Against a background of high rates of teenage pregnancy and an increasing prevalence of sexually transmitted infections, the sexual conduct of young people is vigorously debated. Many teenagers later say that they had sexual intercourse “too early”—but should doctors be advising young people to abstain from sex? Trevor Stammers, who is a tutor in general practice and an author and broadcaster on sexual health, and Roger Ingham, who has done research on sexual conduct and sex education in Britain and other countries, consider whether advising abstinence is an effective response to declining teenage sexual health.
Recent trends in adolescent sexual health in the United Kingdom are cause for concern. In England alone, almost 90 000 teenagers became pregnant in 1997. Slightly fewer than 7700 of these girls were less than 16 years old, and about half had abortions.1-1 In 1995-7, the rate of increase in gonorrhoea among 16-19 year olds was 45%—the highest increase seen in any age group. During the same period and in the same age group, the incidence of chlamydia rose by 53% and that of genital warts by 25%.1-1 Early intercourse often leads to subsequent regret: only two fifths of respondents in a recent study indicated that first intercourse occurred “at about the right time”; 45% of girls and 32% of boys indicated that it had happened too early or should never have happened at all.1-2 Sexually active teenagers are more likely to be emotionally hurt (figure) and have an increased risk of depression and suicide.1-3
Contraception in not enough
These indices reflect the outcome of years of unprecedented availability of contraception among young people and increasing sex education in schools. Contraception as the cornerstone of sexual health promotion for adolescents has manifestly failed. In almost 15 years of general practice I have never seen a single case of unplanned pregnancy resulting from ignorance about or unavailability of contraception. Up to 80% of unplanned pregnancies result from failed contraception.1-4 Data from 1975-91 show a positive correlation between increasing rates of use of condoms at first intercourse and higher rates of teenage conceptions.1-4 Oral contraceptives, while providing the greatest protection from unplanned pregnancy, offer no protection against sexually transmitted diseases and may actually increase the risk of cervicitis.
The younger the age of first intercourse, the greater the risks involved. Early teenage sex is associated with poor use of contraception as well as multiple sexual partners and increased rates of depression and suicide, and it is often part of a wider spectrum of harmful behaviour that includes substance abuse, smoking, and excessive alcohol consumption.1-3 Young people who start having intercourse before they are 16 are three times more likely to become teenage parents than those who wait.1-1
Abstinence makes sense
I am not the first doctor to say in this journal that “sexual activity is far from appropriate” for young teenagers.1-3 It is widely recognised that delaying the onset of intercourse is an important objective in assessing the effectiveness of sexual health promotion and sex education programmes. Medical journals in the United States (where teenage pregnancy rates are now falling) regularly publish articles encouraging healthcare professionals to recommend abstinence and giving detailed advice on how to do so most effectively.1-5 One recent article states, “Abstinence is the greatest sexual health promotion behaviour available to Americans, especially to adolescents.”1-6
Abstinence is effective
The evidence is becoming clearer too that a thoughtful, reasoned advocacy of abstinence does work. A recent overview cites several studies of abstinence programmes showing “a sharp reduction in the number of pregnancies” and that “women who were not participants in the course were as much as fifteen times more likely to have begun sex than were the participants.”1-7 The first randomised controlled trial of an abstinence intervention in the United States showed that participants were less likely to report having sexual intercourse at three, six, and 12 months (though this was statistically significant only at three months.) This abstinence programme provided accurate information, portrayed sex in a positive light, and was not “moralistic.” Although its undoubted effectiveness diminished with longer term follow up, the authors concluded that “future research must seek to increase the longevity of these promising effects.”1-8
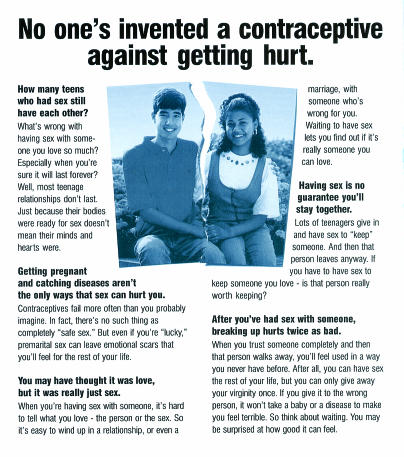
Figure.
