Abstract
Introduction:
A good screening tool, such as a growth chart, should distinguish between children with normal growth and those with perturbed growth. Suitability of synthetic Indian growth references for diagnosing growth-related disorders for under-five children has not been evaluated. To assess the validity of World Health Organization (WHO) 2006 standards vs synthetic Indian references (2019) (by comparing weight, height, body mass index (BMI), standard deviation scores (SDS) and the composite index of anthropometric failure (CIAF)) in differentiating normal children and children with growth-related disorders.
Methods:
Records of 2188 children (0–60 months) attending a tertiary centre paediatric outpatient department (OPD) were retrospectively studied; 1854 children were healthy and 334 were diagnosed with growth-related disorders as per the European Society for Paediatric Endocrinology (ESPE) classification. The anthropometric parameters converted to Z-scores for weight-for-age (WAZ), height-for-age (HAZ), BMI-for-age (BAZ) and a CIAF were computed using WHO and synthetic charts; Student’s t-test was used for assessing differences and Youden’s index for validity.
Results:
Disease status of children and anthropometric failure on WAZ, HAZ, BAZ and CIAF on both WHO and synthetic charts had a significant association (P-value <0.05). WAZ, HAZ on both charts and CIAF on synthetic chart had a fair to moderate agreement (Kappa statistics) with disease status as per diagnosis (P-value <0.05). The sensitivity and negative predictive value for all anthropometric parameters were higher for synthetic charts.
Conclusion:
Indian charts were more sensitive for diagnosing growth-related disorders from birth to 60 months of age when compared to WHO growth standards.
Keywords: Children with growth-related disorders, synthetic Indian growth reference, under-five children, WHO growth standards
INTRODUCTION
The World Health Organization (WHO) multi-centre growth reference study developed growth standards for children from birth to 60 months of age; the children selected were those with optimal child-rearing practices (breastfeeding, non-smoking mothers, etc.) growing in well-off households. The WHO, therefore, prescribed growth standards with which children could be compared on a global platform. However, the suitability of the WHO child growth standards to assess malnutrition on a global platform has been questioned by several studies.
In comparison with the WHO standards, European children were diagnosed to have excessive weight, had higher head circumference and were taller in length/height. However, higher percentage of Asian children were diagnosed to be undernourished on the WHO standards.[1] Our group has reported that the mean Z-scores for weight, height, body mass index (BMI) and weight-for-height for affluent Indian preschool children in the 2- to 5-year age-group were below the WHO growth standard median.[2] Thus, studies suggest that childhood growth may not be appropriately classified using WHO growth standards in some populations[3] Several countries, including India, have constructed ethnic-specific growth references using several methods. One such method is the synthesis of data to create growth charts.
Synthetic reference growth charts integrate specific local anthropometric data and global patterns of human growth provided by principal components that characterise the variability of growth in the reference population.[4] Our group has put forth synthetic growth references for Indian children from 0 to 18 years of age using lambda, mu and sigma (LMS) method.[5] The prevalence of malnutrition as assessed by various anthropometric parameters on these synthetic growth references for rural and urban healthy Indian children below 60 months of age was compared with WHO 2006 growth standards. This field-testing study reported that the prevalence of stunting on WHO charts was higher, while overweight was lower as compared to synthetic reference charts.[6] Further, the use of Indian synthetic references for monitoring growth of under-five children was found to be more accurate and the synthetic charts were able to make a distinction between clinically significant versus clinically acceptable nutritional deficit.[7]
A good screening tool, such as a growth chart, should be able to distinguish children with normal growth from those with perturbed growth in routine patient screening. Patients with a significant growth disorder should fail on at least one anthropometric parameter, and normal children should be within the reference range on all anthropometric parameters, such as height, weight and BMI. Most suitable growth charts should thus be sensitive to pick up an abnormal child with a disorder and specific not to label a normal child as having abnormal growth. A study on the performance of WHO growth standards on children presenting with growth-related disorders in the under-5-year age-group demonstrated that anthropometric interpretation was in line with clinical setting as compared to healthy controls.[8] However, the comparison of WHO standards versus synthetic reference charts for under-five Indian children in growth-related disorders has not been evaluated till date.
