Abstract
The linear, single-stranded enterovirus RNA genome is flanked at either end with a nontranslated region (NTR). By replacing the entire 5′ NTR of coxsackievirus B3 (CVB3) with that from type 1 poliovirus, a progeny virus was obtained following transfection of HeLa cells. The chimeric virus, CPV/49, replicates like the parental CVB3 strain in HeLa cells but is attenuated for replication and yield in primary human coronary artery endothelial cell cultures, in a human pancreas tumor cell line, and in primary murine heart fibroblast cultures. Western blotting analyses of CPV/49 replication in murine heart fibroblast cultures demonstrate that synthesis of CPV/49 proteins is significantly slower than that of the parental CVB3 strain. CPV/49 replicates in murine hearts and pancreata, causing no disease in hearts and a minor pancreatic inflammation in some mice that resolves by 28 days postinoculation. A single inoculation with CPV/49 induces protective anti-CVB3 neutralizing antibody titers that completely protect mice from both heart and pancreatic disease when mice are challenged 28 days p.i. with genetically diverse virulent strains of CVB3. That a chimeric CVB3 strain, created from sequences of two virulent viruses, is sufficiently attenuated to act as an avirulent, protective vaccine strain in mice suggests that chimeric genome technology merits further evaluation for the development of new nonpoliovirus enteroviral vectors.
The six serotypes of the group B coxsackieviruses (CVB1 to CVB6) are enteroviruses in the picornavirus family (17). The enterovirus genus also includes the group A coxsackieviruses, polioviruses (PVs), echoviruses, and several other numbered serotypes. Very similar to PV, the prototype enterovirus, in nucleotide sequence and identical in gene order, the CVB genome is 7,400 nucleotides (nt) in length. The single open reading frame encodes 11 proteins and is flanked by nontranslated regions (NTR). The 5′-terminal nucleotide is linked to a virus-encoded protein, and the 3′ terminus is completed with a polyadenosine tail. The CVB are etiologically linked to a wide range of human diseases ranging from mild, common cold-like symptoms through serious and life-threatening illnesses such as meningitis and inflammatory heart disease (reviewed in reference 38).
The enteroviral 5′ NTR, at about 740 nt in length, represents 10% of the viral genome. The 5′ NTR nucleotide sequence is well maintained among certain enterovirus groups; within the CVB, for example, primary structure is 73% conserved overall, with sequences of individual strains within serotypes much more highly conserved (44). Somewhat greater nucleotide nonidentity can occur between genomes of groups, such as between PV and CVB (26, 42). Notwithstanding an overall 30% nonidentity at the primary structure level, the 5′ NTR of CVB3 was shown to be able to functionally replace that of poliovirus type 1 (PV1) (29, 47), a finding that was confirmed later by others (57). Replacement of a PV 5′ NTR with that from a human rhinovirus also produced infectious virus (24). The construction of 5′ NTR chimeric genomes that produce functional progeny viruses has demonstrated that the 5′ NTR sequences are very similar in overall higher-order structure regardless of the extent of sequence divergence among the enteroviruses. It is not surprising, therefore, that analyses of 5′ NTR sequences in terms of potential higher-order structures demonstrate a significant structural conservation (1, 12, 34, 40, 49), providing a convincing explanation for why the 5′ NTR sequence of one enterovirus can readily substitute in function for that of the parental virus, albeit with some loss of replication efficiency. An even more exotic artificially engineered enterovirus-based chimera has been engineered: Lu and Wimmer demonstrated that the internal ribosome entry site (IRES) from hepatitis C virus (an unrelated positive-strand RNA virus) is functional within a PV genome when substituted for the PV IRES (36).
Here we report the results from studies using a chimeric CVB3 strain that was constructed by replacing the entire 5′ NTR of a cardiovirulent CVB3 strain with that from a neurovirulent PV strain. The progeny virus replicated less efficiently than the CVB3 parental strain in both human and murine cell cultures, did not induce disease in young mice, and induced in inoculated mice protective immunity against inflammatory heart and pancreatic disease induced by virulent CVB3 challenge.
MATERIALS AND METHODS
Cells and viruses.
HeLa, COS-1, Panc-1 (human pancreatic ductal tumor cells; American Type Culture Collection, Manassas, Va.), and murine fetal heart fibroblast (MFHF [55]) primary cultures were maintained in minimal essential medium (MEM)–10% fetal bovine serum–50 μg of gentamicin per ml at 37°C in a humidified 5% CO2-in-air atmosphere. Primary human cardiac artery endothelial cells (HCAEC) were obtained from Clonetics, Inc. (Walkersville, Md.) and were propagated at 37°C in the proprietary medium EGM-2 as directed by the supplier. All HCAEC cultures were between passages 4 and 7.
CVB3/20, a well-characterized cardiovirulent strain of CVB3 that has been cloned as an infectious cDNA and fully sequenced (pCVB3-20; GenBank accession no. M88483 [51, 52]), was propagated from transfection of plasmid pCVB3-20 in HeLa cells. Stocks of virus were prepared and titered in HeLa cells from transfected cultures. Titers of virus are expressed as 50% tissue culture infective dose (TCID50) per milliliter. The infectious cDNA clone of PV1 Mahoney (PV1/M) (pPV20 [48]) provided the PV 5′ NTR for the construction of the chimeric CVB3 cDNA genome. The virulent strains CVB3/AS (53) and CVB3/M (35) were propagated from preexisting virus stocks and titered on HeLa cell monolayers.
Construction and transfection of pCPV-49.
Construction of the infectious cDNA clone pCPV-49 is outlined in Fig. 1. To generate the chimeric genome, the PV 5′ NTR was excised from plasmid pPV20 as an EcoRI-HgiAI fragment (containing PV1 nt 1 to 751). This fragment and a SacI-BglII fragment (containing CVB3 nt 752 to 2043) and a BglII-ClaI fragment [containing CVB3 nt 2044 to 7399 and a poly(A) tract] of pCVB3-20 were ligated into the EcoRI and ClaI sites of pES131 (31). In the recombinant plasmid, the single base mismatch of the PV1 HgiAI site and the CVB3 SacI site was resolved as a SacI site (GTGCT/C_GAGCT/C) with no change of the encoded VP4 protein sequence.
FIG. 1.
Construction of pCPV-49. The restriction fragment (nt 1 to 751) of the PV1/M cDNA genome (48) and restriction fragments (nt 752 to 2043; nt 2043 to 7460) of the CVB3/20 genome (52) were ligated in the pES131 vector (48), using the EcoRI (R), HgiAI (H), SacI (S), BglII (B), and ClaI (C) sites to produce a chimeric genome. PV1/M is indicated by the solid bar; CVB3 is indicated by the empty bar. Drawing is not to scale.
