Abstract
In the treatment of chronic myeloid leukemia (CML), resistance to BCR‐ABL inhibitors makes it difficult to continue treatment and is directly related to life expectancy. Therefore, asciminib was introduced to the market as a useful drug for overcoming drug resistance. While combining molecular targeted drugs is useful to avoid drug resistance, the new BCR‐ABL inhibitor asciminib and conventional BCR‐ABL inhibitors should be used as monotherapy in principle. Therefore, we investigated the synergistic effect and mechanism of the combination of asciminib and imatinib. We generated imatinib‐resistant cells using the human CML cell line K562, examined the effects of imatinib and asciminib exposure on cell survival using the WST‐8 assay, and comprehensively analyzed genetic variation related to drug resistance using RNA‐seq and real‐time PCR. A synergistic effect was observed when imatinib and asciminib were combined with or without imatinib resistance. Three genes, GRRP1, ESPN, and NOXA1, were extracted as the sites of action of asciminib. Asciminib in combination with BCR‐ABL inhibitors may improve the therapeutic efficacy of conventional BCR‐ABL inhibitors and prevent the development of resistance. Its dosage may be effective even at minimal doses that do not cause side effects. Further verification of this mechanism of action is needed. Additionally, cross‐resistance between BCR‐ABL inhibitors and asciminib may occur, which needs to be clarified through further validation as soon as possible.
Keywords: asciminib, BCR‐ABL inhibitors, chronic myelogenous leukemia, drug resistance
Abbreviations
- CML
chronic myeloid leukemia
- PI
propidium iodide
- S.E.
standard error
1. INTRODUCTION
Chronic myelogenous leukemia (CML) is a type of myeloproliferative disease that affects approximately 1 in 100 000 individuals. The Philadelphia chromosome, formed by the translocation of chromosomes 9 and 22 in hematopoietic stem cells, causes this disease. It produces the BCR‐ABL protein that acts as a tyrosine kinase, leading to an overgrowth of white blood cells. 1
CML prognosis considerably improved in therapeutic outcomes with the release of the BCR‐ABL inhibitor imatinib. Second‐generation BCR‐ABL inhibitors nilotinib and dasatinib were developed and led to an earlier complete molecular response and improved efficacy. 2 Currently, third‐ and fourth‐generation agents are available, and the 5‐year survival rate for CML is >90%, offering long‐term survival prospects. 3 , 4
Withdrawal of BCR‐ABL inhibitors after patients have achieved complete remission results in relapse in approximately 60% of patients. 5 Therefore, patients with CML require lifelong BCR‐ABL inhibitor treatment. 1 , 6 However, there are limited BCR‐ABL inhibitors, including imatinib, and when none show efficacy, patients may require transplantation. 7 Transplantation has a lower life expectancy than BCR‐ABL inhibitors, along with numerous long‐term side effects. Therefore, we are developing strategies to prolong the use of existing BCR‐ABL inhibitors.
The primary cause of the reduced efficacy of BCR‐ABL inhibitors is the development of resistance. Factors contributing to resistance include point mutations in BCR‐ABL and abnormal expression of other genes. 8 First, point mutations in BCR‐ABL alter the structure of the BCR‐ABL protein, preventing BCR‐ABL inhibitor binding to the BCR‐ABL protein. 9 More than 90 different gene sites with point mutations have been identified, with the T315I mutation being the most severe and drug‐resistant. 10 A point mutation replaces a single nucleotide, thereby changing the structure of the ATP‐binding pocket of BCR‐ABL1. This conformational change causes resistance to BCR‐ABL inhibitors because tyrosine kinase inhibitors are unable to bind to the ATP‐binding pocket. 11
Ponatinib, a BCR‐ABL inhibitor that also shows efficacy against T315I, has been developed to address point mutation resistance, including T315I mutations; however, its efficacy is limited as it, like imatinib, targets the ATP‐binding site. Therefore, drug resistance due to point mutations remains unaddressed. 12
Asciminib is a new and effective treatment for BCR‐ABL‐resistant CMLs. Asciminib has a different binding site for the BCR‐ABL protein compared to existing BCR‐ABL inhibitors. 13 Therefore, it is predicted to maintain its efficacy in CML with specific point mutations such as T315I. 13 , 14 However, detailed validation is lacking.
The efficacy of BCR‐ABL inhibitors is also reduced by aberrant expression of genes other than the Bcr‐Abl. 15 In particular, the aberrant expression of drug excretion transporters is believed to be a contributory factor in reducing intracellular drug concentration. 16
Combining molecular targeted agents with similar sites of action can produce synergistic effects and delay the development of drug resistance seen with single agents. 17 , 18 Similarly, a combination of asciminib and imatinib, which have different sites of action, may produce synergistic effects. In fact, the benefit of asciminib in combination with Bcr‐Abl inhibitors has begun to be tested and may be useful for CML with point mutations. 19 However, the detailed mechanism of resistance has not been determined and no effective therapy has been found for patients who do not have a genetic mutation yet are resistant to BCR‐ABL inhibitors. 15
Thus, we examined the synergistic effect of the combination of asciminib and imatinib in BCR‐ABL inhibitor‐resistant CML and examined the mechanism of the synergistic effect.
