Abstract
Introduction:
Assessment of genitalia is an important part of the neonatal examination. Regional, racial, and ethnic variations in phallic length have been documented. Clitoral dimensions may also show similar variations. Normal values for neonatal clitoral measurements may help the pediatrician/neonatologist to accurately diagnose clitoromegaly and underlying etiology to guide appropriate investigations. Data on clitoral measurements is limited with only one study from India (Kolkata). Hence we aimed in this study to generate south Indian data on neonatal clitoral dimensions, anogenital distance, and anogenital ratio. Two hundred and fifty two hemodynamically stable term female neonates without ambiguous genitalia/vulval masses born in a community hospital. Hospital-based cross-sectional study. 1. To measure clitoral dimensions, anogenital distance, and anogenital ratio in female neonates. 2. To correlate clitoral dimensions, anogenital distance, and ratio with anthropometric measurements, gestational age, and maternal comorbidities.
Methods:
Measurements were recorded using a digital vernier caliper, under strict aseptic precautions with labia majora gently separated and the baby held in a frog-leg position. Clitoral length, width, and anogenital distance were measured and anogenital ratio and clitoral index were calculated.
Results:
In term neonates, the mean ± SD of clitoral length (CL), clitoral width (CW), anogenital ratio (AGR) were 6.34 ± 1.75 mm, 6.39 ± 1.27 mm and 0.39 ± 0.05, respectively. The 3rd and 97th centiles for mean clitoral length were 3.55 and 9.93 mm, for mean clitoral width were 3.37 and 8.35 mm, and for AGR were 0.28 and 0.48, respectively. These clitoral dimensions in south Indian neonates were higher than those from East India (Kolkata), lower than Nigerian babies, and similar to Israeli neonates. Mean CL and CW had no statistical correlation with birth weight, gestational age, head circumference, or length in term neonates. A significant correlation was noted between pregnancy-induced hypertension and mean clitoral width, and between gestational diabetes and AGR.
Conclusion:
Normative values for clitoral dimensions (length and width) and AGR for south Indian term female neonates have been established. 97th centiles of 9.93 mm (CL) and 8.35 mm (CW) and 0.48 mm (AGR) may be used as practical cut-offs to diagnose clitoromegaly and virilization. Clitoral measurements had no statistical correlation with birth weight, gestational age, or anthropometry. Clitoral measurements exhibit ethnic and racial differences, thus emphasizing the importance of regional cut-offs and need for more studies from different parts of India on CL.
Keywords: Anogenital distance, AGR, clitoral length, clitoral measurements, clitoral width, South Indian data, term neonates
INTRODUCTION
Examination of a newborn baby would be incomplete without assessment of genitalia. It is important to identify ambiguous genitalia and clitoromegaly as a part of virilization in female neonates. Conditions like congenital adrenal hyperplasia that present with virilization require prompt diagnosis and management to avert a potential adrenal crisis. On the other hand, it is important to avoid overzealous evaluation of neonates with apparent clitoromegaly. Prader’s staging of clitoromegaly is subjective and may not be enough to make a diagnosis. Having normal reference values for neonatal clitoral measurements would definitely help clinicians to accurately diagnose clitoromegaly and assess the need for evaluation.
Regional, racial, and ethnic variations in phallic length have been documented. Clitoral dimensions may also show similar variations. However, available data from India is limited; only one study from Kolkata has reported clitoral measurements from India.[1]
Few other studies on AGD have reported that AGD was significantly longer in preterm and term males in comparison to females.[2] A significant difference was noted between male and female AGD in a Nigerian population.[3] Similarly, Asians and Native Americans had consistently smaller AGD when compared to Caucasians.[4] AGD increased from birth to 6 months of age and thereafter reached a plateau.[5] No maternal characteristics like age, gravidity, or parity influenced AGD.[6]
This study is aimed at obtaining normal neonatal clitoral measurements in term, south Indian female neonates. The objectives were to measure clitoral dimensions and anogenital distance, calculate anogenital ratio and clitoral index, and to correlate all these with neonatal and maternal parameters.