Sequence analysis (ThermoSequenase; Amersham Life Sciences, Cleveland Ohio) of the resultant cDNA clone, pCPV-49, verified that the expected PV1/M sequence was intact (data not shown). To generate progeny virus, 10 μg of plasmid pCVB3-49 was electroporated into 106 COS-1 cells in Opti-MEM medium (Life Technologies, Gaithersburg, Md.) with a Cell-Porator (Life Technologies) set to 500 V/cm with a pulse of 15.5 ms and then plated in MEM. After 3 days, the cultures were freeze-thawed and cleared of cellular debris by centrifugation, and one-half of the cleared supernatant was passed onto a nearly confluent HeLa cell monolayer in a 100-mm-diameter dish. Progeny virus, CPV/49 (passage 2), was harvested and titered by TCID50 assay on HeLa cells prior to freezing at 74°C. To assay the sequence of the progeny virus CPV/49 in the 5′ NTR, viral RNA was extracted from this stock (TRlzol; Life Technologies), and sequence analysis was carried out using reverse transcriptase-mediated PCR. Briefly, cDNA was synthesized in a 20-μl reaction volume containing RNA from 0.25 ml of virus, random hexameric primers (0.125 OD260 [optical density at 260 nm] units/ml), and Moloney murine leukemia virus reverse transcriptase (Superscript; Life Technologies) as directed by the supplier. After reverse transcription, 5 μl of the 20-μl reaction mixture was used as the template in a PCR of both the PV1 5′ NTR and CVB3 sequences.
The PCR and sequencing primers used were as follows (nucleotide numbering is based on those of PV1 [GenBank accession no. V01149] and CVB3 [GenBank accession no. M88483] as noted): PV5, 5′-GTTAAAACAGCTCTGGGGTTGTACCCACCCCAGAG (PV nt 1 to 34); JRp64, 5′-ACGGTACCTTTGTGCGCCTGTTTT (PV nt 64 to 88; 45); E7, 5′-GGGTAACAGAAGTGCTTG (PV reverse complement, nt 163 to 179); E2, 5′-TCCGGCCCCTGAATG (PV nt 436 to 460); E3, 5′-ACACGGACACCCAAAGTAGTCGGTTCC (PV reverse complement, nt 533 to 559); and DREV, 5′-GCGTTGATACTTGAGCTCCC (CVB3 reverse complement, nt 745 to 764). Amplifications were performed in a Robocycler (Stratagene, La Jolla, Calif.) for 40 cycles. Annealing temperatures varied according to the primer pair used. DNA amplimers were visualized on 2% agarose gels in 1× Tris-borate-EDTA, isolated from gel slices using GenElute agarose spin columns (Supelco, Bellefonte, Pa.), and then cycle sequenced (ThermoSequenase; Amersham Life Sciences) according to the manufacturer's protocol, using an appropriate primer. Sequences were analyzed with the Wisconsin Package of software (Genetics Computer Group, Madison, Wis.).
Single-step virus growth curves.
Single-step virus growth curves in HeLa, MFHF, HCAEC, and Panc-1 monolayer cell cultures were performed at 37°C as described elsewhere (55). Briefly, 2 × 104 cells were plated per well in 24-well plates; the following day, cells were inoculated with either CPV/49 or CVB3/20 at a multiplicity of infection (MOI) of 20 infectious virus units per cell, washed, and refed. Plates were frozen at intervals and thawed, and the virus titers in the centrifugally cleared media were determined on HeLa cells as described above.
Western blot analysis of viral translation.
MFHF and HeLa cells were plated and inoculated with virus as described above. At 4, 7, 10, and 18 (MFHF) or 3.5, 4.5, and 6 (HeLa) h postinoculation (p.i.), the medium was removed and the cells were harvested into 2× Laemmli buffer (32) containing 2-mercaptoethanol. Electrophoresis of proteins was performed with sodium dodecyl sulfate in 14% polyacrylamide gels (Novex; San Diego, Calif.). Viral proteins were electroblotted for 40 min at 16 V onto Immobilon-P (Millipore Corp., Bedford, Mass.) membranes and then blocked for 1 h at room temperature in 5% (wt/vol) dried milk–1% (vol/vol) normal rabbit serum (Boehringer Mannheim Corp., Indianapolis, Ind.) in phosphate-buffered saline containing 0.01% Tween 80 (PBS-Tween). A 1:25 dilution of the primary antibody, horse polyclonal anti-CVB3 neutralizing antiserum (American Type Culture Collection), and a 1:1,000 dilution of the secondary antibody, horseradish peroxidase-conjugated rabbit anti-horse immunoglobulin G (Jackson ImmunoResearch, West Grove, Pa.), were individually preincubated for 1 h in 1 ml of PBS-Tween containing 1% (vol/vol) normal rabbit serum, centrifuged briefly, and finally diluted in PBS-Tween to 1:1,000 and 1:120,000, respectively. Blocked filters were exposed for 1 h to primary antibody, washed in PBS-Tween, then exposed for 1 h to the second antibody, and washed extensively. Proteins were detected using ECL+Plus (Amersham Life Sciences, Arlington Heights, Ill.) according to the manufacturer's protocol. Filters were exposed at room temperature to ECL Hyperfilm (Amersham Life Sciences) for the time shown.
Mouse studies.
Male C3H/HeJ mice were purchased from The Jackson Laboratory (Bar Harbor, Maine) at 3 to 4 weeks of age and used when body weights were between 9 and 15 g. Mice were inoculated intraperitoneally (i.p.) with CPV/49 at 5 × 105 TCID50/0.1 ml of unsupplemented medium or with sterile unsupplemented medium as described previously (5). No difference was observed when mice were inoculated with a 10-fold-higher dose of CPV/49 (data not shown). Hearts and pancreata from mice sacrificed at days 5, 10, 15, and 28 were excised for pathologic examination and for virus titer determination as described previously (5, 54). At 10 or 28 days after inoculation with CPV/49, mice were challenged i.p. with of CVB3/AS or CVB3/M (each at 5 × 105 TCID50/0.1 ml) or unsupplemented MEM. Hearts and pancreata were excised from mice sacrificed at day 10 postchallenge for pathologic examination.
RESULTS
Characterization of the chimeric virus CPV/49 in cell culture.
The infectious cDNA copy of the chimeric CVB3 genome, pCPV-49, containing the PV1 5′ NTR, was constructed as shown in Fig. 1. Progeny virus, termed CPV/49, was generated by electroporating plasmid pCPV-49 into COS cells. Sequence analysis of both the pCPV-49 clone and the progeny CPV/49 viral RNA demonstrated that both the infectious cDNA clone and the progeny virus contained the intact PV1/M 5′ NTR as expected (data not shown).