“You didn't get pregnant. You didn't get AIDS. So why do you feel so bad?” says the first page of this leaflet produced by US Department of Health and Human Services
Any total abstinence programme will be at a disadvantage when compared with “safer sex” education because abstinence, unlike condom use, runs against the tide of peer pressure. Much, if not most, adolescent sexual activity is about the expression of non-sexual needs.1-9 First intercourse is rarely about love; it is often about peer pressure and the need to conform to it. The strongest predictor of frequency of sexual intercourse among teenagers is the influence of peers.1-9 Effective promotion of abstinence involves equipping teenagers to resist such pressure.
Encouraging parents
This is where parents make such a vital difference. A recent study of over 400 adolescents clearly showed that where parents, especially mothers, were the major source of sexual information, their adolescents' sexual behaviour was less risky.1-10 Those adolescents who reported discussing a greater number of sex based topics with their mothers were more likely to express conservative attitudes about sex and were less likely to have engaged in it. Doctors promoting abstinence for teenagers should encourage parents to talk with their children about sex and be able to recommend resources to help them to do so.1-11,1-12 Parents in the Netherlands communicate much more with their children about sex,1-1 and this may contribute as much to teenage sexual health there as the more usually cited school sex education.
Realistic promotion of abstinence is not the mere mouthing of platitudes such as “Just say ‘No’!” Teenagers often view abstinence as a threat to the development of intimate relationships and will require convincing reasons to regard abstinence as a positive choice for sexual health. They need to understand why there is ultimately no such thing as casual sex—except in the same sense as casual theft. It may be casual in intent but never in its consequences. Sex education should have its prime focus not on contraceptives but rather on sex as a means of communication. Teenagers should be encouraged to think about what they are communicating by their sexual activity and what kinds of relationships are appropriate for varying degrees of sexual intimacy.
Easier availability of contraception and more explicit sex education at an earlier age are tired and inadequate responses to declining teenage sexual health. Great sex involves abandonment and restraint, the excitement of anticipation as well as the thrill of release. The discipline of abstinence in teenage years is a good preparation for fulfilling sex in later life. Doctors should encourage adolescents to avoid early sexual intercourse so that they can enjoy better long term sexual health.—Trevor Stammers
Footnotes
Competing interests: TS is a trustee of Family Education Trust and Family and Youth Concern, London.
References
- 1-1.Department of Health. Teenage pregnancy. London: Social Exclusion Unit, Department of Health; 1999. www.cabinet-office.gov.uk/seu (accessed 20 August 2000). [Google Scholar]
- 1-2.Wright D, Henderson M, Raab G, Abraham C, Buston K, Scott S, et al. Extent of regretted sexual intercourse among young teenagers in Scotland: a cross sectional survey. BMJ. 2000;320:1243–1244. doi: 10.1136/bmj.320.7244.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1-3.Stuart-Smith S. Teenage sex. BMJ. 1996;312:390–391. doi: 10.1136/bmj.312.7028.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1-4.Williams ES. Contraceptive failure may be a major factor in teenage pregnancy. BMJ. 1995;311:807. doi: 10.1136/bmj.311.7008.806b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1-5.Kay L. Adolescent sexual intercourse; strategies for promoting abstinence in teens. Postgrad Med. 1995;97:121–134. [PubMed] [Google Scholar]
- 1-6.Beitz JM. Sexual health promotion in adolescents and young adults: primary prevention strategies. Holist Nurs Pract. 1998;12:27–37. doi: 10.1097/00004650-199801000-00006. [DOI] [PubMed] [Google Scholar]
- 1-7.Genuis SJ, Genuis SK. Adolescent sexual involvement: time for primary prevention. Lancet. 1995;345:240–241. doi: 10.1016/s0140-6736(95)90229-5. [DOI] [PubMed] [Google Scholar]
- 1-8.Jemmott JB, Jemmott LS, Fong GT. Abstinence and safer-sex HIV reduction interventions for African American adolescents. JAMA. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- 1-9.Cohen MW. Adolescent sexual activity as an expression of nonsexual needs. Pediatr Ann. 1995;24:324–329. doi: 10.3928/0090-4481-19950601-10. [DOI] [PubMed] [Google Scholar]
- 1-10.DiLorio C, Kelley M, Hockenberry-Eaton M. Communication about sexual issues: mothers, fathers and friends. J Adolesc Health. 1999;24:181–189. doi: 10.1016/s1054-139x(98)00115-3. [DOI] [PubMed] [Google Scholar]