We thus conducted this study to determine the sensitivity and specificity of WHO 2006 versus synthetic growth charts in normal and investigation-proven children with a growth-related disorder. Our specific objective was to assess the validity of WHO 2006 standards vs synthetic Indian references (2019) (by comparing weight, height, BMI, standard deviation scores (SDS) and the composite index of anthropometric failure (CIAF)) in differentiating normal children and children with growth-related disorders.
MATERIALS AND METHODS
This study was conducted at a tertiary care centre in Pune (Western Maharashtra); data for this retrospective study were mined from records in the time period from 2017 to 2022. All data on infants and children from birth to 60 months of age during this time period were extracted.
Records of children on whom decimal age, gender and anthropometric parameters were available (height and weight) were included in the study. Further, records on healthy children coming for vaccinations (all children were examined by a paediatrician, and records of asymptomatic, healthy children were included) and also children who were investigated and diagnosed to have a growth-related disorder were included. Records with incomplete data (on age and anthropometric parameters) were excluded.
Anthropometric assessment is routinely conducted for all infants and children coming to our centre. Thus, for the records which were extracted, height was measured using a Leicester Height Meter (Child Growth Foundation, UK, accuracy of 0.1 cm), and for children under 2 years of age, recumbent length was measured using an infantometer (Shreeyash Electro Medicals, Infantometer, India, accuracy of 0.1 cm). Weight was measured using electronic weighing scales (Salter, India) with an accuracy of ±5 g. BMI was calculated as kilograms/metre2.[9] All children who presented with growth-related complaints from birth to 60 months of age were clinically examined by a paediatric endocrinologist. Children who were found to be either below or above third and 97th percentile, respectively, for height (short or tall) and weight (wasted) as per the Indian Academy of Paediatrics (IAP) references[10,11] or had clinical features suggestive of any other pathology were further investigated as per the standard protocols to arrive at a diagnosis.[12] An adaptation of the European Society for Paediatric Endocrinology (ESPE) classification of growth disorders[13] was used to classify children into eight different groups as children with: 1) bone diseases, 2) endocrine hyperfunction, 3) endocrine hypofunction, 4) familial short stature, 5) short for gestational age, 6) overweight/obesity, 7) syndromic short stature and 8) other endocrinopathy. All anthropometric parameters were converted to Z-scores using the WHO 2006 growth standards and the synthetic Indian growth references.[5,14] Synthetic references have been previously constructed by the authors’ group on 46421 children using arithmetic means of heights and weights at key ages as well as global LMS values from the literature.[5] Z-scores for anthropometric parameters as per the WHO growth standards were calculated using WHO AnthroPlus app.[15] The synthetic reference-based Z-scores were computed using published median for height/weight and lambda and sigma values.[6] Weight-for-age Z (WAZ) scores, height-for-age Z (HAZ) scores and BMI-for-age Z (BAZ) scores were computed. Based on WAZ-scores, children were categorised as normal or within reference range (between +2 and -2 SD), moderately underweight (between -2 and -3 SD), severely underweight (between -2 and -3 SD) and overweight (>+2 SD). Based on BAZ-scores, children were categorised as within reference range (between +2 and -2 SD), moderate acute malnutrition (≤-2 and ≥-3 SD), severe acute malnutrition (<-3SD) and overweight (>+2 and ≤+3 SD). Based on HAZ, children were categorised as within reference range (<+2 and >-2 SD), moderately stunted (≤-2 and ≥-3 SD), severely stunted (<-3 SD) and tall (>+2SD).[16] Based on anthropometric parameters on both charts, children were categorised into seven different (A–E and Y) groups of CIAF. Svedberg’s model of CIAF (groups A–E) gives aggregate measure to estimate the overall burden of malnutrition, and further, the model was further modified by Nandy to add another group of only underweight population (group Y).[17]
Statistical analysis
Data were analysed using the Statistical Package for the Social Sciences (SPSS) version 26.0 for Windows (IBM SPSS, Bangalore, India). The sample size of 2188 children was sufficient for achieving post hoc power of study (b) 0.84, a 0.05 (type 1 error), with proportion of discordant pairs of 0.15, and odds ratio 1.4 using G-Power version 3.1.9.7. Descriptive statistics for demographic and anthropometric characteristics were computed. Differences in means among normal and children diagnosed with growth-related disorders were compared using Student’s t-test. The Chi-square test was used to compare proportions of normal and children with growth-related disorders classified by anthropometric parameters using WHO and synthetic growth references. Kappa statistics was used to assess measure of agreement between clinical diagnosis and anthropometric parameters on the proposed growth reference charts. Cramer’s V was used to assess the strength of association between categorical variables. P-value less than 0.05 was considered significant. The sensitivity of WHO and synthetic charts to identify normal children as normal and children with growth-related disorders (based on clinical diagnosis) as abnormal was compared separately. Youden’s index was calculated using sensitivity and specificity parameters for measuring performance of diagnostic tests.[18]
Ethical Aspect
The ethics committee gave a waiver for the use of deidentified data (ethics approval dated 15 December 2020, Letter Ref: BVDUMC/IEC/ 55; institutional ethic committee, DCGI Reg. No. ECR 518/ Inst/MH/2014/RR-17). Parents of children who participated in the study have given written informed consent. This study was conducted in accordance with the Declaration of Helsinki (2013).
