Abstract
Introduction:
Menu calorie labeling has been implemented in food service businesses to promote healthy food choices; however, evidence is limited on whether label use is associated with healthier dietary intake. This study examined the association between menu calorie label use and diet quality and whether it varied by weight status.
Methods:
Adults in the National Health and Nutrition Examination Survey 2017-2018 who visited restaurants were included. Menu calorie label use was categorized as did not notice labels, noticed labels, and used labels. Diet quality was measured using the Healthy Eating Index 2015 (maximum score 100) by two 24-hour diet recalls. The association between menu calorie label use and diet quality was examined using multiple linear regression and tested for effect modification by weight status. Data were collected during 2017-2018 and analyzed during 2022-2023.
Results:
Of 3,312 participants (representing 195,167,928 U.S. adults), 43% did not notice labels, 30% noticed labels, and 27% used labels. Using labels was associated with 4.0 points (95% CI 2.2, 5.8) higher Healthy Eating Index 2015 scores than not noticing labels. Healthy Eating Index 2015 scores in those using labels were higher for adults with normal BMI (3.4 points; 95% CI=0.2, 6.7), overweight (6.5 points; 95% CI=3.6, 9.5), and obesity (3.0 points; 95% CI=1.0, 5.1) (p-interaction=0.0004) than those who did not notice labels.
Conclusions:
Using menu calorie labels was associated with modestly healthier diet quality than not noticing labels, regardless of weight status. This suggests that providing caloric information may help some adults with food decisions.
INTRODUCTION
In the past three decades, Americans have increasingly consumed more meals outside their homes, which now accounts for 34% of daily calorie intake.1 During this time, calorie-dense options and larger portion sizes have also become more common in the U.S. food environment.2 Americans underestimate caloric content by a mean 110 calories per restaurant food item,3 contributing to overconsumption of calories at restaurants and increased obesity risk.4 Mean energy intake by Americans is 3,682 calories per day,5,6 which is higher than the federal daily recommendations of 1,600–2,400 calories for women and 2,000–3,000 calories for men.7 With rising rates of overweight, obesity, and cardiometabolic disease in the U.S.,8-12 behavioral interventions to improve food choices when dining out, including nutrition information, portion size control, and social models,13 have become a public health priority.14
Menus with calorie labels displayed for each meal option are an increasingly common public health strategy to support population-level weight control efforts. In 2018, the Patient Protection and Affordable Care Act (ACA) mandated menu calorie labels for all menu items paired with a daily recommended calorie intake statement (e.g., 2,000 calories a day is used for general nutrition advice, but individual calorie needs vary) in chain restaurants across all U.S. states.
Menu calorie labels have the potential to improve public health through multiple pathways, including healthier food purchases by consumers and reformulations of unhealthy items by chain restaurants. In a meta-analysis of 19 studies, menu calorie labeling was associated with a mean decrease of 18.1 kilocalories purchased per meal.15 In adults with obesity, a small study found a 318 kilocalorie (26%) reduction in meal ordering with menu calorie labels compared with other types of labels in a lab setting.16 However, studies in real-world settings show mixed results, suggesting that menu calorie labels may, but inconsistently, influence purchasing at full-service and coffee shop restaurants and largely have no influence in fast-food restaurants.17-19 One reason may be that many consumers do not notice the labels; after city-wide calorie labels were mandated for chain restaurants in New York City, 46% of those surveyed at fast-food restaurants in low-income communities still did not notice them nor did their caloric purchases change after implementation.20 Government mandates for calorie labeling can also decrease caloric content of menu items through reformulations by the restaurant chain.21,22 A study of 57 large U.S. restaurant chains found no reformulation of existing menu items but did find a reduction of 110 calories per new menu item (95% CI= −208.6, −25.2) after implementation of the ACA calorie label mandate.23
Nutrient density is also an important consideration in cardiometabolic disease prevention,24 and frequent consumption of meals away from home is associated with lower diet quality.4 Recent evidence suggests that diet quality contributes to risk of obesity and may be even more influential than calorie restriction for weight loss.25,26 Regardless, most of the prior research on menu calorie labels focus on caloric quantity rather than diet quality.15,27-29 Menu calorie labels may guide individuals with overweight and obesity, who struggle with excess dietary intake of foods with lower diet quality.30,31 Having overweight/obesity is also associated with increased use of calorie labels,32,33 highlighting their potential to improve dietary choices in this population. However, little is known about whether menu calorie labeling influences diet quality among adults with overweight or obesity. Using nationally representative data, this study examined whether menu calorie label use is associated with diet quality among U.S. adults and whether that association differs among individuals with obesity, overweight, or normal BMI.
METHODS
Study Population
The National Health and Nutrition Examination Survey (NHANES) is an annual, cross-sectional study to assess the health and nutritional status of non-institutionalized U.S. residents. Data collected during 2017–2018 in NHANES were used, including questionnaires, body measurements, 24-hour dietary recalls, and the Consumer Behavior Phone Follow-up Module (CBQPFA). NHANES participants completed interviewer-administered questionnaires during a home visit and had anthropomorphic measurements and a 24-hour dietary recall collected at the mobile examination center visit. Participants later completed a telephone visit, with a second 24-hour dietary recall and the CBQPFA. NHANES collected 24-hour dietary recalls using the Automated Multiple-Pass Method34 with a trained dietary interviewer. NHANES recruited participants using a complex, multistage, probability design to create a nationally representative sample. Additional details on NHANES methodology have been previously reported.35
Study participants were adults aged from 18 to 79 years who reported buying food from a restaurant in the past 12 months. Restaurant use data were obtained from the CBQPFA. Individuals were excluded if they were underweight (BMI<18.5; n=80); had implausible dietary recall data (<500 or >5,000 total kilocalories for women and <500 or >8,000 total kilocalories for men; n=341); or had missing data on any covariates except family income or certain comorbidities (n=72; see Statistical Analysis section).