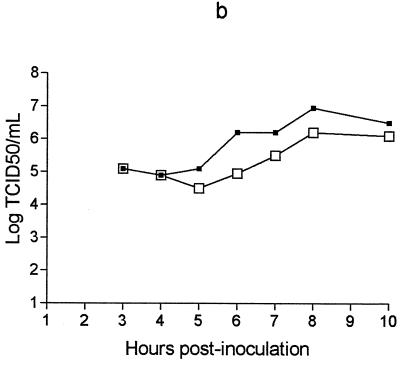
We compared the replication of CPV/49 to that of the parental CVB3/20 in different human and murine cell cultures, using one-step growth curves (Fig. 2). In addition to standard HeLa cells, we also examined HCAEC, MFHF, and Panc-1 cells as hosts for the viruses. These cells were chosen because CVB isolates replicate and cause disease in both human and murine heart and pancreas (10, 13, 14, 22, 23, 43, 46). CPV/49 and the parental CVB3/20 replicated with equivalent rates and to nearly identical titers in HeLa cell cultures (Fig. 2a). Infected HeLa cell cultures were not followed longer than 10 h, as cytopathic effects (CPE; defined as rounding up of cells and detachment from the plastic) were extensive at this time. In contrast to the rapid development of CPE in HeLa cells, neither virus induced CPE discernible by light microscopy in any of the other three cell cultures by 24 h p.i. Replication of both viruses in HCAEC cultures (Fig. 2b) was slower than in HeLa cell cultures, lagging by approximately 1 h and achieving 1- to 2-log-lower titer than in HeLa cells at 8 to 10 h for CVB3/20 and CPV/49, respectively. By 24 h p.i., CVB3/20 increased in titer by 10-fold over CPV/49 (Fig. 2e). The chimera CPV/49 was delayed in replication relative to CVB3/20 in Panc-1 cultures by approximately 2 h, and the yield ranged between 1 and 1.5 logs lower than the parental virus yield at 10 to 24 h p.i. (Fig. 2c and e).
FIG. 2.
One-step growth curve of CPV/49 and CVB3/20 in cell cultures. HeLa (a), HCAEC (b), Panc-1 (c), and MFHF (d) cultures were plated in duplicate and inoculated with either with CPV/49 or CVB3/20 as described in Materials and Methods. Plates were frozen at −74°C at the times shown. Titers were determined on HeLa cell monolayers. □, CPV/49; ■, CVB3/20. (e) Titers of viruses in the three non-HeLa cultures at 24 h p.i. Although virus-inoculated HeLa cell cultures showed typical CPE by 8 to 10 h p.i., no CPE was observed in the other cell cultures used for as long as 24 h p.i.
Replication of CPV/49 was most reduced relative to the parental CVB3 strain in MFHF culture; CPV/49 was delayed in replication relative to CVB3/20 by about 2 h and lagged behind CVB3/20 in titer by 10-fold at 10 h p.i. (Fig. 2d), although continued replication in cells over 24 h partially compensated for the disparity in virus yield (Fig. 2e). These results demonstrate that while it was not possible to differentiate between CPV/49 and the parental strain, CVB3/20, by replication in HeLa cells, the chimera CPV/49 is attenuated for both replication and virus yield relative to the parental virus in human heart- and pancreas-derived cell cultures as well as in a primary murine heart fibroblast culture.
Western analysis of viral translation in cell cultures.
Enterovirus replication upon entry into a cell is initiated by the translation of the enterovirus RNA genome; the enterovirus 5′ NTR provides the site in which viral protein translation is initiated (7, 39; reviewed in reference 28), a complex process that involves the interaction of the viral RNA primary and higher-order structures with the ribosome as well as diverse host cell proteins. Diminished or delayed translation of the chimeric CPV/49 genome might account for the attenuated rates and extents of replication observed in the different cell cultures. We therefore focused on MFHF, as CPV/49 was most attenuated in these cultures relative to the parental virus strain. Translation of the CVB3 proteins was analyzed in infected MFHF culture lysates by using Western analysis and a horse polyclonal anti-CVB3 neutralizing antibody that binds the CVB3 capsid protein 1D. Viral translation in HeLa cells was similar in timing for both CPV/49 and CVB3/20 (Fig. 3B, compare lanes 2 to 4 with lanes 5 to 7), consistent with the equivalent replication rates in these cells (Fig. 2a). However, a lower rate of CPV/49 capsid protein 1D synthesis was observed in MFHF (Fig. 3A, lanes 2 to 5) relative to the CVB3/20-infected cultures (Fig. 3A, lanes 6 to 9). The observation of lower rates and extents of translation in CPV/49-infected MFHF cultures is consistent with the attenuated replication observed in these cells.
FIG. 3.
Western blot analysis of CPV/49-infected cell cultures. (A) MFHF cultures were inoculated with CPV/49 (lanes 2 to 5) or CVB3/20 (lanes 6 to 9) at an MOI of 20. MFHF cultures were harvested at 4 (lanes 2 and 6), 7 (lanes 3 and 7), 10 (lanes 4 and 8), or 18 h (lanes 5 and 9) p.i. Lanes 1 and 9, uninfected cells. (B) HeLa cultures were inoculated with CPV/49 (lanes 2 to 4) or CVB3/20 (lanes 5 to 7) at an MOI of 20. HeLa cultures were harvested at 3.5 (lanes 2 and 5), 4.5 (lanes 3 and 6), or 6 (lanes 4 and 7) h p.i. Lane 1, uninfected cells. Ten microliters (equivalent to ca. 4 × 103 cells) was loaded per lane. A horse polyclonal neutralizing anti-CVB3 antibody was used to detect capsid protein 1D. The HeLa cell blot was exposed to film for 5 s; the MFHF blot was exposed to film for 30 s. Lane 1D, CVB3 capsid protein 1D detected in purified CVB3.
Characterization of CPV/49 in mice.
