Abstract
Non-hepatic causes of hyperammonaemia are uncommon relative to hepatic aetiologies. An adolescent female was admitted to the hospital with a diagnosis of very severe aplastic anaemia. During her treatment with immunosuppressive therapy, she developed neutropenic enterocolitis, pseudomonal bacteraemia and hyperammonaemia. A combination of intermittent haemodialysis and high-volume continuous veno-venous haemodiafiltration (CVVHDF) was required to manage the hyperammonaemia. Despite a thorough investigation, there were no hepatic, metabolic or genetic aetiologies identified that explained the hyperammonaemia. The hyperammonaemia resolved only after the surgical resection of her inflamed colon, following which she was successfully weaned off from the renal support. This is a novel case report of hyperammonaemia of non-hepatic origin secondary to widespread inflammation of the colon requiring surgical resection in an immunocompromised patient. This case also highlights the role of high-volume CVVHDF in augmenting haemodialysis in the management of severe refractory hyperammonaemia.
Keywords: Haematology (drugs and medicines), Infection (gastroenterology), Hepatitis other, Haematology (incl blood transfusion), Paediatric intensive care
Background
Hyperammonaemia is characterised by elevated levels of ammonia in the blood. It can lead to significant neurotoxicity, which may present as an altered level of consciousness and, if left untreated, can progress to coma and death.1 Ammonia is an essential molecule in human metabolism and is used to produce glutamine.2 It is primarily generated by the gastrointestinal (GI) tract, with a smaller proportion being generated in the renal tubules. It is metabolised in the liver into urea and excreted in urine as urea and ammonium. An overabundance of ammonia can occur when the production increases or elimination is reduced. Hyperammonaemia is most commonly attributed to liver failure, though urea cycle disorders must be closely considered. In the context of non-hepatic hyperammonaemia, there are a number of other important diagnostic considerations which have implications for the management of these patients during their acute presentation.3
Here, we present a case of severe non-hepatic hyperammonaemia in a patient with very severe aplastic anaemia.
Case presentation
An adolescent female was diagnosed with very severe aplastic anaemia following an episode of acute hepatitis of unknown origin. Her liver enzymes were found to be elevated (alanine transaminase (ALT): 1235 µ/L; aspartate transaminase (AST): 1257 µ/L; alkaline phosphatase: 129 µ/L; bilirubin, total: 296 µmol/L; bilirubin, conjugated: 246 µmol/L; bilirubin, unconjugated: 50 µmol/L; gamma-glutamyltransferase (GGT): 82 U/L). Although the liver biopsy done at the time of initial presentation was suggestive of a viral aetiology, serologies were negative for common hepatotropic viruses (hepatitis A, B, C, Epstein-Barr virus, cytomegalovirus, toxoplasmosis and parvovirus). Her liver enzymes and function subsequently normalised, suggestive of hepatic recovery. Four weeks later, she presented with pancytopenia (white cell count: 1.73×109/L; red cell count: 2.87×1012/L; hemoglobin: 83 g/L; platelet count: 10×109/L, absolute neutrophil count: 1.25×109/L) and marked bone marrow hypocellularity (estimated at 10%), consistent with very severe aplastic anaemia. The bone marrow biopsy showed hypocellularity for age, absent/markedly reduced trilineage haematopoiesis, morphologically negative for dysplasia and underlying haematolymphoid neoplasm. A comprehensive inherited bone marrow failure workup did not yield an alternative diagnosis or cause. Severe aplastic anaemia following acute hepatitis is a well-known entity and was postulated to be the triggering event in this case.4
Her medical history is significant for cochlear implants at age three for profound congenital sensorineural hearing loss (SNHL), migraine headaches, anxiety, cholestasis, gallstones, previous tonsillectomy and adenoidectomy, and a benign thyroid nodule. Of note, the patient’s mother has a history of SNHL.