2. METHODS
2.1. Reagents
imatinib was obtained from Tokyo Chemical Industry Co., Ltd., Japan. Asciminib was obtained from Cayman Chemical Company, USA. imatinib and ascribed were dissolved in dimethyl sulfoxide.
2.2. Cell culture
K562 cells (a CML cell line) were obtained from RIKEN BioResource Research Center, Japan. Cells were cultured in RPMI 1640 (Nacalai Tesque, Japan) supplemented with 10% fetal bovine serum (Biowest, USA) and 10 mg/mL 1% (v/v) penicillin–streptomycin (Wako, Japan). All cells were cultured at 37°C in a humidified atmosphere containing 5% (v/v) CO2. To develop imatinib‐resistant cell lines, imatinib concentrations were cultured in stepwise increments of 50–500 nmol/L over 3 months.
2.3. Cell survival assay
Cell survival assays were performed using a Cell Counting Kit‐8 (DOJINDO, Japan) according to the manufacturer's protocol. Cells (5000 cells/well) were seeded in 96‐well microplates and treated with or without the drug for 72 h at 37°C under humidified 5% (v/v) CO2. Thereafter, Cell Counting Kit‐8 was added at 10 μL/well and incubated for 3 h. Absorbance was measured at 450 nm (reference wavelength: 630 nm) using a microplate reader Model 680 (Bio‐Rad Laboratories, USA). Cell viability was calculated using the ratio of the absorbance of treated cells to that of the control (100%) with the following formula: viability = (absorbance of treated well − absorbance of blank well)/(absorbance of untreated well − absorbance of blank well) × 100.
The following equation was used to calculate the IC50 of each drug:
A: high concentration across 50%; B: low concentration across 50%; C: cell viability at B; and D: cell viability at A.
2.4. Gene expression analysis
The cells were seeded at 5.0 × 104 cells/mL and divided into four groups (control, imatinib (125 nM), asciminib (3 nM), and imatinib (125 nM) + asciminib (3 nM) groups) and incubated in a 5% CO2 incubator at 37°C for 24 h. Thereafter, RNA was extracted using the RNeasy® Plus Mini Kit (QIAGEN, USA) according to the manufacturer's protocol and processed using the PrimeScript™ RT reagent Kit with gDNA Eraser (Perfect Real Time, Takara, Japan). A PCR Thermal Cycler Dice (Takara) was used for gDNA removal and reverse transcription. Thereafter, the StepOnePlus system (Applied Biosystems, Japan) was used to perform real‐time PCR on each reverse‐transcribed sample using the THUNDERBIRD SYBR qPCR Mix (Toyobo, Japan). Gene expression was quantified via relative expression analysis using the ΔΔCt method with hGAPDH as the internal standard.
2.5. Analysis of the cell cycle and apoptosis
K562 cells were seeded at a density of 5.0 × 104 cells/mL and incubated with various agents for 72 h. For cell cycle analysis, cells were collected, washed with PBS, and resuspended in 70% ice‐cold ethanol overnight at −20°C. After the cells were centrifuged, the ethanol was discarded, and the cells were resuspended in 50 μL PBS containing 0.1 mg/mL RNase (F. Hoffmann‐La Roche, Ltd., Basel, Switzerland) for 30 min at 37°C. After washing with PBS, the cell pellet was incubated in 100 μL propidium iodide (PI) solution (BioLegend, USA) for 10 min and gently resuspended in the dark at 4°C. Apoptosis was measured using an Annexin V‐FITC Apoptosis Detection Kit (Nacalai Tesque) according to the manufacturer's protocol. Measurements were performed using a Cell Sorter SH800S (Sony, Japan). Kaluza software (Beckman Coulter, USA) was used for the analysis.
2.6. RNA sequencing
RNA sequencing analysis was performed using RNA samples generated during gene expression analysis. BCR‐ABL point mutation analysis was performed by Eurofins, Japan, and RNA‐seq analysis was performed by Macrogen, Japan.
2.7. Statistical analysis
Data were expressed as the mean ± S.E. (standard error) for each value. The sample size “n” indicates the number of independent experiments performed on independent plates. Statistical analysis was performed using one‐way ANOVA or Tukey's multiple comparisons among the three groups using IBM SPSS Statistics 29 software. Statistical differences between the two groups were evaluated using Student’s t‐test.