RESULTS
Records on 2188 children from birth to 60 months of age were included in this study (total records identified – 2304, 116 records had incomplete anthropometric data). Of these, 1854 (84.7%) were records of apparently healthy children following up for a routine vaccination visit and they were classified as records on normal/healthy children. Further, 334 (15.3%) children had been clinically diagnosed and classified according to the ESPE classification into eight different disease groups. The mean age for healthy normal and children with disordered growth was 1.6 ± 1.5 and 2.8 ± 1.4 years, respectively. The mean for height, weight, BMI along with WHO standards and synthetic reference-based WAZ, HAZ and BAZ is illustrated in Table 1 for normal and children diagnosed with growth-related disorders. Significant differences were observed between means of WAZ (P-value <0.001), HAZ (P-value <0.001) and BAZ (P-value <0.001) for WHO versus synthetic Z-scores for both normal and children with disordered growth [Table 2].
Table 1.
Mean and standard deviations of anthropometric parameters in healthy children and children with growth-related disorder in the 0- to 5-year age-group
| Healthy children (mean±SD) N=1854 | Children with growth-related disorder (mean±SD) N=334 | |
|---|---|---|
| Age (years) | 1.6±1.5 | 2.8±1.4 |
| Height (cms) | 75.2±17.8 | 79.7±13.6 |
| Weight (kg) | 8.8±4.0 | 10.3±4.6 |
| BMI (kg/m2) | 14.6±2.3 | 15.7±3.3 |
| WHO weight-for-age Z-score | -1.1±1.3 | -2.4±2.7 |
| WHO height-for-age Z-score | -0.8±1.6 | -3.4±2.7 |
| WHO BMI-for-age Z-score | -0.9±1.4 | -0.3±2.3 |
| Synthetic weight-for-age Z-score | -0.6±1.5 | -3.1±3.7 |
| Synthetic height-for-age Z-score | -0.3±1.4 | -2.9±2.4 |
| Synthetic BMI-for-age Z-score | -0.2±1.6 | 0.2±2.2 |
Table 2.
Comparison of anthropometric parameters by paired t-test using WHO 2006 growth standards and synthetic Indian growth references in healthy children and children with growth-related disorders
| Disorder status | Anthropometric parameters | Mean difference | 95% confidence interval | P | Effect size | |
|---|---|---|---|---|---|---|
|
| ||||||
| Lower | Upper | |||||
| Healthy children | Weight-for-age Z-scores | -0.49 | -0.51 | -0.46 | <0.001* | 0.72 |
| Height-for-age Z-scores | -0.45 | -0.48 | -0.42 | <0.001* | 0.76 | |
| BMI-for-age Z-scores | -0.75 | -0.78 | -0.71 | <0.001* | 1.07 | |
| Children with growth-related disorders | Weight-for-age Z-scores | 0.66 | 0.52 | 0.80 | <0.001* | 0.50 |
| Height-for-age Z-scores | -0.54 | -0.60 | -0.49 | <0.001* | 1.07 | |
| BMI-for-age Z-scores | -0.50 | -0.56 | -0.44 | <0.001* | 0.92 | |
*Significance at P value <0.05
As depicted in Table 3, a significant association was noted between the state of disordered growth and synthetic WAZ (Cramer’s V value = 0.485; P-value <0.001); the association was stronger than that for WHO WAZ (Cramer’s V value = 0.408; P-value <0.001). Also, the association between disordered growth and synthetic HAZ (Cramer’s V value = 0.529; P-value <0.001) was stronger than that for WHO HAZ (Cramer’s V value = 0.419; P-value <0.001). CIAF on synthetic charts was significantly associated with disordered growth status (Cramer’s V value = 0.380; P-value <0.001) as was CIAF on WHO charts (Cramer’s V value = 0.262; P-value <0.001). A small but significant association was observed between disordered growth status and synthetic BAZ (Cramer’s V value = 0.064; P-value = 0.003) which was comparatively higher than that of WHO BAZ (Cramer’s V value = 0.054; P-value = 0.011).
