Abstract
Hosting an international outbreak response team can pose a challenge to jurisdictions not familiar with incident management frameworks. Basic principles of team forming, organizing, and executing mission critical activities require simple and flexible communication that can be easily understood by the host country’s public health leadership and international support agencies. Familiarity with incident command system principles before a public health emergency could save time and effort during the initial phases of the response and aid in operationalizing and sustaining complex field activities throughout the response. The 2009 initial outbreak of H1N1 in Mexico highlighted the importance of adequately organizing and managing limited resources and expertise using incident management principles. This case study describes logistical and operational aspects of the response and highlights challenges faced during this response that may be relevant to the organization of public health responses and incidents requiring international assistance and cooperation.
Keywords: emergency management, outbreaks, incident command system, international agencies, public health
INTRODUCTION
Management of an outbreak investigation and associated response of an infectious agent with pandemic potential can pose logistical and operational challenges. Sustaining such a complex response requires an incident management system with sufficient logistical and operational capacity to support the needs of various subject matter experts, such as database managers, epidemiologists, laboratorians, virologists, public health specialists, risk communicators, information technologists, and anthropologists.1 Additionally, it requires resources beyond subject matter experts.2,3 The 2009 H1N1 outbreak in Mexico served as a reminder for public health agencies of the importance of having strong logistical and operational support during public health emergencies.
Mexican health authorities noticed the outbreak in mid-April and activated the Mexican National Pandemic Plan after cases were confirmed as HIN1 Influenza. An international response team arrived at the end of April and within a few days established an incident command system (ICS) to manage the response. The ICS is widely known for facilitating the integration and coordination of all emergency resources and managing a response under one incident commander with one set of objectives. Various versions of ICS (including the United Nation cluster system and the hospital ICS) have increasingly been recognized among public health agencies and healthcare settings as effective systems for organizing public health emergency responses, including disease outbreaks.4–9
Under the ICS, operations and logistics sections fall within the general staff functions (Figure 1). These sections are fundamental to the overall performance of the response and to successful accomplishment of the objectives as established by the incident commander or incident command (IC). During a public health response, operations and logistics manage and support public health field teams by requesting and coordinating provision of resources needed to sustain the response operations. The field teams are typically small, multidisciplinary organizations (called “task forces” in ICS terminology) that focus on the medical or scientific aspects of the response, generally relying on the ICS structure for resource support.
Figure 1.
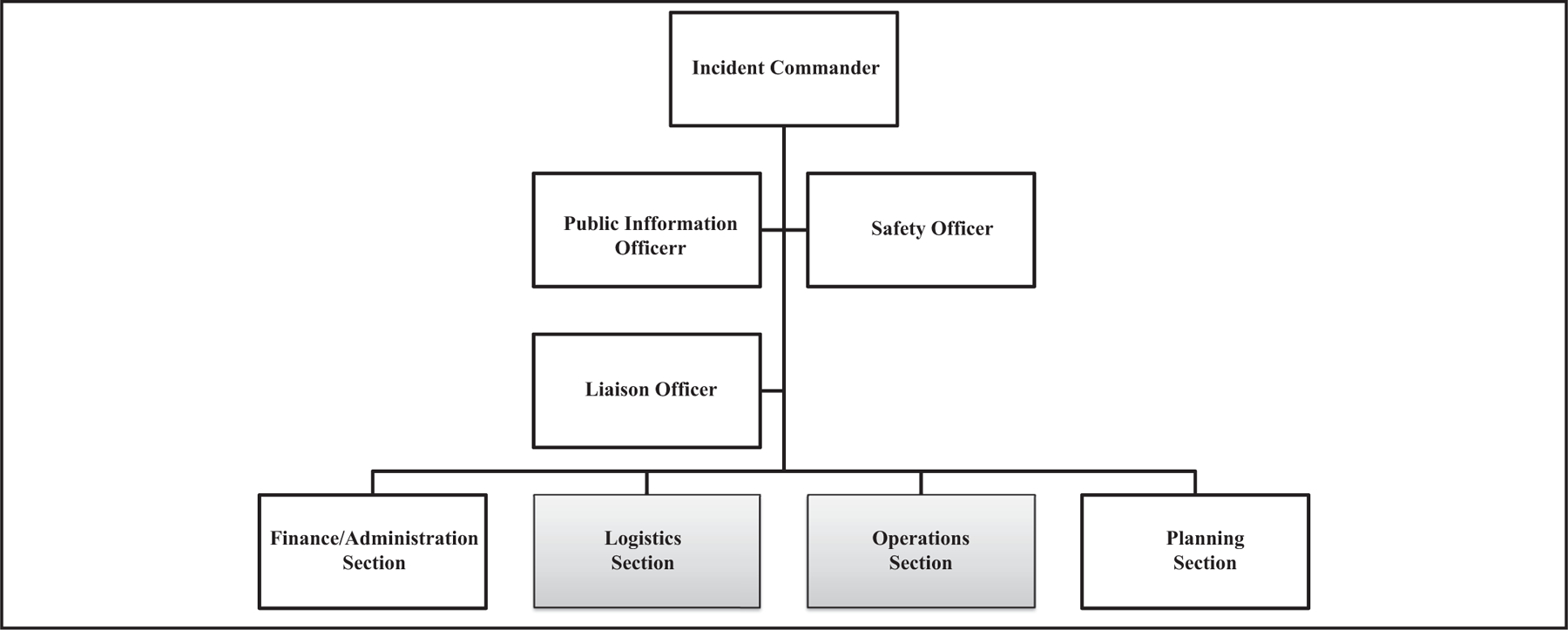