2.8. Nomenclature of targets and ligands
Key protein targets and ligands in this article are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY, 20 and are permanently archived in the Concise Guide to PHARMACOLOGY 2019/20. 21
3. RESULTS
3.1. Asciminib shows synergistic effects when combined with imatinib
Changes in the proliferation of K562 cells exposed to different doses of imatinib or asciminib were evaluated using the WST‐8 assay. K562 cell proliferation was inhibited by imatinib and asciminib in a dose‐dependent manner, with IC50 values of 121 nM and 4.9 nM, respectively (Figure 1A). Simultaneous exposure to imatinib and asciminib resulted in greater inhibition of cell proliferation than a single exposure (Figure 1B). Furthermore, annexin V and PI were used to determine the status of cell death. Apoptosis was detected when imatinib and asciminib were used in combination and when they were used individually (Figure 1C). Similarly, in the cell cycle, imatinib and asciminib exposure increased the percentage of cells in the sub‐G1 phase, and the combination of the two drugs further increased this percentage in the sub‐G1 phase (Figure 1D).
FIGURE 1.
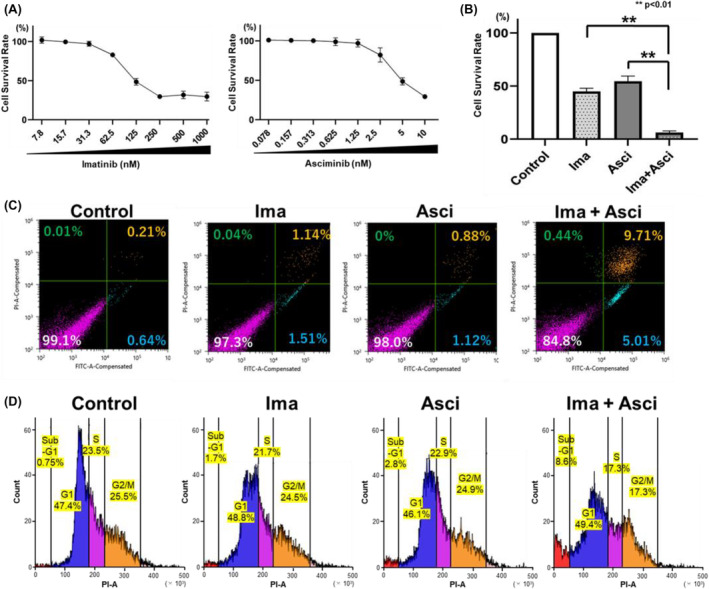
The effect of imatinib or asciminib on cell survival and promotion of angiogenesis. K562 cells, a BCR‐ABL‐positive CML cell line, were used to investigate drug sensitivity. Cells (1 × 105 cells/well) were plated in 96‐well plates with (A) imatinib (7.8–1000 nM), asciminib (0.078–10 nM), (B) imatinib (125 nM), and asciminib (3 nM). After 72 h of incubation, cell viability was determined using the WST‐8 assay. Error bars represent the mean ± SE (n = 3). (C) asciminib enhanced imatinib‐induced apoptosis in BCR‐ABL‐positive CML cells. Cells were cultured with imatinib (125 nM) and asciminib (3 nM) for 24 h and subsequently examined for apoptosis using annexin V and PI staining. (D) asciminib enhanced imatinib‐induced cell cycle arrest in BCR‐ABL‐positive CML cells. Cells were cultured with imatinib (125 nM) and asciminib (3 nM) for 24 h and subsequently examined for cell cycle using PI staining.
3.2. Asciminib shows synergistic effects when combined with imatinib, even among imatinib‐resistant lines
The established imatinib‐resistant K562 cells (K562‐IR1, K562‐IR2, and K562‐IR3) were used for validation. Cells were exposed to different doses of imatinib or asciminib for 72 h, and the inhibition of cell proliferation was evaluated using the WST‐8 assay. Cell proliferation was inhibited in a concentration‐dependent manner by both imatinib and asciminib; the IC50 values for imatinib in imatinib‐resistant K562‐IR1, K562‐IR2, and K562‐IR3 cells were 569, 1386, and 472 nM, respectively (Figure 2A). The IC50 for asciminib in all imatinib‐resistant K562 cells (K562‐IR1, K562‐IR2, and K562‐IR3) was higher than that of the non‐resistant cells, with values of 14.3 nM, 26.1 nM, and 13.2 nM, respectively (Figure 2B). Moreover, concomitant exposure to imatinib and asciminib inhibited cell proliferation to a greater extent than single‐agent exposure (Figure 2C).
FIGURE 2.