- 1-11.Pollard N. Why do they do that?—Understanding teenagers. Oxford: Lion; 1998. [Google Scholar]
- 1-12.Chalke S, Page N. Sex matters. London: Hodder; 1996. [Google Scholar]
Sexual conduct among young people remains a vigorously debated issue. Rates of teenage pregnancy are high in the United Kingdom, and sexually transmitted infections are increasingly prevalent in this age group.2-1 At a psychological level, there is evidence that some young people, especially young women, express regret about the circumstances of their early sexual experiences.2-2,2-3 I am sure that Dr Stammers and I agree completely about the importance of recognising these concerns and the need to respond to them. Where we disagree, however, is over how we should respond and the extent to which personal agendas should affect professional behaviour.
Research into sexual health was uncommon until recently, and views on how doctors and others should respond to young people's sexual conduct were based on personal opinion or religious beliefs, or both. However, the advent of HIV and the increasing concerns about teenage conceptions encouraged funding bodies and scientists to realise that good research was needed into sexual conduct and its relation to physical and psychological health outcomes. Consequently, we now have a clearer understanding of sexual conduct and what does and does not “work.” Our understanding is not complete, but it is certainly better than it was.
What is certain is that we can no longer, in a traditionally confused British way, ignore young people's sexuality and hope that it will just go away. We have to make a choice. In stark terms, the choice is between encouraging abstinence or promoting greater openness in homes, schools, health services, and other settings in order to improve individual knowledge and skills.
Dealing with coercion
The regret expressed by some young people about their early sexual experiences is often related to coercion and pressure—generally that exerted by young men on young women but also occurring within peer groups of both sexes. This can be dealt with by enabling and encouraging young people to be more articulate in expressing their views about what they feel comfortable or uncomfortable doing or not doing, and through encouraging respect for others and for themselves. Merely advising young people not to have sex will not develop these skills.
Better training and services
We know that there are some powerful barriers to use of the health service. These include issues of access and availability, confidentiality, and what are perceived to be disapproving attitudes on the part of staff.2-4 We can deal with this by improving publicity and accessibility, and through training all relevant staff to be welcoming, non-judgmental, and respectful of confidentiality. After levels of deprivation are controlled for, urban areas in which young people have greater access to specialist services are associated with lower rates of teenage conceptions.2-5
Many young people feel let down by adults, especially those who “preach” to them. They want—as, in fact, do most of their parents—earlier, more open, and less biological sex education, and they want more suitable services.2-6,2-7 What rights have professionals to deny young people the opportunity to form relationships and to express their feelings safely in ways that they choose to? We need to accept that in matters of health protection young people have a right to express their views and have them taken into account. This approach, as well as being supported by research data, is compatible with the United Nations' convention on the rights of the child.2-8
An open approach
Doctors, along with others, can and should advise on effective use of contraception and can try to ensure that people are acting in full awareness of the risks involved and are not being subject to pressure or coercion. A policy of advising teenagers simply not to have sex runs the risk that they will become even more alienated from adults and that they will be less likely to use the services available, leading to greater rather than lower risks.
Several countries in Europe, including Norway, Sweden, Denmark, Germany, and the Netherlands, which have teenage conception rates considerably lower than those in the United Kingdom have an earlier and more open approach to sexual issues in schools and in families. This is associated, in the Netherlands at least, with greater levels of discussion and forward planning between partners, later ages at first sexual intercourse, more effective contraceptive use, and lower levels of subsequent regret.2-9
A more open approach to sexual conduct need not be value free—an accusation often levelled by the more conservative organisations. Sex and relationship education can and must be based on values of respect and mutuality, whether or not these are located within specific religious or cultural frameworks.
