/cix165. [DOI] [PubMed] [Google Scholar]
- 105.Schellenberg RS, Tan BJ, Irvine JD, Stockdale DR, Gajadhar AA, Serhir B, et al. An outbreak of trichinellosis due to consumption of bear meat infected with Trichinella nativa, in 2 northern Saskatchewan communities. J Infect Dis. 2003;188:835–843. doi: 10.1086/378094. [DOI] [PubMed] [Google Scholar]
- 106.Cui J, Wang ZQ. Outbreaks of human trichinellosis caused by consumption of dog meat in China. Parasite. 2001;8:S74–S77. doi: 10.1051/parasite/200108s2074. [DOI] [PubMed] [Google Scholar]
- 107.Dworkin MS, Gamble HR, Zarlenga DS, Tennican PO. Outbreak of trichinellosis associated with eating cougar jerky. J Infect Dis. 1996;174:663–666. doi: 10.1093/infdis/174.3.663. [DOI] [PubMed] [Google Scholar]
- 108.Pozio E. Taxonomy of Trichinella and the epidemiology of infection in the Southeast Asia and Australian regions. Southeast Asian J Trop Med Public Health. 2001;32:129–132. [PubMed] [Google Scholar]
- 109.Caron Y, Bory S, Pluot M, Nheb M, Chan S, Prum SH, et al. Human outbreak of trichinellosis caused by Trichinella papuae nematodes, central Kampong Thom province. Cambodia Emerg Infect Dis. 2020;26:1759–1766. doi: 10.3201/eid2608.191497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Intapan PM, Chotmongkol V, Tantrawatpan C, Sanpool O, Morakote N, Maleewong W. Molecular identification of Trichinella papuae from a Thai patient with imported trichinellosis. Am J Trop Med Hyg. 2011;84:994–997. doi: 10.4269/ajtmh.2011.10-0675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kusolsuk T, Kamonrattanakun S, Wesanonthawech A, Dekumyoy P, Thaenkham U, Yoonuan T, et al. The second outbreak of trichinellosis caused by Trichinella papuae in Thailand. Trans R Soc Trop Med Hyg. 2010;104:433–437. doi: 10.1016/j.trstmh.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 112.Khumjui C, Choomkasien P, Dekumyoy P, Kusolsuk T, Kongkaew W, Chalamaat M, et al. Outbreak of trichinellosis caused by Trichinella papuae, Thailand, 2006. Emerg Infect Dis. 2008;14:1913–1915. doi: 10.3201/eid1412.080800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ranque S, Faugère B, Pozio E, La Rosa G, Tamburrini A, Pellissier JF, et al. Trichinella pseudospiralis outbreak in France. Emerg Infect Dis. 2000;6:543–547. doi: 10.3201/eid0605.000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gómez-Morales MA, Mazzarello G, Bondi E, Arenare L, Bisso MC, Ludovisi A, et al. Second outbreak of Trichinella pseudospiralis in Europe: clinical patterns, epidemiological investigation and identification of the etiological agent based on the western blot patterns of the patients’ serum. Zoonoses Public Health. 2021;68:29–37. doi: 10.1111/zph.12761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Britov VA. Trichinellosis in Kamchatka. Wiad Parazytol. 1997;43:287–288. [Google Scholar]
- 116.Andrews JR, Bandi C, Pozio E, Gomez Morales MA, Ainsworth R, Abernethy D. Identification of Trichinella pseudospiralis from a human case using random amplified polymorphic DNA. Am J Trop Med Hyg. 1995;53:185–188. doi: 10.4269/ajtmh.1995.53.185. [DOI] [PubMed] [Google Scholar]
- 117.Jongwutiwes S, Chantachum N, Kraivichian P, Siriyasatien P, Putaporntip C, Tamburrini A, et al. First outbreak of human trichinellosis caused by Trichinella pseudospiralis. Clin Infect Dis. 1998;26:111–115. doi: 10.1086/516278. [DOI] [PubMed] [Google Scholar]
- 118.Lechner A, Kraus J, Hoppe UC, Glawischnig W, Auer H, Allerberger F. Outbreak of human trichinellosis, Austria 2010. Vet Med Austria. 2012;99:20–23. [Google Scholar]
- 119.Scientific Panel on Biological Hazards (BIOHAZ), European Food Safety Authority (EFSA). Opinion of the Scientific Panel on biological hazards (BIOHAZ) on "the suitability and details of freezing methods to allow human consumption of meat infected with Trichinella or Cysticercus". EFSA Journal. 2004;142:1–50.