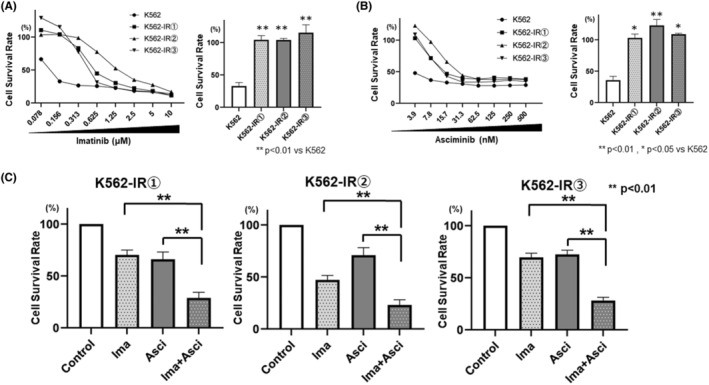
The effect of imatinib or asciminib on cell survival and promotion of angiogenesis in imatinib‐resistant cell lines. K562 and three K562‐IR cell types (density: 1 × 105 cells/well) were plated in 96‐well plates with (A) imatinib or (B) asciminib or (C) imatinib and asciminib, at their respective IC50 values. Treatment concentrations were imatinib 600 nM and asciminib 15 nM for (1), imatinib 1400 nM and asciminib 25 nM for (2), and imatinib 500 nM and asciminib 15 nM for (3). After 72 h of incubation, cell viability was determined using the WST‐8 assay. Error bars represent the mean ± SE (n = 3).
3.3. Confirmation of resistance mechanism of resistant cell lines
The status of point mutations in the established imatinib‐resistant K562 cells was confirmed by RNA sequencing analysis. Two point mutations were detected in K562‐IR1 and one in K562‐IR2; however, none were detected in K562‐IR3 (Figure 3A). Therefore, we focused on K562IR‐3 to identify resistance mechanisms other than point mutations. Using real‐time PCR, we confirmed that the expression of the drug excretion transporters ABCG2 and ABCB1 was upregulated in resistant cells compared to that in non‐resistant cells (Figure 3B). Next, we used febuxostat and verapamil, inhibitors of ABCG2 and ABCB1, respectively, to confirm the effects of ABCG2 and ABCB1 inhibition on the survival of K562‐IR3 cells.
FIGURE 3.
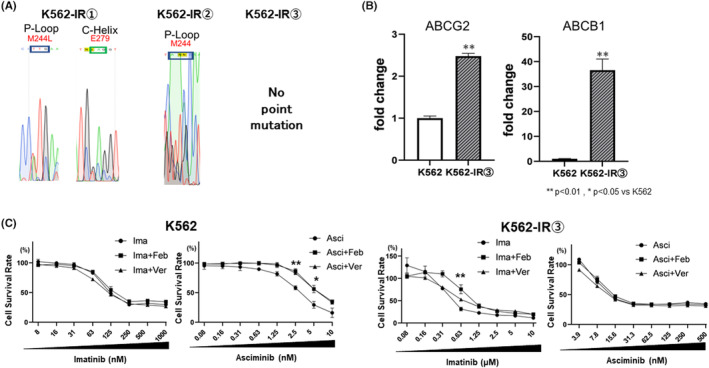
Contribution of point mutations and drug excretion transporters in the imatinib‐resistant K562 cell line. (A) RNA‐seq was performed on K562 cells for the presence of point mutations in the binding sites of Bcr‐Abl inhibitors. Point mutations were found in K562‐IR1 and K562‐IR2; however, no point mutations were found in K562‐IR3. (B) Expression of drug excretion transporter in K562‐IR3 cells (primers are noted in Supply). (C) Validation was conducted in both K562 and K562‐IR3 cells to assess changes in cell viability when exposed to imatinib and asciminib in the presence of drugs inhibiting ABCG2 or ABCB1 were measured. Cell viability was measured after 72 h of drug exposure and 72 h of culture using the WST‐8 assay. Error bars represent the mean ± SE (n = 3).
Exposure to either febuxostat or verapamil in the presence of imatinib or asciminib did not enhance cell growth inhibition compared to that in the imatinib‐alone group (Figure 3C).
3.4. Comprehensive analysis via RNA‐seq
RNA‐seq analysis was performed on K562 cells treated with imatinib, asciminib, and their two‐drug combination. Genes encoding these proteins have been explored for their association with cancer. We analyzed 15 349 genes. Three genes were selected: GRRP1, upregulated by both imatinib and asciminib, and ESPN and NOXA1, upregulated by both imatinib and asciminib (Figure 4).
FIGURE 4.