Personal versus professional stance
Dr Stammers is a trustee of an organisation called Family and Youth Concern (the working title of the Family Education Trust). This small organisation has a history of vociferous campaigning against school sex education and young people's sexual health services. It recently described the British Pregnancy Advisory Service's initiative to make emergency contraception more available as “reckless” and dismissed the Social Exclusion Unit's report on teenage pregnancy as making “tragic reading,” advocating in its stead a return to family values and abstinence.2-10 In a recent article in the Daily Mail, Dr Stammers said: “Today, many sex education teachers are in effect saying: ‘don’t bother to be good. Be careful . . . and here is how to do it.' ”2-11 Unsurprisingly, no reference is cited to support this statement.
As the Social Exclusion Unit's report on teenage pregnancy made clear, poor sexual health among young people is a complex issue and is to some extent related to broader inequalities within our society that may take some time to address.2-12 Meanwhile, many people in health and education services and in the youth and voluntary sectors in the United Kingdom are making strenuous efforts to improve the sexual health of young people by teaching about responsibility and good personal relationships. They are immensely dedicated and sincere in their efforts. “Sexual health experts” (so called by the Daily Mail) who attempt to promulgate their own personal and moral values under the guise of scientifically based medical opinion do not help this work.—Roger Ingham
Footnotes
Competing interests: None declared.
References
- 2-1.Nicoll A, Catchpole M, Cliffe S, Hughes G, Simms I, Thomas D. Sexual health of teenagers in England and Wales: analysis of national data. BMJ. 1999;318:1321–1322. doi: 10.1136/bmj.318.7194.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2-2.Wight D, Henderson M, Raab G, Abraham C, Buston K, Scott S, Hart G. Extent of regretted sexual intercourse among young teenagers in Scotland: a cross sectional survey. BMJ. 2000;320:1243–1244. doi: 10.1136/bmj.320.7244.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2-3.Dickson N, Paul C, Herbison P, Silva P. First sexual intercourse: age, coercion and later regrets reported by a birth cohort. BMJ. 1998;316:29–33. doi: 10.1136/bmj.316.7124.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2-4.Pearson S, Cornah D, Diamond I, Ingham R, Peckham S, Hyde M. Promoting young people's sexual health services. Southampton: Centre for Sexual Health Research, University of Southampton; 1996. . (Report commissioned by the Health Education Authority.) [Google Scholar]
- 2-5.Diamond I, Clements S, Stone N, Ingham R. Spatial variation in teenage conceptions in south and west England. J R Statist Soc A. 1999;162:273–289. [Google Scholar]
- 2-6.Health Education Authority and National Foundation for Educational Research. Parents, schools and sex education—a compelling case for partnership. London: Health Education Authority; 1994. [Google Scholar]
- 2-7.Stone N, Ingham R, Carrera C. Factors affecting sex and sexuality education in and out of school. Final report. Southampton: Centre for Sexual Health Research, University of Southampton; 1998. [Google Scholar]
- 2-8.United Nations. The convention on the rights of the child. Ratification and accession by General Assembly resolution 44/25 of 20 November 1989. New York: United Nations; 1989. [Google Scholar]
- 2-9.Ingham R. Development of an integrated model of sexual conduct amongst young people. Swindon: Economic and Social Science Research Council; 1977. . (Senior research fellowship end of award report No H53427501495.) [Google Scholar]
- 2-10.Family and Youth Concern. Family bulletin. Oxford: Family and Youth Concern; 1999. p. 96. [Google Scholar]
- 2-11.Stammers T. Fear works better than condoms. Daily Mail 21 October 1999:12.
- 2-12.Social Exclusion Unit. Teenage pregnancy. London: Stationery Office; 1999. . (Cmnd 3432.) [Google Scholar]