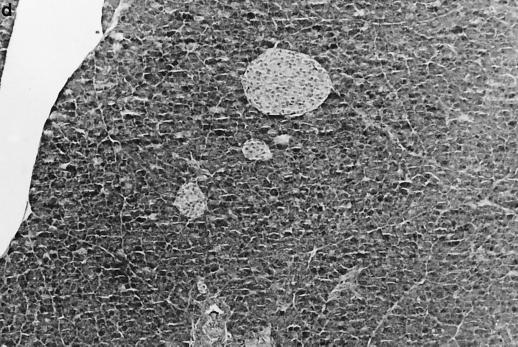
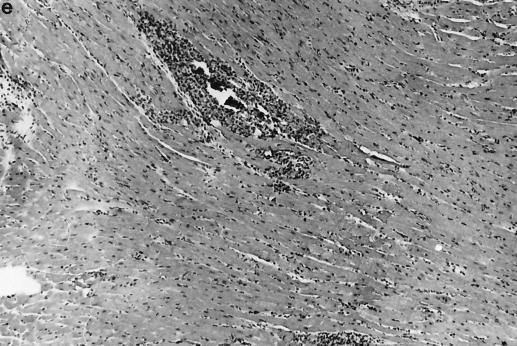
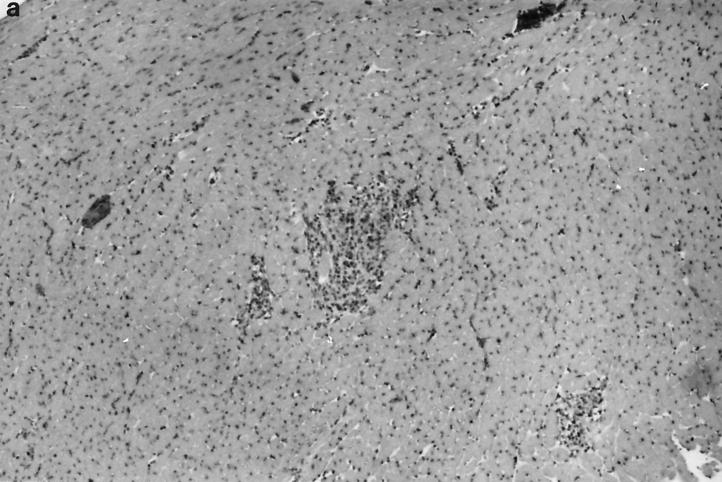
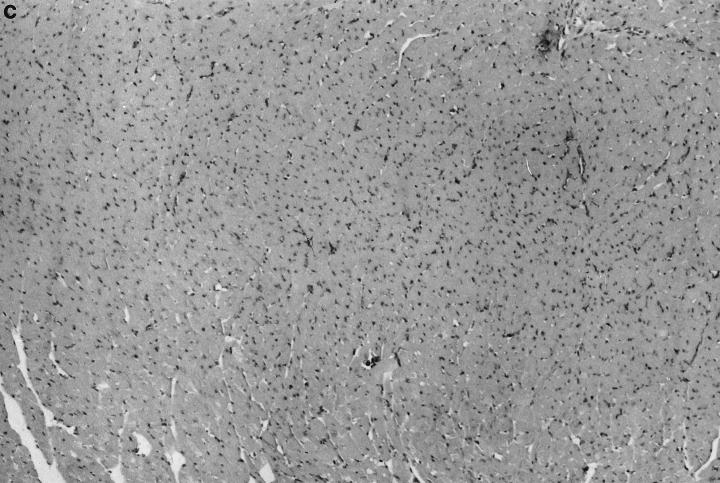
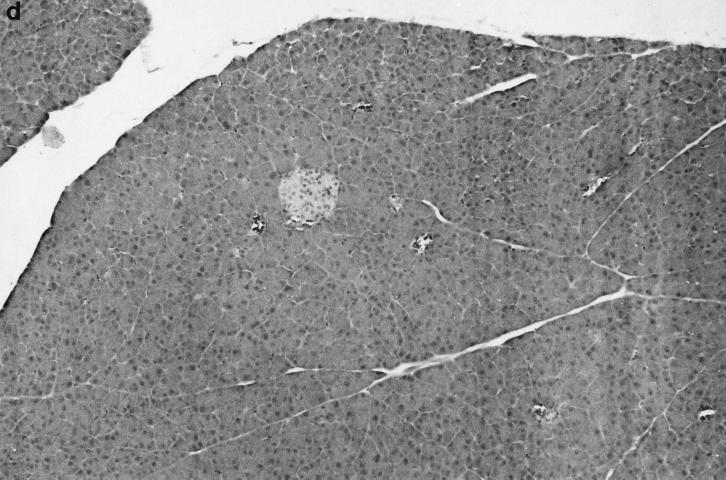
The attenuated (vaccine) phenotype of the Sabin PV strains is primarily due to the diminished translational efficiency of these viruses in cells of neural origin (33, 50; reviewed in reference 56). To determine whether the attenuated replication of CPV/49 in three different cell cultures translated to attenuation of the virulent disease phenotype of the parental CVB3/20 in mice, we inoculated mice with CPV/49 and assayed hearts and pancreata for evidence of pathologic damage by light microscopy at 10, 15, and 28 days p.i. Heart and pancreatic damage due to virulent CVB3 replication have been demonstrated to be clearly evident at 10 days p.i. (52, 55). Hearts from mice inoculated with the chimeric CPV/49 appeared normal (Fig. 4a) and were indistinguishable from organs from uninfected control mice (Fig. 4c). Although a variable and limited amount of pancreatic inflammatory disease was seen in 4 of 10 mice at days 10 and 15 p.i. (Fig. 4b), no pancreatic inflammation was observed in tissue from mice 28 days after CPV/49 inoculation, appearing identical to pancreas from uninfected control mice (Fig. 4d). In marked contrast, the virulent parental CVB3/20 induced inflammatory lesions in heart muscle at 10 days p.i. (Fig. 4e) as well as widespread inflammation and destruction of acinar tissue in pancreata (Fig. 4f). All CVB3/20-inoculated mice had inflammatory lesions in the heart and pancreas. Virus titers in hearts and pancreata of inoculated mice were determined. Hearts from mice sacrificed at 3 days p.i., a time near the peak of cardiac virus titer (52), demonstrated that titers of both the chimeric CPV/49 and the parental CVB3/20 were similar, averaging 2 × 105 TCID50 units of virus per g of heart tissue. CPV/49 replicated to an average titer of 2.78 × 104 TCID50/g in three of five hearts by day 5 p.i.; virus was not detectable in two hearts. Hearts of mice inoculated with CPV/49 taken 10, 15, and 28 days p.i. showed no detectable infectious virus when assayed on HeLa cell monolayers, similar to the established kinetics of clearance in mice of the well-characterized attenuated CVB3 strain, CVB3/0 (11). In contrast, the cardiovirulent CVB3/20 remained detectable 10 days p.i. at titers ranging from 1.8 × 104 to 1.9 × 108 TCID50 per g of heart tissue, consistent with previous observations (52, 55). Pancreatic titers of CPV/49 on day 5 p.i. averaged 2.05 × 107 TCID50/g but had declined by day 10 p.i. to an average of 1.78 × 103 TCID50/g in three mice (virus was not detected in pancreata from two mice). CPV/49 was not detected in pancreata on day 15 or 28 p.i. These results demonstrate that while the chimeric CPV/49 is capable of replicating in mice, it induces little or no disease in hearts or pancreata of susceptible mice, and it is attenuated for prolonged replication in both organs.
FIG. 4.
Characterization of CPV/49 pathology in murine heart and pancreas. Groups of 5 C3H/HeJ male mice were inoculated i.p. with 5 × 105 TCID50 of either CPV/49 or CVB3/20 and then sacrificed 10 days p.i. Control mice were inoculated with unsupplemented medium used to dilute viruses. Hearts and pancreata were harvested 10 days later, fixed in formalin, embedded and sectioned, and then stained with hemotoxylin and eosin. Shown are heart (a) and pancreas (b) from a mouse inoculated with CPV/49, heart (c) and pancreas (d) from a control uninfected mouse and heart (e) and pancreas (f) from a mouse inoculated with CVB3/20. Original magnification, ×100.