Traditional ICS framework. Source: FEMA.GOV.
Logistical duties during outbreak responses include arranging international travel, local transportation, specimen shipping and tracking, purchasing medical and pharmaceutical supplies and equipment, arranging customs clearances, maintaining facility safety and security, and staffing the supporting Emergency Operations Center (EOC).10 The operations section is responsible for managing outbreak activities, teams, resources, and supporting field activities related to the public health operation according to the IC intent.
Aspects of the epidemiological, medical, and public health response associated with the H1N1 outbreak response have been previously discussed in the literature.11–13 For the purpose of this discussion, we share our unique perspective as members of the international response team operations and logistics sections for the team deployed to Mexico during the initial phase of the outbreak of H1N1. We focus on the operational and logistical challenges faced by the joint international team and on the benefits of using an ICS approach to organize this initial outbreak response. Not all disease outbreak events are similar; some may not require full implementation of an organizational framework. However, from the operational and organizational perspectives of future outbreak responses, particularly those involving multiple jurisdictions, the Mexican H1N1 response experience demonstrates the benefits of deciding on the organizational framework early in the response. The experience also shows how systems like ICS can provide familiarity and flexibility needed during outbreak responses.
INITIAL OUTBREAK RESPONSE
On April 12, 2009, the National Epidemiological Surveillance System of the Mexico Ministry of Health (MMOH) identified reports of severe pneumonia cases in the states of Oaxaca, San Luis Potosi, and in Mexico City.11 In the days that followed, a marked increase in cases of respiratory illness was noted, triggering a national epidemiologic alert which was reported to the World Health Organization (WHO). On April 12, US health authorities notified WHO of a similar cluster of cases in California and Texas.11 After these cases were confirmed as H1N1 influenza, the Mexican National Pandemic Plan was activated. To minimize the spread of the illness,14 MMOH moved swiftly to implement its national pandemic response plan. It initiated community mitigation measures and nonpharmaceutical interventions and took the following measures:
provided health education;
closing institutions and businesses;
banning public gatherings and activities;
isolating ill people at home; and
conducting rapid screenings of business patrons and private and public sector workers for signs of illness.
The use of nonpharmaceutical interventions including increased hand washing, social distancing, and wearing personal protective equipment (PPE) such as masks, was encouraged. These preventive efforts brought to a halt most activities in Mexico City, which has a metropolitan area population of approximately 20 million residents.15,16
As the public health response evolved, a number of international public health agencies including the US Centers for Disease Control and Prevention (CDC), the Public Health Agency of Canada (PHAC), and the WHO/Pan-American Health Organization (PAHO) deployed personnel to Mexico to support the MMOH-led response and initial outbreak investigation. Most international team members were Spanish speakers and began arriving on April 24, 2009.