MATERIALS AND METHODS
This hospital-based prospective study was conducted between September 2018 and October 2021. The sample size was calculated as 228, using the formula S = z2 s2/E2, for a 95% confidence interval, assuming a margin of error of 20%, and using the standard deviation (1.54) of CL from the study done by Mondal R. et al. in Kolkata.[1]
Two hundred and fifty two hemodynamically stable, term (≥37 weeks gestation), female neonates of all birth weights, belonging to states Tamil Nadu, Karnataka, Kerala, Andhra Pradesh, and Telangana were consecutively enrolled in the study after written informed consent from one parent. Babies who were sick, preterm, or with apparent genital abnormality suspicious of ambiguous genitalia or vulval hematoma were excluded. Gestational age was determined from the date of the last menstrual period and early ultrasound scans, and if necessary, confirmed using a modified Ballard score.
A semi-structured questionnaire was used to collect maternal data like maternal age, parity, method of conception, maternal risk factors like gestational hypertension, gestational hypothyroidism, steroid intake, hormonal intake, and history of hyperandrogenic states and birth details of the neonates.
All measurements were done by the first author to avoid inter-observer variability. Weight, length, and head circumference of babies were measured using a digital weighing scale (CAS computing scale), an infantometer (AVI Healthcare PVT Ltd), and a non-stretchable tape, respectively. A blunt plastic digital vernier caliper (Sangabery vernier caliper) with a resolution of 0.1 mm and accuracy of ±0.2 mm was used for clitoral measurements.
With the baby in a supine frog-leg position and the perineum exposed adequately, the genital region was first visually examined to determine whether the clitoris was visible or covered by the labia majora [Figure 1]. Clitoral measurements were done with a nurse holding the baby in a frog-leg position and hips flexed to 90 degrees, as shown in the picture [Figure 2]. We measured CL (distance from the crura insertion at the pubic symphysis to the tip of the glans), clitoral width (maximum transverse diameter of the clitoris), and anogenital distance [ano-fourchette distance (AF) (from the center of the anus to posterior fourchette), ano-clitoral distance (AC) (from the center of the anus to the base of the clitoris)] as shown in Figure 3. The mean of two measurements was recorded. Clitoral index (CI) was calculated as the product of CL and CW; anogenital ratio AGR as the AF divided by the AC.
Figure 1.

Naked - eye examination of two different babies with their hips flexed to 90 degree for comparison. One baby had visible clitoris while the other did not
Figure 2.

Baby held in frog-leg position for measurements
Figure 3.
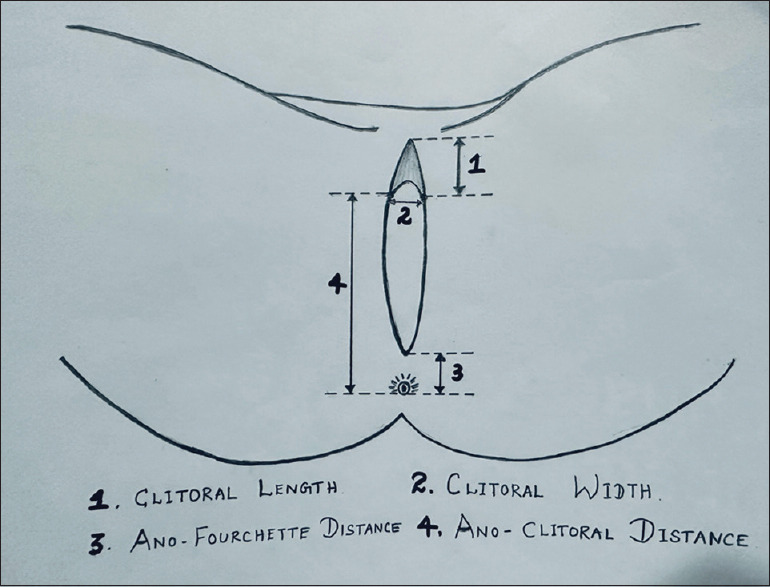
Measurements of clitoral dimensions and anogenital distances
Ethical Aspect
EC approval letter number : IEC 01-13/11/2018. Date of issue is on 13.11.2018. The aim of the study and methodology and were completely explained in the patient information sheet and confidentiality was assured. Either of the parents of the neonates enrolled in the study were asked to sign both the patient information sheet and written informed consent sheet. Then using semi-structured questionnaire, necessary maternal details and baby details were collected. We ensured that no babies were harmed during any part of the study and that the personal details of the mother and the baby were protected. We also made sure to abide by the Declaration of Helsinski as part of our medical research.
