Abstract
Depression during pregnancy is common, and previous research suggests childhood adversity may increase the risk for prenatal depression. Support during pregnancy can buffer these risks, and paternal support is associated with improved maternal well-being during pregnancy. There is evidence to suggest that increased support from fathers may be particularly helpful in combatting depressive symptoms for mothers with adverse childhood experiences. The study aims to explore the role of biological father support as a protective factor against the risks associated with childhood adversity for maternal prenatal depression. Sample included 133 pregnant women recruited from two university-affiliated OB-GYN clinics serving diverse and low-income patients. Participants completed measures on childhood adversity, prenatal depressive symptoms, and father support. Results showed a significant moderating effect of father support on the relation between maternal ACEs and prenatal depressive symptoms, suggesting that higher levels of father support are protective against prenatal depressive symptoms, specifically in mothers with low-to-moderate ACEs. These results highlight the positive impact of paternal support for maternal well-being during pregnancy. Although mothers with low-to-moderate ACEs experience a buffering effect of father support, mothers with high levels of childhood adversity remain at elevated risk for prenatal depressive symptoms even with high father support. As such, screening mothers for ACEs in addition to father support may help identify those at higher risk of prenatal depression.
Keywords: Childhood adversity, Pregnancy, Prenatal depression, Father support
Introduction
Maternal prenatal depression is common, affecting up to 22% of pregnant women (Mukherjee et al. 2016; Avalos et al. 2016). Prenatal depression can have profound negative implications for mothers and their infants, including increased risk of pregnancy and birth complications such as preterm birth and low birthweight (Field et al. 2004), post-birth bonding difficulties (Shin et al. 2006), and impairments in maternal caregiving (Miller, 2002). Recent research indicates women with greater exposure to adverse childhood experiences (ACEs; including childhood abuse, neglect, and household dysfunction; Felitti et al. 1998), are at greater risk for prenatal depression (McDonnell and Valentino, 2016). Social support during pregnancy proves an important buffer against negative mental health outcomes (Nylen et al. 2013), and partner support has been shown to reduce the risk for maternal prenatal depression (Westdahl et al. 2007). Specifically, paternal support (referring to the baby’s biological father) is identified as an important contributor to maternal health (Smith and Howard, 2008; Alio et al. 2011); however, the research on biological fathers’ involvement is limited, and no research has looked at this association in the context of pregnant mothers with histories of childhood adversity. In this study, we use data from a sample of 133 pregnant women in the third trimester to examine if father support is protective against the risks associated with ACEs for maternal prenatal depression. Understanding how childhood experiences and paternal support matter for maternal well-being during pregnancy provides targets for intervention designed to improve maternal and child health and well-being.
Maternal adverse childhood experiences and prenatal depressive symptoms
Although pregnancy is often considered a time of happiness and excitement, it can also be a time for significant change and uncertainty, including shifts in hormonal levels, sleep patterns, emotions, finances, interpersonal relationships, and the onset or exacerbation of psychopathology, including depression (Slade et al. 2009; River et al. 2020). Maternal depression during pregnancy has been shown to pose considerable risks to the well-being of mothers and their infants. Studies have shown prenatal depression influences up to 22% of women during pregnancy (Mukherjee et al. 2016; Avalos et al. 2016), and prenatal depression has been identified as a risk for post-partum depression (Verreault et al. 2014). Experiencing prenatal depressive symptoms is associated with an increase of risky health behaviors during pregnancy, including alcohol and cigarette use (Flynn et al. 2007). Prenatal depression also increases risks for poor fetal and infant outcomes such as altered fetal heartrate and motor activity, neonatal behavioral development, heightened reactivity to stress and pain, fearful temperament, sleep problems, and irritability (Pearlstein, 2015; Stapleton et al. 2012). Risks associated with maternal prenatal depression do not end at birth, and depression during pregnancy has long-term implications for mothers and their children, including insecure attachment, poor infant socioemotional outcomes (Berthelot et al. 2015), lower maternal sensitivity (Carter et al. 2001), postpartum depression, and maternal functional impairment (Dunkel Schetter, 2011).
Most research on outcomes associated with early adverse life events, such as those captured by ACES, has focused on an individual’s own morbidity later in life. Studies have consistently found associations between higher levels of ACES and consequences for physical health (e.g., chronic conditions, early mortality; Felitti et al. 1998) and psychological well-being (e.g., depression, substance abuse, and suicide risk; Chapman et al. 2004; Nurius et al. 2015). Notably, studies have shown that high maternal ACEs are associated with adverse birth outcomes, including miscarriage, low birth weight, premature birth, and NICU admittance (Hillis et al. 2004; Ciciolla et al. 2021). Maternal early life adversity also increases the risk for depressive symptoms during pregnancy (Chung et al. 2008; McDonnell & Valentino, 2016) after accounting for a history of depression (Tebeka et al, 2021), and studies show women who experience 3 or more childhood traumas have a fourfold increase in odds of prenatal depression relative to women with no trauma history (Robertson-Blackmore et al. 2013).
Paternal support during pregnancy
Identifying factors that exacerbate or buffer the impact of early adversity may help parents and clinicians recognize risk or capitalize on available strengths to reduce the impact of early life exposure to adversity on prenatal depression (Chung et al. 2008). Though the psychosocial impacts that fathers contribute during pregnancy are understudied (Misra et al. 2010), research suggests that paternal support (referring to the baby’s biological father) is critical for maternal well-being during pregnancy (Smith and Howard, 2008; Alio et al. 2011). Higher rates of paternal involvement from the baby’s father during pregnancy are associated with higher levels of maternal emotional well-being, such that paternal emotional support, communication, and instrumental support serve as protective factors against antenatal depressive symptoms (Pilkington et al. 2015). Likewise, Easterbrooks and colleagues (2016) followed mothers with depression during the first two years of parenting and found that those whose depression remitted reported higher rates of satisfaction with father support compared to those whose depression persisted.