OPERATIONAL AND ORGANIZATIONAL ASPECTS
Public health response operations of the international team consisted mainly of providing technical support, implementing a number of epidemiological studies, and augmenting the various MMOH public health teams established for surveillance, laboratory, and risk communication. Outbreak activities were coordinated from the MMOH EOC located at the Direccion General Adjunta de Epidemiologia or DGAE (General Directorate of Epidemiology) within the MMOH in Mexico City. Figure 2 describes the organizational incident management structure adopted by MMOH, WHO/PAHO, and CDC in Mexico for the H1N1 outbreak.
Figure 2.
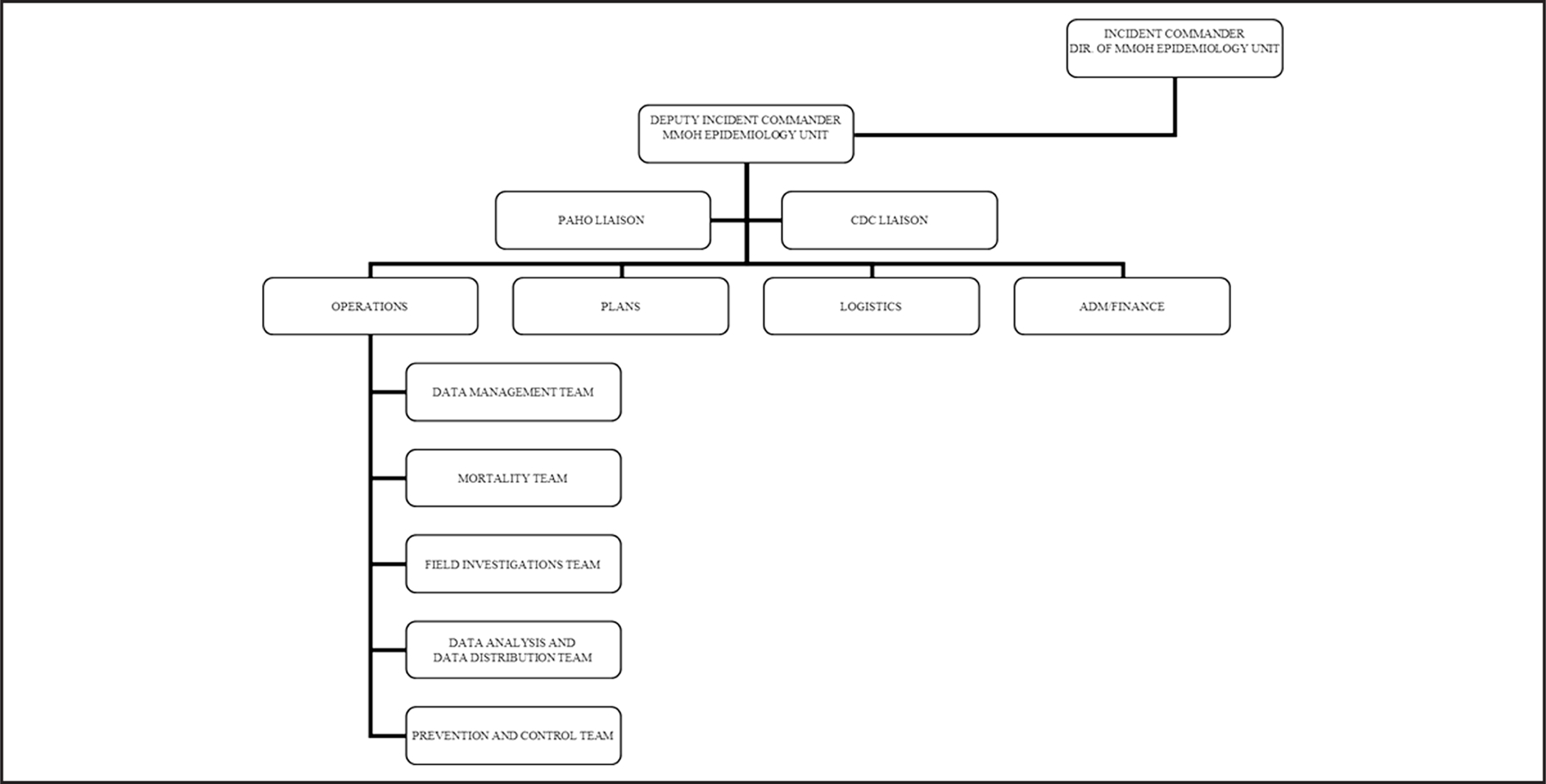
Incident management structure adopted by international team during the H1N1 initial outbreak response in Mexico.