Treatment
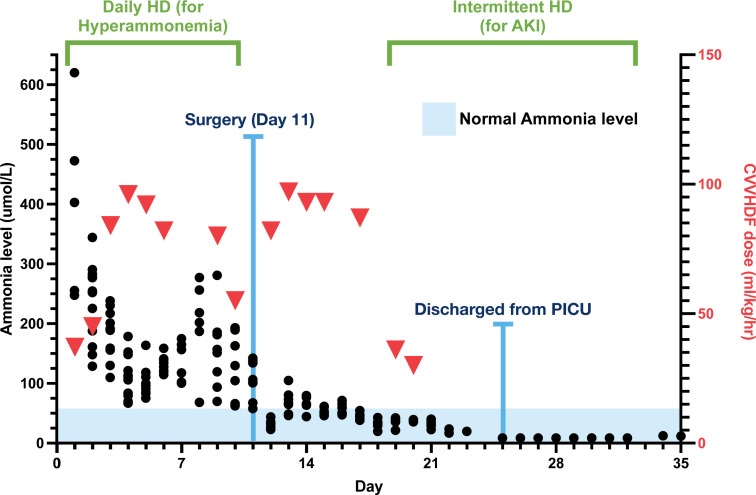
Once the diagnosis of very severe aplastic anaemia was confirmed, the patient was started on immunosuppressive therapy (IST) (corticosteroids, horse anti-thymocyte globulin (h-ATG), ciclosporin and eltrombopag) given the absence of a suitably matched sibling donor.5 While receiving IST, she developed neutropenic enterocolitis and pseudomonal bacteraemia. Neutropenic enterocolitis is a common consequence of prolonged neutropenia and IST.6 She was treated with broad-spectrum antibiotics (piperacillin and tazobactam) for bacteraemia and prescribed bowel rest and analgesics for neutropenic enterocolitis. Despite appropriate antimicrobial therapy and conservative management, she had persistent abdominal pain requiring intravenous pain control. She subsequently deteriorated, acutely developing a decreased level of consciousness requiring transfer to the paediatric intensive care unit (PICU) for further management. This episode correlated with a high serum ammonia level (620 µmol/L). Figure 1 depicts ammonia levels over time, with day 1 representing the day on which her ammonia level was 620 µmol/L and her admission to the PICU. A CT head was performed on day 1, and it found that there was no evidence of bleeding or oedema.
Figure 1.
Ammonia level (µmol/L) indicated by black dots. Cumulative CVVHDF over 24 hours (ml/kg/hour) is shown by red triangles. A normal ammonia level of less than 50 µmol/L is indicated in blue/shaded area. AKI, acute kidney injury, CVVHDF, continuous veno-venous haemodiafiltration; HD, haemodialysis; PICU, paediatric intensive care unit.
On transfer to the PICU, the patient was intubated for controlled ventilation and initiated haemodialysis. After the first treatment with haemodialysis, there was a modest improvement in the ammonia level (620 to 247 µmol/L), but it rebounded after a few hours (figure 1). To facilitate ongoing reduction of the ammonia levels and prevent rebound, she was put on continuous veno-venous haemodiafiltration (CVVHDF). It is important to note that her required dose of CVVHDF to keep the ammonia level in the acceptable range was 90 mL/kg/hour (dialysate 4000 mL/hour+pre-replacement and post-replacement fluids 4000 mL/hour), which is much higher than the dose generally prescribed in critically ill patients (30–50 mL/kg/hour). Her ammonia levels were maintained in the acceptable range using a combination of daily haemodialysis and CVVHDF. Concomitantly, the aetiology of this patient’s hyperammonaemia was under investigation. Given her age and medical history of SNHL, suspicion for a late presentation of a urea cycle disorder was high, specifically ornithine transcarbamylase (OTC) deficiency. Therefore, she was empirically started on L-arginine, sodium benzoate and sodium phenylacetate which promote the removal of ammonium ions. Benzoate conjugates with glycine to form hippurate and phenylacetate conjugates with glutamine to form phenylacetylglutamine. Both hippurate and phenylacetylglutamine are hydrophilic and are excreted in urine.7 As there was no improvement with this therapy, she was also given a therapeutic trial of carglumic acid for presumptive deficiency of N-acetyl glutamate synthase. None of these therapies impacted her ammonia levels or requirement for renal support.
On day 4 of the PICU admission, her neurological status improved with the patient waking on assessment at 22:35. The ammonia level at this time was 67 µmol/L. On day 5, the patient had purposeful movement at 11:30 and was extubated. The ammonia level at this time was 84 µmol/L. The threshold ammonia level that we were targeting was at least below 100 µmol/L, as neurological symptoms usually start once levels are above 100–150 µmol/L.8 Postextubation, her primary issue remained refractory hyperammonaemia and ongoing abdominal pain. She continued daily haemodialysis in combination with high-dose CVVDHF. Several attempts were made to wean off CVVHDF; however, a significant rise in ammonia levels occurred with every attempt. She remained febrile and neutropenic. The option of surgical intervention was discussed with the general surgery team in view of persistent abdominal symptoms, but given the high complication rate associated with surgery in a neutropenic patient, the decision was made to proceed with ongoing conservative management. However, over the subsequent days, she reported progressive abdominal symptoms. A repeat CT scan of the abdomen showed increasing inflammatory changes in the ascending colon and no evidence of perforation. On day 11 of the PICU admission, she became haemodynamically unstable and was taken for an emergent laparotomy. Intraoperatively, she was found to have extensive inflammation of the ascending colon from the cecum to the hepatic flexure and significant large bowel wall oedema and no perforation. Pathology confirmed findings consistent with neutropenic enterocolitis with patchy necrosis and marked oedema (online supplemental figure 1). She underwent a right hemicolectomy with end ileostomy. In the days following surgical resection, she showed a progressive decline in ammonia levels, allowing the dose of CVVHDF to be weaned.