Table 3.
Measures of agreement of anthropometric parameters on WHO growth standards and synthetic charts with clinical diagnosis
| Parameter | Growth chart/reference | χ2 value | P | Cramer’s V value | Kappa value |
|---|---|---|---|---|---|
| Weight-for-age | WHO | 364.53 | <0.001* | 0.408 | 0.374 |
| Synthetic | 514.33 | <0.001* | 0.485 | 0.452 | |
| Height-for-age | WHO | 384.62 | <0.001* | 0.419 | 0.370 |
| Synthetic | 612.69 | <0.001* | 0.529 | 0.511 | |
| BMI | WHO | 6.42 | 0.011* | 0.054 | 0.052 |
| Synthetic | 8.87 | 0.003* | 0.064 | 0.062 | |
| CIAF | WHO | 149.64 | <0.001* | 0.262 | 0.196 |
| Synthetic | 316.70 | <0.001* | 0.380 | 0.335 |
*Statistical significance at P value <0.05
The measure of agreement as tested by Kappa statistics between disordered growth status as per the clinical diagnosis and WAZ and HAZ on both WHO and synthetic charts along with CIAF on synthetic charts was noted to be significantly fair to moderate[19] [Table 3]. However, BAZ on both charts and WHO CIAF had a slight but significant agreement with disordered growth status [Table 3]. Using a 2 × 2 table, for disordered growth status and anthropometric failure for WAZ, HAZ, BAZ and CIAF separately for WHO standard and synthetic reference charts, sensitivity, specificity, positive predictive value and negative predictive value were calculated using Youden’s index. The sensitivity of all four anthropometric parameters was higher for synthetic growth chart when compared to WHO charts [Table 4 and Figures 1-4]. WHO charts were more specific in picking up disordered growth in children failing on HAZ, BAZ and CIAF. Youden’s index was calculated for all the anthropometric parameters on both charts to assess performance of test as illustrated in Table 4.
Table 4.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and Youden’s index for WHO 2006 and synthetic Indian charts against disease status
| Parameter | Growth chart/reference | Sensitivity | Specificity | PPV | NPV | Youden’s J index |
|---|---|---|---|---|---|---|
| Weight-for-age | WHO | 78.21 | 73.65 | 94.28 | 37.85 | 0.52 |
| Synthetic | 81.55 | 78.74 | 95.51 | 43.47 | 0.60 | |
| Height-for-age | WHO | 75.03 | 79.94 | 95.40 | 36.58 | 0.55 |
| Synthetic | 86.03 | 76.35 | 95.28 | 49.61 | 0.62 | |
| BMI | WHO | 75.00 | 29.64 | 85.83 | 18.71 | 0.05 |
| Synthetic | 79.45 | 27.84 | 85.94 | 19.62 | 0.07 | |
| CIAF | WHO | 58.74 | 77.54 | 93.56 | 25.29 | 0.36 |
| Synthetic | 74.16 | 75.75 | 94.44 | 34.56 | 0.50 |
Figure 1.
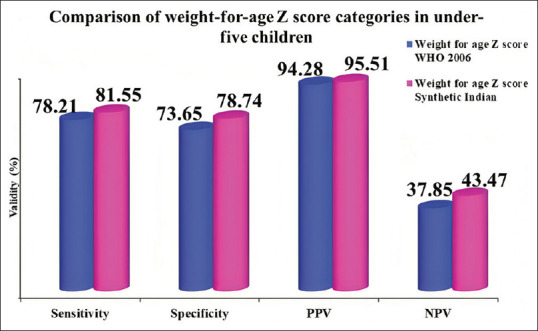
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for weight-for-age Z-scores on WHO 2006 and synthetic Indian charts against disease status
Figure 4.