Participation in NHANES was voluntary, and all NHANES participants provided written informed consent for both the home interview and health examination components during the household visit.35 This secondary analysis using publicly available NHANES data was considered not human research by the Northwestern University IRB.
Measures
The exposure was self-reported menu calorie label use at different types of restaurants where participants purchased food and beverages (sit-down, fast-food, buffet, and coffee shop/juice bar restaurants) within the past 12 months.36 The CBQPFA questionnaire asked the following question about the last time food or beverages were purchased from that site: Did you notice any calorie information on the menu? Responses of no in all settings were categorized as did not notice labels, which included individuals who visited restaurants without calorie labeled menus and those who did not notice them (Appendix Figure 1). The follow-up question to a yes response for each setting was Did you use the information in deciding what to buy? Participants who answered yes in any setting were categorized as used labels, which represented individuals who saw and used a menu calorie label in the most recent restaurant visit. Those who answered no to the follow-up question in all settings were categorized as noticed labels, which represented individuals who saw but did not used a menu calorie label to inform their food choices in the most recent visit.
The primary outcome was diet quality, measured by the Healthy Eating Index 2015 (HEI-2015). The HEI-2015 has a maximum score of 100 points, with higher scores indicating heathier diet quality, which is consistent with the 2015–2020 Dietary Guidelines for Americans.37 Differences of 5 points in HEI-2015 are considered clinically significant.38 Using a SAS macro for the Per Person Simple HEI-2015 Scoring Algorithm,39-41 HEI-2015 total and component scores were generated from the 2-day 24-hour dietary recalls of each participant. Secondary outcomes were the HEI-2015 component scores (Total Fruits, Whole Fruits, Total Vegetables, Greens and Beans, Whole Grains, Dairy, Total Protein Foods, Seafood and Plant Proteins, Fatty Acids, Refined Grains, Sodium, Added Sugars, and Saturated Fats). Raw HEI-2015 component maximum scores are either 5 or 10 depending on the specific component; each component score was standardized to a range of 0 to 100 for comparability with total scores and across component scores. For most HEI-2015 components, a higher score represented greater intake, except for components of moderation (Refined Grains, sodium, Added Sugars, and Saturated fats), for which a higher score represented lower intake.
Weight status was treated as a potential effect modifier. Using the measured BMI of the participants, weight status was categorized as normal BMI (18.5≤BMI<25), overweight (25≤BMI<30), or obesity (BMI≥30).
Statistical Analysis
Weighted percentages with standard errors were used for categorical variables and weighted means with standard deviations for continuous variables to describe demographic, socioeconomic, diet-related comorbidities, and health behavior data by label use and weight status. Multiple linear regression was used to assess the difference in mean HEI-2015 between those who did not notice labels, those who noticed labels, and those who used labels. Covariates included age (continuous; range, 18–80 years), sex (female or male), education level (some high school or less, high-school diploma/associates degree/some college, or 4-year college degree or higher), family income (≤200% or >200% of the federal poverty level), diet-related comorbidities, weight status, weight goal to control or lose weight (yes or no), meals away from home over the past 7 days (continuous; range, 0–21), tobacco smoking in the past 5 days (yes or no), and recreational physical activity (moderate-intensity–equivalent minutes per week). Self-reported high blood pressure, high cholesterol, coronary heart disease, stroke, congestive heart failure, and prediabetes/diabetes were categorized as diet-related comorbidities and analyzed as a count (0–6).42 In NHANES, participants reported the number of days per week and minutes per day that they were engaged in recreational moderate- or vigorous-intensity physical activity. Following a previously validated approach, moderate-intensity–equivalent minutes per week were calculated by multiplying frequency per week and duration per day for physical activities, doubling vigorous-intensity minutes per week, and adding them to moderate-intensity minutes per week.43,44
To determine whether overweight or obesity moderated the relationship between label use and diet quality, an interaction term for label use and weight status was added, adjusting for all covariates included in the primary model. Statistical significance of the interaction was defined by α=0.05, with estimates to be generated within each subsample of weight status if the interaction was statistically significant. Analyses were performed in 2022–2023 using SAS, version 9.4 and 2-day dietary recall weights to account for the complex survey design of NHANES.
RESULTS
The final sample included 3,312 individuals, representing 195.2 million U.S. adults. Weighted mean age was 46.4 (SD=1.1) years, and 49.5% were female. Among those who self-reported using menu calorie labels (Table 1), females, participants with college degrees or higher, and those with family incomes >200% of federal poverty level were more highly represented than those who did not use labels and those who did not notice labels. Diet-related comorbidities, especially hypertension, hyperlipidemia, and diabetes, were less prevalent in those who used labels than in those who did not notice labels. Label use was not different between participants with normal BMI, overweight, or obesity (Table 2).
Table 1.