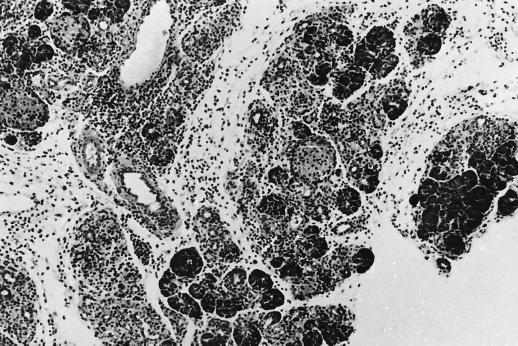
As CPV/49 demonstrated attenuated replication and avirulent disease phenotypes in both MFHF cultures and in mice, we determined whether CPV/49 could induce protective immunity against a subsequent virulent CVB3 infection in mice. Mice were inoculated once with CPV/49 and then challenged 10 or 28 days later with one of two genetically divergent (44) virulent strains of CVB3, CVB3/M (35), or CVB3/AS (53). Age-matched control mice that had received tissue culture medium (unprotected) were challenged at the same time. Ten days after challenge with virulent CVB3, the hearts and pancreata were examined by light microscopy. Seven of the ten control mice that had been challenged 28 days after inoculation with cell culture medium (Fig. 5a and b) showed damage typically induced in heart and pancreas by virulent CVB3 infection in CVB3-naive (unprotected) mice; the damage induced in these mice, as well as in the mice challenged 10 days after mock inoculation, is similar to that documented elsewhere (20). However, all hearts and pancreata the 10 CPV/49-inoculated mice that had been challenged with virulent CVB3/M challenge 28 days appeared normal, with no detectable pathologic changes following exposure to either CVB3/M (Fig. 5c and d). Mice challenged with CVB3/AS 10 days after inoculation with CPV/49 similarly showed no disease in any hearts or pancreata (data not shown).
FIG. 5.
Vaccination of mice with CPV/49. Mice were inoculated i.p. with 5 × 105 TCID50 of CPV/49 (c and d) or unsupplemented medium (a and b). Mice were challenged 28 days later with 5 × 105 TCID50 of CVB3/M. Ten days after challenge, mice were sacrificed, and hearts (a and c) and pancreata (b and d) were fixed in formalin, sectioned, and stained with hemotoxylin and eosin. Mice inoculated with CPV/49 and challenged 10 days later with either CVB3/M or CVB3/AS produced results similar to those shown here (data not shown). Original magnification, ×100.
Sera taken from mice inoculated with CPV/49 10, 15, and 28 days prior were assayed for levels of circulating anti-CVB3 neutralizing antibody. Ten days after CPV/49 inoculation, anti-CVB3 neutralizing titers ranged between 1/8 and 1/256. Titers on day 15 p.i. ranged between 1/4 and 1/64; on day 28 p.i., titers were between 1/4 and 1/8. These ranges are consistent with serum titers reported for mice following a single CVB3 inoculation (21). These data demonstrate that a single inoculation of mice with CPV/49 induced protective humoral immunity that persisted for at least 4 weeks p.i. and protected all inoculated mice from severe pancreatic and cardiac inflammatory disease induced by a virulent CVB3 challenge.
DISCUSSION
As the worldwide vaccination effort to eradicate the PVs as causes of disease moves to completion, the continued widespread use of the PVs both as research tools and as vectors for the development of chimeric vaccines (4) may be proscribed (15). It is therefore important to evaluate alternative non-PV human enterovirus systems to fill this gap. As a first step, it is necessary to explore methodology to attenuate non-PV enteroviruses for use as potential vaccine vectors. Toward this end, we demonstrate here that the replacement of the entire 5′ NTR of the cloned genome of a virulent strain of CVB3 with the 5′ NTR taken from the genome of a neurovirulent PV1 strain results in an attenuated progeny chimeric virus. The chimeric virus is attenuated for replication in cell cultures and prolonged replication in mice, and it serves as a protective vaccine against subsequent virulent CVB3 challenge in mice.
The extent of attenuation of CPV/49 is dependent on the type of cell culture used. While attenuated replication was not apparent in HeLa cells (Fig. 2a), it was observed in the three non-HeLa cell cultures used in this study. CPV/49 replicated less efficiently than the parental CVB3/20 strain in both HCAEC and Panc-1, a human tumor line of pancreatic origin (Fig. 2b and c). The attenuated phenotype was pronounced in MFHF cultures, with the rate of CPV/49 replication slowed and the virus yield 10-fold lower than for the parental CVB3/20 (Fig. 2d). The infectious titer differences in the MFHF cultures were mirrored by the differential translational efficiencies of CPV/49 in this cell type (Fig. 3). The translational differences between CPV/49 and CVB3/20 in HCAEC and Panc-1 cells were evident but less extensive than the distinct difference observed between the two viruses in MFHF cultures (data not shown). These results are similar to those documented in other studies (18, 33, 50) showing that the host cell plays a significant role in determining the rate and extent of PV replication during infection.
Based on these data, we suggest that the replicative attenuation of CPV/49 is most likely due to a combination of differential recognition by CVB3 nonstructural proteins of the PV 5′ NTR as well as differential recruitment of cellular proteins by the PV 5′ NTR (as opposed to the CVB3 5′ NTR) known to bind the enterovirus 5′ NTR (reviewed in references 2 and 6). Host cell proteins such as the La autoantigen (37), polypyrimidine tract-binding protein (25), and poly(rC)-binding proteins (8, 9, 41) have been shown to bind to the IRES and to affect translation of viral proteins. Some of these proteins are also involved in positive-strand RNA replication: the poly(rC)-binding proteins form a ternary complex with 3CD and with the 5′ cloverleaf structure of the 5′ NTR (19, 41) that is essential for viral RNA replication (3). If viral proteins and the 5′ NTR have different origins, as they do in an artificially constructed chimeric virus such as CPV/49, differences in the extents of protein-RNA binding may result which in turn could affect function. Because many of the predicted higher-order structures of enteroviral 5′ NTR RNAs are well conserved (1, 12, 34, 40, 49), the 30% nucleotide nonidentity between the CVB3 and PV1 5′ NTR sequences (51) likely plays some role in attenuating the progeny virus. That the chimera CPV/49 replicated similarly to the parental CVB3 strain in HeLa cells demonstrates that the PV1 5′ NTR is a near-normal functional substitute for that of the related but nonidentical CVB3 in the HeLa cell environment, despite the difference in 5′ NTR primary structures, confirming and extending work done in the PV system (29, 47). Even within the diverse cell cultures studied here, the CPV/49 chimera replicated within 10-fold of the yield of parental virus, demonstrating the functional conservation of the 5′ NTR among divergent enteroviruses. As the PV1 and CVB3 5′ NTR sequences are about at the limit of 5′ NTR sequence divergence within the enterovirus genus (26, 42), we therefore would expect that similar substitutions of enteroviral 5′ NTRs into a CVB genome would achieve results similar to those reported here. The extent to which the virus would replicate would likely depend on the cellular or animal host in which the virus is studied. Such artificially created 5′ NTR chimeric enteroviruses thus ought to constitute useful tools to dissect virus-host cell interactions at the protein-RNA level.