There are several domains of paternal support that prior studies have found to be relevant for maternal well-being during pregnancy including emotional and instrumental support. Higher levels of instrumental support have been linked to lower risk for giving birth to infants with low birth weight (Padilla and Reichman, 2001), and lower levels of maternal depression following childbirth (Smith and Howard, 2008). Paternal support and involvement are critical not only for maternal depressive symptoms (Cheng et al. 2016; Jonsdottir et al. 2017), but also for pregnancy health and birth outcomes, including receipt of regular prenatal care, preterm birth, and pregnancy complications (Cohen et al. 2016). Given the effects of paternal support during pregnancy are already understudied and have not yet been studied in the context of women with histories of adversity, it is important to explore the impact of father support on prenatal depression among mothers with ACEs who are already at higher risks for developing symptoms.
Current study
The current study seeks to fill a gap in the literature, exploring the role of father support (biological father of the infant), specifically in mothers with childhood adversity, in relation to prenatal depression. In consideration of previous findings, we expect that mothers with higher ACEs will report higher prenatal depression scores. We also expect that lower reports of father support will be associated with higher prenatal depressive symptoms. Lastly, we hypothesize that father support would moderate the relationship between maternal ACEs and prenatal depression scores, such that high levels of father support would be protective against prenatal depression.
Data and methods
Sample
Data for the current study are from a prospective study conducted in 2016–2017 of 177 pregnant women (aged 16–38) recruited from two university-affiliated perinatal clinics in a city in the South-Central U.S. during their first prenatal appointment. The participating clinics serve a racially diverse, socioeconomically disadvantaged and medically underserved patient population. Prospective participants were screened by nursing staff at the participating clinics, and those who met eligibility criteria (i.e., between 15–44 years of age, between 8 and 16 weeks pregnant, and planning to give birth and be a custodial parent) were provided information about the study and given the opportunity to enroll. Participants completed online surveys during each trimester of pregnancy and six times over a 22-month period post-birth and were compensated within 24 h of completing assessments via ClinCards (i.e., reloadable debit cards). The study was approved by the authors’ university Institutional Review Board. All participants provided written consent, and those under 18 provided written assent and had parental consent.
The sample for the current study was restricted to the 133 women with available data on prenatal depression collected during the third trimester survey. An attrition analysis was completed to compare the 44 participants lost to attrition between enrollment and the third trimester on relevant demographics and study variables measured at enrollment, including age, economic hardship, race, ACEs, father support, and depressive symptoms. Results from t-test and chi-squared comparisons indicated that participants lost to attrition by the third trimester were significantly younger (t(174) = 2.99, p < 0.001; Mretained = 25.9 years, Mlost = 23.05 years) and had higher depressive symptoms at enrollment (t(163) = −3.45, p < 0.001; Mretained = 14.43, Mlost = 20.63) than participants retained in the study, but did not otherwise differ on demographic or key study variables. These results suggest that participants lost to attrition were at greater risk for prenatal depressive symptoms in the third trimester and that results using the retained sample likely underestimate any reported effects.
Measures
Dependent variable
The dependent variable for the current study, maternal prenatal depression, was measured during the third trimester using the Center for Epidemiologic Studies–Depression Scale (CES-D; Radloff, 1977). Participants responded to the twenty items using a Likert scale from 0 (rarely or none of the time) to 3 (most or almost all the time). Ratings were summed to create a total score ranging from 0 to 60, with scores above 16 indicating clinically significant symptoms of depression.
Independent variables
The primary independent variable in the study was maternal childhood adversity measured using the Adverse Childhood Experiences Scale (ACES; Felitti et al. 1998), which assesses the occurrence of 10 adverse life experiences prior to the age of 18. “Yes” responses were coded as 1 and summed to create an index ranging from 0–10. The ten items assessed for emotional and physical abuse, neglect, and household dysfunction (e.g., living in a household with a parent who uses substances, having a family member incarcerated, parental separation/divorce). Items were summed for a total score, with higher scores indicating greater exposure to adverse childhood experiences.
Participants also completed the Baby’s Father Support scale (Collins et al. 1993), an 8-item validated instrument that assesses overall support received from the baby’s father, including emotional, financial, and instrumental support (e.g., providing money, helping with errands, listening to worries/concerns). Participants responded using a Likert scale, and scores were summed for a total score, with higher scores indicating higher paternal support. Factor analysis in a later article (Neter et al. 1995) revealed that the items loaded highly on one factor and were therefore summed to form a single composite. The scale has high internal consistency (alpha = 0.93; Neter et al. 1995) and is appropriate for samples with racial/ethnic diversity (Pao et al. 2019).
Covariates
Sociodemographic control variables included self-identified race/ethnicity coded into dummy variables for non-Hispanic Black, Hispanic, and Native American, with non-Hispanic White as the reference category. Age was included as a continuous variable, and residential father status was coded from a question asking participants if they were living with the baby’s biological father at the time of the first survey. Responses were coded so that 1 = married or cohabiting with the baby’s biological father and 0 = not living with the baby’s father. Economic hardship was measured using six questions utilized in previous national studies (e.g., Johnson et al. 2009; Mirowsky and Ross, 2005; Ross and Wu, 1995) that assessed for economic hardship. These included the following: In the past year, did any of the following happen to you or members of your household because of a shortage of money… “Could not pay electricity, gas, or telephone bills on times?”; “Could not pay the mortgage or rent on time?”; “Pawned or sold something?”; “Went without meals?”; “Was unable to heat home?”; “Asked for financial help from friends and family?”; “Asked for help from welfare/community organizations?” Responses were coded as 0 = “no” and 1 = “yes” and were summed for a total score ranging from 0–6, with higher scores indicating a higher level of economic hardship.
Analytic strategy
Hierarchical linear regression conducted in Statistical Package for the Social Sciences (SPSS v28.0) was used to examine the associations between study variables, adjusting for sociodemographic characteristics. In models 1 and 2, maternal ACEs and father support were added, respectively. Model 3 included the interaction term between ACEs and father support, and model 4 added demographic covariates, including race, age, residential father status, and economic hardship.