The MMOH designated the director of DGAE as incident commander (IC) for the international response according to the ministry’s pre-existing pandemic influenza response plans. The Command Staff, composed of the director’s deputy and international agency liaisons, supported the IC. A general staff that included operations, planning, logistics, and a combined administration and finance section was also established.
With the exception of the Administration and Finance Section, which was staffed solely by MMOH personnel, the remaining elements of the general staff operated as joint sections under Unified Command (UC) principles. UC is often used in multijurisdictional or multiagency incident management to enable agencies with different legal, geographic, and functional responsibilities to effectively coordinate, plan, and interact while maintaining their individual authority, responsibilities, and accountability. Under UC, agencies manage jointly with a common set of incident or outbreak response objectives and strategies.4 In this case, the agencies shared operations section leadership functions. The operations section directed five joint functional teams: data management, mortality, field investigation, analysis and diffusion, and prevention and control. Field teams were deployed to the other Mexican states to evaluate hospitals and community surveillance systems and to conduct reviews of medical records in healthcare facilities. Public health teams visited homes of identified cases to conduct interviews, collect laboratory specimens, and ascertain transmissibility and risk factors for the disease for cases and contacts. The MMOH EOC in Mexico City coordinated all support activities for the field teams. The Director of DGAE and his deputy performed planning and coordination activities with all the agency leads under Unified Command on leadership meetings which were held twice a day.
Before the arrival of the international team, work and rest schedules were not yet well established, and many of the dedicated public health professionals were working long hours to keep pace with the required tasks. Stakeholders including citizens, media, and government increased domestic and international pressure to characterize this event as soon as possible, a reasonable expectation for an outbreak with pandemic potential. This pressure created a need to pace the staff for what was expected to be a long response, lasting weeks or even months. Additional international personnel were brought in to assist with various outbreak investigation tasks, alleviating MMOH staff workload. In addition, implementation of a stricter daily work schedule and a shuttle-like transportation system allowed for adequate rest periods and flexibility to move team members around the various worksites and facilities.
LOGISTICAL AND OPERATIONAL CHALLENGES
Logistical systems, which often require considerable skill and experience, are fundamental for maintaining response operations and managing large amounts of purchased materials or donations.1,17 MMOH, CDC, and logistics staff from WHO established and jointly staffed the MMOH logistics and resource center. In addition to coordinating transportation, communications, and lodging, the logistics team conducted needs assessments in collaboration with the international staff to address existing stocks of medical supplies, requisition new supplies, and meet an immediate need for the conduct of medical logistics training for MMOH. MMOH personnel were not familiar with WHO logistics software and procedures. WHO conducted “just in time training” for the DGAE logistics personnel to address this need. As a result of the training, the MMOH logistics team was able to effectively manage storage, medical prophylaxis, requisition of PPE, laboratory testing, and other supplies necessary to support field team operations in the federal district and other Mexican states.
Response kits, which included specimen collection supplies, transport media, storage materials (ice coolers, dry ice, or ice packs), PPE, and antivirals such as Tamiflu for team prophylaxis, were developed and stored within the DGAE. These kits helped ensure field teams were protected and had sufficient supplies to conduct their missions. These teams, or “brigades” as they are known in Mexico, consisted mostly of staff from medical schools, other public health programs, and international members under the supervision of DGAE.
Local gaps in supply chain logistics were evident during the initial outbreak investigation, which led to delays in launching field teams. These gaps included initial shortages of supplies and the lack of coordination and control of distribution of materials with the military authorities. After the WHO/PAHO team-provided logistics training, the MMOH/DGAE began to develop a permanent reserve and established adequate stock levels of basic laboratory and testing supplies to cover ongoing field work and investigations during the influenza outbreak in anticipation of potential supply shortages. Our experience showed that having adequate stock levels can be an effective tool to compensate for delays in receiving replacement orders or for market shortages. This type of capacity building could also provide a better foundation for responding immediately to other types of national public health emergencies.