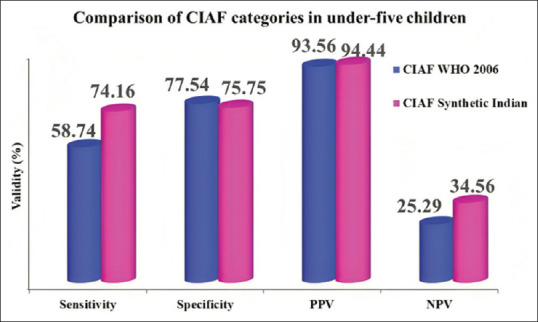
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for CIAF using WHO 2006 and synthetic Indian charts against disease status
Figure 2.
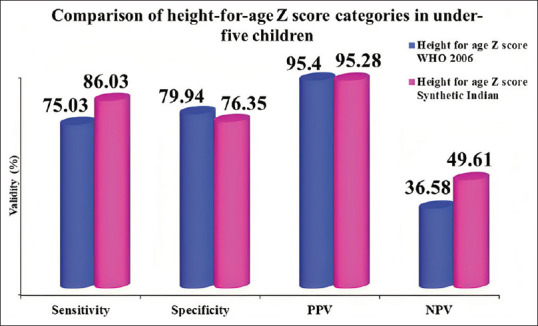
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for height-for-age Z-scores on WHO 2006 and synthetic Indian charts against disease status
Figure 3.
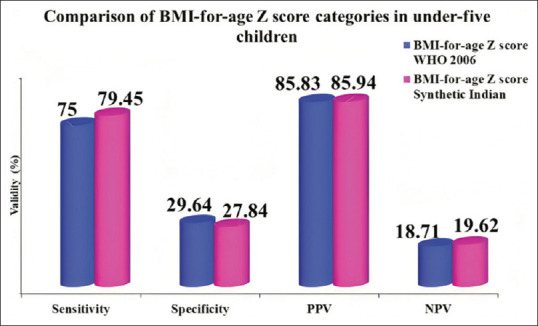
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) for BMI-for-age Z-scores on WHO 2006 and synthetic Indian charts against disease status
DISCUSSION
In our retrospective study on anthropometric records of children from 0 to 60 months of age from a tertiary-level care centre, we found a significant difference between means of Z-scores computed by WHO standards and synthetic references between both healthy children and children with growth-related disorders. The association between disordered growth status and WAZ, HAZ and BAZ was stronger as compared to that with CIAF using both WHO standards and synthetic Indian reference charts. However, all four (WAZ, HAZ, BAZ and CIAF) anthropometric parameters on synthetic reference charts had stronger association as compared to the WHO standards. The sensitivity for picking up the failure of growth on all four anthropometric parameters was higher for synthetic charts (particularly for the CIAF) as compared to WHO standards. The performance of both charts when measured using Youden’s index revealed that synthetic charts were superior to the WHO charts. However, WHO charts were more specific in picking up disordered growth in children failing on HAZ, BAZ and CIAF.