RESULTS
The study included 252 term female neonates. The mean birth weight of the study population was 2.9 Kg (range 1.77–4.6 Kg).
On initial visual examination, 47 (18.6%) out of 252 babies had a covered clitoris, and 207 (82.1%) babies had visible clitoris. We obtained a mean clitoral length (MCL) of 6.34 mm, mean clitoral width (MCW) of 6.39 mm, mean clitoral index (CI) of 41.74, and mean AGR of 0.39. Table 1 shows the mean ± SD and 3rd and 97th centiles of clitoral measurements, clitoral index, and AGR.
Table 1.
Clitoral measurements and indices
| Variables | Mean±Standard deviation | 3rd centile | 97th centile |
|---|---|---|---|
| Clitoral length (CL) (mm) | 6.34± (1.75) | 3.55 | 9.93 |
| Clitoral width (CW) (mm) | 6.39± (1.27) | 3.37 | 8.35 |
| Clitoral Index (mm2) [Clitoral length*Clitoral width] | 41.74± (16.4) | 13.25 | 73.17 |
| Ano-fourchette distance (AF) (mm) | 12.12± (1.91) | 8.7 | 15.64 |
| Ano-clitoral distance (AC) (mm) | 31.30± (3.29) | 26.05 | 38.38 |
| Anogenital ratio (AGR) = (AF)/AC) | 0.39± (0.05) | 0.28 | 0.48 |
Clitoral measurements had no statistical correlation with birth weight, gestational age, or anthropometry as shown in Table 2. MCL had a significant correlation with MCW, clitoral index, and AGR.
Table 2.
Correlation between clitoral measurements and gestational age, birth weight, length, and head circumference
| MCL | MCW | CI | AGR | ||
|---|---|---|---|---|---|
| Gestational age | r | −0.020 | −0.051 | −0.019 | 0.001 |
| P | 0.748 | 0.418 | 0.765 | 0.986 | |
| Birth weight | r | 0.008 | −0.031 | −0.010 | −0.064 |
| P | 0.9 | 0.626 | 0.878 | 0.313 | |
| Length | r | −0.023 | 0.007 | −0.010 | −0.048 |
| P | 0.717 | 0.912 | 0.873 | 0.448 | |
| Head circumference | r | 0.027 | 0.036 | 0.029 | 0.009 |
| P | 0.673 | 0.582 | 0.873 | 0.889 | |
MCL=Mean clitoral length, MCW=Mean clitoral width, CI=Clitoral Index, AGR=Anogenital ratio
Seventy (27.8%) among the 252 mothers had hypothyroidism, 41 (16.3%) had gestational diabetes, 24 (9.5%) had pregnancy-induced hypertension, 4 (1.6%) had a history of progesterone intake, and 3 (1.2%) had taken steroids. None had a history of using oral contraceptive pills, testosterone, danazol, or sodium valproate and none had any virilizing tumors.
The difference in means between pregnancy-induced hypertension and non-pregnancy-induced hypertension women with MCW was statistically significant (P = 0.029) and the difference in means between gestational diabetes mellitus and non-gestational diabetes mellitus women with AGR was statistically significant (P = 0.020) as shown above in Table 3.
Table 3.
Test of significance in mean value between different maternal factors using t-test
| Clitoral dimensions | MCL | MCW | CI | AGR | |||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||
| Maternal factors | Mean | P | Mean | P | Mean | P | Mean | P | |
| Hypothyroidism | Yes (n=70) | 6.51 | 0.349 | 6.49 | 0.406 | 43.32 | 0.344 | 0.006 | 0.934 |
| No (n=182) | 6.27 | 6.35 | 41.13 | 0.004 | |||||
| Gestational diabetes | Yes (n=41) | 6.38 | 0.878 | 6.32 | 0.703 | 41.51 | 0.923 | 0.40 | 0.020 |
| No (n=211) | 6.33 | 6.40 | 41.78 | 0.38 | |||||
| Pregnancy-induced hypertension | Yes (n=24) | 6.00 | 0.323 | 6.93 | 0.029 | 41.97 | 0.943 | 0.38 | 0.921 |
| No (n=228) | 6.37 | 6.33 | 41.72 | 0.38 | |||||
| Progesterone | Yes (n=4) | 7.20 | 0.325 | 6.56 | 0.787 | 50.43 | 0.287 | 0.42 | 0.157 |
| No (n=248) | 6.32 | 6.38 | 41.60 | 0.38 | |||||
MCL=Mean clitoral length, MCW=Mean clitoral width, CI=Clitoral Index, AGR=Anogenital ratio
DISCUSSION
This study has generated south Indian data for normal neonatal clitoral dimensions and AGR. We obtained a MCL of 6.34 ± 1.75 mm and MCW of 6.39 ± 1.27 mm. From a clinician’s point of view, the 97th centile for CL of 9.93 mm and width of 8.35 mm may be used as cut-off for diagnosing clitoromegaly and to proceed for further evaluation.