- 120.Newman A. Investigation of a human case of trichinellosis on a farm in southwest Ontario. Environ Health Rev. 2014;57:93–96. doi: 10.5864/d2014-029. [DOI] [Google Scholar]
- 121.García E, Mora L, Torres P, Jercic MI, Mercado R. First record of human trichinosis in Chile associated with consumption of wild boar (Sus scrofa) Mem Inst Oswaldo Cruz. 2005;100:17–18. doi: 10.1590/S0074-02762005000100003. [DOI] [PubMed] [Google Scholar]
- 122.Cvitković A, Miletić-Medved M, Gjenero-Margan I. An epidemic of trichinellosis in autumn 2004 in Slavonski Brod. Acta Med Croatica. 2007;61:215–218. [PubMed] [Google Scholar]
- 123.European Centre for Disease Prevention and Control. Trichinellosis. In: ECDC. Annual epidemiological report for 2019. Stockholm: ECDC; 2022.
- 124.Sayed ASM, Hussein AAA, Arafa MI, Abdo BRN. Epidemiological study on trichinellosis in pigs and man in upper Egypt. Assiut Vet Med J. 2010;56:1–8. [Google Scholar]
- 125.Lassen B, Janson M, Viltrop A, Neare K, Hütt P, Golovljova I, et al. Serological evidence of exposure to globally relevant zoonotic parasites in the estonian population. PLoS One. 2016;11:e0164142. doi: 10.1371/journal.pone.0164142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Melese A, Mohammed M, Ketema W, Toma A. A case of trichinellosis in a 14-year-old male child at Hawassa University Comprehensive Specialized Hospital, Hawassa, Sidama, Ethiopia. Case Rep Infect Dis. 2021;2021:3624687. doi: 10.1155/2021/3624687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Barruet R, Devez A, Dupouy-Camet J, Karadjian G, Plavsa D, Chydériotis G, et al. A common source for a trichinellosis outbreak reported in France and Serbia in 2017. Euro Surveill. 2020;25:1900527. doi: 10.2807/1560-7917.ES.2020.25.24.1900527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pun KK, Wong WT, Wong PH. The first documented outbreak of trichinellosis in Hong Kong Chinese. Am J Trop Med Hyg. 1983;32:772–775. doi: 10.4269/ajtmh.1983.32.772. [DOI] [PubMed] [Google Scholar]
- 129.Glatz K, Danka J, Kucsera I, Pozio E. Human trichinellosis in Hungary from 1965 to 2009. Parasite. 2010;17:193–198. doi: 10.1051/parasite/2010173193. [DOI] [PubMed] [Google Scholar]
- 130.Sharma RK, Raghavendra N, Mohanty S, Tripathi BK, Gupta B, Goel A. Clinical & biochemical profile of trichinellosis outbreak in north India. Indian J Med Res. 2014;140:414–419. [PMC free article] [PubMed] [Google Scholar]
- 131.Chomel BB, Kasten R, Adams C, Lambillotte D, Theis J, Goldsmith R, et al. Serosurvey of some major zoonotic infections in children and teenagers in Bali, Indonesia. Southeast Asian J Trop Med Public Health. 1993;24:321–326. [PubMed] [Google Scholar]
- 132.Kim G, Choi MH, Kim JH, Kang YM, Jeon HJ, Jung Y, et al. An outbreak of trichinellosis with detection of Trichinella larvae in leftover wild boar meat. J Korean Med Sci. 2011;26:1630–1633. doi: 10.3346/jkms.2011.26.12.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sohn WM, Kim HM, Chung DI, Yee ST. The first human case of Trichinella spiralis infection in Korea. Korean J Parasitol. 2000;38:111–115. doi: 10.3347/kjp.2000.38.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Barennes H, Sayasone S, Odermatt P, De Bruyne A, Hongsakhone S, Newton PN, et al. A major trichinellosis outbreak suggesting a high endemicity of Trichinella infection in northern Laos. Am J Trop Med Hyg. 2008;78:40–44. doi: 10.4269/ajtmh.2008.78.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Haim M, Efrat M, Wilson M, Schantz PM, Cohen D, Shemer J. An outbreak of Trichinella spiralis infection in southern Lebanon. Epidemiol Infect. 1997;119:357–362. doi: 10.1017/S0950268897007875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chapa-Ruiz MR, González-Pantaleón D, Morales-Galán A, Contreras-Ramos A, Salinas-Tobón MR, Martínez YZ. A follow-up study of the human class and subclass antibody response developed against the adult stage of Trichinella spiralis. Parasite. 2001;8(Suppl 2):S163–S167. doi: 10.1051/parasite/200108s2163. [DOI] [PubMed] [Google Scholar]
- 137.Richardson EKB. Aspects of Trichinella spiralis in New Zealand: a thesis presented in partial fulfilment of the requirements for the degree of Master of Veterinary Studies in Epidemiology at Massey University. Palmerston North: Massey University; 2006.