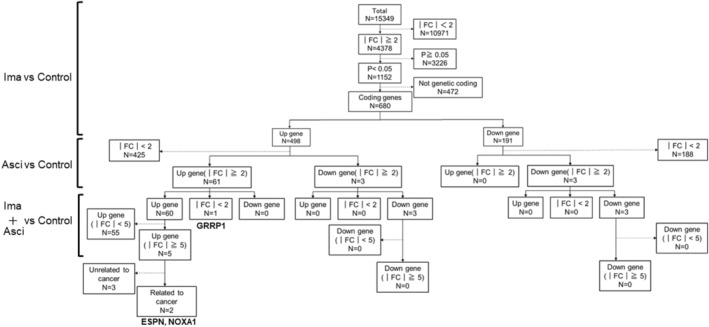
Comprehensive analysis of genes associated with imatinib and/or asciminib. RNA‐seq analysis was performed on K562 cells treated with imatinib (125 nM) and asciminib (3 nM) for 24 h and extracted RNA samples. A total of 15 349 genes were included in the analysis. Of these, 1152 genes had a significant twofold or greater change in gene expression due to imatinib exposure. n = the number of genes included. Among them, 680 gene‐encoding proteins were validated. Then, genes whose expression was upregulated more than twofold in both imatinib and asciminib groups compared to the untreated group were included in the analysis, and 61 genes were applicable. Furthermore, with regard to the variation when imatinib was combined with asciminib, 2 genes whose expression was upregulated were reported to be associated with cancer, and 3 genes whose expression was not yet reported. Thresholds are indicated by FC and the amount of variation compared to the drug untreated group. For the amount of variation, p < .05 is indicated as a significant variation.
3.5. Comprehensive analysis via RNA‐seq
For the three genes extracted by RNA‐seq, the variation in expression levels in drug‐resistant strains was verified by real‐time PCR using K562 and K562‐IR3. For GRRP1, expression was found to be decreased in resistant cells compared to non‐resistant cells. On the other hand, no significant variation in expression was observed for ESPN and NOXA1 (Figure 5A). Therefore, we exposed K562 to imatinib and asciminib and confirmed the variation of GRRP1 gene expression; the expression level tended to increase after exposure to imatinib and asciminib, and further increase was observed when both drugs were combined (Figure 5B).
FIGURE 5.
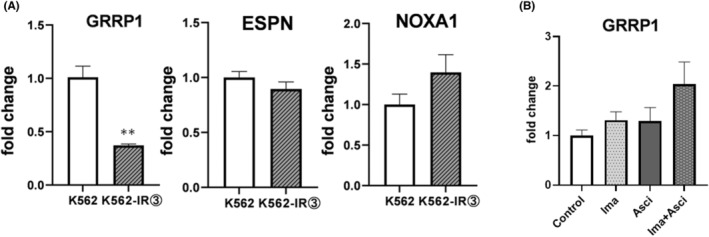
Expression levels for a group of genes that may be related to drug resistance. (A) Gene expression of GRRP1 in K562 and K562‐IR3 cells was tested for differences in gene expression of GRRP1 in cells that developed drug resistance. Error bars represent mean ± SE (n = 3). (B) Gene expression of GRRP1 was analyzed using RNA samples extracted after culturing cells in imatinib (125 nM) and asciminib (3 nM) for 24 h in K562. Error bars represent mean ± SE (n = 3).
4. DISCUSSION
BCR‐ABL inhibitors have significantly altered CML treatment. 2 , 3 , 4 However, owing to drug resistance to BCR‐ABL inhibitors and other factors, some patients exhaust these options and require hematopoietic stem cell transplantation. 4 Therefore, it is important to elucidate the mechanism of resistance to BCR‐ABL inhibitors.
In this study, although both imatinib and asciminib inhibited BCR‐ABL, no competitive antagonism was observed when both drugs were used together. Instead, synergistic effects were observed. The combination increased apoptotic cells in annexin V and PI analysis. In addition, cell cycle analysis using flow cytometry showed an increase in the percentage of cells in the sub‐G1 phase, indicating an increase in apoptotic cells. 22 , 23 These results supported the possibility that the combination of imatinib and asciminib does not induce substantial toxicity. The reason for the synergistic effect may be because the mechanism of BCR‐ABL inhibition by asciminib is different from that of existing BCR‐ABL inhibitors. 13 , 14 Additionally, the combination of two molecular targeted agents with a close point of action decreases the risk of developing resistance to these agents. 17 , 18 Although the current approval for asciminib and imatinib is limited to single‐agent use, their combination may reduce the risk of drug resistance compared with the single‐agent use of each agent. The optimal dose of asciminib when combined with the two drugs needs further validation. The risk of side effects may be low if the dosage of asciminib is small when compared with the currently indicated dosage.
Resistance to BCR‐ABL inhibitors is another major challenge in CML treatment. Factors contributing to resistance to BCR‐ABL inhibitors include point mutations in BCR‐Abl and abnormal expression of all other genes. 8 asciminib, with a distinct mechanism of action from conventional BCR‐ABL inhibitors, is not expected to induce resistance, even in the case of point mutations. 14 Therefore, asciminib has been used in clinical practice for patients with CML who show resistance to BCR‐ABL inhibitors. 24 Thus, we established multiple imatinib‐resistant K562 cell lines and tested their sensitivity to asciminib.