Participant Characteristics of 3,312 Participants Representing 195,167,928 U.S. Adults by Label Use
| Characteristics | Did not notice labels, weighted % (SE) (n=1,591; 42.5%) |
Noticed labels, weighted % (SE) (n=930; 30.3%) |
Used labels, weighted % (SE) (n=791; 27.2%) |
|---|---|---|---|
| Age, in years, mean (SD) | 49.6 (1.2) | 41.7 (1.5) | 42.9 (1.6) |
| Female | 46.9 (1.8) | 46.2 (3.0) | 57.3 (2.4) |
| Race/ethnicity | |||
| Asian | 5.2 (1.0) | 5.1 (1.2) | 5.9 (1.5) |
| Black | 12.1 (1.7) | 11.3 (2.0) | 10.6 (2.0) |
| Hispanic | 17.6 (2.1) | 14.0 (2.8) | 16.7 (2.6) |
| Multiracial/additional | 4.1 (0.5) | 4.9 (1.1) | 4.0 (0.9) |
| White | 61.0 (3.1) | 64.7 (4.1) | 62.9 (3.8) |
| Education | |||
| Some HS or lower | 15.8 (1.3) | 8.4 (0.7) | 8.0 (1.2) |
| HS diploma, AA/AS degree, or some college | 58.6 (2.9) | 62.5 (3.4) | 46.7 (4.3) |
| ≥4-year college degree | 25.6 (2.9) | 29.1 (3.4) | 45.2 (5.2) |
| Family income | |||
| ≤200% FPL | 35.7 (2.3) | 26.2 (2.1) | 19.0 (1.7) |
| >200% FPL | 53.5 (2.7) | 67.3 (2.8) | 73.1 (2.2) |
| Missing data | 10.8 (1.2) | 6.4 (1.8) | 7.9 (1.6) |
| Diet-related comorbidities | |||
| Hypertension | 35.6 (2.9) | 29.9 (2.3) | 27.3 (3.2) |
| Hyperlipidemia | 36.4 (2.0) | 26.2 (2.5) | 30.1 (2.5) |
| Diabetes | 14.8 (1.6) | 10.5 (1.2) | 7.7 (1.0) |
| Prediabetes | 12.0 (2.1) | 9.7 (1.1) | 12.1 (1.9) |
| Coronary artery disease | 3.6 (0.6) | 3.2 (0.6) | 3.2 (0.8) |
| Congestive heart failure | 2.3 (0.5) | 1.1 (0.4) | 1.6 (0.5) |
| Stroke | 3.6 (0.6) | 2.7 (0.5) | 2.7 (0.5) |
| Controlling or losing weight | 60.7 (2.2) | 61.8 (2.2) | 80.3 (2.0) |
| Meals away from home over past 7 days, mean (SD) | 3.3 (0.4) | 3.9 (0.3) | 4.2 (0.4) |
| Recent tobacco smoking | 22.2 (2.0) | 21.1 (2.7) | 12.2 (1.4) |
| Recreational physical activity, MIEMs/week, mean (SD) | 234 (52) | 234 (39) | 389 (60) |
AA, Associate of Arts; AS, Associate of Science; FPL, federal poverty level; HS, high school; MIEM, moderate-intensity–equivalent minute; SE, standard error.
Table 2.
Participant Characteristics of 3,312 Participants Representing 195,167,928 U.S. Adults by Weight Status
| Characteristics | Normal BMI, Weighted % (SE) (n=848; 26.3%) |
Overweight, weighted % (SE) (n=976; 29.0%) |
Obese, weighted % (SE) (n=1,488; 44.7%) |
|---|---|---|---|
| Age, in years, mean (SD) | 40.6 (1.9) | 48.0 (1.9) | 46.6 (1.4) |
| Female | 56.1 (3.2) | 45.9 (2.9) | 48.0 (2.2) |
| Race/ethnicity | |||
| Asian | 8.5 (1.6) | 7.4 (1.5) | 2.2 (0.4) |
| Black | 10.2 (1.5) | 9.6 (1.9) | 13.4 (2.2) |
| Hispanic | 11.4 (1.7) | 18.8 (2.7) | 17.5 (2.2) |
| Multiracial/additional | 3.7 (0.7) | 4.3 (1.1) | 4.3 (1.1) |
| White | 66.2 (2.9) | 59.9 (4.6) | 59.9 (4.6) |
| Education | |||
| Some HS or lower | 14.5 (1.7) | 10.1 (1.5) | 10.6 (0.8) |
| HS diploma, AA/AS degree, or some college | 48.2 (3.6) | 52.1 (3.1) | 64.4 (2.6) |
| Four-year college degree or higher | 37.3 (4.5) | 37.8 (3.2) | 25.1 (2.5) |
| Family income | |||
| ≤200% FPL | 27.6 (2.3) | 25.3 (2.6) | 30.7 (1.6) |
| >200% FPL | 61.4 (2.7) | 66.2 (2.6) | 61.9 (2.4) |
| Missing data | 11.0 (1.8) | 8.5 (1.5) | 7.4 (1.2) |
| Diet-related comorbidities | |||
| Hypertension | 14.4 (2.3) | 30.0 (2.2) | 41.2 (2.9) |
| Hyperlipidemia | 23.1 (2.5) | 33.8 (2.5) | 33.4 (2.0) |
| Diabetes | 4.6 (0.8) | 9.6 (1.0) | 16.5 (1.4) |
| Prediabetes | 4.1 (0.9) | 12.5 (2.4) | 14.7 (1.7) |
| Coronary artery disease | 2.1 (0.7) | 3.3 (0.7) | 4.1 (0.8) |
| Congestive heart failure | 0.3 (0.2) | 1.0 (0.3) | 3.0 (0.4) |
| Stroke | 2.0 (0.6) | 2.2 (0.7) | 4.2 (0.9) |
| Controlling or losing weight | 46.1 (2.6) | 68.1 (2.6) | 77.1 (1.7) |
| Meals away from home over past 7 days, mean (SD) | 3.8 (0.6) | 3.7 (0.5) | 3.7 (0.3) |
| Recent tobacco smoking | 20.0 (2.4) | 17.8 (1.5) | 19.6 (1.4) |
| Recreational physical activity, MIEMs/week, mean (SD) | 318 (71) | 289 (36) | 243 (46) |
| Label use | |||
| Did not notice labels | 43.7 (3.3) | 41.2 (1.7) | 42.7 (1.7) |
| Noticed labels | 31.2 (2.5) | 29.8 (3.2) | 30.1 (1.8) |
| Used labels | 25.1 (3.0) | 29.0 (2.3) | 27.2 (2.6) |
AA, Associate of Arts; AS, Associate of Science; FPL, federal poverty level; HS, high school; MIEM, moderate-intensity–equivalent minute.