- 138.Różycki M, Korpysa-Dzirba W, Bełcik A, Pelec T, Mazurek J, Cencek T. Analysis of a trichinellosis outbreak in Poland after consumption of sausage made of wild boar meat. J Clin Med. 2022;11:485. doi: 10.3390/jcm11030485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Reiterová K, Kinceková J, Snábel V, Marucci G, Pozio E, Dubinský P. Trichinella spiralis-outbreak in the Slovak Republic. Infection. 2007;35:89–93. doi: 10.1007/s15010-007-6122-z. [DOI] [PubMed] [Google Scholar]
- 140.Kaewpitoon N, Kaewpitoon SJ, Philasri C, Leksomboon R, Maneenin C, Sirilaph S, et al. Trichinosis: epidemiology in Thailand. World J Gastroenterol. 2006;12:6440–6445. doi: 10.3748/wjg.v12.i40.6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.McAuley JB, Michelson MK, Hightower AW, Engeran S, Wintermeyer LA, Schantz PM. A trichinosis outbreak among Southeast Asian refugees. Am J Epidemiol. 1992;135:1404–1410. doi: 10.1093/oxfordjournals.aje.a116251. [DOI] [PubMed] [Google Scholar]
- 142.Van De N, Thi Nga V, Dorny P, Vu Trung N, Ngoc Minh P, Trung Dung D, et al. Trichinellosis in Vietnam. Am J Trop Med Hyg. 2015;92:1265–1270. doi: 10.4269/ajtmh.14-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nguyen TH, Nguyen THL, Nguyen THN, Le THH, Tranh D. Human trichinosis in rural area mountainous provinces in Vietnam in 2015–2016. Glob J Infect Dis Clin Res. 2017;3:9–14. doi: 10.17352/2455-5363.000012. [DOI] [Google Scholar]
- 144.Tada K, Suzuki H, Sato Y, Morishima Y, Nagano I, Ishioka H, et al. Outbreak of Trichinella T9 infections associated with consumption of bear meat. Japan Emerg Infect Dis. 2018;24:1532–1535. doi: 10.3201/eid2408.172117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ribicich M, Gamble HR, Rosa A, Bolpe J, Franco A. Trichinellosis in Argentina: an historical review. Vet Parasitol. 2005;132:137–142. doi: 10.1016/j.vetpar.2005.05.042. [DOI] [PubMed] [Google Scholar]
- 146.Despotović D, Nenadović K, Sladojević Ž, Dimitrijević S, Ilić T. Epidemiology and risk factors of trichinellosis in Bosnia and Herzegovina from 1961 to 2021. Parasitol Res. 2023;122:635–643. doi: 10.1007/s00436-022-07767-2. [DOI] [PubMed] [Google Scholar]
- 147.Pozio E. World distribution of Trichinella spp. infections in animals and humans. Vet Parasitol. 2007;149:3–21. doi: 10.1016/j.vetpar.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 148.Zhang XZ, Wang ZQ, Cui J. Epidemiology of trichinellosis in the People’s Republic of China during 2009–2020. Acta Trop. 2022;229:106388. doi: 10.1016/j.actatropica.2022.106388. [DOI] [PubMed] [Google Scholar]