First, we examined sensitivity to asciminib alone, observing decreased sensitivity in all imatinib‐resistant cells to asciminib compared to non‐resistant strains. Although the combination with asciminib did not restore sensitivity to imatinib, the synergistic effect of the combination was confirmed. These results suggested that greater efficacy may have been achieved if asciminib alone or in combination with a BCR‐ABL inhibitor had been used in the same patient at the initial onset of CML, before BCR‐ABL inhibitor resistance development. Based on these results, further validation is essential, including clinical practice verification of cross‐resistance, comparing asciminib resistance in samples taken at the time of initial CML onset with that in samples taken at the time of resistance to BCR‐ABL inhibitors.
Point mutations may not be involved in the development of drug resistance. Therefore, we further investigated K562‐IR3, an established resistant strain lacking a point mutation. Activation of the drug excretion transporters ABCB1 and ABCG2 is a typical cause of drug resistance to BCR‐ABL inhibitors. 25 , 26 We observed that the expression of these genes was upregulated in K562‐IR3. However, exposing K562‐IR3 cells to the inhibitors of ABCB1, verapamil, 27 and the inhibitor of ABCG2, febuxostat, 28 did not restore sensitivity to imatinib or asciminib. Therefore, it is unlikely that ABCB1 or ABCG2 contributes to asciminib or imatinib resistance in K562‐IR3 cells. In cells that develop resistance to a molecularly targeted drug, the use of the drug may reverse target activation. 29 In this study, using ABCG2 or ABCB1 inhibitors increased cell viability compared to the untreated group. This may be due to the activation of the signaling pathway resulting from increased intracellular concentrations of imatinib and asciminib. Since these observations were verified in basic research, further investigation using clinical samples is planned to determine whether they also occur in clinical patients.
Next, RNA‐seq analysis was performed to investigate the mechanism of the synergistic effect of imatinib and asciminib, considering asciminib is a new drug and the majority of its secondary effects are unknown. This may contribute to understanding the mechanism by which CML cells acquire drug resistance to imatinib. Therefore, we performed a comprehensive search for protein‐coding genes using RNA‐seq. Three genes, GRRP1, ESPN, and NOXA1, were identified as active sites. These genes are associated with cancer growth. 30 , 31 , 32 , 33 However, there are no related reports on asciminib, imatinib, or CML, which may be novel sites of action that show synergistic effects.
Therefore, we examined the expression levels of GRRP1 in drug‐resistant cells and found that GRRP1 expression was significantly downregulated in resistant cells compared to non‐resistant cells, while no significant changes in expression were observed for ESPN and NOXA1. Thus, we exposed imatinib and asciminib to K562 and confirmed the changes in GRRP1 gene expression. The expression levels tended to increase after exposure to imatinib and asciminib, and a further increase was observed when both drugs were used in combination. These results suggest that GRRP1 may be involved in the synergistic effects of imatinib and asciminib and in drug resistance.
In this study, the use of asciminib in combination with Bcr‐Abl inhibitors improved the therapeutic efficacy of conventional BCR‐ABL inhibitors and prevented the development of resistance. It may be effective even at minute doses without causing any side effects. In addition, cross‐resistance may occur between BCR‐ABL inhibitors and asciminib, and it may be important to use asciminib from the initial stage of the disease before the development of resistance. However, whether cross‐resistance to BCR‐ABL inhibitors occurs when resistance develops to asciminib remains unclear, necessitating further validation. We found GRRP1 as a new point of action involved in these drug resistance and synergistic effects. GRRP1 is involved in the induction of cell differentiation, 31 and decreased GRRP1 expression may have increased the number of undifferentiated cells, resulting in decreased drug sensitivity. Although further validation of the detailed mechanism of action of GRRP1 is needed, GRRP1 may be a valuable point of action in the treatment of CML.
AUTHOR CONTRIBUTIONS
KY, FA, and KI wrote the manuscript; KY, SI, and SS designed the research; KY, SI, MT, FA, TN, KM, and YI performed the research; and KY, SI, MT, MG, KK, NO, and KI analyzed the data.
FUNDING INFORMATION
This study was supported by a Grant‐in‐Aid (KAKENHI) from the Japan Society for the Promotion of Science (JSPS) (grant numbers: 20 K16044 and 22 K15340). The funding source had no role in the study design; collection, analysis, and interpretation of data; writing of the report; or decision to submit the article for publication.
DECLARATIONS OF INTEREST
None.
Supporting information
Table S1: xxx
ACKNOWLEDGMENTS
The authors would like to thank Editage (www.editage.com) for the English language editing.