Results
Table 1 presents descriptive statistics for study variables for the overall sample and by low (0–2), moderate (3–5), and high (6 +) ACEs to maintain consistency with previous literature showing that the association between ACEs and psychosocial functioning tends to follow a graded dose–response relationship (Felitti et al. 1998; Ciciolla et al. 2021). Of the sample, 39.4% of participants reported their race/ethnicity as White; 28% as Black, 13.6% as Hispanic, and 17.8% as Native American. Participants reported a fairly high depression score on average (M = 15.08; range 1–47), with approximately 38.3% of participants endorsing clinically significant symptoms above the cutoff point of 16 (Roberts and Vernon, 1983). The average ACE score was 3.25 (SD = 2.93), and average father support score was 27.35 (SD = 8.07). The most frequently reported ACE was parent separation/divorce (63.9%), followed by verbal abuse (48.5%) and emotional neglect (33.8%) (see Fig. 1). Furthermore, the sexual abuse and household violence ACE categories were reported only by participants in the moderate and high ACE groups, with no participants in the low ACE group reporting these experiences. Results of univariate analysis of variance (ANOVA) and chi-squared tests indicated that participants in the current sample with the highest ACEs were more likely to report economic hardship, were more likely to report their racial identity as White, and less likely to report their racial identity as Black (see Table 1).
Table 1.
Descriptive statistics for study variables and demographics by low, moderate, and high ACEs
| Full sample n = 133 |
0–2 ACEs n = 64 |
3–5 ACEs n = 38 |
6 + ACEs n = 31 | ANOVA or Chi-square | |
|---|---|---|---|---|---|
| Variables |
M (SD)
% (n) |
M (SD)
% (n) |
M (SD)
% (n) |
M (SD)
% (n) |
FACEs or χ2 |
| Depressive symptoms | 15.08 (9.64) | 13.36 (9.72) | 16.29 (10.41) | 17.13 (8.04) | 2.03 |
| Total ACE score | 3.25 (2.93) | 0.67 (.74) | 4.03 (.79) | 7.61 (1.17) | 685.65** |
| Father support scale | 27.35 (8.07) | 28.72 (6.65) | 25.00 (9.61) | 27.24 (8.45) | 2.51 |
| Age (years) | 25.86 (5.6) | 26.03 (4.93) | 25.92 (4.93) | 25.45 (6.45) | .11 |
| Residing with baby’s father (yes/no) | 52.6% (70) | 50% (32) | 50% (19) | 61.3% (19) | 1.22 |
| Economic hardship | 1.52 (1.87) | 1.07 (1.53) | 1.74 (2.06) | 2.17 (2.09) | 4.01* |
| Race | |||||
| Black/African American | 28% (37) | 34.9% (22) | 31.6% (12) | 9.7% (3) | 6.89* |
| Native American | 17.8% (24) | 20.6% (13) | 10.8% (4) | 22.6% (7) | 1.99 |
| Hispanic | 13.6% (18) | 9.5% (6) | 23.7% (9) | 9.7% (3) | 4.57 |
| White | 39.4% (52) | 34.9% (22) | 31.6% (12) | 58.1% (18) | 6.03* |
ACE, adverse childhood experiences; residential father = living with biological father of the baby; economic hardship is scored 0–6, with higher scores indicating greater economic hardship;
p < .05;
p < .01
Fig. 1.
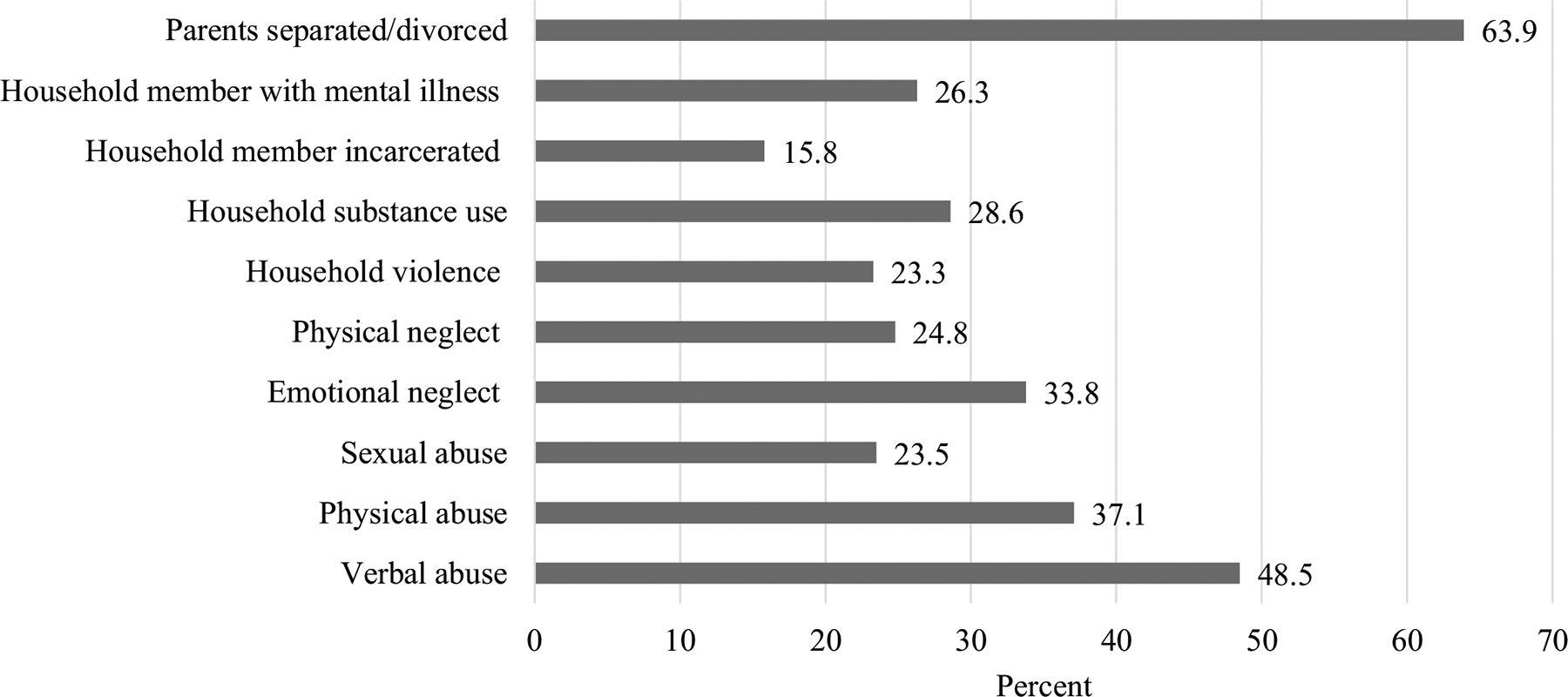
Percentage of responses to each of the 10 items on the adverse childhood experiences (ACEs) questionnaire. n = 133
Table 2 presents the results from the hierarchical linear regression analysis. Model 1 indicated that participants with higher ACE scores reported significantly higher levels of prenatal depression, F(1, 120) = 4.34, p < 0.05. With the addition of father support, model 2 indicated that mothers reporting higher father support scored lower on prenatal depression, F(2, 119) = 13.43, p < 0.01, and ACEs was no longer significant. In model 3, the addition of the interaction term between ACEs and father support indicated a statistically significant moderating effect, F(3, 118) = 11.23, p < 0.01. Finally, model 4 included covariates of race, age, economic hardship, and residential father status, F(9, 112) = 5.51, p < 0.01. Follow-up analyses