- 149.Murrell KD, Pozio E. Worldwide occurrence and impact of human trichinellosis, 1986–2009. Emerg Infect Dis. 2011;17:2194–2202. doi: 10.3201/eid1712.110896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ivanov KS, Antonov VS, Knysh GG, Khadzhaeva AN, Antykova LP, Lavrova VP, et al. The clinical characteristics of 2 outbreaks of trichinelliasis. Med Parazitol (Mosk) 1990;4:41–42. [PubMed] [Google Scholar]
- 151.Møller LN, Koch A, Petersen E, Hjuler T, Kapel CM, Andersen A, et al. Trichinella infection in a hunting community in East Greenland. Epidemiol Infect. 2010;138:1252–1256. doi: 10.1017/S0950268810000282. [DOI] [PubMed] [Google Scholar]
- 152.Kia E, Meamar A, Zahabiun F, Soodbaksh A, Kordbacheh P. An outbreak of human trichinellosis due to consumption of boar meat infected with Trichinella sp. Iran J Infect Dis Trop Med. 2008;41:35–38. [Google Scholar]
- 153.Food Safety Authority of Ireland. Survey on the prevalence of Trichinella in pigs in local authority supervised slaughterhouses. In: Monitoring & surveillance series. Dublin: Food Safety Authority of Ireland; 2010. p. 1–40.
- 154.Hefer E, Rishpon S, Volovik I. Trichinosis outbreak among Thai immigrant workers in the Hadera sub-district. Harefuah. 2004;143:656–60, 694. [PubMed] [Google Scholar]
- 155.Marva E, Markovics A, Gdalevich M, Asor N, Sadik C, Leventhal A. Trichinellosis outbreak. Emerg Infect Dis. 2005;11:1979–1981. doi: 10.3201/eid1112.050461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Conlan JV, Vongxay K, Khamlome B, Gomez-Morales MA, Pozio E, Blacksell SD, et al. Patterns and risks of trichinella infection in humans and pigs in northern Laos. PLoS Negl Trop Dis. 2014;8:e3034. doi: 10.1371/journal.pntd.0003034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Caplinskas S, Bartuliene A, Zagrebneviene G. Human trichinellosis: epidemiological situation in Lithuania, 2008–2017. Immunochem Immunopathol. 2018;4:130. doi: 10.4172/2469-9756.1000130. [DOI] [Google Scholar]
- 158.Pinelli E, Mommers M, Homan W, van Maanen T, Kortbeek LM. Imported human trichinellosis: sequential IgG4 antibody response to Trichinella spiralis. Eur J Clin Microbiol Infect Dis. 2004;23:57–60. doi: 10.1007/s10096-003-1039-7. [DOI] [PubMed] [Google Scholar]
- 159.Ozeretskovskaya NN, Mikhailova LG, Sabgaida TP, Dovgalev AS. New trends and clinical patterns of human trichinellosis in Russia at the beginning of the XXI century. Vet Parasitol. 2005;132:167–171. doi: 10.1016/j.vetpar.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 160.Lipilkina T, Popov I, Lipilkin P, Ermakov A. Trichinosis in the Rostov oblast. IOP Conf Ser Earth Environ Sci. 2021;937:022013. doi: 10.1088/1755-1315/937/2/022013. [DOI] [Google Scholar]
- 161.Dupouy-Camet J, Murrell KD. FAO/WHO/OIE guidelines for the surveillance, management, prevention and control of trichinellosis. Rome: Food & Agriculture Organization; 2007.