The CL in our study was significantly higher than that reported by the other study from East India (Kolkata).[1] CL at birth varies significantly as reported from different parts of the world, and probably even among different communities in the same region, as shown by the difference in MCL between Israeli babies of Jewish and Bedouin origins [Figure 4].
Figure 4.
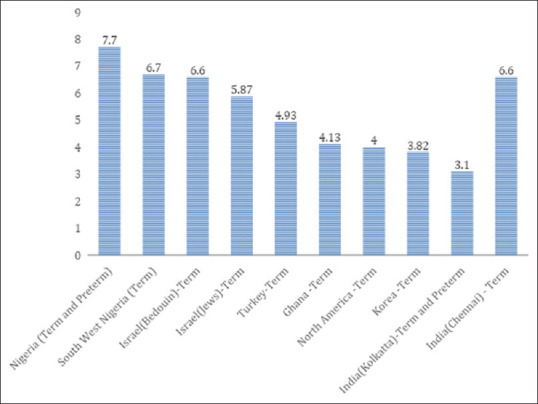
Comparison of MCL among various countries in millimeters. Reference:[1,7,8,9,10,11,12,13]
CW was also higher in our study as compared to the Kolkata study and correlated with CL. None of the maternal or neonatal parameters studied correlated with clitoral dimensions. There was an association of higher CW with maternal hypertension, but the numbers were small and the clinical significance is unclear.
AGR is a sensitive marker of early virilization in the fetal period as previously reported. This again has regional and ethnic variations.[14] Higher AGR was observed among neonates born to mothers with gestational diabetes in our study. Again, the significance cannot be commented upon as the numbers were small and this was not the primary objective of our study.
Although not our primary aim, we tried to correlate conditions suggestive of maternal hyperandrogenism with clitoromegaly and AGR >0.5. The number of mothers with a history suggestive of polycystic ovary syndrome, hypothyroidism, gestational diabetes, and antenatal steroid intake was very low to have any meaningful clinical interpretation. However, studies with a larger number of babies of mothers with such conditions may be done to explore any significant correlations.
The significance of naked-eye examination of the clitoris was emphasized in a study by Kutlu et al., he suggested a cut-off CL of 4.69 mm below which the clitoris was covered by labia majora when the baby was held in a frog-leg position.[11] Their study also suggested that a diagnosis of clitoromegaly could be made if the clitoris is exposed when the baby’s hip is flexed in a frog-leg position of 90°. We too attempted a similar naked-eye examination in our study. However, we observed that 207 out of 252 (82.1%) babies had clitoris visible in the frog-leg position. We, therefore, do not advocate this method of diagnosis of clitoromegaly and suggest actual measurement of the clitoris with regional cut-offs to confirm clitoromegaly.
CONCLUSION
Normative values for clitoral dimensions (length and width) and AGR for south Indian term female neonates have been established. 97th centiles of 9.93 mm (CL) and 8.35 mm (CW) and 0.48 mm (AGR) may be used as practical cut-offs to diagnose clitoromegaly and virilization.
Clitoral measurements had no statistical correlation with birth weight, gestational age, or anthropometry.
Clitoral measurements exhibit ethnic and racial differences, thus emphasizing the importance of regional cut-offs and need for more studies from different parts of India on CL.[10,15]
Limitation
This study included only term neonates and not preterm neonates.
Calibrations using a vernier caliper can have a negligible error of 0.01–0.02 mm.
This study included only babies born to mothers in South Indian states.