The anthropometric parameters on WHO growth standards vary substantially from those derived using synthetic growth references. Healthy children showed significant difference in their mean anthropometric parameters when plotted on WHO growth standards versus synthetic Indian growth reference. Synthetic Indian growth references could classify a significant proportion of healthy children in our study with normal BMI. Also, growth references based on local anthropometric data had greater impact when identifying children with abnormal BMI. We found no Indian studies which had conducted these comparisons; hence, we compared our results with international studies. Early excessive weight gain in infancy in bottle-fed infants was observed longitudinally in Canadian infants when BMI Z-scores were plotted on WHO growth standards as compared to Centres for Disease Control and Prevention (CDC)-US growth charts.[20] In a study from the United States, a significant difference was noted in mean BMI percentiles for obese and overweight children on CDC-US growth chart vs Cole et al. reference curves vs Must et al. growth reference curves.[21] In contrast, while tracking normal growth in French under-five children, national growth curves overestimated weight gain in first few years suggesting no agreement with WHO growth standards (Kappa = -0.26) and, hence, proposing the use of WHO growth standards.[22]
In our study, all anthropometric parameters on both charts were found to be in concordance with clinical diagnosis of under-five children. A significant difference was found between mean anthropometric parameters in children with growth-related disorders computed using WHO growth standard and synthetic Indian growth references, and a significant association was also found with the clinical diagnosis. A study performed in under-five children with growth-related morbidity in the north-eastern part of Maharashtra, India, found moderate agreement (Cohen’s kappa = 0.41) between WHO growth standards and IAP reference charts while diagnosing malnutrition.[23]
The national growth references in European countries, including the Czech Republic, Denmark, Germany, the Netherlands, Norway, Sweden and Switzerland, had categorised a significantly greater proportion of children <5 years with growth hormone deficiency (GHD) and Turner syndrome (TS) and those born small-for-gestational age (SGA) (height SDS cut-off below -2.5) as being short (height SDS cut-off below -2) as compared to WHO growth standards. However, France and the UK had lower proportion of children below the said cut-off for height SDS on national growth reference.[3] Children with end-stage renal disease in age-group between 2 and 18 years had significantly lower mean height SDS on Euro-Growth references when compared to WHO and CDC growth standards; subsequently, more proportion on national references (44% vs 34%) met the criteria for growth hormone (rhGH) therapy.[24] Australian children were underestimated for eligibility of rhGH therapy using CDC and WHO HAZ threshold < first centile (below -2.3 height SDS).[25,26] It is argued that the time at which data were collected in these studies and the time span when national growth references/WHO standards were constructed need to be in consonance with more accurate analysis.
In our study, synthetic charts were more sensitive in picking up children with growth-related disorder failing on HAZ-scores when compared to WHO charts with a better Youden’s index. Finnish growth charts have been reported to have higher sensitivity (72% vs 36% with third percentile threshold for height and 55% vs 20% with first percentile threshold for height) as compared to WHO growth charts for children aged 2 years with TS.[27] In a French study, different clinical algorithms were validated against WHO growth standards and national growth references. Authors found a significant difference in sensitivity in the diagnosis of GHD with pituitary stalk interruption syndrome (GHD-PSIS) using the Grote clinical decision rule when tested with WHO vs national growth references (54% vs 44.2%). Also, the median theoretical reduction in time to diagnosis for GHD-PSIS and TS was greater with WHO in comparison with national references, while there were no differences for Celiac disease regardless of the growth chart used.[28] WHO weight-for-length standard cut-offs showed comparatively lower sensitivity for children with cystic fibrosis when compared to the CDC growth charts in a study from the United States.[29]
The CIAF computed using synthetic Indian growth reference was found to be more sensitive (74.16% vs 58.74%) and had higher ability to predict true negatives (NPV 34.56% vs 25.29%) as compared to WHO growth standards for recognition of children with growth-related disorders. We could not find any study for performance of growth reference curves based on CIAF in children with growth-related disorders. The implementation of CIAF in diagnosing endocrine disorders was also found to be fruitful.
Although the association of BMI Z-scores on both WHO standards and synthetic growth reference with disordered growth status was poor, probably due to inclusion of children having extremes of BMI values with overgrowth syndromes, yet it was statistically significant. Synthetic references constructed using the recent anthropometric data were not only found to be more valid for the assessment of growth among normal children but also for those with growth-related disorders and may be more useful during clinical assessments.
The strength of our study was its large sample size, and all patients whose records were analysed were examined by a single paediatric endocrinologist. The ESPE classification was used for more accurate categorisation of children with growth-related disorder. Synthetic references were constructed using the LMS method with anthropometric means at key ages. Our study was limited by the fact that we majorly worked with data on urban population and there was no rural representation. Further, it was a single-centre retrospective study design with a lack of multicentric data. Also, as there was paucity of data on the comparison of Indian growth references and WHO growth standards in children with growth-related disorders, we have presented comparisons with international studies.
CONCLUSION
To conclude, synthetic Indian charts performed well and were found to be more sensitive for all anthropometric parameters, including WAZ, HAZ, BAZ and CIAF, for diagnosing growth-related disorders in a clinical setting from birth to 60 months of age when compared to WHO growth standards. Further prospective multicentric studies (in both urban and rural settings) are required to confirm the use of synthetic/ethnic-specific references for the detection of growth-related disorders in Indian children.