- 162.Lo YC, Hung CC, Lai CS, Wu Z, Nagano I, Maeda T, et al. Human trichinosis after consumption of soft-shelled turtles, Taiwan. Emerg Infect Dis. 2009;15:2056–2058. doi: 10.3201/eid1512.090619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Akimov I, Didyk Y. Trichinellosis of wild animals in Ukraine and its danger to the public. Zoodiversity. 2020;54:411–418. doi: 10.15407/zoo2020.05.411. [DOI] [Google Scholar]
- 164.Mohamed SA, El Nahla S, Hosni KS. World wide epidemiology of helminths infection. In: Luis R, editor. Human helminthiasis. Rijeka: Intech Open; 2017. pp. 1–16. [Google Scholar]
- 165.Pullan RL, Brooker SJ. The global limits and population at risk of soil-transmitted helminth infections in 2010. Parasit Vectors. 2012;5:81. doi: 10.1186/1756-3305-5-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Eiras J, Zhu XQ, Yurlova N, Pedrassani D, Yoshikawa M, Nawa Y. Dioctophyme renale (Goeze, 1782) (Nematoda, Dioctophymidae) parasitic in mammals other than humans: a comprehensive review. Parasitol Int. 2021;81:102269. doi: 10.1016/j.parint.2020.102269. [DOI] [PubMed] [Google Scholar]
- 167.Russo ZH, Callirgos JC, García-Ayachi A, Wetzel EJ. Review of Dioctophyme renale: etiology, morphology, biology, ecoepidemiology, pathogenesis, symptomatology, diagnosis, treatment, and prevention. J Parasitol. 2022;108(2):180–191. doi: 10.1645/21-65. [DOI] [PubMed] [Google Scholar]
- 168.Jairajpuri MS. Parasite diversity with specific reference to nematodes. J Parasit Dis. 2005;29:81–84. [Google Scholar]
- 169.Norouzi R, Manochehri A, Hanifi M. A case report of human infection with Dioctophyma Renale from Iran. Urol J. 2017;14:3043–3045. [PubMed] [Google Scholar]
- 170.Katafigiotis I, Fragkiadis E, Pournaras C, Nonni A, Stravodimos KG. A rare case of a 39 year old male with a parasite called Dioctophyma renale mimicking renal cancer at the computed tomography of the right kidney. A case report. Parasitol Int. 2013;62:459–460. doi: 10.1016/j.parint.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 171.Gu Y, Li G, Zhang J, Zhang Y. Dioctophyma renale infection masquerading as a malignancy. Kidney Int. 2012;82:1342. doi: 10.1038/ki.2012.315. [DOI] [PubMed] [Google Scholar]
- 172.WHO. World Health Organization and partners unveil new coordinated approach to treat millions suffering from neglected tropical diseases. 2006. https://apps.who.int/mediacentre/news/releases/2006/pr60/en/index1.html. Accessed 26 Oct 2023.
- 173.Bansal R, Huang T, Chun S. Trichuriasis. Am J Med Sci. 2018;355:e3. doi: 10.1016/j.amjms.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 174.Borba V, Enoki M, Lopes-Torres EJ, Machado-Silva JR, Iñiguez AM. New data on eggshell structure of capillariid species: a SEM perspective. Parasitol Res. 2021;120:963–970. doi: 10.1007/s00436-020-07032-4. [DOI] [PubMed] [Google Scholar]
- 175.Borba VH, Martin C, Machado-Silva JR, Xavier SCC, de Mello FL, Iñiguez AM. Machine learning approach to support taxonomic species discrimination based on helminth collections data. Parasit Vectors. 2021;14:230. doi: 10.1186/s13071-021-04721-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Fuehrer HP. An overview of the host spectrum and distribution of Calodium hepaticum (syn. Capillaria hepatica): part 1-Muroidea. Parasitol Res. 2014;113:619–40. doi: 10.1007/s00436-013-3691-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Gonçalves AQ, Ascaso C, Santos I, Serra PT, Julião GR, Orlandi PP. Calodium hepaticum: household clustering transmission and the finding of a source of human spurious infection in a community of the Amazon region. PLoS Negl Trop Dis. 2012;6:e1943. doi: 10.1371/journal.pntd.0001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wang L, Zhang Y, Deng Y, Li X, Zheng X, Wang F, et al. Clinical and laboratory characterizations of hepatic capillariasis. Acta Trop. 2019;193:206–210. doi: 10.1016/j.actatropica.