The dominant factor contributing to the relatively poor prognosis for colorectal cancer is the advanced stage of the disease at the time of initial presentation: up to a third of patients have locally advanced or metastatic disease, which precludes surgical cure. Even in the patients who undergo apparently curative resection, almost half die within five years.
In the west of Scotland, for example, about a third of 1842 patients presenting with colorectal cancer to seven hospitals between 1991 and 1994 presented as emergencies. Potentially curative resection was achieved in about 70% of patients presenting electively; the curative resection rate was lower in those presenting as emergencies. Five per cent of patients admitted for elective surgery and 13% of those admitted as emergencies died. Almost 60% of elective patients survived two years, compared with 44% of patients admitted as emergencies. These results are typical of population based studies in the United Kingdom.
Variation among surgeons
Most surgeons acknowledge that the incidence of postoperative complications varies widely among individual surgeons. It is now almost 20 years since Fielding and his colleagues in the large bowel cancer project drew attention to differences in anastomotic leak and local recurrence rates after resection for large bowel cancer.
Variation in outcome, by surgeon, after curative resection (n=338)
| Overall rate (%) | Range among surgeons (%) | |
| Anastomotic leak | 9 | 0-25 |
| Local recurrence | 11 | 0-21 |
| Postoperative mortality | 6 | 0-20 |
| Survival (10 years) | 41 | 20-63 |
Data are from the original Glasgow Royal Infirmary study (McArdle et al, BMJ 1991;302:1501-5)
In the original Glasgow Royal Infirmary study, which was conducted in the 1980s, similar differences in postoperative morbidity and mortality were noted. Furthermore, after apparently curative resection, survival at 10 years varied threefold among surgeons.
Presentation, type of surgery, and postoperative mortality, by hospital and surgeon (n=1842), west of Scotland study. Values are percentages
| All(mean) | Hospital(range) | Surgeon(range) | |
| Emergency admission | 33 | 24-41 | 10-50 |
| Dukes's classification A or B | 49 | 43-56 | 29-68 |
| Curative resection | 68 | 63-75 | 45-82 |
| Palliative resection | 25 | 15-29 | 11-48 |
| Postoperative mortality: | |||
| Elective | 5 | 0-7 | 0-17 |
| Emergency | 13 | 9-24 | 4-38 |
One might argue that these are historical data and therefore bear little relevance to the current situation. In the current west of Scotland study, however, although overall 33% of patients presented as emergencies, the proportion varied among hospitals from 24% to 41% and among surgeons from 10% to 50%.
Similarly, the proportion of patients undergoing curative resection varied among surgeons from 45% to 82%; postoperative mortality, in patients presenting electively, also varied, from 0% to 17%. Several out of the 16 surgeons studied performed less well than their colleagues.
Influences, apart from surgeon's skill, on immediate and long term outcome of colorectal surgery
Case mix
Non-specialist surgeons tend to have a high proportion of elderly patients, often with concomitant disease, who present as emergencies with advanced lesions; specialist surgeons may have fewer emergencies, with most patients being younger, fitter, and with less advanced disease
Surgical philosophy
Faced with the same problem, an aggressive surgeon might undertake radical surgery, thereby risking technical complications, in an attempt to improve quality and duration of life, whereas a conservative surgeon might opt for limited surgery, thereby minimising the risk of postoperative complications (but in doing so, he or she may compromise long term survival)
Assessment of cure
The decision on whether a resection is curative or palliative is often based on the surgeon's subjective impression at the time of laparotomy. In patients in whom the adequacy of resection was borderline an optimistic surgeon might believe a cure had been achieved, whereas a more pessimistic surgeon might believe that only palliation had been achieved
Quality of pathological reporting
Limited sampling might suggest that the lymph nodes and the lateral resection margins were clear of tumour, whereas more rigorous sampling might show the presence of more extensive disease. The resultant pathological stage migration might therefore alter expectation of outcome and lead to in inappropriate interpretation of the results
Other prognostic factors
Other factors—for example, socioeconomic deprivation—should be taken into consideration
Small numbers
Most surgeons at times have a cluster of patients who do less well than expected. This will vary from year to year. Any conclusion based on a small sample is likely to be misleading as it pertains to the individual surgeon
Several factors apart from the individual surgeon's skill might influence these measurements of immediate and long term outcome: case mix; surgical philosophy; assessment of cure; quality of pathological reporting; other prognostic factors; small numbers (see box). Despite these factors it seems likely that the differences in the immediate postoperative morbidity and mortality observed among surgeons in the above studies are genuine. There have now been several analyses of immediate outcome after colorectal cancer surgery, and in each study, the results have been broadly comparable.
Effect of volume of surgery
Two explanations are possible for the differences in outcome among surgeons—namely, the number of patients treated by individual surgeons and whether these surgeons are specialists.
Although good evidence exists for other types of surgery that volume of work is important, in colorectal cancer convincing evidence that volume affects outcome is lacking. In the Lothian and Borders study, 5 of 20 consultants were responsible for 50% of the rectal cancer procedures. These five surgeons had a significantly lower anastomotic leak rate, but this may reflect specialisation rather than volume of work. In the German multicentre study, a group of surgeons with low work volume and performing only a few rectal cancer procedures had local recurrence rates well within the range of results obtained by individual surgeons with high work loads. Furthermore, in a recent analysis of outcome in 927 patients treated in the Manchester area, after correction for non-prognostic variables no relation between volume and outcome was noted.