Authors’ contribution
NSD, Vaman Khadilkar, VK, SM, SY and AVK were involved in study conceptualization, subject recruitment and actual conduct of the study. NSD, Vaman Khadilkar and KG were involved in data curation and formal analysis. NSD, Vaman Khadilkar, SM, SY and AVK were involved in visualization, writing and reviewing the manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We wish to express our sincere thanks to all the children and their parents who participated in this study.
REFERENCES
- 1.Natale V, Rajagopalan A. Worldwide variation in human growth and the World Health Organization growth standards: A systematic review. BMJ Open. 2014;4:e003735. doi: 10.1136/bmjopen-2013-003735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khadilkar VV, Khadilkar AV, Chiplonkar SA. Growth performance of affluent Indian preschool children: A comparison with the new WHO growth standard. Indian Pediatr. 2010;47:869–72. doi: 10.1007/s13312-010-0147-6. [DOI] [PubMed] [Google Scholar]
- 3.Christesen HT, Pedersen BT, Pournara E, Petit IO, Júlíusson PB. Short stature: Comparison of WHO and national growth standards/references for height. PLoS One. 2016;11:e0157277. doi: 10.1371/journal.pone.0157277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hermanussen M, Stec K, Aßmann C, Meigen C, Van Buuren S. Synthetic growth reference charts. Am J Hum Biol. 2016;28:98–111. doi: 10.1002/ajhb.22759. [DOI] [PubMed] [Google Scholar]
- 5.Khadilkar V, Khadilkar AV, Kajale N. Indian growth references from 0-18-year-old children and adolescents-A comparison of two methods. Indian J Endocrinol Metab. 2019;23:635–44. doi: 10.4103/ijem.IJEM_555_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehta S, Oza C, Karguppikar M, Khadilkar V, Khadilkar A. Field testing of synthetic growth charts in 1-60-month-old indian children. Indian J Endocrinol Metab. 2022;26:180–85. doi: 10.4103/ijem.ijem_9_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khadilkar V, Ekbote V, Gondhalekar K, Khadilkar A. Comparison of nutritional status of under-five Indian children (NFHS 4 Data) using WHO 2006 charts and 2019 Indian synthetic Charts. Indian J Endocrinol Metab. 2021;25:136–41. doi: 10.4103/ijem.IJEM_18_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prasad HK, Ekbote V, Rustagi V, Borade A, Chiplonkar S, Khadilkar V, et al. Performance of WHO growth standards on Indian children with growth related disorders. Indian J Pediatr. 2012;79:884–90. doi: 10.1007/s12098-012-0687-y. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. 2022. [Last accessed on 2023 Jun 19]. Available from: Body Mass Index (BMI). https://www.cdc.gov/healthyweight/assessing/bmi/index.html .
- 10.Agarwal DK, Agarwal KN. Physical growth in Indian affluent children (birth-6 years) Indian Pediatr. 1994;31:377–413. [PubMed] [Google Scholar]
- 11.Vaman K. 1st ed. Jaypee Brothers Medical Publishers; 2019. IAP Textbook on Pediatric Endocrinology; p. 689. [Google Scholar]
- 12.Oostdijk W, Grote FK, de Muinck Keizer-Schrama SM, Wit JM. Diagnostic approach in children with short stature. Horm Res. 2009;72:206–17. doi: 10.1159/000236082. [DOI] [PubMed] [Google Scholar]
- 13.Wit JM. International classification of Pediatric endocrine diagnoses. Horm Res Paediatr. 2016;86:212–14. doi: 10.1159/000448893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bloem M. The 2006 WHO child growth standards. BMJ. 2007;334:705–6. doi: 10.1136/bmj.39155.658843.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Growth reference 5-19 years - Application tools. [Last accessed on 2023 Jun 16]. Available from:https://www.who.int/tools/growth-reference-data-for-5to19-years/application-tools .