bcr-2023-256225supp001.pdf (13.3MB, pdf)
Outcome and follow-up
She made a complete neurological recovery and was discharged from PICU once she was off of the CVVHDF. Intermittent haemodialysis was continued for the next 2 weeks for the management of acute renal failure, not for hyperammonaemia. While her renal function normalised, she continued in the hospital for ongoing medical management pending neutrophil recovery. Four and a half months post-IST, her very severe aplastic anaemia relapsed with progressive bone marrow failure, including severe neutropenia, and ultimately underwent a 9/10 matched related donor bone marrow transplant (BMT). She was conditioned using treosulfan, fludarabine, cyclophosphamide and alemtuzumab without further episodes of hyperammonaemia through her transplant or post-transplant course.
Discussion
Hyperammonaemia results from increased production or decreased elimination of ammonia, or a combination of both. Hepatic failure is the most common cause of disruption to the ammonia elimination pathway, followed by urea cycle disorders. Less commonly, acquired hyperammonaemia is due to urease-producing organism infections9 10 and as a postsurgery complication following gastric bypass surgery.11 12 Another rare cause of non-hepatic hyperammonaemia was a case of a patient with a bowel perforation.13 Hyperammonaemia in the paediatric population is rare, particularly in immunosuppressed paediatric patients, though previous cases have been published; one due to a drug reaction,14 one due to urea cycle disorder15 and five due to infection.16–18
This case highlights the importance of a thorough history of recent trauma, short bowel and kidney disease, pregnancy and postpartum stress and GI bleeding, given that these have been reported as a trigger for urea cycle disorders and resultant hyperammonaemia.19
This patient underwent extensive whole-exome testing for a suspected urea cycle defect, in particular OTC deficiency, and we did not identify a genetic cause for a urea cycle defect. Blueprint genetics whole-exome DNA sequencing with comprehensive hearing loss and deafness panel plus hyperammonaemia and urea cycle disorder panel (ID 99851), which covers 4080 regions within 249 genes, did not identify an underlying genetic cause for hyperammonaemia. The metabolic workup also did not support an underlying urea cycle defect. An organic acid profile was performed day 2 and orotic acid was not found in the urine. Plasma glutamine level was mildly elevated at 845 µmol/L (ref: 240–800) on day 2, and on day 10, plasma glutamine was normal at 358 µmol/L. On day 2, citrulline was low at 5 µM and remained low <5 µM on day 10. Generally, low amino acid levels were observed on day 10 (proline, glycine, alanine, citrulline, valine, cystine, methionine, isoleucine, leucine, lysine and histidine). This clinical picture is unclear but could point to an underlying subclinical metabolic process that was exacerbated by our patient’s clinical course.