calculated and graphed the simple slopes of the significant interaction at low (FS = 18.95), mean (FS = 27.15), and high (FS = 35.00) levels of father support (see Fig. 2). Results of the simple slopes analysis and the Johnson Neyman procedure indicated that the relation between father support and prenatal depression is statistically significant for values of ACEs below 5.18 (low-to-moderate ACEs), and that the relation between ACEs and prenatal depression is significant for values of father support above 29.55. That is, higher father support (FS > 29.55) was associated with lower prenatal depressive symptoms relative to those with average to low father support among participants with a low-to-moderate history of ACEs (ACEs < 5.18). Participants with high ACEs showed consistently high levels of prenatal depressive symptoms at all levels of father support.
Table 2.
Hierarchical regression estimating third trimester prenatal depressive symptoms
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | β | b | SE | β | b | SE | β | b | SE | β | |
| Total ACE Score | .61 | .29 | .19* | .51 | .27 | .16 | − 1.85 | 1.02 | − .56 | − 1.93 | 1.04 | − .59 |
| Father support scale | − .46 | .10 | − .39** | − .77 | .16 | − .65** | − .69 | .16 | − .58** | |||
| ACEs × father support | .08 | .04 | .78* | .08 | .04 | .78* | ||||||
| Covariates | ||||||||||||
| Residential father | − .38 | 1.77 | − .02 | |||||||||
| Economic hardship | .83 | .47 | .16 | |||||||||
| Age | − .32 | .15 | − .19* | |||||||||
| Black/African American | .96 | 2.08 | .04 | |||||||||
| Native American | 4.81 | 2.29 | .19* | |||||||||
| Hispanic | .42 | 2.58 | .01 | |||||||||
| Intercept | 13.15** | 1.28 | 25.96** | 2.99 | 34.99** | 4.77 | 39.29** | 6.41 | ||||
| Adj. R2 | .03* | .17** | .20** | .25** | ||||||||
n = 121; ACE, adverse childhood experiences; residential father = living with biological father of the baby; economic hardship is scored 0–6, with higher scores indicating greater economic hardship;
p < .05;
p < .01
Fig. 2.
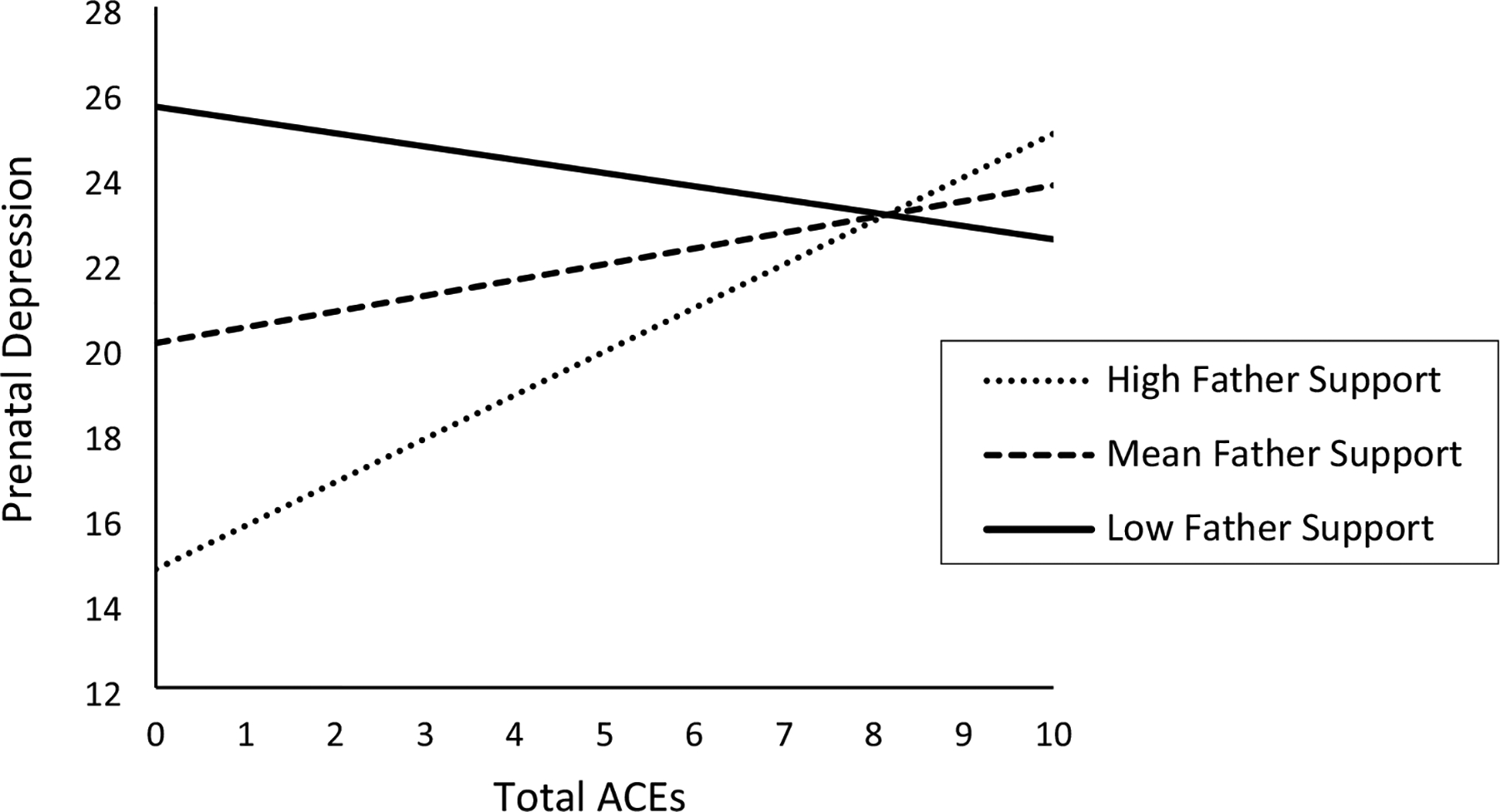
The simple slopes of prenatal depression symptoms on adverse childhood experiences (ACEs) total score at low (FS = 18.95), mean (FS = 27.15), and high (FS = 35.00) levels of father support. The Johnson Neyman procedure indicates that the relation between father support and prenatal depression is statistically significant for values of ACEs below 5.18 (low to moderate ACEs), and that the relation between ACEs and prenatal depression is significant for values of father support above 29.55
Discussion
Findings from the current study suggest that adverse childhood experiences increase the risk for symptoms of prenatal depression and that father support may serve as a protective factor against prenatal depression symptoms. Specifically, mothers who reported receiving greater support from fathers reported lower symptoms of prenatal depression; however, this protective effect was found only among women with low to moderate ACE scores less than 5.13. Notably, mothers with higher ACE scores had consistently high symptoms of prenatal depression at all levels of father support and did not experience a protective effect from high father support, suggesting that a more severe history of childhood adversity is an especially potent risk factor for prenatal depression.