Okamoto N, Yagi K, Imawaka S, et al. Asciminib, a novel allosteric inhibitor of BCR‐ABL1, shows synergistic effects when used in combination with imatinib with or without drug resistance. Pharmacol Res Perspect. 2024;12:e1214. doi: 10.1002/prp2.1214
Naoki Okamoto and Kenta Yagia contributed equally to this work.
DATA AVAILABILITY STATEMENT
Data pertaining to this article will be available by the corresponding author upon reasonable request.
REFERENCES
- 1. Soverini S, Mancini M, Bavaro L, Cavo M, Martinelli G. Chronic myeloid leukemia: the paradigm of targeting oncogenic tyrosine kinase signaling and counteracting resistance for successful cancer therapy. Mol Cancer. 2018;17(1):1‐5. doi: 10.1186/s12943-018-0780-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wei G, Rafiyath S, Liu D. First‐line treatment for chronic myeloid leukemia: dasatinib, nilotinib, or imatinib. J Hematol Oncol. 2010;3:1‐10. doi: 10.1186/1756-8722-3-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ohnishi K, Nakaseko C, Takeuchi J, et al. Long‐term outcome following imatinib therapy for chronic myelogenous leukemia, with assessment of dosage and blood levels: the JALSG CML202 study. Cancer Sci. 2012;103(6):1071‐1078. doi: 10.1111/j.1349-7006.2012.02253.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hochhaus A, Larson RA, Guilhot F, et al. IRIS investigators. Long‐term outcomes of imatinib treatment for chronic myeloid leukemia. N Engl J Med. 2017;376(10):917‐927. doi: 10.1056/NEJMoa1609324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mahon FX, Réa D, Guilhot J, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre stop imatinib (STIM) trial. Lancet Oncol. 2010;11(11):1029‐1035. doi: 10.1016/S1470-2045(10)70233-3 [DOI] [PubMed] [Google Scholar]
- 6. Experts in Chronic Myeloid Leukemia . The price of drugs for chronic myeloid leukemia (CML) is a reflection of the unsustainable prices of cancer drugs: from the perspective of a large group of CML experts. Blood. 2013;121(22):4439‐4442. doi: 10.1182/blood-2013-03-490003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hochhaus A, Baccarani M, Silver RT, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34(4):966‐984. doi: 10.1038/s41375-020-0776-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Loscocco F, Visani G, Galimberti S, Curti A, Isidori A. BCR‐ABL independent mechanisms of resistance in chronic myeloid leukemia. Front Oncol. 2019;9:939. doi: 10.3389/fonc.2019.00939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shah NP, Nicoll JM, Nagar B, et al. Multiple BCR‐ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell. 2002;2(2):117‐125. doi: 10.1016/s1535-6108(02)00096-x [DOI] [PubMed] [Google Scholar]
- 10. Laganà A, Scalzulli E, Carmosino I, Martelli M, Breccia M. Asciminib as a third line option in chronic myeloid leukemia. Int J Hematol. 2023;117(1):16‐23. doi: 10.1007/s12185-022-03432-7 [DOI] [PubMed] [Google Scholar]
- 11. Tamai M, Inukai T, Kojika S, et al. T315I mutation of BCR‐ABL1 into human Philadelphia chromosome‐positive leukemia cell lines by homologous recombination using the CRISPR/Cas9 system. Sci Rep. 2018;8(1):9966. doi: 10.1038/s41598-018-27767-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kinstrie R, Copland M. Targeting chronic myeloid leukemia stem cells. Curr Hematol Malig Rep. 2013;8(1):14‐21. doi: 10.1007/s11899-012-0148-8 [DOI] [PubMed] [Google Scholar]
- 13. Hughes TP, Mauro MJ, Cortes JE, et al. Asciminib in chronic myeloid leukemia after ABL kinase inhibitor failure. N Engl J Med. 2019;381(24):2315‐2326. doi: 10.1056/NEJMoa1902328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Manley PW, Barys L, Cowan‐Jacob SW. The specificity of asciminib, a potential treatment for chronic myeloid leukemia, as a myristate‐pocket binding ABL inhibitor and analysis of its interactions with mutant forms of BCR‐ABL1 kinase. Leuk Res. 2020;98:106458. doi: 10.1016/j.leukres.2020.106458 [DOI] [PubMed] [Google Scholar]
- 15. Sinclair A, Latif AL, Holyoake TL. Targeting survival pathways in chronic myeloid leukaemia stem cells. Br J Pharmacol. 2013;169(8):1693‐1707. doi: 10.1111/bph.12183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dohse M, Scharenberg C, Shukla S, et al. Comparison of ATP‐binding cassette transporter interactions with the tyrosine kinase inhibitors imatinib, nilotinib, and dasatinib. Drug Metab Dispos. 2010;38(8):1371‐1380. doi: 10.1124/dmd.109.031302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Flaherty KT, Infante JR, Daud A, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. N Engl J Med. 2012;367(18):1694‐1703. doi: 10.1056/NEJMoa1210093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Greger JG, Eastman SD, Zhang V, et al. Combinations of BRAF, MEK, and PI3K/mTOR inhibitors overcome acquired resistance to the BRAF inhibitor GSK2118436 dabrafenib, mediated by NRAS or MEK mutations. Mol Cancer Ther. 2012;11(4):909‐920. doi: 10.1158/1535-7163.MCT-11-0989 [DOI] [PubMed] [Google Scholar]