In those who did not notice labels, the unadjusted mean HEI-2015 total score was 51.2 (SD=1.3). Among those who used menu calorie labels, HEI-2015 total scores were 4.0 points higher (95% CI 2.2, 5.8) than in those who did not notice labels. Those who used labels had higher HEI-2015 component scores than those who did not notice labels for whole fruits (adjusted difference=7.6; 95% CI=0.4, 14.8), total vegetables (adjusted difference=7.1; 95% CI=2.5, 11.8), greens and beans (adjusted difference=11.7; 95% CI=4.1, 19.3), total protein (adjusted difference=2.9; 95% CI=0.1, 5.7), and seafood and plant proteins (adjusted difference=8.6; 95% CI=3.4, 13.8). Among those who used labels, all other HEI-2015 component scores aside from sodium were also higher than that of those who did not notice labels, although the CIs contained the null value (Table 3). In those who noticed labels, HEI-2015 total and components scores were not different from those who did not notice labels, except for whole fruits (adjusted difference=7.3; 95% CI=1.9, 12.6) and sodium (adjusted difference=3.8; 95% CI=0.2, 7.4).
Table 3.
Crude and Adjusted Odds Ratios of the Association Between Menu Calorie Label Use and Healthy Eating Index 2015 Scores
| Outcomes | Did not notice labels (ref) |
Noticed labels | Used labels | ||
|---|---|---|---|---|---|
| Unadjusted mean (SD) |
Crude difference (95% CI) |
Adjusteda difference (95% CI) |
Crude difference (95% CI) |
Adjusteda difference (95% CI) |
|
| Total HEI-2015 | 51.2 (49.8, 52.7) | −0.3 (−2.5, 2.0) | 0.6 (−1.4, 2.6) | 4.7 (2.6, 6.7)b | 4.0 (2.2, 5.8)b |
| Total fruits | 41.4 (37.4, 45.4) | 0.4 (−5.8, 6.6) | 3.0 (−2.4, 8.4) | 4.7 (−1.5, 11.0) | 4.3 (−1.0, 9.5) |
| Whole fruits | 44.1 (39.1, 49.0) | 4.2 (−2.1, 10.5) | 7.3 (1.9, 12.6)b | 9.2 (1.3, 17.1)b | 7.6 (0.4, 14.8)b |
| Total veg | 62.5 (59.7, 65.4) | −3.7 (−8.6, 1.1) | −3.3 (−8.3, 1.8) | 9.8 (5.2, 14.4)b | 7.1 (2.5, 11.8)b |
| Greens/beans | 37.9 (32.5, 43.3) | −5.5 (−14.1, 3.2) | −5.4 (−13.9, 3.2) | 15.1 (7.6, 22.6)b | 11.7 (4.1, 19.3)b |
| Whole grains | 26.6 (23.1, 30.1) | −1.4 (−4.6, 1.7) | 0.3 (−3.4, 3.9) | 5.5 (−0.0, 11.0) | 4.4 (−0.6, 9.4) |
| Dairy | 49.1 (46.2, 52.1) | 2.3 (−1.6, 6.3) | 0.8 (−3.2, 4.8) | 2.1 (−1.8, 6.0) | 0.5 (−3.4, 4.3) |
| Total protein | 89.7 (87.9, 91.6) | 0.4 (−1.6, 2.3) | 0.6 (−1.0, 2.2) | 2.8 (−0.1, 5.6) | 2.9 (0.1, 5.7)b |
| Seafood/plant proteins |
54.1 (49.5, 58.7) | 1.4 (−4.3, 7.2) | 2.2 (−3.7, 8.1) | 11.3 (6.7, 15.8)b | 8.6 (3.4, 13.8)b |
| Fatty acids | 46.1 (43.1, 49.2) | 0.8 (−4.4, 6.1) | 1.1 (−3.8, 6.1) | 5.2 (1.6, 8.7)b | 4.2 (−0.1, 8.5) |
| Refined grains | 61.3 (56.7, 66.0) | −1.6 (−7.5, 4.3) | -0.1 (−6.8, 6.5) | 4.2 (−2.9, 11.3) | 5.2 (−2.4, 12.9) |
| Sodium | 42.7 (39.7, 45.7) | 0.5 (−3.3, 4.3) | 3.8 (0.2, 7.4)b | −6.3 (−11.3, −1.2)b | −2.6 (−7.6, 2.3) |
| Added sugars | 69.2 (66.3, 72.0) | −1.7 (−5.0, 1.7) | −2.6 (−5.6, 0.5) | 8.0 (2.4, 13.7)b | 5.1 (−0.2, 10.5) |
| Saturated fats | 52.6 (48.4, 56.7) | −0.2 (−6.0, 5.6) | 0.4 (−4.8, 5.6) | 1.5 (−4.4, 7.4) | 1.8 (−3.9, 7.5) |
Adjusted for age, sex, education, family income level, total diet-related comorbidities, weight goals, weight status, meals away from home, smoking, and recreational physical activity.
indicates 95% CIs that do not contain the null value.