Pregnancy is a critical period of transition in a woman’s life, which Slade et al. (2009) considered to be the “developmental crisis of pregnancy”—a crucial period that influences the health and well-being of mother and child. Early life experiences of adversity may interfere with mothers’ ability to cope with changes during pregnancy and the anticipated role of caregiver (Slade et al. 2009). If a mother’s own needs were unmet by her caregiver, she may feel psychologically unprepared to meet the needs of her own child or provide a safe environment (Huth-Bocks et al. 2013). Moreover, memories of childhood abuse and neglect have the potential of evoking thoughts and feelings that can exacerbate symptoms of prenatal depression (Choi and Sikkema, 2016; Huth-Bocks et al. 2013), particularly in the context of pregnancy when repeated physical exams associated with routine obstetric care may be salient trauma reminders. In alignment with previous literature positing maternal early life adversity increases the risk for depressive symptoms during pregnancy (Chung et al. 2008; McDonnell and Valentino, 2016; Tebeka et al, 2021; Robertson-Blackmore et al. 2013), our findings suggest the effects of childhood adversity on prenatal depression are potent and even high levels of father support may not serve to protect against these risks.
Over half of our sample (52.7%) reported living with the biological father of their infant, and it is important to recognize the contributing factors of intimate or romantic relationships on maternal mental health, especially in women with histories of adversity. Previous work shows romantic relationships that are experienced as low quality may be reminders of neglect and abuse experienced during childhood and can serve as confirmation of previously formed schemas or beliefs about the self and others (Wright et al. 2009). Young (1999) theorized that these maladjusted schemas are formed within the context of childhood maltreatment, whereby childhood adversity may contribute to the expectation that others are threatening or to beliefs about one’s worthlessness and fear of being abandoned by others. For example, childhood adversity has been associated with lower quality of romantic relationships (River et al. 2020), which may be a result of the self-fulfilling belief that romantic partners are inaccessible and non-supportive. Furthermore, Colman and Widom (2004) found that women with histories of abuse or neglect were less likely to perceive their partners as caring, supportive, and open to communication, which may help to explain why mothers with high ACEs still had elevated depressive symptoms despite reporting high levels of father support. Histories of childhood maltreatment have also been associated with an increased likelihood to experience intimate partner violence in adulthood (McMahon et al. 2015), which may also contribute to poorer mental health outcomes in women with high ACEs.
It is also important to consider the social determinants of health related to our findings given the demographic makeup of our sample. Firstly, childhood adversity is negatively associated with income potential, adult education, and employment status (Metzler et al. 2017), suggesting those with histories of adversity may be more likely to experience economic hardship as adults (Nurius et al. 2012). Furthermore, our sample included women of racially marginalized groups (e.g., non-Hispanic Black Americans and Native Americans/Alaskan Natives), and although our analyses did not indicate specific risk associated with racial identity, there is substantial research indicating that racially marginalized groups have high rates of exposure to childhood adversity, including racism, and are more likely to experience economic hardship (Goldstein et al. 2021; Nurius et al. 2012). Furthermore, experiencing financial hardship as a new mother has been shown to increase antenatal and postpartum depressive symptoms (Rich-Edwards et al. 2006). Within our study, the additional stress of financial hardships in women with a history of childhood adversity may have exacerbated depressive symptoms during pregnancy and further reduced any potential benefit from having a supportive father.