- 19. Wylie A, Schoepfer J, Jahnke W, et al. The allosteric inhibitor ABL001 enables dual targeting of BCR–ABL1. Nature. 2017;543:733‐737. doi: 10.1038/nature21702 [DOI] [PubMed] [Google Scholar]
- 20. Harding SD, Sharman JL, Faccenda E, et al. The IUPHAR/BPS guide to PHARMACOLOGY in 2018: updates and expansion to encompass the new guide to IMMUNOPHARMACOLOGY. Nucleic Acids Res. 2018;46(D1):D1091‐D1106. doi: 10.1093/nar/gkx1121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Alexander SPH, Christopoulos A, Davenport AP, et al. The concise guide to pharmacology 2019/20: G protein‐coupled receptors. Br J Pharmacol. 2019;176(Suppl 1):S21‐S141. doi: 10.1111/bph.14748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Biswas R, Mondal A, Chatterjee S, Ahn JC. Evaluation of synergistic effects of sulforaphene with photodynamic therapy in human cervical cancer cell line. Lasers Med Sci. 2016;31(8):1675‐1682. doi: 10.1007/s10103-016-2037-1 [DOI] [PubMed] [Google Scholar]
- 23. Stevens JJ, Graham B, Dugo E, Berhaneselassie‐Sumner B, Ndebele K, Tchounwou PB. Arsenic trioxide induces apoptosis via specific signaling pathways in HT‐29 colon cancer cells. J Cancer Sci Ther. 2017;9(1):298‐306. [PMC free article] [PubMed] [Google Scholar]
- 24. Réa D, Mauro MJ, Boquimpani C, et al. A phase 3, open‐label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs. Blood. 2021;138(21):2031‐2041. doi: 10.1182/blood.2020009984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eadie LN, Hughes TP, White DL. Interaction of the efflux transporters ABCB1 and ABCG2 with imatinib, nilotinib, and dasatinib. Clin Pharmacol Ther. 2014;95(3):294‐306. doi: 10.1038/clpt.2013.208 [DOI] [PubMed] [Google Scholar]
- 26. Hegedus C, Ozvegy‐Laczka C, Apáti A, et al. Interaction of nilotinib, dasatinib and bosutinib with ABCB1 and ABCG2: implications for altered anti‐cancer effects and pharmacological properties. Br J Pharmacol. 2009;158(4):1153‐1164. doi: 10.1111/j.1476-5381.2009.00383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sabnis DH, Storer LCD, Liu JF, et al. A role for ABCB1 in prognosis, invasion and drug resistance in ependymoma. Sci Rep. 2019;9(1):10290. doi: 10.1038/s41598-019-46700-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Toyoda Y, Takada T, Suzuki H. Inhibitors of human ABCG2: from technical background to recent updates with clinical implications. Front Pharmacol. 2019;10:208. doi: 10.3389/fphar.2019.00208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Higuchi M, Ishiyama K, Maruoka M, Kanamori R, Takaori‐Kondo A, Watanabe N. Paradoxical activation of c‐Src as a drug‐resistant mechanism. Cell Rep. 2021;34(12):108876. doi: 10.1016/j.celrep.2021.108876 [DOI] [PubMed] [Google Scholar]
- 30. Yang H, Gou X, Feng C, et al. Computed tomography‐detected extramural venous invasion‐related gene signature: a potential negative biomarker of immune checkpoint inhibitor treatment in patients with gastric cancer. J Transl Med. 2023;21(1):1‐7. doi: 10.1186/s12967-022-03845-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cunningham TJ, Yu MS, McKeithan WL, et al. Id genes are essential for early heart formation. Genes Dev. 2017;31(13):1325‐1338. doi: 10.1101/gad.300400.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li SH, Lu HI, Huang WT, et al. An Actin‐binding protein ESPN is an independent prognosticator and regulates cell growth for esophageal squamous cell carcinoma. Cancer Cell Int. 2018;18:219. doi: 10.1186/s12935-018-0713-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Honjo T, Otsui K, Shiraki R, et al. Essential role of NOXA1 in generation of reactive oxygen species induced by oxidized low‐density lipoprotein in human vascular endothelial cells. Endothelium. 2008;15(3):137‐141. doi: 10.1080/10623320802125433 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: xxx
Data Availability Statement
Data pertaining to this article will be available by the corresponding author upon reasonable request.