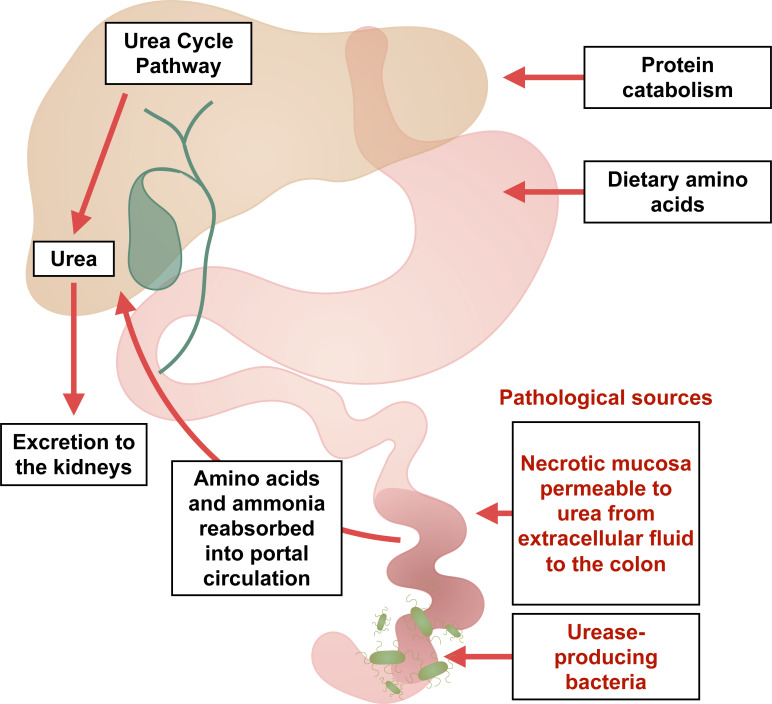
In our patient, there was a significant decrease in ammonia levels following resection of the bowel, much like a previously reported case when ammonia levels normalised after the hemicolectomy of a perforated bowel.13 However, our case was in a paediatric patient, and there was no bowel wall perforation. We propose that the cause of the hyperammonaemia was secondary to enterocolitis and necrotic bowel. Hyperammonaemia secondary to enterocolitis has been reported in humans and is hypothesised to be caused by urease-producing bacteria in the gut.20 To the best of our knowledge, this is the first case report of hyperammonaemia secondary to enterocolitis in a paediatric patient with an underlying diagnosis of severe aplastic anaemia. In our patient, ammonia levels were more than three times higher than those previously published (1055 µg/dL (620 mmol/L) compared with 324 µg/dL (190 mmol/L)).20 We hypothesise this could be secondary to profound neutropenia and dampened immune response. The proposed three-step mechanism for this phenomenon is: first, because of the immunodeficiency, the colon was colonised by an organism that damaged the patient’s mucosal lining. The damaged and eventually necrotic mucosa became permeable to urea which passed from the extracellular fluid into the colon. Second, this provided abundant substrate for an increased population of urease-producing bacteria in the diseased intestine leading to excessive production of ammonia from the breakdown of proteins and urea.21 Third, the abundant absorption of ammonia from the bowel lumen into the circulation was facilitated through an inflamed and necrosed mucosa22 (figure 2). Despite pursuing a haematopoietic stem cell transplant, she did not experience further hyperammonaemia, which supports our hypothesis that the aetiology was due to increased production within the inflamed GI tract. Furthermore, extensive genetic testing judiciously excluded non-GI causes of hyperammonaemia. This careful approach facilitated our patient to move forward with subsequent BMT.
Figure 2.
A schematic representation of the sources of ammonia production and its excretory pathway. Ammonia is primarily generated by the small intestine, metabolised in the liver into urea and subsequently excreted in urine as urea and ammonium. The liver’s urea cycle pathway becomes the most vital process to eliminate ammonia. The ammonia level can become high if there is a problem in liver, urea cycle pathway or if they both are normal but are overwhelmed by increased production. In our case, we propose a pathological additional source of ammonia in the colon via urease-producing bacteria and increased absorption of ammonia through the necrosed bowel.
The high blood flow rate in intermittent haemodialysis rapidly clears the ammonia making it a preferred modality.23 However, like our case, post haemodialysis rebound has been reported in the literature.24 To overcome the issue of rebound, CVVHDF has been used in combination with haemodialysis.25 In CVVHDF, ammonia clearance is closely related to the ultrafiltration rate.26 High-volume ultrafiltration has been successfully used in the management of hyperammonaemia in a few case reports.27 28 Our case affirms the utility of high-volume CVVHDF in conjunction with intermittent haemodialysis in managing acute hyperammonaemia.
Clinicians should consider GI pathology as a cause of high ammonia levels, especially in patients who have refractory disease in the absence of an underlying hepatic or metabolic aetiology. This should be further considered in immunocompromised patients, who have heightened complications with neutropenic enterocolitis. This case contributes to the limited body of data on hyperammonaemia with an unknown underlying genetic or metabolic cause, emphasising the importance of a broad differential diagnosis. This case also highlights the utility of high-volume (90 mL/kg/hour) CVVHDF in ammonia clearance.
Patient’s perspective.