Strengths
This study fills a gap in the literature by exploring the importance of paternal support from the biological father of the infant for maternal prenatal mental health among mothers with histories of childhood adversity. The current study has several notable strengths, including a diverse sample of low-income pregnant women with higher ACE scores than the national average (Giano et al. 2020). Furthermore, rather than retrospective reports of paternal support, the study is prospective and captures current perceptions of father support and prenatal depressive symptoms.
Limitations and future directions
Despite its strengths, this study has several limitations that should be addressed in future research. Firstly, our variables only capture support of the baby’s biological father and do not consider support from other parental figures or partners (i.e., stepfathers, grandparents, same-sex partners, or romantic partners that are not biologically related to the baby). As previous research exhibits the positive influence of general social support for mothers (Nylen et al. 2013), it is important to recognize support may come from a variety of different figures in the baby’s life and is not limited to their biological father. Additionally, future research should examine how father involvement and support matter across pregnancy and into the postpartum period. It is unclear whether we will continue to see a strong buffering impact of paternal support on maternal well-being over time, particularly in the first year following childbirth, as the transition to parenthood can be particularly stressful for all parents (Nyström and Öhrling, 2004) and especially for women with a history of trauma (Seng et al. 2013). Second, our data only included maternal reports of father support. Whereas maternal perceptions of father support may be particularly meaningful for her own mental health outcomes, they may not be as accurate as if we had father reports or objective measures of fathers’ involvement and support. Future research should integrate multiple reporters or more objective indicators of support.
Implications of study findings
This study has important implications for health care providers who work with women during pregnancy. Although there has been increased attention in recent years to the importance of prenatal screening for depression (Gaynes et al. 2005), trauma histories and emotional distress often go unrecognized during routine prenatal care visits (Durant et al. 2000; Roter et al. 1995; Sperlich et al. 2017). Probing both adverse childhood experiences as well as paternal support will help providers identify women who might be at risk for having or developing prenatal depression, and women may benefit from more focused interventions. Reducing depression during pregnancy can help prevent postpartum depression (Field et al. 2010), which has critical implications for infant development (Barker et al. 2011). Education on healthy relationships can also help women determine if their partners are meeting their needs, assist them with promotive conflict resolution, and help them identify and meet their needs for support (River et al. 2020). Similarly, psychoeducation programs on the effects of ACEs developed to address pregnancy specific needs have been shown to be beneficial for women with histories of adversity in regard to mental health outcomes (e.g., Seng et al. 2011). Lastly, our findings have important implications for engaging fathers during pregnancy and highlight the impact father support can have on maternal mental health and well-being.
Acknowledgements
The authors would like to thank the HATCH Project participating clinics, and particularly Drs. Karen Gold, Jameca Price, and Lance Frye for their support. For more information, contact: Karina M. Shreffler.
Funding
This research was supported by the National Institute of General Medical Sciences of the National Institutes of Health (P20GM109097; Jennifer Hays-Grudo, PI). Funding for open access publication was supported by the Cyndy Ellis-Purgason Endowed Chair held by KS at the University of Oklahoma Health Sciences Center, Fran and Earl Ziegler College of Nursing.
Footnotes
Conflict of interest The authors declare no competing interests.
References
- Alio AP, Bond MJ, Padilla YC, Heidelbaugh JJ, Lu M, Parker WJ (2011) Addressing policy barriers to paternal involvement during pregnancy. Matern Child Health J 15:425–430. 10.1007/s10995-011-0781-1 [DOI] [PubMed] [Google Scholar]
- Avalos LA, Raine-Bennett T, Chen H, Adams AS, Flanagan T (2016) Improved perinatal depression screening, treatment, and outcomes with a universal obstetric program. Obstet Gynecol 127(5):917. 10.1097/AOG.0000000000001403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker ED, Jaffee SR, Uher R, Maughan B (2011) The contribution of prenatal and postnatal maternal anxiety and depression to child maladjustment. Depress Anxiety 28(8):696–702. 10.1002/da.20856 [DOI] [PubMed] [Google Scholar]
- Berthelot N, Ensink K, Bernazzani O, Normandin L, Luyten P, Fonagy P (2015) Intergenerational transmission of attachment in abused and neglected mothers: the role of trauma-specific reflective functioning. Infant Ment Health J 36(2):200–212. 10.1002/imhj.21499 [DOI] [PubMed] [Google Scholar]
- Carter AS, Garrity-Rokous FE, Chazan-Cohen R, Little C, Briggs-Gowan MJ (2001) Maternal depression and comorbidity: predicting early parenting, attachment security, and toddler social-emotional problems and competencies. J Am Acad Child Adolesc Psychiatry 40(1):18–26. 10.1097/00004583-200101000-00012 [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF (2004) Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord 82(2):217–225. 10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- Cheng E, Rifas-Shiman S, Perkins M, Rich-Edwards J, Gillman M, Wright R, Taveras E (2016) The influence of antenatal partner support on pregnancy outcomes. J Women’s Health 25(7):672–679. 10.1089/jwh.2015.5462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KW, Sikkema KJ (2016) Childhood maltreatment and perinatal mood and anxiety disorders: a systematic review. Trauma Violence Abuse 17(5):427–453. 10.1177/1524838015584369 [DOI] [PubMed] [Google Scholar]