HEI-2015, Health Eating Index 2015
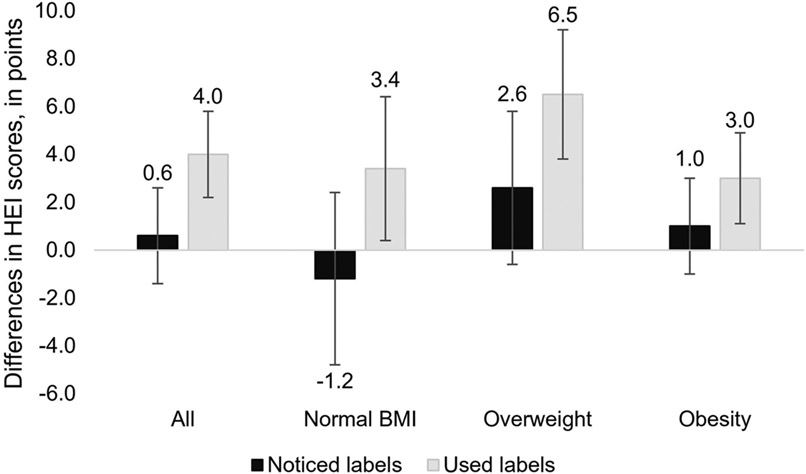
When stratified by weight status, unadjusted mean HEI-2015 total scores for adults who did not notice labels with normal BMI was 54.1 (SD=2.5), with overweight was 51.7 (SD=1.9), and with obesity was 49.3 (SD=1.1). The interaction between label use and weight status was significant (p=0.0004). In stratified analyses within subsamples of weight status, those who used labels had higher HEI-2015 total scores than those who did not notice labels regardless of whether they had normal BMI (adjusted difference=3.4; 95% CI=0.2, 6.7), overweight (adjusted difference=6.5; 95% CI=3.6, 9.5), or obesity (adjusted difference=3.0; 95% CI=1.0, 5.1). Those who noticed labels did not have different HEI-2015 total scores compared with those who did not notice labels, regardless of weight status (Figure 1).
Figure 1.
Adjusted differences in Healthy Eating Index 2015 scores with 95% CIs in noticed labels group and used labels group compared with those who did not notice labels by weight status
Note: Models were adjusted for age, sex, education, family income level, total diet-related comorbidities, smoking, and recreational physical activity. Unadjusted mean HEI-2015 scores in those who did not notice labels were as follows: All 51.3 (SD=1.4), normal BMI 54.1 (SD=2.5), overweight 51.7 (SD=1.9), and obesity 49.3 (SD=1.1).
HEI-2015, Healthy Eating Index 2015.
DISCUSSION
When purchasing food from restaurants, American adults who reported using menu calorie labels had healthier overall diet quality than adults who did not notice any calorie labels, as shown by modestly higher HEI-2015 scores. Specifically, individuals who reported using labels had greater intake of fruits, vegetables, and healthy proteins. Individuals who used menu calorie labels had higher diet quality than those who did not notice menu labels, regardless of weight status. This suggests that calorie labeled menus may improve food choices among individuals seeking lower-calorie menu selections. Adults who noticed but did not use menu calorie labels reported similar diet quality as those who did not notice labels, suggesting that calorie labels are beneficial only in those who actively use them to guide decisions.
These findings suggested higher menu calorie label use nationally than prior studies. A prior NHANES study found growing consumer use of menu calorie labels from 2007 to 2014, with increases from 7.8% to 18.1% in fast-food restaurant visits and increases from 8.3% to 13.6% in sit-down restaurant visits.45 In this study with data from 2017 to 2018, menu calorie label use was higher at 27.3%, which may be related to increasing prevalence of labels over time and expansion to additional restaurant settings like coffee shops and buffets. Before activation of the ACA mandate, 71% of the top 90 restaurant chains in the U.S. had partially or fully implemented labeling,46 and after the mandate went into effect, this grew to 94% among 197 top restaurant chains.47 Menu calorie label use examined in Philadelphia showed that individuals with obesity had similar to greater rates of label use as those with normal weight.32 In this analysis, weight status was not correlated with the use of menu calorie labels.
Although the rates of label use may be rising, >70% of adults continue to report not using or noticing menu calorie labels. Possible explanations for this may be that some individuals prioritize either taste or value over health in food ordering, believe they already know what foods are calorie-dense, or find calorie labels difficult to use because of low healthy literacy or numeracy.48,49 Hence, complementary labeling approaches that address cognitive barriers should be explored.