- 16.Guideline: Assessing and Managing Children at Primary Health-Care Facilities to Prevent Overweight and Obesity in the Context of the Double Burden of Malnutrition: Updates for the Integrated Management of Childhood Illness (IMCI) [Internet] Geneva: World Health Organization; 2017. [[cited 2023 Jun 19]]. (WHO Guidelines Approved by the Guidelines Review Committee) Available from:http://www.ncbi.nlm.nih.gov/books/NBK487902/ PMID 29578661. [PubMed] [Google Scholar]
- 17.Nandy S, Svedberg P. The Composite Index of Anthropometric Failure (CIAF): An Alternative Indicator for Malnutrition in Young Children. In: Handbook of anthropometry: Physical measures of human form in health and disease, editor. 2012. :127–37. [Google Scholar]
- 18.Naga Rajeev L, Saini M, Kumar A, Osmond C, Sachdev HS. Comparison of weight for height and BMI for age for estimating overnutrition burden in under-five populations with high stunting prevalence. Indian Pediatr. 2023;60:17–26. [PubMed] [Google Scholar]
- 19.McHugh ML. Interrater reliability: The kappa statistic. Biochem Med (Zagreb) 2012;22:276–82. [PMC free article] [PubMed] [Google Scholar]
- 20.Van Dijk CE, Innis SM. Growth-curve standards and the assessment of early excess weight gain in infancy. Pediatrics. 2009;123:102–8. doi: 10.1542/peds.2007-3382. [DOI] [PubMed] [Google Scholar]
- 21.Flegal KM, Ogden CL, Wei R, Kuczmarski RL, Johnson CL. Prevalence of overweight in US children: Comparison of US growth charts from the centers for disease control and prevention with other reference values for body mass index. Am J Clin Nutr. 2001;73:1086–93. doi: 10.1093/ajcn/73.6.1086. [DOI] [PubMed] [Google Scholar]
- 22.Bois C, Servolin J, Guillemot G. [Monitoring infant growth: Comparative use of WHO standards and French national reference curves. Arch Pediatr. 2010;17:1035–41. doi: 10.1016/j.arcped.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Patel A, Badhoniya N, Dibley M, Raynes-Greenow CH. Differential estimates of underweight-for-age and growth related morbidity according to different growth standards in Indian children. Indian J Pediatr. 2015;82:19–24. doi: 10.1007/s12098-014-1460-1. [DOI] [PubMed] [Google Scholar]
- 24.Bonthuis M, van Stralen KJ, Verrina E, Edefonti A, Molchanova EA, Hokken-Koelega AC, et al. Use of national and international growth charts for studying height in European children: Development of up-to-date European height-for-age charts. PLoS One. 2012;7:e42506. doi: 10.1371/journal.pone.0042506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hughes I, Harris M, Cotterill A, Garnett S, Bannink E, Pennell C, et al. Comparison of centers for disease control and prevention and world health organization references/standards for height in contemporary Australian children: Analyses of the Raine Study and Australian National Children's Nutrition and Physical Activity cohorts. J Paediatr Child Health. 2014;50:895–901. doi: 10.1111/jpc.12672. [DOI] [PubMed] [Google Scholar]
- 26.Hughes IP, Choong CS, Cotterill A, Harris M, Davies PS Australasian paediatric endocrine group. The influence of secular trend for height on ascertainment and eligibility for growth hormone treatment. Clin Endocrinol (Oxf) 2010;73:760–8. doi: 10.1111/j.1365-2265.2010.03874.x. [DOI] [PubMed] [Google Scholar]
- 27.Saari A, Sankilampi U, Dunkel L. Multiethnic WHO growth charts may not be optimal in the screening of disorders affecting height: Turner syndrome as a model. JAMA Pediatr. 2013;167:194–5. doi: 10.1001/jamapediatrics.2013.436. [DOI] [PubMed] [Google Scholar]
- 28.Scherdel P, Matczak S, Léger J, Martinez-Vinson C, Goulet O, Brauner R, et al. Algorithms to define abnormal growth in children: External validation and head-to-head comparison. J Clin Endocrinol Metab. 2019;104:241–49. doi: 10.1210/jc.2018-00723. [DOI] [PubMed] [Google Scholar]
- 29.Machogu E, Cao Y, Miller T, Simpson P, Levy H, Quintero D, et al. Comparison of WHO and CDC growth charts in predicting pulmonary outcomes in cystic fibrosis. J Pediatr Gastroenterol Nutr. 2015;60:378–83. doi: 10.1097/MPG.0000000000000610. [DOI] [PMC free article] [PubMed] [Google Scholar]