Role of specialisation
The question of specialisation is more complex. Clearly rectal cancer surgery represents a greater technical challenge than colonic surgery. It therefore seems reasonable to expect—but it is remarkably difficult to show (largely because of the small numbers of patients treated by individual surgeons)—that specialist surgeons achieve better outcome. Analysis of outcome in almost 1400 patients with rectal cancer randomised in the Swedish preoperative radiotherapy studies, suggested that local recurrence and death rates were significantly lower in those patients operated on by surgeons with more than 10 years' experience as a specialist.
Local recurrence and disease specific survival (n=683), according to specialisation and volume of work. Values are percentages
| Training in colorectal surgery | Surgeons performing <21 resections (323 procedures) | Surgeons performing⩾21 resections (360 procedures) |
| No (n=574): | ||
| Local recurrence | 44.6 | 27.8 |
| Survival | 39.2 | 49 |
| Yes (n=109): | ||
| Local recurrence | 21.1 | 10.4 |
| Survival | 54.5 | 67.3 |
Data are from the Canadian study (Porter et al, Ann Surg 1998;227:157-67)
Even if confounding variables are taken into account, some surgeons seem to be less competent than others, with poorer outcomes
Perhaps the best information, however, comes from the Canadian study in which 683 patients with rectal cancer were treated by 52 different surgeons, five of whom were trained in colorectal surgery. These five surgeons performed 109 (16%) of the procedures. Independent of the type of training received by the surgeons, 323 procedures (47%) were performed by surgeons who each did fewer than 21 resections over the study period. Multivariate analysis showed that the risk of local recurrence was increased in patients treated both by surgeons not trained in colorectal surgery and by surgeons performing fewer than 21 resections. Similarly, disease specific survival was lower in the patients treated by these two groups of surgeons. These results suggest that both specialisation and volume may be important independent factors determining outcome.
Surgeons are currently under intense scrutiny, partly because readily available measures of outcome exist and partly because outcome seems to differ substantially among surgeons. The issues, however, are complex. Small numbers, annual accounting, and failure to take into account case mix, surgical intent, quality of staging, and prognostic factors may lead to inappropriate conclusions.
Nevertheless, the results of the studies discussed here suggest that some surgeons are less competent than their colleagues and that these factors may compromise survival. Considerable effort and resources are currently being poured into large multicentre studies of adjuvant chemotherapy and radiotherapy in an effort to provide a marginal improvement in the survival of patients with colorectal cancer. If, by specialisation, the overall results of surgery could be improved—and evidence suggests that this is so—the impact on survival might be greater than that of any of the adjuvant therapies currently under study.
Further reading
Holm T, Johansson H, Cedermark B, Ekelund G, Rutqvist L-E. Influence of hospital and surgeon related factors and outcome after treatment of rectal cancer with or without pre-operative radiotherapy. Br J Surg 1997;87:657-63.
McArdle CS, Hole D. Impact of variability among surgeons on post-operative morbidity and mortality and ultimate survival. BMJ 1991;302:1501-5.
Parry JM, Collins S, Mathers J, Scott NA, Woodman CBJ. Influence of volume of work on the outcome of treatment for patients with colorectal cancer. Br J Surg 1998;86:475-81.
Porter GA, Soskolne CL, Yakimets WW, Newman SC. Surgeon-related factors and outcome in rectal cancer. Ann Surg 1998;227:157-67.
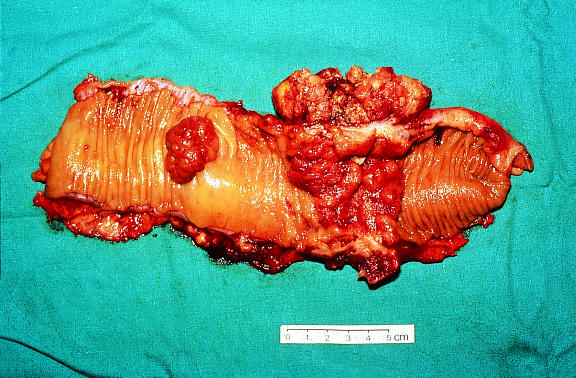
Figure.
Colorectal adenoma and tumour—does a patient's survival depend on which surgeon operates?
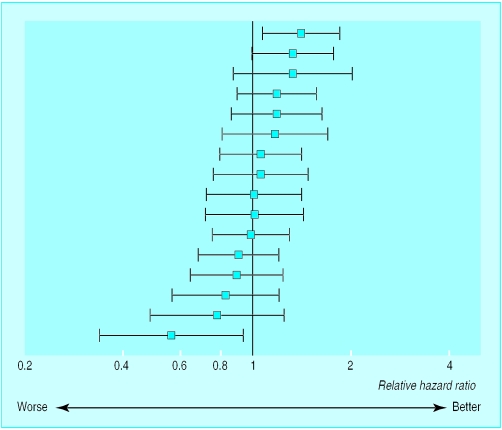
Figure.
95% confidence intervals for relative risk of outcome, for all resections, by surgeon (n=16), west of Scotland study
Figure.
Outcome seems to differ substantially among surgeons performing colorectal surgery—specialisation rather than volume of work might be a way of improving overall outcome
Footnotes
Colin McArdle is professor in the university department of surgery at the Royal Infirmary, Edinburgh
The ABC of colorectal cancer is edited by D J Kerr, professor at the Institute for Cancer Studies, University of Birmingham; Annie Young, research fellow at the School of Health Sciences, University of Birmingham; and F D Richard Hobbs, professor in the department of primary care and general practice, University of Birmingham. The series will be published as a book by the end of 2000.