The chimeric CPV/49 virus proved to be a protective vaccine strain when tested in mice. A single inoculation of the chimeric virus protected all mice challenged 28 days later with a dose of virulent CVB3 that induced severe pancreatic and heart disease in the uninoculated age-matched control mice. CPV/49 induced minor amounts of pancreatic inflammatory disease (pancreatitis) in less than half of the mice examined on days 10 and 15, but there was no evidence of disease by day 28 p.i. No myocarditis was observed in any of the hearts from mice inoculated with CPV/49. Infectious CPV/49 was not detectable in hearts and found at only extremely low titers in pancreas by 10 days p.i.; no virus was detectable in either organ after this time. These data resemble those derived for another well-characterized, artificially attenuated strain of CVB3, CVB3/0 (11), in which the attenuated CVB3/0 is cleared from the mouse within a week p.i. While the mechanism for the different extents of persistence is not clear, it may be reasonably hypothesized that a virus, attenuated for replication in murine cells, will produce fewer rounds of infection over time, thus presenting a lower virus load and fewer infectious centers for the host immune response to neutralize. Notwithstanding the limited replication of CPV/49 in mice, a single dose of CPV/49 protected mice from disease when the mice were challenged with either of two virulent strains of CVB3, demonstrating that CPV/49 rapidly induces a protective immune response in the murine host.
The genetic stability of attenuated chimeric enteroviruses is an important issue that will require continued study. The PV Sabin strains have proven to be excellent vaccine strains, but the fact that they readily revert within days to a neurovirulent phenotype during replication in humans makes it imperative that any new generation of enteroviral vaccine and expression vectors be engineered to be as genetically stable as possible. Single base attenuating mutations in enteroviruses revert quickly, as has been demonstrated not only for the PV vaccine strains in humans (16) but in experimental animal studies of coxsackieviruses as well. Tu et al. (55) showed that a single attenuating mutation (U234C) in the CVB3 5′ NTR was responsible for attenuating the CVB3/0 strain, but that the attenuating C reverted rapidly to U both in cell culture and during replication in scid mice.
The construct CPV/49 is a chimera formed from two virulent strains of virus. Although clearly attenuated with respect to its parental virulent CVB3/20 strain, it is worth speculating that a similar chimera, formed using the genome of an avirulent CVB3 strain and the 5′ NTR from another avirulent enterovirus, or an artificially attenuated one such as a Sabin PV strain, might be completely attenuated when tested in mice and yet able to induce protective immunity. Specific nonlethal deletions may be another useful approach, in addition to 5′ NTR chimeric genomes, to generating a stable attenuated enterovirus population. Nomoto and colleagues demonstrated that various deletions just upstream of the translational initiation site in PV1 and CVB1 resulted in progeny virus and, in the case of CVB1, also attenuated the viral virulence phenotype in mice (27, 30). In preliminary work, we determined the 5′ NTR sequence from virus isolated from feces of mice inoculated 3 days prior with CPV/49 and observed no changes in the PV1/M sequence in two separate experiments (S. Tracy, J. Leser, and N. Chapman, unpublished data). These preliminary data suggest not only that a dissimilar 5′ NTR can function within a different enterovirus but that the sequence can remain stable for at least several replication cycles in mice. Experiments to characterize the biology of serially passaged CPV/49 from diverse cell cultures as well as mice will continue.
It is understood that no artificially attenuated enterovirus vaccine strain will likely remain unchanged during passage in an animal host. Selection for randomly generated mutant strains as well as revertants at the artificially mutated site(s) begins immediately upon initial replication due to the error rate inherent in the enteroviral RNA polymerase; the strain with the competitive advantage rapidly founds the next dominant quasispecies population. As the attenuated (vaccine) strain must replicate in a host in which the wild-type virus has a long history of adaptation, the presence of wild-type like variants within the vaccine strain population will force significant and rapid changes in the makeup of the viral quasispecies. The challenge for designing a new generation of enteroviral vaccine and expression vectors will be to understand how nucleotide sequence changes that are tolerated and maintained during many rounds of replication could serve to attenuate these viruses for disease.
ACKNOWLEDGMENTS
We thank the Barrick family, the Jurgensmier family, and E. Barnett for generous donations in support of this work in memory of Mary Barrick, Jason Jurgensmier, and Sharon Ann Watson, respectively. This work was also supported in part by grants from the American Heart Association (N.M.C. and S.T.), the USPHS (N.M.C. and B.L.S.), and the Technology Advancement Group at UNMC (N.M.C. and S.T.).