To address obesity, use of menu calorie labels should extend beyond decreasing calorie quantity to increasing diet quality. Unlike most prior studies that focus on caloric quantity, this study focused on the association between labels and diet quality. Increased label use was associated with increased fruit and vegetable intake, even after adjusting for other health-related behaviors correlated with diet quality. This suggests that menu labels may improve general dietary intake, through both diet quality and calorie quantity. A prior study demonstrated that menu calorie labels with a daily recommended calorie intake statement decreased caloric consumption during and after a labeled meal compared with no labels, suggesting that ACA-mandated menu calorie labels can have spillover effects that improve dietary intake.50 A prior study found that implementation of menu calorie label laws was associated with a 1.5% decrease in BMI and 12% reduction in obesity risk in participants surveyed by the Behavioral Risk Factor Surveillance System.51 Population-wide, the national menu calorie label law is projected to reduce risk of cardiometabolic morbidity and mortality.52 These findings together demonstrate that the effects of menu calorie labels, through improving diet quality and calorie intake, may prevent obesity and chronic disease at the population level. As menu calorie labels become more prevalent in the U.S. because of the ACA, elucidating the mechanisms through which calorie labels influence individual's diet and extend their effects outside of labeled meals can help improve their reach and effectiveness.
When stratified by weight status, menu calories labels were associated with higher diet quality among those with normal BMI, overweight, or obesity. This suggests that individuals with different weight statuses can benefit from menu calorie labels, which is important for the prevention and mitigation of overweight and obesity. The fact that menu calorie labels are reaching a subpopulation of adults regardless of weight status shows that they may have a role in public health and chronic disease prevention.
This study has limitations. Because NHANES data are cross-sectional, associations from this analysis may not be causal; that is, people who have higher dietary quality may be more likely to take note of menu calorie labels. In addition, dietary recall data used to calculate diet quality may not correspond to the same day as the exposure to the menu calorie label, because it does not capture time lags between when participants were exposed to labels and when diet quality was measured. The method of assessing menu calorie label exposure in the most recent visit does not differentiate a participant visiting a restaurant that does not have menu calorie labels from a participant who does not notice labels when they are present nor does it capture an individual's typical exposure to menu calorie labels, leading to potential misclassification that could bias results toward the null. Dietary recall data also has inherent bias, including under-reporting of unhealthy dietary components among adults with overweight and obesity.53 Dietary comorbidities may have been underestimated owing to missing data, partly because of NHANES asking for certain comorbidities only for adults aged ≥20 years. Lastly, there is likely residual confounding in the relationship between menu calorie label use and diet quality, although the analysis adjusted for important demographic, socioeconomic, behavioral, and medical characteristics that are all related to diet quality.
CONCLUSIONS
Americans eat one in three meals outside the home, creating a growing opportunity to offer guidance on healthier food choices at restaurants to enhance public health. U.S. adults who noticed menu calorie labels in restaurants reported healthier diet quality than those who were unexposed to or did not notice calorie labels, after adjusting for sociodemographic and medical factors and health behaviors. This difference was driven by an increased intake of healthy dietary components, particularly fruits, vegetables, and healthy proteins. This association was robust regardless of weight status, suggesting that menu calorie labels may be an acceptable strategy to help some adults make behavioral changes. To maximize the utility of these point-of-purchase labels, further research should focus on why individuals notice or use calorie labels and which types of menu labels are effective for those who are most vulnerable to weight gain.
Supplementary Material
ACKNOWLEDGMENTS
Funding sources did not play any role in study design; data collection, analysis, or interpretation; writing the manuscript; or the decision to submit the manuscript for publication. The research presented in this paper is that of the authors and does not reflect the official policy of NIH.
LV reported receiving grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development during the conduct of the study.
JAL reported receiving grants from the National Institute on Aging (P30AG059988, R01AG069762, R01AG074245, P30AG024968, R01AG070054, R33AG057395) and the Agency for Healthcare Research and Quality (R01HS026506, R01HS028127).
RTA reported receiving grants from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Aging, and Centers for Disease Control and Prevention during the conduct of the study. NRK reported receiving grants from the National Heart, Lung, and Blood Institute (K24HL155897) and the National Cancer Institute during the conduct of the study. MJO reported receiving grants from the National Institute of Diabetes and Digestive and Kidney Diseases (P30-DK092949) during the conduct of the study. No other conflicts of interest were reported by the authors of this paper.
Footnotes
No financial disclosures have been reported by the authors of this paper.
CREDIT AUTHOR STATEMENT
Jenny Jia: Conceptualization, Methodology, Software, Writing – original draft, Visualization. Linda Van Horn: Conceptualization, Writing – review & editing. Jeffrey A. Linder: Writing – review & editing. Ronald T. Ackermann: Writing – review & editing. Namratha R. Kandula: Methodology, Writing – review & editing. Matthew J. O'Brien: Conceptualization, Methodology, Writing – review & editing.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2023.07.003
REFERENCES
- 1.Saksena MJ, Okrent AM, Anekwe TD, et al. America’s eating habits: food away from home. https://www.ers.usda.gov/webdocs/publications/90228/eib-196.pdf?v=4969.3. Accessed June 2, 2023. [Google Scholar]
- 2.Division of Nutrition and Physical Activity. Do increased portion sizes affect how much we eat? Research to Practice No. 2. Centers for Disease Control and Prevention. https://www.cdc.gov/nccdphp/dnpa/nutrition/pdf/portion_size_research.pdf. Accessed June 2, 2023. [Google Scholar]
- 3.Piacenza J. Americans are actually pretty good at counting calories. Morning Consult. https://morningconsult.com/2018/07/18/americans-actually-pretty-good-counting-calories/. Accessed May 25, 2023.