Authors’ contribution
Acquisition of data: Dr.Priyadarshini.K
All authors contributed to study design and concept, methodology, data analysis and interpretation, manuscript drafting, critical revision of the article, final approval for the version to be published and agree to be accountable for the integrity of the data in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors gratefully acknowledge the help received from Dr.Vanishree Shriraam and Dr.Suganya with statistics.
REFERENCES
- 1.Mondal R, Chatterjee K, Samanta M, Hazra A, Ray S, Sabui TK, et al. Clitoral length and anogenital ratio in Indian newborn girls. Indian Pediatr. 2016;53:299–303. doi: 10.1007/s13312-016-0840-1. [DOI] [PubMed] [Google Scholar]
- 2.Jain VG, Goyal V, Chowdhary V, Swarup N, Singh RJ, Singal A, et al. Anogenital distance is determined during early gestation in humans. Hum Reprod. 2018;33:1619–27. doi: 10.1093/humrep/dey265. [DOI] [PubMed] [Google Scholar]
- 3.Orish CN, Didia BC. Anogenital distance in human male and female newborns: A look at a cross section of a Nigerian population. Intern J Biol Anthropol. 2009;3:8. [Google Scholar]
- 4.Sathyanarayana S, Beard L, Zhou C, Grady R. Measurement and correlates of ano-genital distance in healthy, newborn infants. Int J Androl. 2010;33:317–23. doi: 10.1111/j.1365-2605.2009.01044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fischer MB, Ljubicic ML, Hagen CP, Thankamony A, Ong K, Hughes I, et al. Anogenital distance in healthy Infants: Method-, age-and sex-related reference ranges. J Clin Endocrinol Metab. 2020;105:2996–3004. doi: 10.1210/clinem/dgaa393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singal AK, Jain VG. Maternal and infant characteristics influencing the anogenital distance and penile length in newborns. Andrologia. 2016;48:708–13. doi: 10.1111/and.12507. [DOI] [PubMed] [Google Scholar]
- 7.Oberfield SE, Mondok A, Shahrivar F, Klein JF, Levine LS. Clitoral size in full term infants. Am J Perinatol. 1989;6:453–4. doi: 10.1055/s-2007-999638. [DOI] [PubMed] [Google Scholar]
- 8.Jarrett OO, Ayoola OO, Jonsson B, Albertsson-Wikland K, Ritzen EM. Penile size in healthy Nigerian newborns: Country based reference values and international comparisons. Acta Pediatr. 2014;103:442–6. doi: 10.1111/apa.12517. [DOI] [PubMed] [Google Scholar]
- 9.Phillip M, De Boer C, Pilpel D, Karplus M, Sofer S. Clitoral and penile sizes of full term newborns in two different ethnic groups. J Pediatr Endocrinol Metab. 1996;9:175–9. [PubMed] [Google Scholar]
- 10.Adekoya AO, Fetuga MB, Jarrett OO, Ogunlesi TA, Chanoine JP, Adekoya AO. Clitoral sizes and anogenital distances in term newborns in Nigeria. Int J Pediatr Endocrinol. 2019;2019:5. doi: 10.1186/s13633-019-0069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kutlu HA, Akbiyik F. Clitoral length in female newborns: A new approach to the assessment of clitoromegaly. Turk J Med Sci. 2011;41 doi:10.3906/sag-1006-907. [Google Scholar]
- 12.Asafo-Agyei SB, Ameyaw E, Chanoine JP, Zacharin M, Nguah SB. Clitoral size in term newborns in Kumasi, Ghana Int J Pediatr Endocrinol. 2017;2017:6. doi: 10.1186/s13633-017-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee KH, Koh MW. The clitoral size of the korean female newborn and the relationship in clitoral hypertrophy and androgen levels. Korean J Obstetr Gynecol. 2001;44:1591–5. [Google Scholar]
- 14.Callegari C, Everett S, Ross M, Brasel JA. Anogenital ratio: Measure of fetal virilization in premature and full-term newborn infants. J Pediatr. 1987;111:240–3. doi: 10.1016/s0022-3476(87)80075-6. [DOI] [PubMed] [Google Scholar]
- 15.Mahadevan S, Prabhu SR. Clitoral length in Indian newborn girls: Need for regional references. Indian Pediatr. 2016;53:289–90. doi: 10.1007/s13312-016-0838-8. [DOI] [PubMed] [Google Scholar]