REFERENCES
- 1.Agol V. The 5′ untranslated region of picornaviral genomes. Adv Virus Res. 1991;40:103–180. doi: 10.1016/S0065-3527(08)60278-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andino R, Boddeker N, Silvera D, Gamarnik A. Intracellular determinants of picornavirus replication. Trends Microbiol. 1999;7:76–82. doi: 10.1016/s0966-842x(98)01446-2. [DOI] [PubMed] [Google Scholar]
- 3.Andino R, Rickehof G E, Baltimore D. Poliovirus RNA synthesis utilizes an RNP complex formed around the 5′ end of the viral RNA. EMBO J. 1993;12:3587–3598. doi: 10.1002/j.1460-2075.1993.tb06032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andino R, Silvera D, Suggett S D, Achaso P L, Miller C J, Baltimore D, Feinberg M. Engineering poliovirus as a vaccine vector for the expression of diverse antigens. Science. 1994;265:1448–1451. doi: 10.1126/science.8073288. [DOI] [PubMed] [Google Scholar]
- 5.Beck M, Tracy S. Murine cell-mediated immune response recognizes an enterovirus group-specific antigen(s) J Virol. 1989;63:4148–4156. doi: 10.1128/jvi.63.10.4148-4156.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belsham G J, Sonenberg N. RNA-protein interactions in regulation of picornavirus RNA translation. Microbiol Rev. 1996;60:499–511. doi: 10.1128/mr.60.3.499-511.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bienkowska-Szewczyk K, Ehrenfeld E. An internal 5′-noncoding region required for translation of poliovirus RNA in vitro. J Virol. 1988;62:3068–3072. doi: 10.1128/jvi.62.8.3068-3072.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blyn L B, Swiderek K M, Richards O, Stahl D C, Semler B L, Ehrenfeld E. Poly(rC) binding protein 2 binds to stemloop IV of the poliovirus RNA 5′ noncoding region: identification by automated liquid chromatography-tandem mass spectrometry. Proc Natl Acad Sci USA. 1996;93:11115–11120. doi: 10.1073/pnas.93.20.11115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blyn L B, Towner J S, Semler B L, Ehrenfeld E. Requirement of poly(rC) binding protein 2 for translation of poliovirus RNA. J Virol. 1997;71:6243–6246. doi: 10.1128/jvi.71.8.6243-6246.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chapman N M, Ramsingh A I, Tracy S. Genetics of coxsackievirus virulence. Curr Top Microbiol Immunol. 1997;223:227–258. doi: 10.1007/978-3-642-60687-8_11. [DOI] [PubMed] [Google Scholar]
- 11.Chapman N M, Tu Z, Tracy S, Gauntt C J. An infectious cDNA copy of the genome of a non-cardiovirulent coxsackievirus B3 strain: its complete sequence analysis and comparison to the genomes of cardiovirulent coxsackieviruses. Arch Virol. 1994;135:115–130. doi: 10.1007/BF01309769. [DOI] [PubMed] [Google Scholar]
- 12.Currey K M, Shapiro B A. Secondary structure computer prediction of the poliovirus 5′ non-coding region is improved by a genetic algorithm. Comput Appl Biosci. 1997;13:1–12. doi: 10.1093/bioinformatics/13.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Dalldorf G. The coxsackie viruses. Annu Rev Microbiol. 1955;9:277–296. doi: 10.1146/annurev.mi.09.100155.001425. [DOI] [PubMed] [Google Scholar]
- 14.Dalldorf G, Gifford R. Adaptation of group B coxsackie virus to adult mouse pancreas. J Exp Med. 1952;95:491–497. doi: 10.1084/jem.96.5.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dowdle W R, Featherstone D A, Birmingham M F, Hull H F, Aylward R. Poliomyelitis eradication. Virus Res. 1999;62:185–192. doi: 10.1016/s0168-1702(99)00044-1. [DOI] [PubMed] [Google Scholar]
- 16.Evans D, Dunn G, Minor P D, Schild G C, Cann A J, Stanway G, Almond J W, Currey K, Maizel J. Increased neurovirulence associated with a single nucleotide change in a noncoding region of the Sabin type 3 poliovaccine genome. Nature. 1985;314:548–550. doi: 10.1038/314548a0. [DOI] [PubMed] [Google Scholar]
- 17.Francki R, Fauquet C, Knudson D, Brown F. Classification and nomenclature of viruses. Vienna, Austria: Springer-Verlag; 1991. [Google Scholar]
- 18.Freistadt M S, Eberle K E. Correlation between poliovirus type 1 Mahoney replication in blood cells and neurovirulence. J Virol. 1996;70:6486–6492. doi: 10.1128/jvi.70.9.6486-6492.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gamarnik A V, Andino R. Two functional complexes formed by KH domain containing proteins with the 5′ noncoding region of poliovirus RNA. RNA. 1997;3:882–892. [PMC free article] [PubMed] [Google Scholar]
- 20.Gauntt C J, Gomez P T, Duffey P S, Grant J A, Trent D W, Witherspoon S M, Paque R E. Characterization and myocarditic capabilities of coxsackievirus B3 variants in selected mouse strains. J Virol. 1984;52:598–605. doi: 10.1128/jvi.52.2.598-605.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Godeny E, Arizpe H M, Gauntt C J. Characterization of the antibody response in vaccinated mice protected against coxsackievirus B3 induced myocarditis. Viral Immunol. 1987;1:305–314. doi: 10.1089/vim.1987.1.305. [DOI] [PubMed] [Google Scholar]
- 22.Gomez R M, Lascano E F, Berria M I. Murine acinar pancreatitis preceding necrotizing myocarditis after coxsackievirus B3 inoculation. J Med Virol. 1991;35:71–75. doi: 10.1002/jmv.1890350202. [DOI] [PubMed] [Google Scholar]
- 23.Gomez R M, Cui X, Castagnino C G, Berria M I. Differential behavior in pancreas and heart of two coxsackievirus B3 variants. Intervirology. 1993;36:153–160. doi: 10.1159/000150334. [DOI] [PubMed] [Google Scholar]
- 24.Gromeier M, Alexander L, Wimmer E. Internal ribosomal entry site substitution eliminates neurovirulence in intergeneric poliovirus recombinants. Proc Natl Acad Sci USA. 1996;93:2370–2375. doi: 10.1073/pnas.93.6.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gutierrez A L, Denova-Ocampo M, Racaniello V R, del Angel R M. Attenuating mutations in the poliovirus 5′ untranslated region alter its interaction with polypyrimidine tract-binding protein. J Virol. 1997;71:3826–3833. doi: 10.1128/jvi.71.5.3826-3833.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hyypia T, Hovi T, Knowles N, Stanway G. Classification of enteroviruses based on molecular and biological properties. J Gen Virol. 1997;78:1–11. doi: 10.1099/0022-1317-78-1-1. [DOI] [PubMed] [Google Scholar]
- 27.Iizuka N, Yonekawa H, Nomoto A. Nucleotide sequences important for translation initiation of enterovirus RNA. J Virol. 1991;65:4867–4873. doi: 10.1128/jvi.65.9.4867-4873.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jackson R J, Kaminski A. Internal initiation of translation in eukaryotes: the picornavirus paradigm and beyond. RNA. 1995;1:985–1000. [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson V H, Semler B L. Defined recombinants of poliovirus and coxsackievirus: sequence-specific deletions and functional substitutions in the 5′-noncoding regions of viral RNAs. Virology. 1988;162:47–57. doi: 10.1016/0042-6822(88)90393-5. [DOI] [PubMed] [Google Scholar]