- 4.Todd JE, Mancino L, Lin B-H. The Impact of Food Away From Home on Adult Diet Quality (USDA-ERS Economic Research Report Paper No. 90). https://www.ers.usda.gov/webdocs/publications/46352/8170_err90_1_pdf. Accessed May 25, 2023. [Google Scholar]
- 5.Gould S. 6 charts that show how much more Americans eat than they used to. https://www.businessinsider.com/daily-calories-americans-eat-increase-2016-07. Accessed May 25, 2023. [Google Scholar]
- 6.Food and Agriculture Organization of the United Nations, Data, FAO-STAT (Statistical Database), 2013, Rome, Italy. https://www.fao.org/faostat/en/#data. Accessed June 2, 2023. [Google Scholar]
- 7.Dietary guidelines for Americans 2020–2025. Department of Health and Human Services, Department of Agriculture. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf. Accessed May 25, 2023.
- 8.Drozdz D, Alvarez-Pitti J, W'ojcik M, et al. Obesity and cardiometabolic risk factors: from childhood to adulthood. Nutrients. 2021;13 (11):4176. 10.3390/nu13114176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Church T, Martin CK. The obesity epidemic: a consequence of reduced energy expenditure and the uncoupling of energy intake? Obesity (Silver Spring). 2018;26(1):14–16. 10.1002/oby.22072. [DOI] [PubMed] [Google Scholar]
- 10.Inoue Y, Qin B, Poti J, Sokol R, Gordon-Larsen P. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. 2018;7(4):276–288. 10.1007/s13679-018-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381 (25):2440–2450. 10.1056/NEJMsa1909301. [DOI] [PubMed] [Google Scholar]
- 12.O’Hearn M, Lauren BN, Wong JB, Kim DD, Mozaffarian D. Trends and disparities in cardiometabolic health among U.S. adults, 1999-2018. J Am Coll Cardiol. 2022;80(2):138–151. 10.1016/j.jacc.2022.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright B, Bragge P. Interventions to promote healthy eating choices when dining out: a systematic review of reviews. Br J Health Psychol. 2018;23(2):278–295. 10.1111/bjhp.12285. [DOI] [PubMed] [Google Scholar]
- 14.Food and Drug Administration. Food labeling; nutrition labeling of standard menu items in restaurants and similar retail food establishments (79 FR 71155). Fed Regist. https://www.federalregister.gov/documents/2014/12/01/2014-27833/food-labeling-nutrition-labeling-of-standard-menu-items-in-restaurants-and-similar-retail-food. Accessed June 2, 2023. [PubMed] [Google Scholar]
- 15.Long MW, Tobias DK, Cradock AL, Batchelder H, Gortmaker SL. Systematic review and meta-analysis of the impact of restaurant menu calorie labeling. Am J Public Health. 2015;105(5):e11–e24. 10.2105/AJPH.2015.302570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reale S, Flint SW. Menu labelling and food choice in obese adults: a feasibility study. BMC Obes. 2016;3(1):17. 10.1186/s40608-016-0095-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petimar J, Ramirez M, Rifas-Shiman SL, et al. Evaluation of the impact of calorie labeling on McDonald’s restaurant menus: a natural experiment. Int J Behav Nutr Phys Act. 2019;16(1):99. 10.1186/s12966-019-0865-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernandes AC, Oliveira RC, Proenc a RP, Curioni CC, Rodrigues VM, Fiates GM. Influence of menu labeling on food choices in real-life settings: a systematic review. Nutr Rev. 2016;74(8):534–548. 10.1093/nutrit/nuw013. [DOI] [PubMed] [Google Scholar]
- 19.VanEpps EM, Roberto CA, Park S, Economos CD, Bleich SN. Restaurant menu labeling policy: review of evidence and controversies. Curr Obes Rep. 2016;5(1):72–80. 10.1007/s13679-016-0193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood). 2009;28(6):w1110–w1121. 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 21.Vandevijvere S, Vanderlee L. Effect of formulation, labelling, and taxation policies on the nutritional quality of the food supply. Curr Nutr Rep. 2019;8(3):240–249. 10.1007/s13668-019-00289-x. [DOI] [PubMed] [Google Scholar]
- 22.Petimar J, Zhang F, Rimm EB, et al. Changes in the calorie and nutrient content of purchased fast food meals after calorie menu labeling: a natural experiment. PLoS Med. 2021;18(7):e1003714. 10.1371/journal.pmed.1003714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grummon AH, Petimar J, Soto MJ, et al. Changes in calorie content of menu items at large chain restaurants after implementation of calorie labels. JAMA Netw Open. 2021;4(12):e2141353. 10.1001/jamanetworkopen.2021.41353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rizza W, Veronese N, Fontana L. What are the roles of calorie restriction and diet quality in promoting healthy longevity? Ageing Res Rev. 2014;13:38–45. 10.1016/j.arr.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Jacob R, Bertrand C, Llewellyn C, et al. Dietary mediators of the genetic susceptibility to obesity-results from the Quebec family study. J Nutr. 2022;152(1):49–58. 10.1093/jn/nxab356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gardner CD, Trepanowski JF, Del Gobbo LC, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA. 2018;319(7):667–679. 10.1001/jama.2018.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bleich SN, Economos CD, Spiker ML, et al. A systematic review of calorie labeling and modied calorie labeling interventions: impact on consumer and restaurant behavior. Obesity (Silver Spring). 2017;25 (12):2018–2044. 10.1002/oby.21940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiszko KM, Martinez OD, Abrams C, Elbel B. The influence of calorie labeling on food orders and consumption: a review of the literature. J Community Health. 2014;39(6):1248–1269. 10.1007/s10900-014-9876-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crockett RA, King SE, Marteau TM, et al. Nutritional labelling for healthier food or non-alcoholic drink purchasing and consumption. Cochrane Database Syst Rev. 2018;2(2):CD009315. 10.1002/14651858.CD009315.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asghari G, Mirmiran P, Yuzbashian E, Azizi F. A systematic review of diet quality indices in relation to obesity. Br J Nutr. 2017;117(8):1055–1065. 10.1017/S0007114517000915. [DOI] [PubMed] [Google Scholar]