When I first became unwell, I felt my life flip like a switch. I went from being a healthy normal kid to fighting for my life within weeks. I’ve faced obstacles and challenges that I never thought even existed. I learned things that I felt I was too young to know. I have become a stronger person and more aware of myself and my health. I went from being diagnosed with SAA to being in induced comas and dealing with ammonia levels so high that we didn’t know how I would make it out. As I lay in the hospital bed listening to doctors and nurses try to figure out what was wrong, I convinced myself to keep fighting daily. Being sick has taken a mental and physical toll on me, but I never let it take over; I fought. I’ve been through test on test, medications on medications, and I’ve even heard the worst news you could imagine. I now live with a colostomy bag which I hated more than anything, but I’ve realized it saved my life when I went septic, so I’ll forever be thankful for it. I learned to walk again; I spent months on months in the hospital with kidney problems, ammonia levels, comas, bone marrow treatment and much more. Nine months after my initial hospitalization, I had a bone marrow transplant with my dad as my donor, and I’ve been doing amazing since. What matters most is I’m here today. I’ve become so strong. I’ve learned so much. I am someone completely different, and that’s a blessing because I have learned so much about life and to never take it for granted. I’ll forever be thankful for the IWK and all my amazing doctors and nurses.
Learning points.
Ammonia levels should be considered in patients with acute enterocolitis who present with altered level of consciousness.
In the absence of an underlying metabolic disorder, one should consider gastrointestinal pathology as the cause of high ammonia levels.
High-dose (as high as 90 mL/kg/hour) continuous veno-venous haemodiafiltration can be used to maintain ammonia levels in an acceptable range.
Footnotes
@adrienne_borrie
Contributors: The following authors were responsible for drafting of the text, sourcing and editing of clinical images, investigation results, drawing original diagrams and algorithms, and critical revision for important intellectual content: AEB, MP, NV and SV. The following authors gave final approval of the manuscript: AEB, MP, NV and SV.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1. Walker V. Ammonia metabolism and hyperammonemic disorders. Adv Clin Chem 2014;67:73–150. 10.1016/bs.acc.2014.09.002 [DOI] [PubMed] [Google Scholar]
- 2. Adeva MM, Souto G, Blanco N, et al. Ammonium metabolism in humans. Metabolism 2012;61:1495–511. 10.1016/j.metabol.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 3. Bachmann C. Mechanisms of hyperammonemia. Clin Chem Lab Med 2002;40:653–62. 10.1515/CCLM.2002.112 [DOI] [PubMed] [Google Scholar]
- 4. Weiler-Normann C, Hartl J, Weidemann S, et al. Acute hepatitis as a Prequel to very severe aplastic anemia. Z Gastroenterol 2018;56:51–4. 10.1055/s-0043-121737 [DOI] [PubMed] [Google Scholar]
- 5. Peffault de Latour R, Kulasekararaj A, Iacobelli S, et al. Eltrombopag added to immunosuppression in severe aplastic anemia. N Engl J Med 2022;386:11–23. 10.1056/NEJMoa2109965 [DOI] [PubMed] [Google Scholar]
- 6. Alioglu B, Avci Z, Ozcay F, et al. Neutropenic enterocolitis in children with acute leukemia or aplastic anemia. Int J Hematol 2007;86:364–8. 10.1532/IJH97.E0739 [DOI] [PubMed] [Google Scholar]
- 7. Husson M-C, Schiff M, Fouilhoux A, et al. Efficacy and safety of I.V. sodium Benzoate in urea cycle disorders: a multicentre retrospective study. Orphanet J Rare Dis 2016;11:127. 10.1186/s13023-016-0513-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kundra A, Jain A, Banga A, et al. Evaluation of plasma ammonia levels in patients with acute liver failure and chronic liver disease and its correlation with the severity of hepatic encephalopathy and clinical features of raised intracranial tension. Clin Biochem 2005;38:696–9. 10.1016/j.clinbiochem.2005.04.013 [DOI] [PubMed] [Google Scholar]
- 9. Stergachis AB, Mogensen KM, Khoury CC, et al. A retrospective study of adult patients with noncirrhotic hyperammonemia. J Inherit Metab Dis 2020;43:1165–72. 10.1002/jimd.12292 [DOI] [PubMed] [Google Scholar]