This incident emphasized the need for an operational logistics position inside the DGAE. The duties of this position could include establishing mechanisms to address future medical and laboratory supply chain gaps. CDC and WHO assisted DGAE logistics personnel in researching existing logistics training provided by other government agencies in Mexico such as the Sistema Nacional de Proteccion Civil, Mexico’s Emergency Management Agency.18
OUTBREAK RESPONSE LESSONS LEARNED
The magnitude and scope of H1N1 in Mexico presented an unprecedented challenge to all agencies involved. On the basis of our experience and field observations during the H1N1 response in Mexico, we have identified lessons that could be applied to future outbreak responses. Agencies could consider the following:
Anticipating supply and logistic shortfalls in support of field operations and implementing a standardized system for maintaining stocks of essential supplies. The creation of a joint logistics team enabled the rapid coordination of logistics efforts including requisitioning, purchasing, and managing bulk donations and private donations of services and equipment. Acquiring and training a logistics officer on the software could be helpful for this purpose.
Training staff in international logistics including acquiring supplies, shipping specimens, and managing customs requirements as quickly and efficiently as possible.
Maintaining permanent reserves or stock levels of essential items with a minimum buffer stock prior to a national emergency. This reserve would allow teams to conduct field work and investigations while a more reliable resupply chain is established. Partners could provide simple logistics training for its partners, so that reliable permanent stocks can be maintained for public health emergencies. Establishing standardized operational procedures for accessing global purchasing mechanisms could also help alleviate this issue.
Collaborating with respective embassies and consulates to explore efficient means for supporting logistics for all incident response personnel.
Integrating other emergency agencies as part of the public health team. During our experience in Mexico, military authorities and emergency managers from Sistema Nacional de Proteccion Civil were not part of the actual public health incident management team. As a result, public health struggled with transportation and logistics issues instead of asking for help from a more experienced group. Emergency management agencies in Mexico are trained in ICS in preparation for natural disasters such as earthquakes, hurricanes, and volcanic eruptions. The public health program could consider incorporating personnel from other agencies into the incident management structure particularly in the areas of logistics management, transportation, safety, and security. This goal might be accomplished using or developing mutual aid agreements with other organizations that have strong logistics capabilities like the military, the Civil Protection Agency, UN agencies, international NGOs, or private logistics training services.
DISCUSSION
During this response, the team faced several unprecedented operational and logistical challenges, such as shortages of basic laboratory supplies and PPE supplies for equipping field teams even when trying to purchase supplies in open markets. Other countries trying to buy the same emergency resources reduced the existing inventory of available resources. At times, procuring equipment proved to be over-whelming to the public health logistics team, run by personnel not trained in logistics. For future events, both strong logistical training and support for managing all aspects of the supply chain are needed, including the requisition of medical material and the management of donated medical material goods. The issues faced by the joint logistics team could have been minimized by having MMOH staff trained to manage health and medical logistics operations during a large public health emergency. The “just in time” logistics training provided by WHO provided a good base of knowledge for ad hoc logistics staff, and implementing that formal training in public health logistics systems is a fundamental activity needed for future events. Despite many logistical and supply shortfalls and challenges, epidemiological studies and enhanced surveillance activities were safely and successfully conducted in Mexico.
This incident demonstrated the utility of using an ICS-based incident management system. The decision to use an ICS-based system was not arbitrary or one sided. Rather, it was the result of analysis and discussion of the best option for organizing the operation. The implementation of an ICS-based incident management system occurred as a result of early discussions between senior emergency operations staff from each of the various international teams. The unity of command created a stronger focus on the objectives as one unified team rather than as separate components. ICS has enhanced public health emergency management and operations by providing an easy-to-understand framework for managing responses. ICS has increasingly been used in the last few years for various types of public health events and activities.19
Over the past several years, ICS has demonstrated broad applications for all-hazard public health responses.5,6,20–22 ICS has been used during core public health operations ranging from organizing toxicological and infectious disease outbreak investigations, responses to a pandemic, vaccinations campaigns, and natural disasters.8,9,23–30 Given this record of success, international public health agencies that provide operations and logistical support might want to consider providing basic ICS and specific function (logistics, operations, etc) training for staff.