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 179.Chitwood M, Valesquez C, Salazar N. Physiological changes in a species of Capillaria (Trichuroidea) causing a fatal case of human intestinal capillariasis. Proc 1st Int Congr Parasit. 1964;2:797–8. [Google Scholar]
- 180.Pradatsundarasar A, Pecharanónd K, Chintanawóngs C, Ungthavórn P. The first case of intestinal capillariasis in Thailand. Southeast Asian J Trop Med Public Health. 1973;4:131–134. [PubMed] [Google Scholar]
- 181.Traversa D, Di Cesare A, Conboy G. Canine and feline cardiopulmonary parasitic nematodes in Europe: emerging and underestimated. Parasit Vectors. 2010;3:62. doi: 10.1186/1756-3305-3-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Aftandelians R, Raafat F, Taffazoli M, Beaver PC. Pulmonary capillariasis in a child in Iran. Am J Trop Med Hyg. 1977;26(1):64–71. doi: 10.4269/ajtmh.1977.26.64. [DOI] [PubMed] [Google Scholar]
- 183.Lalosević D, Lalosević V, Klem I, Stanojev-Jovanović D, Pozio E. Pulmonary capillariasis miming bronchial carcinoma. Am J Trop Med Hyg. 2008;78:14–16. doi: 10.4269/ajtmh.2008.78.14. [DOI] [PubMed] [Google Scholar]
- 184.Samorek-Pieróg M, Cencek T, Łabuć E, Pac-Sosińska M, Pieróg M, Korpysa-Dzirba W, et al. Occurrence of Eucoleus aerophilus in wild and domestic animals: a systematic review and meta-analysis. Parasit Vectors. 2023;16:245. doi: 10.1186/s13071-023-05830-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Nithikathkul C, Saichua P, Royal L, Cross JH. Capillariosis. In: Palmer SR, Soulsby L, Torgerson P, Brown DWG, editors. Oxford textbook of zoonoses: biology, clinical practice, and public health control. Oxford: Oxford University Press; 2011. pp. 727–737. [Google Scholar]
- 186.Crisóstomo-Jorquera V, Landaeta-Aqueveque C. The genus Trichinella and its presence in wildlife worldwide: a review. Transbound Emerg Dis. 2022;69:e1269–e1279. doi: 10.1111/tbed.14554. [DOI] [PubMed] [Google Scholar]
- 187.Bruschi F, Murrell KD. New aspects of human trichinellosis: the impact of new Trichinella species. Postgrad Med J. 2002;78:15–22. doi: 10.1136/pmj.78.915.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Pozio E, Zarlenga DS. Recent advances on the taxonomy, systematics and epidemiology of Trichinella. Int J Parasitol. 2005;35:1191–1204. doi: 10.1016/j.ijpara.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 189.Pozio E, Owen IL, La Rosa G, Sacchi L, Rossi P, Corona S. Trichinella papuae n. sp. (Nematoda), a new non-encapsulated species from domestic and sylvatic swine of Papua New Guinea. Int J Parasitol. 1999;29:1825–39. doi: 10.1016/S0020-7519(99)00135-6. [DOI] [PubMed] [Google Scholar]
- 190.Rawla P, Sharma S. Trichinella Spiralis. Treasure Island: StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 191.McKelvie P, Reardon K, Bond K, Spratt DM, Gangell A, Zochling J, et al. A further patient with parasitic myositis due to Haycocknema perplexum, a rare entity. J Clin Neurosci. 2013;20:1019–1022. doi: 10.1016/j.jocn.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 192.DPDx. Capillariasis - Biology - Life Cycle of Capillaria philippinensis. 2020. https://www.cdc.gov/parasites/capillaria/biology_c_philippinensis.html. Accessed 26 Oct 2023.