- 30.Kuge S, Nomoto A. Construction of viable deletion and insertion mutants of the Sabin strain of type poliovirus: function of the 5′ noncoding sequence in viral replication. J Virol. 1987;61:1478–1487. doi: 10.1128/jvi.61.5.1478-1487.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuhn R J, Wimmer E, Semler B L. Expression of the poliovirus genome from infectious cDNA is dependent upon arrangements of eukaryotic and prokaryotic sequences in recombinant plasmids. Virology. 1987;157:560–564. doi: 10.1016/0042-6822(87)90302-3. [DOI] [PubMed] [Google Scholar]
- 32.Laemmli U. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 33.La Monica N, Racaniello V R. Differences in replication of attenuated and neurovirulent polioviruses in human neuroblastoma cell line SH-SY5Y. J Virol. 1989;63:2357–2360. doi: 10.1128/jvi.63.5.2357-2360.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le S Y, Zuker M. Common structures of the 5′ non-coding RNA in enteroviruses and rhinoviruses. J Mol Biol. 1990;216:729–741. doi: 10.1016/0022-2836(90)90395-3. [DOI] [PubMed] [Google Scholar]
- 35.Lee C, Maull E, Chapman N, Tracy S, Wood J, Gauntt C. Generation of an infectious cDNA of a highly cardiovirulent coxsackievirus B3(CVB3m) and comparison to other infectious CVB3 cDNAs. Virus Res. 1997;50:225–235. doi: 10.1016/s0168-1702(97)00059-2. [DOI] [PubMed] [Google Scholar]
- 36.Lu H, Wimmer E. Poliovirus chimeras replicating under the translational control of genetic elements of hepatitis C virus reveal unusual properties of the internal ribosomal entry site of hepatitis C virus. Proc Natl Acad Sci USA. 1996;93:1412–1417. doi: 10.1073/pnas.93.4.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meerovitch K, Svitkin Y V, Lee H S, Lejbkowicz F, Kenan D J, Chan E K, Agol V I, Keene J D, Sonenberg N. La autoantigen enhances and corrects aberrant translation of poliovirus RNA in reticulocyte lysate. J Virol. 1993;67:3798–3807. doi: 10.1128/jvi.67.7.3798-3807.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Modlin J F, Rotbart H A. Group B coxsackievirus disease in children. Curr Top Microbiol Immunol. 1997;223:53–80. doi: 10.1007/978-3-642-60687-8_4. [DOI] [PubMed] [Google Scholar]
- 39.Nicholson R, Pelletier J, Le S Y, Sonenberg N. Structural and functional analysis of the ribosome landing pad of poliovirus type 2: in vivo translation studies. J Virol. 1991;65:5886–5894. doi: 10.1128/jvi.65.11.5886-5894.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Palmenberg A C, Sgro J-Y. Topological organization of picornaviral genomes: statistical prediction of RNA structural signals. Semin Virol. 1997;8:231–241. [Google Scholar]
- 41.Parsley T B, Towner J S, Blyn L B, Ehrenfeld E, Semler B L. Poly (rC) binding protein 2 forms a ternary complex with the 5-terminal sequences of poliovirus RNA and the viral 3CD proteinase. RNA. 1997;3:1124–1134. [PMC free article] [PubMed] [Google Scholar]
- 42.Poyry T, Kinnunen L, Hyypia T, Brown B, Horsnell C, Hovi T, Stanway G. Genetic and phylogenetic clustering of enteroviruses. J Gen Virol. 1996;77:1699–1717. doi: 10.1099/0022-1317-77-8-1699. [DOI] [PubMed] [Google Scholar]
- 43.Ramsingh A I, Chapman N M, Tracy S. Coxsackieviruses and diabetes. Bioessays. 1997;19:793–800. doi: 10.1002/bies.950190909. [DOI] [PubMed] [Google Scholar]
- 44.Romero J R, Price C, Dunn J J. Genetic divergence among group B coxsackieviruses. Curr Top Microbiol Immunol. 1997;223:97–152. doi: 10.1007/978-3-642-60687-8_6. [DOI] [PubMed] [Google Scholar]
- 45.Romero J R, Rotbart H A. Sequence analysis of the downstream 5′ nontranslated region of seven echoviruses with different neurovirulence phenotypes. J Virol. 1995;69:1370–1375. doi: 10.1128/jvi.69.2.1370-1375.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schoub B D, Johnson S, McAnerney J M, Dos Santos I L, Klaassen K I. Epidemic coxsackie B virus infection in Johannesburg, South Africa. J Hyg (London) 1985;95:447–455. doi: 10.1017/s0022172400062872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Semler B L, Johnson V H, Tracy S. A molecular recombinant plasmid from cDNA clones of poliovirus and coxsackievirus produces an infectious virus that is temperature sensitive. Proc Natl Acad Sci USA. 1986;83:1777–1781. doi: 10.1073/pnas.83.6.1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Semler B L, Dorner A, Wimmer E. Production of infectious poliovirus from cloned cDNA is dramatically increased by SV40 transcription and replication signals. Nucleic Acids Res. 1984;12:5123–5141. doi: 10.1093/nar/12.12.5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Skinner M, Racaniello V, Dunn G, Cooper J, Minor P D, Almond J W. New model for the secondary structure of the 5′ non-coding RNA of poliovirus is supported by biochemical and genetic data that also show that RNA secondary structure is important in neurovirulence. J Mol Biol. 1989;207:379–392. doi: 10.1016/0022-2836(89)90261-1. [DOI] [PubMed] [Google Scholar]
- 50.Svitkin Y V, Maslova S V, Agol V I. The genomes of attenuated and virulent poliovirus strains differ in their in vitro translation efficiencies. Virology. 1985;147:243–252. doi: 10.1016/0042-6822(85)90127-8. [DOI] [PubMed] [Google Scholar]
- 51.Tracy S, Chapman N M, Liu H L. Molecular cloning and partial characterization of the coxsackievirus B3 genome. Arch Virol. 1985;85:157–163. doi: 10.1007/BF01317016. [DOI] [PubMed] [Google Scholar]
- 52.Tracy S, Chapman N M, Tu Z. Coxsackievirus B3 from an infectious cDNA copy of the genome is cardiovirulent in mice. Arch Virol. 1992;122:399–409. doi: 10.1007/BF01317202. [DOI] [PubMed] [Google Scholar]
- 53.Tracy S, Gauntt C J. Phenotypic and genotypic differences among naturally occurring coxsackie B3 virus variants. Europ Heart J. 1988;8(Suppl. J):445–448. [Google Scholar]
- 54.Tracy, S., K. Höfling, S. Pirruccello, P. H. Lane, S. M. Reyna, and C. J. Gauntt. Group B coxsackievirus myocarditis and pancreatitis in mice: connection between viral virulence phenotypes. J. Med. Virol., in press. [DOI] [PubMed]
- 55.Tu Z, Chapman N M, Hufnagel G, Tracy S, Romero J R, Barry W H, Currey K, Shapiro B. The cardiovirulent phenotype of coxsackievirus B3 is determined at a single site in the genomic 5′ nontranslated region. J Virol. 1995;69:4607–4618. doi: 10.1128/jvi.69.8.4607-4618.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wimmer E, Hellen C U, Cao X. Genetics of poliovirus. Annu Rev Genet. 1993;27:353–436. doi: 10.1146/annurev.ge.27.120193.002033. [DOI] [PubMed] [Google Scholar]
- 57.Zell R, Klingel K, Sauter M, Fortmuller U, Kandolf R. Coxsackieviral proteins functionally recognize the polioviral cloverleaf structure of the 5′NTR of a chimeric enterovirus RNA: influence of species specific host cell factors on virus growth. Virus Res. 1995;39:871–873. doi: 10.1016/0168-1702(95)00075-5. [DOI] [PubMed] [Google Scholar]