CONCLUSION
Logistics and operations are essential to a successful public health response. Often, the primary tasks of any public health response are choosing an operational framework and assessing the logistical capabilities for sustaining the response. The response to the H1N1 event reinforced the importance of key operational concepts like ICS that can be applied to execute the incident commander’s intent and for managing field teams. The H1N1 international response in Mexico highlighted the benefits of MMOH public health responders having a basic understanding of the ICS concept for management and long-term support of the response. This response also demonstrated that field teams deployed during complex, international responses can still achieve a high level of integration and efficiency if they are supported by strong logistics and operations sections. A full understanding of the utility of ICS still has to be demonstrated by public health agencies. However, additional evidence-based approaches could reveal more about the effectiveness of the ICS framework for managing all-hazard public health responses.
Contributor Information
Miguel A. Cruz, Office of Environmental Health Emergencies, US Centers for Disease Control and Prevention, Atlanta, Georgia..
Nicole M. Hawk, Office of Public Health Preparedness and Response, US Centers for Disease Control and Prevention, Atlanta, Georgia..
Christopher Poulet, Division of Regional Operations, Agency for Toxic Substances and Disease Registry, Denver, Colorado..
Jose Rovira, Emergency and Humanitarian Assistance, World Health Organization, Geneva, New York..
Edward N. Rouse, Office of Public Health Preparedness and Response, US Centers for Disease Control and Prevention, Atlanta, Georgia..
REFERENCES
- 1.Cruz-Vega F, Sun C, Brink B, et al. : 5th Asia-Pacific Conference on Disaster Medicine. Theme 6: multidisciplinary team interaction: summary and action plan. Prehosp Disaster Med 2001; 16(1): 39–41. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization: Guiding principles for international outbreak alert and response. Available at http://www.who.int/csr/outbreaknetwork/guidingprinciples/en/. Accessed July 20, 2010.
- 3.Pesik N, Keim M: Logistical considerations for emergency response resources. Pacific Health Dialog. 2002; 9: 97–103. [PubMed] [Google Scholar]
- 4.Department of Homeland Security: National Incident Management System. December 2008. Available at http://www.fema.gov/pdf/emergency/nims/NIMS_core.pdf. Accessed February 15, 2014.
- 5.Zane R, Prestipino AL: Implementing the hospital emergency incident system: An integrated delivery system’s experience. Prehosp Disaster Med 2004; 19(4): 311–317. [DOI] [PubMed] [Google Scholar]
- 6.Kim-Ferley RJ, Celentano JT, Gunter C, et al. : Standardized emergency management system and response to a smallpox emergency. Prehosp Disaster Med 2003; 18(4): 313–320. [DOI] [PubMed] [Google Scholar]
- 7.King RV, North CS, Larkin GL, et al. : Attributes of effective disaster responders: Focus group discussions with key emergency response leaders. Disaster Med Public Health Prep 2010; 4: 332–338. [DOI] [PubMed] [Google Scholar]
- 8.Cruz MA, Keim ME, Schier JG, et al. : Organizational and command aspects for coordinating the public health response to an outbreak of acute renal failure, Republic of Panama, 2006. Prehosp Disaster Med 2011; 26: 219–225. [DOI] [PubMed] [Google Scholar]
- 9.Papagiotas SS, Frank M, Bruce S, et al. : From SARS to 2009 H1N1 influenza: The evolution of a public health incident management system at CDC. Public Health Rep 2012; 127: 267–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mignone AT, Davidson R: Public health response actions and the use of emergency operations centers. Prehosp Disaster Med 2003; 18: 217–218. [DOI] [PubMed] [Google Scholar]
- 11.CDC: Swine influenza A (H1N1) infection in two children— Southern California, April 2009. MMWR Morb Mortal Wkly Rep 2009; 58: 400–402. [PubMed] [Google Scholar]
- 12.Global Alert and Response (GAR)—Influenza-like illness in the United States and Mexico. World Health Organization. Available at http://www.who.int/csr/don/2009_04_24/en/. Accessed May 25, 2009.