- Chung EK, Mathew L, Elo IT, Coyne JC, Culhane JF (2008) Depressive symptoms in disadvantaged women receiving prenatal care: the influence of adverse and positive childhood experiences. Ambul Pediatr 8(2):109–116. 10.1016/j.ambp.2007.12.003 [DOI] [PubMed] [Google Scholar]
- Ciciolla L, Shreffler KM, Tiemeyer S (2021) Maternal childhood adversity as a risk for perinatal complications and NICU hospitalization. J Pediatr Psychol 46(7):801–813. 10.1093/jpepsy/jsab027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen K, Capponi S, Nyamukapa M, Baxter J, Crawford A, Worly B (2016) Partner involvement during pregnancy and maternal health behaviors. Matern Child Health J 20:2291–2298. 10.1007/s10995-016-2048-3 [DOI] [PubMed] [Google Scholar]
- Collins NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC (1993) Social support in pregnancy: psychosocial correlates of birth outcomes and postpartum depression. J Pers Soc Psychol 65(6):1243. 10.1037/0022-3514.65.6.1243 [DOI] [PubMed] [Google Scholar]
- Colman RA, Widom CS (2004) Childhood abuse and neglect and adult intimate relationships: a prospective study. Child Abuse Negl 28(11):1133–1151. 10.1016/j.chiabu.2004.02.005 [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C (2011) Psychological science on pregnancy: stress processes, biopsychosocial models, and emerging research issues. Annu Rev Psychol 62:531–558. 10.1146/annurev.psych.031809.130727 [DOI] [PubMed] [Google Scholar]
- Durant T, Colley Gilbert B, Saltzman LE, Johnson CH (2000) Opportunities for intervention: discussing physical abuse during prenatal care visits. Am J Prev Med 19:238–244. 10.1016/S0749-3797(00)00232-4 [DOI] [PubMed] [Google Scholar]
- Easterbrooks M, Kotake C, Raskin M, Bumgarner E (2016) Patterns of depression among adolescent mothers: resilience related to father support and home visiting program. Am J Orthopsychiatry 86(1):61. 10.1037/ort0000093 [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, … and Bendell D (2004) Prenatal depression effects on the fetus and the newborn. Infant Behav Dev 27(2):216–229. 10.1016/j.infbeh.2003.09.010 [DOI] [Google Scholar]
- Field T, Diego M, Hernandez-Reif M (2010) Prenatal depression effects and interventions: a review. Infant Behav Dev 33(4):409–418. 10.1016/j.infbeh.2010.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med 14(4):245–258. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Flynn HA, Walton MA, Chermack ST, Cunningham RM, Marcus SM (2007) Brief detection and co-occurrence of violence, depression and alcohol risk in prenatal care settings. Arch Womens Ment Health 10(4):155–161. 10.1007/s00737-007-0188-6 [DOI] [PubMed] [Google Scholar]
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. (2005) Perinatal depression: prevalence, screening accuracy, and screening outcomes. Summary. AHRQ Evid Rep Summ 119 Agency for Healthcare Research and Quality. Rockville, MD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giano Z, Wheeler DL, Hubach RD (2020) The frequencies and disparities of adverse childhood experiences in the US. BMC Public Health 20(1):1–12. 10.1186/s12889-020-09411-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein E, Topitzes J, Miller-Cribbs J, Brown RL (2021) Influence of race/ethnicity income on the link between adverse childhood experiences and child flourishing. Pediatr Res 89(7):1861–1869. 10.1038/s41390-020-01188-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS (2004) The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics 113(2):320–327. 10.1542/peds.113.2.320 [DOI] [PubMed] [Google Scholar]
- Huth-Bocks AC, Krause K, Ahlfs-Dunn S, Gallegher E, Scott S (2013) Relational trauma and posttraumatic stress syndrome among pregnant women. Psychodynamic Psychiatry 41(2):277–301. 10.1521/pdps.2013.41.2.277 [DOI] [PubMed] [Google Scholar]
- Johnson DR, McQuillan J, Jacob MC, Greil AL, Lacy N, Scheuble LK, … and Young R (2009) National survey of fertility barriers: methodology report for wave 1 [Google Scholar]
- Jonsdottir S, Thome M, Steingrimsdottir T, Lydsdottir L, Sigurdsson J, Olafsdottir H, Swahnberg K (2017) Partner relationship, social support and perinatal distress among pregnant Icelandic women. Women Birth 30:46–e55. 10.1016/j.wombi.2016.08.005 [DOI] [PubMed] [Google Scholar]
- McDonnell CG, Valentino K (2016) Intergenerational effects of childhood trauma: evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreat 21(4):317–326. 10.1177/1077559516659556 [DOI] [PubMed] [Google Scholar]
- McMahon K, Hoertel N, Wall MM, Okuda M, Limosin F, Blanco C (2015) Childhood maltreatment and risk of intimate partner violence: a national study. J Psychiatr Res 69:42–49. 10.1016/j.jpsychires.2015.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC (2017) Adverse childhood experiences and life opportunities: shifting the narrative. Child Youth Serv Rev 72:141–149. 10.1016/j.childyouth.2016.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LJ (2002) Postpartum depression. JAMA 287(6):762–765. 10.1001/jama.287.6.762 [DOI] [PubMed] [Google Scholar]
- Mirowsky J, and Ross CE (2005) Aging, status, and sense of control (ASOC). New York, NY: Aldine de Gruyter [Google Scholar]
- Misra DP, Caldwell C, Young AA, Abelson S (2010) Do fathers matter? Paternal contributions to birth outcomes and racial disparities. Am J Obstet Gynecol 202(2):99–100. 10.1016/j.ajog.2009.11.031 [DOI] [PubMed] [Google Scholar]
- Mukherjee S, Trepka MJ, Pierre-Victor D, Bahelah R, Avent T (2016) Racial/ethnic disparities in antenatal depression in the United States: a systematic review. Matern Child Health J 20(9):1780–1797. 10.1007/s10995-016-1989-x [DOI] [PubMed] [Google Scholar]
- Neter E, Collins NL, Lobel M, Dunkel Schetter C (1995) Psychosocial predictors of postpartum depressed mood in socioeconomically disadvantaged women. Women’s Health: Res Gender, Behav, Policy 1(1):51–75 [PubMed] [Google Scholar]