- 31.Christensen EL, Harding IH, Voigt K, Chong TTJ, Verdejo-Garcia A. Neural underpinnings of food choice and consumption in obesity. Int J Obes (Lond). 2022;46(1):194–201. 10.1038/s41366-021-00974-4. [DOI] [PubMed] [Google Scholar]
- 32.Breck A, Cantor J, Martinez O, Elbel B. Who reports noticing and using calorie information posted on fast food restaurant menus? Appetite. 2014;81:30–36. 10.1016/j.appet.2014.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Christoph MJ, Larson N, Laska MN, Neumark-Sztainer D. Nutrition facts panels: who uses them, what do they use, and how does use relate to dietary intake? J Acad Nutr Diet. 2018;118(2):217–228. 10.1016/j.jand.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Food Surveys Research Group, AMPM. USDA automated multiple-pass method. Agricultural Research Service, U.S. Department of Agriculture. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/ampm-usda-automated-multiple-pass-method/. Accessed June 2, 2023. [Google Scholar]
- 35.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National Health and Nutrition Examination Survey: plan and operations. National Center for Health Statistics. https://www.cdc.gov/nchs/data/series/sr_01/sr01_056.pdf. Accessed June 2, 2023. [PubMed] [Google Scholar]
- 36.National health and nutrition examination survey, 2017–2018 Data Documentation, Codebook, and Frequencies: Consumer Behavior Phone Follow-Up Module - Adult (CBQPFA_J). https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/CBQPFA_J.htm. Accessed June 2, 2023.
- 37.U.S. Department of Health and Human Services, U.S. Department of Agriculture. Dietary Guidelines for Americans. https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf. Updated July 28, 2020. Accessed July 10, 2020.
- 38.Kirkpatrick SI, Reedy J, Krebs-Smith SM, et al. Applications of the Healthy Eating Index for surveillance, epidemiology, and intervention research: considerations and caveats. J Acad Nutr Diet. 2018;118 (9):1603–1621. 10.1016/j.jand.2018.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. 10.1016/j.jand.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reedy J, Lerman JL, Krebs-Smith SM, et al. Evaluation of the healthy eating Index-2015. J Acad Nutr Diet. 2018;118(9):1622–1633. 10.1016/j.jand.2018.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Division of Cancer Control and Population Sciences, National Cancer Institute. The Healthy Eating Index: SAS code. National Cancer Institute. https://epi.grants.cancer.gov/hei/sas-code.html. Accessed June 2, 2023. [Google Scholar]
- 42.Jia J, Fung V, Meigs JB, Thorndike AN. Food insecurity, dietary quality, and health care utilization in lower-income adults: a cross-sectional study. J Acad Nutr Diet. 2021;121(11):2177–2186 .e3. 10.1016/j.jand.2021.06.001. [DOI] [PubMed] [Google Scholar]
- 43.Whitfield GP, Ussery EN, Carlson SA. Combining data from assessments of leisure, occupational, household, and transportation physical activity among US adults, NHANES 2011–2016. Prev Chronic Dis. 2020;17:E117. 10.5888/pcd17.200137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim Y, Canada JM, Kenyon J, et al. Physical activity, sedentary behaviors and all-cause mortality in patients with heart failure: findings from the NHANES 2007–2014. PLoS One. 2022;17(7):e0271238. 10.1371/journal.pone.0271238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Feng W, Fox A. Menu labels, for better, and worse? Exploring socioeconomic and race-ethnic differences in menu label use in a national sample. Appetite. 2018;128:223–232. 10.1016/j.appet.2018.06.015. [DOI] [PubMed] [Google Scholar]
- 46.Cleveland LP, Simon D, Block JP. Compliance in 2017 with federal calorie labeling in 90 chain restaurants and 10 retail food outlets prior to required implementation. Am J Public Health. 2018;108(8):1099–1102. 10.2105/AJPH.2018.304513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cleveland LP, Simon D, Block JP. Federal calorie labelling compliance at US chain restaurants. Obes Sci Pract. 2020;6(2):207–214. 10.1002/osp4.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.VanEpps EM, Downs JS, Loewenstein G. Calorie label formats: using numeric and traffic light calorie labels to reduce lunch calories. J Public Policy Mark. 2016;35(1):26–36. 10.1509/jppm.14.112. [DOI] [Google Scholar]
- 49.Berry C, Burton S, Howlett E, Newman CL. Understanding the calorie labeling paradox in chain restaurants: why menu calorie labeling alone may not affect average calories ordered. J Public Policy Mark. 2019;38 (2):192–213. 10.1177/0743915619827013. [DOI] [Google Scholar]
- 50.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–318. 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Restrepo BJ. Calorie labeling in chain restaurants and body weight: evidence from New York. Health Econ. 2017;26(10):1191–1209. 10.1002/hec.3389. [DOI] [PubMed] [Google Scholar]
- 52.Liu J, Mozaffarian D, Sy S, et al. Health and economic impacts of the national menu calorie labeling law in the United States: a Microsimulation Study. Circ Cardiovasc Qual Outcomes. 2020;13(6):e006313. 10.1161/CIRCOUTCOMES.119.006313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lissner L. Measuring food intake in studies of obesity. Public Health Nutr. 2002;5(6A):889–892. 10.1079/PHN2002388. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.