- 13.CDC: Outbreak of swine-origin influenza A (H1N1) virus infection—Mexico, March-April 2009. MMWR Morb Mortal Wkly Rep 2009; 58: 467–470. [PubMed] [Google Scholar]
- 14.Cordova JA, Sarti E, Arzoz-Padres J, et al. : The Influenza A (H1N1) epidemic in Mexico. Lessons learned. Health Res Policy Syst 2009; 7: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stern AM, Markel H: What Mexico taught the world about pandemic influenza preparedness and community mitigation strategies. JAMA 2009; 302: 1221–1222. [DOI] [PubMed] [Google Scholar]
- 16.Aburto NJ, Pevzner E, Lopez-Ridaura R, et al. : Knowledge and adoption of community mitigation efforts in Mexico during the 2009 H1N1 pandemic. Am J Prev Med 2010; 39: 395–402. [DOI] [PubMed] [Google Scholar]
- 17.Donahue AK, Tuohy RV: Lessons we don’t learn: A study of the lessons of disasters, why we repeat them, and how we can learn them. Homeland Secur Aff 2006; 2: 1–28. [Google Scholar]
- 18.Secretaria de Gobernación: Sistema Nacional de Protección Civil. Available at http://www.proteccioncivil.gob.mx/. Accessed September 26, 2013.
- 19.Burkle FM, Hsu EB, Loehr M, et al. : Definition and functions of health unified command and emergency operations centers for large-scale bioevent disasters within the existing ICS. Disaster Med Public Health Prep 2007; 1: 135–141. [DOI] [PubMed] [Google Scholar]
- 20.Akselrod H, Mercon M, Kirkeby R, et al. : Creating a process for incorporating epidemiological modeling into outbreak management decisions. J Bus Contin Emer Plan. 2012; 6: 68–83. [PubMed] [Google Scholar]
- 21.Powers R: Organization of a hospital-based victim decontamination plan using the incident command structure. Disaster Manag Response. 2007; 5: 119–123. [DOI] [PubMed] [Google Scholar]
- 22.Elledge BL, Boatright DT, Woodson P, et al. : Learning from Katrina: Environmental health observations from the SWCPHP response team in Houston. J Environ Health. 2007; 70: 22–26. [PubMed] [Google Scholar]
- 23.Freedman AM, Mindlin M, Morley C, et al. : Addressing the gap between public health emergency planning and incident response. Disaster Health. 2013; 1: 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guh A, Heyman ML, Barden D, et al. : Lessons learned from the investigation of a cluster of cutaneous anthrax cases in Connecticut. J Public Health Manag Pract 2010; 16: 201–210. [DOI] [PubMed] [Google Scholar]
- 25.Adams EH, Scanlon E, Callahan JJ, et al. : Utilization of an incident command system for a public health threat: West Nile virus in Nassau County, New York, 2008. J Public Health Manag Pract 2010; 16: 309–315. [DOI] [PubMed] [Google Scholar]
- 26.Enanoria WT, Crawley AW, Tseng W, et al. : The epidemiology and surveillance response to pandemic influenza A (H1N1) among local health departments in the San Francisco Bay area. BMC Public Health. 2013; 13: 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamberlain AT, Seib K, Wells K, et al. : Perspectives of immunization program managers on 2009–10 H1N1 vaccination in the United States: a national survey. Biosecur Bioterror 2012; 10: 142–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porter D, Hall M, Hartl B, et al. : Local health department 2009 H1N1 influenza vaccination clinics-CDC staffing model comparison and other best practices. J Public Health Manag Pract 2011; 17: 530–533. [DOI] [PubMed] [Google Scholar]
- 29.Fishbane M, Kist A, Schieber RA: Use of the emergency incident command system for school-located mass influenza vaccination clinics. Pediatrics. 2012; 129(S): 101–106. [DOI] [PubMed] [Google Scholar]
- 30.Ringel JS, Chandra A, Leuschner KJ, et al. : Lessons learned from the state and local response to hurricane Katrina. Working Paper. Rand. Gulf States Policy Institute and RAND Health, February 2007. Available at http://www.rand.org/content/dam/rand/pubs/working_papers/2007/RAND_WR473.pdf. Accessed December 20, 2013.