- Nurius PS, Logan-Greene P, Green S (2012) Adverse childhood experiences (ACE) within a social disadvantage framework: distinguishing unique, cumulative, and moderated contributions to adult mental health. J Prev Interv Community 40(4):278–290. 10.1080/10852352.2012.707443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurius PS, Green S, Logan-Greene P, Borja S (2015) Life course pathways of adverse childhood experiences toward adult psychological well-being: a stress process analysis. Child Abuse Negl 45:143–153. 10.1016/j.chiabu.2015.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylen KJ, O’Hara MW, Engeldinger J (2013) Perceived social support interacts with prenatal depression to predict birth outcomes. J Behav Med 36(4):427–440. 10.1007/s10865-012-9436-y [DOI] [PubMed] [Google Scholar]
- Nyström K, Öhrling K (2004) Parenthood experiences during the child’s first year: literature review. J Adv Nurs 46(3):319–330. 10.1111/j.1365-2648.2004.02991.x [DOI] [PubMed] [Google Scholar]
- Padilla YC, Reichman NE (2001) Low birthweight: do unwed fathers help? Child Youth Serv Rev 23(4–5):427–452. 10.1016/S01907409(01)00136-0 [DOI] [Google Scholar]
- Pao C, Guintivano J, Santos H, Meltzer-Brody S (2019) Postpartum depression and social support in a racially and ethnically diverse population of women. Arch Womens Ment Health 22(1):105–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlstein T (2015) Depression during pregnancy. Best Pract Res Clin Obstet Gynaecol 29:754–764. 10.1016/j.bpobgyn.2015.04.004 [DOI] [PubMed] [Google Scholar]
- Pilkington P, Milne L, Cairns K, Lewis J, Whelan T (2015) Modifiable partner factors associated with perinatal depression and anxiety: a systematic review and meta-analysis. J Affect Disord 178:165–180. 10.1016/j.jad.2015.02.023 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1(3):385–401 [Google Scholar]
- Rich-Edwards JW, Kleinman K, Abrams A, Harlow BL, McLaughlin TJ, Joffe H, Gillman MW (2006) Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health 60(3):221–227. 10.1136/jech.2005.039370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- River LM, Narayan AJ, Atzl VM, Rivera LM, Lieberman AF (2020) Past made present: the legacy of childhood maltreatment for romantic relationship quality and psychopathology during pregnancy. Psychol Viol 10(3):324–333. 10.1037/vio0000273 (ISSN: 2152–0828) [DOI] [Google Scholar]
- Roberts RE, Vernon SW (1983) The center for epidemiologic studies depression scale: its use in a community sample. Am J Psychiatry 140(1):41–46. 10.1176/ajp.140.1.41 [DOI] [PubMed] [Google Scholar]
- Robertson-Blackmore E, Putnam FW, Rubinow DR, Matthieu M, Hunn JE, Putnam KT, … and Thomas GO (2013) Antecedent trauma exposure and risk of depression in the perinatal period. J Clin Psychiatry 74(10):811. 10.4088/JCP.13m08364 [DOI] [PubMed] [Google Scholar]
- Ross CE, Wu CL (1995) The links between education and health. Am Sociol Rev 60:719–745. 10.2307/2096319 [DOI] [Google Scholar]
- Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP (1995) Improving physicians’ interviewing skills and reducing patients’ emotional distress. A randomized clinical trial. Arch Intern Med 155:1877–1884. 10.1001/archinte.1995.00430170071009 [DOI] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, Rowe H, Cameron H, Harris A, Rauch SA, Bell SA (2011) The survivor moms’ companion: open pilot of a posttraumatic stress specific psychoeducation program for pregnant survivors of childhood maltreatment and sexual trauma. Int J Childbirth 1(2):111–121. 10.1891/2156-5287.1.2.111 [DOI] [Google Scholar]
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I (2013) Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. J Midwif Women’s Health 58(1):57–68. 10.1111/j.1542-2011.2012.00237.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin H, Park YJ, Kim MJ (2006) Predictors of maternal sensitivity during the early postpartum period. J Adv Nurs 55(4):425–434. 10.1111/j.1365-2648.2006.03943.x [DOI] [PubMed] [Google Scholar]
- Slade A, Cohen LJ, Sadler LS, Miller M (2009) The psychology and psychopathology of pregnancy. Handbook Infant Mental Health 3:22–39 [Google Scholar]
- Smith LE, Howard KS (2008) Continuity of paternal social support and depressive symptoms among new mothers. J Fam Psychol 22(5):763–773. 10.1037/a0013581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperlich M, Seng JS, Li Y, Taylor J, Bradbury-Jones C (2017) Integrating trauma-informed care into maternity care practice: conceptual and practical issues. J Midwifery Womens Health 62(6):661–672. 10.1111/jmwh.12674 [DOI] [PubMed] [Google Scholar]
- Stapleton L, Schetter C, Rini C, Hobel C, Westling E, Glynn L, Sandman C (2012) Perceived partner support in pregnancy predicts lower maternal and infant distress. J Fam Psychol 26(3):453–463. 10.1037/a0028332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebeka S, Le Strat Y, Etain B, Ray M, Mullaert J, Dubertret C, IGEDEPP Study Group (2021) Childhood trauma and perinatal depression: data from the IGEDEPP cohort. J Clin Psychiatry 82(5):20m13664. 10.4088/JCP.20m13664 [DOI] [PubMed] [Google Scholar]
- Verreault N, Da Costa D, Marchand A, Ireland K, Dritsa M, Khalifé S (2014) Rates and risk factors associated with depressive symptoms during pregnancy and with postpartum onset. J Psychosom Obstet Gynecol 35(3):84–91. 10.3109/0167482X.2014.947953 [DOI] [PubMed] [Google Scholar]
- Westdahl C, Milan S, Magriples U, Kershaw TS, Rising SS, Ickovics JR (2007) Social support and social conflict as predictors of prenatal depression. Obstet Gynecol 110(1):134–140. 10.1097/01.AOG.0000265352.61822.1b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright MO, Crawford E, Del Castillo D (2009) Childhood emotional maltreatment and later psychological distress among college students: the mediating role of maladaptive schemas. Child Abuse Negl 33:59–68. 10.1016/j.chiabu.2008.12.007 [DOI] [PubMed] [Google Scholar]
- Young JE (1999). Cognitive therapy for personality disorders: A schema-focused approach (3rd ed.). Professional Resource Press/Professional Resource Exchange [Google Scholar]