- 10. Bharat A, Cunningham SA, Scott Budinger GR, et al. Disseminated Ureaplasma infection as a cause of fatal hyperammonemia in humans. Sci Transl Med 2015;7:284re3. 10.1126/scitranslmed.aaa8419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fenves AZ, Shchelochkov OA, Mehta A. Hyperammonemic syndrome after Roux-en-Y gastric bypass. Obesity (Silver Spring) 2015;23:746–9. 10.1002/oby.21037 [DOI] [PubMed] [Google Scholar]
- 12. Reddy V, Patel JK, Weerasinghe D, et al. Hyperammonemic encephalopathy: a complication of gastric bypass surgery. Cureus 2020;12:e9864. 10.7759/cureus.9864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Melnyk JL, Cavaliere KR, Roth NC. 2204 non-hepatic hyperammonemia associated with acute bowel perforation. Am J Gastroenterol 2019;114:S1235–6. 10.14309/01.ajg.0000598348.10384.ef [DOI] [Google Scholar]
- 14. Bertrand P, Faro A, Cantwell P, et al. Intravenous ribavirin and hyperammonemia in an immunocompromised patient infected with adenovirus. Pharmacotherapy 2000;20:1216–20. 10.1592/phco.20.15.1216.34582 [DOI] [PubMed] [Google Scholar]
- 15. Silvera-Ruiz SM, Gemperle C, Peano N, et al. Immune alterations in a patient with hyperornithinemia-hyperammonemia-Homocitrullinuria syndrome: a case report. Front Immunol 2022;13:861516. 10.3389/fimmu.2022.861516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Placone N, Kao RL, Kempert P, et al. Hyperammonemia from ureaplasma infection in an immunocompromised child. J Pediatr Hematol Oncol 2020;42:e114–6. 10.1097/MPH.0000000000001414 [DOI] [PubMed] [Google Scholar]
- 17. Smith M, Crews JD, Cheek N, et al. Hyperammonemic encephalopathy due to Ureaplasma Parvum infection in an immunocompromised child. Pediatrics 2019;144:e20190601. 10.1542/peds.2019-0601 [DOI] [PubMed] [Google Scholar]
- 18. Delafoy M, Goutines J, Fourmont A-M, et al. Case report: hyperammonemic encephalopathy linked to Ureaplasma Spp. and/or Mycoplasma Hominis systemic infection in patients treated for leukemia, an emergency not to be missed. Front Oncol 2022;12:912695. 10.3389/fonc.2022.912695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Summar ML, Barr F, Dawling S, et al. Unmasked adult-onset urea cycle disorders in the critical care setting. Crit Care Clin 2005;21:S1–8. 10.1016/j.ccc.2005.05.002 [DOI] [PubMed] [Google Scholar]
- 20. Otsuji K, Simizu S, Endo T, et al. A case of infectious enterocolitis with hyperammonemia. J UOEH 2017;39:271–6. 10.7888/juoeh.39.271 [DOI] [PubMed] [Google Scholar]
- 21. Levitt DG, Levitt MD. A model of blood-ammonia homeostasis based on a quantitative analysis of nitrogen metabolism in the multiple organs involved in the production, catabolism, and excretion of ammonia in humans. Clin Exp Gastroenterol 2018;11:193–215. 10.2147/CEG.S160921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Walker V. Severe hyperammonaemia in adults not explained by liver disease. Ann Clin Biochem 2012;49:214–28. 10.1258/acb.2011.011206 [DOI] [PubMed] [Google Scholar]
- 23. Gupta S, Fenves AZ, Hootkins R. The role of RRT in hyperammonemic patients. Clin J Am Soc Nephrol 2016;11:1872–8. 10.2215/CJN.01320216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lévesque R, Leblanc M, Cardinal J, et al. Haemodialysis for severe hyperammonaemic coma complicating urinary diversions. Nephrol Dial Transplant 1999;14:458–61. 10.1093/ndt/14.2.458 [DOI] [PubMed] [Google Scholar]
- 25. McBryde KD, Kershaw DB, Bunchman TE, et al. Renal replacement therapy in the treatment of confirmed or suspected inborn errors of metabolism. J Pediatr 2006;148:770–8. 10.1016/j.jpeds.2006.01.004 [DOI] [PubMed] [Google Scholar]
- 26. Slack AJ, Auzinger G, Willars C, et al. Ammonia clearance with haemofiltration in adults with liver disease. Liver Int 2014;34:42–8. 10.1111/liv.12221 [DOI] [PubMed] [Google Scholar]
- 27. Boer DP, Mourik SL, van den Hoogen MWF, et al. Successful treatment of severe hyperammonaemia with ultra-high dose continuous veno-venous haemodiafiltration. Blood Purif 2019;48:283–5. 10.1159/000499829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Spinale JM, Laskin BL, Sondheimer N, et al. High-dose continuous renal replacement therapy for neonatal hyperammonemia. Pediatr Nephrol 2013;28:983–6. 10.1007/s00467-013-2441-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bcr-2023-256225supp001.pdf (13.3MB, pdf)