- 193.Gamble HR, Bessonov AS, Cuperlovic K, Gajadhar AA, van Knapen F, Noeckler K, et al. International Commission on Trichinellosis: recommendations on methods for the control of Trichinella in domestic and wild animals intended for human consumption. Vet Parasitol. 2000;93:393–408. doi: 10.1016/S0304-4017(00)00354-X. [DOI] [PubMed] [Google Scholar]
- 194.Pozio E. Adaptation of Trichinella spp. for survival in cold climates. Food Waterborne Parasitol. 2016;4:4–12. doi: 10.1016/j.fawpar.2016.07.001. [DOI] [Google Scholar]
- 195.Marocco C, Bangert M, Joseph SA, Fitzpatrick C, Montresor A. Preventive chemotherapy in one year reduces by over 80% the number of individuals with soil-transmitted helminthiases causing morbidity: results from meta-analysis. Trans R Soc Trop Med Hyg. 2017;111:12–17. doi: 10.1093/trstmh/trx011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Bah YM, Bah MS, Paye J, Conteh A, Saffa S, Tia A, et al. Soil-transmitted helminth infection in school age children in Sierra Leone after a decade of preventive chemotherapy interventions. Infect Dis Poverty. 2019;8:41. doi: 10.1186/s40249-019-0553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Shumbej T, Menu S, Girum T, Bekele F, Gebru T, Worku M, et al. Impact of annual preventive mass chemotherapy for soil-transmitted helminths among primary school children in an endemic area of Gurage zone: a prospective cross-sectional study. Res Rep Trop Med. 2019;10:109–118. doi: 10.2147/RRTM.S208473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.WHO. Guidelines approved by the Guidelines Review Committee. In: Guideline: preventive chemotherapy to control soil-transmitted helminth infections in at-risk population groups. Geneva: World Health Organization; 2017. [PubMed]
- 199.Else KJ, Keiser J, Holland CV, Grencis RK, Sattelle DB, Fujiwara RT, et al. Whipworm and roundworm infections. Nat Rev Dis Primers. 2020;6:44. doi: 10.1038/s41572-020-0171-3. [DOI] [PubMed] [Google Scholar]
- 200.Vaz Nery S, Pickering AJ, Abate E, Asmare A, Barrett L, Benjamin-Chung J, et al. The role of water, sanitation and hygiene interventions in reducing soil-transmitted helminths: interpreting the evidence and identifying next steps. Parasit Vectors. 2019;12:273. doi: 10.1186/s13071-019-3532-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Bartram J, Cairncross S. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med. 2010;7:e1000367. doi: 10.1371/journal.pmed.1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Di Cesare A, Morelli S, Morganti G, Simonato G, Veronesi F, Colombo M, et al. Efficacy of milbemycin oxime/afoxolaner chewable tablets (NEXGARD SPECTRA®) against Capillaria aerophila and Capillaria boehmi in naturally infected dogs. Parasit Vectors. 2021;14:143. doi: 10.1186/s13071-021-04648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Bowman DD, Hendrix CM, Lindsay DS, Barr SC. Feline clinical parasitology. Ames: Iowa State University Press; 2002. pp. 338–339. [Google Scholar]
- 204.Morelli S, Diakou A, Colombo M, Di Cesare A, Barlaam A, Dimzas D, et al. Cat respiratory nematodes: current knowledge, novel data and warranted studies on clinical features, treatment and control. Pathogens. 2021;10:454. doi: 10.3390/pathogens10040454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Tang B, Li J, Li T, Xie Y, Guan W, Zhao Y, et al. Vaccines as a strategy to control trichinellosis. Front Microbiol. 2022;13:857786. doi: 10.3389/fmicb.2022.857786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Vargová M, Hurníková Z, Revajová V, Lauková A, Dvorožňáková E. Probiotic bacteria can modulate murine macrophage’s superoxide production in Trichinella spiralis infection. Helminthologia. 2020;57:226–234. doi: 10.2478/helm-2020-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Boros Z, Băieș MH, Vodnar DC, Gherman CM, Borșan SD, Cozma-Petruț A, et al. Antiparasitic action of Lactobacillus casei ATCC 393 and Lactobacillus paracasei CNCM strains in CD-1 mice experimentally infected with Trichinella britovi. Pathogens. 2022;11:296. doi: 10.3390/pathogens11030296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Partridge FA, Murphy EA, Willis NJ, Bataille CJ, Forman R, Heyer-Chauhan N, et al. Dihydrobenz[e][1,4]oxazepin-2(3H)-ones, a new anthelmintic chemotype immobilising whipworm and reducing infectivity in vivo. PLoS Negl Trop Dis. 2017;11:e0005359. doi: 10.1371/journal.pntd.0005359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during this study are available from the corresponding author upon reasonable request.